Abstract
This report examined baseline affective response to binge eating as a predictor of binge-eating disorder (BED) treatment outcome. Baseline affective response was defined as: (1) each individual’s average net change (i.e., area under the curve [AUC]) of positive affect (PA) or negative affect (NA) before and after binge-eating episodes and (2) post-binge eating slope of PA or NA across seven-days of ecological momentary assessment (EMA). Adults with BED completed Integrative Cognitive-Affective Therapy (ICAT-BED) or cognitive behavioral therapy guided self-help (CBTgsh). Individuals with greater net increases in PA (AUC) following binge eating at baseline exhibited better treatment response in ICAT-BED at end-of-treatment and follow-up. NA affective response was only significant at end-of-treatment; individuals with less rapid post-binge improvements in NA (slope) did better in ICAT-BED, while individuals with lower net improvements in NA (AUC) did better in CBTgsh. Affective response to binge eating may be a marker of BED treatment response.
Keywords: Affective response, binge eating disorder, treatment, affect, ecological momentary assessment
Binge eating disorder (BED) is characterized by episodes of binge eating without regular compensatory behaviors and is associated with obesity and psychiatric impairment (Kessler et al., 2013). Treatments for BED are moderately effective; however, there is wide variability in outcome and a high degree of relapse (Linardon, 2018). Identifying predictors of BED treatment outcome can potentially increase treatment efficacy and effectiveness by informing the development of novel targets as well as determining which individuals may be susceptible to poor treatment course. In addition, identifying pre-treatment characteristics that predict BED treatment outcome could be used to personalize treatments. Previous research has identified overvaluation of shape and weight and rapid response to treatment as predictors of BED treatment outcome (Grilo, 2017), but more research is needed to examine how putative causal and maintenance processes are related to treatment outcome.
The affect regulation model of binge eating suggests that affect is a salient momentary driver of binge eating (Haedt-Matt & Keel, 2011). Further, the model proposes that affective response to binge-eating episodes is an important maintenance factor, such that if binge eating produces sustained decreases in negative affect (NA) or increases in positive affect (PA), the behavior is more likely to be maintained via reinforcement processes. Ecological momentary assessment (EMA) research, analyzed with a multilevel modeling approach using all available data points located in time in relation to binge-eating episodes, on trajectories of NA surrounding binge eating has shown that, on average, NA increases prior to binge eating and decreases afterwards, providing support for the affect regulation model (Berg et al., 2017).
While previous research generally supports the proposition that, on average, binge eating produces momentary reductions in NA and increases in PA (e.g., Berg et al., 2013; Engel et al., 2016), heterogeneity in affective responses to binge eating has not been investigated. Affective responses to other behaviors, particularly health-related behaviors (e.g., physical activity, smoking), have been shown to vary across individuals (De Young et al., 2013; Liao et al., 2017). That is, there is variation in whether individuals increase or decrease in PA and NA states following engaging in various health-related behaviors. Further, individual differences in affective response to such behaviors have been shown to predict long-term outcomes, although the majority of research has focused on physical activity (Kenford et al., 2002; Rhodes & Kates, 2015). For example, in a sample of sedentary adults, greater positive affective response to exercise predicted greater physical activity at six- and twelve-month follow-up (Williams et al., 2008). Yet, it is unclear the extent to which affective response to binge eating relates to treatment outcome in BED. Hypothetically, those who have a more rewarding affective response to binge eating—i.e., more reductions NA and increases in PA—may be less likely to respond to treatment.
While several psychological therapies have been developed to treat BED, integrative cognitive-affective therapy (ICAT; Wonderlich et al., 2015) was recently developed for bulimia nervosa and BED and focuses on the underlying affective motivations for binge eating by providing emotion regulation and coping skills. This is accomplished by increasing participants’ awareness of momentary emotion and its relationship with binge eating and supporting adaptive emotion regulation skill development. This therapeutic approach differs from the cognitive-behavioral approaches to current standard treatment for BED--cognitive behavioral therapy, including guided self-help (CBTgsh; Fairburn, 2008), which emphasizes consistent self-monitoring, the development of regular eating patterns, identification of alternative activities to avoid binge eating, problem-solving, and relapse prevention. Because ICAT-BED targets affective motivations for binge eating, individuals who have a more rewarding affective response to binge eating at baseline may do better in ICAT-BED as it may be more successful at providing alternative emotion regulation and coping strategies.
Given the hypothesized salience of momentary affective reinforcement processes (i.e., decreased post-binge NA and increased post-binge PA) in binge-eating maintenance (Haedt-Matt & Keel, 2011), as well as ICAT’s focus on targeting problematic affect-binge eating relationships, the current paper examined baseline affective response to binge eating (prior to treatment) in the natural environment as a predictor of treatment outcome (i.e., binge-eating frequency) in ICAT-BED versus CBTgsh among individuals with BED. Specifically, individual affective response trajectories before and after binge-eating episodes were modeled using EMA data, and features of those trajectories (i.e., pre-binge eating to post-binge eating change in slope and pre-binge eating to post-binge eating change in area under the curve [AUC, which takes into account peak and slope of affect]) were tested as predictors of binge-eating frequency at end of treatment (EOT) and six-month follow-up.
