This review summarizes evidence that self-limited delayed puberty, largely considered to be benign, may in fact have both detrimental and protective effects on adult health.
Abstract
Delayed puberty is a common condition defined as the lack of sexual maturation by an age ≥2 SD above the population mean. In the absence of an identified underlying cause, the condition is usually self-limited. Although self-limited delayed puberty is largely believed to be a benign developmental variant with no long-term consequences, several studies have suggested that delayed puberty may in fact have both harmful and protective effects on various adult health outcomes. In particular, height and bone mineral density have been shown to be compromised in some studies of adults with a history of delayed puberty. Delayed puberty may also negatively affect adult psychosocial functioning and educational achievement, and individuals with a history of delayed puberty carry a higher risk for metabolic and cardiovascular disorders. In contrast, a history of delayed puberty appears to be protective for breast and endometrial cancer in women and for testicular cancer in men. Most studies on adult outcomes of self-limited delayed puberty have been in small series with significant variability in outcome measures and study criteria. In this article, we review potential medical and psychosocial issues for adults with a history of self-limited delayed puberty, discuss potential mechanisms underlying these issues, and identify gaps in knowledge and directions for future research.
Delayed puberty is commonly defined as the absence of physical signs of puberty by an age ≥2 SD beyond the population mean for pubertal entry, a statistical definition necessitated by our incomplete understanding of how the timing of puberty is determined.1 For girls, delayed puberty is commonly defined as the absence of breast development by age 13 years and for boys as the absence of testicular enlargement by age 14 years. Of note, these clinical conventions do not reflect variation in pubertal timing between racial and ethnic groups or a recent trend toward earlier pubertal timing that has been observed in the United States and other developed countries.2–13
In the absence of any identifiable cause, delayed puberty usually resolves by age 18 years, and in this review, this condition is referred to as “self-limited delayed puberty.” This condition is also called constitutional delay of puberty, development, or maturation, with the word “growth” also frequently included (eg, constitutional delay of growth and puberty [CDGP]).
Self-limited delayed puberty is considered by many to be a benign developmental variant with no long-term consequences.14,15 Thus, the mainstay of treatment is an observational, “watchful waiting” approach with reassurance for the patient and family. However, some reports have suggested that the condition can have lasting physical and psychological effects, which raises the question whether sex-steroid therapy should be initiated by a certain age in all individuals with self-limited delayed puberty to prevent or temper any of these effects. These studies were conducted predominantly in Caucasian populations and used traditional cutoffs for delayed puberty and may thus be limited in their generalizability; nonetheless, they provide insight into the potential consequences of self-limited delayed puberty. In this review, we examine consequences of self-limited pubertal delay on height, bone mineral density (BMD), psychosocial functioning, and educational achievement, as well as associations between delayed puberty and the risks for adult cancers and cardiovascular disorders.
Methods
The PubMed database was searched using the following medical subject heading terms and keywords: delayed puberty, adult height, BMD, fracture, depression, substance use, self-esteem, educational achievement, breast cancer, endometrial cancer, testicular cancer, prostate cancer, cardiovascular disease, myocardial infarction, peripheral arterial disease, stroke, hypertension, and metabolic syndrome. All relevant articles published from 2006 to 2016 were included in the review. Articles published before 2006 were included if they provided key background information, demonstrated a new or significant finding in the field, and/or summarized previous findings in a review and/or meta-analyses. References of selected articles were reviewed for additional articles not identified on the initial search.
Height
Puberty is marked by a period of rapid skeletal growth, the pubertal growth spurt.16 Because this growth acceleration is delayed in individuals with self-limited delayed puberty, these individuals are typically shorter during the teenage years than peers with normal pubertal timing.17,18 Further compounding the short stature during early adolescence is the fact that, in addition to having a delayed pubertal growth spurt, individuals with self-limited delayed puberty often have a slow growth velocity before puberty.19 When these individuals do eventually undergo a pubertal growth spurt, the conventional teaching is that this growth spurt, albeit delayed, allows them to “catch up” and attain their full genetic height potential.20
Conflicting Observations
Consistent with this teaching, several observational studies report that children with self-limited delayed puberty eventually achieve their genetic height potential, with no significant difference between measured adult height and predicted adult height (ie, midparental target height) (Tables 1 and 2).21–25 However, other studies suggest that these individuals fall short of their target height by 0.6 to 1.5 SD, ∼4 to 11 cm (Tables 1 and 2).26–32 These disparate findings may be due to variation in study populations due to ascertainment criteria, inclusion criteria (which sometimes include growth delay), and/or use of sex-steroid treatment. Thus, these findings have prompted attempts to identify features that may predict which individuals will fail to meet their genetic height potential.
TABLE 1.
Final Adult Height and Target Height in Boys with Self-Limited Delayed Puberty
| Study (Reference) | Year | Subgroup | N | FH (SD or cm) | TH (SD or cm) | Difference |
|---|---|---|---|---|---|---|
| Bramswig et al26 | 1990 | — | 37 | −0.7 | — | — |
| Crowne et al27 | 1990 | — | 43 | −1.6 | −0.6 | −1.0 SD |
| LaFranchi et al29 | 1991 | — | 29 | 169.5 | 174.6 | −5.1 cm |
| von Kalckreuth et al22 | 1991 | — | 14 | 171.3 | 173.9 | −2.6 cm |
| Albanese and Stanhope30 | 1993 | — | 98 | −1.9 | −0.5 | −1.4 SD |
| Albanese and Stanhope31 | 1995 | — | 78 | −2.0 | −0.5 | −1.5 SD |
| Sperlich et al32 | 1995 | — | −1 | −0.4 | −0.6 SD | |
| Arrigo et al23 | 1996 | Untreated | 27 | −0.9 | −0.7 | −0.2 SD |
| Testosterone treated | 22 | −0.6 | −0.8 | 0.2 SD | ||
| Bertelloni et al24 | 1998 | Untreated | 7 | −0.7 | −0.4 | −0.3 SD |
| Testosterone treated | 6 | −0.6 | −0.7 | 0.1 SD | ||
| Oxandrolone treated | 8 | −0.7 | −0.7 | 0 SD | ||
| Rensonnet et al25 | 1999 | Untreated | 28 | −0.76 | −0.56 | −0.2 SD |
| Testosterone treated | 11 | −0.29 | −0.35 | 0.06 SD | ||
| Kelly et al33 | 2003 | — | 64 | 168.9 | 170.4 | −1.5 cm |
| — | 168.2 | 171.1 | −2.9 cm | |||
| Butenandt et al34 | 2005 | — | 12 | 1.9 | 1.2 | 0.7 SD |
| Poyrazoglu et al35 | 2005 | — | 105 | −1.8 | −0.9 | −0.9 SD |
| Wehkalampi et al36 | 2007 | Early reduction in height | 18 | −0.65 | −0.02 | −0.63 SD |
| No early reduction in height | 22 | 0.3 | 0.25 | 0.05 SD | ||
| Cools et al37 | 2008 | — | 33 | −0.2 | −0.3 | 0.1 SD |
| Zucchini et al38 | 2008 | Untreated | 17 | −1.02 | −1.12 | 0.1 SD |
| GH treated | 25 | −0.92 | −1.26 | 0.34 SD | ||
| Testosterone treated | 12 | −1.39 | −1.45 | 0.06 SD |
FH, final height; GH, growth hormone; TH, target height; — , not available.
TABLE 2.
Final Adult Height and Target Height in Girls With Self-Limited Delayed Puberty
| Study (Reference) | Year | Subgroup | N | FH (SDS or cm) | TH (SDS or cm) | Difference |
|---|---|---|---|---|---|---|
| Bramswig et al26 | 1990 | — | 32 | −0.7 | — | — |
| von Kalckreuth et al22 | 1991 | — | 6 | 155.9 | 155.7 | 0.2 cm |
| Crowne et al28 | 1991 | — | 15 | −1.5 | −0.8 | −0.7 SD |
| LaFranchi et al29 | 1991 | — | 13 | 156.4 | 161.7 | −5.3 cm |
| Albanese and Stanhope30 | 1993 | — | 34 | −2.3 | −0.8 | −1.5 SD |
| Butenandt et al34 | 2005 | — | 21 | 2.1 | 1.5 | 0.6 SD |
| Poyrazoglu et al35 | 2005 | — | 46 | −1.34 | −1 | −0.34 SD |
| Zucchini et al38 | 2008 | Untreated | 16 | −0.78 | −0.88 | 0.1 SD |
| GH treated | 7 | −0.92 | −0.43 | −0.49 SD | ||
| Wehkalampi et al39 | 2011 | Untreated | 32 | 0.1 | 0.3 | −0.2 SD |
| Estrogen treated | 7 | −0.6 | −0.1 | −0.5 SD |
FH, final height; GH, growth hormone; TH, target height; — , not available.
Role of Familial Short Stature
One factor that appears to influence whether target height is ultimately attained in self-limited delayed puberty is the target height itself. Delayed puberty is often (although not always) seen in the context of familial short stature, which can exacerbate concerns regarding short stature.1 Individuals with self-limited delayed puberty with at least 1 tall parent (defined as height greater than the 90th percentile)34 or with a target height that is not short (defined as target height less than –1.5 SDs)37 were found to reach or exceed their target height (Tables 1 and 2). These studies suggest that individuals with familial short stature in combination with self-limited delayed puberty are particularly likely to fall short of their target height.
