Abstract
We assessed whether race moderates the association between flourishing and all-cause mortality. We used panel data from the Midlife in the United States Study (MIDUS) (1995–2016; n = 2,851). Approximately 19% of White respondents and 23% of Black respondents in the baseline sample died over the course of the 21-year study period (n = 564). Cox proportional hazard models showed that Blacks had a higher mortality rate relative to Whites and higher levels of flourishing were associated with a lower mortality rate. Furthermore, a significant interaction between flourishing and race in predicting death was observed. Blacks with higher levels of flourishing had a mortality rate that was not significantly different from that of Whites. However, Blacks, but not Whites, with low flourishing scores had a higher mortality rate. As such, health-promotion efforts focused on enhancing flourishing among Black populations may reduce the Black–White gap in mortalityrate.
Keywords: flourishing, death, health disparities, race
Abbreviations
- BMI
body mass index
- CI
confidence interval
- HR
hazard ratio
- MIDUS
Midlife in the United States Study
- RERI
relative excess risk due to interaction
The Black–White gap in life expectancy is stark. In 2017, the life expectancy at birth was 75.6 years for Blacks and 78.5 years for Whites, a difference of 3.6 years (1). In addition, racial disparities in death persist through much of the life course, with Black Americans experiencing higher mortality rates than White Americans at nearly every age (2). Investigations into the causes of these differences have primarily focused on the role of socioeconomic (3), behavioral (4), or biomedical (5) risk factors, with much less attention paid to the role that psychosocial resources may play in shaping Black–White differences in mortality rates. This is an important omission, because psychosocial resources have the potential to protect against or help individuals cope with the noxious health consequences associated with being a member of a racial minority group (e.g., discrimination, social inequality) (6, 7). Indeed, some authors have reported that psychosocial resources can have a positive impact on longevity across the lifespan that is similar to the impact of diet and behavioral indicators such as smoking and alcohol consumption (8–10).
Increasing evidence links psychosocial resources, such as flourishing, to death (11). Flourishing is a multidimensional construct of well-being that integrates psychological, emotional, and social domains of well-being to capture complete mental health; that is, the ability to both feel good and function well in life (11, 12). The World Health Organization has defined complete mental health as “a state of well-being enabling individuals to realize their abilities, cope with the normal stresses of life, work productively and fruitfully and make contributions to their community” (13 (p12)). It has been argued that flourishing should be promoted because it is a means to a better, more productive, and healthy life (14). Several mechanisms have been proposed to delineate how flourishing “gets under the skin” to influence health. For instance, flourishing may protect health by promoting restorative health behaviors (e.g., physical activity, restful sleep, healthful food consumption) as well as by supporting more positive biological function (e.g., greater parasympathetic control, regulation of autonomic nervous system, lower levels of inflammation) (15). Moreover, individuals who are flourishing have lower prevalence of mood and anxiety disorders (16), chronic physical disease, health limitations of instrumental activities of daily living (12), and all-cause mortality at all ages (11). For example, Keyes and Simoes (11) found that adults who were flourishing had 62% lower odds of death at a 10-year follow-up relative to adults who were not flourishing. However, questions remain about whether the association between flourishing and death differs byrace.
We draw on 2 contrasting perspectives derived from existing work to situate race as a moderator of the flourishing and death association. The first perspective posits that psychosocial resources will be more beneficial for groups that have fewer alternative resources and worse socioeconomic conditions (17). If this is the case, then higher levels of flourishing will be more protective against death for Blacks than for Whites, because Black Americans are disproportionately exposed to social conditions that deplete psychosocial resources, including poverty, residential segregation, neighborhood insecurity, and racism (18). Consistent with this view, authors of some studies have found that religious attendance more strongly predicts lower mortality rates for Blacks than for Whites (19). For Whites, access to higher levels of psychosocial resources, like social support and sense of control (20, 21), as well as socioeconomic resources (22) may make any 1 resource, such as flourishing, less critical for health. In this view, the association between higher levels of flourishing and death will be greater for Blacks than for Whites, because they have fewer alternative resources to call on to protect their health.
In contrast, a second perspective suggests that higher levels of flourishing will be less beneficial for Blacks and more salutary for Whites. There is some evidence that psychosocial resources, such as sense of control over one’s life and general self-efficacy, reduce the risk of all-cause mortality for Whites but not Blacks (23, 24). These study findings suggest that Blacks receive fewer health benefits than Whites from the same psychosocial resource. Thus, the utility of flourishing, or any psychosocial resource, for racial minorities may be undermined by structural disadvantages that potentially offset the positive impact of a resource (25). This perspective implies the Black–White gap in death will increase as flourishing increases.