Affective response was examined in two ways. First, slopes of NA and PA trajectories following binge eating episodes, which indicate the rate of change in affective states, were assessed. Second, changes in AUC of the NA and PA trajectories prior to and after binge episodes were calculated. The AUC measures the total exposure to a particular affect (i.e., positive affect and negative affect) during a given time period (e.g., the total negative affect reported following a binge eating episode); therefore, change in AUC values between the time period before and after binge-eating episodes reflects the overall net change in affective experience resulting from binge eating. Given that a rewarding affective response to a behavior has been shown to increase or maintain a behavior over time (e.g., Kenford et al., 2002; Rhodes & Kates, 2015), it was hypothesized that individuals who showed a more rewarding affective response to binge eating (i.e., greater net reductions in NA and increases in PA) at baseline (prior to treatment) would report lower binge-eating frequency following ICAT-BED compared to CBTgsh.
Method
Participants
Participants were drawn from a sample of 112 adults (82.1% women) who met full Diagnostic and Statistical Manual of Mental Disorders-5 criteria for BED (American Psychiatric Association, 2013). Exclusion criteria for the study included severe comorbid psychopathology (i.e., lifetime history of psychotic symptoms or bipolar disorder, substance use disorder within six months of enrollment) medical or psychiatric instability (e.g. active suicidality), clinically significant purging behavior, eating or weight loss treatment, or a medical condition affecting eating or weight (see Peterson et al., 2020 for detailed exclusion criteria).
Procedure
Participants were recruited from eating disorder clinics, community advertisements, and social media postings at two sites in the Midwest United States. Following an initial eligibility screening, participants completed a baseline assessment comprised of semi-structured clinical interviews assessing eating disorder symptoms and comorbid psychopathology, and a seven-day EMA protocol to assess experiences of affect and binge eating in the natural environment. Following completion of the baseline assessment, participants were randomized to 17 weeks of ICAT-BED (n=56) or CBTgsh (n=56) and assessed at end of treatment (EOT) and six-month follow-up. Supervision was provided by two authors with extensive experience delivering psychotherapy for eating disorders (authors S.A.W. and C.B.P.). As compensation, participants received $150 for assessments following study completion. Institutional review board approval for the study was obtained at each site.
Measures
Eating Disorder Examination 16.0 (EDE; Fairburn et al., 2008).
The EDE was administered by trained assessors to confirm the diagnosis of DSM-5 BED as indicated by at least one objective binge-eating (OBE) episode per week, on average, for the 12 weeks prior to the interview. The EDE was administered at EOT and six-month follow-up assessments. The past 28-day frequency of OBEs was used to assess outcome. Interrater reliability for current BED diagnosis, which was assessed in a random subset of the sample (20%; n=22), indicated perfect agreement among raters.
Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Version (SCID-I/P; First, Spitzer, Gibbon & Williams, 1995).
The SCID-I/P is a semi-structured interview, which assesses current and lifetime history of DSM-IV Axis I psychiatric disorders and was used to assess psychiatric comorbid diagnoses for inclusion criteria and study sample description.
EMA measures.
Participants completed a seven-day period of EMA to assess affect and binge eating at baseline. The EMA protocol utilized both signal and interval contingent recordings. Specifically, participants were prompted to complete assessments throughout the day in response to five semi-random signals, which were distributed around five anchor points between 8 am and 10 pm. In addition, participants completed a final assessment at the end of the day (i.e., bedtime). For each recording, participants were asked to rate their current mood and to report any eating behaviors that had not yet been recorded. Participants indicated the timing of reported eating episodes, in order to locate that eating behavior in time and establish temporality.
Binge eating.
Participants indicated the extent to which each recorded eating episode was characterized by both overeating and loss of control over eating using a Likert-type scale ranging from 1 (not at all) to 5 (extremely). To assess overeating, participants rated the following two items: (a) “To what extent do you feel that you overate?”, and (b) “To what extent do you feel that you ate an excessive amount of food?”. To assess loss of control, participants rated each of the following four questions: (a) “While you were eating, to what extent did you feel a sense of loss of control?”, (b) “While you were eating, to what extent did you feel that you could not resist eating?”, (c) “While you were eating, to what extent did you feel that you could not stop eating once you had started?”, and (d) “While you were eating, to what extent did you feel driven or compelled to eat?”. The two overeating and four loss of control items were averaged to create composite scores reflecting overeating and loss of control eating severity at each eating episode. The occurrence of a binge-eating episode was defined as an episode in which both the overeating and loss of control eating composite scores were ≥4. This dichotomous binge-eating variable was used in subsequent analyses to estimate affect response to binge eating in the natural environment.
Affect.