Correlations With Prepubertal Growth
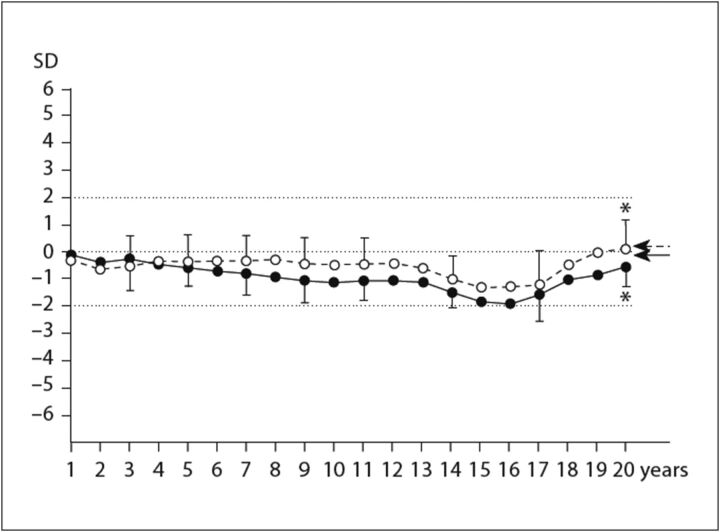
Another factor that has been suggested to play a role in determining adult height in individuals with self-limited delayed puberty is the rate of growth during the childhood years before puberty, with a slow rate of prepubertal growth associated with failure to attain target height in both boys and girls with an otherwise unremarkable medical evaluation.36,39 In boys, such individuals had adult heights 0.63 SD (∼4 cm) less than predicted, whereas those with normal rates of prepubertal growth had no such height deficits (Fig 1). Height gain during the pubertal growth spurt was comparable between the 2 groups, and thus the growth during puberty did not compensate for the prepubertal growth deficit in individuals with slow prepubertal growth (Table 1).36 In both boys and girls, individuals with slower growth rates in childhood also had shorter parents, which support previous conclusions that familial short stature may limit individuals from reaching their target height and suggests a possible genetic component to the slow growth rate.34,37
FIGURE 1.
Mean SD score for height and mean target height (arrows) of boys with delayed puberty who either had (filled circles and solid line) or did not have (open circles and dashed line) an early reduction in height. *P = .01 between final adult heights. (Reprinted with permission from page 102 of Wehkalampi K, Vangonen K, Laine T, Dunkel L. Progressive reduction of relative height in childhood predicts adult stature below target height in boys with constitutional delay of growth and puberty. Horm Res. 2007;68(2):99–104.)
Effects of Sex-Steroid Therapy
Sex-steroid therapy (eg, testosterone in boys, estradiol in girls) can be offered to ameliorate psychosocial distress related to delayed puberty.1 Several observational studies and 2 randomized trials have examined the effects of sex-steroid therapy on height in boys with self-limited delayed puberty.40,41 These studies have reported no difference in adult height between those treated with sex steroids and those who underwent observation alone (Tables 1 and 2).23–25,33,35,36,38,39 Thus, although there may be other beneficial effects, treatment with sex steroids does not appear to enhance or reduce adult height.
Summary
Some individuals with self-limited delayed puberty, particularly those with familial short stature and slower prepubertal growth, fail to attain their genetic target height. Sex-steroid therapy after the age of 14 years in boys and 12 years in girls does not appear to enhance or reduce adult height. However, if started too early (some suggest bone age <10 years), such therapy may lead to premature closure of the growth plates and loss of adult height.
BMD and Fracture Risk
Most bone mass is acquired during puberty. Peak bone mass is attained at the end of skeletal growth in the mid-20s and is an important predictor of the development of osteoporosis later in life.42 In 2001, the National Institutes of Health Consensus on Osteoporosis Prevention, Diagnosis, and Therapy emphasized the need to better understand how pubertal delay affects bone mass and to develop strategies to maximize peak bone mass.43
BMD in Men
In 1992, Finkelstein et al reported that men with a history of self-limited delayed puberty had lower areal BMD measured by dual x-ray absorptiometry (DXA) than men with normal timing of puberty (Table 3).44,45 Two additional studies, Kindblom et al and Kuh et al, have similarly reported that men with later puberty have lower volumetric BMD as directly measured by peripheral quantitative computed tomography (Table 3).46,47 However, 2 other studies, by Bertelloni et al and Yap et al, found no significant difference in volumetric BMD (derived from areal DXA measurements) between men with a history of self-limited delayed puberty and controls (Table 3).24,48
TABLE 3.
BMD in Men With a History of Self-Limited Delayed Puberty
| Study (Ref) | Year | Delayed Puberty Criteria | Subgroup | N | Age at Evaluation, Years ± SD | Outcome Variable | Conclusion | ||
|---|---|---|---|---|---|---|---|---|---|
| Location | aBMD, g/cm2 | vBMD, g/cm3 | |||||||
| Finkelstein et al44 | 1992 | Puberty onset >15 y as defined by pubic hair stage and height | DP | 23 | 26 ± 2 | Radius | 0.73 | 0.5 | aBMD and vBMD lower in DP vs normal controls at both sites, all Ps < .009 |
| LS | 1.03 | 0.13 | |||||||
| Controls | 21 | 24 ± 3 | Radius | 0.8 | 0.54 | ||||
| LS | 1.13 | 0.14 | |||||||
| Bertonelloni et al24 | 1998 | Testicular vol 4 mL achieved at ≥14 y | DP | 21 | 21.8 ± 1.7 | LS | 1.101 | 0.327 | aBMD lower in DP vs normal controls, P < .009; no difference in vBMD, P = NS |
| Controls | 12 | 19.3 ± 1.3 | LS | 1.222 | 0.337 | ||||
| Yap et al48 | 2004 | Testicular vol 4 mL achieved at ≥14 y | DP | 32 | 24.7 ± 3.4 | Total body | 1.184 | — | Total body aBMD lower in DP vs controls, P = .016; LS aBMD lower in DP vs controls, P = .044, no difference in LS vBMD, P = NS; no difference in FN aBMD or vBMD |
| LS | 1.2 | 0.37 | |||||||
| FN | 1.1 | 0.67 | |||||||
| Controls | 45 | 23.5 ± 2.9 | Total body | 1.237 | — | ||||
| LS | 1.28 | 0.37 | |||||||
| FN | 1.16 | 0.67 | |||||||
| Kindbloom et al46 | 2006 | PHV in the latest tertile | Late-tertile PHV | 214 | 18.9 ± 0.5 | Total body | 1.23 | — | Total body aBMD lower in late PHV versus average PHV, P = .001; no difference in LS or FN aBMD; radius aBMD and vBMD lower in late PHV versus average PHV, P all <0.001; tibia vBMD lower in DP versus controls, P all < 0.001 |
| LS | 1.21 | — | |||||||
| FN | 1.14 | — | |||||||
| Radius | 0.56 | Cort: 1.155; Trab: 0.209 | |||||||
| Tibia | Cort: 4.36; Trab: 0.254 | ||||||||
| Middle-tertile PHV | 214 | 18.9 ± 0.5 | Total body | 1.25 | — | ||||
| LS | 1.24 | — | |||||||
| FN | 1.18 | — | |||||||
| Radius | 0.58 | Cort: 1.165; Trab: 0.221 | |||||||
| Tibia | — | Cort: 4.44; Trab: 0.267 | |||||||
| Kuh et al47 | 2016 | Lack of or limited genital development, voice breaking, and pubic hair growth | Preadolescent at 14.5 y | 65 | 60–64 | Radius | — | Cort: 1.162; Trab: 0.197 | Trab vBMD lower in "preadolescent" by 9% vs "fully mature," 95% CI 14% to –4%; P = .001 |
| LS | 1.01 | — | |||||||
| Total hip | 0.97 | — | |||||||
| Early puberty at 14.5 y | 222 | 60–64 | Radius | — | Cort: 1.161; Trab: 0.201 | ||||
| LS | 1.05 | — | |||||||
| Total hip | 0.99 | — | |||||||
| Advanced puberty at 14.5 y | 200 | 60–64 | Radius | — | Cort: 1.159; Trab: 0.205 | ||||
| LS | 1.04 | — | |||||||
| Total hip | 1.00 | — | |||||||
| Fully mature at 14.5 y | 168 | 60–64 | Radius | — | Cort: 1.153; Trab: 0.216 | ||||
| LS | 1.08 | — | |||||||
| Total hip | 1.02 | — | |||||||
aBMD, areal bone marrow density; CI, confidence interval; Cort, cortical; DP, delayed puberty; FN, femoral neck; LS, lumbar spine; NS, not significant; PHV, peak height velocity; Trab, trabecular; vBMD, volumetric bone marrow density; —, not available.
One potential explanation for the variability in findings is that the studies used different definitions of pubertal delay with varying cutoff ages (14 vs 15 years) and ages at follow-up (mean of 19–64 years; Table 3). In addition, only 2 studies (Kindblom et al and Kuh et al) measured volumetric BMD directly46,47; the other studies reported estimated volumetric BMD as calculated from DXA, and concerns have been raised that such calculations may underestimate BMD in smaller individuals even after corrections for body size.49–51 Future studies to resolve these questions may require direct measurements in later adulthood of volumetric BMD.
