Abstract
More than 70 years after its original report, the hypoxic pulmonary vasoconstriction (HPV) response continues to spark scientific interest on its mechanisms and clinical implications, particularly for anesthesiologists involved in thoracic surgery. Selective airway intubation and one-lung ventilation (OLV) facilitates the surgical intervention on a collapsed lung while the HPV redirects blood flow from the “upper” non-ventilated hypoxic lung to the “dependent” ventilated lung. Therefore, by limiting intrapulmonary shunting and optimizing ventilation-to-perfusion (V/Q) ratio, the fall in arterial oxygen pressure (PaO2) is attenuated during OLV. The HPV involves a biphasic response mobilizing calcium within pulmonary vascular smooth muscles, which is activated within seconds after exposure to low alveolar oxygen pressure and that gradually disappears upon re-oxygenation. Many factors including acid-base balance, the degree of lung expansion, circulatory volemia as well as lung diseases and patient age affect HPV. Anesthetic agents, analgesics and cardiovascular medications may also interfer with HPV during the perioperative period. Since HPV represents the homeostatic mechanism for regional ventilation-to-perfusion matching and in turn, for optimal pulmonary oxygen uptake, a clear understanding of HPV is clinically relevant for all anesthesiologists.
Keywords: Hypoxemia, inhalational anesthesia, intrapulmonary shunt, intravenous anesthesia, pulmonary flow, ventilation-perfusion mismatch
Introduction
Hypoxic pulmonary vasoconstriction (HPV) represents an intrinsic property of pulmonary vascular smooth muscle cells (VSCMs) and an important homeostatic mechanism that helps to ensure correct gas exchange in physiological and pathological conditions.
In 1946, von Euler and Liljestrand, first described the opposing hypoxic responses in the pulmonary and systemic circulations as manifested by vasoconstriction and vasodilatation, respectively.[1] Until delivery, the non-ventilated lungs of the baby exhibit a low alveolar O2 pressure (PAO2) that triggers widespread HPV resulting in elevated pulmonary vascular resistance (PVR) and subsequent diversion of the oxygenated placental blood flow through the foramen ovale and the ductus arteriosus directly into the systemic arteries. Upon the first breath at birth, sensing the rising alveolar PAO2 by pulmonary VSCMs interrupts the HPV response in the newborn, allowing the deoxygenated blood flow to be distributed to the ventilated lung areas through a low resistive pulmonary circulation whereas the foramen ovale and the ductus arteriosus obliterate to prevent right-left shunting.
The HPV plays an important role in patients presenting with heterogenous lung diseases such as pneumonia, atelectasis, chronic obstructive bronchopulmonary disease and acute respiratory distress syndrome. The severity of hypoxemia is attenuated by adapting the ventilation-to-perfusion (V/Q) ratio in various parts of the lungs.[2] In contrast, when the whole lung is exposed to hypoxia (e.g., high altitude, sleep apnea, pulmonary fibrosis), HPV can be detrimental resulting in pulmonary hypertension and acute cor pulmonale owing to progressive increase in right ventricular afterload.
The HPV also plays an important role during one-lung ventilation (OLV) in thoracic surgery and during pneumological procedures to reduce intrapulmonary shunt and preserve blood oxygenation. During awake fiberoptic bronchoscopy, the HPV response has been described using technetium-99m labeled macroaggregated albumin lung perfusion scan.[3] After inflating a balloon-tipped catheter within the left lower bronchus, as the PAO2 and alveolar carbon dioxide pressure (PACO2) distal to the tip of the occluding balloon reach almost the same value as mixed venous PO2 and PCO2 within 80-300 sec, lobar blood flow decreases by 50% and the majority of blood is redistributed to well ventilated parts of the lungs.
Given the importance of oxygen supply in body homeostasis and survival, this review describes the HPV response and its modulating factors that interact in patients undergoing thoracic surgery.
Physiology of Hypoxic Pulmonary Vasoconstriction (HPV)
The hypoxic signal in different tissues
Phylogenetically, the mammalian homeostatic O2 sensing system has developed a multicomponent defense mechanism involving a network of specialized cells such as VSMCs and endothelial cells (ECs), glomic cells in the carotid body, renal myofibroblasts, adrenomedullary chromaffin cells and neuroepithelial bodies in the airways.[4] Detection of low O2 tension by these cells initiates organ-specific responses orchestrated by the hypoxic inducible factor (HIF) involving the HPV, the release of catecholamines, vascular endothelial growth factors and erythropoietin. Accordingly, to adapt to the high-altitude hypoxic environment, mountainers develop various degree of hyperventilation, pulmonary hypertension, polycythemia, stimulation of the sympathetic system as well as increased density of muscular capillaries and intracellular mitochondria to optimize oxygen delivery and aerobic performance.[5]
The HPV response chiefly operates within arteriolar and venular pulmonary vessels (diameter <900 microns), veins accounting for 20% of the total increase in PVR. By distorting the alveolar wall, contractile interstitial cells located within the alveolar septa further contribute to reduce capillary blood flow and increase PVR.[6] In addition, the ECs modulate the HPV through the local release of vasodilators (nitric oxide [NO], prostacyclin [PGI2]) and vasoconstrictors (endothelin [ET], epoxyeicosatrienoic acid [EET], thromboxane A2 [TXA2], and platelet activating factor [PAF]).[7,8]
From ex-vivo ventilated/perfused lungs in whom alveolar and blood O2 tension were modified independently, Marshall et al. demonstrated that acute elevation in PVR was predominantly triggered by sensing low PAO2 and less by sensing deoxygenated blood in mixed venous blood (PmvO2).[9,10] Accordingly, the stimulus of HPV (PO2S) has been modeled using the following equation: PO2 S = PA O20.62 + PmvO20.38
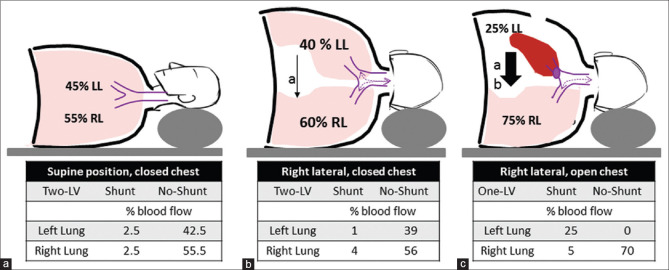
When pulmonary VSCMs or isolated lungs are exposed to decremental levels of local PO2, the HPV develops at a threshold of 85-90 mmHg, to reach a maximum around 65-70 mmHg and declining thereafter to stop around 5 mmHg [Figure 1].[11]
Figure 1.
