Abstract
Objective
To estimate and compare unmet health care needs of persons with spinal cord injury (SCI) across countries, the causes of these shortfalls, and the role of income.
Data Sources
We analyzed cross‐sectional data of 20 countries from the International Spinal Cord Injury (InSCI) survey, a compendium of comparable data on the living situation of persons with SCI. Data included information on high‐, middle‐, and low‐income countries. The survey comprises information on 12,095 participants.
Study Design
We used logit regressions to estimate the probability of unmet health care needs of persons with SCI and its causes. We adjusted the results by the individuals' characteristics and countries' fixed effects. We disaggregated the results by income decile of individuals in each country.
Data Collection/Extraction Methods
The inclusion criteria for the InSCI survey were adults aged 18 years and older with SCI living in the community, who were able to respond to the survey and who provided informed consent.
Principal Findings
Unmet health care needs are significant for people with long‐term conditions like SCI, where people in low‐income groups tend to be more affected. Among the barriers to meeting health care needs, the foremost is health care cost (in 11 of the 20 countries), followed by transportation and service availability. Persons with SCI in Morocco reported the highest probability of unmet health care needs in the sample, 0.54 (CI: 047–0.59), followed well behind by South Africa, 0.27 (CI: 0.20–0.33), and Brazil, 0.26 (CI: 0.20–0.33). In contrast, persons with SCI in Spain, 0.06 (CI: 0.04–0.08), reported the lowest probability of unmet health care needs, closely followed by Norway, 0.07 (CI: 0.05–0.09), Thailand, 0.08 (CI: 0.05–0.11), France, 0.08 (CI: 0.06–0.11), and Switzerland, 0.09 (CI: 0.07–0.10).
Conclusions
SCI is a long‐term, irreversible health condition characterized by physical impairment and a series of chronic illness. This makes SCI a high‐need, high‐cost group that faces significant unmet health care needs, which are mainly explained by the costs of health services, transportation, and services availability. This situation is prevalent in low‐, middle‐, and high‐income countries, where persons in lower income groups are disproportionately affected. To improve the situation, a combination of measures from the health and social systems are required.
Keywords: health care access, income inequality, out‐of‐pocket expenditure, spinal cord injury, unmelt health care needs
What is known on this topic
Unmet health care needs are a prevalent issue even in countries purporting to have universal health care.
Affordability is the main reason for unmet health care needs, closely followed by transportation.
In general, lower income groups are more likely to have unmet health care needs.
What this study adds
We compared unmet health care needs of high‐need, high‐cost persons among 20 countries.
The main barriers to get health care are the costs, transportation, and service availability.
The cross‐country comparison helps to identify target areas for improvement in each country.
1. INTRODUCTION
Population dynamics forecast a shift in the health care needs transitioning from infectious diseases to noncommunicable diseases and injuries where low‐ and middle‐income countries will bear the highest burden. 1 , 2 This implies that disability will be at the core of population health, where its consequences go beyond the health of a person, but on how people function in the society. In general, people suffering from a long‐term health conditions or impairments face many barriers in their daily living, 3 , 4 which translates in higher unemployment rates, lower educational outcomes, higher levels of financial hardship, and poverty. This reality not only affects their activity and participation in society but also have long‐term effects on people's health, which in turn exacerbate inequalities. 5 , 6 , 7 Therefore, the health system and its service provisions have a key role, as the quality of life of persons with impairments is heavily dependent on their response and efficacy. 8 , 9 , 10 This puts a disproportionate pressure on the health care system, where the role of the social system becomes more relevant.
This paper analyzes the unmet health care needs of persons with spinal cord injury (SCI). SCI is a long‐term, irreversible physical condition that is generally accompanied by a series of chronic illness. Although the incidence of SCI is low compared to other health conditions, 11 SCI is of special interest to the study of health systems as its treatment requires the interaction and intervention of health care services at different levels, which makes its treatment very expensive. 12 Persons with SCI are thus high‐frequency users of health care services; however, there is no group of medical specialists that can cover all of their needs. 13 The most frequent secondary health conditions associated to SCI are spasticity, constipation, urinary tract infections, chronic pain, sexual dysfunction, fatigue, and mental health disorders. 14 , 15 , 16 In general, their main medical contact is primary care providers, followed by outpatient clinics and inpatient hospitals. More specifically, persons with SCI seek attention from general physicians, physiotherapists, urologists, and spine specialists. 17 , 18 , 19 , 20 , 21 In addition, and depending on the injury level (i.e., paraplegia or tetraplegia), people with SCI require regular support and care from other persons to perform day‐to‐day activities, which means SCI has important spillovers. 22 Finally, as SCI can be the result of traumatic or nontraumatic events, it impacts populations regardless of age and socioeconomic status, which gives the framework for studying disability across the life span. 23 , 24 This study is, therefore, a reflection of how health systems respond to one of the most vulnerable groups across the continuum of care, from the rescue phase to clinical and rehabilitation services to primary and community care.
The objective of this article is to identify how likely a person with SCI is to face unmet health care needs and why. We disaggregated our results to identify the role income plays, where we estimated the situation for the average individual. We compared the results between low‐ and high‐income groups across 20 countries to identify areas for intervention.
2. METHODOLOGY
2.1. Data
We used data from the International Spinal Cord Injury (InSCI) survey. The first edition of this questionnaire was launched in 2017 and included 12,591 participants from 22 countries around the world. The survey collected information on people living with SCI to identify the factors that impact their functioning and well‐being. The survey implemented the International Classification of Functioning, Disability and Health in Rehabilitation instrument to account for differences inherent not only to the health condition SCI but also environmental factors and personal characteristics. 25 The questionnaire includes 125 questions addressing functioning (bodily functions, structures, activities, and participation), contextual factors (environmental and personal factors), lesion characteristics, and an appraisal of health and well‐being. 26 Persons eligible to participate in the InSCI survey were adults aged 18 years and older living in the community with SCI due to traumatic or nontraumatic causes. The survey included all residents in participating countries living with SCI who provided informed consent and were able to respond to the questionnaire. 8 , 27 , 28
To date, exact numbers on the incidence, prevalence, and survival rates of SCI are inexistent. Most of the existent studies rely on approximations that show a great variability from country to country. 24 , 29 The study protocol on InSCI and its power analysis computed a minimum of 200 participants to take part in the survey in each country for comparability purposes. The power analysis was estimated using data from the Swiss Spinal Cord Injury survey, which is the largest survey in Switzerland about people with SCI living in the community. 30 As in many countries registries of persons with SCI were nonexistent, different sampling strategies were implemented. In eight countries, data were collected using a predefined sampling, 14 countries recruited patients directly from health care facilities, that included specialized rehabilitation centers and acute and general hospitals, or patient organizations. Government agencies and pre‐existing databases were also used as sources for recruiting persons with SCI. While six countries uniquely based their recruitment in a sole source, 16 countries used multiple sources. Due to the context in each country, the invitation to participate in the survey applied different strategies as follows: invitation letters, e‐mails, telephone calls, text messages, and face‐to‐face invitations. Sixteen countries sent reminders to potential participants using phone calls and e‐mails when possible. Six countries could not send reminders because participants filled the questionnaires on‐site, and other eligible participants directly refused to participate. The response rate, showing the number of people who participated compared to the total eligible number, varied from 23% in China to 54% in South Africa. Nevertheless, this number was calculated assuming that all the persons who could not be contacted were also eligible to participate. 27 Participants filled the questionnaire using a paper–pencil option, an online version, or an in‐person or telephone interviews.