BMD in Women
Many early studies have associated late menarche, a proxy of delayed puberty, with lower BMD.52–58 However, most of these studies did not explicitly exclude women who had underlying causes of late menarche such as hypothalamic amenorrhea (a functional form of gonadotropin-releasing hormone deficiency triggered by physical, environmental, and/or psychosocial stressors), which is known to be associated with reduced bone density.42 One prospective, longitudinal study of 124 healthy women that specifically excluded women with risk factors for hypothalamic amenorrhea reported that subjects with menarche occurring later than the median age for the cohort (12.94 years) had lower BMD at the femoral neck and tibia compared with those with menarche occurring before the median age for the cohort (Table 4), with the negative correlation between menarchal timing and BMD observed across all ages from 8 to 18 years.59,60 Extending to later adulthood, several observational studies have demonstrated that the age at menarche may influence the risk of osteoporosis during both the premenopausal52,54,55,61 and postmenopausal years.53,55,56,58,61
TABLE 4.
BMD in Women With a History of Self-Limited Delayed Puberty
| Study (Reference) | Year | N | Subgroup | Age at Evaluation, Years ± SD | Outcome Variable | Conclusion | ||
|---|---|---|---|---|---|---|---|---|
| Location | aBMD, g/cm2 | vBMD, g/cm3 | ||||||
| Fox et al53 | 1993 | 2230 | 71 ± 4.8 | |||||
| Late menarche (no criteria provided) | Radius | 0.36 | Each year increment in age at menarche, postmenopausal BMD decreased by 0.9% (P = .02) | |||||
| Early menarche (no criteria provided) | Radius | 0.371 | ||||||
| Tuppurainen et al55 | 1995 | 53.4 ± 2.9 | ||||||
| 223 | Late menarche (>15 y) | LS | 1.077 | LS and FN aBMD lower in late menarche vs early menarche group, all Ps <.05 | ||||
| FN | 0.896 | |||||||
| 1382 | Early menarche (<15 y) | LS | 1.105 | |||||
| FN | 0.919 | |||||||
| Chevalley et al62 | 2009 | 62 | Later pubertal timing (menarche >12.94 y) | 8.9 ± 0.5 | Total body | 0.599 | aBMD lower in later vs earlier pubertal timing group at all sites, all Ps <.02 | |
| Radius | 0.445 | |||||||
| FN | 0.636 | |||||||
| LS | 0.630 | |||||||
| 20.4 ± 0.6 | Total body | 0.900 | ||||||
| Radius | 0.701 | |||||||
| FN | 0.838 | |||||||
| LS | 1.026 | |||||||
| 62 | Earlier pubertal timing (menarche <12.94 y) | 9.0 ± 0.5 | Total body | 0.620 | ||||
| Radius | 0.456 | |||||||
| FN | 0.658 | |||||||
| LS | 0.651 | |||||||
| 20.4 ± 0.6 | Total body | 0.927 | ||||||
| Radius | 0.719 | |||||||
| FN | 0.878 | |||||||
| LS | 1.060 | |||||||
| Chevalley et al60 | 2009 | 62 | Later pubertal timing (menarche >12.94 y) | 20.4 ± 0.6 | FN | 0.838 | FN and tibia aBMD and vBMD lower in later vs earlier pubertal timing group in both young adult and premenopausal women, all Ps <.004 | |
| Tibia | 0.314 | |||||||
| 60 | 46.0 ± 3.7 | FN | 0.785 | |||||
| Tibia | 0.295 | |||||||
| 62 | Earlier pubertal timing (menarche <12.94 y) | 20.4 ± 0.6 | FN | 0.878 | ||||
| Tibia | 0.334 | |||||||
| 60 | 45.6 ± 3.1 | FN | 0.825 | |||||
| Tibia | 0.322 | |||||||
aBMD, areal bone marrow density; DP, delayed puberty; FN, femoral neck; LS, lumbar spine; NS, not significant; vBMD, volumetric bone marrow density.
The effect of pubertal timing on BMD in women has been largely attributed to differences in estrogen exposure. Specifically, both a later age at menarche and earlier age at menopause have been associated with lower BMD, suggesting that a greater lifetime duration of estrogen exposure may have a protective effect on BMD.42 However, in 1 prospective study, differences in BMD were observed even before the onset of puberty, with a lower areal BMD observed as early as 9 years of age in subjects who went on to have menarche later than the median age (Table 4).62 These observations suggest that factors other than estrogen exposure may influence BMD, possibly genetic and environmental factors that affect both pubertal timing and bone mass.62
Although these studies in women suggest that menarche occurring later but still within the normal age range may be associated with lower BMD during both young and later adulthood, only 1 study specifically reported BMD in women with frankly delayed puberty. In this study of postmenopausal women, late menarche (>15 years) was associated with reduced BMD at the lumbar spine and femoral neck when compared with BMD of women who underwent menarche before age 15 years (Table 4). However, it is still unclear from the preceding studies whether the finding of a lower BMD in women with later menarche is due to a protective effect of earlier menarche or a detrimental effect of later menarche. Future studies on BMD specifically in women with frankly delayed puberty in comparison with those with normal pubertal timing are needed to resolve this question.
Fracture Risk
In young adult men, Kindblom et al found that each 1-year increase in age of puberty was associated with a 39% increase in odds of upper extremity fractures during adolescence (Table 5).46 A similar association was reported in a longitudinal study of young women; individuals who experienced a fracture in childhood or adolescence had significantly later age of menarche and lower volumetric BMD at the distal radius than those who did not experience a fracture despite similar nutritional intake and physical activity level in the 2 groups (Table 5).63 However, the risk associated with frankly delayed puberty was not reported.
TABLE 5.
Fracture Risk in Individuals With Delayed Puberty
| Study (Reference) | Year | Name | N | Age at Evaluation, Years ± SD | Outcome Variable | Conclusion |
|---|---|---|---|---|---|---|
| Johnell et al64 | 1995 | MEDOS | 2086 women | 78.1 ± 9.4 | Hip fracture | RR: 1.45, 95% CI: 1.12 to 1.87 for age at menarche ≥15 y vs ≤11 y |
| Roy et al65 | 2003 | EPOS | 3173 men, 3402 women | 63.1 ± 7.8 (men), 62.2 ± 7.6 (women) | Vertebral fracture | RR: 1.8, 95% CI: 1.24 to 2.63 for age at menarche ≥16 y vs <16 y |
| Silman et al66 | 2003 | EPOS | 3173 men, 3402 women | 63.1 ± 7.8 (men), 62.2 ± 7.6 (women) | Colles’ fracture | RR: 1.5, 95% CI: 1.1 to 2.0 for age at menarche >15 y vs ≤15 y |
| Kindblom et al46 | 2006 | GOOD | 642 men | 18.9 ± 0.6 | Upper extremity fracture | OR: 1.39, 95% CI: 1.08 to 1.79, P = .01 for each 1-y increment to PHV |
| Chevalley et al63 | 2012 | 42 women | 20.4 ± 0.6 | Fracture | OR: 2.09, 95% CI: ∼1.3 to 3.3, P = .002 for each 1.2-y delay in menarche; mean age at menarche greater for fracture group vs no fracture group (13.45 vs 12.78, P = .003) |
CI, confidence interval; EPOS, European Prospective Osteoporosis Study; GOOD, Gothenburg Osteoporosis and Obesity Determinants; MEDOS, Mediterranean Osteoporosis Study; OR, odds ratio; RR, relative risk; PHV, peak height velocity.
One study did identify women who had frankly delayed menarche (at 16 years or later) and found that these women had an 80% increased risk of incident vertebral fracture in later adulthood compared with those with menarche before 16 years.65 Similarly, those with menarche at 15 years or later had a 50% increased risk of Colles fracture compared with those with menarche before 15 years (Table 5).66 Another study showed a 45% increase in the risk of hip fracture in those with menarche at age 15 years or later compared with those with menarche at 11 years or younger (Table 5).64 In contrast, at the other end of reproductive life, the age at menopause was not significantly associated with Colles or vertebral fracture65,66 and had a smaller effect than age at menarche on the risk of hip fracture,64 suggesting that lifetime duration of estrogen exposure is not the only factor that influences fracture risk. To date, associations between pubertal timing and fracture risk in men have not been reported, possibly due to a relatively lower fracture incidence in men and difficulty with assessing age at pubertal initiation.65,66
Sex-Steroid Therapy
One intervention that may temper any reduction in BMD in individuals with self-limited delayed puberty is sex-steroid therapy. However, Yap et al and Bertelloni et al both found that androgen treatment of 6 to 28 months did not significantly affect BMD in young adult men with a history of delayed puberty.24,48 The influence of sex-steroid therapy on BMD in women has not been reported.
Summary
Studies in men with a history of self-limited delayed puberty variably report low or normal BMD, and previous androgen therapy does not appear to influence BMD in these men. In women, later age at menarche is associated with decreased BMD in early adulthood, late adulthood, and even before pubertal onset. Later age at pubertal initiation has also been associated with an increase in fracture risk during adolescence for both boys and girls and during adulthood for women.
Psychosocial Outcomes
In addition to being a period of dramatic physical development, adolescence is also a time of marked psychosocial changes. Studies have examined the effect of pubertal timing on multiple psychosocial aspects, including self-esteem, psychopathology, and behavior, with a predominant focus on the adolescent period and with limited follow-up into adulthood.