Thresholds for physiological responses to low oxygen tension. HIF, hypoxic inducible factor; HPV, hypoxic pulmonary vasoconstriction; HV, hypoxic ventilation
The O2 sensing area is thought to extend from precapillary arterioles to upstream pulmonary arteries with different vasoconstrictive responses according to the size of the vessels.[12] The small arteries (diameter < 0.5 mm) are closely exposed to PAO2 (from outside) and to PmvO2 (from inside) whereas larger arteries (diameter of 0.5 to 2 mm) are not exposed to PAO2 but to PmvO2 (from inside) and to arterial O2 pressure (PaO2 from outside, through vasa vasorum). Hence, variable diffusion O2 gradients are generated through the wall of pulmonary arteries that determine the true stimulus for HPV (PO2S), being predominant in smaller than in larger arteries. Interestingly, when mild hypoxemia starts (PaO2 < 80 mmHg), bronchial arteries progressively dilate (like any systemic vessel) and the HPV response is attenuated by collateral intrapulmonary flow in pathological conditions such as cyanotic heart diseases, mitral stenosis and pulmonary thromboembolism.[13]
The oxygen sensing and effector mechanisms of HPV
In eukaryotic cells, mitochondria are acting as powerhouses using O2 to convert nutrients into chemical energy in the form of adenosine triphosphate (ATP). Since mitochondrial respiration continues even at very low O2 level (~7 mmHg) to generate ATP, it is unlikely that variations in ATP concentrations may trigger the hypoxic response.[14] Series of oxidation-reduction reactions involve the transfer of electrons from nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FADH2) across the electron transport chain (ETC).
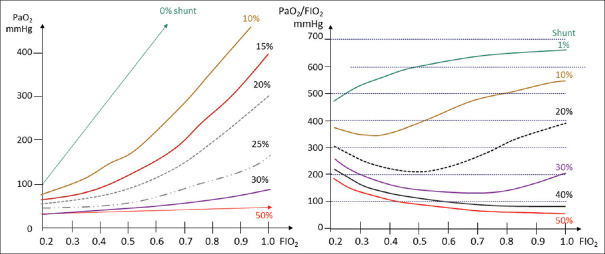
Through the process of oxidative phosphorylation, O2 serves as the terminal electron acceptor of the ETC to form H2O while leaking electrons at multiple sites along the ETC react with O2, forming reactive oxygen species (ROSs) such as superoxide and hydrogen peroxide. In pulmonary VSMCs, the most plausible mechanism to detect hypoxia is the mitochondrial PO2-sensitive system that adjust the production of diffusible ROSs and/or alter the cytosolic redox state. Although controversies surround the issue on whether ROSs generated by the ETC decrease or increase in response hypoxia, there is strong evidence that HPV is triggered by mitochondrial signals that launch a coordinated response involving membranar and sarcolemnal potassium and calcium channel receptors [Figure 2].[15] As proposed by Smith and Schumacker,[15] upon exposure to hypoxia, mitochondrial ROSs promote an intracytoplasmic shift from oxidized to reduced cellular redox state (e.g., proteins, glutathione and NAD/NADH). These hypoxia-induced ROS and redox changes trigger calcium mobilization by: 1) inhibition of voltage-gated potassium channels (Kv) causing membrane depolarization which promotes the opening of voltage-gated calcium channel (VGCC), 2) activation of phospholipase C (PLC) to generate diacycl glycerol (DAG) and inositol 1,4,5-triphosphate (IP3) that stimulate calcium release respectively from membranar receptor-operating channels (ROC) and sarcolemnal IP3 receptor, 3) activation of ryanodine receptors (RyR) by oxidation of cysteine residues, 4) by increasing the ratio of adenosine monophosphate (AMP) to ATP, low O2 tension stimulates AMP-kinase (AMPK) resulting in activation of the RyRs and further calcium release from the sarcoplasmic reticulum. Taken together, the elevation of intracellular calcium concentrations induces calcium binding to calmodulin, subsequent activation of myosine light chain (MLC) kinase, myosin phosphorylation and ultimately contractions of VSMCs. Moreover, after activation of Rho kinase and MLC phosphatase, myofibrillar proteins become more sensitized to the effects of calcium sensitization resulting in sustained contractions of pulmonary VSMCs.
Figure 2.
Oxygen sensing and cellular response (reproduced from Smith and Shumacker[15]). CaM, calmodulin; CRAC, calcium release-activated Ca2; DAG, diacylglycerol; IP3, inositol 1,4,5-trisphosphate; KV channels, voltage gated-potassium channel; MLC, myosin light chain; MLCK, myosin light chain kinase (MLCK); PIP2, phosphatidylinositol bisphosphate; PLC, phospholipase; ROCC, receptor-operated Ca2+ channels; ROS, reactive oxygen species; RyR, ryanodine receptors; SR, sarcoplasmic reticulum; VDCC, voltage-dependent Ca2+ channels
When exposed to hypoxia, both pulmonary and systemic VSCMs share the same effector mechanisms of calcium-mediated changes in vascular tone while pulmonary VSCMCs present the unique property to detect low levels of O2 tension and transmit signals to mobilize calcium close to myofibrillar proteins. Mitochondria are located closer to plasmalemmal membrane in pulmonary VSMCs compared with systemic VSMCs.[16] Therefore, a greater structural and functional coupling between mitochondria and Kv channels in pulmonary VSMCs could explain the specific O2 sensitivity and HPV response.
Time course of HPV
Hypoxic exposure of pulmonary VSCMs results in a biphasic vasoconstrictive response. The early phase starts within 100 msec, peaking at 5-20 min as a result of transient elevations of intracellular calcium concentrations. The phase 2 develops more gradually peaking at 60-120 min as a result of myofibrillar calcium-sensitization coupled with enhanced endothelial release of vasoconstrictive compounds (ET-1 and EET) and decreased production of NO [Figure 3].[11] When normoxia is restored after a short hypoxic phase (<20 min), the HPV declines and PVR normalizes as pulmonary blood flow increases in the re-oxygenated areas. In contrast, after a prolonged period of hypoxia, the HPV only disappears after several hours despite full re-oxygenation, resulting in greater ventilation-perfusion (V/Q) mismatch and consequently larger alveolar-to-arterial O2 pressure gradient (A-aPO2).