We used data from the National Survey of Midlife Development in the United States (MIDUS) cohort study (1995–2016) to examine the relationship between race, flourishing, and all-cause mortality. This is the first study, to our knowledge, to determine whether race moderates the association between flourishing and death. Here we discuss the implications of this research for policy and highlight the importance of considering the role that psychosocial resources play in the Black–White patterning of death in US society.
METHODS
We used data from MIDUS, a sample of 3,032 English-speaking, noninstitutionalized adults who were 25 to 74 years of age when the study was launched in 1995 (wave 1). Follow-up waves were conducted in 2004–2006 (MIDUS II) and 2013–2014 (MIDUS III), with high retention rates (e.g., 77% of living participants responded to the MIDUS III telephone survey). The MIDUS sampling weights were used in analyses to adjust for selection probabilities and nonresponse to ensure that the sample was representative of the US population. In the analyses we report on here, we selected only respondents identifying as Black or White who had valid death data; this resulted in a sample of 2,851 individuals, of whom 92% were White (n = 2,622) and 8% were Black (n = 229). The unweighted MIDUS sample slightly underrepresents Blacks.
Measures
We examined time to death (measured in months) as our dependent variable. MIDUS respondents from the baseline survey were linked to the 2016 National Death Index, the most recent mortality records available. Only all-cause mortality records were available in the National Death Index data linked to MIDUS respondents.
Following Keyes’ definition (26), composite flourishing was assessed with the components of emotional, psychological, and social well-being. Although there are multiple ways to measure flourishing (27, 28), we opted to use Keyes’ measure of flourishing because it is an established scale for measuring flourishing, is well validated, and has good psychometric properties (29). All components of flourishing were measured at wave 1 of MIDUS in our study. We followed a procedure developed by Chen et al. (30) to create a continuous measure of flourishing. Past research tended to rely on a binary indicator of flourishing based on being in the top tertile of the sample in flourishing (11). However, due to the potential limitations of using researcher-determined thresholds (e.g., top tertile split), we used a continuous measure of flourishing to capture its full distribution in the population. Results of prior research suggested evidence of a dose–response relationship between flourishing and death (11), thus supporting the treatment of flourishing as a continuous measure in the present study.
The first component of the flourishing score was emotional well-being. Two aspects of emotional well-being—positive affect and life satisfaction—were measured (11) using a 6-item, validated positive affect scale and a 1-item measure of life satisfaction. An overall emotional well-being score (α = 0.72) was calculated by summing the standardized positive affect and life satisfaction scores.
Psychological well-being was assessed with Ryff’s validated 18-item scale (31). The scale measured 6 dimensions of subjective well-being, including self-acceptance, positive relations with others, personal growth, purpose in life, environmental mastery, and autonomy (α = 0.71).
Finally, social well-being was measured with Keyes’ validated 15-item scale (32). The scale is used to assess 5 dimensions of social functioning: social acceptance, social actualization, social contribution, social coherence, and social integration. An overall social well-being score (α = 0.74) was calculated by summing scores on all 5 subscales.
An overall flourishing scale was then created by summing the standardized emotional, psychological, and social well-being scores. In our sample, flourishing scores ranged from –12.84 to 5.31. A full list of all scale items composing our measure of flourishing can be found in the Web Appendix (available at https://doi.org/10.1093/aje/kwab067).
Race was dichotomized as Black or White. We controlled for several demographic variables measured at wave 1 of MIDUS. We included the respondent’s age (in years) and the square of age to model the nonlinear relationship between age and death. We also adjusted for sex (male and female), marital status (married/marriage-like partnership and other) and education (less than a high school degree, high school degree or equivalent, some college, and university degree or higher). We also included in analyses a measure of household income, adjusted for the number of adults aged 18 years or older in the household. To adjust for the non-normality of the income variable, we categorized the household-size adjusted income into quintiles.
Analyses also were adjusted for a series of health conditions and health behaviors that could confound the relationship among race, flourishing, and death. First, we adjusted for several self-reported health conditions by including a dichotomous indicator to denote whether the respondent had experienced high blood pressure, lung problems, heart problems, stroke, diabetes, and cancer (except skin cancer, which is typically nonlethal). These are considered serious health conditions (33) and present the most acute risk of death. We also adjusted for respondents’ body mass index (BMI) (defined as underweight, BMI < 18.5; normal weight, 18.5 ≤ BMI < 25; overweight, 25 ≤ BMI < 30; obese class I, 30 ≤ BMI < 35; obese class II, 35 ≤ BMI < 40; and obese class III, BMI ≥ 40). Second, we included measures of health behaviors. We included 2 measures of cigarette smoking behavior (i.e., former smoker vs. never smoked and current smoker vs. never smoked). We also included a measure of self-reported monthly frequency of moderate or vigorous exercise (range = 0–27 days). Finally, we adjusted for sleep problems. Respondents were asked, “During the past 30 days, how often have you had trouble getting to sleep or staying asleep?” Answers were categorical, as follows: not at all, once a month, several times a month, once a week, several times a week, and almost everyday.
