Abstract
Two frequently encountered but underrecognized challenges for causal inference in studying the long-term health effects of disasters among survivors include 1) time-varying effects of disasters on a time-to-event outcome and 2) selection bias due to selective attrition. In this paper, we review approaches for overcoming these challenges and demonstrate application of the approaches to a real-world longitudinal data set of older adults who were directly affected by the 2011 Great East Japan Earthquake and Tsunami (n = 4,857). To illustrate the problem of time-varying effects of disasters, we examined the association between degree of damage due to the tsunami and all-cause mortality. We compared results from Cox regression analysis assuming proportional hazards with those derived using adjusted parametric survival curves allowing for time-varying hazard ratios. To illustrate the problem of selection bias, we examined the association between proximity to the coast (a proxy for housing damage from the tsunami) and depressive symptoms. We corrected for selection bias due to attrition in the 2 postdisaster follow-up surveys (conducted in 2013 and 2016) using multivariable adjustment, inverse probability of censoring weighting, and survivor average causal effect estimation. Our results demonstrate that analytical approaches which ignore time-varying effects on mortality and selection bias due to selective attrition may underestimate the long-term health effects of disasters.
Keywords: causal inference, disasters, inverse probability weighting, selection bias, standardization, survival analysis, survivor average causal effect
Abbreviations
- CI
confidence interval
- IPCW
inverse probability of censoring weighting
- IPTW
inverse probability of treatment weighting
- JAGES
Japan Gerontological Evaluation Study
- RR
risk ratio
- SACE
survivor average causal effect
Major disasters not only cause immediate injury and loss of life but also appear to elevate the risk of long-term adverse physical and mental health outcomes among disaster survivors (1). Evidence on the lingering, long-term health sequelae of disaster exposure during the months and years following disasters has begun to accumulate (2–8). However, accurate assessment of long-term health consequences of a disaster among survivors is often hampered by major methodological challenges.
Socioeconomic and preexisting health problems can function as prior common causes of disaster vulnerability and later health problems, inducing confounding bias. For example, persons suffering from depression may be more likely to be victims of disaster (e.g., because they may be slower to evacuate ahead of a tsunami warning) (9). These same individuals may be at greater risk of illness after the disaster, regardless of their experience of disaster-related trauma (10). Adjustment for such confounding is particularly challenging in disaster epidemiology because researchers typically collect data after the disaster and do not have information on survivors predating the disaster. Several studies have taken advantage of “natural experiment” study designs, in which disasters affected participants in prospective cohort studies that were already in progress, thereby allowing for control of a rich set of predisaster information (4, 11, 12).
However, even with the availability of predisaster data with which to adjust for confounding, causal inference for the long-term effects of disasters remains challenging because of 2 additional and underrecognized causal inference challenges: 1) violation of the proportional hazards assumption due to time-varying effects of exposure on long-term health outcomes and 2) bias in estimating exposure-outcome associations due to selective attrition. In this article, we review each challenge and the existing methodologies for overcoming the problems. We then demonstrate the application of the methods to real-world data stemming from the 2011 Great East Japan Earthquake and Tsunami as motivating examples and discuss the implications for future studies.
CHALLENGE 1: ANALYSIS OF A TIME-TO-EVENT OUTCOME WHEN THE EFFECT OF AN EXPOSURE IS TIME-VARYING
The first challenge for causal inference emerges when the outcome of interest is the time to an event (e.g., death, onset of diseases). A common approach to the analysis of such outcomes adjusting for potential confounders is to use a Cox proportional hazards model and report a single hazard ratio as a measure of causal effect (13). However, the hazard ratio has been criticized as a flawed measure of causal effect (14–16), for 2 reasons.
The first reason is that a Cox proportional hazards model assumes that hazard ratios are constant over time, even though hazard ratios are time-varying for most situations in the real world. Assuming constant hazard ratios when assessing the long-term impacts of disaster exposure on the health of survivors ignores the fact that there are distinct postdisaster phases (e.g., the immediate postdisaster phase vs. the long-term recovery phase) during which traumatic disaster-related experiences may exert different adverse effects. When the hazard ratios are time-varying, the single hazard ratio estimate from a Cox model is a weighted average of the time-varying hazard ratios, which is often not informative since it is not intuitive and may mask significant changes in the pattern of effects over time (17).
The second reason is that estimating time-specific hazard ratios instead of assuming a constant hazard ratio is also problematic, because the time-specific hazard ratios do not have a causal interpretation due to selection bias. A hazard at a given time point is, by definition, the instantaneous probability density of event onset conditional on survival up to that time point. In examining the association between disaster-related damage and mortality, for instance, the probability of survival is lower in proportion to the scale of the disaster (18–21). Moreover, persons with baseline susceptibility to death (e.g., those with preexisting health problems) are less likely to survive up to any given time point. Thus, survival is a common effect (i.e., collider) of disaster damage and baseline health conditions and, if conditioned, induces selection bias (22). Although estimating a series of weighted averages of time-varying hazard ratios for increasingly longer periods of follow-up is a valid approach for examining time-varying effects while avoiding selection bias built into the time-specific hazard ratios, the approach allows estimation of exposure effects on the relative scale (i.e., hazard ratios) only.
Notably, the use of hazard ratios is problematic even in the absence of loss to follow-up or missing outcome data and resulting selection bias, which we discuss below in challenge 2.
Parametric survival curves with confounding adjustment
An alternative analytical approach for time-to-event outcomes is to estimate cumulative survival probabilities or cumulative incidence rates (i.e., risks, 1 − survival probabilities) at each time point instead of hazards and to plot survival curves. An advantage of this approach is that the survival curves allow us to visualize trajectories of absolute risks, which may be more intuitive and informative than a series of average hazard ratios (14). Moreover, the effects of an exposure can be computed on both the additive (i.e., cumulative incidence differences) and relative (i.e., cumulative incidence ratios) scales. Because these effect measures are not conditional on survival up to a certain time point, they are not susceptible to the same type of selection bias as time-specific hazard ratios.
The approach with which to parametrically estimate survival curves with confounding adjustment (a.k.a. causal survival analysis) is outlined by Hernán and Robins (16). In Figure 1 and Web Appendix 1 (available at https://doi.org/10.1093/aje/kwab064), we summarize the steps needed to adjust for confounding via standardization and obtain counterfactual survival curves that would have been observed if everyone had received a certain level of exposure. These counterfactual survival curves offer a full picture of the time-varying effects of the exposure. Although confounding adjustment can also be done via inverse probability of treatment weighting (IPTW), we will not focus on that approach in this article because estimation of inverse probability of treatment weights is complicated when the categorical exposure has 3 or more levels.
Figure 1.

Estimation of parametric survival curves with confounding adjustment via standardization. A = exposure; Ci = a vector of covariates for individual i; Ti = time of death for individual i (follow-up ends at Tmax because of administrative censoring); Dt = death by the end of follow-up;  − conditional hazard of death for individual i at time t under treatment level A = a. In the “long” data created after step 1, person-time for each individual was separated into rows.
− conditional hazard of death for individual i at time t under treatment level A = a. In the “long” data created after step 1, person-time for each individual was separated into rows.
CHALLENGE 2: SELECTION BIAS DUE TO SELECTIVE ATTRITION
When evaluating long-term associations between disaster exposure and health, a common practice in disaster epidemiology is to 1) enroll survivors at a given time point (typically several months or years after the event), 2) measure health outcomes (e.g., depression) by means of surveys over the course of follow-up, and 3) analyze data only from individuals whose outcome was measured. However, associations from such analyses may not represent the causal effect of a disaster on health, even when the disaster exposure can be considered to have happened randomly.