Five items (i.e., afraid, nervous, upset, ashamed, and hostile) from the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) were used to measure momentary NA, and five items from the PANAS were used to assess PA (i.e., alert, inspired, determined, attentive, and active). At each recording, participants indicated their current affect on a scale from 1 (not at all) to 5 (extremely). NA and PA items were averaged to create composite measures of NA and PA intensity at each signal. The internal consistency for NA and PA were .80 and .88, respectively.
Statistical Analyses
Slope and area under the curve (AUC) calculations.
To examine individuals’ affective responses to binge eating, slope and AUC indices were calculated for each individual in separate n=1 models based on the trajectories of NA and PA leading up to and following EMA-measured binge eating episodes during the pre-treatment EMA monitoring period. To estimate these slope and AUC values, the trajectories of NA and PA in the four hours leading up to and following binge eating episodes were calculated using generalized estimating equations (GEEs), consistent with prior EMA studies (e.g., Berg et al., 2015). Given the limited number of data points (i.e., six signals per day), each GEE model included only linear functions (i.e., slopes), which indicated the rate of change in NA and PA before and after binge-eating episodes. Autoregressive covariance structures (AR1) were used to account for serial correlations between EMA ratings. If more than one binge-eating episode was reported during the same day, only the first episode was used to prevent possible confounding relationships between affect ratings in relation to multiple binge-eating episodes throughout any given day. The slope and intercept parameter estimates from the NA and PA GEE trajectory analyses were extracted for each individual, which provided the first index of interest (i.e., post-binge NA and PA slopes for each individual). Thus, for a given individual, lower post-binge NA slope values reflected a greater rate of improvement in NA after binge-eating episodes, and higher post-binge PA slope values reflected a greater rate of improvement in PA after binge-eating episodes.
In order to calculate the NA and PA AUC changes for each individual, their intercept, slope, and time parameters from the GEE analyses were used to calculate pre- and post-binge NA and PA AUC values based on the trapezoidal method. This involved calculating individual AUC values separately for (1) pre-binge PA AUC, (2) pre-binge NA AUC, (3) post-binge PA AUC, and (4) post-binge NA AUC using the following formula,
| (Equation 1) |
where h is the intercept derived from the GEE (i.e., NA or PA at the time of a binge eating episode), and 𝑏 indicates time in hours (i.e., four hours prior to or after the binge-eating episode). The parameter 𝑎 in Equation 1 was solved for based on Equations 2 and 3 below. This required first calculating the parameter c is based on the linear regression equation (y = intercept + slope * time), where h is the negative and positive intercept derived from the GEE, slope is the pre- or post-binge episode NA or PA slope derived from the GEE, and time is specified as the four hours prior to or following the binge episode:
| (Equation 2) |
Next, the parameter 𝑎 was solved for based on Pythagorean theorem, where ℎ is the intercept derived from the GEE, b is the time prior to or after the binge episode (4 hours), and c is the value derived from Equation 2:
| (Equation 3) |
Thus, the final AUC equation reduces to the following based on Equations 1–3:
After each of the four AUC indices were calculated (i.e., pre-binge PA AUC, pre-binge NA AUC, post-binge PA AUC, and post-binge NA AUC), difference scores were calculated by subtracting the pre-binge AUC value from the post-binge AUC value for both NA and PA. Thus, higher AUC change scores reflect net increases in NA or PA exposure after binge eating episodes, whereas lower AUC change scores reflect net decreases in NA or PA exposure after binge eating episodes. Accordingly, the reinforcing effects of binge eating are indicated by (1) lower NA AUC change scores (including negative scores), reflecting a stronger reduction in NA, and/or (2) higher PA AUC change scores, reflecting a stronger increase in PA.
Associations with treatment response.
Next, we examined the associations between affect responses to binge eating (i.e., operationalized as NA and PA post-binge slopes and changes in NA and PA AUC following binge eating episodes) and treatment response, which was assessed by OBE frequency at EOT and six-month follow-up. In addition, the moderating effect of treatment group (i.e., CBTgsh vs. ICAT-BED) was examined. Separate generalized linear models (GLM) were estimated for each set of independent variables (i.e., NA and PA AUC change scores; NA and PA post-binge slopes) for OBE frequency at each time point (i.e., EOT and follow-up). Each GLM included the main effects of treatment group and affect response indices and the interactions between treatment group and affect response indices. Negative binomial distributions were used to account for non-normal distributions of dependent variables. All GLMs included pre-treatment measures of the dependent variable, age, gender, and body mass index (BMI) as covariates. Analyses were conducted in SPSS version 25 using only available data.
Results
Descriptive and Compliance Data
At baseline, there was sufficient available data for 70 participants to calculate AUC and slope values. Independent samples t-tests indicated that participants who did (n=70) and did not (n=46) have sufficient data to calculate AUC and slope values at baseline (prior to randomization; n=116) did not differ significantly with respect to global eating pathology (t[113]=.39, p=.70), age (t[111]=.48, p=.63), BMI (t[114]=.67, p=.50), or race (χ2[3]=1.66, p=.65); sample sizes varied slightly due to missing data. Groups significantly differed with respect to gender (χ2[1]=4.69, p=.03), such that men were less likely to have sufficient data compared to women. Of the 70 participants with sufficient data, 33 (47.1%) were randomized to ICAT and 36 (51.4%) were randomized to CBTgsh. Of these, 59 completed EOT and 61 completed follow-up assessment.