Self-Esteem
Two studies from the 1950s suggested that boys and girls who mature later than their peers have more negative beliefs and attitudes toward self at age 17,67,68 although a subsequent study suggested that it is short stature rather than delayed puberty itself that affected self-image.69 However, 2 studies in boys and girls with CDGP found no significant difference in self-esteem scores in early adulthood between those with CDGP and those with normal development despite moderately shorter stature (–1.6 and –1.5 SD, respectively). Race and ethnicity may modulate the effect of pubertal timing, as 1 study of adolescents with self-perceived late puberty found a significant decrease in body image with late development in Hispanic and black boys, but not in white or Asian boys. For girls with late development, lower body-image scores were observed in Hispanic girls only.70
Psychopathology and Behavior
Many studies have associated early pubertal timing with adverse psychosocial outcomes including depression, delinquency, and early sexual behavior.71–75 Fewer studies have examined psychosocial outcomes for men and women who experienced later pubertal timing (summarized in Table 6). One study of a large UK birth cohort observed that girls with menarche ≥13.5 years had up to a 52% reduction in odds of experiencing depressive symptoms in adolescence compared with girls with normal menarche, but this association disappeared by young adulthood.76 Similarly, a study in New Zealand did not find any association between menarche at ages 14 to 15 and major depression during adolescence.77 In contrast, a study in Finland identified a 70% higher risk of depression in women who had delayed puberty (menarche ≥16 years),78 but in a recent meta-analysis of both the New Zealand and Finland studies, this association was no longer seen.79 Further supporting the overall results of the meta-analysis, 2 recent studies, the Growing Up Today Study, a follow-up of the Nurses’ Health Study II, and the UK Biobank Study found that later menarche (>14.3 and >15 years) was not associated with depressive symptoms in young and later adulthood, respectively.80,81
TABLE 6.
Psychopathology in Individuals With Delayed Puberty
| Study (Reference) | Year | Location/Name | N | Age at Evaluation, Years ± SD or Range | Outcome Variable | Conclusion |
|---|---|---|---|---|---|---|
| Joinson et al76 | 2013 | United Kingdom | 3648 women | 14–16.5 | Depressive symptoms | OR up to 1.52, 95% CI: 1.12 to 2.05 for age at menarche 11.5 to 13.5 y vs ≥13.5 y, P = .007 |
| 18–19 | No difference in OR for age at menarche 11.5 to 13.5 y vs ≥13.5 (OR 1.07–1.18, all Ps >.05) | |||||
| Boden et al77 | 2011 | New Zealand | 497 women | 15–18 | Major depression | No difference in % outcome for age at menarche 14–15 y vs 12–13 y (32.5% vs 30.9%, P > .50) |
| Herva et al78 | 2004 | Northern Finland | 3952 women | 31 | Depression | OR 1.7, 95% CI: 1.1 to 1.6 for age at menarche ≥16 y vs 12–15 y |
| Galvao et al79 | 2014 | Meta-analysis: New Zealand and Northern Finland | 4449 women | 15–31 | Major depression/ depression | No significant risk of depression for age at menarche ≥14 y vs <14 y (RR 1.28, 95% CI: 0.87 to 1.88) |
| Opoliner et al80 | 2014 | United States/ Growing Up Today Study | 9039 women | 20–26 | Depressive symptoms | No difference in OR for age at menarche >14.3 y vs 12–14.3 y (OR 0.91, 95% CI: 0.70 to 1.18) |
| Day et al81 | 2015 | United Kingdom/UK Biobank Study | 250 037 women | 40–69 | Depression | No difference in OR for age at menarche 15–19 y vs 12–14 y (OR 1.07, 95% CI: 1.02 to 1.13, P > 7.48 × 10–5) |
| Conley and Rudolph82 | 2009 | United States | 82 men | 13.4 | Depression | Later perceived pubertal timing was associated higher levels of depression (β = −0.31, P < .05) |
| Graber et al83 | 2004 | United States | 392 men | 24.2 | Disruptive behavior disorder | OR 2.1, 95% CI: 1.1 to 4.5 for perceived late pubertal timing vs on time |
| Substance use | OR 2.5, 95% CI: 1.1 to 5.9 for perceived late pubertal timing vs on time | |||||
| Day et al81 | 2015 | United Kingdom/UK Biobank Study | 197 714 men | 40–69 | Anxiety/panic attacks | OR 1.43, 95% CI: 1.22 to 1.67 for perceived late voice breaking vs on time, P < 7.48 × 10–5 |
| Depression | OR 1.36, 95% CI: 1.25 to 1.49 for perceived late voice breaking vs on time, P < 7.48 × 10–5 |
CI, confidence interval; OR, odds ratio; RR, relative risk.
Although there is no clear evidence for lasting psychosocial consequences of delayed puberty in women, late pubertal timing has been suggested to be associated with psychological issues in men. Perceived late pubertal timing in boys has been associated with higher levels of depression in settings with high levels of peer stress,82 disruptive behavior disorder and substance use in young adulthood,83 and depression and anxiety in later adulthood (Table 6).81 A review of psychological outcomes associated with pubertal timing in boys supported these findings and concluded that the effects of late pubertal timing appear to be limited to higher rates of internalizing symptoms (associated with depression or anxiety) and substance use in both adolescence and young adulthood.84
Studies on educational achievement in individuals with self-limited delayed puberty have reported worse academic performance during childhood85–87 and either no difference88,89 or better performance during young adulthood.83
Summary
Delayed puberty may be associated with increased internalizing symptoms and poorer academic performance in adolescence, but it remains to be determined whether it has significant long-term effects on psychological outcomes and academic achievement in later adulthood.
Malignancy
Breast Cancer
The influence of pubertal timing on the risk for breast cancer is well established, with studies in the 1960s and 1970s demonstrating an association between early age at menarche and increased risk of breast cancer90; subsequent studies further established an association between delayed age at menarche and reduced breast cancer risk.91,92 One such study found that menarche ≥15 years was associated with a twofold reduction in the risk of breast cancer among premenopausal women compared with normally timed menarche.91 Furthermore, a 2-year delay in menarche has been associated with a 10% decrease in the risk of breast cancer in both pre- and postmenopausal women92 and late initiation of breast development (≥13 years) with a 20% decrease in risk compared with breast development occurring at age 11 to 12 years.93
The protective effect of delayed puberty on breast cancer risk has been proposed to be due to a shorter lifetime duration of estrogen exposure and, in turn, less breast cell proliferation and a lower chance of incurring carcinogenic mutations.93 Another factor that has been suggested to independently affect both pubertal timing and breast cancer risk is genetic variation. A recent study found that 2 single nucleotide polymorphisms associated with earlier age at menarche were also associated with an increased risk for breast cancer even after controlling for age at menarche, suggesting that these genetic loci affect breast cancer risk independently of their effect on menarchal timing.94
Endometrial Cancer
Numerous case-control studies have associated early menarche with increased risk of endometrial cancer, but only 2 studies have specifically evaluated the effect of late menarche. A retrospective case-control study in Italy found that menarche ≥14 years was associated with a 32% decrease in the odds of endometrial cancer compared with menarche at age <12 years.95 A prospective study across Europe reported similar findings in women with menarche ≥15 years compared with women with menarche <12 years, with a 7% to 8% reduction in risk per year that menarche is delayed.96 Of note, neither study explicitly compared late menarche with normal menarche, so it is unclear if late menarche is protective against endometrial cancer, if early menarche is a risk factor, or both.
Testicular Cancer
In men, studies examining the relationship between pubertal timing and testicular cancer have produced inconsistent results. Some studies have suggested that later onset of puberty is associated with an ∼40% to 65% decrease in the odds of testicular cancer,97–101 but other studies have reported no association.102–107 A recent meta-analysis of 8 studies found that later age at reported onset of puberty was associated with a 19% reduced odds of testicular cancer.108
Prostate Cancer
The role of pubertal timing on prostate cancer risk is under active investigation with inconclusive findings. Although some studies have reported up to a 25% decrease in the odds of prostate cancer in individuals with later puberty,109–111 others have reported either no association112,113 or up to a 6% increase in the odds of prostate cancer for each year of pubertal delay.114 Difficulty in assessment of pubertal timing in men may be a contributor to the discrepant results; thus, 1 study used a genetic risk score calculated from 13 single nucleotide polymorphisms as a proxy for pubertal development. Although the researchers did not find a significant association between genetic risk score and the presence of prostate cancer, they did identify an association between a higher genetic risk score (later onset of puberty) and a 24% reduction in the odds of high-grade prostate cancer per score tertile.115
Summary
Late pubertal onset in girls is protective against breast cancer and possibly against endometrial cancer. Recent studies suggest that some genetic loci independently affect both breast cancer risk and age at menarche. Late pubertal onset in boys appears to be protective for testicular cancer, but the role of pubertal timing in prostate cancer remains unclear.
Metabolic and Cardiovascular Outcomes
Most studies of the effect of pubertal timing on metabolic and cardiovascular disease have focused on early pubertal maturation, which has been linked to increased risk for obesity, metabolic syndrome, and overall cardiovascular mortality.116 There is now evidence that delayed puberty has negative effects as well.