By design, postdisaster health status cannot be ascertained for people who 1) were alive but chose not to participate in the survey (pattern 2 in Figure 2A) or 2) died before the time of the outcome assessment (pattern 3 in Figure 2A). Thus, analyzing only those survivors who participate in the follow-up wave is equivalent to conditioning on censoring due to death and study nonparticipation (represented by a box around censoring S = 0 of a directed acyclic graph in Figure 2B and Figure 2C). When exposure A (e.g., disaster-related experience) affects the probability of being censored and there is a common cause for censoring S and outcome Y, as illustrated by C in Figure 2B and C and U in Figure 2C, such conditioning on censoring status (i.e., a collider) would induce selection bias (22).
Figure 2.
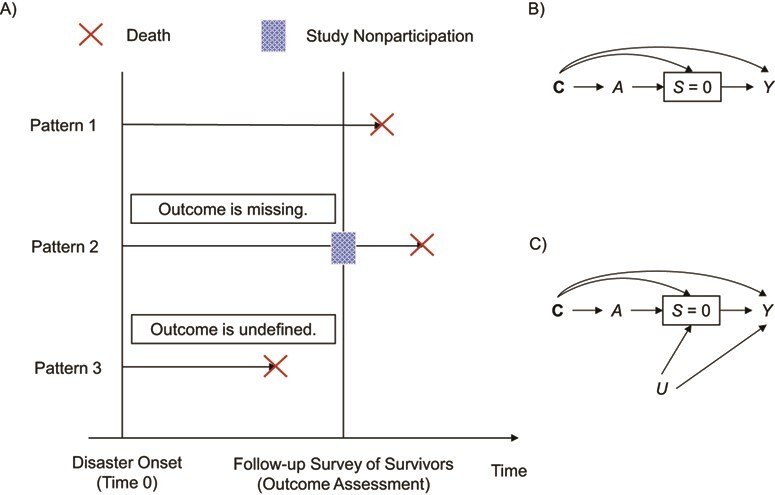
Illustration of selection bias due to selective attrition. A) Attrition by death and study nonparticipation in studies of the association between disasters and health outcomes, assessed in a follow-up survey of survivors. B) Directed acyclic graph where an association between an exposure A and an outcome Y is biased due to confounding by measured covariates C and selection bias of conditioning on no censoring, S = 0. C) Directed acyclic graph where an association between an exposure A and an outcome Y is biased due to confounding by measured covariates C and selection bias induced by C and U, both of which cause no censoring S = 0 and an outcome Y.
Selection bias due to selective attrition is particularly relevant in disaster epidemiology. For example, disaster-related damage, A, is likely to affect the probability of censoring, S, due to the effects of natural disasters on mortality discussed in challenge 1 or study nonparticipation due to acute mental health effects (depression and posttraumatic stress disorder) (18–21, 23, 24). Persons with predisaster health problems (e.g., depression) (C or U) may be at greater risk of poor health (Y) after the disaster and more likely to be censored (S = 1). Although the direction and magnitude of resulting selection bias depend on how the 2 causes of censoring (i.e., A and C/U) interact and cannot be known without a full understanding of the underlying selection mechanism, such selective attrition would often result in the underestimation of the true causal effect of disaster exposure (A) on health (Y) (22, 25, 26).
There are a few common approaches for dealing with the selection bias. These common approaches, if the necessary assumptions hold, estimate one of the 2 counterfactual estimands: 1) effects of disaster exposure on health that would have been observed if no one had been censored or 2) effect of the exposure in a subset of the population who would have been uncensored regardless of their exposure status. For each of the analytical methods we discuss, corresponding causal estimands, their interpretation, and underlying assumptions are shown in Table 1.
Table 1.
Analytical Methods for Dealing With Selection Bias Due to Selective Attrition by Death and Study Nonparticipationa
| Method | Causal Estimand | Interpretation | Assumptions b |
|---|---|---|---|
| Multivariable adjustmentc |
|
Risk of Y that would have been observed if everyone had been exposed to A and everyone had remained in the study divided by risk of Y if no one had been exposed to A and everyone had remained in the study conditional on C | No unmeasured common cause for an A-Y relationship ( ) )No unmeasured common cause for an S-Y relationship (  ) )No model misspecification for the outcome (Y) model conditional on A and C |
| IPTW and IPCWc |
|
Risk of Y that would have been observed if everyone had been exposed to A and everyone had remained in the study divided by risk of Y if no one had been exposed to A and everyone had remained in the study among the study population | No unmeasured common cause for an A-Y relationship ( ) )No unmeasured common cause for an S-Y relationship (  ) )No model misspecification for the exposure (A) model conditional on C No model misspecification for death and attrition (S) conditional on A and C |
| SACEd,e |
|
Risk of Y that would have been observed if everyone had been exposed to A divided by risk of Y if no one had been exposed to A conditional on C in a study population subset of persons who would have remained in the study regardless of the exposure level | No unmeasured common cause for an A-Y relationship ( ) )Cross-world exchangeability for an S-Y relationship (  ) )Linear association between U and Y conditional on A and C on the log scalef Linear association between U and S conditional on A and C on the logit scaleg No model misspecification for death and attrition (S) conditional on A and C A does not influence U conditional on Ch Location shift relationship between U and (A, C) given S = 0i |
Abbreviations: IPCW, inverse probability of censoring weighting; IPTW, inverse probability of treatment weighting; SACE, survivor average causal effect.
a Y is a binary outcome, A is a binary exposure, S = 0 indicates that the person remained in the study (i.e., no censoring), C is a vector of covariates, U is an unmeasured common cause of an outcome and censoring,  is a potential outcome under exposure A = a, and
is a potential outcome under exposure A = a, and  is a potential outcome under exposure A = a and S = 0.
is a potential outcome under exposure A = a and S = 0.
b All approaches also assumed consistency and positivity.
c Multivariable adjustment and inverse probability weights were based on conditional exchangeability, implied by the directed acyclic graph in Figure 2B.
d Approach proposed by Tchetgen Tchetgen et al. (37). Assumptions for unmeasured confounder(s) U and model specification are also shown in the original article.
e The SACE approach was based on conditional exchangeability, implied by the directed acyclic graph in Figure 2C.
f The log-linear model for the outcome Y conditional on A, U, and C fitted to those who remained in the study (S = 0) was specified as follows:  , where
, where  is a flexible function of C.
is a flexible function of C.
g The logistic model for the censoring S conditional on A, U, and C was specified as follows:  , where
, where  .
.
h Formally, this assumption is written as  .
.
i Formally, the assumption states that the residual for U ( ) is independent of A and C given S = 0.
) is independent of A and C given S = 0.
Effects if none of the survivors had been censored
The most common approach for dealing with selection bias is to estimate and compare counterfactual outcomes that would have been observed had no one been censored. Formally, this counterfactual estimand for a binary outcome Y and a binary exposure A on the risk ratio scale is defined by
 |
where  represents the potential outcome under exposure
represents the potential outcome under exposure  and no censoring
and no censoring  . This counterfactual quantity, conditional on covariates or marginally, can be estimated via either multivariable-adjusted outcome regression or inverse probability of censoring weighting (IPCW). Both approaches are valid when a vector of measured covariates C suffices to remove all selection bias (i.e., block all open backdoor paths) due to prior common causes of exposure A and outcome Y and of the censoring variable S and the outcome Y (e.g., Figure 2B). The estimation procedure and the underlying assumptions for each analytical method are described in detail in Table 1 and Web Appendix 2. The causal estimands that multivariable-adjusted outcome regression and IPCW target would coincide when there is no effect-measure modification by the covariates C (i.e., the effect of an exposure is constant across levels of C).