2.2. Income distribution
To account for the role income plays in unmet health care needs of persons with SCI, it was necessary to standardize the reported income in the survey. Standardization helped to identify how rich or poor a person was in the context of each country in order to make comparisons across countries. We followed related articles working with InSCI data and built income deciles for each participant. 31 To do so, we merged the InSCI survey with external data sources that identified the income distribution in each country at population level and included the following databases: Luxemburg Income Study, World Inequality, European Commission (Eurostat), and single country‐specific databases.
2.3. Outcomes
Study participants were asked to report whether, in the 12 months prior to the survey, they did not get needed health care and the causes for it. To simplify the several reported causes, we classified them into six groups: (1) cost of health care services, (2) transportation, (3) unavailability of health care service, (4) the person was badly treated the last time, (5) lack of information, (6) inadequate provider, (7) could not take time off work, and (8) other reasons.
2.4. Statistical analysis
To assess the extent to which income differences determine unmet health care needs of persons with SCI, we performed a logistic regression that calculated the probability of a person having unmet health care needs and its causes. The regressions adjusted for sex, income status of a person in each country, whether the person was paraplegic or tetraplegic, and the country‐fixed effects.
The results are reported as the probability of unmet health care needs for persons with SCI by cause in each country. The average estimated probabilities by country were computed at the median income decile (D5) to understand the situation of the median income earner. However, we also disaggregated our results by income decile to compare the situation between poor‐ and rich‐income groups in each country. To compare the results, we built a heatmap that displays unmet health care needs by cause in each of the 20 countries.
3. RESULTS
3.1. Sample characteristics
On average, the age of people with SCI reflected significant variations within and between countries, ranging from 38 years in Romania and Morocco to almost 59 years old in the Netherlands. A similar situation was observed in the number of years respondents had lived with their injury—from 3 years in Brazil to 20 years in Japan. The sex distribution in the sample was in line with the ratio (3:1) of SCI among men versus women worldwide. The paraplegia/tetraplegia share changed from country to country, where middle‐income countries showed significant fewer cases of tetraplegia. Nevertheless, in all countries, we observed more individuals with paraplegia, with the exception of Germany, Japan, and Poland, where we have almost a 50/50 paraplegia/tetraplegia share. The income distribution, reported in income deciles, showed that our sample is composed mostly by people whose income falls just below the country median income, with the exception of Australia, Brazil, China, Romania, and the United States, where people were just above the median country income.
In terms of etiology, the great majority of the persons in our sample have SCI due to a traumatic event. The main causes were traffic and work accidents in almost every country, with the exception of Brazil and South Africa where SCI was mostly a result of violence. In Norway, falls and accidents due to leisure or sports were indicated as the main causes of SCI. In Switzerland, traffic and leisure/sport accidents were equally reported as the main causes of SCI (Tables 1).
TABLE 1.
Descriptive statistics
| Country | Sex = male | Age | Years with the injury | Paraplegia | Income decile a | Nontraumatic SCI | Traumatic SCI | N | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Work | Traffic | Leisure/sports | Violence | Falls | Others | ||||||||
| Australia | 73.30% | 57.5 (14.4) | 17.2 (14) | 61.10% | 6.66 (3.08) | 16.30% | 12.90% | 32.60% | 25.60% | 1.10% | 17.40% | 6.00% | 1579 |
| Brazil | 79.10% | 44.2 (16.7) | 3.3 (4.4) | 59.70% | 6.43 (2.89) | 29.90% | 10.00% | 13.90% | 8.50% | 18.90% | 16.90% | 3.00% | 201 |
| China | 71.10% | 49.7 (13.7) | 4.5 (4.2) | 66.90% | 5.37 (2.6) | 32.30% | 12.00% | 19.90% | 9.70% | 1.80% | 23.10% | 2.40% | 1354 |
| France | 72.60% | 51.6 (14.4) | 18.1 (13.7) | 66.30% | 2.96 (2.33) | 18.90% | 10.90% | 44.30% | 11.90% | 1.90% | 16.70% | 2.70% | 413 |
| Germany | 72.00% | 55.4 (14.9) | 12.9 (12.1) | 50.70% | 2.87 (2.37) | 20.20% | 10.90% | 29.30% | 18.10% | 0.70% | 23.30% | 6.10% | 1617 |
| Greece | 73.00% | 46.7 (12.6) | 15 (10.7) | 67.80% | 3.76 (2.66) | 14.00% | 12.00% | 48.00% | 8.50% | 1.50% | 14.50% | 5.50% | 200 |
| Italy | 74.30% | 50.9 (14.6) | 12.1 (9.6) | 73.80% | 3.57 (2.4) | 29.60% | 9.70% | 40.80% | 9.70% | 1.00% | 17.00% | 0.00% | 206 |
| Japan | 84.10% | 54.8 (14.9) | 20 (14.5) | 49.80% | 4.58 (3.63) | 9.90% | 31.10% | 42.70% | 13.20% | 0.00% | 30.80% | 0.30% | 302 |
| Lithuania | 62.80% | 42.3 (11.4) | 15.7 (10) | 70.00% | 3.38 (2.15) | 6.40% | 3.70% | 40.80% | 37.20% | 3.70% | 18.30% | 1.40% | 218 |
| Morocco | 72.50% | 38.6 (13.2) | 7 (8.4) | 74.00% | 1.84 (1.67) | 22.60% | 20.00% | 34.50% | 6.50% | 1.30% | 21.30% | 0.30% | 385 |
| The Netherlands | 66.50% | 58.6 (13.6) | 15.2 (13.8) | 62.30% | 3.73 (2.75) | 36.50% | 10.00% | 20.40% | 16.90% | 1.90% | 12.70% | 6.90% | 260 |
| Norway | 68.50% | 57.2 (16.3) | 8.3 (5.1) | 58.50% | 2.83 (2.44) | 30.00% | 10.30% | 16.40% | 20.70% | 1.50% | 28.20% | 7.20% | 610 |
| Poland | 83.10% | 46.8 (12.7) | 13.8 (10) | 53.50% | 3.31 (2.79) | 10.70% | 16.70% | 31.30% | 23.00% | 1.10% | 28.20% | 4.70% | 971 |
| Romania | 72.20% | 38.2 (11.8) | 8.2 (7.8) | 69.30% | 5.6 (3.13) | 16.20% | 13.00% | 28.70% | 16.20% | 0.50% | 29.60% | 1.90% | 216 |
| South Africa | 75.00% | 38.4 (12.6) | 10.3 (9.1) | 60.70% | 4.9 (2.67) | 7.50% | 4.00% | 31.50% | 17.00% | 34.50% | 7.00% | 0.50% | 200 |
| South Korea | 75.90% | 48 (11.7) | 15.6 (10.1) | 60.20% | 3.19 (2.54) | 7.80% | 14.70% | 47.20% | 11.10% | 0.70% | 21.60% | 4.40% | 890 |
| Spain | 70.00% | 51.3 (13.9) | 16.3 (12.6) | 63.00% | 3.91 (2.62) | 22.50% | 13.90% | 37.60% | 11.80% | 1.70% | 13.90% | 2.60% | 417 |
| Switzerland | 71.20% | 57.2 (14.7) | 19.1 (13.2) | 69.40% | 4.27 (2.74) | 20.40% | 12.00% | 27.50% | 27.50% | 2.00% | 21.60% | 5.50% | 1530 |
| Thailand | 71.20% | 45 (15.6) | 8.3 (8.5) | 74.10% | 2.94 (2.34) | 13.80% | 11.30% | 51.60% | 1.90% | 6.30% | 15.00% | 0.90% | 320 |
| USA | 58.10% | 45 (15.4) | 12.7 (11.4) | 61.20% | 6.89 (2.59) | 0.00% | 3.40% | 32.50% | 28.10% | 9.40% | 10.80% | 22.20% | 203 |
| Total | 72.90% | 51.7 (15.2) | 13.3 (12) | 62.00% | 4.18 (3) | 19.30% | 12.70% | 31.50% | 18.00% | 2.40% | 21.10% | 4.60% | 12,092 |
Note: For continuous variables, the reported numbers are the mean. Standard deviations are in parentheses.