Statistical analysis
We conducted a series of Cox proportional hazard models on an analytic sample of 2,851 cases. Approximately 20% of the people in the baseline sample died over the course of the 21-year study period (n = 564), leaving 2,287 respondents censored.
In the Cox proportional hazards models, we used multiple imputation using chained equations to deal with missing data (34); 50 imputed data sets were created. This procedure yielded 2,851 cases for analysis. Results were also consistent using the listwise deletion method of handling missing data. To verify the proportional hazards assumption of Cox regression, Schoenfeld residuals were used (35). This test was nonsignificant (P > 0.05), yielding no evidence that the proportional hazards assumption was violated.
RESULTS
Table 1 presents a comparative overview of the sample characteristics by race. Approximately 19% of White respondents and 23% of Black respondents died over the study period, suggesting a slightly higher likelihood of Blacks dying before the end of the study period. Moreover, we found expected heterogeneity in flourishing scores by race: Whites had a mean flourishing score of 0.10 (standard deviation = 2.25), whereas Blacks had a significantly lower mean flourishing score of 0.002 (standard deviation = 2.39).
Table 1. Sample Descriptive Statistics of Participants (n = 2,851) by Race, Midlife in the United States Study, 1995–2016.
| Variable | Total Sample (n = 2,851) | % Missing Data | White (n = 2,622) | Black (n = 229) | T or Χ 2 (P Value) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Range | Mean (SD) a | No. | Mean (SD) | No. | Mean (SD) | No. | |||
| Flourishing (standardized) | −12.84, 5.31 | 0.01 (2.38) | 2,851 | 0 | 0.10 (2.25) | 2,622 | 0.002 (2.39) | 229 | <0.001 |
| Demographic Covariates | |||||||||
| Age | 21–75 | 48.11 (13.08) | 2,821 | <1 | 48.24 (13.13) | 2,601 | 46.25 (12.55) | 220 | <0.001 |
| Sex (Male = 1; referent) | 0.48 | 1,371 | 0 | 0.49 | 1,284 | 0.38 | 87 | <0.01 | |
| Adulthood Achieved Characteristics | |||||||||
| Married | 0.64 | 1825 | <1 | 0.66 | 1723 | 0.48 (102) | 102 | <0.001 | |
| Education | <1 | ||||||||
| < High school | 0.09 | 264 | 0.09 | 228 | 0.17 (36) | 36 | <0.001 | ||
| High school or equivalent | 0.30 | 828 | 0.29 | 770 | 0.27 (58) | 58 | |||
| Some college education | 0.31 | 891 | 0.31 | 822 | 0.33 (69) | 69 | |||
| University degree or higher | 0.30 | 851 | 0.31 | 802 | 0.23 (49) | 49 | |||
| Household Income, quintiles, USD | 3.3 | ||||||||
| 1 (0–22,500) | 0.20 | 536 | 0.18 | 448 | 0.44 (88) | 88 | <0.001 | ||
| 2 (22,501–40,500) | 0.20 | 557 | 0.20 | 524 | 0.16 (33) | 33 | |||
| 3 (40,501–64,500) | 0.20 | 551 | 0.21 | 526 | 0.12 (25) | 25 | |||
| 4 (64,501–111,500) | 0.20 | 554 | 0.21 | 528 | 0.13 (26) | 26 | |||
| 5 (111,501–≥300,000) | 0.20 | 564 | 0.21 | 535 | 0.14 (29) | 29 | |||
| Health conditions | |||||||||
| Cancer | 0.01 | 27 | <1 | 0.05 | 26 | 0.07 | 1 | 0.46 | |
| Heart problems | 0.13 | 348 | <1 | 0.13 | 327 | 0.10 | 21 | 0.26 | |
| Lung problems | 0.15 | 430 | <1 | 0.15 | 401 | 0.14 | 29 | 0.63 | |
| Diabetes | 0.06 | 149 | <1 | 0.05 | 130 | 0.09 | 19 | 0.01 | |
| Stroke | 0.01 | 29 | <1 | 0.01 | 26 | 0.01 | 3 | 0.54 | |
| BMI | <1 | ||||||||
