Abstract
The Adolescent Brain Cognitive Development (ABCD) Study of 11,880 youth incorporates a comprehensive range of measures assessing predictors and outcomes related to mental health across childhood and adolescence in participating youth, as well as information about family mental health history. We have previously described the logic and content of the mental health assessment battery at Baseline and 1-year follow-up. Here, we describe changes to that battery and issues and clarifications that have emerged, as well as additions to the mental health battery at the 2-, 3-, 4-, and 5-year follow-ups. We capitalize on the recent release of longitudinal data for caregiver and youth report of mental health data to evaluate trajectories of dimensions of psychopathology as a function of demographic factors. For both caregiver and self-reported mental health symptoms, males showed age-related decreases in internalizing and externalizing symptoms, while females showed an increase in internalizing symptoms with age. Multiple indicators of socioeconomic status (caregiver education, family income, financial adversity, neighborhood poverty) accounted for unique variance in both caregiver and youth-reported externalizing and internalizing symptoms. These data highlight the importance of examining developmental trajectories of mental health as a function of key factors such as sex and socioeconomic environment.
Keywords: Psychopathology, Assessment, Mental health, Longitudinal assessment
1. Introduction
As described in numerous publications to date, the Adolescent Brain Cognitive Development℠ (ABCD) Study is a unique longitudinal study of almost 12,000 youth in the United States that will inform our understanding of the environmental, genetic, neurobiological, and behavioral factors that promote health and well-being, as well as those that put youth at risk for challenges in adaptive functioning and mental health. The ABCD Study® started when youth were 9 and 10 years old, and will run for at least 10 years. As described previously (Barch and Albaugh, 2018, Casey and Cannonier, 2018, Iacono and Heath, 2018, Luciana and Bjork, 2018, Hagler and Hatton, 2019, Karcher and Barch, 2020) and in other papers in this special issue, the ABCD Study is collecting a large range of data on each youth, including physical health data, neuroimaging data, biomarkers (e.g., hormones, DNA), assessment of cognitive function, reported substance exposures and use, as well as measures of the youth’s family and environment, including measures of the youth’s neighborhood and societal environment. As a central part of understanding well-being in youth, the ABCD Study assesses a broad range of constructs that both predict and denote outcomes related to adaptive function and mental health. In a previous publication (Barch et al., 2018), we described the process and principles that drove the development of the baseline battery of mental health-relevant measures. Here, we describe updates and changes to the mental health battery that have been or are being incorporated over the first six in-person assessment waves of the study, the principles that are driving decisions about what assessments are added to the study, which measures will continue to be assessed and at what frequency, and which measures have been dropped. We also overview known issues or considerations with measures that are being collected, and provide new data on longitudinal trajectories of both caregiver and youth reported mental health in relation to a number of important demographic factors (sex, race, caregiver education, socioeconomic status). The current membership of the ABCD Mental Health Assessment Workgroup is shown in Table S1.
2. Brief overview of the baseline ABCD demographics mental health battery
We described the justification and purpose of the baseline ABCD baseline demographics and mental health battery in the first ABCD Special Issue in Development Cognitive Neuroscience. The development of this battery was guided by the existing literature in relevant constructs and measures, developmental appropriateness and ability to be usable across adolescence, the feasibility and reliability of use across many sites, evidence about the psychometric properties of the instruments, ability to harmonize with previous or ongoing studies where possible, and measures that have been recommended as common data elements by the PhenX initiative (Stover and Harlan, 2010, Hamilton and Strader, 2011, Maiese and Hendershot, 2013, McCarty and Huggins, 2014) or other NIH assessment initiatives (Conway and Vullo, 2014, Barch and Gotlib, 2016). These same principles continued to guide our decisions about updates and expansions to the ABCD Mental Health Battery over the ongoing waves of assessment.
As shown in Table 1, Table 2, we assess constructs relevant to the youth’s adaptive function and mental health from the perspective of the caregiver, the youth themselves, and the youth’s teachers. In terms of demographics, we collect a range of information about socioeconomic status and financial insecurity (Diemer et al., 2012), household composition (McLoyd, 1998, Smith and Marsden, 2015), race and ethnicity of the youth and the extended family, gender identity and sexual orientation. Since the publication of the original paper on the mental health assessments in the ABCD, Gender Identity and Sexual Health has become a stand-alone workgroup, and thus the changes to the measures of gender identity and sexual orientation are described in another paper in this special issue and modifications to the demographic measures over assessment waves are described in Section 3.1 below. We also ask both youth and caregivers to report on school performance, numbers of friends and friendship quality and bullying (see Section 3.5 for additional measures of peer relationships (Prinstein and Boergers, 2001, De Los Reyes and Prinstein, 2004) and cyberbullying (Stewart et al., 2014) added in Year 2).
Table 1.
Caregiver report about youth and self/family.
| Baseline | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
|---|---|---|---|---|---|---|
| Ages | Ages 9.0–11.1 | Ages 9.7–12.4 | Ages 10.6–13.6 (though 1/2020) | Ages 12–14 (projected) | Ages 13–15 (projected) | Ages 14–16 (projected) |
| Month/Years of Data Collection | 2016–2018 | 2017–2021 | 2018–2021 | 2019–2021 | 2020-(ongoing) | 2021-(ongoing) |
| Measure | ||||||
| Caregiver Report About Youth | ||||||
| Demographics (Income, Financial Stability, Household composition, race, ethnicity, occupation, etc.) | X | X | X | X | X | X |
| KSADS Background (school performance, mental health treatment, friends, bullying, etc.) | X | X | X | X | X | X |
| KSADS-COMP | X | X | X | X | X | X |
| Child Behavior Checklist (CBCL) | X | X | X | X | X | X |
| General Behavior Inventory 10 item Mania Scale (GBMI) | X | X | X | – | X | X |
| Short Social Responsiveness Scale (SSRS) | – | X | – | – | – | X |
| Life Events Experienced by Youth | – | X | X | X | X | X |
| Early Adolescent Temperament Questionnaire (EATQ) | – | – | X | – | – | – |
| Difficulty in Emotion Regulation Scale (DERS) | – | – | – | X | X | X |
| Caregiver Report About Self/Family | ||||||
| Family History Assessment Module | X | – | – | – | – | – |
| Adult Self Report | X | – | X | – | X | – |
| Adult Behavior Checklist | – | – | X | – | X | – |
| Perceived Stress Scale | – | – | – | X | – | – |
| Parent Self-Report Brief Diagnostic Assessment Module | – | – | – | – | – | – |
| Other Parent-Report Brief Diagnostic Assessment Module | – | – | – | – | – | – |
Table 2.
Youth report about self.
| Baseline | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
|---|---|---|---|---|---|---|
| Ages | Ages 9.0–11.1 | Ages 9.7–12.4 | Ages 10.6–13.6 (though 1/2020) | Ages 12–14 (projected) | Ages 13–15 (projected) | Ages 14–16 (projected) |
| Month/Years of Data Collection | 2016–2018 | 2017–2021 | 2018–2021 | 2019–2021 | 2020-(ongoing) | 2021-(ongoing) |
| Measure | ||||||
| KSADS Background (school performance, mental health treatment, friends, bullying, etc.) | X | X | X | X | X | X |
| KSADS-COMP (Kobak et al., 2013) | X | X | X | X | X | X |
| Brief Problem Monitor-Youth (BPM-Y) | – | X | X | X | X | X |
| NIH Toolbox Positive Affect Items | – | X | – | X | – | X |
| 7-Up Mania Scale (7-UP) | – | X | – | X | – | X |
| Psychosis Questionnaire-Brief Child (PQ-BC) | X | X | X | X | X | X |
| Urgency, Perseverance, Premeditation, and Sensation Seeking (UPPS-Child) | X | – | X | – | X | – |
| Behavioral Inhibition and Behavioral Activation Scale (BIS-BAS) | X | – | X | – | X | – |
| 10-Item Delinquency Scale | – | X | X | X | X | – |
| Life Events Experienced by Youth | – | X | X | X | X | X |
| Emotion Regulation Questionnaire | – | – | – | X | X | X |
| Number of Friends and Close Friends | ||||||
| Peer Experiences Questionnaire | – | – | X | X | X | X |
| Cyberbullying Questionnaire | – | – | X | X | X | X |
2.1. Mental health diagnoses
From caregiver and youth perspective, information is obtained about both current and lifetime mental health diagnoses of the youth using a validated and computerized Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS) for DSM-5 (KSADS-COMP), developed by Dr. Joan Kaufman and Dr. Ken Kobak with NIH Small Business Innovation Research support (Kobak and Kratochvil, 2013, Kobak and Kaufman, 2015). This is a self-administered, computerized version that does not involve a clinician for either the caregiver or the youth, though the youth are supported in completing the KSADS-COMP by trained research assistants. In Section 3.2 below, we provide more information about changes in this measure over assessment waves and known issues or considerations in the use of data from the KSADS-COMP.
2.2. Dimensional measures of mental health relevant constructs
Dimensional measures of mental health from caregivers, youth and teachers were also obtained. As shown in Table 1, starting at baseline, caregivers report annually about the youth’s behavior using the Child Behavior Checklist (CBCL) (Achenbach, 2009) as a broad measure of many domains and about dimensional mania symptoms using the ten-item Mania Scale (Youngstrom et al., 2008) derived from the 73-item Parent General Behavior Inventory (PGBI) for Children and Adolescents (Youngstrom et al., 2001). As shown in Table 2, youth reported about their own mental health every six months (starting at the first six month mid-year assessment) using the Brief Problem Monitor for youth (BPM-Y) (Achenbach, 2009) and the positive affect items from the NIH Toolbox Battery (Gershon and Wagster, 2013, Salsman and Butt, 2013). In Section 3.3 below, plans to move the assessment from the BPM-Y to the more comprehensive Youth Self-Report (YSR) are outlined. Youth also report annually on psychotic-like experiences using the Prodromal Questionnaire Brief Version-Child (Karcher and Barch, 2018, Karcher and Loewy, 2020), and bi-annually on impulsivity using a brief urgency, perseverance, premeditation, and sensation seeking (UPPS) scale (Watts et al., 2020), mania using the 7-item child report of mania called the 7-Up (Youngstrom et al., 2013) (starting at Year 1), and on behavioral activation and inhibition using the BIS-BAS (Carver and White, 1994, Pagliaccio and Luking, 2016).
At the Year 1 assessment, as shown in Table 1, Table 2, caregivers also started reporting on behaviors relevant to the autism spectrum, using the brief Social Responsiveness Scale (Reiersen et al., 2008). We also started asking youth at Year 1 to annually report on their own delinquency-relevant behaviors using a 10-item shortened version of the scale developed for use in the Causes and Correlates of Delinquency Program (Hoeve and Blokland, 2008, Theobald and Farrington, 2014). See Section 3.4 for issues related to the use and interpretation of data from this measure. As described in more detail in Section 3.8, at Year 1 we also began annual administration of the Adverse Life Events Scale (Tiet and Bird, 2001, Grant and Compas, 2004) from the PhenX collection asking for both caregiver and youth reports about events that the youth experienced. At Year 2, we also added a caregiver report measure of youth temperament called the Early Adolescent Temperament Scale (Latham et al., 2020) at Year 2 (see Table 1 and Section 3.7) and both caregiver (Difficulties in Emotion Regulation Scale (Bardeen and Fergus, 2016, Lee and Witte, 2016, Benfer and Bardeen, 2019, Bunford and Dawson, 2020)) and youth (Emotion Regulation Questionnaire (Gullone and Taffe, 2012)) report measures of emotion regulation starting at Year 3 (see Table 1, Table 2 and Section 3.6).