The mean age of the sample at baseline was 39.6±13.3, and the mean BMI was 34.8±8.4 kg/m2. Most of the sample was Caucasian (92.9%; 1.4% Hispanic 1.4% Asian; 4.3% Other or missing); had attended or finished college (70.0%); were currently employed full-time (60.0%) or part-time (11.4%); and had never been married (40.0%). Baseline EMA compliance was 73.96%. Missingness was not related to demographics, history of mood/substance use/anxiety disorder, or eating disorder psychopathology. There were no significant correlations between affective response parameters and binge-eating frequency at baseline (see Supplementary Table 1). Also, there were no significant differences between treatment groups on baseline affective response parameters (see Supplementary Table 2).
Associations with Binge-eating Frequency at EOT
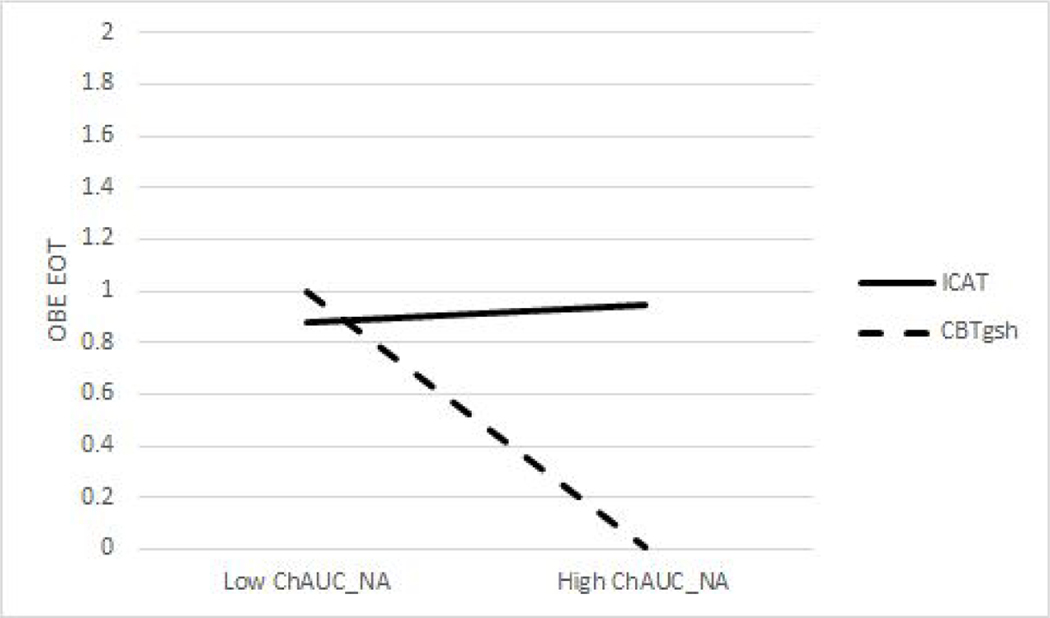
Table 1 displays the results of GLMs examining associations between binge eating frequencies at the end of treatment and 1) NA and PA changes in AUC from before to after binge eating episodes assessed prior to treatment and 2) post-binge NA and PA slopes, measured prior to treatment, 3) the effect of treatment group, and 4) the interaction of both affect response metrics and treatment type. First, there was a significant interaction between pre-treatment NA AUC and treatment type predicting end of treatment OBE frequency. As shown in Figure 1, for those who had higher NA AUC values (reflecting less pre-treatment NA affective reinforcement from binge eating), CBT-gsh was more effective than ICAT-BED; there were no differences between ICAT-BED and CBT-gsh for individuals with high pre-treatment NA affective reinforcement.
Table 1.