Early studies suggested a protective effect of delayed puberty for cardiovascular disease. In a retrospective population-based study in Germany, menarche ≥15 years was associated with a 52% reduced odds of peripheral arterial disease compared with menarche at age 12 to 15 years.117 The same study also found an association between later age at menarche and lower BMI, waist circumference, fasting glucose, and 2-hour glucose, trends that extended into the late menarche group (≥15 years).118
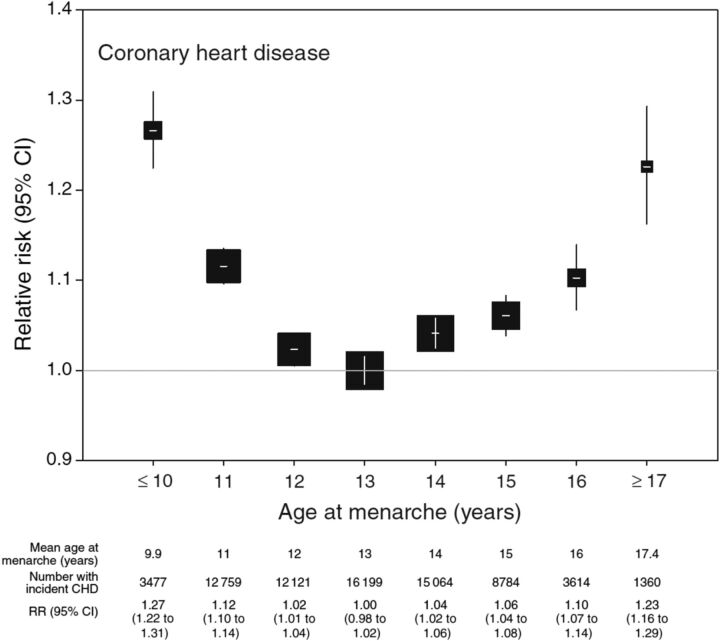
More recent studies have suggested that later pubertal timing in fact has a negative effect. The association between coronary heart disease and menarchal timing exhibits a U-shaped curve, with an increased risk of coronary heart disease associated with both earlier and later pubertal timing. In a recent study of >1 million women in the United Kingdom, both early and late menarche were associated with an increase in risk of coronary heart disease: compared with women with an average age at menarche (13 years), those with menarche at 11 years had a 12% increase in risk and those with menarche at 15 years had a 6% increase in risk after adjustment for covariates including BMI, smoking, and socioeconomic status (Fig 2). The highest risks were observed for menarche at ≤10 years and at ≥17 years, with >20% increase in risk for each group. A similar but less pronounced relationship was found between age at menarche and other conditions, with menarche at ≥17 years associated with a 13% increase in risk for cerebrovascular disease and a 7% increase in risk for hypertensive disease compared with age at menarche at 13 years. Whether this increased risk for cardiovascular disease extends to increased risk for mortality remains unclear.119–123
FIGURE 2.
Relative risk and 95% confidence intervals (CI) of coronary heart disease by age at menarche. Reference category is menarche at 13 years of age. The area of the square is inversely proportional to the variance of the log risk. CHD, coronary heart disease; CI, confidence interval. (Reprinted with permission from page 240 of Canoy D, Beral V, Balkwill A, et al; Million Women Study Collaborators. Age at menarche and risks of coronary heart and other vascular diseases in a large UK cohort. Circulation. 2015;131(3):237–244.)
Few studies have examined the effect of pubertal timing on metabolic and cardiovascular disease in men.116 One study suggested that an earlier age at perceived age of voice breaking was associated with up to a 39% increase in the odds of angina, heart attack, hypertension, and type 2 diabetes, with no observed effect in men with later perceived age of voice breaking.81
Potential Mechanisms Linking Pubertal Timing to Cardiovascular Risk
One proposed explanation for the association between earlier puberty and cardiovascular risk is the association between early puberty and childhood obesity. A review of studies on childhood BMI showed that in 5 of 8 studies, adjusting for childhood obesity attenuated the association between early menarche and higher adult BMI, but only partially, suggesting the presence of additional, yet-to-be-identified factors.116 Similarly, later exposure to sex steroids in individuals with delayed puberty may have effects on metabolic function and cardiovascular health either directly or by affecting other factors such as BMI and lipid metabolism.
Notably, recent genome-wide association studies have identified overlap between genetic loci that influence timing of menarche and those associated with adult BMI.124,125 In one meta-analysis, the influence of these loci on age at menarche was not attenuated by adjustment for BMI.126 These findings suggest that these genetic factors affect pubertal timing and BMI independently and serve as a common genetic link that may account, at least in part, for the association between timing of menarche and the risk for cardiovascular disease. Data from large electronic health record databases,127,128 phenotyping studies,129 and genetic studies may reveal how pubertal timing influences cardiovascular disease risk and in turn how this risk is determined more generally.
Summary
Emerging evidence shows a U-shaped association curve, with both earlier and later onset of pubertal timing associated with an increased risk of cardiovascular disease in women. Factors that may contribute to this association include common genetic links and obesity.
Conclusions and Future Directions
The findings that delayed pubertal timing may have lasting negative consequences raise several questions.
Does delayed puberty truly have lasting negative consequences? There are discrepancies in the existing literature on nearly all outcomes of delayed puberty that have been examined, and publication bias may be a contributing factor. Nevertheless, the studies reviewed in this article raise the possibility that delayed puberty may not be a completely benign entity, particularly with regard to height, BMD, psychological outcomes, and cardiovascular disease.
Are there subsets of individuals with self-limited delayed puberty who are at greatest risk for negative outcomes? The studies cited in this review suggest that familial short stature and slow growth rates before puberty are associated with lower adult height, and race and ethnicity may influence psychosocial outcomes (eg, self-esteem). Most reports have studied primarily Caucasian populations, and the implications for other racial and ethnic groups remain unclear. Further identification of subgroups, which could be achieved through large-scale phenotyping studies or “big data” approaches to analyze medical records,129 may reconcile discrepancies between existing studies. Genetic analyses may identify specific genetic loci associated with these phenotypes and allow for improved prediction of adverse outcomes.
Does current clinical practice need to change? Reassurance and observation remain the foundations for management of individuals with delayed puberty. We do not feel the existing evidence is sufficiently definitive to alter this approach, but we recommend that reassurance be provided with appropriate caveats. Tempered expectations should be set regarding adult height, and clinicians must be careful to not be dismissive or overly optimistic when counseling these patients.
Treatment with sex steroids is an option for individuals with delayed puberty, but its effects on adult outcomes remain unclear. Because it would be difficult to perform a definitive clinical trial to determine whether treatment can avert potential negative outcomes of delayed puberty, an alternative approach to addressing this question may come from large electronic health record databases. Such data may be limited by clinical confounders, but they can shed light on whether sex-steroid treatment of delayed puberty can modify bone density, cardiovascular disease risk, and other adult outcomes and, if so, the age at which such treatment is maximally effective.127,128
Contrary to what is commonly taught, self-limited delayed puberty may not be an entirely benign entity and may be associated with shorter stature, lower BMD, negative psychological outcomes, and increased risk for cardiovascular disease. Further investigations incorporating pubertal timing into both genotype- and phenotype-association studies can further inform our understanding of the links between pubertal timing and these outcomes and, more broadly, the physiology underlying growth, bone health, psychosocial development, and cardiovascular health.
Glossary
- BMD
bone mineral density
- CDGP
constitutional delay of growth and puberty
- DXA
dual x-ray absorptiometry
Footnotes
Dr Zhu conducted the initial literature review, wrote the first draft, and revised the manuscript; Dr Chan conceptualized the review and reviewed and revised the manuscript; and both authors approved the final manuscript as submitted.
FUNDING: Dr Chan was supported by a Doris Duke Clinical Scientist Development Award (grant 2013110).
Contributor Information
Jia Zhu, Division of Endocrinology, Department of Medicine, Boston Children’s Hospital, Boston, Massachusetts.
Yee-Ming Chan, Division of Endocrinology, Department of Medicine, Boston Children’s Hospital, Boston, Massachusetts.