. This counterfactual quantity, conditional on covariates or marginally, can be estimated via either multivariable-adjusted outcome regression or inverse probability of censoring weighting (IPCW). Both approaches are valid when a vector of measured covariates C suffices to remove all selection bias (i.e., block all open backdoor paths) due to prior common causes of exposure A and outcome Y and of the censoring variable S and the outcome Y (e.g., Figure 2B). The estimation procedure and the underlying assumptions for each analytical method are described in detail in Table 1 and Web Appendix 2. The causal estimands that multivariable-adjusted outcome regression and IPCW target would coincide when there is no effect-measure modification by the covariates C (i.e., the effect of an exposure is constant across levels of C).
Although these approaches can deal with selection bias, the resulting counterfactual estimand has been criticized because of conceptual problems with its interpretation. First, the interpretation of the estimand requires conceptualizing a hypothetical intervention that would eliminate censoring (27, 28). Since no realistic intervention could plausibly prevent all deaths and study nonparticipation resulting from disaster exposure, the causal estimand may not have a meaningful interpretation in practice. Second, the outcome for persons who died before the follow-up assessment is not simply missing (i.e., inadequate collection of information that could have been observed in principle) but is undefined, because the outcome that deceased individuals would have experienced is never known even with perfect data collection (pattern 3 in Figure 2A) (29, 30).
Survivor average causal effect
The second approach to addressing selection bias due to conditioning on posttreatment censoring is to estimate the effect of the exposure in a subset of the population who would have been uncensored regardless of their exposure status. Since the target population for inference is now restricted to people who never experience censoring, the problems with IPCW (i.e., conceptualizing hypothetical interventions that eliminate all censoring, as well as undefined outcomes for deceased individuals) are removed. This causal estimand is often called the survivor average causal effect (SACE), a form of the principal strata causal effect (31, 32). Formally, the SACE for a binary outcome Y and a binary exposure A on the risk ratio scale is defined by
 |
Various approaches have been proposed for point estimates or bounds of the SACE under different identifiability assumptions (30, 33–38). In this article, we highlight a technique developed by Tchetgen Tchetgen et al. (37) using a 2-stage regression to obtain a point estimate of the SACE conditional on covariates. Specifically, we first fit a model for censoring conditional on the exposure and the covariates to compute conditional probabilities of being censored (S = 1); and then, in the second stage, we fit a model for the outcome Y conditional on the exposure, the same set of covariates as in the previous model, and the predicted probabilities of being censored as an additional covariate. We chose this method for its simplicity and robustness to unmeasured common causes for censoring and outcome (e.g., U in Figure 2C). The estimation procedure and underlying assumptions are described in detail in Table 1 and Web Appendix 3.
The conditional SACE and the causal estimand that the multivariable-adjusted outcome regression targets (i.e., the effect of an exposure had no one been censored conditional on covariates) will coincide if there are no unmeasured common causes for censoring and outcome (e.g., U in Figure 2C; see Web Appendix 4 for proof).
While the SACE is a useful estimand for avoiding selection bias, the approach has also been criticized because the “survivors” (i.e., people with  ) cannot be empirically identified, since the definition is based on counterfactuals, which we cannot observe in reality (15, 28).
) cannot be empirically identified, since the definition is based on counterfactuals, which we cannot observe in reality (15, 28).
MOTIVATING EXAMPLES
The Iwanuma Study
We illustrate application of the methods described above using a cohort of disaster survivors from the 2011 Great East Japan Earthquake and Tsunami, which struck the northeastern coast of Japan on March 11, 2011. Our analytical sample comprised residents of Iwanuma City in Miyagi Prefecture, located approximately 80 km (50 miles) west of the earthquake epicenter. Iwanuma was one of the field sites in a nationwide cohort study of Japanese adults aged 65 years or more, the Japan Gerontological Evaluation Study (JAGES), which was established 7 months prior to the disaster (39, 40). The tsunami killed 180 residents, damaged 5,542 houses, and inundated 48% of the land area in Iwanuma (see Web Figure 1) (41).
At baseline (August 2010), a census was conducted of all Iwanuma City residents aged 65 years or more (n = 8,576), and valid responses were obtained from a total of 4,957 residents (response rate = 57.8%). Two waves of follow-up surveys were conducted in the aftermath of the disaster: October 2013 (2.5 years after disaster onset) and November 2016 (5.5 years after disaster onset).
Notably, the Iwanuma Study has a rich set of information on the characteristics of the subjects predating the disaster. Thus, we were able to use the predisaster information to 1) examine the presence of selective attrition and adjust for resulting selection bias and 2) adjust for confounding by sociodemographic characteristics that were distributed differently across the levels of disaster damage.
The data underlying this article were provided by the JAGES investigators with permission. Data will be shared upon request to the corresponding author, with the permission of the JAGES investigators.
Example 1: Causal survival analysis
Question and problem.
We examined the effect of predisaster distance from the coast on all-cause mortality among survivors in the Iwanuma Study. We performed causal survival analysis to parametrically estimate survival curves adjusting for confounding via standardization.
Methods.
We used the data of all disaster survivors in the Iwanuma sample (n = 4,857) (see Web Figure 2 for selection of the analytical sample). Information on dates of death due to all causes was obtained through linkage to the national long-term care insurance database. The time to death or administrative censoring at the end of the 6-year follow-up period was available for everyone in the analytical sample; hence there was no loss to follow-up. Predisaster distance from the coast was categorized into 3 levels—<1,000 m, 1,000–3,000 m, and >3,000 m—as a proxy for complete home loss, major housing damage, and less severe damage, respectively (see Web Figure 3B). We adjusted for age, sex, depressive symptoms, self-rated health, education, household income, current smoking, current alcohol intake, and treatment for major diseases (including hypertension, stroke, diabetes, and dyslipidemia) prior to onset of the disaster.
We first performed conventional analyses for a time-to-event outcome including the Kaplan-Meier estimator and a Cox proportional hazards model. In pooled logistic regression of causal survival analysis, we modeled time as a quadratic function and included product terms between the exposure and time to allow time-varying hazard ratios. We estimated counterfactual survival curves as well as the trajectories of cumulative incidence differences and cumulative incidence ratios. Multiple imputation by chained equations (m = 20) was used to impute missing data on the covariates, assuming that the data were missing at random (42). Standard errors were obtained by bootstrapping with 1,000 replications.
Results.
Baseline demographic characteristics of the analytical sample are shown in Table 2 by level of exposure. People who lived closer to the coast (<1,000 m) were more likely to be older, depressed, and less educated, and they reported poorer self-rated health and lower household income than those who lived far from the coast (>3,000 m).
Table 2.