Abbreviation: SCI, spinal cord injury.
The income variable is reported in deciles, from the poorest (1) to the richest 10).
3.2. Unmet health care needs and income disparities
Figure 1 displays the probability of unmet health care needs by income group in the 20 analyzed countries. On average, people in the lowest income group are twice as likely to have unmet health care needs compared to people in the upper income group (black dashed line). The negative relationship means that as people climb the income ladder, unmet health care needs decline. Persons with SCI who have a median income have a 15% probability of their health care needs being unmet—10 points less than for those at the lowest incomes and two points higher than those in the highest income group.
FIGURE 1.
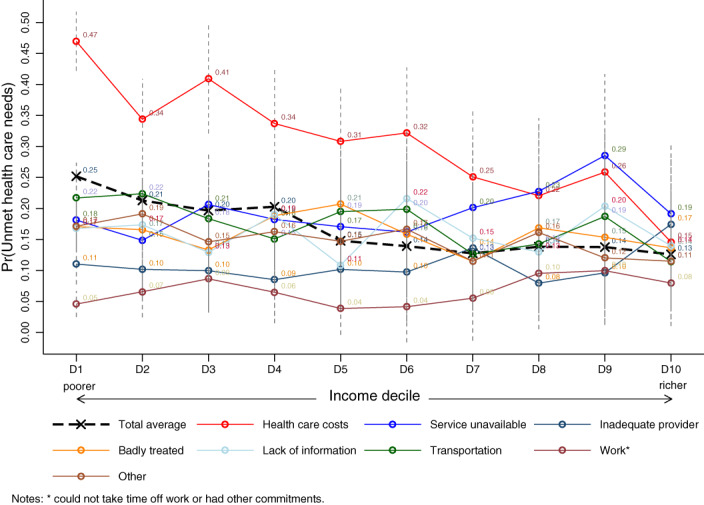
Estimated probability of unmet health care needs by barrier and income decile [Color figure can be viewed at wileyonlinelibrary.com]
The difference in average unmet health care needs between income groups is mainly explained by the cost of health care services. For persons in the poorest groups, the main cause for unmet health care needs is the cost of health care services—three times the probability reported for persons in the richest group. Nevertheless, despite the cost of health care services being less prohibitive for richer groups, this cause emerged among the top causes in all income groups. For upper‐income groups in the last three income deciles (D8–D10), health care costs are the second most reported barrier to accessing health care services, surpassed only by the availability of health services and lack of information. Barriers like inadequate provider or work seem to affect all income groups similarly, the latter being least mentioned across all income groups.
3.3. Comparison across countries
Figure 2 depicts a heatmap that reports estimated probabilities of unmet health care needs by barrier and by country. Due to the several reported barriers, it was not possible to disaggregate the estimates by income decile. Therefore, we provided estimates of unmet health care needs at the median income to better describe the situation for the “average” person with SCI. The results are sorted by country—darker colors represent a higher probability of unmet health care needs. In the first column (orange palette), we reported the average unmet health care needs in each country; in red, we reported unmet health care needs disaggregated by barrier. See Table 2 for confidence intervals (CI).
FIGURE 2.
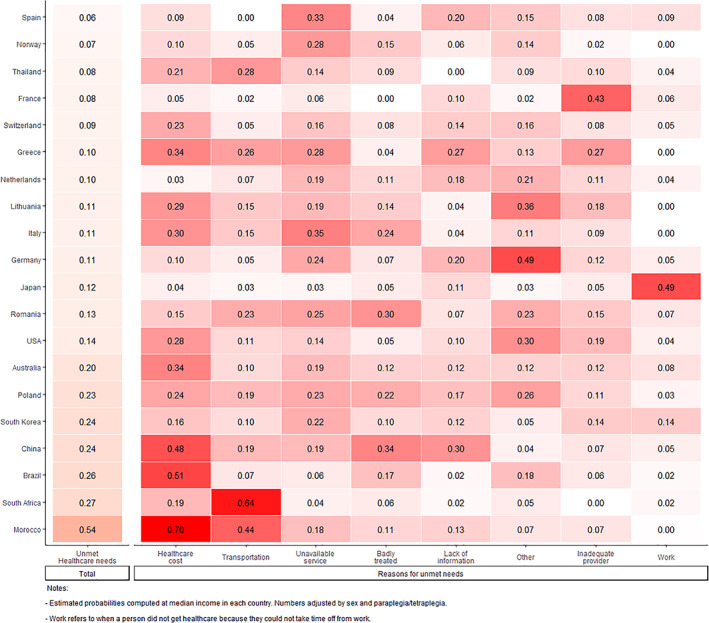
Estimated probability of unmet health care needs total and by barrier [Color figure can be viewed at wileyonlinelibrary.com]
TABLE 2.