References
- 1.Palmert MR, Dunkel L. Clinical practice. Delayed puberty. N Engl J Med. 2012;366(5):443–453 [DOI] [PubMed] [Google Scholar]
- 2.Herman-Giddens ME, Slora EJ, Wasserman RC, et al. Secondary sexual characteristics and menses in young girls seen in office practice: a study from the Pediatric Research in Office Settings network. Pediatrics. 1997;99(4):505–512 [DOI] [PubMed] [Google Scholar]
- 3.Liu YX, Wickland KA, Karlberg J. New reference for the age at childhood onset of growth and secular trend in the timing of puberty in Swedish. Acta Paediatr. 2000;89(6):637–643 [DOI] [PubMed] [Google Scholar]
- 4.Sun SS, Schubert CM, Chumlea WC, et al. National estimates of the timing of sexual maturation and racial differences among US children. Pediatrics. 2002;110(5):911–919 [DOI] [PubMed] [Google Scholar]
- 5.Wu T, Mendola P, Buck GM. Ethnic differences in the presence of secondary sex characteristics and menarche among US girls: the Third National Health and Nutrition Examination Survey, 1988–1994. Pediatrics. 2002;110(4):752–757 [DOI] [PubMed] [Google Scholar]
- 6.Anderson SE, Must A. Interpreting the continued decline in the average age at menarche: results from two nationally representative surveys of U.S. girls studied 10 years apart. J Pediatr. 2005;147(6):753–760 [DOI] [PubMed] [Google Scholar]
- 7.Sørensen K, Aksglaede L, Petersen JH, Juul A. Recent changes in pubertal timing in healthy Danish boys: associations with body mass index. J Clin Endocrinol Metab. 2010;95(1):263–270 [DOI] [PubMed] [Google Scholar]
- 8.Susman EJ, Houts RM, Steinberg L, et al; Eunice Kennedy Shriver NICHD Early Child Care Research Network. Longitudinal development of secondary sexual characteristics in girls and boys between ages 9 1/2 and 15 1/2 years. Arch Pediatr Adolesc Med. 2010;164(2):166–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goldstein JR. A secular trend toward earlier male sexual maturity: evidence from shifting ages of male young adult mortality. PLoS One. 2011;6(8):e14826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma HM, Chen SK, Chen RM, et al; Pubertal Study Group of the Society of Pediatric Endocrinology and Genetic Disease; Chinese Medical Association . Pubertal development timing in urban Chinese boys. Int J Androl. 2011;34(5 Pt 2):e435–e445 [DOI] [PubMed] [Google Scholar]
- 11.Monteilh C, Kieszak S, Flanders WD, et al. Timing of maturation and predictors of Tanner stage transitions in boys enrolled in a contemporary British cohort. Paediatr Perinat Epidemiol. 2011;25(1):75–87 [DOI] [PubMed] [Google Scholar]
- 12.Herman-Giddens ME, Steffes J, Harris D, et al. Secondary sexual characteristics in boys: data from the Pediatric Research in Office Settings Network. Pediatrics. 2012;130(5):Available at www.pediatrics.org/cgi/content/full/130/5/e1058 [DOI] [PubMed] [Google Scholar]
- 13.Biro FM, Greenspan LC, Galvez MP, et al. Onset of breast development in a longitudinal cohort. Pediatrics. 2013;132(6):1019–1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasegawa T. Disorders of pubertal development. In: Runge M, Patterson C, eds. Principles of Molecular Medicine. Totawa, NJ: Humana Press; 2006 [Google Scholar]
- 15.Jameson JL, de Kretser D, Marshall JC. Delayed puberty. In: Jameson JL, De Groot LJ, eds. Endocrinology: Adult and Pediatric Reproductive Endocrinology., 6th ed. Philadelphia, PA: Elsevier Saunders; 2013 [Google Scholar]
- 16.Tanner JM, Whitehouse RH, Marubini E, Resele LF. The adolescent growth spurt of boys and girls of the Harpenden growth study. Ann Hum Biol. 1976;3(2):109–126 [DOI] [PubMed] [Google Scholar]
- 17.Tanner JM, Whitehouse RH. Clinical longitudinal standards for height, weight, height velocity, weight velocity, and stages of puberty. Arch Dis Child. 1976;51(3):170–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Albanese A, Stanhope R. Investigation of delayed puberty. Clin Endocrinol (Oxf). 1995;43(1):105–110 [DOI] [PubMed] [Google Scholar]
- 19.Sedlmeyer IL, Palmert MR. Delayed puberty: analysis of a large case series from an academic center. J Clin Endocrinol Metab. 2002;87(4):1613–1620 [DOI] [PubMed] [Google Scholar]
- 20.Prader A. Delayed adolescence. Clin Endocrinol Metab. 1975;4(1):143–155 [DOI] [PubMed] [Google Scholar]
- 21.Volta C, Ghizzoni L, Buono T, Ferrari F, Virdis R, Bernasconi S. Final height in a group of untreated children with constitutional growth delay. Helv Paediatr Acta. 1988;43(3):171–176 [PubMed] [Google Scholar]
- 22.von Kalckreuth G, Haverkamp F, Kessler M, Rosskamp RH. Constitutional delay of growth and puberty: do they really reach their target height? Horm Res. 1991;35(6):222–225 [DOI] [PubMed] [Google Scholar]
- 23.Arrigo T, Cisternino M, Luca De F, et al. Final height outcome in both untreated and testosterone-treated boys with constitutional delay of growth and puberty. J Pediatr Endocrinol Metab. 1996;9(5):511–517 [DOI] [PubMed] [Google Scholar]
- 24.Bertelloni S, Baroncelli GI, Ferdeghini M, Perri G, Saggese G. Normal volumetric bone mineral density and bone turnover in young men with histories of constitutional delay of puberty. J Clin Endocrinol Metab. 1998;83(12):4280–4283 [DOI] [PubMed] [Google Scholar]
- 25.Rensonnet C, Kanen F, Coremans C, Ernould C, Albert A, Bourguignon JP. Pubertal growth as a determinant of adult height in boys with constitutional delay of growth and puberty. Horm Res. 1999;51(5):223–229 [DOI] [PubMed] [Google Scholar]
- 26.Brämswig JH, Fasse M, Holthoff ML, von Lengerke HJ, von Petrykowski W, Schellong G. Adult height in boys and girls with untreated short stature and constitutional delay of growth and puberty: accuracy of five different methods of height prediction. J Pediatr. 1990;117(6):886–891 [DOI] [PubMed] [Google Scholar]
- 27.Crowne EC, Shalet SM, Wallace WH, Eminson DM, Price DA. Final height in boys with untreated constitutional delay in growth and puberty. Arch Dis Child. 1990;65(10):1109–1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crowne EC, Shalet SM, Wallace WH, Eminson DM, Price DA. Final height in girls with untreated constitutional delay in growth and puberty. Eur J Pediatr. 1991;150(10):708–712 [DOI] [PubMed] [Google Scholar]
- 29.LaFranchi S, Hanna CE, Mandel SH. Constitutional delay of growth: expected versus final adult height. Pediatrics. 1991;87(1):82–87 [PubMed] [Google Scholar]
- 30.Albanese A, Stanhope R. Does constitutional delayed puberty cause segmental disproportion and short stature? Eur J Pediatr. 1993;152(4):293–296 [DOI] [PubMed] [Google Scholar]
- 31.Albanese A, Stanhope R. Predictive factors in the determination of final height in boys with constitutional delay of growth and puberty. J Pediatr. 1995;126(4):545–550 [DOI] [PubMed] [Google Scholar]
- 32.Sperlich M, Butenandt O, Schwarz HP. Final height and predicted height in boys with untreated constitutional growth delay. Eur J Pediatr. 1995;154(8):627–632 [DOI] [PubMed] [Google Scholar]
- 33.Kelly BP, Paterson WF, Donaldson MD. Final height outcome and value of height prediction in boys with constitutional delay in growth and adolescence treated with intramuscular testosterone 125 mg per month for 3 months. Clin Endocrinol (Oxf). 2003;58(3):267–272 [DOI] [PubMed] [Google Scholar]
- 34.Butenandt O, Bechtold S, Meidert A. Final height in patients with constitutional delay of growth and development from tall statured families. J Pediatr Endocrinol Metab. 2005;18(2):165–169 [DOI] [PubMed] [Google Scholar]
- 35.Poyrazoğlu S, Günöz H, Darendeliler F, Saka N, Bundak R, Baş F. Constitutional delay of growth and puberty: from presentation to final height. J Pediatr Endocrinol Metab. 2005;18(2):171–179 [DOI] [PubMed] [Google Scholar]
- 36.Wehkalampi K, Vangonen K, Laine T, Dunkel L. Progressive reduction of relative height in childhood predicts adult stature below target height in boys with constitutional delay of growth and puberty. Horm Res. 2007;68(2):99–104 [DOI] [PubMed] [Google Scholar]
- 37.Cools BL, Rooman R, Op De Beeck L, Du Caju MV. Boys with a simple delayed puberty reach their target height. Horm Res. 2008;70(4):209–214 [DOI] [PubMed] [Google Scholar]
- 38.Zucchini S, Wasniewska M, Cisternino M, et al. Adult height in children with short stature and idiopathic delayed puberty after different management. Eur J Pediatr. 2008;167(6):677–681 [DOI] [PubMed] [Google Scholar]
- 39.Wehkalampi K, Päkkilä K, Laine T, Dunkel L. Adult height in girls with delayed pubertal growth. Horm Res Paediatr. 2011;76(2):130–135 [DOI] [PubMed] [Google Scholar]
- 40.Rosenfeld RG, Northcraft GB, Hintz RL. A prospective, randomized study of testosterone treatment of constitutional delay of growth and development in male adolescents. Pediatrics. 1982;69(6):681–687 [PubMed] [Google Scholar]
- 41.Soliman AT, Khadir MM, Asfour M. Testosterone treatment in adolescent boys with constitutional delay of growth and development. Metabolism. 1995;44(8):1013–1015 [DOI] [PubMed] [Google Scholar]
- 42.Bonjour JP, Chevalley T. Pubertal timing, bone acquisition, and risk of fracture throughout life. Endocr Rev. 2014;35(5):820–847 [DOI] [PubMed] [Google Scholar]
- 43.NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy . Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285(6):785–795 [DOI] [PubMed] [Google Scholar]