Results of generalized linear models examining associations between affective response with binge-eating frequency at end of treatment
| AUC models | B | SE | Lower CI | Upper CI | Wald χ2 | p |
|---|---|---|---|---|---|---|
| Intercept | 2.31 | 1.28 | −0.21 | 4.82 | 3.23 | 0.072 |
| Gendera | −1.13 | 0.58 | −2.27 | 0.01 | 3.76 | 0.053 |
| Groupb | 1.49 | 0.47 | 0.57 | 2.41 | 10.02 | 0.002 |
| Baseline binge eating | −0.02 | 0.03 | −0.07 | 0.03 | 0.39 | 0.532 |
| BMI | −0.04 | 0.03 | −0.10 | 0.02 | 1.97 | 0.161 |
| Age | 0.00 | 0.01 | −0.03 | 0.03 | 0.02 | 0.885 |
| Δ NA AUC | 5.90 | 4.33 | −2.58 | 14.39 | 1.86 | 0.173 |
| Δ PA AUC | −31.38 | 16.70 | −64.10 | 1.34 | 3.53 | 0.060 |
| Group X ΔNA AUC | −95.73 | 37.79 | −169.79 | −21.67 | 6.42 | 0.011 |
| Group X ΔPA AUC | 45.61 | 19.59 | 7.21 | 84.01 | 5.42 | 0.020 |
| Slope models | ||||||
|
| ||||||
| Intercept | 1.98 | 1.26 | −0.48 | 4.45 | 2.49 | 0.114 |
| Gendera | −0.20 | 0.64 | −1.45 | 1.05 | 0.10 | 0.758 |
| Groupb | 2.21 | 0.52 | 1.20 | 3.22 | 18.40 | 0.000 |
| Baseline binge eating | −0.02 | 0.02 | −0.07 | 0.03 | 0.62 | 0.431 |
| BMI | −0.06 | 0.03 | −0.12 | −0.01 | 4.89 | 0.027 |
| Age | −0.01 | 0.02 | −0.04 | 0.02 | 0.19 | 0.666 |
| NA post -binge slope | −10.63 | 3.19 | −16.87 | −4.38 | 11.13 | 0.001 |
| PA post-binge slope | 0.77 | 2.19 | −3.53 | 5.07 | 0.12 | 0.726 |
| Group X NA post-binge slope | 22.06 | 5.68 | 10.94 | 33.19 | 15.11 | <0.001 |
| Group X PA post-binge slope | 1.87 | 3.22 | −4.43 | 8.17 | 0.34 | 0.561 |
Note.
Reference group was men;
Reference group was ICAT-BED
Figure 1.
Interaction of treatment group and change in negative affect (NA) area under the curve (AUC) predicting objective binge eating (OBE) at end of treatment (EOT). High and low values reflect 1 SD above and below sample means. OBE EOT is binge-eating frequency over the past four weeks controlling for baseline frequency.
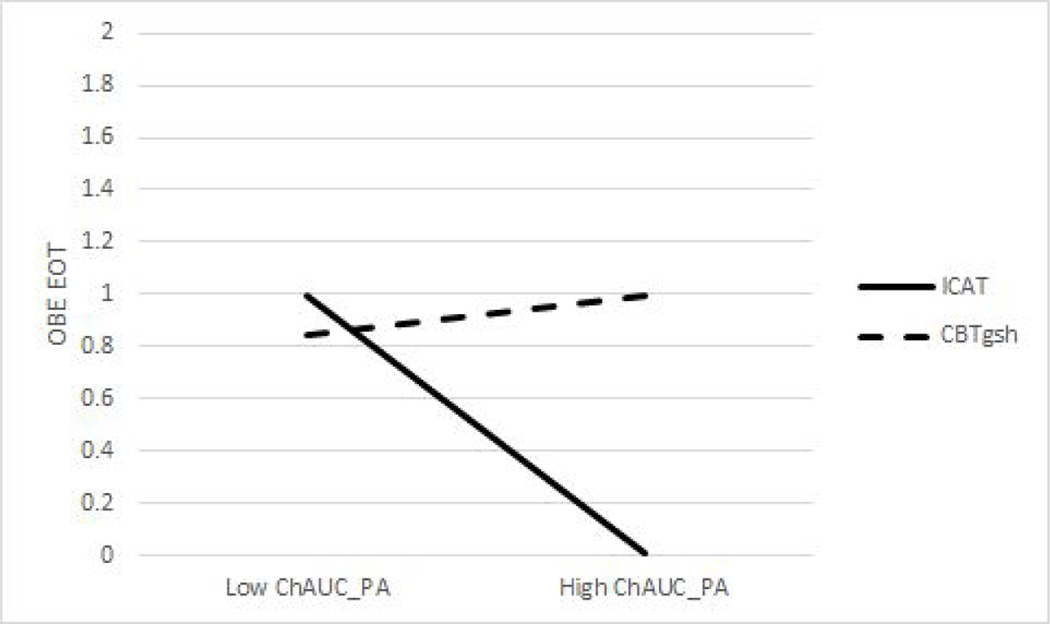
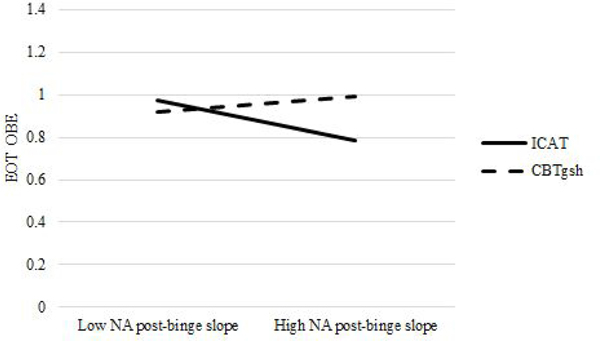
Second, there was a significant interaction between pre-treatment PA AUC and treatment group predicting OBE frequency. As shown in Figure 2, for those who had higher PA AUC pre- treatment values (reflecting more PA affective reinforcement from binge eating), ICAT-BED was more effective than CBT-gsh; there were no differences between ICAT-BED and CBT-gsh for individuals with low pre-treatment PA affective reinforcement. Third, there was a significant interaction between post-binge NA slope assessed before treatment and treatment group predicting OBE frequency at EOT. As shown in Figure 3, for those who had higher NA post binge slope pre-treatment values (reflecting less NA affective reinforcement from binge eating), ICAT-BED was more effective than CBT-gsh; there were no differences between ICAT-BED and CBT-gsh for individuals with low pre-treatment NA affective reinforcement.