| Underweight | 0.02 | 60 | 0.02 | 59 | 0.01 | 10 | <0.001 | ||
| Normal weight | 0.37 | 1,052 | 0.38 | 998 | 0.25 | 44 | |||
| Overweight | 0.35 | 1,001 | 0.35 | 927 | 0.35 | 74 | |||
| Obese class I | 0.14 | 397 | 0.14 | 359 | 0.18 | 38 | |||
| Obese class II | 0.04 | 127 | 0.04 | 113 | 0.06 | 14 | |||
| Obese class III | 0.07 | 197 | 0.06 | 166 | 0.14 | 31 | |||
| Health behaviors | |||||||||
| Former smoker | 0.31 | 877 | <1 | 0.31 | 820 | 0.27 | 57 | 0.18 | |
| Current smoker | 0.23 | 646 | <1 | 0.23 | 606 | 0.19 | 40 | 0.04 | |
| Exercise frequency | 0–27 | 14.61 (8.72) | 2,842 | <1 | 15.23 (8.66) | 2,622 | 11.58 (8.47) | 220 | <0.001 |
| Sleep problems | 1.8 | 0.09 | |||||||
| Not at all | 0.47 | 1,323 | 0.47 | 1,207 | 0.56 | 116 | |||
| Once a month | 0.14 | 404 | 0.15 | 380 | 0.12 | 24 | |||
| Several times a month | 0.15 | 415 | 0.15 | 386 | 0.14 | 29 | |||
| Once a week | 0.05 | 151 | 0.06 | 146 | 0.02 | 5 | |||
| Several times a week | 0.11 | 316 | 0.11 | 297 | 0.09 | 19 | |||
| Almost every day | 0.07 | 192 | 0.07 | 178 | 0.07 | 14 | |||
Abbreviations: BMI, body mass index; SD, standard deviation.
a Values are expressed as standard deviations.
Table 2 presents the hazard models for race, flourishing, and all-cause mortality. Model 1 was the baseline model of the association among race, flourishing, and death, in which only demographic covariates were adjusted for. In general, Blacks had a higher mortality rate relative to Whites (hazard ratio (HR) = 1.16, 95% confidence interval (CI): 1.03, 1.29), and those with higher flourishing scores had a lower mortality rate (HR = 0.94, 95% CI: 0.90, 0.99).
Table 2. Cox Proportional Hazard Models Predicting Death (n = 2,851), Midlife in the United States Study, 1995–2016.
| Characteristic | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Flourishing (standardized) | 0.94a | 0.90, 0.99 | 0.95a | 0.92, 0.98 | 0.98 | 0.93, 1.02 |
| Black race | 1.16a | 1.03, 1.29 | 1.20a | 1.05, 1.35 | 1.16 | 0.88, 1.54 |
| Flourishing × Black | 0.83b | 0.72, 0.95 | ||||
| Demographic covariate | ||||||
| Age, years | 1.07a | 1.00, 1.16 | 1.03 | 0.96, 1.10 | 1.05 | 0.97, 1.11 |
| Age, years2 | 1.00 | 0.99, 1.00 | 1.00 | 0.99, 1.00 | 1.00 | 0.99, 1.00 |
| Sex (Male = 1; referent) | 1.21 | 0.97, 1.50 | 1.28a | 1.03, 1.60 | 1.31a | 1.05, 1.62 |
| Married | 0.87 | 0.71, 1.08 | 0.94 | 0.75, 1.16 | 0.94 | 0.76, 1.16 |
| Education | ||||||
| High school or equivalent | 0.93 | 0.68, 1.26 | 0.97 | 0.72, 1.31 | 0.94 | 0.71, 1.26 |
| Some college education | 1.01 | 0.74, 1.37 | 0.99 | 0.72, 1.36 | 0.96 | 0.71, 1.30 |
| University degree or higher | 0.88 | 0.65, 1.19 | 0.97 | 0.70, 1.35 | 0.91 | 0.66, 1.25 |
| Household income, quintiles (1 = referent) | ||||||
| 2 | 0.70a | 0.52, 0.95 | 0.75 | 0.55, 1.02 | 0.77 | 0.57, 1.05 |
| 3 | 0.59c | 0.44, 0.80 | 0.59c | 0.44, 0.81 | 0.62c | 0.45, 0.84 |
| 4 | 0.73 | 0.52, 1.02 | 0.75 | 0.56, 1.02 | 0.78 | 0.58, 1.04 |
| 5 | 0.65c | 0.49, 0.86 | 0.72a | 0.53, 0.97 | 0.75 | 0.56, 1.02 |
| Health conditions | ||||||
| Had cancer | 1.08 | 0.43, 2.64 | 1.07 | 0.46, 2.46 | ||
| High blood pressure | 1.35c | 1.09, 1.68 | 1.37c | 1.10, 1.70 | ||
| Heart problems | 1.78b | 1.42, 2.22 | 1.77b | 1.42, 2.22 | ||
| Lung problems | 1.06 | 0.81, 1.39 | 1.08 | 0.82, 1.41 | ||