- 44.Finkelstein JS, Neer RM, Biller BM, Crawford JD, Klibanski A. Osteopenia in men with a history of delayed puberty. N Engl J Med. 1992;326(9):600–604 [DOI] [PubMed] [Google Scholar]
- 45.Finkelstein JS, Klibanski A, Neer RM. A longitudinal evaluation of bone mineral density in adult men with histories of delayed puberty. J Clin Endocrinol Metab. 1996;81(3):1152–1155 [DOI] [PubMed] [Google Scholar]
- 46.Kindblom JM, Lorentzon M, Norjavaara E, et al. Pubertal timing predicts previous fractures and BMD in young adult men: the GOOD study. J Bone Miner Res. 2006;21(5):790–795 [DOI] [PubMed] [Google Scholar]
- 47.Kuh D, Muthuri SG, Moore A, et al. Pubertal timing and bone phenotype in early old age: findings from a British birth cohort study. Int J Epidemiol. 2016;45(4):1113–1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yap F, Högler W, Briody J, Moore B, Howman-Giles R, Cowell CT. The skeletal phenotype of men with previous constitutional delay of puberty. J Clin Endocrinol Metab. 2004;89(9):4306–4311 [DOI] [PubMed] [Google Scholar]
- 49.Prentice A, Parsons TJ, Cole TJ. Uncritical use of bone mineral density in absorptiometry may lead to size-related artifacts in the identification of bone mineral determinants. Am J Clin Nutr. 1994;60(6):837–842 [DOI] [PubMed] [Google Scholar]
- 50.Kröger H, Vainio P, Nieminen J, Kotaniemi A. Comparison of different models for interpreting bone mineral density measurements using DXA and MRI technology. Bone. 1995;17(2):157–159 [DOI] [PubMed] [Google Scholar]
- 51.Finkelstein JS, Klibanski A, Neer RM. Evaluation of lumber spine bone mineral density (BMD) using dual energy x-ray absorptiometry (DXA) in 21 young men with histories of constitutionally-delayed puberty. J Clin Endocrinol Metab. 1999;84(9):3400–3401 [DOI] [PubMed] [Google Scholar]
- 52.Rosenthal DI, Mayo-Smith W, Hayes CW, et al. Age and bone mass in premenopausal women. J Bone Miner Res. 1989;4(4):533–538 [DOI] [PubMed] [Google Scholar]
- 53.Fox KM, Magaziner J, Sherwin R, et al; Study of Osteoporotic Fractures Research Group . Reproductive correlates of bone mass in elderly women. J Bone Miner Res. 1993;8(8):901–908 [DOI] [PubMed] [Google Scholar]
- 54.Ito M, Yamada M, Hayashi K, Ohki M, Uetani M, Nakamura T. Relation of early menarche to high bone mineral density. Calcif Tissue Int. 1995;57(1):11–14 [DOI] [PubMed] [Google Scholar]
- 55.Tuppurainen M, Kröger H, Saarikoski S, Honkanen R, Alhava E. The effect of gynecological risk factors on lumbar and femoral bone mineral density in peri- and postmenopausal women. Maturitas. 1995;21(2):137–145 [DOI] [PubMed] [Google Scholar]
- 56.Orwoll ES, Bauer DC, Vogt TM, Fox KM; Study of Osteoporotic Fractures Research Group. Axial bone mass in older women. Ann Intern Med. 1996;124(2):187–196 [DOI] [PubMed] [Google Scholar]
- 57.Löfman O, Larsson L, Ross I, Toss G, Berglund K. Bone mineral density in normal Swedish women. Bone. 1997;20(2):167–174 [DOI] [PubMed] [Google Scholar]
- 58.Varenna M, Binelli L, Zucchi F, Ghiringhelli D, Gallazzi M, Sinigaglia L. Prevalence of osteoporosis by educational level in a cohort of postmenopausal women. Osteoporos Int. 1999;9(3):236–241 [DOI] [PubMed] [Google Scholar]
- 59.Chevalley T, Bonjour JP, Ferrari S, Rizzoli R. Influence of age at menarche on forearm bone microstructure in healthy young women. J Clin Endocrinol Metab. 2008;93(7):2594–2601 [DOI] [PubMed] [Google Scholar]
- 60.Chevalley T, Bonjour JP, Ferrari S, Rizzoli R. Deleterious effect of late menarche on distal tibia microstructure in healthy 20-year-old and premenopausal middle-aged women. J Bone Miner Res. 2009;24(1):144–152 [DOI] [PubMed] [Google Scholar]
- 61.Ribot C, Pouilles JM, Bonneu M, Tremollieres F. Assessment of the risk of post-menopausal osteoporosis using clinical factors. Clin Endocrinol (Oxf). 1992;36(3):225–228 [DOI] [PubMed] [Google Scholar]
- 62.Chevalley T, Bonjour JP, Ferrari S, Rizzoli R. The influence of pubertal timing on bone mass acquisition: a predetermined trajectory detectable five years before menarche. J Clin Endocrinol Metab. 2009;94(9):3424–3431 [DOI] [PubMed] [Google Scholar]
- 63.Chevalley T, Bonjour JP, van Rietbergen B, Rizzoli R, Ferrari S. Fractures in healthy females followed from childhood to early adulthood are associated with later menarcheal age and with impaired bone microstructure at peak bone mass. J Clin Endocrinol Metab. 2012;97(11):4174–4181 [DOI] [PubMed] [Google Scholar]
- 64.Johnell O, Gullberg B, Kanis JA, et al. Risk factors for hip fracture in European women: the MEDOS Study. Mediterranean Osteoporosis Study. J Bone Miner Res. 1995;10(11):1802–1815 [DOI] [PubMed] [Google Scholar]
- 65.Roy DK, O’Neill TW, Finn JD, et al. ; European Prospective Osteoporosis Study (EPOS) . Determinants of incident vertebral fracture in men and women: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int. 2003;14(1):19–26 [DOI] [PubMed] [Google Scholar]
- 66.Silman AJ. Risk factors for Colles’ fracture in men and women: results from the European Prospective Osteoporosis Study. Osteoporos Int. 2003;14(3):213–218 [DOI] [PubMed] [Google Scholar]
- 67.Mussen PH, Jones MC. Self-conceptions, motivations, and interpersonal attitudes of late- and early-maturing boys. Child Dev. 1957;28(2):243–256 [DOI] [PubMed] [Google Scholar]
- 68.Jones MC, Mussen PH. Self-conceptions, motivations, and interpersonal attitudes of early- and late-maturing girls. Child Dev. 1958;29(4):491–501 [DOI] [PubMed] [Google Scholar]
- 69.Apter A, Galatzer A, Beth-Halachmi N, Laron Z. Self-image in adolescents with delayed puberty and growth retardation. J Youth Adolesc. 1981;10(6):501–505 [DOI] [PubMed] [Google Scholar]
- 70.Siegel JM, Yancey AK, Aneshensel CS, Schuler R. Body image, perceived pubertal timing, and adolescent mental health. J Adolesc Health. 1999;25(2):155–165 [DOI] [PubMed] [Google Scholar]
- 71.Obeidallah D, Brennan RT, Brooks-Gunn J, Earls F. Links between pubertal timing and neighborhood contexts: implications for girls’ violent behavior. J Am Acad Child Adolesc Psychiatry. 2004;43(12):1460–1468 [DOI] [PubMed] [Google Scholar]
- 72.Lynne SD, Graber JA, Nichols TR, Brooks-Gunn J, Botvin GJ. Links between pubertal timing, peer influences, and externalizing behaviors among urban students followed through middle school. J Adolesc Health. 2007;40(2):181.e7–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sontag LM, Graber JA, Brooks-Gunn J, Warren MP. Coping with social stress: implications for psychopathology in young adolescent girls. J Abnorm Child Psychol. 2008;36(8):1159–1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.DeRose LM, Shiyko MP, Foster H, Brooks-Gunn J. Associations between menarcheal timing and behavioral developmental trajectories for girls from age 6 to age 15. J Youth Adolesc. 2011;40(10):1329–1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vaughan EB, Van Hulle CA, Beasley WH, Rodgers JL, D’Onofrio BM. Clarifying the associations between age at menarche and adolescent emotional and behavioral problems. J Youth Adolesc. 2015;44(4):922–939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Joinson C, Heron J, Araya R, Lewis G. Early menarche and depressive symptoms from adolescence to young adulthood in a UK cohort. J Am Acad Child Adolesc Psychiatry. 2013;52(6):591–598.e592 [DOI] [PubMed] [Google Scholar]
- 77.Boden JM, Fergusson DM, Horwood LJ. Age of menarche and psychosocial outcomes in a New Zealand birth cohort. J Am Acad Child Adolesc Psychiatry. 2011;50(2):132–140.e5 [DOI] [PubMed] [Google Scholar]
- 78.Herva A, Jokelainen J, Pouta A, et al. Age at menarche and depression at the age of 31 years: findings from the Northern Finland 1966 Birth Cohort Study. J Psychosom Res. 2004;57(4):359–362 [DOI] [PubMed] [Google Scholar]
- 79.Galvao TF, Silva MT, Zimmermann IR, Souza KM, Martins SS, Pereira MG. Pubertal timing in girls and depression: a systematic review. J Affect Disord. 2014;155:13–19 [DOI] [PubMed] [Google Scholar]
- 80.Opoliner A, Carwile JL, Blacker D, Fitzmaurice GM, Austin SB. Early and late menarche and risk of depressive symptoms in young adulthood. Arch Women Ment Health. 2014;17(6):511–518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Day FR, Elks CE, Murray A, Ong KK, Perry JR. Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci Rep. 2015;5:11208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Conley CS, Rudolph KD. The emerging sex difference in adolescent depression: interacting contributions of puberty and peer stress. Dev Psychopathol. 2009;21(2):593–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Graber JA, Seeley JR, Brooks-Gunn J, Lewinsohn PM. Is pubertal timing associated with psychopathology in young adulthood. J Am Acad Child Adolesc Psychiatry. 2004;43(6):718–726 [DOI] [PubMed] [Google Scholar]
- 84.Mendle J, Ferrero J. Detrimental psychological outcomes associated with pubertal timing in adolescent boys. Dev Rev. 2012;32(1):49–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gold RF. Constitutional growth delay and learning problems. J Learn Disabil. 1978;11(7):427–429 [DOI] [PubMed] [Google Scholar]
- 86.Duke PM, Carlsmith JM, Jennings D, et al. Educational correlates of early and late sexual maturation in adolescence. J Pediatr. 1982;100(4):633–637 [DOI] [PubMed] [Google Scholar]