2.3. Teacher report
To provide converging evidence about the youth’s behavior, families are asked to give permission to allow their youth’s teacher to complete the Brief Problem Monitor – Teacher Form (Achenbach, 2009) at each assessment wave. See Section 3.3 for discussion of how teachers were selected and considerations in the use of BPM-T data.
2.4. Caregiver/family mental health and personality
As shown in Table 1, at baseline we used a version of the Family History Assessment Module Screener (FHAM-S) (Rice et al., 1995) that was used in the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study (http://www.ncanda.org/index.php) (Brown et al., 2015). The engaged caregiver reports on the presence/absence of symptoms associated with alcohol use disorder, substance use disorder, depression, mania, psychosis, and antisocial personality disorder in all 1st and 2nd degree “blood relatives” of the youth, defined as biological relatives including full and half-siblings, parents, grandparents, and aunts and uncles. See Section 3.9 for more information on the scoring of the FHAM-S data and interpretation. We also ask the study-engaged caretaker to complete the Adult Self Report (Achenbach, 2009) bi-annually, and to also complete the Adult Behavior Checklist (Achenbach, 2009) about the other caregiver bi-annually starting at Year 2. See Section 3.3 on how the other caregiver was selected and interpretation of these data. We began asking the study-engaged caretaker to complete the Perceived Stress Scale (Cohen et al., 1983) about their own level of stress bi-annually starting at Year 3 (see Section 3.10). Ideally, it is the same caregiver every year, but this has not always been the case. A more detailed update on caregiver mental health history (both engaged caregiver and report on other caregiver) is planned for Year 6 (see Section 3.9).
3. Updates and known issues in the demographic and mental health assessments in the ABCD study
In this section, we provided updates/additions to the different subdomains of assessment under demographics and mental health, followed by known issues or specific considerations when present.
3.1. Update: demographic assessments
Caregivers complete demographic assessments at every visit. Every year, caregivers provide demographic information about the child, themself and a partner, which specifically refers ‘to any significant person in [the] child’s life that helps in raising [the] child or has helped for more than 2 years and who is involved in 40% or more of the daily activities of [the] child’. Information about both the caregiver and child includes age, sex, race, ethnicity, gender identity, religious preferences and experiences and native language. The caregiver additionally provides information about their current marital status, highest education level, current employment status, work sector, income, and their partner’s relationship to child, highest education level, employment status, work sector and income, and a combined total household income. In addition, every year caregivers also report how much time the child spends in different households, how people live at their address, household member’s relationship to the caregiver and details of any financial difficulties faced in the past 12 months (e.g. could not afford food, had services turned off because payments were not made). At Year 1 (and continuing annually), additional questions were introduced regarding whether the child was covered by any health insurance or coverage plans at the time of data collection. At Year 2 (and continuing annually), an occupation survey was added to provide a detailed characterization of both the caregiver and partner’s work sector and job title to allow a more precise quantification of socioeconomic status (SES). Occupations are being coded based on the American Community Survey/Census categories.
3.2. Update and known issues: KSADS-COMP for DSM 5
Table S2 shows the KSADS modules completed by caregivers and youth at each annual assessment There are a number of modules that caregivers have reported on every year (psychosis, eating disorders, ADHD, conduct disorder) since we did not have other assessments of these constructs. Most of the other modules are completed every other year by caregivers. For youth, the only module they complete every year is the suicidality module, as this is the only self-report of this information, with mood disorders, social anxiety, generalized anxiety and sleep every other year starting at baseline, and eating disorders and conduct disorder added at year two. Youth complete the alcohol or drug use modules starting in Year 1 if they report use of any substances. As can be seen in Table S2, caregivers are completing many more modules than youth, particularly at the early assessment waves. This was purposeful, both from the perspective of burden on the youth (they have many assessments to complete) and because we felt that there were many domains on which caregivers would be much better reporters than children (e.g., externalizing disorders, tics) earlier in adolescence. However, we have been gradually adding more modules for youth to complete over the assessment waves, as we feel they are better able to accurately report on facets of their behavior. The first three years of assessments (baseline, Year 1, Year 2) used the KSADS 1.0, which was the version available at the time that the study started. We switched to the KSADS 2.0 at Year 3 as this updated version incorporates several improved features, including better assessments of Autism Spectrum and Psychotic disorders.
There are several important issues that inform the use of the KSADS data. First, the KSADS-COMP was designed to be an efficient self-administered evaluation of DSM symptoms, therefore, response options across the current (past two-weeks) and past (ever) questions do not necessarily correspond to recommended criterion thresholds for DSM symptoms. For example, the questions framed as ever experiencing a symptom or displaying a behavior are evaluated with a two-choice (yes/no) option. For disorders, such as Conduct Disorder or Major Depressive Disorder, where the behaviors should occur repeatedly or over a certain number of days to meet the symptom criterion, the KSADS-COMP diagnosis is most conservatively conceptualized as an estimated or approximated DSM diagnosis. Second, while there is an item labeled “Diagnosis - Other Specified Neurodevelopmental Disorder, Autism Spectrum Disorder, full criteria not assessed (F88.0)” this should not be used as an indication of an Autism Spectrum Disorder. The KSADS 1.0 asks questions about some behavioral features relevant to Autism Spectrum Disorder, but does not do a full evaluation nor does it generate a diagnosis. Third, there are diagnoses for Schizophrenia, Schizophreniform and Schizoaffective disorder in KSADS 1.0, but they were not based on a full evaluation and thus should not be used as indicators of a diagnosis. Fourth, the Agoraphobia questions were accidentally omitted when we changed platforms for a brief period of time (6 months). Fifth, all of the diagnoses and symptoms are presented as 0 (absent) or 1 (present), and do not use the more elaborated coding typically used in the KSADS (0 = not enough information, 1 = absent, 2 = subthreshold, 3 = present), though we are working on generating these data for future releases. Sixth, the KSADS uses a screening module, and then additional questions are asked if items on the screening module are answered affirmatively. For symptom items, we coded them separately if they were deliberately not asked (888) because the individual did not answer screening items affirmatively (i.e., due to branching logic), as compared to not administered at that wave (555). Sixth, the computerized KSADS 1.0 shows higher than expected rates of caregiver- and youth-reported past manic episodes (i.e., the caregiver-reported prevalence of Bipolar I Disorder, most recent past episode manic is 2.6%). To address for these higher than expected rates, we recommend rescoring Bipolar I Disorder, most recent past episode manic so that the youth has to meet criteria for past manic episode and any current or past depressive disorder (e.g., major depressive disorder, persistent depressive disorder, other specified depressive disorder) in order to meet diagnostic criteria.
Lastly, in May of 2021, the KSADS-COMP originators did a review of diagnostic criteria used in the programming algorithms, and found several errors that likely led to overestimates of diagnoses. The needed modifications are: a) need to include impairment in the diagnostic criteria for Major Depression and Persistent Depressive Disorder; b) need to include onset before age 10 in the diagnostic criteria for Disruptive Mood Dysregulation Disorders; c) need to require impairment in two domains, not just one, for Attention Deficit Hyperactivity Disorder; d) need to require an illness duration of 6 months or more for Agoraphobia; e) need to include an illness duration of three months or longer for Anorexia; and f) need to include the presence of all three criterion A symptoms for Autism (relevant to the 2.0 version). The KSADS-COMP will be modified with these updated criteria by June 1 of 2021, and the ABCD team is working with KSADS-COMP to correct diagnoses in already acquired data.
3.3. Update: ASEBA scales in the ABCD: BPM-Y, BPM-T, YSR, ASR and ABCL
The Achenbach System of Empirically Based Assessment (ASEBA) was employed in order to obtain longitudinal, dimensional assessments of child and caregiver psychopathology. This family of instruments assesses a number of empirically derived syndromes that were developed in a “bottom up” fashion using factor analytic methods (Achenbach and Rescorla, 2001). The structure of these empirically derived syndromes are remarkably stable across various societies and cultures—making it an ideal set of instruments given ABCD’s large and diverse sample (Achenbach and Rescorla, 2007, Achenbach and Rescorla, 2015). ASEBA empirically derived syndromes can be assessed across the developmental span, allowing for the same psychopathological constructs to be measured longitudinally across ABCD’s 10-year duration. The ASEBA battery has been used in other large longitudinal studies such as Generation R study in the Netherlands (Jaddoe et al., 2006), which will allow for cross-cultural comparison and facilitate communication of findings.
The ASEBA family of instruments affords for multi-informant assessment of developmental psychopathology. This methodological feature is capitalized upon in the ABCD Study, enabling multiple informants to rate child behavior in different settings (e.g., home, school). Starting at the baseline visit, the caregiver annually completes the Child Behavior Checklist (CBCL) on their child’s behavior. Beginning at the 6-month follow-up, the youth version of the Brief Problem Monitor (BPM-Y) is administered every 6 months. Thus, the BPM-Y is particularly useful in monitoring the longitudinal course of youth functioning. Complementing caregiver- and self-report, teachers complete the Brief Problem Monitor teacher’s form (BPM-T) on youth. In selecting the BPM-T informant, caregivers were asked to choose the teacher who had the most frequent contact with their child (preferably not Gym/Physical Education teachers unless there were no academic teachers available). An email was then sent to the identified teacher which included a confidential link to the web-based BPM-T. If a child had a study visit during the summer months, study staff would wait to gather teacher information at the 6-month follow-up phone call. This was done to ensure that the teacher completing the BPM-T was familiar with the child. To date, 42%, 54%, and 54% of teachers have provided reports for Baseline, Year 1, and Year 2 respectively.
The BPM-Y and BPM-T were administered in lieu of the longer Youth Self-Report (YSR) and Teacher’s Report Form (TRF) measures (Achenbach and Rescorla, 2001, Achenbach and McConaughy, 2017) to lessen the burden on participants and teachers. The BPM-Y and BPM-T consist of a subset of items from the YSR and TRF (19 and 18 items, respectively) and yield scores for Internalizing, Attention Problems, Externalizing, and Total Problems scales (Achenbach et al., 2017), though they do not address psychosis. The YSR will be administered mid-year during Year 4 which will provide comprehensive coverage of all ASEBA empirically derived syndromes.
Lastly, caregiver functioning is a vital component of the family environment. Conveniently, ASEBA allows for the same empirically derived psychopathological constructs to be assessed in caregivers. Beginning at the baseline visit, the parent/caregiver annually completes the Adult Self Report (ASR) on their own behavior (Achenbach and Rescorla, 2003). At Year 2, the parent/caregiver also completes the Adult Behavior Checklist (ABCL) (Achenbach and Rescorla, 2003) on the other biological parent who lives with the child, or on the other caregiver in the home who has lived with the child for at least 6 months. If the primary parent/caregiver did not live with the child's other parent/caregiver, the ABCL was still completed provided the child had regular contact with the other parent/caregiver.