| Diabetes | 1.35a | 1.02, 1.79 | 1.35a | 1.02, 1.80 | ||
| Stroke | 1.22 | 0.73, 2.01 | 1.22 | 0.73, 2.02 | ||
| Underweight | 2.42c | 1.34, 4.40 | 2.54b | 1.40, 4.60 | ||
| Overweight | 0.81 | 0.63, 1.03 | 0.82 | 0.65, 1.05 | ||
| Obese class I | 1.03 | 0.76, 1.40 | 1.03 | 0.76, 1.40 | ||
| Obese class II | 1.15 | 0.72, 1.84 | 1.09 | 0.68, 1.74 | ||
| Obese class III | 0.92 | 0.64, 1.34 | 0.94 | 0.65, 1.37 | ||
| Health behaviors | ||||||
| Former smoker | 0.95 | 0.74, 1.39 | 0.93 | 0.73, 1.20 | ||
| Current smoker | 1.44c | 1.10, 1.89 | 1.46c | 1.08, 1.79 | ||
| Exercise frequency, days | 0.98b | 0.97, 0.99 | 0.98b | 1.12, 1.89 | ||
| Sleep problems | ||||||
| Once a month | 1.01 | 0.73, 1.39 | 0.96 | 0.70, 1.32 | ||
| Several times a month | 1.21 | 0.91, 1.61 | 1.17 | 0.89, 1.55 | ||
| Once a week | 1.27 | 0.63, 2.56 | 1.26 | 0.64, 2.49 | ||
| Several times a week | 0.79 | 0.58, 1.08 | 0.77 | 0.56, 1.05 | ||
| Almost every day | 1.00 | 0.69, 1.45 | 0.97 | 0.67, 1.40 | ||
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio.
a P < 0.05.
b P < 0.001.
c P < 0.01.
Model 2 retained all covariates from model 1, but we added in health covariates (namely, chronic disease diagnoses and health behaviors). However, the adjustment for a host of serious health conditions, and both positive and negative health behaviors (e.g., smoking, exercise) did little to change the hazard ratio between race and death or flourishing and death. Blacks continued to have a higher mortality rate relative to Whites (HR = 1.20, 95% CI: 1.05, 1.35), and higher flourishing scores again were linked with a lower mortality rate (HR = 0.95, 95% CI: 0.92, 0.98).
Finally, in model 3, we considered the interaction between flourishing and race. The significant interaction term indicated that the association between flourishing and death was greater among Blacks compared with Whites (HR = 0.83, 95% CI: 0.72, 0.95). There was no strong evidence of the relationship between flourishing and death for Whites (HR = 0.98, 95% CI: 0.93, 1.02). These findings were replicated in supplementary analyses (not shown) that were stratified by race. In addition, we also tested whether a flourishing by race interaction was significant in models 1 and 2. Results indicated that the flourishing by race interaction was significant across all models. These associations are seen more clearly in Figure 1, which presents a series of hazard curves depicting the relationship among race, flourishing, and death. We used 2 different cut points to determine high versus low flourishing: the mean (Figure 1A) and 1 standard deviation above the mean (Figure 1B), adjusting for the full range of study covariates.
Figure 1.
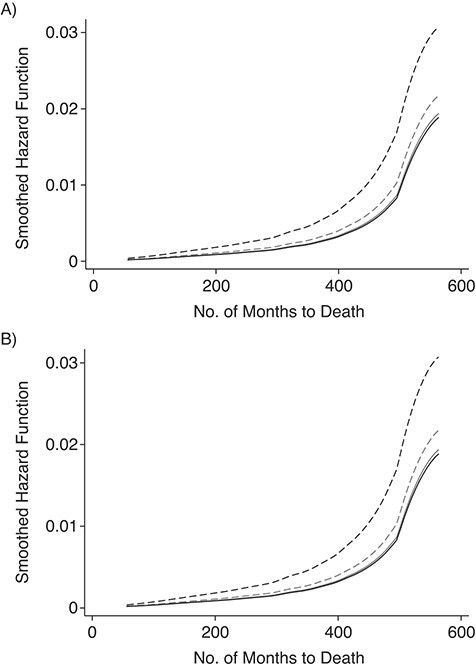
Hazard curves by race predicting A) months to death, using the mean level of flourishing to distinguish high versus low flourishing; B) months to death using 1 standard deviation above the mean level of flourishing to distinguish high versus low flourishing. Data are from the Midlife in the United States Study, 1995–2016 (n = 2,851). Dashed light grey line, Whites with low flourishing; solid light grey line, Whites with high flourishing; dashed black line, Blacks with low flourishing; solid black line, Blacks with high flourishing.