Estimated probability of unmet health care needs (ll and ul are the lower and upper bound limits of the confidence intervals)
| Country | Unmet health care needs | ll | ul | Health care costs | ll | ul | Transportation | ll | ul | Unavailable service | ll | ul | Badly treated | ll | ul |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spain | 0.06 | 0.04 | 0.08 | 0.09 | 0.00 | 0.19 | 0.33 | 0.14 | 0.52 | 0.04 | 0.00 | 0.11 | |||
| Norway | 0.07 | 0.05 | 0.09 | 0.10 | 0.03 | 0.18 | 0.05 | 0.00 | 0.10 | 0.28 | 0.15 | 0.41 | 0.15 | 0.06 | 0.25 |
| Thailand | 0.08 | 0.05 | 0.11 | 0.21 | 0.08 | 0.34 | 0.28 | 0.13 | 0.44 | 0.14 | 0.01 | 0.27 | 0.09 | 0.00 | 0.19 |
| France | 0.08 | 0.06 | 0.11 | 0.05 | 0.00 | 0.11 | 0.02 | 0.00 | 0.06 | 0.06 | 0.00 | 0.14 | |||
| Switzerland | 0.09 | 0.07 | 0.10 | 0.23 | 0.15 | 0.32 | 0.05 | 0.01 | 0.09 | 0.16 | 0.09 | 0.24 | 0.08 | 0.02 | 0.13 |
| Greece | 0.10 | 0.06 | 0.14 | 0.34 | 0.12 | 0.55 | 0.26 | 0.08 | 0.44 | 0.28 | 0.09 | 0.46 | 0.05 | 0.00 | 0.13 |
| The Netherlands | 0.10 | 0.07 | 0.14 | 0.03 | 0.00 | 0.08 | 0.07 | 0.00 | 0.16 | 0.19 | 0.04 | 0.34 | 0.11 | 0.00 | 0.22 |
| Lithuania | 0.11 | 0.07 | 0.15 | 0.29 | 0.13 | 0.45 | 0.15 | 0.02 | 0.28 | 0.19 | 0.05 | 0.34 | 0.14 | 0.01 | 0.26 |
| Italy | 0.11 | 0.07 | 0.15 | 0.30 | 0.13 | 0.47 | 0.15 | 0.01 | 0.29 | 0.35 | 0.15 | 0.55 | 0.24 | 0.07 | 0.42 |
| Germany | 0.11 | 0.10 | 0.13 | 0.10 | 0.06 | 0.14 | 0.05 | 0.02 | 0.08 | 0.24 | 0.17 | 0.31 | 0.07 | 0.03 | 0.11 |
| Japan | 0.13 | 0.09 | 0.17 | 0.04 | 0.00 | 0.11 | 0.03 | 0.00 | 0.08 | 0.03 | 0.00 | 0.08 | 0.05 | 0.00 | 0.13 |
| Romania | 0.13 | 0.08 | 0.18 | 0.15 | 0.01 | 0.29 | 0.23 | 0.06 | 0.39 | 0.25 | 0.09 | 0.42 | 0.30 | 0.13 | 0.47 |
| USA | 0.14 | 0.08 | 0.19 | 0.28 | 0.07 | 0.50 | 0.11 | 0.00 | 0.25 | 0.14 | 0.00 | 0.28 | 0.05 | 0.00 | 0.14 |
| Australia | 0.20 | 0.17 | 0.22 | 0.34 | 0.27 | 0.41 | 0.10 | 0.06 | 0.14 | 0.19 | 0.14 | 0.24 | 0.13 | 0.08 | 0.17 |
| Poland | 0.23 | 0.20 | 0.25 | 0.24 | 0.19 | 0.30 | 0.19 | 0.14 | 0.24 | 0.23 | 0.17 | 0.29 | 0.23 | 0.17 | 0.28 |
| South Korea | 0.24 | 0.21 | 0.27 | 0.16 | 0.12 | 0.21 | 0.10 | 0.06 | 0.13 | 0.22 | 0.16 | 0.28 | 0.10 | 0.06 | 0.14 |
| China | 0.25 | 0.22 | 0.27 | 0.48 | 0.42 | 0.53 | 0.19 | 0.15 | 0.23 | 0.19 | 0.15 | 0.23 | 0.34 | 0.29 | 0.39 |
| Brazil | 0.26 | 0.20 | 0.33 | 0.51 | 0.36 | 0.67 | 0.07 | 0.00 | 0.14 | 0.06 | 0.00 | 0.13 | 0.17 | 0.06 | 0.28 |
| South Africa | 0.27 | 0.20 | 0.33 | 0.19 | 0.09 | 0.29 | 0.64 | 0.50 | 0.77 | 0.04 | 0.00 | 0.09 | 0.06 | 0.00 | 0.12 |
| Morocco | 0.54 | 0.49 | 0.59 | 0.70 | 0.63 | 0.77 | 0.44 | 0.36 | 0.51 | 0.18 | 0.12 | 0.23 | 0.11 | 0.07 | 0.16 |
| Country | Lack of information | ll | ul | Other | ll | ul | Inadequate provider | ll | ul | Work related | ll | ul |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spain | 0.20 | 0.04 | 0.36 | 0.15 | 0.01 | 0.29 | 0.08 | 0.00 | 0.19 | 0.09 | 0.00 | 0.20 |
| Norway | 0.06 | 0.00 | 0.12 | 0.14 | 0.05 | 0.23 | 0.02 | 0.00 | 0.06 | |||
| Thailand | 0.09 | 0.00 | 0.18 | 0.10 | 0.00 | 0.21 | 0.04 | 0.00 | 0.11 | |||
| France | 0.10 | 0.01 | 0.20 | 0.02 | 0.00 | 0.07 | 0.43 | 0.27 | 0.59 | 0.06 | 0.00 | 0.15 |
| Switzerland | 0.14 | 0.07 | 0.22 | 0.16 | 0.08 | 0.23 | 0.08 | 0.02 | 0.14 | 0.05 | 0.00 | 0.09 |
| Greece | 0.27 | 0.09 | 0.46 | 0.13 | 0.00 | 0.27 | 0.27 | 0.09 | 0.46 | |||
| The Netherlands | 0.18 | 0.04 | 0.33 | 0.21 | 0.06 | 0.36 | 0.11 | 0.00 | 0.23 | 0.04 | 0.00 | 0.12 |
| Lithuania | 0.04 | 0.00 | 0.10 | 0.36 | 0.18 | 0.54 | 0.19 | 0.04 | 0.33 | |||
| Italy | 0.04 | 0.00 | 0.12 | 0.11 | 0.00 | 0.24 | 0.09 | 0.00 | 0.20 | |||
| Germany | 0.20 | 0.14 | 0.26 | 0.49 | 0.41 | 0.58 | 0.12 | 0.07 | 0.17 | 0.05 | 0.02 | 0.09 |
| Japan | 0.11 | 0.01 | 0.21 | 0.03 | 0.00 | 0.08 | 0.05 | 0.00 | 0.13 | 0.49 | 0.32 | 0.66 |
| Romania | 0.07 | 0.00 | 0.17 | 0.23 | 0.07 | 0.38 | 0.15 | 0.01 | 0.28 | 0.07 | 0.00 | 0.16 |
| USA | 0.10 | 0.00 | 0.23 | 0.30 | 0.10 | 0.51 | 0.19 | 0.02 | 0.36 | 0.04 | 0.00 | 0.12 |
| Australia | 0.12 | 0.08 | 0.17 | 0.12 | 0.08 | 0.17 | 0.13 | 0.08 | 0.17 | 0.08 | 0.05 | 0.12 |
| Poland | 0.17 | 0.12 | 0.22 | 0.26 | 0.20 | 0.32 | 0.11 | 0.07 | 0.15 | 0.03 | 0.01 | 0.06 |
| South Korea | 0.13 | 0.08 | 0.17 | 0.05 | 0.03 | 0.08 | 0.15 | 0.10 | 0.19 | 0.15 | 0.09 | 0.20 |
| China | 0.30 | 0.25 | 0.35 | 0.04 | 0.02 | 0.06 | 0.07 | 0.04 | 0.10 | 0.05 | 0.02 | 0.07 |
| Brazil | 0.02 | 0.00 | 0.06 | 0.18 | 0.07 | 0.29 | 0.06 | 0.00 | 0.13 | 0.02 | 0.00 | 0.06 |
| South Africa | 0.02 | 0.00 | 0.06 | 0.05 | 0.00 | 0.11 | 0.02 | 0.00 | 0.06 | |||
| Morocco | 0.13 | 0.08 | 0.18 | 0.07 | 0.04 | 0.11 | 0.08 | 0.04 | 0.11 | 0.01 | 0.00 | 0.02 |
Note: Probabilities estimated at median income. Numbers adjusted by sex and paraplegia/tetraplegia. Confidence intervals estimated at 95% level.