Baseline (2010) Sociodemographic Characteristics of the Analytical Sample Before the 2011 Earthquake and Mortality During the 6-Year Follow-up Period (2011–2017) According to Preexposure Residential Distance From the Coast, Iwanuma, Japan
| Distance From Coast | ||||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | Total | >3,000 m | 1,000–3,000 m | <1,000 m | ||||
| No. | % | No. | % | No. | % | No. | % | |
| No. of participants | 4,857 | 100.0 | 4,129 | 100.0 | 467 | 100.0 | 261 | 100.0 |
| No. of deaths during follow-up period | 806 | 16.7 | 650 | 15.7 | 95 | 20.3 | 61 | 23.4 |
| Sex | ||||||||
| Male | 2,105 | 43.3 | 1,817 | 44.0 | 190 | 40.7 | 98 | 37.5 |
| Female | 2,752 | 56.7 | 2,312 | 55.0 | 277 | 59.3 | 163 | 62.5 |
| Depression in 2010a | ||||||||
| Mild or severe depression | 1,444 | 29.7 | 1,222 | 29.6 | 133 | 28.5 | 89 | 34.1 |
| No depression | 2,682 | 55.2 | 2,302 | 55.8 | 253 | 54.2 | 127 | 48.7 |
| Missing data | 731 | 15.1 | 605 | 14.7 | 81 | 17.3 | 45 | 17.2 |
| Self-rated health in 2010 | ||||||||
| Very good | 538 | 11.1 | 445 | 10.8 | 57 | 12.2 | 36 | 13.8 |
| Good | 3,140 | 64.6 | 2,710 | 65.6 | 286 | 61.2 | 144 | 55.2 |
| Bad | 862 | 17.7 | 724 | 17.5 | 85 | 18.2 | 53 | 20.3 |
| Very bad | 227 | 4.7 | 180 | 4.4 | 26 | 5.6 | 21 | 8.0 |
| Missing data | 90 | 1.9 | 70 | 1.7 | 13 | 2.8 | 7 | 2.7 |
| Duration of education in 2010, years | ||||||||
| <6 | 123 | 2.5 | 95 | 2.3 | 13 | 2.8 | 15 | 5.7 |
| 6–9 | 1,634 | 33.6 | 1,260 | 30.5 | 240 | 51.4 | 134 | 51.3 |
| 10–12 | 1,938 | 39.9 | 1,767 | 42.8 | 122 | 26.1 | 49 | 18.8 |
| ≥13 | 916 | 18.9 | 846 | 20.5 | 54 | 11.6 | 16 | 6.1 |
| Other | 52 | 1.1 | 32 | 0.8 | 11 | 2.4 | 9 | 3.4 |
| Missing data | 194 | 4.0 | 129 | 3.1 | 27 | 5.8 | 38 | 14.6 |
| Current smoking status in 2010 | ||||||||
| Nonsmoker | 3,938 | 81.1 | 3,386 | 82.0 | 347 | 74.3 | 205 | 78.5 |
| Smoker | 496 | 10.2 | 410 | 9.9 | 63 | 13.5 | 23 | 8.8 |
| Missing data | 423 | 8.7 | 333 | 8.1 | 57 | 12.2 | 33 | 12.6 |
| Current alcohol drinking status in 2010 | ||||||||
| Drinker | 1,624 | 33.4 | 1,431 | 34.7 | 132 | 28.3 | 61 | 23.4 |
| Nondrinker | 3,114 | 64.1 | 2,611 | 63.2 | 316 | 67.7 | 187 | 71.6 |
| Missing data | 119 | 2.5 | 87 | 2.1 | 19 | 4.1 | 13 | 5.0 |
| Current treatment for hypertension in 2010 | ||||||||
| No | 2,729 | 56.2 | 2,326 | 56.3 | 252 | 54.0 | 151 | 57.9 |
| Yes | 2,001 | 41.2 | 1,710 | 41.4 | 194 | 41.5 | 97 | 37.2 |
| Missing data | 127 | 2.6 | 93 | 2.3 | 21 | 4.5 | 13 | 5.0 |
| Current treatment for stroke in 2010 | ||||||||
| No | 4,594 | 94.6 | 3,929 | 95.2 | 429 | 91.9 | 236 | 90.4 |
| Yes | 136 | 2.8 | 107 | 2.6 | 17 | 3.6 | 12 | 4.6 |
| Missing data | 127 | 2.6 | 93 | 2.3 | 21 | 4.5 | 13 | 5.0 |
| Current treatment for diabetes in 2010 | ||||||||
| No | 4,064 | 83.7 | 3,461 | 83.8 | 388 | 83.1 | 215 | 82.4 |
| Yes | 666 | 13.7 | 575 | 13.9 | 58 | 12.4 | 33 | 12.6 |
| Missing data | 127 | 2.6 | 93 | 2.3 | 21 | 4.5 | 13 | 5.0 |
| Current treatment for dyslipidemia in 2010 | ||||||||
| No | 4,274 | 88.0 | 3,638 | 88.1 | 399 | 85.4 | 237 | 90.8 |
| Yes | 456 | 9.4 | 398 | 9.6 | 47 | 10.1 | 11 | 4.2 |
| Missing data | 127 | 2.6 | 93 | 2.3 | 21 | 4.5 | 13 | 5.0 |
| Age in 2010, yearsb | 74.7 (6.97) | 74.6 (6.79) | 74.5 (7.38) | 77.1 (8.40) | ||||
| Equivalized household income in 2010 (10,000 yen)b,c | 228 (147) | 234 (148) | 202 (140) | 170 (126) | ||||
| Missing data | 977 | 20.1 | 791 | 19.2 | 103 | 22.1 | 83 | 31.8 |
a Depression was defined as scoring 5 or more points on the Geriatric Depression Scale.
b Values are expressed as mean (standard deviation).
c Household income was divided by the square root of household size.
Table 3 shows hazard ratio estimates from the Cox models. After adjustment for confounding, living 1,000–3,000 m (vs. >3,000 m) from the coast was associated with a greater hazard of death (hazard ratio (HR) = 1.32, 95% confidence interval (CI): 1.06, 1.65), whereas there was no strong evidence of an association with mortality for persons who lived less than 1,000 m from the coast (HR = 1.22, 95% CI: 0.93, 1.61).
Table 3.
Association Between Pre-Earthquake Residential Distance From the Coast and Mortality in Cox Proportional Hazards Models, Iwanuma, Japan, 2010–2017
| Distance From Coast in 2010, m | Crude | Confounder-Adjusted a | ||
|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | |
| >3,000 | 1.00 | Referent | 1.00 | Referent |
| 1,000–3,000 | 1.33 | 1.07, 1.65 | 1.32 | 1.06, 1.65 |
| <1,000 | 1.59 | 1.23, 2.07 | 1.22 | 0.93, 1.61 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
a Adjusted for sex, age, depressive symptoms, self-rated health, education, household income, current smoking, current alcohol intake, and treatment for major diseases (including hypertension, stroke, diabetes, and dyslipidemia).
Figure 3 shows the results of causal survival analysis. Estimated parametric survival curves without confounding adjustment (Figure 3A) were identical to the nonparametric curves obtained via the Kaplan-Meier estimator (Web Figure 4), suggesting that our model specifications for conditional discrete hazards were appropriate. Figure 3B shows parametric survival curves after confounding adjustment via standardization. We observed that on the absolute scale, increasingly higher levels of the exposure (i.e., living closer to the coast before the disaster) were associated with higher mortality throughout the follow-up period (Figure 3C). After adjustment for confounding (Figure 3D), the risk of death was greater in the <1,000-m group (vs. >3,000 m) for the first 3 years (e.g., cumulative incidence difference at 36 months = 0.024 (95% CI: 0.001, 0.057). Results on the relative scale also showed similar trends before (Figure 3E) and after (Figure 3F) confounding adjustment (e.g., cumulative incidence ratio at 36 months = 1.33 (95% CI: 1.01, 1.79). However, at 48 months, the association for the <1,000-m group remained similar on the absolute scale (cumulative incidence difference = 0.023, 95% CI: −0.006, 0.055) but was attenuated on the relative scale (cumulative incidence ratio = 1.22, 95% CI: 0.94, 1.57). The associations became even less evident in the later period of follow-up. See Web Table 1 for estimates and confidence intervals.
Figure 3.