Figure 2.
Interaction of treatment group and change in positive affect (PA) area under the curve (AUC) predicting objective binge eating (OBE) at end of treatment (EOT). High and low values reflect 1 SD above and below sample means. OBE EOT is binge-eating frequency over the past four weeks controlling for baseline frequency.
Figure 3.
Interaction of treatment group and post-binge negative affect (NA) slope predicting objective binge eating (OBE) frequency at end of treatment (EOT). High and low values reflect 1 SD above and below sample means. OBE EOT is binge-eating frequency over the past four weeks controlling for baseline frequency.
Associations with Binge-eating Frequency at Follow-up
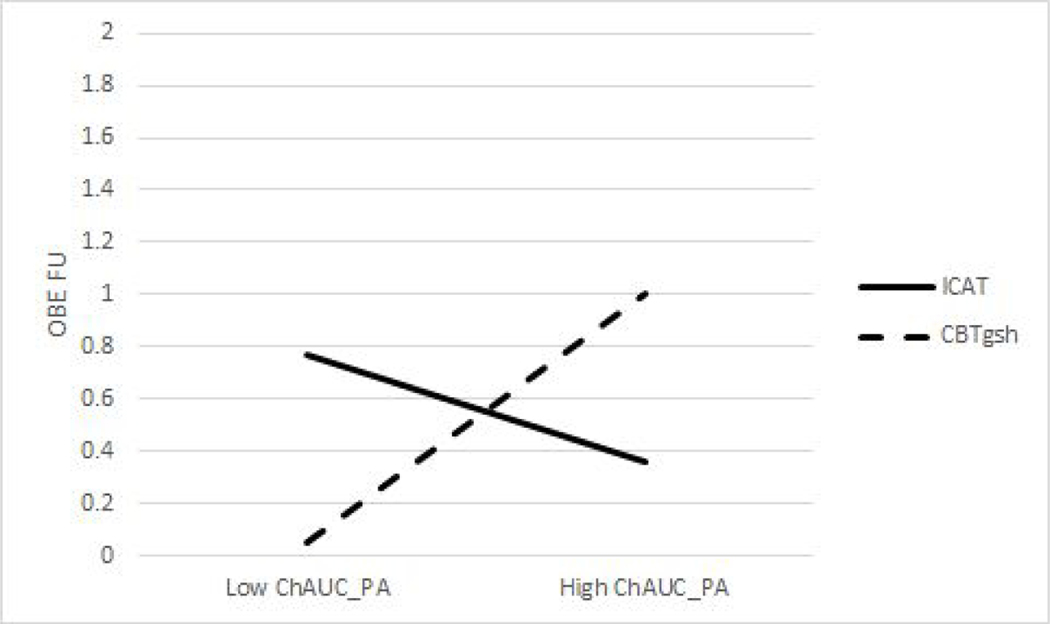
Table 2 displays the results of GLMs examining associations between pre-treatment assessed NA and PA AUC changes after binge-eating episodes and post-binge NA and PA slopes, measured prior to treatment, treatment group, and their interactions as predictors of binge-eating frequency at follow-up. There was a significant interaction between PA AUC and treatment type predicting OBE frequency at follow up. As shown in Figure 4, for those who had higher PA AUC pre-treatment values (reflecting more PA affective reinforcement from binge eating), ICAT-BED was associated with greater reductions in binge eating compared to CBTgsh. For those who had lower PA AUC pre-treatment values (reflecting less PA affective reinforcement from binge eating), CBTgsh was associated with greater reductions in binge eating compared to ICAT-BED.
Table 2.