The country reporting the highest probability of unmet health care needs is Morocco with 0.54 (CI: 0.49–0.59), followed well behind by South Africa (0.27, CI: 0.20–0.33) and Brazil (0.26, CI: 0.20–0.33). In contrast, Spain, with 0.06 (CI: 0.04–0.08), exhibited the lowest probability of unmet health care needs in the sample, closely followed by Norway 0.07 (CI: 0.05–0.09), Thailand (0.08, CI: 0.05–0.11), France (0.08, CI: 0.06–0.011), and Switzerland (0.09, CI: 0.07–0.10). In the middle, we find Greece and the United States with values ranging from above 0.10 to 0.14. Australia, Poland, South Korea, and China display values above 0.20.
The heatmap also serves as a tool to identify the most common barriers to accessing health care in each country. Not surprisingly, health care costs appear among the top barriers (either first or second most mentioned barrier) for unmet health care needs in 11 of 20 analyzed countries, except for the Netherlands (0.03, CI: 0.0–0.08) where costs appear in the last positions. Japan (0.04, CI: 0.0–0.1) and France (0.05, CI: 0.0–0.1) display very low levels of unmet health care needs related to costs; however, other barriers are even less important for these two countries. Interestingly, as the probability of unmet health care needs increases, the most likely barrier is the costs of health services.
As for other barriers, transportation—referring to either its availability or cost—appeared as the most significant barrier to accessing health care in South Africa (0.64, CI: 0.50–0.77) and Thailand (0.28, CI: 0.13–0.44). In Morocco (0.44, CI: 0.36–0.51), transportation was the second most significant barrier. Service availability affected almost half of the countries, being the most common barrier in Spain (0.33, CI: 0.14–0.52), Norway (0.28, CI: 0.15–0.41), Italy (0.35, CI: 0.15–0.55), and South Korea (0.22, CI: 0.16–0.28). Having received bad treatment was an issue in China (0.34, CI: 0.29–0.39), Romania (0.30, CI: 0.13–0.47), Italy (0.24, CI: 0.07–0.42), and Poland (0.23, CI: 0.17–0.28). Lack of information affected people in China (0.30, CI: 0.25–0.35), Greece (0.27, CI: 0.09–0.46), Germany (0.20, CI: 0.14–0.26), Spain (0.20, ci: 0.04–0.36), the Netherlands (0.18, CI: 0.04–0.33), and Poland (0.17, CI: 0.12–0.22). Other reasons appeared mostly in Germany (0.49, CI: 0.41–0.58) as the main barrier to accessing health care, followed by Lithuania (0.36, CI: 0.18–0.54), the United States (0.30, CI: 0.10–0.51), Poland (0.26, CI: 0.20–0.32), and the Netherlands (0.21, CI: 0.06–0.36). Inadequate provider was the most reported barrier in France (0.43, CI: 0.27–0.59) and work in Japan (0.49, CI: 0.32–0.66).
To account for income disparities omitted in the heatmap, we included Figure 3, which disaggregates unmet health care needs by income group—low‐income groups that include the first two deciles (D1–D2) and high‐income groups that include the last three income deciles (D8–10). The results show that even in countries with a low probability of unmet health care needs, the situation was not homogeneous for all persons, and this was linked to income status. In general, people in low‐income groups have a significantly higher probability of unmet health care needs compared to people in high‐income groups in the same country. This situation is more evident in Germany, South Africa, China, and South Korea. In the case of Germany, for example, while people in the highest income groups reported almost no unmet health care needs, those in low‐income groups reported unmet health care needs (0.16) comparable to low‐income groups only in Italy or the United States. A similar situation is observed in more inequitable countries like China or South Africa, where people in high‐income groups reported unmet health care needs (0.12) comparable to the situation of people in Switzerland or Norway (0.11). In contrast, in the same countries, people in low‐income groups reported unmet health care needs (0.42–0.49) comparable to levels revealed by Morocco, the country with the highest probability of unmet health care needs in the sample.
FIGURE 3.
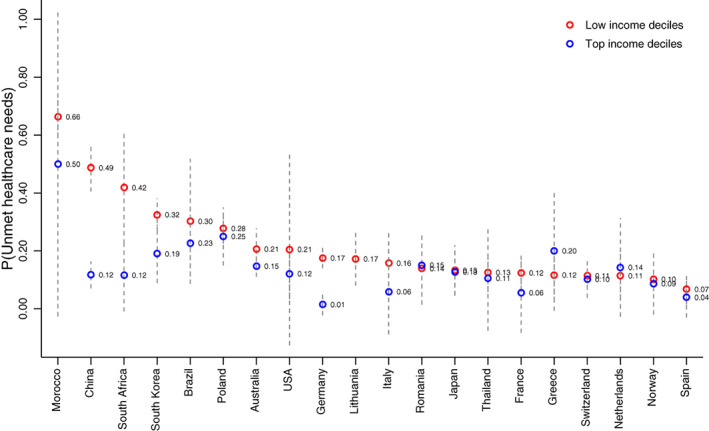
Estimated probability of unmet health care needs by income groups [Color figure can be viewed at wileyonlinelibrary.com]
Finally, there are several countries in our sample in which income differences play a less important role in identifying unmet health care needs. This is the case in Spain, Norway, Switzerland, Thailand, Japan, the Netherlands, Australia, Romania, and Poland, where high‐ and low‐income groups reported a similar probability of unmet health care needs. In the case of Lithuania, the sample was composed only of people in low‐income groups, which made it impossible to disaggregate unmet health care needs by income group.