Figure 3.
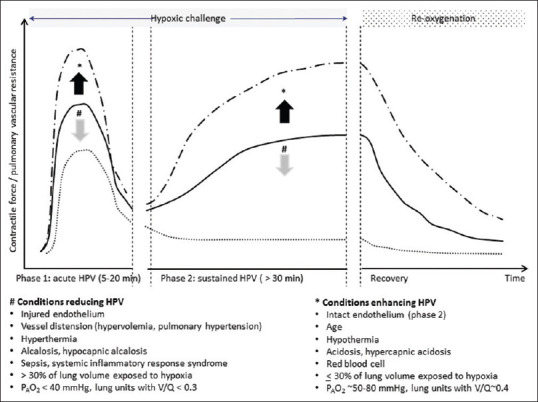
Time course and factors influencing hypoxic pulmonary vasoconstriction (HPV)
After starting the second stage of bilateral surgical procedures, the residual and prolonged HPV response on the dependent ventilated lung (non-ventilated lung during the first stage) causes V/Q mismatch and impaired O2 uptake that requires higher inspiratory oxygen fraction (FIO2) to maintain satisfactory PaO2.
Neurohumoral modulation of HPV
Exposures to intermittent or chronic hypoxia (e.g., pulmonary diseases, altitude) represent stressful challenges that, by stimulating the sympathetic nervous and renin-angiotensin-aldosterone systems (SNS and RAAS), result in elevation of systemic and pulmonary arterial pressures.
Airways and pulmonary vessels are innervated by autonomic and sensory nerve fibers, the highest density of noradrenergic and cholinergic neural endings being found around extrapulmonary and hilar arteries and decreasing towards the periphery (artery size >60-80 mm).[17] Vagal stimulation causes mild vasorelaxation mediated by the endothelial release of NO and vasoactive intestinal factor. Stimulation of the sympathetic nervous system produces the release of norepinephrine from sympathetic neural endings close to arterial wall and of epinephrine from the adrenal medulla in the blood stream. Stimulation of alpha-1-adrenergic-receptors (AAR-1) with norepinephrine causes vasoconstriction whereas stimulation of beta-1 and beta-2 adrenergic receptors (BAR-1 and BAR-2) with epinephrine results in potent vasodilatation owing to activation of the cAMP-dependent protein kinase pathway and the release of NO from ECs. In contrast with normoxic conditions where the sympatho-vagal system plays a negligible role on the pulmonary vasomotor tone, in hypoxic conditions, pulmonary BAR-mediated vasodilatation predominates over AAR-1 vasoconstriction, partially blunting the potent acute HPV.[18] Therefore, in patients with sleep apnea, BAR-mediated relaxation of pulmonary arteries offsets HPV, mitigates the elevation of PVR and alleviates the workload of the right ventricle. Lending support to these clinical findings, experimental data have demonstrated that the HPV response is attenuated with alpha-adrenergic blockers and enhanced with beta-adrenergic blockers.[19]
Hypoxic challenge also stimulates the renin angiotensin aldosterone system (RAAS). Indeed, exposure to hypoxia has been shown to increase the activity of renal adrenergic receptors (AA-1 and BAR-1) in juxtaglomerular cells resulting in increased renin secretion and release of angiotensin II (Ang II) by the action of angiotensin converting enzymes (ACE) largely present in the endothelium of pulmonary capillaries and in other tissues (e.g., brain, heart). In VSCMs, Ang II exerts dual effects on angiotensin receptors type 1 and 2, vasoconstriction mediated by AT-1R and vasodilatation mediated by AT-2.[20] The attenuation of HPV in patients chronically treated with ACE inhibitors supports the predominant constrictive effect of Ang II.[21]
Altogether, there is strong evidence suggesting that hypoxia-induced stimulation of the SNS and RAAS results in systemic cardiovascular and renal changes (e.g., tachycardia, hypertension, oliguria), a blunted HPV response owing to the predominant pulmonary BAR-2 vasodilatory effects which partially offset the constricting effects on AAR-1 and AT-1 receptors.[22] Interestingly, a preserved HPV response has been reported in patients after bilateral lung transplantation, despite the loss of the autonomic neural innervation.[23]
Physiological variations in HPV responses
In healthy individuals breathing air at sea level, pulmonary vessels are almost fully dilated, atelectatic areas are absent and consequently HPV is inactive.[24] Noteworthy, the pressure-flow relationship is not linear since pulmonary vessels offer greater distensibility and recruitability than systemic arteries to accommodate to higher blood flow and to minimize therefore the initial elevation in pulmonary arterial pressure (PAP).[25] For instance, a reduction in CO (e.g., head-up position, blood loss) leads to a larger drop in pulmonary vascular driving pressure, even though the vasomotor tone remains per se unchanged.[26] Conversely, as pressure along the entire circuit increases, the pressure-flow curve becomes more linear since the fully distended vessels are by definition no longer distensible. Hence, when left atrial pressure increases with fluid loading or head-down position, the ability of HPV to redirect blood flow or reduce conductance is curtailed. This concept of HPV dependence on circulatory volume supports the clinical observations that restrictive fluid regimen compared with liberal strategy are associated with better oxygenation in patients with acute lung injury.[27]
Lung volume also influences pulmonary vascular resistance (PVR) as described by the parabolic U-shaped PVR-Volume curve. The PVR reaches a nadir at the functional residual capacity (FRC) and it increases at higher inflating pressures as alveolar capillaries are “squeezed” by elevated alveolar pressures or, when breathing operates below the FRC as the extra-alveolar vessels become distorted and obstructed offering greater resistance to blood flow.
Besides the PAO2 and PmvO2 levels, the strength of HPV also depends on the basal vascular tone and the volume of the lung exposed to hypoxia. A more potent HPV response is elicited when PVR is low (near FRC) and it decreases when the lung is overdistended or collapsed. From animal studies, we know that if exposure to hypoxia exceeds 40% of the whole lung areas, the redistribution of blood flow to non-hypoxic pulmonary areas is decreased suggesting that the increased PAP tends to overcome the increased local arteriolar resistance generated by HPV.[28] In isolated ventilated-perfused lungs, HPV is enhanced by hypercapnia and blunted by metabolic alkalosis and hyperventilation-induced hypocapnia.[29]
Senescence
During exercise, elderly exhibit larger increases in PAP than in younger subjects, given lesser release of vasodilating mediators from the ECs, stiffening of the vascular wall and left ventricular diastolic dysfunction.[30] Moreover, the greater fall in PmvO2 due to a lesser increase in CO and higher O2 extraction in active skeletal muscles, may further enhance HPV and contribute to PAP elevation during intense aerobic exercise.