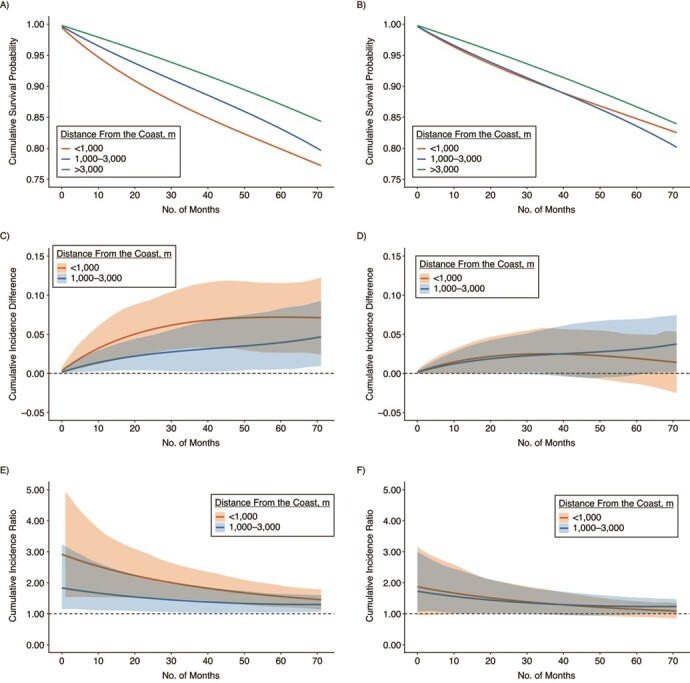
Parametric curves for mortality during the follow-up period (2011–2017) by predisaster distance from the coast among survivors of the 2011 earthquake in Iwanuma, Japan. A) Cumulative survival probability without confounding adjustment; B) cumulative survival probability with confounding adjustment; C) cumulative incidence difference without confounding adjustment; D) cumulative incidence difference with confounding adjustment; E) cumulative incidence ratio without confounding adjustment; F) cumulative incidence ratio with confounding adjustment. Panels A, C, and E (left column) show crude associations between predisaster distance from the coast and mortality. Panels B, D, and F (right column) show results adjusted for sex, age, depressive symptoms, self-rated health, education, household income, current smoking, current alcohol intake, and treatment for major diseases (including hypertension, stroke, diabetes, and dyslipidemia) via standardization. The 95% confidence intervals (shaded areas) were obtained via bootstrapping with 1,000 replications.
Discussion.
Our results indicate that using a Cox regression ignoring time-varying effects of disasters may result in the misleading conclusion that the degree of disaster damage (i.e., living less than 1,000 m from the coastline before the disaster vs. living at least 1,000 m away) did not have a causal effect on mortality over the 6-year follow-up period. Estimation of parametric survival curves adjusted for confounding is a more appropriate approach for assessing trajectories of the associations between a disaster exposure and risk of death. We demonstrated that living closer to the coast appeared to exert an adverse influence on the risk of mortality for at least the first 3 years after the disaster.
Example 2: Selection bias adjustment
Question and problem.
We examined the effect of disaster-related housing damage on depression in 2013 and 2016. Web Figure 5 shows the selection of the analytical sample. Among the disaster survivors (n = 4,857), the outcome of interest was measured only among people who survived up to and participated in the follow-up surveys in 2013 and 2016 (n = 3,567 for 2013 and n = 2,781 for 2016) and was censored for the rest. The severity of disaster-related damage is likely to be correlated with the probability of because of the disaster’s impacts on mortality during the immediate postdisaster phase and nonparticipation in follow-up surveys. In addition, censoring is likely to share common prior causes (e.g., predisaster health status) with depression assessed in 2013 and 2016. Thus, a naive analysis of people without missing outcome information would result in selection bias and underestimate the effect of disaster damage on depression.
Methods.
Our outcome was mild or severe depression, defined as scoring 5 points or higher on the validated Japanese short version of the Geriatric Depression Scale (43). For our exposure, as a proxy for housing damage due to the tsunami, we used the distance from each participant’s residential address and the coastline. As illustrated in Web Figure 1 and Web Figure 3A, people who lived closer to the coastline were more likely to experience inundation by the tsunami and property damage. We dichotomized the distance variable and created a binary indicator (<1,000 m and ≥1,000 m) representing distance from the coastline, because this demarcated the extent of inundation by the tsunami and thus correlated with complete home loss (see Web Figure 3B). In turn, previous evidence has documented that complete home loss was a unique predictor of increased depressive symptoms (44).
We compared 4 approaches to estimate the associations between predisaster distance from the coast and depression: 1) crude univariate Poisson regression, 2) multivariable-adjusted Poisson regression, 3) Poisson regression weighted by IPTW and IPCW, and 4) SACE estimation. Poisson regression was used because depression was common in our sample and odds ratios from logistic regression may not approximate risk ratios (45). Approaches 2–4 adjusted for age, sex, depressive symptoms, self-rated health, education, household income, and marital status prior to disaster onset. Multiple imputation by chained equations (m = 20) was used to impute missing data on covariates, assuming the data were missing at random (42). Standard errors were obtained by bootstrapping with 1,000 replications.
Results.
Table 4 shows the prevalence of depression and baseline sociodemographic characteristics in the analytical samples (n = 3,567 for 2013 and n = 2,781 for 2016) and among persons who were censored. The prevalence of depression was 28.8% for 2013 and 22.7% for 2016. Compared with the analytical sample, people who died between the disaster onset and the follow-up surveys (n = 342 for 2013 and n = 740 for 2016) and people who were alive but did not participate in the follow-up surveys (n = 948 for 2013 and n = 1,336 for 2016) were more likely to have experienced severe damage (i.e., living less than 1,000 m from the coast before the disaster). Moreover, the censored individuals were more likely to be depressed, less educated, not married, and older compared with members of the analytical sample who remained in the study, and they reported poorer self-rated health.
Table 4.