4. DISCUSSION
Unmet health care needs are significant among people with impairments like SCI that tend to affect people in low‐income groups more. Among the highest barriers to meeting health care needs, we found first health care cost (the barrier most reported in 11 of the 20 countries), followed by transportation and service availability. In general, our results show that when a country exhibits high unmet health care needs due to the cost of health services or transportation, as in the cases of Morocco, South Africa, or Brazil, other barriers almost disappear. This suggests that when people cannot afford health care, they are almost completely barred from the system, making them unable to evaluate other characteristics, such as the quality of services, quality of treatment, or information given by health care providers. In contrast, in countries where unmet health care needs are attributed to reasons other than cost, as in the cases of Germany, Spain, or Japan, other characteristics of the system emerge as barriers.
Certain cases in our results are worth highlighting. For example, Spain exhibits the lowest level of unmet health care needs in the sample. Nevertheless, when the results are disaggregated by income, Germany takes over the first position, as richer groups in the country report the lowest levels of unmet needs in the sample. Nevertheless, people in poorer groups are significantly better positioned in Spain compared to Germany.
On average, middle‐income countries show a higher probability of unmet health care needs compared to high‐income countries, with the exception of Thailand. People with SCI in Thailand report unmet health care needs comparable to Switzerland, yet its annual per capita health expenditure (in purchasing power parity [PPP]) is about 722 USD, compared to 8113 USD in Switzerland, 32 less than one‐tenth the amount. Interestingly, both countries have a high insurance coverage, and their main barrier to access health care services is the cost of health services. A potential explanation for this result may be the marked differences in out‐of‐pocket (OOP) expenditure—Thailand reports 80 USD (in PPP), while in Switzerland, this indicator is around 2270 USD. 33 A similar situation is observed in Lithuania for which we unfortunately have no participants in the high‐income group. Nevertheless, the results reflected by the low‐income group place Lithuania among the countries with low levels of unmet health care needs. The case is the same in Romania where people with SCI in the low‐ and high‐income groups show a probability of unmet health care needs comparable only to the Netherlands.
It is also pertinent to analyze results in relation to the context of each count, especially for barriers not directly related to the health system, such as transportation or work‐related factors. In the first case, even though some countries have high‐quality infrastructure, the use of private vehicles is generalized. Therefore, unmet health care needs might not be attributable to the lack of transportation but rather to specific preferences—vehicles adapted for persons with disabilities are more expensive and therefore affect low‐income groups more. Similarly, with regard to work‐related factors, the barrier may not be the impossibility of taking time off from work to seek health care but rather the preference of users not to leave work for a health visit. In this case, unmet health care needs should not be analyzed as an issue needing to be addressed by the health system but rather as a cultural factor.
Finally, it is interesting that for some countries in the sample, the gap between income groups is almost negligible, like in Spain, Norway, the Netherlands, Switzerland, Thailand, Japan, Romania, and Poland. These numbers may reflect the existence of additional support measures targeting low‐income groups to guarantee their access to health care. 34 In fact, all countries in the sample provide disability insurance to persons with SCI, money that is supposed to cover for the income loss due to their health condition. Depending on the country, however, the amount of the allowance has big variations, and, in many cases, it is only a subsistence allowance. Some countries have more generous schemes, where persons with SCI can make a living with it. 35 In many cases, the disability insurance is conditioned to the working status of the beneficiary, which may push them away from the labor market. Nevertheless, the evidence on the impact of disability insurance is quite heterogeneous and depends on its regulations and the context of each country. 36
Our results are in line with related literature reporting that unmet health care needs are a latent issue in many countries. In general, most studies found that affordability is the main barrier to accessing health services, and they recommended that health systems redefine their insurance schemes in order to increase their coverage. Likewise, several studies reviewing affordability found that poorer groups are always in a worse situation. 37 Nevertheless, in countries where health care coverage is broad, tending toward universality, or in countries with strong welfare programs, despite the impact of unmet health care needs, 32 barriers such as cost of services are significantly reduced. To our knowledge, this is the first study that analyzes and compares unmet health care needs and their causes for a specific high‐needs group, like persons with SCI.
Our results have implications for practice and policy making pertaining to disability issues that include the health and social systems. In the case of the health system, the results can be used to prioritize areas for action in each country, which can also improve effectiveness and efficiency in the provision of health services. In fact, and even when most countries in our sample have publicly funded insurances, the insurance coverage is still deficient. Either people cannot afford to buy an insurance, or those covered still face high OOP expenses, reality that is more prevalent among low‐income groups. 38 An alternative could be for the health care system to design pro‐poor insurance schemes that eliminate copayments or cap the OOP expenditure for low‐income groups. Nevertheless, for persons with SCI, insurance coverage might not be the sole solution as this group requires a series of health services, which sometimes are not covered by the insurances. In such cases, the health care system can opt to design specific health care packages for persons with SCI, which include the most cost‐effective clinical interventions. 39
In the case of the social system, it can support the health system by designing support measures aiming at financial protection for high‐needs groups, like persons with SCI. These measures can target barriers that are not directly linked to the health system, such as transportation or the lack of information. In the first case, social insurance can subsidize public transportation to persons facing disability or schedule health care visits to people living in remote locations. In the case of information, the social system can design program aiming at health literacy, where people can learn how to navigate the health care and social systems to get support. In many countries, the social system also provides direct financial support to pay for the additional needs persons with SCI face. These measures include helplessness allowances, assistance allowance, tax deductions, among others.
Finally, the comparisons across countries illustrate the situation of each country and how it compares to others. Such comparisons give accountability to the citizens and provide an overview of a system's performance, which may help identify areas needing improvement, even in countries with high performance and low levels of unmet health care needs. Taking action on time can not only save many lives and have long‐term effects on the overall health of this group but also could reduce the costs for the health and social systems. 40
4.1. Limitations of the current study
Existing information about the incidence and prevalence of SCI is very limited. To date, exact numbers are nonexistent, and the available information varies greatly, both between and within countries. Therefore, designing representative samples of persons with SCI is challenging. In fact, as detailed in the methodology section, some countries were unable to randomize their sample, and convenience sampling had to be implemented, which translated into some countries' data having been collected from a single source. Although we addressed this problem by disaggregating our results by income deciles, there may be some unobserved heterogeneity within the context of each country that could affect our results. Among them, we can list three factors: (1) special insurance schemes targeting specific groups; (2) additional support measures from the social system designed for people with disabilities; and (3) lack of information from the highest income groups.