At rest, middle-aged subjects exposed to moderate alveolar hypoxia (PAO2 ~50 mmHg) over 20 min exhibit a greater increase in PAP compared with younger individuals (+9 mmHg).[31] Such age-related enhancement of HPV could be explained by a greater sensitivity of the O2 sensing apparatus, greater propensity for calcium cell entry and/or greater activity of the calcium-calmoduline-dependent myosin light chain kinase within pulmonary VSMCs.[31]
Effects of Patient Position, Anesthetic Technique and Mechanical Ventilation in Gas Exchange
From wakefulness to anesthetized state
The effectiveness of blood oxygenation is largely determined by the distribution of V/Q ratio through the lungs and the integrity of the alveolar-capillary layer. The multi-compartment lung model enables physiologists and clinicians to predict the changes in PAO2 based on V/Q ratio [Figure 4].[32,33] As the strongest pulmonary vasoconstrictive effect occurs at a PAO2 around 65-70 mmHg and given the slope of the hemoglobin-O2 dissociation curve, the effectiveness of HPV is greatest in lung units with moderately reduced V/Q ratio (~0.4) whereas in atelectatic areas (V/Q <0.1), the very low PAO2 s produces a weaker stimulus for HPV[34] that is enhanced by low PmvO2 values and attenuated by low PaO2 (dilatation of bronchial arteries with enhanced collateral flow).
Figure 4.
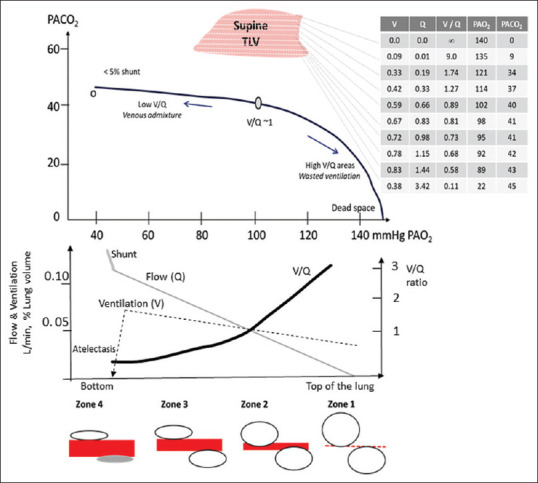
Distribution of blood flow (Q) and ventilation (V), V/Q ratio and alveolar partial pressure of oxygen (PAO2) and carbon dioxide (PACO2) through the lung in supine position
In spontaneously breathing volunteers, Nyren et al. using single photon emission computed tomography showed that sevoflurane anesthesia at 1 minimal alveolar concentration [MAC] resulted in greater heterogeneity of V/Q ratios, a trend towards smaller median V/Q ratios and similar ventral-to-dorsal distribution of tidal volume compared with awake conditions.[35]
Under mechanical positive pressure ventilation, the impairment in blood oxygenation is attributed to the generation of atelectactic areas and a wider dispersion of V/Q ratios, with preferential distribution of ventilation toward ventral lung regions whereas gravitational forces tend to direct blood flow in dorsal regions.[36] Ventilation using oxygen-nitrogen mixture (FIO2 <80%), PEEP and recruitment maneuvers have been shown to mitigate atelectasis formation, optimize V/Q ratios and improve respiratory compliance.[37]
Body position
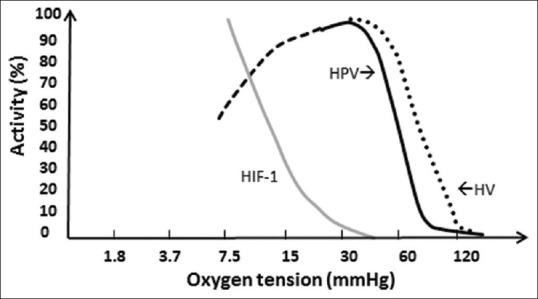
After anesthesia induction, the left and right lungs receive on average 45% and 55% of total CO. After turning the patient from supine to lateral position, blood flow as well as venous and capillary blood volumes are partially shifted from the non-dependent to the dependent lung [Figure 5].[38] The dependent lung receives a larger proportion of CO (+5%) since the gravitational forces generate a vertical pressure gradient through the pulmonary circulation, PAP (and venous pressure) decreasing by 10 to 20 mmHg towards the top of the non-dependent lung. Alveolar areas with V/Q between 0.8 and 1.3 are located in the lower middle part of the dependent lung, the most dependent lung areas (V/Q <0.5) contribute to venous admixture while” wasted” ventilation develops in the upper pulmonary zones (V/Q >3, dead space).
Figure 5.
Perioperative changes in shunted and non-shunted pulmonary blood flow, in supine position (a), right lateral decubitus (b) and one-lung-ventilation (c). a, gravitational forces b, hypoxic vasoconstriction, loss of negative pleural pressure, elastic lung recoil, surgical manipulation
In advanced stages of chronic obstructive pulmonary disease, the HPV response is less effective and the impact of patient's position plays a greater role as gravitational forces augments the redirection of perfusion to the dependent lung and improves oxygenation.[39]
This physiological concept supports the clinical practice of positioning critically-ill patients with unilateral hypoxemic pulmonary diseases with the “good lung down” in order to optimize V/Q matching.
In contrast to lung surgery that requires lateral positioning, cardiac robot-assisted surgery is performed in supine position and OLV facilitates the harvesting of the internal mammary artery. In a cohort study of 255 consecutive patients, Liu et al. reported only 9 cases of hypoxemic event (PaO2 <70 mmHg despite increases in PEEP level and FIO2), the mean PaO2 level decreasing by approximately 30% on average, similar to the fall observed in thoracic surgery when patients are installed in lateral decubitus.[40] These observations underline the importance of HPV during OLV in V/Q matching, patient position and gravity forces playing a minor role on pulmonary blood flow in healthy lungs.