3.4. Update and known issues: brief delinquency measure
While the baseline ABCD protocol includes some items in which caregivers reported on youth delinquent behaviors (e.g., KSADS conduct disorder), youth self-report in this arena was not included. “Delinquent behaviors” may be defined as antisocial acts that violate societal norms and laws (Isen et al., in press). Since youth may engage in delinquent acts (i.e., violating social norms and laws (Isen et al., in press)) that escape detection by caregivers and may not be recorded in official records, self-reported delinquency has become central to the study of adolescent delinquent and/or criminal behavior (Piquero et al., 2002). To provide a brief assessment of a range of delinquent behaviors varying in severity, ten items were selected from a version of the Self-Reported Delinquency Scale (SRD) (Elliot et al., 1989) adapted for the Pittsburgh Youth Study and the Pittsburgh Girls Study (Loeber et al., 2008). The ten items, titled the Brief Delinquency Measure, were added starting in Year 1 (see Clark et al. Table 1 for items).
In recent work, we have conducted analyses of measurement invariance across race and sex on the SRD and examined the items for differential item functioning. These analyses, which are reported in detail in Clark et al. (in preparation) revealed evidence of differential item function. The item related to being arrested by the police showed that, for the same putative level of trait delinquency, Black youth were much more likely to have been arrested by police. This pattern is consistent with the evidence of systemic racism in regard to Black youths’ experience with police. As such, we moved the item about being arrested to a new measure that asks more extensive questions about the role of police in a child’s community to assess this information in a broader cultural and environmental context. Further, it was noted that other items asked about youth being told they are being too rowdy, which may reflect differential experiences of Black youth rather than delinquency per se (Fadus et al., 2020). The general review of measures related to delinquency and antisocial behavior also revealed concerns that this 10-item SRD measure needed to be modified and supplemented by items from other scales to more fully capture a broader range of delinquent behaviors in a more comprehensive and, potentially, less biased manner. Thus, the choice has been made to discontinue the SRD starting at the Year 4 follow up, and to instead modify the Conduct Disorder section of the KSADS-COMP such that all youth are asked all of the potential behavioral indicators of Conduct Disorder, and the Callous and Unemotional trait questions are asked of any youth that endorses 1 or more Conduct Disorder indicators. This will reduce redundancy across measures in the ABCD and ensure that a broader set of behaviors relevant to delinquency are assessed. The ABCD study recognizes the importance of conducting such invariance analyses for all measures, and is working to identify ways to support such analyses.
3.5. Update: peer relationships and cyberbullying
Peer relationships are a key part of adolescent life. Peer victimization (both being a perpetrator and/or victim of bullying) has negative associations with outcomes that last well beyond adolescence. To capture these experiences, beginning in Year 2, youth complete the Revised Peer Experiences Questionnaire (Prinstein and Boergers, 2001, De Los Reyes and Prinstein, 2004). This is an 18-item questionnaire that yields scores for overt, relational and reputational aggression (both being a victim and perpetrator). Adolescent peer relationships occur both in person and virtually, and so two questions were added to capture cyberbullying (Stewart et al., 2014). Youth are asked “Have you ever been cyberbullied, where someone was trying on purpose to harm you or be mean to you online, in texts, or group texts, or on social media (like Instagram or Snapchat)?” They are also asked about cyberbullying another person.
3.6. Updates to emotion regulation
Emotion regulation, or the ability to modulate one’s emotions, is important for healthy functioning and undergoes substantial change across development (Cole et al., 1994). Moreover, difficulties with emotion regulation have been identified as a transdiagnostic risk factor for many forms of psychopathology (Southam-Gerow and Kendall, 2002, Aldao and Gee, 2016). To assess emotion regulation in the ABCD Study, we added the child-reported Emotion Regulation Questionnaire for Children and Adolescents (ERQ-CA; (Gullone and Taffe, 2012)) and caregiver-reported Difficulties in Emotion Regulation Scale (DERS-P; (Bunford et al., 2020)). The ERQ-CA, which was developed based on the original Emotion Regulation Questionnaire (Gross and John, 2003), examines the tendency to use two specific emotion regulatory strategies—cognitive reappraisal and expressive suppression. We selected 3 items assessing cognitive reappraisal (e.g., “When I want to feel less bad (e.g., sad, angry, worried) about something, I think about something different”) and 3 items assessing expressive suppression (e.g., “I control my feelings by not showing them”) from the 10-item measure. The ERQ-CA has shown good internal consistency and test-retest reliability over 12 months in a sample of 10–18 year-olds. The DERS-P examines difficulties across domains related to nonacceptance, goals, impulses, strategies, awareness, and clarity. The DERS-P was validated in a sample of 11–17 year-olds and has been shown to have good concurrent and convergent validity (Bunford et al., 2020). We selected 29 items from the DERS-P, eliminating 7 items administered in the original study that did not load onto any factors.
3.7. Update: temperament and personality
In Year 2, the Early Adolescent Temperament Questionnaire-Revised (EATQ-R; parent version) (Capaldi and Rothbart, 1992) was added to the caregiver assessment battery. The EATQ-R, designed to assess temperament in adolescents from ages 9–15, assesses eight primary dimensions of temperament, two dimensions of behavior, and three higher-order dimensions that subsume these primary dimensions. The eight primary temperament dimensions include: Activation Control-capacity to perform an action when there is a strong tendency to avoid it, Affiliation-desire for warmth and closeness with others, independent of shyness or extraversion, Attention-capacity to focus attention as well as to shift attention when desired, Fear-unpleasant affect related to anticipation of distress, Frustration-negative affect related to interruption of ongoing tasks or goal blocking, Surgency/High Intensity Pleasure-pleasure derived from activities involving high intensity or novelty, Inhibitory Control-capacity to plan, and to suppress inappropriate responses, and Shyness-behavioral inhibition to novelty and challenge, especially social. The two behavioral scales include: Aggression-hostile and aggressive actions (person & object directed physical violence, direct & indirect verbal aggression, hostile reactivity) and Depressive Mood-unpleasant affect and lowered mood, loss of enjoyment and interest in activities.
Inclusion of caregiver-rated, dimensional, temperamental traits is useful for obtaining perceptions of individual differences from the perspective of an adult who interacts considerably with the youth. Future personality assessments will maintain the focus on impulsivity-related traits given their relevance for understanding substance use disorders and other externalizing psychopathology, and on behavioral inhibition for understanding internalizing disorders. In future waves, we plan to assess youth-reported “Big Five” traits to have a well-established framework for characterizing personality more generally and track personality development into late adolescence and young adulthood.
3.8. Update: life events
The original Adverse Life Events Scale (Tiet et al., 2001) is a 25-item questionnaire that includes a variety of events such as whether caregiver(s) had drug problems, lost a job, went to jail, was away from home more than usual, left home/divorced; family member or close friend was injured, seriously sick, or died; participant was seriously sick or injured; or participant saw a crime/accident or was the victim of a crime. Updates to the protocol at Year 4 included items for caregiver being deported; youth being placed in foster care; seeing someone getting beaten up in school/neighborhood or shot at; and having a lockdown at school due to concerns about violence. At the yearly study visit, the youth and caregivers indicate whether each life event happened to them in the prior year (yes/no). For all events that did happen, caregivers and youth are asked whether the experience was good or bad (mostly good, mostly bad, not applicable, or don’t know). They are then asked how much the event affected them (not at all, a little, some, or a lot). Scoring yields the number of total events; events characterized by the participant as bad (response of mostly bad and a little, some or a lot bad); and events characterized by the participant as good (response of mostly good and a little, some or a lot good).
3.9. Update: family history
As described previously, in ABCD we employed a version of the Family History Assessment Module Screener (FHAM-S) (Rice et al., 1995) that was used in the National Consortium on Alcohol and Neurodevelopment in Adolescence (NCANDA) study (http://www.ncanda.org/index.php). In the ABCD FHAM-S version, we had a caregiver report on the presence/absence of symptoms associated with alcohol use disorder, substance use disorder, depression, mania, psychosis, and antisocial personality disorder in all 1st and 2nd degree “blood relatives” of the youth. (That is, biological relatives including full and half-siblings, parents, grandparents, and aunts and uncles.) Note, however, that these assessments are quite abbreviated. Still, assessing each participant’s pedigree in this way allowed us to characterize not only the family history of each participant with respect to each of the classes of disorder listed above but also to create alternative indices beyond simple global designations such as the presence or absence of a family history of a given disorder. Because of complexities in scoring the interview, our data release now includes summary variables of reported parental disorders (e.g., mother only, father only, both father and mother) for each of the classes of disorders assessed. Users can derive more complex pedigree measures (e.g., multigenerational typologies, family history density measures) that includes measures ranging from continuous indices of genetic risk such as family history density that considers the number of affected 1st and 2nd degree relatives in the pedigree (Stoltenberg et al., 1998) whether or not the family history is unilineal or bilineal (i.e., matrilineal, patrilineal, or both) (Volicer et al., 1983) or unigenerational (parental generation only) or multigenerational (i.e., parent and grandparent on one side) (Finn et al., 1990). However, because of the various permutations of such approaches, users must create their own based on the needs of their own particular study.
Examination of the frequencies of reported parental alcohol problems, drug problems, conduct/antisocial problems, problems associated with “nervousness”, mania, psychotic symptoms, suicidality, professional help-seeking, and inpatient hospitalization yielded overall prevalence and sex differences consistent with expectation. Aggregating across different conditions (e.g., creating a history of parental externalizing disorders by aggregating across substance use disorders and antisocial behavior, internalizing by aggregating “nerves” and depression, and thought problems by aggregating across mania and psychotic symptoms) showed higher prevalence than their constituent conditions. Further aggregation, combining externalizing, internalizing, and thought problems yielded prevalence indicating that nearly half of the ABCD families (47%) reported one or both biological parents to have been affected by one or more of the conditions assessed.
At the time of baseline assessment, some members of a pedigree had yet to enter their period of risk or were still transitioning through early stages of their period of risk for the disorders being assessed. Additionally, informants may only become aware of a problem in a relative subsequent to the baseline assessment. Consequently, reassessment of family history is planned for a future follow-up, most likely the Year 5 or 6 follow-up. It has not yet been determined if the same family history interview will be readministered (which has the virtue of maintaining the same method) or will be replaced by a more complete assessment that comports better with contemporary diagnostic constructs. In addition, in the course of collecting the family history data we discovered that the interview program was not robust to fully assessing some large pedigrees (e.g., no more than five maternal aunts could be assessed but some informants indicated 6 or more maternal aunts). In the next follow-up, no constraints will be imposed on pedigree size. While the planned re-administration will strengthen the assessment of family history beyond the baseline assessment, the assessment will nonetheless remain somewhat crude owing to the burden of more complete assessment of all 1st and 2nd degree relatives and users should be mindful of the fact that family history methodology is known to have relatively low sensitivity.
3.10. Caregiver perceived stress
A relationship between perceived stress and behavioral and health outcomes is well established (DeVries and Craft, 2007, Mukhara and Banks, 2018, Turkson and Kloster, 2019). The Perceived Stress Scale (PSS) was first published by Cohen and colleagues in 1983 (Cohen et al., 1983). The PSS is an accessible and effective metric of perceived stress, and has demonstrated utility in understanding the relationship between stress and a myriad of both behavioral and health endpoints (Golden-Kreutz and Thornton, 2005, Robles and Garey, 2016, Whitehead and Bergeman, 2017, Barutcu Atas and Aydin Sunbul, 2021). In addition to predictive value for outcomes specific to the individual completing the PSS, this metric has also proven useful in understanding the role of parental perceived stress in adolescent-related outcomes (Slaughter and Hamilton, 2020, Koning and Vink, 2021, Tara and Turpyn, 2021). The role of caregiver behaviors and caregiver perceived stress are salient influences during adolescence; therefore, a PSS assessment that caregivers complete about their own stress has been added to the collected metrics.