Baseline Sociodemographic Characteristics of the Analytical Sample and Depression Outcomes by Censoring Status in 2013 and 2016, Iwanuma, Japan, 2010–2016
| 2013 | 2016 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Censored | Censored | |||||||||||||
| Characteristic | All Disaster Survivors | Not Censored | Died | Withdrew | Not Censored | Died | Withdrew | |||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Total | 4,857 | 100.0 | 3,567 | 100.0 | 342 | 100.0 | 948 | 100.0 | 2,781 | 100.0 | 740 | 100.0 | 1,336 | 100.0 |
| Depression status in follow-up wavesa,b | ||||||||||||||
| Mild or severe depression | N/A | 1,027 | 28.8 | N/A | N/A | 630 | 22.7 | N/A | N/A | |||||
| No depression | N/A | 2,072 | 58.1 | N/A | N/A | 1,430 | 51.4 | N/A | N/A | |||||
| Missing data | N/A | 468 | 13.1 | N/A | N/A | 721 | 25.9 | N/A | N/A | |||||
| Distance from home address to the coast in 2010, m | ||||||||||||||
| ≥1,000 | 3,424 | 96.0 | 305 | 89.2 | 867 | 91.5 | 2,685 | 96.5 | 682 | 92.2 | 1,229 | 92.0 | ||
| <1,000 | 143 | 4.0 | 37 | 10.8 | 81 | 8.5 | 96 | 3.5 | 58 | 7.8 | 107 | 8.0 | ||
| Sex | ||||||||||||||
| Male | 2,105 | 43.3 | 1,552 | 43.5 | 173 | 50.6 | 380 | 40.1 | 1,208 | 43.4 | 367 | 49.6 | 530 | 39.7 |
| Female | 2,752 | 56.7 | 2,015 | 56.5 | 169 | 49.4 | 567 | 59.9 | 1,573 | 56.6 | 373 | 50.4 | 806 | 60.3 |
| Depression in 2010a | ||||||||||||||
| Mild or severe depression | 1,444 | 29.7 | 984 | 27.6 | 140 | 40.9 | 320 | 33.8 | 730 | 26.2 | 300 | 40.5 | 414 | 31.0 |
| No depression | 2,682 | 55.2 | 2,090 | 58.6 | 136 | 39.8 | 456 | 48.1 | 1,703 | 61.2 | 298 | 40.3 | 681 | 51.0 |
| Missing data | 731 | 15.1 | 493 | 13.8 | 66 | 19.3 | 172 | 18.1 | 348 | 12.5 | 142 | 19.2 | 241 | 18.0 |
| Self-rated health in 2010 | ||||||||||||||
| Very good | 538 | 11.1 | 423 | 11.9 | 23 | 6.7 | 92 | 9.7 | 347 | 12.5 | 50 | 6.8 | 141 | 10.6 |
| Good | 3,140 | 64.6 | 2,420 | 67.8 | 157 | 45.9 | 563 | 59.4 | 1,940 | 69.8 | 380 | 51.4 | 820 | 61.4 |
| Bad | 862 | 17.7 | 537 | 15.1 | 107 | 31.3 | 218 | 23.0 | 374 | 13.4 | 207 | 28.0 | 281 | 21.0 |
| Very bad | 27 | 4.7 | 121 | 3.4 | 51 | 14.9 | 55 | 5.8 | 71 | 2.6 | 89 | 12.0 | 67 | 5.0 |
| Missing data | 90 | 1.9 | 66 | 1.9 | 4 | 1.2 | 20 | 2.1 | 49 | 1.8 | 14 | 1.9 | 27 | 2.0 |
| Duration of education in 2010, years | ||||||||||||||
| <6 | 123 | 2.5 | 47 | 1.3 | 26 | 7.6 | 50 | 5.3 | 25 | 0.9 | 55 | 7.4 | 43 | 3.2 |
| 6–9 | 1,634 | 33.6 | 1,183 | 33.2 | 121 | 35.4 | 330 | 34.8 | 866 | 31.1 | 269 | 36.4 | 499 | 37.4 |
| 10–12 | 1,938 | 39.9 | 1,486 | 41.7 | 114 | 33.3 | 338 | 35.7 | 1,214 | 43.7 | 244 | 33.0 | 480 | 35.9 |
| ≥13 | 916 | 18.9 | 713 | 20.0 | 43 | 12.6 | 160 | 16.9 | 596 | 21.4 | 102 | 13.8 | 218 | 16.3 |
| Other | 52 | 1.1 | 31 | 0.9 | 12 | 3.5 | 9 | 0.9 | 17 | 0.6 | 19 | 2.6 | 16 | 1.2 |
| Missing data | 194 | 4.0 | 107 | 3.0 | 26 | 7.6 | 61 | 6.4 | 63 | 2.3 | 51 | 6.9 | 80 | 6.0 |
| Marital status in 2010 | ||||||||||||||
| Not married | 1,483 | 30.5 | 984 | 27.6 | 149 | 43.6 | 350 | 36.9 | 700 | 25.2 | 306 | 41.4 | 477 | 35.7 |
| Married | 3,173 | 65.3 | 2,460 | 69.0 | 170 | 49.7 | 543 | 57.3 | 1,999 | 71.9 | 391 | 52.8 | 783 | 58.6 |
| Missing data | 201 | 4.1 | 123 | 3.4 | 23 | 6.7 | 55 | 5.8 | 82 | 2.9 | 43 | 5.8 | 76 | 5.7 |
| Age in 2010, yearsc | 74.7 (6.97) | 73.6 (6.29) | 81.7 (7.95) | 76.1 (7.32) | 72.8 (5.73) | 80.6 (7.60) | 75.4 (6.99) | |||||||
| Equivalized household income in 2010 (10,000 yen)c,d | 228 (147) | 230 (142) | 230 (171) | 220 (157) | 232 (138) | 223 (154) | 223 (161) | |||||||
| Missing data | 977 | 20.1 | 656 | 18.4 | 79 | 23.1 | 242 | 25.5 | 458 | 16.5 | 182 | 24.6 | 337 | 25.2 |
Abbreviation: N/A, not applicable.
a Depression was defined as scoring 5 or more points on the Geriatric Depression Scale.
b Information on the prevalence of depression in 2013 and 2016 was available only for persons who were not censored in each wave.
c Values are expressed as mean (standard deviation).
d Household income was divided by the square root of household size.
Compared with those who lived far (≥1,000 m) from the coast before the disaster, persons who lived closer to the coast (<1,000 m) showed a greater risk of depression 2.5 years postdisaster (2013; Figure 4A) across all alternative analytical approaches. However, the SACE estimate (risk ratio (RR) = 1.94, 95% CI: 1.41, 2.50) was larger than the risk ratios from other approaches adjusting for confounding and selection bias (RR = 1.69 (95% CI: 1.33, 2.07) for the multivariable-adjusted regression; RR = 1.66 (95% CI: 1.21, 2.08) for IPTW and IPCW). In the second follow-up survey, conducted 5.5 years after the disaster (2016; Figure 4B), we did not find strong evidence of an association between distance from the coast and depression risk in the models with multivariable adjustment (RR = 1.34, 95% CI: 0.96, 1.68) or with IPTW and IPCW (RR = 1.21, 95% CI: 0.70, 1.69). By contrast, the SACE approach continued to show an elevated risk of depression in 2016 for persons living less than 1,000 m from the coast before the disaster (RR = 2.00, 95% CI: 1.21, 2.87).
Figure 4.
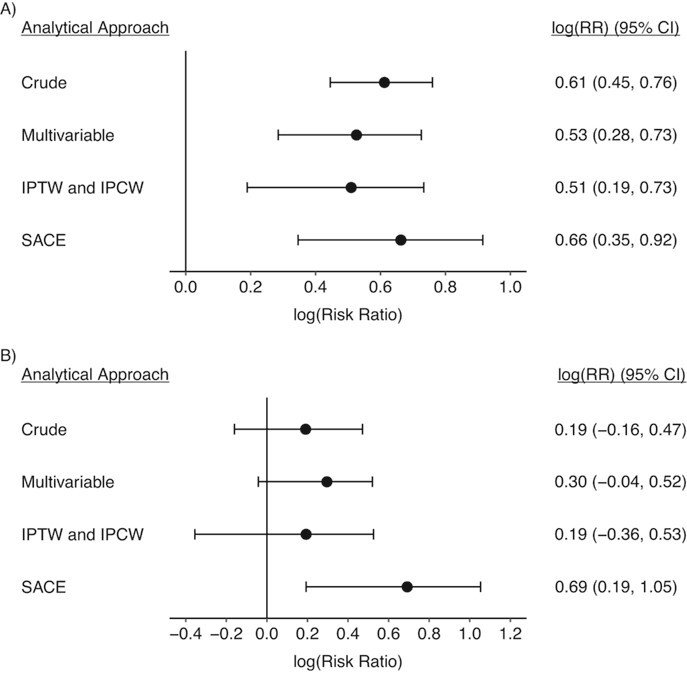
Risk ratio (RR) estimates for associations between pre-earthquake residential distance from the coast (<1,000 m vs. ≥1,000 m) and depression in 2013 (A) and 2016 (B) among survivors of the 2011 earthquake in Iwanuma, Japan, with or without selection bias adjustment. The crude model shows the univariate association between pre-earthquake distance from the coast and mild/severe depression in 2013 and 2016. Other models adjusted for potential confounding and selection bias by predisaster sociodemographic characteristics, including age, sex, Geriatric Depression Scale score, self-rated health, education, income, and marital status. In the survivor average causal effect (SACE) approach, results were further adjusted for selection bias due to unmeasured variable(s), which satisfies the conditions described in the paper by Tchetgen Tchetgen et al. (37). The 95% confidence intervals (CIs; bars) were obtained via bootstrapping with 1,000 replications. IPCW, inverse probability of censoring weighting; IPTW, inverse probability of treatment weighting.