From two-lung to one lung ventilation
At the start of thoracic surgery, switching mechanical ventilation from two lungs ventilation to OLV, always results in declining PaO2 levels (-30 to 50%) consequent to the reduced surface area available for gas exchange and variable intrapulmonary shunting.[41] Within the first 10 min after OLV, oxygen transfer from alveola to capillaries in the non-ventilated lung contribute to maintain blood oxygenation and the HPV is elicited when PAO2 progressively declines below a thresholds value of 85 mmHg. Then, the activated HPV in the “hypoxic” lung redirects blood flow to the dependent ventilated lung to minimize shunting (QS/QT) and venous admixture through the operated lung [Figure 5].[42]
In the dependent lung, the distensibility and recruitability of pulmonary vessels attenuate the increase in PAP and right ventricular afterload while providing a larger capillary surface area for gas exchange to mitigate the fall in diffusion capacity. Along a vertical bottom-up distance, ventilation increases and perfusion of lung areas decreases that results in wider spread of V/Q ratios. Moreover, the weight of the mediastinal and abdominal organs on the dependent hemithorax results in higher pleural pressure (PPleural, +0.25 cmH2O per cm from upper to lower areas) that causes a further reduction in FRC in addition to the effects of anesthetic and neuromuscular agents on respiratory muscle tone.[43] Therefore, both higher PInsp and PEEP levels are required to deliver the tidal volume and to maintain FRC, the driving pressure remaining unchanged (△P = PInsp – PPleural). Interestingly, Spadaro et al. reported that setting PEEP at 10 cmH20 during OLV resulted in lower shunt fraction, decreased driving pressure and dynamic compliance along with improved oxygenation compared with PEEP at 5 cmH20.[44] As the increased capillary blood flow tends to match the alveolar ventilation through the dependent lung with increasing V/Q ratios, the efficacy of gas exchange can be ensured during OLV.
Chest opening
Within 10-20 min after chest opening, the elastic lung recoil forces acting in the non-ventilated lung results in a progressive collapse of the lung. Several measures may accelerate lung deflation: 1) ventilation with 100% O2 before lung exclusion to enhance resorption atelectasis, 2) transient ventilator disconnection (1-2 min) with balloon deflation to facilitate alveolar gas clearance, 3) external lung compression by the surgeon. Besides HPV, mechanical vascular closure that parallels the collapse of bronchoalveolar tissues plays a secondary role in shifting pulmonary blood flow towards the dependent ventilated lung to minimize intrapulmonary shunt.[45]
Impact of anesthetic drugs
In vitro studies[46] using denervated pulmonary arteries and in vivo experiments using isolated perfused lungs strongly support a dose-response inhibition of HPV by volatile anesthetics in contrast to intravenous drugs such as propofol, ketamine, droperidol and barbiturates anesthetics which have no (or minimal) effect on the HPV response [Table 1].[46,47]
Table 1.
Impact of perioperative drug and anesthetic management on cardiovascular control and hypoxic pulmonary vasoconstriction
| HR | MAP | SVR | PVR | CO | HPV | Raw | |
|---|---|---|---|---|---|---|---|
| Intravenous Anesthetics | |||||||
| Ketamine | + | + | + | +/0 | + | 0 | - |
| Etomidate | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Propofol | 0/- | -- | -- | 0 | - | 0 | 0 |
| Midazolam | 0 | 0/- | 0/- | 0 | 0/- | 0 | 0 |
| Analgesics | |||||||
| Opiates | 0 | 0 | 0 | 0 | 0 | 0 | 0 (+) |
| Dexmedetomidine | - | - | - | 0 | - | 0 | 0 |
| Nonsteroidal anti-inflammatory drugs | 0 | 0 | 0 | 0 | 0 | (-/0/+) | 0 |
| Volatil anesthetics | |||||||
| Isoflurane | 0/- | -- | -- | -- | -- | -- | - |
| Sevoflurane | 0/- | - | - | - | - | - | - |
| Desflurane | 0/- | - | - | - | - | - | - |
| Inotropes, vasopressors, bronchodilators | |||||||
| Dobutamine, Dopamine | + | +/0/- | 0/- | 0/- | + | - | 0 |
| Phenyléphrine | 0/- | + | + | + | 0/- | 0 | 0 |
| Milrinone | 0 (-) | ||||||
| Salbutamol | + | +/0/- | + | 0/- | + | - | - |
| Anti-hypertensive drugs | 0/- | -- | -- | - | 0/+ | - | |
| CCB | 0/- | -- | -- | - | 0/+ | - | 0 |
| NTG, NPS | 0/+ | -- | -- | - | + | - | 0 |
| ACEI, ATA | 0 | - | - | 0/- | + | 0/- | 0((+) |
| Beta-blockers | - | - | 0/+ | 0/+ | - | 0 | 0/+ |
0, no change; +, increased; -, decreased; --, more decreased; CO, cardiac output; HPV, hypoxic pulmonary vasoconstriction; HR, heart rate; MAP, mean arterial pressure; PVR, pulmonary vascular resistance; Raw, airway resistance; SVR, systemic vascular resistance. ACEI, angiotensin-converting enzyme inhibitor; ATA, angiotensin II antagonist; CCB, calcium-channel blocker; NPS, nitroprussiate; NTG, nitroglycerine
In intact animal models, the HPV response is determined by the interaction between vasodilatory and cardio-depressive effects of anesthetic agents. The direct inhibition of HPV by volatile anesthetics is partially offset by their cardio-depressive effects, the decreased CO causing flow diversion and the low PmvO2 directly enhancing the HPV response. In contrast, ketamine and propofol exert less negative inotropic effects, therefore HPV is maintained and slightly potentiated with propofol through inhibition of pulmonary vasodilatation mediated by KATP channels.[48]
During thoracic surgery, intravenous anesthetic drugs result in preserved or even enhanced HPV whereas inhalational anesthetics cause mild-to-moderate inhibition of HPV and peripheral vasodilation that mitigate cardiac depression by reducing left ventricular afterload. In a meta-analysis of 23 randomized controlled trials, volatile anesthetics were associated with higher intrapulmonary shunt (QS/QT 33% vs 27%, mean difference of - 5.4%), higher cardiac index (3.2 vs 2.9 L/min, mean difference of 0.19 L/min) and lower oxygenation index during OLV (PaO2 with mean difference of -27 mmHg) compared with intravenous anesthesia.[49] These data confirm that volatil anesthetics within the clinical dose range (from 0.5 to 1.5 MAC) slightly impair lung oxygen uptake by reducing the HPV response with a consequent increase in venous admixture. The impairment in lung oxygen uptake by inhalational anesthesia should be balanced against important benefits of volatil anesthetics: 1) direct bronchodilatation, particularly valuable in patients with asthma and COPD,[50] 2) larger attenuation of the release of alveolar inflammatory mediators and oxidative stress coupled with reduced adhesion of platelets and leucocytes in endothelial pulmonary capillaries,[51,52] 3) lesser incidence of postoperative pulmonary complications resulting from anesthetic preconditioning and protection of the alveolar-capillary membrane.