4. Trajectories of Caregiver and child-report mental health
As described above, one of the benefits of the ABCD Study is the longitudinal assessments of both caregiver and child reported mental health in a large non-treatment seeking sample. There have been several previous studies using epidemiological or non-treatment seeking samples that have reported data on longitudinal trajectories of mental health, as well as the relationship of various demographic factors relevant to understanding mental health among youth. In terms of age-related differences in mental health, there is consistent evidence from studies in both the United States, Canada and Europe that levels of depression tend to increase from school age into adolescence (Strohschein, 2005, Van Oort and Greaves-Lord, 2009, Robbers and Bartels, 2010, Ormel and Oldehinkel, 2012, Ferro and Gorter, 2015, Coley and O'Brien, 2019, Antolin-Suarez and Nieto-Casado, 2020), with evidence that this increase is greater in females than males (Bongers et al., 2003). Patterns for anxiety are more mixed, with some evidence for decreases in various forms of anxiety from school age to adolescence (Van Oort and Greaves-Lord, 2009, Ormel and Oldehinkel, 2012). In general, the data suggest that aggressive, attentional and rule-breaking problems tend to decrease from middle childhood to adolescence (Bongers and Koot, 2003, Strohschein, 2005, Fanti and Henrich, 2010, Robbers and Bartels, 2010), but with some exceptions (Keiley and Bates, 2000, Ormel and Oldehinkel, 2012). In terms of sex relationships, evidence consistently shows higher rates of depression among females (Faravelli et al., 2013), typically diverging at early adolescence (Bongers and Koot, 2003, Brown and Meadows, 2007, Robbers and Bartels, 2010). In contrast, rates of anxiety show less evidence of sex differences in childhood/adolescence (Faravelli et al., 2013), and rates of externalizing problems tend to be higher in boys across childhood and adolescence (Robbers and Bartels, 2010, Robbers and van Oort, 2011), though with some evidence for convergence in later adolescence (Bongers et al., 2003).
It is also important to examine trajectories of mental health as a function of racial identity or ethnicity so as to understand the social, economic, cultural, and political factors that may contribute differentially to mental health experiences as a function of identity. The evidence about differences in levels of depression, anxiety, and externalizing symptoms in childhood and adolescence as a function of race or ethnicity is more mixed. In the Monitoring the Future study, Black students reported lower symptoms of depression in 10th and 12th grade compared to White students, but other students of color reported higher levels of depression (Coley et al., 2019). In the National Longitudinal Study of Youth, depression was lower among non-Hispanic Black youth than white youth In the National Longitudinal Study of Youth, non-Hispanic Black youth reported less depression than White youth (Strohschein, 2005). In the National Longitudinal Study of Adolescent to Adult Health, Hispanic and Asian youth showed the highest levels of depression and white youth the lowest, with Black youth falling in between (Brown et al., 2007). In the National Comorbidity Survey Replication-Adolescent supplement, Hispanic youth and non-Hispanic Black youth had higher rates of mood and anxiety disorders than non-Hispanic white youth (Georgiades et al., 2018). However, these differences were eliminated when sociodemographic factors including caregiver education and family income were considered (Georgiades et al., 2018). In the National Survey of Children’s Health from 2003, 2007, and 2011, rates of attention deficit disorder symptoms were highest among White children (Collins and Cleary, 2016). In the National Longitudinal Study of Youth, conduct problems were higher among non-Hispanic Black youth than White youth, but it was not clear if these race-related differences were eliminated or reduced with socioeconomic factors were considered (Strohschein, 2005). In contrast, the National Comorbidity Survey Replication-Adolescent supplement, non-Hispanic Black youth and Asian youth had lower rates of behavior disorders than non-Hispanic white youth (Georgiades et al., 2018). Notably, essentially none of these major national epidemiology studies examine mental health among Native American or Alaska Native youth, though there is evidence for high rates of depression and suicide in this population (Health, 2021). Critically, few of these studies address critical contextual factors that are often confounded with race and ethnicity, including factors such as socio-economic status of families and neighborhoods, or other stressors such as discrimination experiences and the effects of systemic racism, all of which likely influence mental health. By systemic racism, we mean both the interpersonal experience of implicit or explicit bias in a youth’s everyday life, as well as the structural political, social, and economic factors that influence youth’s life experiences and opportunities.
Apropos the concerns about contextual factors often confounded with race and ethnicity, the evidence in regards to the relationship between socioeconomic status (SES) and mental health in children and adolescents is robust, with youth living in lower SES households showing consistently higher rates of depression, anxiety, and externalizing symptoms in both the United States and Europe (Goodman and Huang, 2003, Strohschein, 2005, Amone-P'Olak and Burger, 2009, Robbers and Bartels, 2010, Letourneau and Duffett-Leger, 2011, van Oort and van der Ende, 2011, Reiss, 2013, Coley and O'Brien, 2019, Antolin-Suarez and Nieto-Casado, 2020). However, what is less clear is whether different facets of SES relate differentially to youth mental health, such as family income, caregiver education, indices of financial insecurity or neighborhood SES (Denny and Lewycka, 2016, Coley and O'Brien, 2019).
4.1. Current analyses
We used the data from the most recent ABCD data release to characterize the trajectories of both caregiver and child reported internalizing (depression and anxiety) and externalizing (ADHD, oppositional defiant disorder, conduct disorder) symptoms between the ages of 9 and 13 as a function of demographic features. Based on the existing literature, we expected both caregiver and child reports of internalizing symptoms to increase across the course of development, particularly among girls. In regards to externalizing symptoms, we expected rates to be higher in boys and to decrease as a function of age. In regards to race and ethnicity, we did not have strong a priori hypotheses, as we conducted these analyses including a variety of SES related factors that may have influenced race/ethnicity related differences in mental health in prior studies. Based on the existing literature, we expected that lower socioeconomic status (lower caregiver education, lower family income, greater financial insecurity) would be associated with overall higher reports of internalizing and externalizing symptoms. However, we did not have strong a priori hypotheses as to whether the different indicators of SES would relate differentially to child mental health.
4.2. Methods
4.2.1. Participants
Data were from caregiver and youth participants from the current ABCD Data Release 3.0 (http://dx.doi.org/10.15154/1519007), which includes 3 waves of annual data and 3 waves of phone assessments collected through January 15th of 2020: baseline (N = 11,878), 6 Months (N = 11,398), Year 1 (N = 11,235), 18 Months (N = 9911), Year 2 (N = 6571), and 30 Months (N = 3601). In terms of race/ethnicity groupings, youth were grouped into non-Hispanic White youth (n = 6181), non-Hispanic Black youth (n = 1784), Hispanic youth (n = 2412), Asian Youth (n = 252), Native American/Alaska Native youth (n = 289), Multi-racial youth (n = 830) and Additional race youth (n = 128) groups. In the ABCD study, caregivers are asked to indicate whether or not they would describe their child has being Hispanic, and also asked to choose one or more racial identities that they think best describe their child. To create these groups, if a caregiver indicated that a youth had Hispanic ethnicity (the only ethnicity assessed for youth), the youth was placed in the Hispanic group regardless of what racial identity(ies) the caregiver also endorsed. If a caregiver endorsed non-Hispanic ethnicity and chose only White or Black for race, then the youth was placed in the non-Hispanic White or Black youth groups respectively. If a caregiver endorsed one or more of the following racial identities and no other, the child was placed in the Asian group: Japanese, Chinese, Korean, Vietnamese, Filipino, Asian Indian or Other Asian. If the caregiver chose Native American or Alaska Native, then the child was placed in that group. If the caregiver chose Native Hawaiian, Guamanian, or Samoan, Other Race, or refused to choose a racial category, the youth was placed in the “additional” race group as there were too few youth in each of these categories individually for separate analysis. If the caregiver endorsed more than one race (other than only multiple races in the Asian group), the youth was placed in the Multi-racial group. We used caregiver-reported sex at birth, and future work with the ABCD Study will examine gender identity. The demographic distribution of youth in this sample is shown in Table S3.
4.2.2. Caregiver reported mental health symptoms
As described above, caregivers completed the Child Behavior Checklist at each annual wave. Here we examined raw scores for the following DSM-Oriented symptom subscales: a) total problems; b) internalizing; c) externalizing; d) depression; e) anxiety; f) ADHD; g) oppositional; and h) conduct problems. We used raw scores rather than age and sex-adjusted t-scores to better address relationships to developmental and sex differences.
Child Reported Mental Health Symptoms: As described above, youth completed the Brief-Problem Monitor (BPM-Y) every six months starting at the first mid-year phone assessment, for a total of 5 waves of assessment (6-Month, Year 1, 18-Month, Year 2, 30-Month). Here we examined raw scores for the four BPM-Y Scales: a) total problems; b) internalizing; c) externalizing; d) attention. We again used raw scores rather than age and sex-adjusted t-scores to better address our questions of interest.
4.2.3. Neighborhood poverty
The ABCD Study uses the primary current home address provided by the caregiver via the Residential History Questionnaire. This address is used to generate the Area Deprivation Index (ADI) for the census tract that contains this address (Singh, 2003, Kind and Buckingham, 2018). The census data that is used here is from the 2010 Census and some supplementary American Community Survey information. The ADI consists of 17 census variables that use census tracts to reference different aspects of SES. We used the National Percentile metric for the baseline assessment.
4.2.4. Income-to-needs
Family income at baseline was assessed using the income-to-needs calculated by dividing the reported total household income by the federal poverty line for a given household size (Gonzalez et al., 2020). A higher value indicates higher SES. The gross household income and the number of individuals in the family are reported by the caregiver on the Parent Demographics Survey (Barch et al., 2018).
4.2.5. Financial adversity
In addition to Income-to-Needs, we used the Parent-Reported Financial Adversity Questionnaire (PRFQ) (Diemer et al., 2012) assessed at baseline. The PRFQ asked questions designed to determine whether families generally have enough money to pay for basic life expenses like food and healthcare. There are seven questions and each one is scored a 0 or 1. A summary score was created by summing the seven items. PRFQ indexes self-report of finances that may better account for the association of income level to area cost-of-living.
4.2.6. Caregiver education
The child’s caregiver reports their education on the Parent Demographics survey. We used the baseline reports and coded 8th grade or lower education as a 1, 9th to 12th without a diploma as a 2, high school, GED or equivalent as a 3, partial college or Associates/vocational degree as a 4, college diploma as a 5, Masters degree as a 6, and a professional or doctorate as a 7. This variable was treated as an ordinal variable, and these groupings were used rather than more granular ones to provide reasonably sized groupings in terms of sample size while still capturing differences in education likely to be associated with differences in economic status.