Results of generalized linear models examining associations between affective response with binge-eating frequency at six-month follow-up
| AUC models | B | SE | Lower CI | Upper CI | Wald χ2 | p |
|---|---|---|---|---|---|---|
| Intercept | 0.47 | 1.06 | −1.61 | 2.55 | 0.19 | 0.661 |
| Gendera | −0.94 | 0.54 | −2.00 | 0.12 | 3.04 | 0.081 |
| Groupb | 1.15 | 0.40 | 0.36 | 1.93 | 8.15 | 0.004 |
| Baseline binge eating | 0.04 | 0.02 | −0.01 | 0.09 | 2.55 | 0.111 |
| BMI | 0.01 | 0.03 | −0.04 | 0.06 | 0.07 | 0.785 |
| Age | 0.00 | 0.01 | −0.03 | 0.02 | 0.04 | 0.835 |
| Δ NA AUC | −1.64 | 3.92 | −9.32 | 6.05 | 0.17 | 0.676 |
| Δ PA AUC | −1.28 | 1.12 | −3.47 | 0.91 | 1.31 | 0.252 |
| Group X ΔNA AUC | −31.11 | 16.08 | −62.63 | 0.42 | 3.74 | 0.053 |
| Group X ΔPA AUC | 9.10 | 3.99 | 1.28 | 16.93 | 5.20 | 0.023 |
| Slope models | ||||||
|
| ||||||
| Intercept | −0.59 | 1.02 | −2.58 | 1.41 | 0.33 | 0.566 |
| Gendera | −1.02 | 0.59 | −2.17 | 0.13 | 3.03 | 0.082 |
| Groupb | 1.32 | 0.45 | 0.43 | 2.21 | 8.49 | 0.004 |
| Baseline binge eating | 0.01 | 0.02 | −0.03 | 0.05 | 0.17 | 0.677 |
| BMI | 0.03 | 0.02 | −0.02 | 0.08 | 1.63 | 0.201 |
| Age | 0.01 | 0.01 | −0.01 | 0.03 | 0.58 | 0.446 |
| NA post -binge slope | −5.37 | 3.12 | −11.50 | 0.75 | 2.96 | 0.086 |
| PA post-binge slope | −1.09 | 1.69 | −4.39 | 2.22 | 0.41 | 0.520 |
| Group X NA post-binge slope | 5.20 | 3.80 | −2.24 | 12.64 | 1.88 | 0.171 |
| Group X PA post-binge slope | 1.49 | 2.35 | −3.11 | 6.08 | 0.40 | 0.527 |
Note.
Reference group was men;
Reference group was ICAT-BED
Figure 4.
Interaction of treatment group and change in positive affect (PA) area under the curve (AUC) predicting objective binge eating (OBE) at follow-up (FU). High and low values reflect 1 SD above and below sample means. OBE EOT is binge-eating frequency over the past four weeks controlling for baseline frequency.
Discussion
This study examined affective response to binge eating as a predictor of binge-eating treatment outcome in BED. According to the affect regulation model of binge eating, NA decreases and PA increases after binge eating are hypothesized to be important maintenance factors for binge eating. ICAT emphasizes the importance targeting momentary affect based on the affect regulation model. Therefore, it was hypothesized that individuals who showed a more rewarding affective response to binge eating (e.g., greater net reductions in NA and increases in PA) at baseline would have more reductions in binge eating at EOT and follow-up in ICAT-BED. Analyses provided some support for this hypothesis, particularly in PA AUC analyses.
PA AUC analyses showed that individuals who had greater net increases in PA in response to binge eating at baseline showed greater reductions in binge eating in ICAT-BED compared to CBTgsh at both EOT and follow-up. This finding underscores PA affective response as an important mechanism underlying treatment for BED and the need for emotion-focused interventions for these patients with BED. In the present study, it is plausible that individuals who experience significant affective reward related to binge eating are particularly able to utilize the functional analytic nature of ICAT-BED to better understand the promotion of positive emotional states associated with their binge eating and use skills to enhance positive emotional responding without binge eating.
NA affective response was only significant at EOT, and there were opposing findings for models examining AUC versus slope. AUC analyses indicated that individuals who reported less total NA improvement from binge eating at baseline experienced better treatment response in CBT-gsh. In contrast, slope analyses indicated that individuals who reported less rapid NA improvement following binge eating experienced better treatment response in ICAT-BED. One possible explanation is that less negative affect improvement in terms of higher AUC could also reflect net increases in NA from a statistical standpoint (which occurred in approximately 29% of binge-eating episodes at baseline). That is, people who find binge eating more distressing, rather than reinforcing, may do better in ICAT-BED, possibly because emotion regulation skills may help individuals cope with distress that is exacerbated via binge eating. Nevertheless, these opposing findings underscore the importance of distinction between slope as the rate of change in affect over time (regardless of where people were prior to the binge) versus AUC as the total net change (between pre and post binge). Future studies should therefore consider the timing of reinforcing effects from binge eating, as immediate relief from aversive affective states following binge eating may have a different effect on future behavior compared to potentially larger, more gradual changes following binge eating.
Strengths of the study included the use of EMA within an intervention study, an approach that has seldom been used in eating disorders research; examination of theoretically-relevant predictor variables of BED treatment outcomes; and the use of standardized treatment and assessment protocols. Despite these strengths, several limitations are worth noting. This study examined affective response using general NA, although, studies have shown that guilt may be an important facet of NA worth exploring (Berg et al., 2015). Further, this treatment-seeking sample consisted primarily of Caucasian women with overweight/obesity. As such, findings may not generalize to other demographic groups with BED. Also, all participants did not have adequate data for analysis which limited the sample size.