Effects of analgesics
Administration of iv opiates (e.g., morphine, fentanyl, sufentanil, buprenorphine) does not impair the capacity of the pulmonary circulation to respond to hypoxia. The lack of interference of opiates with the HPV response has been strongly established in animal and clinical studies.[53,54]
Dexmedetomidine, an alpha-2 adrenergic agonist has been shown to preserve (or enhance) HPV response.[55,56] Improvement in oxygenation and favorable clinical outcome in patients receiving dexmedetomidine could be attributed to lesser need for volatile anesthetics, blunting the neuroendocrine stress response, higher dynamic lung compliance, lower oxidative stress and anti-inflammatory effects.[57,58,59]
With non-selective cyclooxygenase (COX) inhibitors that are used in the postoperative setting, the HPV response is minimally altered as the balance between vasoconstrictive (TXA2) and vasodilatory mediators (PGI2) remains stable.[60] The production of PGI2 is predominantly related to COX-1 activity in acute hypoxia and to COX-2 in chronic hypoxia. Therefore, celexocib, a COX-2 inhibitor, was reported to attenuate the HPV in subjects exposed to a hypoxic environment, as the vasodilatory effects of PGI2 are unopposed by the lower concentrations of TXA2. In contrast, in patients with chronic hypoxemic pulmonary diseases, the HPV response can be re-inforced owing to reduced PGI2 activity when COX-2 inhibitors are given.[61,62]
Effects of cardiovascular drugs
Inotropes such as dobutamine, dopamine and epinephrine increase ventricular contractility and reduced ventricular afterload by activating cardiac BAR-1 and vascular BAR-2, respectively. The consequent increase in O2 transport and O2 availability may result in improved kidney, splanchnic or cerebral function in patients with heart failure. However, the BAR-2 mediated dilatation of pulmonary vessels attenuates the HPV response causing intrapulmonary shunt as manifested by greater PA-aO2 gradient and impaired blood oxygenation.[63]
Phenylephrine, an agonist acting on AAR-1, exerts both pulmonary and systemic vasoconstrictor effects. Ephedrine, an alkaloid derived from ephedra herb, stimulates the release of NE from sympathetic nerve endings and also acts directly on AARs and BARs. During OLV, administration of phenylephrine or ephedrine was shown effective to normalize blood pressure while blood oxygenation was maintained (or improved) and QS/QT unchanged.[64] Likewise, Doering et al. reported that, in some patients with ARDS, a continuous infusion of phenylephrine resulted in higher PaO2 (mean gain of 15 mmHg) suggesting the ability of AAR-1 agonists to enhance HPV along with minor increase in PAP and unchanged CO.[65]
With inhaled BAR-2 agonists such as salbutamol or terbutaline, the occurrence of O2 desaturation in bronchospastic patients has been attributed to greater heterogeneity in V/Q ratios owing to BAR-2 mediated vasorelaxation and blunting of the HPV response.[66]
Most anti-hypertensive drugs such as NO donors (nitroglycerin, nitroprussiate), phosphodiesterase inhibitors, AAR-1 blockers, calcium-channel blockers, ACE inhibitors and angiotensin receptor antagonists (ATA), all attenuate HPV by acting on EC-derived modulators as well as signal transduction pathways in pulmonary VSCMs that limit calcium mobilization and gene-transcription. The vasodilatory effects of these drugs are particularly helpful to unload the right ventricule in patients with pulmonary hypertension. Interestingly, treatment with ACE inhibitors or ATA has been shown to attenuate the acute pulmonary hypertensive response in volunteers breathing a hypoxic mixture.[21,67] After long-term therapy with ACEI in patients with heart failure, improvement in oxygenation has been observed that suggests a limited role in drug-induced V/Q mismatch and the prominent effects of better O2 delivery to respiratory muscles.[68]
Non-selective beta-blockers such as propranolol have been shown to augment O2 content in hypoxemic critically ill patients by blocking the pulmonary vasodilatation depending on BAR-2 and by reducing ventricular contractility depending on BAR-1.[69] The diminished CO and in turn the reduced PmvO2 could enhance the HPV response in low V/Q lung areas.[70]
Almitrine besylate, a diphenylmethylpiperazine derivative was initially used in COPD patients to improve gas exchange by a chemoreflex-mediated increase in minute ventilation and by optimizing V/Q matching along with enhanced HPV.[71] In patients with acute respiratory failure, iv administration of almitrine has produced short-term improvement in blood oxygenation, particularly when it was combined with selective vasorelaxant drugs (e.g., inhaled NO and PGI2) however, it has been abandoned given the occurrence of lactic acidosis, worsening pulmonary hypertension and liver dysfunction.[72] In thoracic surgery, almitritine has been shown effective to attenuate the fall in PaO2 during OLV under iv anesthesia but not under sevoflurane anesthesia.[73,74,75]
Thoracic epidural anesthesia (TEA)
In unstressed individuals in supine position, the sympatho-adrenergic system is barely activated. Therefore, blocking the sympathetic efferent nerves with thoracic epidural anesthesia produces a mild reduction in blood pressure owing to vasodilatory effects in the visceral and cutaneous compartments.[76]
During stressful perioperative events (e.g., hemorrhage, pain), activation of the sympatho-adrenal pathways results in systemic vasoconstriction (AAR-1), cardiac hyperactivity (BAR-1) as well as vasodilatation in the pulmonary circulation. Importantly, blunting of cardiac and vascular sympathetic drive induced by TEA with even low dose of local anesthetics (LA) results in vagal predominance along with attenuation of the baroreflex response, rendering patients less tolerant to cope appropriately with acute hypovolemia due to sudden blood losses.[77]
Blood oxygenation has been reported to be unaffected, slightly impaired or enhanced by TEA, depending on the dose of LA, the general anesthetic regimen and the prevailing hemodynamic conditions.[78,79,80,81] A dose-response has been observed between the concentrations of ropivacaine (0.75%, 0.5% and 0.25%) and the development of intra-pulmonary shunting with hypoxemia[82] At the highest concentrations of ropivacaine (0.75-0.5%), the potent sympathetic blockade produces prominent cardiac depression and inhibition of AA1-mediated vasoconstriction in large pulmonary arteries. Attenuation of the HPV is mitigated by the TEA-induced reduction in CO, the consequent lower PmvO2 as well as by the lower anesthetic requirement if volatile anesthetics are used. At the lowest concentrations of LA which are routinely used in thoracic anesthesia, cardiac depression is less pronounced and the HPV response is barely affected, particularly under total iv anesthesia.