Statistical Analysis: We examined trajectories of mental health as a function of age using mixed effects models (MLM’s) in “R” version 4.03 using lme4 version 1.1.25 for each of the variables that included both random intercept and random slope components (with an unstructured covariance matrix between the two), as well as family and site. Time was coded as age at assessments and data were also nested within participant to capture within participant age-related change (see Supplement for sample R code). The models included sex at birth (female, male), race (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, Native American/Alaska Native, Additional Races, Multi-racial, factor coded with the largest group (White) as the reference group), income-to-needs ratio, financial adversity, caregiver education, and Area Deprivation Index. Maximum likelihood estimation was used. There was missing data for some of the baseline predictors (caregiver education = 23, financial adversity = 22, income-to-needs = 1216, Area Deprivation Index = 697). Thus, we used multiple imputation (N = 5) using mice version 3.13.0. Youth missing income-to-needs or area deprivation index data were more likely to be Black or Hispanic and more likely to have caregivers with lower education. However, as recommended by best practices, all of the variables used in the MLM were included in the imputation model (age, sex, race/ethnicity, caretaker education, income-to-needs, financial adversity, area deprivation index and the mental health outcome for that analyses) (Wilkinson, 1999, Collins and Schafer, 2001, Sterne, 2009, Azur and Stuart, 2011). Further, although dealing with missing data by analyzing only complete cases is thought to potentially create significant bias (Wilkinson, 1999, Collins and Schafer, 2001, Sterne, 2009, Azur and Stuart, 2011), all analyses with imputed data were repeated with the non-imputed data (see Supplement Tables S6–S9), with identical results. All continuous predictors were scaled prior to entry into a model using the “scale_datlist” function in miceadds version 3.11-6 to facilitate interpretation of the estimates in terms of effect size. To focus the discussion of effects, and given the large sample size, we employed an ad hoc cutoff of p = .01. A full accounting of effects is reported in the text and tables.
4.3. Results
The demographic distribution of the baseline sample is shown in Table S3.
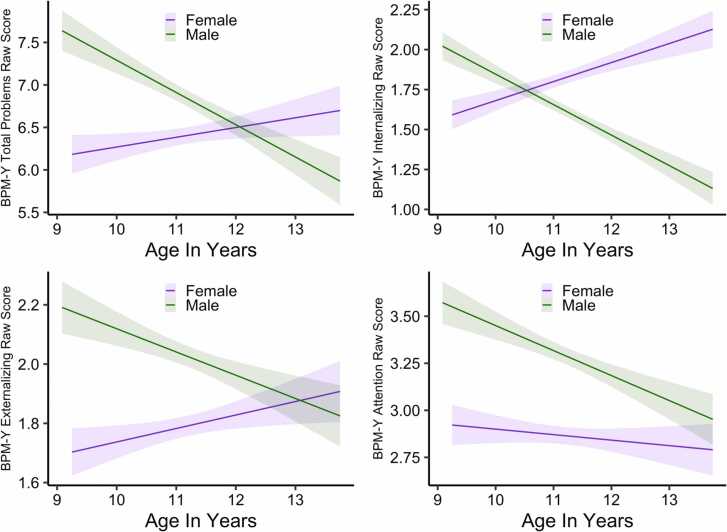
4.3.1. Brief problem monitor-youth report
As shown in Table 3 and Figs. 1 and S1, there were main effects of sex for all measures, as well as interactions of sex with age. To parse the source of these interactions, we created subsets of the imputed data and ran the analyses separately for females and males. As shown in Figs. 1 and S1, males showed a significant decrease in all symptoms domains with age (all Std. Bs < − 0.05, all ps < 0.0086). In contrast, females showed a significant increase in total problems (Std. B = 0.25, p = < 0.0001), internalizing (Std. B = 0.17, p = < 0.0001), and externalizing symptoms (Std. B = 0.05, p = .0056) with age, and no significant changes as a function of age in attention problems (Std. B = 0.05, p = .061).
Table 3.
Results of analyses of the Brief Problem Monitor Youth (BPM-Y) Report.
 |
Abbreviations. Std. Β = standardized beta statistic; 95% CI = 95% confidence interval; t = t-statistic; p = p-value.
Note: Dark gray indicates effects significant at p < .01, while light gray indicates effects significant at p < .05.
Fig. 1.
Sex differences in trajectories of youth reported mental health using raw data: graphs illustrating sex differences in youth-reported Total Problem, Internalizing, Externalizing and Attention Problems on the Brief Problem Monitor. The shaded areas indicate the 99th percentile confidence intervals around the estimated linear slope. Graphs were created in R using ggplot2 version 3.3.2 using one of the five imputed datasets and present the “raw” data. The analogous graph created using ggpredict plotting the relationships to sex using estimated marginal means controlling for all other factors in the model is shown in Fig. S1.
Also as shown in Table 3, there were both main effects of race/ethnicity and interactions with age. As shown in Figs. S2 and S3, non-Hispanic Black youth did not report overall differences in any problem domain compared to the other race/ethnicity groups, but reported a decrease in total, internalizing, and attention problems with age. The Hispanic youth reported overall higher attention problems compared to non-Hispanic White and Asian youth, and reported a significant increase in externalizing problems with age, both of a small effect size. The Native American/Alaska Native youth reported higher rates of total problems, externalizing, and attention problems of a moderate effect size, but no significant change with age. The Multi-race youth reported overall higher total, externalizing, and attention problems compared to non-Hispanic White and Asian youth. The Additional race group reported lower internalizing symptoms than the non-Hispanic White group.
As shown in Table 3 and Figs. S4 and S5, there were main effects of caretaker education, income-to-needs, financial adversity, and area deprivation index for every youth reported problem domain (except caretaker education for internalizing problems). These were all simultaneously significant. Higher income-to-needs was associated with lower youth reported problems in all domains, while higher financial adversity and area deprivation were associated with higher youth reported problems in all domains. Higher caretaker education was associated with overall lower youth reported externalizing problems across ages with no significant change as a function of age. Further, there were significant interactions of caretaker education with age for total, internalizing and attention domains. As shown in Figs. S4 and S5, while lower caretaker education was associated with greater youth-reported total, internalizing and attentional problems at younger ages, problem reports converged for youth with higher and lower caretaker education as youth grew older.
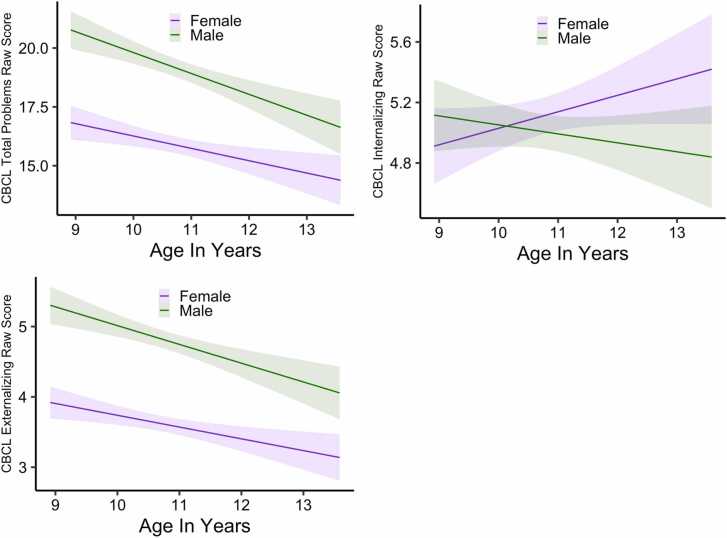
4.3.2. Child Behavior Checklist-Caregiver Report
There were again main effects of sex and/or interactions of sex with age for the CBCL summary measures (Table 4). As shown in Figs. 2 and S6, caregivers reported males having overall higher total and externalizing problems. Reports of both total and externalizing problems decreased for both males as females as they grew older, with a steeper decline for males than females. For internalizing problems, males and females were initially rated similarly, but reports increased for females as they moved into puberty, while they decreased for males. There were also main effects of race/ethnicity for all summary measures, with Asian, non-Hispanic Black Youth, and Hispanic youth reported as having lower Total and Externalizing problems compared to Non-Hispanic White youth once SES factors were accounted for (Table 4). There was a similar pattern for internalizing, though it was not significant for Hispanic youth. A significant interaction with age for Non-Hispanic Black youth for internalizing problems also emerged, with a decline in caretaker reported problems with age (Figs. S7 and S8). The caretakers of Native American/Alaska Native youth reported overall higher total problems of a moderate effect size compared to Hispanic, non-Hispanic White and Black youth, and Asian youth, and a greater increase in internalizing symptoms with age, but no differences in externalizing symptoms. There were no significant differences in caregiver reports for Multi-racial or Additional race youth.
Table 4.
Results of analyses of the global scales for Child Behavior Checklist (CBCL) Caregiver Report.
 |
Abbreviations. Std. Β = standardized beta statistic; 95% CI = 95% confidence interval; t = t-statistic; p = p-value.
Note: Dark gray indicates effects significant at p < .01, while light gray indicates effects significant at p < .05.
Fig. 2.
Sex differences in trajectories of caregiver reported mental health summary scores using raw data: graphs illustrating sex differences in caregiver-reported Total Problem, Internalizing, Externalizing on the Child Behavior Checklist. The shaded areas indicate the 99th percentile confidence intervals around the estimated linear slope. Graphs were created in R using ggplot2 version 3.3.2 using one of the five imputed datasets and present the “raw” data. The analogous graph created using ggpredict plotting the relationships to sex using estimated marginal means controlling for all other factors in the model is shown in Fig. S6.
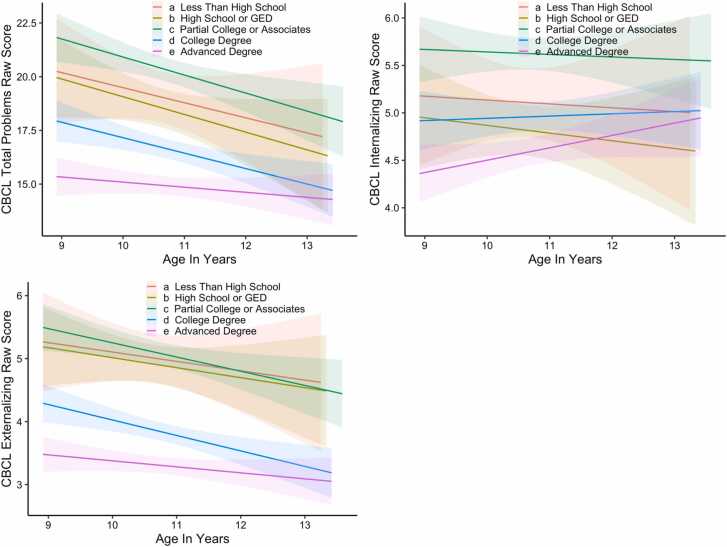
Significant interactions of caretaker education with age for both total and externalizing problems were also found. As shown in Figs. 3 and S9, there were overall lower problem reports for youth among more highly educated caregivers, and less change over time among the youth of caregivers with advanced degrees compared to those with less education. There were main effects of Income-to-Needs for all summary scores, with higher Income-to-Needs associated with lower caregiver reports of problems. There were also main effects and/or interactions with financial adversity for all summary domains. As shown in Fig. S10, caretakers with financial adversity reported higher problems for their youth in all domains, with less of a decrease in total problems over time compared to caretakers without financial adversity. Further, caretakers with financial adversity reported an increase in internalizing problems in their youth with age, but not those with no financial adversity. Interestingly, there were no significant unique effects of Area Deprivation Index for caregiver reported mental health, in contrast to youth reported mental health. Results for the DSM Syndrome Scores of depression, anxiety, ADHD, oppositional, and conduct problems are provided in the Supplemental materials (Tables S4 and S5, Figs. S11–S17).