In the first case, special insurance schemes in some countries may place certain groups, especially low‐income groups, in a better position than the “average” individual within that group. Such is the case of military insurance, special insurance for civil servants, or insurance for low‐income groups that, in general, provide more comprehensive coverage and do not require copayments. In the case of military insurance, we do not consider this an important issue, as SCI in our sample was mostly caused by traumatic events related to work or car accidents for which standard insurances are more relevant. In the case of health insurance for civil servants, only Thailand, in a country case report, described this insurance as part of the national health system. 41 In the case of insurance for low‐income groups, such as Medicaid, or insurances for older people, such as Medicare, in the United States, a country report for persons with SCI suggested that this is significant support, especially for vulnerable populations. However, some drawbacks exist with both insurances, as many users reported the need for supplemental insurance to guarantee access to some services. In addition, there were reports of objection to Medicare's and Medicaid's cumbersome reimbursement process on the part of some providers. 42 When this is the case, people covered under these insurance schemes face additional challenges highly correlated to their income position in accessing health services.
In the second case, support measures from the social system at the national or local level, or in some cases, from patients' associations, may put some of our respondents in a better financial position. Most countries sampled declared having a disability pension, which means that the potential bias in our results is more related to the scope of the pension and its regulations than to the fact of receiving such a pension. In fact, in many countries the disability pension was linked to the working status of a person, where the unemployed were more likely to qualify. Unfortunately, we had no data about specific support measures in each country. Future research should look at the different sources of household income to see how much unmet health care needs change when additional support measures exist.
Finally, to compare results across countries, we needed comparable measures of income in each country to identify how rich or poor an individual was. As we did not have information about income distribution at every income decile, the results, in some cases, exclude data of the extremes of the distribution (i.e., the top 1%) in which income inequality can be more pervasive. Therefore, our results can be seen as underestimating differences in unmet health care needs among income groups.
5. CONCLUSIONS
Unmet health care needs for persons with SCI are a latent issue explained by the costs of health care services, transportation, and services availability. This situation happens is low‐, middle‐, and high‐income countries, where low‐income groups are disproportionately affected. There exist measures the health and social system can undertake in order to reduce the problem. In the case of the health system, it is important to design insurance schemes that limit copayments, or reduce OOP expenses, especially for low‐income groups. Also, as SCI is a high‐need, high‐cost group, the system can design basic care packages to guarantee access to the most cost‐effective interventions. At the same time, the social system can support persons with SCI aiming at financial protection, which include cash allowances, tax deductions, and subsidies. Over time, reducing unmet health care needs can bring long‐term benefits that translate into more vibrant economies with higher productivity and individual well‐being.
ACKNOWLEDGMENTS
This study is based on data from the International Spinal Cord Injury (InSCI) Community Survey (Ref. Am J Phys Med Rehabil. 2017;96[suppl]: S23‐S34). The members of the InSCI Steering Committee are J. Middleton, J. Patrick Engkasan, G. Stucki, M. Brach, J. Bickenbach, C. Fekete, C. Thyrian, L. Battistella, J. Li, B. Perrouin‐Verbe, C. Gutenbrunner, C. Rapidi, L.K. Wahyuni, M. Zampolini, E. Saitoh, B.S. Lee, A. Juocevicius, N. Hasnan, A. Hajjioui, M.W.M. Post, J.K. Stanghelle, P. Tederko, D. Popa, C. Joseph, M. Avellanet, M. Baumberger, A. Kovindha, and R. Escorpizo.
Pacheco Barzallo D, Oña A, Gemperli A. Unmet health care needs and inequality: A cross‐country comparison of the situation of people with spinal cord injury. Health Serv Res. 2021;56(Suppl. 3):1429‐1440. 10.1111/1475-6773.13738
REFERENCES
- 1. Disease burden from non‐communicable diseases. Our world in data. https://ourworldindata.org/grapher/disease-burden-from-ncds. Accessed August 7, 2020.
- 2. WHO, The Global Health Observatory . Noncommunicable diseases. https://www.who.int/data/gho/data/themes/noncommunicable-diseases. Accessed July 12, 2021.
- 3. Casey R. Disability and unmet health care needs in Canada: A longitudinal analysis. Disabil Health J. 2015;8(2):173–181. 10.1016/j.dhjo.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 4. McColl MA, Jarzynowska A, Shortt SED. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010;25(2):205‐218. 10.1080/09687590903537406 [DOI] [Google Scholar]
- 5. Iezzoni LI, Kurtz SG, Rao SR. Trends in U.S. adult chronic disability rates over time. Disabil Health J. 2014;7(4):402–412. 10.1016/j.dhjo.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hughes C. Poverty and Disability. Career Dev Transit Except Individ. 2013;36(1):37–42. 10.1177/2165143413476735. [DOI] [Google Scholar]
- 7. Hughes C, Avoke S. The elephant in the room: poverty, disability, and employment. Res Pract Persons Severe Disabil, 2010;35(1‐2). https://doi.org/10.2511/rpsd.35.1-2.5. [Google Scholar]
- 8. Pacheco Barzallo DP, Gross‐Hemmi M, Bickenbach J, et al. Quality of life and the health system: a 22‐country comparison of the situation of people with spinal cord injury. Arch Phys Med Rehabil. 2020;101(12):2167‐2176. 10.1016/j.apmr.2020.04.030 [DOI] [PubMed] [Google Scholar]
- 9. Goodridge D, Rogers M, Klassen L, et al. Access to health and support services: perspectives of people living with a long‐term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil. 2015;37(16):1401‐1410. 10.3109/09638288.2014.972593 [DOI] [PubMed] [Google Scholar]
- 10. Gulley SP, Rasch EK, Chan L. The complex web of health: relationships among chronic conditions, disability, and health services. Public Health Rep. 2011;126(4):495–507. 10.1177/003335491112600406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kang Yi, Ding H, Zhou H, Wei Z, Liu L, Pan D, Feng S. Epidemiology of worldwide spinal cord injury: a literature review. J Neurorestoratol. 2017;6:1–9. 10.2147/jn.s143236. [DOI] [Google Scholar]