Choice of General Anesthetics
Worldwide, the majority of thoracic procedures are performed under inhalational anesthesia.[83] Thoracic anesthesiologists justify this choice by valuable reasons: 1) safe and easy control of the depth of anesthesia, 2) relaxation of bronchial muscle tone, 3) potentiation of the effects of neuromuscular blockers on the motor end-plate, 4) organ protection against ischemia-reperfusion and septic-induced injuries.[83]
In cardiac surgery, anesthetic preconditioning with volatile agents (e.g., isoflurane, desflurane or sevoflurane) is associated with lesser myocardial injury and shorter ICU stay.[84,85] In thoracic surgery, a meta-analysis of 23 RCTs has demonstrated a 50% reduction in PPCs in patients receiving volatile anesthetics compared with those receiving total intravenous anesthesia.[49] In agreement with these findings, an analysis of a multicentric cohort of patients undergoing non-cardiac surgery (N = 124'497), including 4'880 thoracic interventions, has demonstrated a dose-dependent protective effect of volatile anesthetics against PPCs, along with reduced 30-day mortality rate and lower hospital costs.[86] However these anesthetic-organ preconditioning effects are opposed by a higher rate in cancer recurrence and a reduction in long-term survival in patients exposed to volatile agents compared with intravenous anesthesia.[87,88] Experimental data lend support to the inhibitory effects of volatile anesthetics on cell-based immunity (e.g., natural killer cell activity) along with upregulation of the transcription of HIF, insulin growth factor and vascular endothelial growth factor which may facilitate intraoperative “seeding” of tumor cells, remodeling of lymphatic vessels and angiogenesis-induced tumor growth that may promote later cancer recurrence and metastasis.[89] In contrast, propofol inhibits the host immunity to a lower extent, as the natural killer cell activity is better preserved. Moreover, propofol has demonstrated anti-tumor effects in non-small cell lung carcinoma resulting from disrupted regulation of HIF.[90] Co-administration of low doses of ketamine may represent a valuable way to reduce the dose of volatil anesthetics, to attenuate surgery-induced immunosuppression through its analgesic and anti-inflammatory effects, reducing leucocyte reactivity, ROS generation and cytokines overproduction while preserving interleukin-2 activity, a key regulator of both cellular and humoral immune response.[91]
So far, clinical studies comparing intravenous and inhalational anesthesia have reported mixed results regarding long-term clinical outcome. A systematic review including 7'800 patients undergoing lung, oesophageal or breast cancer resection found that iv anesthesia was associated with improved recurrence-free survival compared with inhalation anesthesia (Hazard Ratio of 0.78, 95% confidence interval 0.65 to 0.94).[92] Given the heterogeneity of patient populations, the various surgical procedures and the retrospective nature of the studies (one RCT, 5 cohorts), large randomized trials should be designed to confirm or refute the immunomodulatory effects of anesthetic agents.
Management of Intraoperative Hypoxemia
Application of minimal monitoring standards including pulse oximetry since the 1990s has contributed to a 20-fold decrease in anesthesia-related mortality, much of this decline being attributed to earlier diagnosis and correction of hypoxemia.[93] Intraoperative hypoxemia is classically defined by SpO2<90% corresponding to PaO2 <58-62 mmHg (7.7-8.3 kPa) and severe hypoxemia by SpO2<85% corresponding to PaO2 <50-54 mmHg (6.7-7.2 kPa). Due to the sigmoid shape of O2-Hb dissociation curve, changes in SpO2 poorly reflect the early impairment in blood oxygenation, particularly when high FIO2 are used. Based on electronic anesthesia records, hypoxemic events were reported in 6.8% and severe hypoxemia in 3.5% of 95'407 non-thoracic cases. During thoracic surgery with OLV, the incidence of sustained oxygen desaturation (SpO2<90%) ranges between 2 to 10% but the limits of tolerability and impact on postoperative outcome remain debatable.[41,94] Interestingly, hypoxic preconditioning characterized by three cycles of 5-min “no-ventilation” with 3 min ventilation of the dependent lung has been shown to increase intraoperative PaO2/FIO2 ratio (+10%), to enhance recovery of lung function and reduce the hospital length of stay after VATS.[95]
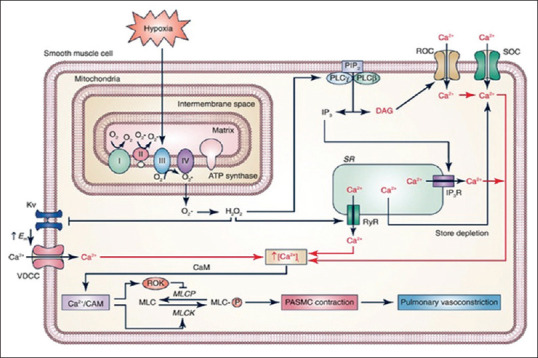
The mechanism of intraoperative hypoxemia is chiefly related to intrapulmonary shunting and venous admixture under general anesthesia and mechanical ventilation. Anesthesia-related atelectasis, misplacement of the double-lumen tube or bronchial blocker, acute bronchospasm and accumulation of secretions or blood in the airways all may result in heterogenous distribution of tidal volume and increase in lung areas with very low V/Q ratio. If the total intrapulmonary shunt (anatomical and physiologic) is less than 15 to 20% of the CO, hypoxemia can easily be corrected by increasing FIO2, whereas lesser gains in PaO2 are achieved in the presence of shunt exceeding 20% as the slope of the PaO2-FIO2 curve decreases and flattens when the shunt approximates 50% [Figure 6].[96,97]
Figure 6.