- 87.Dubas JS, Graber JA, Petersen AC. The effects of pubertal development on achievement during adolescence. Am J Educ. 1991;99(4):444–460 [Google Scholar]
- 88.Gordon M, Post EM, Crouthamel C, Richman RA. Do children with constitutional delay really have more learning problems? J Learn Disabil. 1984;17(5):291–293 [DOI] [PubMed] [Google Scholar]
- 89.Petersen AC, Crockett L. Pubertal timing and grade effects on adjustment. J Youth Adolesc. 1985;14(3):191–206 [DOI] [PubMed] [Google Scholar]
- 90.Kelsey JL. A review of the epidemiology of human breast cancer. Epidemiol Rev. 1979;1:74–109 [DOI] [PubMed] [Google Scholar]
- 91.Helmrich SP, Shapiro S, Rosenberg L, et al. Risk factors for breast cancer. Am J Epidemiol. 1983;117(1):35–45 [DOI] [PubMed] [Google Scholar]
- 92.Hsieh CC, Trichopoulos D, Katsouyanni K, Yuasa S. Age at menarche, age at menopause, height and obesity as risk factors for breast cancer: associations and interactions in an international case-control study. Int J Cancer. 1990;46(5):796–800 [DOI] [PubMed] [Google Scholar]
- 93.Bodicoat DH, Schoemaker MJ, Jones ME, et al. Timing of pubertal stages and breast cancer risk: the Breakthrough Generations Study. Breast Cancer Res. 2014;16(1):R18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.He C, Chasman DI, Dreyfus J, et al. Reproductive aging-associated common genetic variants and the risk of breast cancer. Breast Cancer Res. 2012;14(2):R54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zucchetto A, Serraino D, Polesel J, et al. Hormone-related factors and gynecological conditions in relation to endometrial cancer risk. Eur J Cancer Prev. 2009;18(4):316–321 [DOI] [PubMed] [Google Scholar]
- 96.Dossus L, Allen N, Kaaks R, et al. Reproductive risk factors and endometrial cancer: the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2010;127(2):442–451 [DOI] [PubMed] [Google Scholar]
- 97.Swerdlow AJ, Huttly SR, Smith PG. Testis cancer: post-natal hormonal factors, sexual behaviour and fertility. Int J Cancer. 1989;43(4):549–553 [DOI] [PubMed] [Google Scholar]
- 98.United Kingdom Testicular Cancer Study Group . Aetiology of testicular cancer: association with congenital abnormalities, age at puberty, infertility, and exercise. BMJ. 1994;308(6941):1393–1399 [PMC free article] [PubMed] [Google Scholar]
- 99.Møller H, Skakkebaek NE. Risks of testicular cancer and cryptorchidism in relation to socio-economic status and related factors: case-control studies in Denmark. Int J Cancer. 1996;66(3):287–293 [DOI] [PubMed] [Google Scholar]
- 100.Weir HK, Kreiger N, Marrett LD. Age at puberty and risk of testicular germ cell cancer (Ontario, Canada). Cancer Causes Control. 1998;9(3):253–258 [DOI] [PubMed] [Google Scholar]
- 101.Coupland CA, Chilvers CE, Davey G, Pike MC, Oliver RT, Forman D; United Kingdom Testicular Cancer Study Group . Risk factors for testicular germ cell tumours by histological tumour type. Br J Cancer. 1999;80(11):1859–1863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Depue RH, Pike MC, Henderson BE. Estrogen exposure during gestation and risk of testicular cancer. J Natl Cancer Inst. 1983;71(6):1151–1155 [PubMed] [Google Scholar]
- 103.Haughey BP, Graham S, Brasure J, Zielezny M, Sufrin G, Burnett WS. The epidemiology of testicular cancer in upstate New York. Am J Epidemiol. 1989;130(1):25–36 [DOI] [PubMed] [Google Scholar]
- 104.Gallagher RP, Huchcroft S, Phillips N, et al. Physical activity, medical history, and risk of testicular cancer (Alberta and British Columbia, Canada). Cancer Causes Control. 1995;6(5):398–406 [DOI] [PubMed] [Google Scholar]
- 105.McGlynn KA, Sakoda LC, Rubertone MV, et al. Body size, dairy consumption, puberty, and risk of testicular germ cell tumors. Am J Epidemiol. 2007;165(4):355–363 [DOI] [PubMed] [Google Scholar]
- 106.Trabert B, Sigurdson AJ, Sweeney AM, Amato RJ, Strom SS, McGlynn KA. Baldness, acne and testicular germ cell tumours. Int J Androl. 2011;34(4 pt 2):e59–e67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Richiardi L, Vizzini L, Pastore G, et al. Lifetime growth and risk of testicular cancer. Int J Cancer. 2014;135(3):695–701 [DOI] [PubMed] [Google Scholar]
- 108.Maule M, Malavassi JL, Richiardi L. Age at puberty and risk of testicular cancer: a meta-analysis. Int J Androl. 2012;35(6):828–834 [DOI] [PubMed] [Google Scholar]
- 109.Giles GG, Severi G, English DR, et al. Early growth, adult body size and prostate cancer risk. Int J Cancer. 2003;103(2):241–245 [DOI] [PubMed] [Google Scholar]
- 110.Sarre S, Määttänen L, Tammela TL, Auvinen A, Murtola TJ. Postscreening follow-up of the Finnish Prostate Cancer Screening Trial on putative prostate cancer risk factors: vitamin and mineral use, male pattern baldness, pubertal development and non-steroidal anti-inflammatory drug use. Scand J Urol. 2016;50(4):267–273 [DOI] [PubMed] [Google Scholar]
- 111.Nair-Shalliker V, Yap S, Nunez C, et al. Adult body size, sexual history and adolescent sexual development, may predict risk of developing prostate cancer: Results from the New South Wales Cancer Lifestyle and Evaluation of Risk Study (CLEAR). Int J Cancer. 2017;140(3):565–574 [DOI] [PubMed] [Google Scholar]
- 112.Habel LA, Van Den Eeden SK, Friedman GD. Body size, age at shaving initiation, and prostate cancer in a large, multiracial cohort. Prostate. 2000;43(2):136–143 [DOI] [PubMed] [Google Scholar]
- 113.Barba M, Terrenato I, Schünemann HJ, et al. Indicators of sexual and somatic development and adolescent body size in relation to prostate cancer risk: results from a case-control study. Urology. 2008;72(1):183–187 [DOI] [PubMed] [Google Scholar]
- 114.Lope V, García-Esquinas E, Ruiz-Dominguez JM, et al. Perinatal and childhood factors and risk of prostate cancer in adulthood: MCC-Spain case-control study. Cancer Epidemiol. 2016;43:49–55 [DOI] [PubMed] [Google Scholar]
- 115.Bonilla C, Lewis SJ, Martin RM, et al. ; PRACTICAL consortium . Pubertal development and prostate cancer risk: Mendelian randomization study in a population-based cohort. BMC Med. 2016;14:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Prentice P, Viner RM. Pubertal timing and adult obesity and cardiometabolic risk in women and men: a systematic review and meta-analysis. Int J Obes. 2013;37(8):1036–1043 [DOI] [PubMed] [Google Scholar]
- 117.Stöckl D, Döring A, Thorand B, et al. Reproductive factors and its association with peripheral arterial disease in women aged 52-81 years: the KORA F4 study. Atherosclerosis. 2013;228(1):224–229 [DOI] [PubMed] [Google Scholar]
- 118.Stöckl D, Meisinger C, Peters A, et al. Age at menarche and its association with the metabolic syndrome and its components: results from the KORA F4 study. PLoS One. 2011;6(10):e26076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jacobsen BK, Heuch I, Kvåle G. Association of low age at menarche with increased all-cause mortality: a 37-year follow-up of 61,319 Norwegian women. Am J Epidemiol. 2007;166(12):1431–1437 [DOI] [PubMed] [Google Scholar]
- 120.Jacobsen BK, Oda K, Knutsen SF, Fraser GE. Age at menarche, total mortality and mortality from ischaemic heart disease and stroke: the Adventist Health Study, 1976–88. Int J Epidemiol. 2009;38(1):245–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tamakoshi K, Yatsuya H, Tamakoshi A; JACC Study Group . Early age at menarche associated with increased all-cause mortality. Eur J Epidemiol. 2011;26(10):771–778 [DOI] [PubMed] [Google Scholar]
- 122.Charalampopoulos D, McLoughlin A, Elks CE, Ong KK. Age at menarche and risks of all-cause and cardiovascular death: a systematic review and meta-analysis. Am J Epidemiol. 2014;180(1):29–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Canoy D, Beral V, Balkwill A, et al; Million Women Study Collaborators . Circulation. 2015;131(3):237–244 [DOI] [PubMed] [Google Scholar]
- 124.Elks CE, Ong KK. Whole genome associated studies for age at menarche. Brief Funct Genomics. 2011;10(2):91–97 [DOI] [PubMed] [Google Scholar]
- 125.Perry JR, Day F, Elks CE, et al. ; Australian Ovarian Cancer Study; GENICA Network; kConFab; LifeLines Cohort Study; InterAct Consortium; Early Growth Genetics (EGG) Consortium . Parent-of-origin-specific allelic associations among 106 genomic loci for age at menarche. Nature. 2014;514(7520):92–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Elks CE, Perry JR, Sulem P, et al. ; GIANT Consortium . Thirty new loci for age at menarche identified by a meta-analysis of genome-wide association studies. Nat Genet. 2010;42(12):1077–1085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Olson JE, Ryu E, Johnson KJ, et al. The Mayo Clinic Biobank: a building block for individualized medicine. Mayo Clin Proc. 2013;88(9):952–962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Carey DJ, Fetterolf SN, Davis FD, et al. The Geisinger MyCode community health initiative: an electronic health record-linked biobank for precision medicine research. Genet Med. 2016;18(9):906–913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Bush WS, Oetjens MT, Crawford DC. Unravelling the human genome-phenome relationship using phenome-wide association studies. Nat Rev Genet. 2016;17(3):129–145 [DOI] [PubMed] [Google Scholar]