This study highlights the predictive utility of EMA-measured affective response at baseline as a moderator of outcomes of psychological treatment. Because affective response to binge eating appears to be an important predictor of changes in binge-eating frequency in BED, novel therapeutic approaches addressing momentary affective responses to binge eating should continue to be developed. Results of this investigation indicate that individuals who receive more total PA improvement from binge eating may be more responsive to ICAT-BED whereas individuals with low total NA or PA improvement from binge eating may be more responsive to CBTgsh. Neither treatment was uniquely effective for individuals with higher total NA reinforcement from binge eating. Further, total affective change appears to be more important compared to slope in predicting treatment outcome, particularly for PA.
Supplementary Material
Acknowledgments
This research was supported by grants R34MH099040 and R34MH098995 from the National Institute of Mental Health.
Role of Authors: C.B.P. and S.A.W. received grant funding. Testing and data collection were performed by C.B.P, S.A.W., R.D.C., and S.G.E. K.E.S. performed the data analysis and interpretation. T.B.M. and K.E.S. drafted the paper. All authors provided critical revisions and approved the final version of the paper.
References
- Alonso-Alonso M, Woods SC, Pelchat M, Grigson PS, Stice E, Farooqi S, ... & Beauchamp GK (2015). Food reward system: current perspectives and future research needs. Nutrition Reviews, 73, 296–307. 10.1093/nutrit/nuv002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Berg KC, Cao L, Crosby RD, Engel SG, Peterson CB, Crow SJ, ... & Wonderlich SA (2017). Negative affect and binge eating: Reconciling differences between two analytic approaches in ecological momentary assessment research. International Journal of Eating Disorders, 50, 1222–1230. 10.1002/eat.22770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, & Peterson CB (2015). Negative affect prior to and following overeating‐only, loss of control eating‐only, and binge eating episodes in obese adults. International Journal of Eating Disorders, 48, 641–653. 10.1002/eat.22401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger K, & Stice E (2011). Variability in reward responsivity and obesity: Evidence from brain imaging studies. Current Drug Abuse Reviews, 4, 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawe S, & Loxton NJ (2004). The role of impulsivity in the development of substance use and eating disorders. Neuroscience & Biobehavioral Reviews, 28, 343–351. 10.1016/j.neubiorev.2004.03.007 [DOI] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Wonderlich SA, Crosby RD, Engel SG, Mitchell JE, ... & Le Grange D (2013). Moderators of post-binge eating negative emotion in eating disorders. Journal of Psychiatric Research, 47, 323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders. Guilford Press. [Google Scholar]
- Fairburn CG, Cooper Z, & O’Connor M (2008). The eating disorder examination. In Fairburn CG, Cognitive behavioral therapy and eating disorders. Guilford Press, New York. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1995). Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). New York, New York State Psychiatric Institute. Biometrics Research. [Google Scholar]
- Grilo CM (2017). Psychological and behavioral treatments for binge-eating disorder. The Journal of Clinical Psychiatry, 78, 20–24. doi: 10.4088/JCP.sh16003su1c.04 [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, & Keel PK (2011). Revisiting the affect regulation model of binge eating: A meta-analysis of studies using ecological momentary assessment. Psychological Bulletin, 137, 660–681. 10.1037/a0023660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenford SL, Smith SS, Wetter DW, Jorenby DE, Fiore MC, & Baker TB (2002). Predicting relapse back to smoking: Contrasting affective and physical models of dependence. Journal of Consulting and Clinical Psychology, 70, 216–227. 10.1037/0022-006X.70.1.216 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, ... & Bruffaerts R (2013). The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological Psychiatry, 73, 904–914. 10.1016/j.biopsych.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Y, Solomon O, & Dunton GF (2017). Does the Company of a Dog Influence Affective Response to Exercise? Using Ecological Momentary Assessment to Study Dog-Accompanied Physical Activity. American Journal of Health Promotion, 31, 388–390. 10.1177/0890117116666947 [DOI] [PubMed] [Google Scholar]
- Linardon J (2018). Rates of abstinence following psychological or behavioral treatments for binge‐eating disorder: Meta‐analysis. International Journal of Eating Disorders, 51, 785–797. 10.1002/eat.22897 [DOI] [PubMed] [Google Scholar]
- Peterson CB, Engel SG, Crosby RD, Strauman T, Smith TL, Klein M, Mitchell JE, Crow SJ, & Wonderlich SA (2020). Integrative Cognitive-Affective Therapy (ICAT) compared to guided self-help cognitive-behavioral therapy (CBTgsh) for the treatment of binge-eating disorder: A randomized clinical trial. International Journal of Eating Disorders. Advanced online publication. 10.1002/eat.23324 [DOI] [Google Scholar]
- Rhodes RE, & Kates A (2015). Can the affective response to exercise predict future motives and physical activity behavior? A systematic review of published evidence. Annals of Behavioral Medicine, 49, 715–731. 10.1007/s12160-015-9704-5 [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. [DOI] [PubMed] [Google Scholar]
- Williams DM, Dunsiger S, Ciccolo JT, Lewis BA, Albrecht AE, & Marcus BH (2008). Acute affective response to a moderate-intensity exercise stimulus predicts physical activity participation 6 and 12 months later. Psychology of Sport and Exercise, 9, 231–245. 10.1016/j.psychsport.2007.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.