Discussion.
We found that people who were censored before the follow-up surveys were more likely to have experienced severe disaster-related damage and to have characteristics that potentially put them at higher risk of depression. Moreover, the prevalence of depression was lower in the analytical sample for 2016—data collected with more attrition—than in the 2013 sample, which had less attrition, indicating that persons with preexisting depression may be selectively censored over time. The results from the descriptive analysis suggest that ignoring censoring would probably result in underestimation of the true causal effect.
The SACE estimate indicates that greater damage due to the tsunami is associated with elevated risk of depression even 5.5 years postdisaster in the subset of the population who would have remained in the study regardless of their exposure status. Such evidence for a long-term effect on depression was not observed when we estimated the effect of disaster exposure that would have been observed if no one had been censored, using multivariable adjustment or IPTW and IPCW. Since the estimate from multivariable adjustment would also have the same interpretation as the conditional SACE if there is no unmeasured common cause for censoring and outcome, the discrepancy in estimates is probably driven by the presence of additional selection bias that was adjusted for in the SACE estimation (37). Our findings underscore the importance of choosing the appropriate causal estimand and adjusting for selection bias in the presence of selective attrition over time.
ADDITIONAL CHALLENGES IN DISASTER EPIDEMIOLOGY
There are several other issues to consider that complicate causal inference in epidemiologic studies of the long-term health effects of disasters.
First, we have demonstrated how to parametrically estimate survival curves as well as trajectories of differences and ratios of cumulative incidence, or risk, as an alternative measure of causal effect. Although this approach for time-to-event outcomes has some advantages over estimating a series of average hazard ratios, both effect measures are averages of time-varying effects, and their interpretation is dependent on the length of follow-up. That is, both of the average effect measures become more likely to mask important time-varying effects as the duration of follow-up gets longer. Thus, the issue of time-varying effects merits attention even when methods other than Cox regression are used.
Second, some methods of “adjusting for” selection bias that we reviewed (IPCW and SACE) require information on the exposure and common causes for censoring and the outcome among both the censored and uncensored individuals. In the Iwanuma Study, we had a rich set of information on the predisaster characteristics of survivors to predict their probabilities of not being censored. If we only had information from persons who participated in the follow-up survey, such bias correction would not be feasible. Notably, even with the availability of predisaster information, had the relevant exposure been assessed in the follow-up survey (e.g., retrospective reporting of disaster-related traumatic experiences), it would not have been possible to calculate the probabilities of no censoring conditional on the exposure. This problem of misalignment of “time 0” (i.e., exposure assignment and measurement are separated in time) and the resulting selection bias is prevalent not only in disaster epidemiology but also in any observational studies of traumatic experiences, such as adverse childhood experiences (46). In such cases, where selection bias correction is infeasible, investigators could at least perform sensitivity analyses to simulate the range of causal effects by specifying plausible parameters representing the magnitude of potential selection bias (30, 47).
Third, there is no “silver bullet” causal estimand in the presence of censoring. The interpretation of the estimated causal effects after bias correction that we have discussed is either 1) the effect of an exposure that requires conceptualizing hypothetical interventions that eliminate all censoring (multivariable adjustment or IPCW) or 2) the effect of an exposure in a subset of the population that cannot be identified empirically (SACE). Neither of these estimands is particularly informative from a policy-making perspective (28). Methodologists have recently begun to develop alternative causal estimands in the presence of selection bias (27).
Lastly, studies assessing long-term impacts of disaster experiences are meaningful when the target of inference is disaster survivors. Thus, we excluded persons killed directly by the tsunami (n = 34; 0.7% of the baseline participants). Although our focus in this paper was on selective attrition due to postdisaster data collection, such exclusion may have induced selection bias.
In conclusion, we have illustrated 2 challenges for causal inference that are common in studies of long-term effects of disasters on the health of survivors, namely, analysis of time-to-event outcome data when the effect of an exposure varies over time and selection bias due to selective attrition. Using data from the 2011 Great East Japan Earthquake and Tsunami, we demonstrated that conventional analytical approaches which ignore these challenges underestimate the long-term health effects of the earthquake. Such bias may give rise to the misleading conclusion that disasters do not adversely affect the long-term health of survivors and misguided policies for supporting the well-being of survivors.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Social and Behavioral Sciences, T.H. Chan School of Public Health, Harvard University, Boston, Massachusetts, United States (Koichiro Shiba, Ichiro Kawachi); Department of Epidemiology, T.H. Chan School of Public Health, Harvard University, Boston, Massachusetts, United States (Koichiro Shiba); Clinical Research Promotion Center, University of Tokyo Hospital, Tokyo, Japan (Takuya Kawahara); Division of Regional Community Development, Liaison Center for Innovative Dentistry, Graduate School of Dentistry, Tohoku University, Sendai, Japan (Jun Aida); Department of Oral Health Promotion, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University, Tokyo, Japan (Jun Aida); Center for Preventive Medical Sciences, Chiba University, Chiba, Japan (Katsunori Kondo); Center for Gerontology and Social Science, National Center for Geriatrics and Gerontology, Aichi, Japan (Katsunori Kondo); Departments of Health and Social Behavior, School of Public Health, University of Tokyo, Tokyo, Japan (Naoki Kondo); Department of Population Medicine, Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston, Massachusetts, United States (Peter James); Department of Environmental Health, T.H. Chan School of Public Health, Harvard University, Boston, Massachusetts, United States (Peter James); and Department of Urban Studies and Planning, Massachusetts Institute of Technology, Cambridge, Massachusetts, United States (Mariana Arcaya).
This study was supported by the US National Institutes of Health (grant R01 AG042463), the Japan Society for the Promotion of Science (grants KAKENHI 15H01972, KAKENHI 23243070, KAKENHI 22390400, KAKENHI 22592327, and KAKENHI 24390469), the Japanese Ministry of Health, Labour and Welfare (Health and Labour Sciences Research Grants H22-Choju-Shitei-008, H24-Choju-Wakate-009, H25-Choju-Ippan-003, H28-Choju-Ippan002, and H30-Junkankito-Ippan-004), the Japan Agency for Medical Research and Development (grants 16dk0110017h0002 and JP19dk0110034), the Japanese National Center for Geriatrics and Gerontology (Research Funding for Longevity Sciences grant 29-42), and the World Health Organization Centre for Health Development (WHO Kobe Centre) (grant WHO APW 2017/713981).
Conflict of interest: none declared.