In Figure 1, we plotted time to death as a function of months. Figure 1 shows that Blacks with low flourishing scores had the highest mortality rate over time. Yet, Blacks with high flourishing had a mortality rate that was not significantly different than that of Whites. Post hoc pairwise comparisons of hazard ratios revealed that Blacks who had flourishing scores that fell 1 standard deviation above the sample mean had a mortality rate that was indistinguishable from that of Whites (P > 0.05). In contrast, Whites had a similar mortality rate regardless of level of flourishing.
We tested for an interaction on the additive scale as defined by Rothman (36) for calculating the relative excess risk due to interaction (RERI), using the methods outlined by Andersson et al. (37) and Knol and VanderWeele (38). We tested the additive interaction of 2 categorical variables (Blacks and Whites) and flourishing (high vs. low, with +1 standard deviation above the mean used to denote high vs. low flourishing), with controls in the model, but on our unweighted MIDUS sample, because weights are not yet supported in this method. RERI and the associated 95% confidence intervals were computed by the δ method, yielding and RERI of −0.58 (95% CI: −1.16, −0.01; P = 0.0467). A negative RERI value indicates a greater impact of high flourishing for Blacks in reducing mortality risk compared with that of Whites. The RERI value of −0.58 refers to an absolute risk difference; this suggests that the relative risk of death of Blacks with high levels of flourishing compared with that of Whites is 0.58 less than if there were no interaction.
We performed a series of robustness and sensitivity tests. First, a dichotomized measure of flourishing was created following initial criteria of Keyes and Simoes (11). To be characterized as flourishing, participants need to show high levels (i.e., top tertile) of emotional well-being on at least 1 of the 2 subscales (i.e., positive affect or life satisfaction) as well as high levels (i.e., top tertile) of psychological and social well-being on at least 6 of the 11 subscales (e.g., self-acceptance, social integration). Similar to what Keyes and Simoes (11) found with the MIDUS data, 18% of our sample met the criteria for flourishing. Second, to better capture functioning across all subdomains, we also created a count measure of flourishing that summed the number of subscales on which the participant had a score in the top tertile, ranging from 0 to 13 (30). The main pattern of results reported previously in this section was replicated with both alternative measures of flourishing.
Full results of these analyses can be found in Web Table 1 and Web Table 2. We conducted additional analyses (not shown) in which we also separately considered each component scale of flourishing, and results remained the same. This finding suggests that patterns observed and reported in the present study are not driven by 1 or 2 flourishing subscales.
DISCUSSION
This study provides new evidence of the additive and interactive relationships between race and flourishing on all-cause mortality. Our results support 3 key conclusions. First, we were able to reproduce the previously observed association between flourishing and death in a more recent MIDUS sample (11). Higher levels of flourishing were associated with lower rates of all-cause mortality. Second, we found that Blacks generally have lower levels of flourishing than Whites. Yet, despite this overall disadvantage, high levels of flourishing were protective for Blacks and not for Whites. Thus, our third key finding was that the association between flourishing and death was moderated by race. The racial gap in death became nonsignificant among persons with high levels of flourishing. In other words, Blacks with high levels of flourishing had the same mortality rate as Whites.
The beneficial impact of high levels of flourishing on death for Blacks, but not Whites, may be attributable to the fact that Blacks have fewer alternative socioeconomic resources, such as power, authority, and earnings, to draw on than do Whites, resulting in flourishing being especially protective against death for Blacks. From this perspective, flourishing substitutes for the lack of other health protective resources, which makes Blacks depend more heavily on flourishing than Whites. As such, high levels of flourishing may be a way that Blacks can compensate for some of the disadvantages associated with being Black in the United States. However, it is also important to note that Blacks with low levels of flourishing experience higher rates of mortality than do Whites for the very reason that they have fewer resources to call on to protect their health, making flourishing a particularly important resource for Black Americans.
The strengths of this study include the longitudinal design, the duration of the follow-up (21 years), and the examination of death, an objective outcome that is not biased by self-reports. However, this study was not without limitations. First, though the MIDUS data usefully linked respondents to national death records, we were unable to identify the specific causes of death. Thus, we could not test whether the relationship between race and flourishing persisted regardless of the cause of death (e.g., disease type vs. natural causes). Second, the MIDUS consists of a small sample of Blacks (n = 220), with approximately 51 Blacks dying over the study period, which limited our ability to draw definitive conclusions from our analyses. As such, our analyses should be replicated in a larger sample of Blacks.