Fig. 3.
Caretaker education differences in trajectories of caregiver reported mental health summary scores using raw data: graphs illustrating differences in caregiver-reported Total Problem, Internalizing, Externalizing on the Child Behavior Checklist as a function of caretaker education. The shaded areas indicate the 99th percentile confidence intervals around the estimated linear slope. Graphs were created in R using ggplot2 version 3.3.2 using one of the five imputed datasets and present the “raw” data. The analogous graph created using ggpredict plotting the relationships to caretaker education using estimated marginal means controlling for all other factors in the model is shown in Fig. S9.
4.4. Discussion of mental health trajectory results
These analyses of the trajectories of youth and caregiver reported mental health resemble findings from prior work in a number of important ways, but also provide new insights into relationships with socioeconomic disadvantage. In terms of age and sex-related trajectories, like much prior research, we found that both youth and caregiver reports of attentional and externalizing problems were higher for males, but declined with age for both males and females (Bongers and Koot, 2003, Strohschein, 2005, Fanti and Henrich, 2010, Robbers and Bartels, 2010) in terms of caregiver report. Intriguingly, in terms of youth report, females actually reported greater externalizing symptoms as they transitioned into puberty, a finding somewhat different than prior work. Also similar to prior research, we found that both youth and caregiver of internalizing symptoms increased with age for females, though not for males (Strohschein, 2005, Van Oort and Greaves-Lord, 2009, Robbers and Bartels, 2010, Ormel and Oldehinkel, 2012, Ferro and Gorter, 2015, Coley and O'Brien, 2019, Antolin-Suarez and Nieto-Casado, 2020), with elevated rates for females emerging in adolescence (Bongers and Koot, 2003, Brown and Meadows, 2007, Robbers and Bartels, 2010, Faravelli and Alessandra Scarpato, 2013). These data add to those in the literature suggesting that the majority of patterns of age and sex-related differences in externalizing and internalizing have maintained over secular changes in society and across a number of different cultures, though with some variation across youth and caregiver report.
Our results in regards to race/ethnicity differences are also intriguing, and suggest relatively few race/ethnicity differences when SES factors are included in models. For youth report, there were only modest race/ethnicity differences, with Native American/Alaska Native and Multi-racial youth reporting higher total, externalizing and attentional problems, and non-Hispanic Black youth reporting greater decreases in total, internalizing, and attention symptoms than other racial/ethnic groups over time. There were more differences in caregiver-reports, with the caregivers of non-Hispanic White youth reporting higher levels of total, internalizing, and externalizing problems compared to most of the other racial/ethnic groups other than the other-race group when accounting for socio-demographic factors. In addition, caregivers of Native American/Alaska Native youth reported higher overall rates of total problems and increase in internalizing symptoms with age compared to non-Hispanic White and Black youth and Asian youth (and non-Hispanic Black youth for internalizing symptoms). As noted above, prior findings in regards to race/ethnicity differences in mental health among Black, Asian and Hispanic youth have been somewhat mixed, but our findings are consistent with a number of studies showing lower rates of internalizing symptoms among non-Hispanic Black youth (Coley et al., 2019) and findings that attention symptoms were higher among White youth (Collins and Cleary, 2016). There have been few studies of youth that have separately examined Native American/Alaska Native youth. However, we would still caution any strong interpretations of these data, as we were not able to address a range of other potentially contextualizing factors, such as cultural differences in reporting of mental health related symptoms, or experiences of discrimination or other forms of systemic racism that may influence mental health.
Consistent with the robust previous literature on SES and mental health, we found that all indicators of lower SES were related to greater total, internalizing, and externalizing problems in youth reports. Critically, other than a few exceptions, all SES indicators accounted for simultaneous unique variance in youth mental-health reports, including income-to-needs, caretaker education, financial adversity, and area deprivation index. For caregiver reports, all SES indicators other than Area Deprivation Index also accounted for unique variance in reports of youth mental health, though caregiver education effects were less consistent than income-to-needs and financial adversity. It is intriguing that neighborhood poverty has stronger effects on youth reported mental health than caregiver reported mental health. It is unclear why this was so, but it is possible that youth’s experiences with their peers, in their schools, and in their neighborhoods are likely to be reflected in their own introspective reports than in their caregiver’s. Overall, these data once again indicate the huge importance of SES in understanding youth mental health, and indicate the need to understand the many different facets of SES given that they each account for independent variance in the trajectory of youth mental health.
Of note, all of these data were collected prior to the onset of the COVID-19 pandemic, and thus it will be important in future analyses to examine discontinuities that may occur following the onset of the pandemic, and how individual differences in pre-pandemic factors predict response to the pandemic restrictions or to COVID-19 infection itself. In particular, it will be important to examine how various facets of SES related to the impact of COVID-19, and whether youth who were showing particular trajectories of change in mental health (e.g., greater than average increase in internalizing, etc.) are more likely to have been negatively impacted by facets of the pandemic. Sadly, COVID-19 may also create an experiment of nature by which we are able to examine the relationships of changes in SES to changes in youth mental health, as the SES of many ABCD families, like so many families across the world, was negatively impacted by COVID-19.
5. Summary and conclusions
This manuscript outlined the logic and known issues with the measures of mental health that have been included in the ABCD Study since baseline and which have been added over time. Further, we have tried to outline known issues to alert the field to some of the challenges with certain measures, as well as the promise afforded by this rich, multi-informant, longitudinal database. We believe that the analyses of the longitudinal trajectories of both youth and caregiver reported mental health illustrate the power of this data set in identifying the ways in which mental health evolves in children as a function of a variety of factors, including age, sex, and SES. As additional waves of ABCD data are released, we will be able to examine additional factors that may impact mental health among youth in the United States, and began to examine leading and lagging relationships of risk factors for increasing mental health challenges, resilience factors that may protect some youth, and the consequences of changes in mental health over time.
CRediT authorship contribution statement
Deanna M. Barch: Conceptualization, Methodology, Formal analysis, Writing – original draft, Project administration, Funding acquisition. Matthew D. Albaugh: Conceptualization, Methodology, Writing – original draft, Writing – review & editing, Project administration. Arielle Baskin-Sommers: Conceptualization, Methodology, Formal analysis, Writing – original draft, Project administration, Funding acquisition. Brittany E. Bryant: Conceptualization, Methodology, Writing – review & editing, Project administration. Duncan B. Clark: Conceptualization, Methodology, Writing – original draft, Project administration, Funding acquisition. Anthony Steven Dick: Conceptualization, Methodology, Writing – review & editing, Formal analysis. Eric Feczko: Writing – review & editing, Formal analysis. John J. Foxe: Conceptualization, Methodology, Writing – review & editing, Project administration, Funding acquisition. Dylan G. Gee: Conceptualization, Methodology, Writing – original draft, Project administration, Funding acquisition. Jay Giedd: Conceptualization, Methodology, Writing – review & editing, Project administration. Meyer D. Glantz: Conceptualization, Methodology, Writing – review & editing. James J. Hudziak: Conceptualization, Methodology, Writing – review & editing. Nicole R. Karcher: Conceptualization, Methodology, Writing – original draft. Kimberly LeBlanc: Conceptualization, Methodology, Writing – review & editing. Melanie Maddox: Writing – review & editing, Project administration. Erin C. McGlade: Conceptualization, Methodology, Writing – review & editing. Carrie Mulford: Conceptualization, Methodology, Writing – review & editing. Bonnie J. Nagel: Conceptualization, Methodology, Writing – review & editing, Project administration, Funding acquisition. Gretchen Neigh: Conceptualization, Methodology, Writing – review & editing. Clare E Palmer: Conceptualization, Methodology, Writing – review & editing. Alexandra S. Potter: Conceptualization, Methodology, Writing – original draft, Project administration, Funding acquisition. Kenneth J. Sher: Conceptualization, Methodology, Writing – original draft. Susan F. Tapert: Conceptualization, Methodology, Writing – original draft, Project administration, Funding acquisition. Wesley K. Thompson: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Project administration, Funding acquisition. Laili Xie: Writing – review & editing, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We wish to thank all of the wonderful families who participate in the ABCD Study, and all of the outstanding staff who make this work possible. We also wish to thank Drs. Ken Kobak and Dr. Joan Kaufman for their support of the KSADs assessments and Dr. Thomas Achenbach for his support for the CBCL, BPM, ASR, ABCL, and YSR assessments. We also wish to thank Dr. Marybel Robledo Gonzalez for sharing her computation of income-to-needs ratios for use in our analyses.
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award nos. U01DA041022, U01DA041028, U01DA041048, U01DA041089, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/nih-collaborators. A listing of participating sites an d a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html.ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from http://dx.doi.org/10.15154/1519007. DOIs can be found at https://nda.nih.gov/abcd/query/abcd-curated-annual-release-3.0.html.
Grant Support
U01DA041120-01 (DMB, KS); U01DA041148 (ASP, MDA, JJH); U01DA041028 (DBC); U01DA041089 (SFT); U01DA041134 (DYT); U01DA041174 (NAK); U01DA041089 (MPP); U01DA041022 (DP); U01DA041106 (BZ); U01DA041117 (LC); U24DA041147 (TJ, SFT); K05AA017242 (KS); U01DA050988 (JJF); U01DA041148 (BJN); U24DA041123 (WKT); 1RF1MH120025 (WKT).
Conflict Disclosures
MA, DMB, ABS, BB, DC, ASD, EF, DGG, JJF, JG, MDG, JH, NRK, BK, KL, MM, ECM, CM, BJN, GN, CEP, ASP, KS, SFT, WKT, and XL have no conflicts to report. All Federal representatives contributed to the interpretation of the data and participated in the preparation, review and approval of the manuscript, consistent with their roles on the ABCD Federal Partners Group. The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.dcn.2021.101031.
Contributor Information
Deanna M. Barch, Email: dbarch@wustl.edu.
Matthew D. Albaugh, Email: matthew.albaugh@med.uvm.edu.
Arielle Baskin-Sommers, Email: arielle.baskin0sommers@yale.edu.
Brittany E. Bryant, Email: goldsmib@musc.edu.
Duncan B. Clark, Email: clarkdb@upmc.edu.
Anthony Steven Dick, Email: adick@fiu.edu.
Eric Feczko, Email: feczk001@umn.edu.
John J. Foxe, Email: john_foxe@urmc.rochester.edu.
Dylan G. Gee, Email: dylan.gee@yale.edu.
Jay Giedd, Email: jgiedd@ucsd.edu.
Meyer D. Glantz, Email: mglantz@nida.nih.gov.
James J. Hudziak, Email: james.hudziak@med.uvm.edu.
Nicole R. Karcher, Email: nkarcher@wustl.edu.
Kimberly LeBlanc, Email: kimberly.leblanc@nih.gov.
Melanie Maddox, Email: melanie.maddox@hsc.utah.edu.
Erin C. McGlade, Email: erin.mcglade@hsc.utah.edu.
Carrie Mulford, Email: carrie.nulford@nih.gov.
Bonnie J. Nagel, Email: nagelb@ohsu.edu.
Gretchen Neigh, Email: gretchen.mccandless@vcuhealth.org.
Clare E. Palmer, Email: cepalmer@ucsd.edu.
Alexandra S. Potter, Email: alexandra.potter@uvm.edu.
Kenneth J. Sher, Email: SherK@missouri.edu.
Susan F. Tapert, Email: stapert@ucsd.edu.