- 12. Yoon J, Chee CP, Su P, Almenoff P, Zulman DM, Wagner TH. Persistence of high health care costs among VA patients. Health Serv Res. 2018;53(5):3898‐3916. 10.1111/1475-6773.12989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organization , The International Spinal Cord Society . In Bickenbach J, Officer A, Shakespeare T, von Groote P (Eds.), International Perspectives on Spinal Cord Injury. Geneva: World Health Organization; 2013. http://www.who.int/disabilities/policies/spinal_cord_injury/en/. Accessed September 25, 2019. [Google Scholar]
- 14. Brinkhof MWG, Al‐Khodairy A, Eriks‐Hoogland I, et al. Health conditions in people with spinal cord injury: contemporary evidence from a population‐based community survey in Switzerland. J Rehabil Med. 2016;48(2):197‐209. 10.2340/16501977-2039 [DOI] [PubMed] [Google Scholar]
- 15. Jensen MP, Truitt AR, Schomer KG, Yorkston KM, Baylor C, Molton IR. Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord. 2013;51(12):882–892. 10.1038/sc.2013.112. [DOI] [PubMed] [Google Scholar]
- 16. Lavis T, Goetz LL. Comprehensive care for persons with spinal cord injury. Phys Med Rehabil Clin N Am. 2019;30(1):55‐72. 10.1016/j.pmr.2018.08.010 [DOI] [PubMed] [Google Scholar]
- 17. Skelton F, Hoffman JM, Reyes M, Burns SP. Examining health‐care utilization in the first year following spinal cord injury. J Spinal Cord Med. 2015;38(6):690–695. 10.1179/2045772314y.0000000269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stillman MD, Frost KL, Smalley C, Bertocci G, Williams S. Health care utilization and barriers experienced by individuals with spinal cord injury. Arch Phys Med Rehabil. 2014;95(6):1114–1126. 10.1016/j.apmr.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 19. Gemperli A, Ronca E, Scheel‐Sailer A, Koch HG, Brach M, Trezzini B. Health care utilization in persons with spinal cord injury: part 1—outpatient services. Spinal Cord. 2017;55(9):823–827. 10.1038/sc.2017.44. [DOI] [PubMed] [Google Scholar]
- 20. Ronca E, Scheel‐Sailer A, Koch HG, Gemperli A. Health care utilization in persons with spinal cord injury: part 2—determinants, geographic variation and comparison with the general population. Spinal Cord. 2017;55(9):828–833. 10.1038/sc.2017.38. [DOI] [PubMed] [Google Scholar]
- 21. Sikka S, Callender L, Driver S, et al. Healthcare utilization following spinal cord injury: Objective findings from a regional hospital registry. J Spinal Cord Med. 2019;42(2):194–200. 10.1080/10790268.2018.1505330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Guilcher SJT, Craven BC, Lemieux‐Charles L, Casciaro T, McColl MA, Jaglal SB. Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil. 2013;35(11):894‐906. 10.3109/09638288.2012.721048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. DeVivo M J. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50(5):365–372. 10.1038/sc.2011.178. [DOI] [PubMed] [Google Scholar]
- 24. Wyndaele M, Wyndaele J‐J. Incidence, prevalence and epidemiology of spinal cord injury: what learns a worldwide literature survey?. Spinal Cord. 2006;44(9):523–529. 10.1038/sj.sc.3101893. [DOI] [PubMed] [Google Scholar]
- 25. Stucki G, Bickenbach J. The international spinal cord injury survey and the learning health system for spinal cord injury. Am J Phys Med Rehabil. 2017;96(2 suppl 1):S2‐S4. 10.1097/PHM.0000000000000678 [DOI] [PubMed] [Google Scholar]
- 26. Fekete C, Post MWM, Bickenbach J, et al. A structured approach to capture the lived experience of spinal cord injury: data model and questionnaire of the international spinal cord injury community survey. Am J Phys Med Rehabil. 2017;96(2 suppl 1):S5‐S16. 10.1097/PHM.0000000000000622 [DOI] [PubMed] [Google Scholar]
- 27. Fekete C, Brach M, Ehrmann C, et al. Cohort Profile of the International Spinal Cord Injury Community Survey Implemented in 22 Countries. Arch Phys Med Rehabil. 2020;101(12):2103–2111. 10.1016/j.apmr.2020.01.022. [DOI] [PubMed] [Google Scholar]
- 28. Gross‐Hemmi M, Post MW, Ehrmann C, et al. Study protocol of the international spinal cord injury (InSCI) community survey. Am J Phys Med Rehabil. 2017;96(2). 10.1097/PHM.0000000000000647 [DOI] [PubMed] [Google Scholar]
- 29. Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52(2):110–116. 10.1038/sc.2012.158. [DOI] [PubMed] [Google Scholar]
- 30. Brinkhof MWG, Fekete C, Chamberlain JD, Post MWM, Gemperli A, SwiSCI Study Group . Swiss national community survey on functioning after spinal cord injury: protocol, characteristics of participants and determinants of non‐response. J Rehabil Med. 2016;48(2):120‐130. 10.2340/16501977-2050 [DOI] [PubMed] [Google Scholar]
- 31. Oña A, Strøm V, Lee B‐S, et al. Health inequalities and income for people with spinal cord injury. A comparison between and within countries. SSM ‐ Population Health. 2021;15:100854. 10.1016/j.ssmph.2021.100854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Current health expenditure per capita, PPP (current international $). Data. https://data.worldbank.org/indicator/SH.XPD.CHEX.PP.CD. Accessed March 9, 2021.
- 33.Health expenditure data. Global health expenditure database; 2021. https://apps.who.int/nha/database/ViewData/Indicators/en. Accessed February 6, 2021.
- 34. Michalopoulos C, Wittenburg D, Israel DAR, Warren A. The effects of health care benefits on health care use and health: a randomized trial for disability insurance beneficiaries. Med Care. 2012;50(9):764‐771. [DOI] [PubMed] [Google Scholar]
- 35. Börsch‐Supan A. Health and disability insurance. ZAF. 2011;44(4):349‐362. 10.1007/s12651-011-0058-6 [DOI] [Google Scholar]
- 36. Maestas N, Mullen KJ, Strand A. Does disability insurance receipt discourage work? Using examiner assignment to estimate causal effects of SSDI receipt. Am Econ Rev. 2013;103(5):1797‐1829. 10.1257/aer.103.5.1797 [DOI] [Google Scholar]
- 37. Hwang J. Understanding reasons for unmet health care needs in Korea: what are health policy implications? BMC Health Serv Res. 2018;18(1):557. 10.1186/s12913-018-3369-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pacheco Barzallo D, Gross‐Hemmi MH. The cross‐cultural societal response to SCI: health and related systems. Am J Phys Med Rehabil. 2017;96(2):S41‐S54. 10.1097/PHM.0000000000000664 [DOI] [PubMed] [Google Scholar]
- 39. Baeten R, Spasova S, Vanhercke B, Coster S, European Commission . Inequalities in Access to Healthcare. A Study of National Policies. 2018. 10.2767/371408 [DOI] [Google Scholar]
- 40. Jamison DT, Summers LH, Alleyne G, et al. Global health 2035: a world converging within a generation. The Lancet. 2013;382(9908):1898–1955. 10.1016/s0140-6736(13)62105-4. [DOI] [PubMed] [Google Scholar]
- 41. Kovindha A. People with spinal cord injury in Thailand. Am J Phys Med Rehabil. 2017;96(2 suppl 1):S120‐S123. 10.1097/PHM.0000000000000585 [DOI] [PubMed] [Google Scholar]
- 42. Richards C, MacKenzie N, Roberts S, Escorpizo R. People with Spinal Cord Injury in the United States. Am J Phys Med Rehabil. 2017;96(2):S124–S126. 10.1097/phm.0000000000000620. [DOI] [PubMed] [Google Scholar]