Although the Black–White gap in death has narrowed in the United States, higher rates of mortality among Blacks than Whites have been characterized as a public health priority (39), in part because there is a general consensus that such inequalities are preventable (40). In this study, we found that high levels of flourishing were protective against death for Blacks but not for Whites. As such, promotion efforts should aim to develop flourishing among Blacks, especially Blacks who exhibit noticeably low levels of flourishing. Moreover, results from supplementary analyses indicate that emotional and social well-being are particularly important determinants of death. As such, interventions should especially focus on emotional and social well-being, although we believe that to flourish, emotional, social, and psychological well-being is necessary. Although the development of flourishing among at-risk populations may provide an approach to help reduce racial disparities in death, it is likely that a focus on individual-level interventions to enhance flourishing may not be sufficient to fully protect against the negative impact of social and economic hardships (41). As such, more research is needed to identify the modifiable conditions that produce flourishing in the first place, and at what stage of the life course they may best be implemented. Some evidence has indicated that employment (30), education (30), and income (30, 42) are particularly important determinants of flourishing, suggesting that programs that target the social determinants of health may increase flourishing in at-risk populations. Moreover, policy interventions that aim to reduce or eliminate social closures, where 1 group monopolizes valued resources by closing off opportunities to another group, have the potential to promote well-being (43, 44). Examples include enforcing laws that prohibit discriminatory practices that prevent Blacks from moving into White neighborhoods, or changing admissions practices that allow Blacks greater access into prestigious universities. More research should is needed to investigate how reducing social closure inequalities may lead to enhancing flourishing in Black communities. Taken together, individual health-promotion efforts to enhance flourishing among Black populations should occur alongside national policies aimed at addressing the social determinants of health, which may also decrease Black–White differences in death.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Sociology, University of Washington, Seattle, Washington, United States (Patricia Louie); Department of Sociology, Baylor University, Waco, Texas, United States (Laura Upenieks); Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada (Arjumand Siddiqi); Harvard T.H. Chan School of Public Health, Harvard University, Cambridge, Massachusetts, United States (David R. Williams); and Department of Sociology, School of Social Work, University of Washington, Seattle, Washington, United States (David T. Takeuchi).
Data availability: The data we used are publicly available through the Inter-university Consortium for Political and Social Research (https://www.icpsr.umich.edu/icpsrweb/ICPSR/series/203).
We thank Dr. Faraz Vahid Shahidi for helpful comments.
Conflict of interest: none declared.
REFERENCES
- 1. Kochanek KD, Murphy SL, Xu J, et al. Deaths: final data for 2017. Natl Vital Stat Rep. 2019;68(9):1–76. https://www.cdc.gov/nchs/products/index.htm. Accessed February 26, 2021. [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . African-American death rate drops 25 percent. 2017. https://www.cdc.gov/media/releases/2017/p0502-aa-health.html. Accessed February 26, 2021.
- 3. Howard G, Anderson RT, Russell G, et al. Race, socioeconomic status, and cause-specific mortality. Ann Epidemiol. 2000;10(4):214–223. [DOI] [PubMed] [Google Scholar]
- 4. Krueger PM, Saint Onge JM, Chang VW. Race/ethnic differences in adult mortality: the role of perceived stress and health behaviors. Soc Sci Med. 2011;73(9):1312–1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cohen SS, Signorello LB, Cope EL, et al. Obesity and all-cause mortality among black adults and white adults. Am J Epidemiol. 2012;176(5):431–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145–161. [DOI] [PubMed] [Google Scholar]
- 7. Gayman MD, Cislo AM, Goidel AR, et al. SES and race-ethnic differences in the stress-buffering effects of coping resources among young adults. Ethn Health. 2014;19(2):198–216. [DOI] [PubMed] [Google Scholar]
- 8. Yang YC, Boen C, Gerken K, et al. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci U S A. 2016;113(3):578–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ross CE, Mirowsky J. The sense of personal control: social structural causes and emotional consequences. In: Aneshensel CS, Phelan JC, Bierman A, eds. Handbook of the Sociology of Mental Health. Dordrecht, the Netherlands: Springer; 2013:379–402. [Google Scholar]
- 11. Keyes CLM, Simoes EJ. To flourish or not: positive mental health and all-cause mortality. Am J Public Health. 2012;102(11):2164–2172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Keyes CLM. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95–108. [DOI] [PubMed] [Google Scholar]