REFERENCES
- 1. Noji EK. The Public Health Consequences of Disasters. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 2. Raker EJ, Lowe SR, Arcaya MC, et al. Twelve years later: the long-term mental health consequences of Hurricane Katrina. Soc Sci Med. 2019;242:112610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bland SH, Valoroso L, Stranges S, et al. Long-term follow-up of psychological distress following earthquake experiences among working Italian males: a cross-sectional analysis. J Nerv Ment Dis. 2005;193(6):420–423. [DOI] [PubMed] [Google Scholar]
- 4. Shiba K, Hikichi H, Aida J, et al. Long-term associations between disaster experiences and cardiometabolic risk: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Am J Epidemiol. 2019;188(6):1109–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khachadourian V. Effect of Earthquake-Related Losses and Post-Earthquake Events on Morbidity and Mortality: Causal Mediation Analysis of the Prospective Cohort Data of the 1988 Earthquake Survivors in Armenia [dissertation]. Los Angeles, CA: University of California, Los Angeles; 2019. [Google Scholar]
- 6. Holman EA. Psychological distress and susceptibility to cardiovascular disease across the lifespan: implications for future research and clinical practice. J Am Coll Cardiol. 2015;66(14):1587–1589. [DOI] [PubMed] [Google Scholar]
- 7. Mozaffarian D, Hao T, Rimm EB, et al. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Winning A, Glymour MM, McCormick MC, et al. Psychological distress across the life course and cardiometabolic risk: findings from the 1958 British Birth Cohort Study. J Am Coll Cardiol. 2015;66(14):1577–1586. [DOI] [PubMed] [Google Scholar]
- 9. Aida J, Hikichi H, Matsuyama Y, et al. Risk of mortality during and after the 2011 Great East Japan Earthquake and Tsunami among older coastal residents. Sci Rep. 2017;7(1):16591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Glymour MM, Avendano M, Kawachi I. Socioeconomic status and health. Soc Epidemiol. 2014;2:17–63. [Google Scholar]
- 11. Hikichi H, Aida J, Kondo K, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc Natl Acad Sci U S A. 2016;113(45):E6911–E6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hikichi H, Aida J, Tsuboya T, et al. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku earthquake and tsunami. Am J Epidemiol. 2016;183(10):902–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cox DR. Regression models and life-tables. J R Stat Soc B Methodol. 1972;34(2):187–202. [Google Scholar]
- 14. Hernán MA. The hazards of hazard ratios. Epidemiology. 2010;21(1):13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Young JG, Stensrud MJ, Tchetgen Tchetgen EJ, et al. A causal framework for classical statistical estimands in failure-time settings with competing events. Stat Med. 2020;39(8):1199–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hernán M, Robins J. Causal survival analysis. In: Causal Inference: What If. Boca Raton, FL: Chapman & Hall/CRC; Press; 2020:209–219. [Google Scholar]
- 17. Stensrud MJ, Hernán MA. Why test for proportional hazards? JAMA. 2020;323(14):1401–1402. [DOI] [PubMed] [Google Scholar]
- 18. Kario K, Ohashi T. Increased coronary heart disease mortality after the Hanshin-Awaji earthquake among the older community on Awaji Island. J Am Geriatr Soc. 1997;45(5):610–613. [DOI] [PubMed] [Google Scholar]
- 19. Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334(7):413–419. [DOI] [PubMed] [Google Scholar]
- 20. Muller JE, Verrier RL. Triggering of sudden death—lessons from an earthquake. N Engl J Med. 1996;334(7):460–461. [DOI] [PubMed] [Google Scholar]
- 21. Ogawa K, Tsuji I, Shiono K, et al. Increased acute myocardial infarction mortality following the 1995 Great Hanshin-Awaji Earthquake in Japan. Int J Epidemiol. 2000;29(3):449–455. [PubMed] [Google Scholar]
- 22. Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–625. [DOI] [PubMed] [Google Scholar]
- 23. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38(4):467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. North CS, Kawasaki A, Spitznagel EL, et al. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J Nerv Ment Dis. 2004;192(12):823–829. [DOI] [PubMed] [Google Scholar]
- 25. Mayeda ER, Tchetgen Tchetgen EJ, Power MC, et al. A simulation platform for quantifying survival bias: an application to research on determinants of cognitive decline. Am J Epidemiol. 2016;184(5):378–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Glymour MM, Vittinghoff E. Commentary: selection bias as an explanation for the obesity paradox: just because it’s possible doesn’t mean it’s plausible. Epidemiology. 2014;25(1):4–6. [DOI] [PubMed] [Google Scholar]
- 27. Stensrud MJ, Young JG, Didelez V, et al. Separable effects for causal inference in the presence of competing events [published online ahead of print June 24, 2020]. J Am Stat Assoc. (doi: 10.1080/01621459.2020.1765783). [DOI] [Google Scholar]
- 28. Hernán MA, Schisterman EF, Hernández-Díaz S. Invited commentary: composite outcomes as an attempt to escape from selection bias and related paradoxes. Am J Epidemiol. 2014;179(3):368–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chaix B, Evans D, Merlo J, et al. Commentary: weighing up the dead and missing: reflections on inverse-probability weighting and principal stratification to address truncation by death. Epidemiology. 2012;23(1):129–131. [DOI] [PubMed] [Google Scholar]
- 30. Chiba Y, VanderWeele T. A simple method for principal strata effects when the outcome has been truncated due to death. Am J Epidemiol. 2011;173(7):745–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Frangakis CE, Rubin DB. Principal stratification in causal inference. Biometrics. 2002;58(1):21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vanderweele TJ. Principal stratification—uses and limitations. Int J Biostat. 2011;7(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Egleston BL, Scharfstein DO, MacKenzie E. On estimation of the survivor average causal effect in observational studies when important confounders are missing due to death. Biometrics. 2009;65(2):497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ding P, Geng Z, Yan W, et al. Identifiability and estimation of causal effects by principal stratification with outcomes truncated by death. J Am Stat Assoc. 2011;106(496):1578–1591. [Google Scholar]
- 35. Shardell M, Hicks GE, Ferrucci L. Doubly robust estimation and causal inference in longitudinal studies with dropout and truncation by death. Biostatistics. 2015;16(1):155–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tchetgen Tchetgen EJ. Identification and estimation of survivor average causal effects. Stat Med. 2014;33(21):3601–3628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Tchetgen Tchetgen EJ, Phiri K, Shapiro R. A simple regression-based approach to account for survival bias in birth outcomes research. Epidemiology. 2015;26(4):473–480. [DOI] [PubMed] [Google Scholar]
- 38. Uemura Y, Taguri M, Kawahara T, et al. Simple methods for the estimation and sensitivity analysis of principal strata effects using marginal structural models: application to a bone fracture prevention trial. Biom J. 2019;61(6):1448–1461. [DOI] [PubMed] [Google Scholar]
- 39. Kondo K. Progress in aging epidemiology in Japan: the JAGES project. J Epidemiol. 2016;26(7):331–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kondo K, Rosenberg M, eds. Advancing Universal Health Coverage Through Knowledge Translation for Healthy Ageing: Lessons Learnt From the Japan Gerontological Evaluation Study. Geneva, Switzerland: World Health Organization; 2018. https://apps.who.int/iris/bitstream/handle/10665/279010/9789241514569-eng.pdf. Accessed March 1, 2020. [Google Scholar]
- 41. Miyagi Prefectural Government . Damage caused by the Great East Japan Earthquake as of February 29, 2016 [table; in Japanese]. Sendai, Japan: Miyagi Prefectural Government; 2016. http://www.pref.miyagi.jp/uploaded/attachment/347652.pdf. Accessed March 1, 2020. [Google Scholar]
- 42. Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3). (doi: 10.18637/jss.v045.i03). [DOI] [Google Scholar]
- 43. Sugishita K, Sugishita M, Hemmi I, et al. A validity and reliability study of the Japanese version of the Geriatric Depression Scale 15 (GDS-15-J). Clin Gerontol. 2017;40(4):233–240. [DOI] [PubMed] [Google Scholar]
- 44. Tsuboya T, Aida J, Hikichi H, et al. Predictors of depressive symptoms following the Great East Japan Earthquake: a prospective study. Soc Sci Med. 2016;161:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Knol MJ, Le Cessie S, Algra A, et al. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184(8):895–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hernán MA, Sauer BC, Hernández-Díaz S, et al. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. 2016;79:70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Smith LH, VanderWeele TJ. Bounding bias due to selection. Epidemiology. 2019;30(4):509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