Wesley K. Thompson, Email: wkthompson@ucsd.edu.
Laili Xie, Email: lxie@health.ucsd.edu.
Appendix A. Supplementary material
Supplementary material
Supplementary material
References
- Achenbach T.M. The Achenbach System of Empirically Based Assessment (ASEBA): Development, Findings, Theory and Applications. University of Vermont Research Center for Children, Youth and Families; Burlington, VT: 2009. [Google Scholar]
- Achenbach T.M., McConaughy S.H., et al. Manual for the ASEBA Brief Problem Monitor for Ages 6–18 (BPM/6-18) ASEBA; Burlington, VT: 2017. [Google Scholar]
- Achenbach T.M., Rescorla L. Manual for the ASEBA School-age Forms & Profiles: An Integrated System of Multi-informant Assessment. ASEBA; Burlington, VT: 2001. [Google Scholar]
- Achenbach T.M., Rescorla L. Manual for the ASEBA Adult Forms & Profiles: For Ages 18–59: Adult Self-report, Adult Behavior Checklist. ASEBA; Burlington, VT: 2003. [Google Scholar]
- Achenbach T.M., Rescorla L. Multicultural Supplement to the Manual for the Aseba School-age Forms & Profiles: Child Behavior Checklist for Ages 6–18, Teacher’s Report Form, Youth Self-report: An Integrated System Fo Multi-informant Assessment. ASEBA; Burlington, VT: 2007. [Google Scholar]
- Achenbach T.M., Rescorla L. Multicultural Supplement to the Manual for the ASEBA Adult Forms & Profiles: For Ages 18–59, Adult Self-report, Adult Behavior Checklist: An Integrated System of Multi-informant Assessment. ASEBA; Burlington, VT: 2015. [Google Scholar]
- Aldao A., Gee D.G., et al. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: current and future directions. Dev. Psychopathol. 2016;28(4pt1):927–946. doi: 10.1017/S0954579416000638. [DOI] [PubMed] [Google Scholar]
- Amone-P’Olak K., Burger H., et al. Socioeconomic position and mental health problems in pre- and early-adolescents: the TRAILS study. Soc. Psychiatry Psychiatr. Epidemiol. 2009;44(3):231–238. doi: 10.1007/s00127-008-0424-z. [DOI] [PubMed] [Google Scholar]
- Antolin-Suarez L., Nieto-Casado F.J., et al. Demographic, social, and economic factors of internalizing problems in referred and non-referred adolescents. Int. J. Environ. Res. Public Health. 2020;17:14. doi: 10.3390/ijerph17145195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azur M.J., Stuart E.A., et al. Multiple imputation by chained equations: what is it and how doesit work? Int. J. Methods Psychiatr. Res. 2011;20(1):40–49. doi: 10.1002/mpr.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch D.M., Albaugh M.D., et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev. Cogn. Neurosci. 2018;32:55–66. doi: 10.1016/j.dcn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barch D.M., Gotlib I.H., et al. Common measures for National Institute of Mental Health funded research. Biol. Psychiatry. 2016;79(12):e91–e96. doi: 10.1016/j.biopsych.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen J.R., Fergus T.A., et al. Addressing psychometric limitations of the difficulties in emotion regulation scale through item modification. J. Pers. Assess. 2016;98(3):298–309. doi: 10.1080/00223891.2015.1091774. [DOI] [PubMed] [Google Scholar]
- Barutcu Atas D., Aydin Sunbul E., et al. The association between perceived stress with sleep quality, insomnia, anxiety and depression in kidney transplant recipients during Covid-19 pandemic. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0248117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benfer N., Bardeen J.R., et al. Factor structure and incremental validity of the original and modified versions of the difficulties in emotion regulation scale. J. Pers. Assess. 2019;101(6):598–608. doi: 10.1080/00223891.2018.1492927. [DOI] [PubMed] [Google Scholar]
- Bongers I.L., Koot H.M., et al. The normative development of child and adolescent problem behavior. J. Abnorm. Psychol. 2003;112(2):179–192. doi: 10.1037/0021-843x.112.2.179. [DOI] [PubMed] [Google Scholar]
- Brown J.S., Meadows S.O., et al. Race-ethnic inequality and psychological distress: depressive symptoms from adolescence to young adulthood. Dev. Psychol. 2007;43(6):1295–1311. doi: 10.1037/0012-1649.43.6.1295. [DOI] [PubMed] [Google Scholar]
- Brown S.A., Brumback T., et al. The national consortium on alcohol and neurodevelopment in adolescence (NCANDA): a multisite study of adolescent development and substance use. J. Stud. Alcohol Drugs. 2015;76(6):895–908. doi: 10.15288/jsad.2015.76.895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunford N., Dawson A.E., et al. The difficulties in emotion regulation scale-parent report: a psychometric investigation examining adolescents with and without ADHD. Assessment. 2020;27(5):921–940. doi: 10.1177/1073191118792307. [DOI] [PubMed] [Google Scholar]
- Capaldi D.M., Rothbart M.K. Development and validation of an early adolescent temperament measure. J. Early Adolesc. 1992;12:153–173. [Google Scholar]
- Carver C.S., White T. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: the BIS/BAS scales. J. Pers. Social Psychol. 1994;67:319–333. [Google Scholar]
- Casey B.J., Cannonier T., et al. The Adolescent Brain Cognitive Development (ABCD) study: imaging acquisition across 21 sites. Dev. Cogn. Neurosci. 2018 doi: 10.1016/j.dcn.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, D.A., S.J. Brislin, et al., 2021. Differential Item functioning in the assessment of delinquency between black and white youth in the ABCD study: evidence of psychometric bias in reports of arrest. (in preparation).
- Cohen S., Kamarck T., et al. A global measure of perceived stress. J. Health Soc. Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cole P.M., Michel M.K., et al. The development of emotion regulation and dysregulation: a clinical perspective. Monogr. Soc. Res. Child Dev. 1994;59(2–3):73–100. [PubMed] [Google Scholar]
- Coley R.L., O’Brien M., et al. Secular trends in adolescent depressive symptoms: growing disparities between advantaged and disadvantaged schools. J. Youth Adolesc. 2019;48(11):2087–2098. doi: 10.1007/s10964-019-01084-1. [DOI] [PubMed] [Google Scholar]
- Collins K.P., Cleary S.D. Racial and ethnic disparities in parent-reported diagnosis of ADHD: national survey of children’s health (2003, 2007, and 2011) J. Clin. Psychiatry. 2016;77(1):52–59. doi: 10.4088/JCP.14m09364. [DOI] [PubMed] [Google Scholar]
- Collins L.M., Schafer J.L., et al. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol. Methods. 2001;6(4):330–351. [PubMed] [Google Scholar]
- Conway K.P., Vullo G.C., et al. Data compatibility in the addiction sciences: an examination of measure commonality. Drug Alcohol Depend. 2014;141:153–158. doi: 10.1016/j.drugalcdep.2014.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A., Prinstein M.J. Applying depression-distortion hypotheses to the assessment of peer victimization in adolescents. J. Clin. Child Adolesc. Psychol. 2004;33(2):325–335. doi: 10.1207/s15374424jccp3302_14. [DOI] [PubMed] [Google Scholar]
- Denny S., Lewycka S., et al. The association between socioeconomic deprivation and secondary school students’ health: findings from a latent class analysis of a national adolescent health survey. Int. J. Equity Health. 2016;15(1):109. doi: 10.1186/s12939-016-0398-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVries A.C., Craft T.K., et al. 2006 Curt P. Richter award winner: social influences on stress responses and health. Psychoneuroendocrinology. 2007;32(6):587–603. doi: 10.1016/j.psyneuen.2007.04.007. [DOI] [PubMed] [Google Scholar]
- Diemer M.A., Mistry R.S., et al. Best practices in conceptualizing and measure social class in psycholgocial research. Anal. Social Issues Pub. Policy. 2012;13(1):77–113. [Google Scholar]
- Elliot D.S., Huizinga D., et al. Multiple Problem Youth: Delinquency, Substance Use, and Mental Health Problems. Springer-Verlag; New York, NY: 1989. [Google Scholar]
- Fadus M.C., Valadez E.A., et al. Racial disparities in elementary school disciplinary actions: findings from the ABCD study. J. Am. Acad. Child Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanti K.A., Henrich C.C. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: findings from the National Institute of Child Health and Human Development Study of Early Child Care. Dev. Psychol. 2010;46(5):1159–1175. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- Faravelli C., Alessandra Scarpato M., et al. Gender differences in depression and anxiety: the role of age. Psychiatry Res. 2013;210(3):1301–1303. doi: 10.1016/j.psychres.2013.09.027. [DOI] [PubMed] [Google Scholar]
- Ferro M.A., Gorter J.W., et al. Trajectories of depressive symptoms during the transition to young adulthood: the role of chronic illness. J. Affect. Disord. 2015;174:594–601. doi: 10.1016/j.jad.2014.12.014. [DOI] [PubMed] [Google Scholar]
- Finn P.R., Kleinman I., et al. The lifetime prevalence of psychopathology in men with multigenerational family histories of alcoholism. J. Nerv. Ment. Dis. 1990;178(8):500–504. [PubMed] [Google Scholar]
- Georgiades K., Paksarian D., et al. Prevalence of mental disorder and service use by immigrant generation and race/ethnicity among U.S. adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57(4):280–287. doi: 10.1016/j.jaac.2018.01.020. (e282) [DOI] [PubMed] [Google Scholar]
- Gershon R.C., Wagster M.V., et al. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80(11 Suppl. 3):S2–S6. doi: 10.1212/WNL.0b013e3182872e5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden-Kreutz D.M., Thornton L.M., et al. Traumatic stress, perceived global stress, and life events: prospectively predicting quality of life in breast cancer patients. Health Psychol. 2005;24(3):288–296. doi: 10.1037/0278-6133.24.3.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez M.R., Palmer C.E., et al. Positive economic, psychosocial, and physiological ecologies predict brain structure and cognitive performance in 9-10-year-old children. Front. Hum. Neurosci. 2020;14 doi: 10.3389/fnhum.2020.578822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E., Huang B., et al. A multilevel analysis of the relation of socioeconomic status to adolescent depressive symptoms: does school context matter? J. Pediatr. 2003;143(4):451–456. doi: 10.1067/S0022-3476(03)00456-6. [DOI] [PubMed] [Google Scholar]
- Grant K.E., Compas B.E., et al. Stressors and child and adolescent psychopathology: measurement issues and prospective effects. J. Clin. Child Adolesc. Psychol. 2004;33(2):412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Gross J.J., John O.P. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Gullone E., Taffe J. The emotion regulation questionnaire for children and adolescents (ERQ-CA): a psychometric evaluation. Psychol. Assess. 2012;24(2):409–417. doi: 10.1037/a0025777. [DOI] [PubMed] [Google Scholar]
- Hagler D.J., Jr., Hatton S., et al. Image processing and analysis methods for the adolescent brain cognitive development study. Neuroimage. 2019;202 doi: 10.1016/j.neuroimage.2019.116091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton C.M., Strader L.C., et al. The PhenX Toolkit: get the most from your measures. Am. J. Epidemiol. 2011;174(3):253–260. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health, N.I.o.M.H.M.M., 2021. Mental and Behavioral Health - American Indians/Alaska Natives. from 〈https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=39〉.