- 13. World Health Organization . Promoting Mental Health: Concepts, Emerging Evidence, Practice. Geneva, Switzerland: World Health Organization; 2004. https://www.who.int/mental_health/evidence/en/promoting_mhh.pdf. Accessed February 26, 2021. [Google Scholar]
- 14. Magyar JL, Keyes CLM. Defining, measuring, and applying subjective well-being. In: Gallagher MW, Lopez SJ, eds. Positive Psychological Assessment: A Handbook of Models and Measures. 2nd ed. Washington, DC: American Psychological Association; 2019:389–415. [Google Scholar]
- 15. Boehm JK, Kubzansky LD. The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012;138(4):655–691. [DOI] [PubMed] [Google Scholar]
- 16. Schotanus-Dijkstra M, Have MT, Lamers SMA, et al. The longitudinal relationship between flourishing mental health and incident mood, anxiety and substance use disorders. Eur J Public Health. 2017;27(3):563–568. [DOI] [PubMed] [Google Scholar]
- 17. Ross CE, Mirowsky J. Sex differences in the effect of education on depression: resource multiplication or resource substitution? Soc Sci Med. 2006;63(5):1400–1413. [DOI] [PubMed] [Google Scholar]
- 18. Williams DR, Mohammed SA, Leavell J, et al. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann N Y Acad Sci. 2010;1189:69–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li S, Okereke OI, Chang S-C, et al. Religious service attendance and lower depression among women—a prospective cohort study. Ann Behav Med. 2016;50(6):876–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barnes LL, Mendes De Leon CF, Bienias JL, et al. A longitudinal study of Black-White differences in social resources. J Gerontol B Psychol Sci Soc Sci. 2004;59(3):146–153. [DOI] [PubMed] [Google Scholar]
- 21. Oates GL, Goode J. Racial differences in effects of religiosity and mastery on psychological distress: evidence from national longitudinal data. Soc Ment Health. 2013;3(1):40–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325–334. [DOI] [PubMed] [Google Scholar]
- 23. Assari S. Race, sense of control over life, and short-term risk of mortality among older adults in the United States. Arch Med Sci. 2017;13(5):1233–1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Assari S. General self-efficacy and mortality in the USA; racial differences. J Racial Ethn Health Disparities. 2017;4(4):746–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. [DOI] [PubMed] [Google Scholar]
- 26. Keyes CLM. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–222. [PubMed] [Google Scholar]
- 27. Vanderweele TJ. On the promotion of human flourishing. Proc Natl Acad Sci U S A. 2017;114(31):8148–8156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Huppert FA, So TTC. Flourishing across Europe: application of a new conceptual framework for defining well-being. Soc Indic Res. 2013;110(3):837–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Keyes CLM. Brief description of the Mental Health Continuum Short Form (MHC-SF). 2009. https://www.aacu.org/sites/default/files/MHC-SFEnglish.pdf. Accessed February 26, 2021.
- 30. Chen Y, Kubzansky LD, VanderWeele TJ. Parental warmth and flourishing in mid-life. Soc Sci Med. 2019;220:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57(6):1069–1081. [Google Scholar]
- 32. Keyes CLM. Social well-being. Soc Psychol Q. 1998;61(2):121–140. [Google Scholar]
- 33. Ferraro KF, Farmer MM. Utility of health data from social surveys: is there a gold standard for measuring morbidity? Am Sociol Rev. 1999;64(2):303–315. [Google Scholar]
- 34. Royston P. Multiple imputation of missing values: update of Ice. Stata J. 2005;5(4):527–536. [Google Scholar]
- 35. Winnett A, Sasieni P. A note on scaled Schoenfeld residuals for the proportional hazards model. Biometrika. 2001;88(2):565–571. [Google Scholar]
- 36. Rothman KJ. Epidemiology: An Introduction. New York, NY: Oxford University Press; 2002. [Google Scholar]
- 37. Andersson T, Alfredsson L, Källberg H, et al. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20(7):575–579. [DOI] [PubMed] [Google Scholar]
- 38. Knol MJ, VanderWeele TJ. Recommendations for presenting analyses of effect modification and interaction. Int J Epidemiol. 2012;41(2):514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Roberts MT, Reither EN, Lim S. Contributors to Wisconsin’s persistent black-white gap in life expectancy. BMC Public Health. 2019;19(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the department of health and human services. Health Aff. 2011;30(10):1822–1829. [DOI] [PubMed] [Google Scholar]
- 41. Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100(4):590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Adkins L, Ylöstalo H. Experimenting with wellbeing: basic income, immaterial labour and changing forms of productivity. Crit Socio. 2021;47(3):373–387. [Google Scholar]
- 43. Bruch SK, Rosenthal AJ, Soss J. Unequal positions: a relational approach to racial inequality trends in the US states, 1940–2010. Soc Sci Hist. 2019;43(1):159–184. [Google Scholar]
- 44. Tilly C. Durable Inequality. Los Angeles, CA: University of California Press; 1998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