- Hoeve M., Blokland A., et al. Trajectories of delinquency and parenting styles. J. Abnorm. Child Psychol. 2008;36(2):223–235. doi: 10.1007/s10802-007-9172-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono W.G., Heath A.C., et al. The utility of twins in developmental cognitive neuroscience research: how twins strengthen the ABCD research design. Dev. Cogn. Neurosci. 2018;32:30–42. doi: 10.1016/j.dcn.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isen J.D., Tuvblad C., et al. Developmental trajectories of delinquent and aggressive behavior: Evidence for differential heritability. Child Psychiatry Hum. Dev. 2021 doi: 10.1007/s10578-020-01119-w. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaddoe V.W., Mackenbach J.P., et al. The generation R study: design and cohort profile. Eur. J. Epidemiol. 2006;21(6):475–484. doi: 10.1007/s10654-006-9022-0. [DOI] [PubMed] [Google Scholar]
- Karcher N.R., Barch D.M. The ABCD study: understanding the development of risk for mental and physical health outcomes. Neuropsychopharmacology. 2020 doi: 10.1038/s41386-020-0736-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karcher N.R., Barch D.M., et al. Assessment of the prodromal questionnaire-brief child version for measurement of self-reported psychoticlike experiences in childhood. JAMA Psychiatry. 2018;75(8):853–861. doi: 10.1001/jamapsychiatry.2018.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karcher N.R., Loewy R.L., et al. Replication of associations with psychotic-like experiences in middle childhood from the adolescent brain cognitive development (ABCD) study. Schizophr. Bull. Open. 2020;1(1) doi: 10.1093/schizbullopen/sgaa009. (sgaa009) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiley M.K., Bates J.E., et al. A cross-domain growth analysis: externalizing and internalizing behaviors during 8 years of childhood. J. Abnorm. Child Psychol. 2000;28(2):161–179. doi: 10.1023/a:1005122814723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind A.J.H., Buckingham W.R. Making neighborhood-disadvantage metrics accessible – the neighborhood atlas. N. Engl. J. Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak K.A., Kaufman J. KSADS-COMP. Center for Telepsychology; Madison, WI: 2015. [Google Scholar]
- Kobak K.A., Kratochvil C.J., et al. Computerized screening of comorbidity in adolescents with substance or psychiatric disorders. Anxiety Disord. Depr. 2013 [Google Scholar]
- Koning M., Vink J., et al. Maternal stress and depressive symptoms and adolescents’ body mass index: a prospective study. BMC Public Health. 2021;21(1):675. doi: 10.1186/s12889-021-10721-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latham M.D., Dudgeon P., et al. Factor structure of the early adolescent temperament questionnaire-revised. Assessment. 2020;27(7):1547–1561. doi: 10.1177/1073191119831789. [DOI] [PubMed] [Google Scholar]
- Lee D.J., Witte T.K., et al. A factor analytic evaluation of the difficulties in emotion regulation scale. J. Clin. Psychol. 2016;72(9):933–946. doi: 10.1002/jclp.22297. [DOI] [PubMed] [Google Scholar]
- Letourneau N.L., Duffett-Leger, et al. Socioeconomic status and child development: a meta-analysis. J. Emot. Behav. Disord. 2011;21(3):211–224. [Google Scholar]
- Loeber R., Farrington D.P., et al. Routledge; New York, NY: 2008. Violence and Serious Theft: Development and Prediction from Childhood to Adulthood. [Google Scholar]
- Luciana M., Bjork J.M., et al. Adolescent neurocognitive development and impacts of substance use: overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev. Cogn. Neurosci. 2018;32:67–79. doi: 10.1016/j.dcn.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maiese D.R., Hendershot T., et al. RTI Press; Research Triangle Park, NC: 2013. PhenX: Establishing A Consensus Process to Select Common Measures for Collaborative Research (RTI Press Publication NO MR-0027-1310) [PubMed] [Google Scholar]
- McCarty C.A., Huggins W., et al. PhenX RISING: real world implementation and sharing of PhenX measures. BMC Med. Genom. 2014;7:16. doi: 10.1186/1755-8794-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoyd V.C. Socioeconomic disadvantage and child development. Am. Psychol. 1998;53(2):185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Mukhara D., Banks M.L., et al. Stress as a risk factor for substance use disorders: a mini-review of molecular mediators. Front. Behav. Neurosci. 2018;12:309. doi: 10.3389/fnbeh.2018.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J., Oldehinkel A.J., et al. The TRacking adolescents’ individual lives survey (TRAILS): design, current status, and selected findings. J. Am. Acad. Child. Adolesc. Psychiatry. 2012;51(10):1020–1036. doi: 10.1016/j.jaac.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Pagliaccio D., Luking K.R., et al. Revising the BIS/BAS Scale to study development: measurement invariance and normative effects of age and sex from childhood through adulthood. Psychol. Assess. 2016;28(4):429–442. doi: 10.1037/pas0000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piquero A.R., Macintosh A.R., et al. The validity of self-reported delinquency scale: comparisons across gender, age, race and place of residence. Sociol. Methods Res. 2002;30(4):492–529. [Google Scholar]
- Prinstein M.J., Boergers J., et al. Overt and relational aggression in adolescents: social-psychological adjustment of aggressors and victims. J. Clin. Child Psychol. 2001;30(4):479–491. doi: 10.1207/S15374424JCCP3004_05. [DOI] [PubMed] [Google Scholar]
- Reiersen A.M., Constantino J.N., et al. Evidence for shared genetic influences on self-reported ADHD and autistic symptoms in young adult australian twins. Twin Res. Hum. Genet. 2008;11(6):579–585. doi: 10.1375/twin.11.6.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc. Sci. Med. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- Rice J.P., Reich T., et al. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol. Clin. Exp. Res. 1995;19(4):1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- Robbers S.C., Bartels M., et al. A twin-singleton comparison of developmental trajectories of externalizing and internalizing problems in 6- to 12-year-old children. Twin Res. Hum. Genet. 2010;13(1):79–87. doi: 10.1375/twin.13.1.79. [DOI] [PubMed] [Google Scholar]
- Robbers S.C., van Oort F.V., et al. Trajectories of CBCL attention problems in childhood. Eur. Child Adolesc. Psychiatry. 2011;20(8):419–427. doi: 10.1007/s00787-011-0194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles Z., Garey L., et al. Examining an underlying mechanism between perceived stress and smoking cessation-related outcomes. Addict. Behav. 2016;58:149–154. doi: 10.1016/j.addbeh.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsman J.M., Butt Z., et al. Emotion assessment using the NIH toolbox. Neurology. 2013;80(11 Suppl. 3):S76–S86. doi: 10.1212/WNL.0b013e3182872e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G.K. Area deprivation and widening inequalities in US mortality, 1969–1998. Am. J. Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slaughter R.I., Hamilton A.S., et al. Relationships between parent and adolescent/young adult mental health among hispanic and non-hispanic childhood cancer survivors. J. Psychosoc. Oncol. 2020;38(6):746–760. doi: 10.1080/07347332.2020.1815924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T.W., Marsden P., et al. NORC at the University of Chicago; Chicago: 2015. General Social Surveys, 1972–2012: Cumulative Codebook. [Google Scholar]
- Southam-Gerow M.A., Kendall P.C. Emotion regulation and understanding: implications for child psychopathology and therapy. Clin. Psychol. Rev. 2002;22(2):189–222. doi: 10.1016/s0272-7358(01)00087-3. [DOI] [PubMed] [Google Scholar]
- Sterne J.A.C. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. Brit. Med. J. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart R.W., Drescher C.F., et al. The development and psychometric investigation of the cyberbullying scale. J. Interpers. Violence. 2014;29(12):2218–2238. doi: 10.1177/0886260513517552. [DOI] [PubMed] [Google Scholar]
- Stoltenberg S.F., Mudd S.A., et al. Evaluating measures of family history of alcoholism: density versus dichotomy. Addiction. 1998;93(10):1511–1520. doi: 10.1046/j.1360-0443.1998.931015117.x. [DOI] [PubMed] [Google Scholar]
- Stover P.J., Harlan W.R., et al. PhenX: a toolkit for interdisciplinary genetics research. Curr. Opin. Lipidol. 2010;21(2):136–140. doi: 10.1097/MOL.0b013e3283377395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strohschein L. Household income histories and child mental health trajectories. J. Health Soc. Behav. 2005;46(4):359–375. doi: 10.1177/002214650504600404. [DOI] [PubMed] [Google Scholar]
- Tara M.C., Turpyn C.C., et al. Parenting-focused mindfulness intervention reduces stress and improves parenting in highly-stressed mothers of adolescents. Mindfulness. 2021;12(2):450–462. doi: 10.1007/s12671-018-1026-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theobald D., Farrington D.P., et al. Scaling up from convictions to self-reported offending. Crim. Behav. Ment. Health. 2014;24(4):265–276. doi: 10.1002/cbm.1928. [DOI] [PubMed] [Google Scholar]
- Tiet Q.Q., Bird H.R., et al. Relationship between specific adverse life events and psychiatric disorders. J. Abnorm. Child Psychol. 2001;29(2):153–164. doi: 10.1023/a:1005288130494. [DOI] [PubMed] [Google Scholar]
- Turkson S., Kloster A., et al. Neuroendocrine drivers of risk and resilience: the influence of metabolism & mitochondria. Front. Neuroendocrinol. 2019;54 doi: 10.1016/j.yfrne.2019.100770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Oort F.V., Greaves-Lord K., et al. The developmental course of anxiety symptoms during adolescence: the TRAILS study. J. Child Psychol. Psychiatry. 2009;50(10):1209–1217. doi: 10.1111/j.1469-7610.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- van Oort F.V., van der Ende J., et al. Cross-national comparison of the link between socioeconomic status and emotional and behavioral problems in youths. Soc. Psychiatry Psychiatr. Epidemiol. 2011;46(2):167–172. doi: 10.1007/s00127-010-0191-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volicer B.J., Volicer L., et al. Variation in length of time to development of alcoholism by family history of problem drinking. Drug Alcohol Depend. 1983;12(1):69–83. doi: 10.1016/0376-8716(83)90055-8. [DOI] [PubMed] [Google Scholar]
- Watts A.L., Smith G.T., et al. Factor structure, measurement and structural invariance, and external validity of an abbreviated youth version of the UPPS-P Impulsive Behavior Scale. Psychol. Assess. 2020;32(4):336–347. doi: 10.1037/pas0000791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead B.R., Bergeman C.S. The effect of the financial crisis on physical health: perceived impact matters. J. Health Psychol. 2017;22(7):864–873. doi: 10.1177/1359105315617329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson L.T.F. Statistical methods in psychology journals. Am. Psychol. 1999;54:594–604. [Google Scholar]
- Youngstrom E.A., Findling R.L., et al. Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychol. Assess. 2001;13(2):267–276. [PubMed] [Google Scholar]
- Youngstrom E.A., Frazier T.W., et al. Developing a 10-item mania scale from the parent general behavior inventory for children and adolescents. J. Clin. Psychiatry. 2008;69(5):831–839. doi: 10.4088/jcp.v69n0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Youngstrom E.A., Murray G., et al. The 7 up 7 down inventory: a 14-item measure of manic and depressive tendencies carved fron the general behavior inventory. Psychol. Assess. 2013;25:1377–1383. doi: 10.1037/a0033975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Supplementary material