Iso-shunt diagram describing the relationship between PaO2 or PaO2/FIO2 ratio and FIO2 in the presence of variable pulmonary shunt fraction (adapted from Feiner et al.[61] and Benatar et al.[62])
The stepwise approach of intraoperative management of hypoxemia entails the following sequence[94,98]: 1) increase the FIO2 level, avoid hypervolemia and restore normal blood pressure (vasopressor, head up/down position), 2) ensure proper lung isolation technique by adjusting the position of the double-lumen tube or bronchial blocker, 3) exclude any obstruction in the ventilator tubings and airways, clear any secretions or blood clot, alleviate any bronchospasm with a beta-1 adrenergic agonist, 4) re-expand collapsed alveola in the dependent lung by a recruitment maneuver and titrate the level of PEEP to improve respiratory compliance, 4) enhance the collapse of operated lung by disconnecting the ventilator from the airway, deflating the tube's balloon and asking the surgeon to “squeeze” parts of the lung to facilitate gas elimination, 5) alternatively, cautious re-expansion of the operated lung by continuous positive airway pressure, intermittent low positive pressure or apneic oxygenation (e.g., high jet ventilation) that lead to increase the surface area available for blood gas exchange.[99] Finally, switching from inhalational to iv anesthesia is the last option to manage refractory hypoxemia by favoring the HPV response. In case of pneumonectomy, clamping of the pulmonary artery by the surgeon eliminates the shunt through the operated lung resulting in better oxygenation.
Conclusions
The HPV is a physiological reflex response effective in pulmonary diseases and during OLV that minimizes intrapulmonary shunt, optimizes V/Q ratios and limits alterations in blood oxygenation.
The initiation of OLV is always associated with a fall in PaO2 but the incidence of severe hypoxemia is low and can be avoided/treated by proper placement of the double-lumen tube/bronchial blocker and adjustment of ventilatory settings while ensuring hemodynamic control.[94]
The strongest pulmonary vasoconstrictive effect occurs when 20-40% of the lung volume is exposed to PAO2 around 65-70 mmHg and it results in diversion of blood flow to the remaining ventilated areas. After the start of OLV and chest opening, pulmonary blood flow is preferentially directed to the dependent ventilated lung according to gravitational forces and the effectiveness of the HPV response through the non-dependent “hypoxic” lung.
With TEA and intravenous anesthetic agents (e.g., ketamine and propofol), the HPV is well preserved and reduces the intrapulmonary shunt by 20-40% during OLV in lateral position [Figure 7]. Volatile anesthetics dose-dependently attenuate the HPV response although within the clinical dose range (0.5 to 1.5 MAC), the impairment in lung oxygen uptake is relatively mild owing to small increases in venous admixture. Moreover, modern agents such as sevoflurane and desflurane offer valuable benefits in terms of bronchial relaxation, organ protection and anti-inflammatory effects that contribute to lower the risk of postoperative pulmonary complications.
Figure 7.
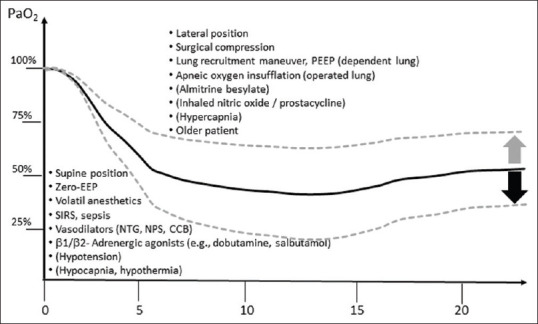
Time course of arterial PO2 after initiation of one-lung ventilation and modulating factors
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Liljestrand G. Regulation of pulmonary arterial blood pressure. Arch Intern Med (Chic) 1948;81:162–72. doi: 10.1001/archinte.1948.00220200050006. [DOI] [PubMed] [Google Scholar]
- 2.Hughes JM. Hypoxic pulmonary vasoconstriction: Clinical implications. Eur Respir J. 2016;47:31–4. doi: 10.1183/13993003.01753-2015. [DOI] [PubMed] [Google Scholar]
- 3.Morrell NW, Nijran KS, Biggs T, Seed WA. Changes in regional pulmonary blood flow during lobar bronchial occlusion in man. Clin Sci (Lond) 1994;86:639–44. doi: 10.1042/cs0860639. [DOI] [PubMed] [Google Scholar]
- 4.Shimoda LA, Laurie SS. HIF and pulmonary vascular responses to hypoxia. J Appl Physiol (1985) 2014;116:867–74. doi: 10.1152/japplphysiol.00643.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirota K. Basic biology of hypoxic responses mediated by the transcription factor hifs and its implication for medicine. Biomedicines. 2020;8:32. doi: 10.3390/biomedicines8020032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kapanci Y, Assimacopoulos A, Irle C, Zwahlen A, Gabbiani G. “Contractile interstitial cells” in pulmonary alveolar septa: A possible regulator of ventilation-perfusion ratio.Ultrastructural, immunofluorescence, and in vitro studies? J Cell Biol. 1974;60:375–92. doi: 10.1083/jcb.60.2.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.al-Tinawi A, Krenz GS, Rickaby DA, Linehan JH, Dawson CA. Influence of hypoxia and serotonin on small pulmonary vessels. J Appl Physiol (1985) 1994;76:56–64. doi: 10.1152/jappl.1994.76.1.56. [DOI] [PubMed] [Google Scholar]
- 8.Gao Y, Raj JU. Role of veins in regulation of pulmonary circulation. Am J Physiol Lung Cell Mol Physiol. 2005;288:L213–26. doi: 10.1152/ajplung.00103.2004. [DOI] [PubMed] [Google Scholar]
- 9.Benumof JL, Pirlo AF, Johanson I, Trousdale FR. Interaction of PVO2 with PAO2 on hypoxic pulmonary vasoconstriction. J Appl Physiol Respir Environ Exerc Physiol. 1981;51:871–4. doi: 10.1152/jappl.1981.51.4.871. [DOI] [PubMed] [Google Scholar]
- 10.Marshall BE, Clarke WR, Costarino AT, Chen L, Miller F, Marshall C. The dose-response relationship for hypoxic pulmonary vasoconstriction. Respir Physiol. 1994;96:231–47. doi: 10.1016/0034-5687(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 11.Sylvester JT, Shimoda LA, Aaronson PI, Ward JP. Hypoxic pulmonary vasoconstriction. Physiol Rev. 2012;92:367–520. doi: 10.1152/physrev.00041.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jameson AG. Diffusion of gases from alveolus to precapillary arteries. Science. 1963;139:826–8. doi: 10.1126/science.139.3557.826. [DOI] [PubMed] [Google Scholar]
- 13.Fishman AP. The clinical significance of the pulmonary collateral circulation. Circulation. 1961;24:677–90. doi: 10.1161/01.cir.24.3.677. [DOI] [PubMed] [Google Scholar]
- 14.Sommer N, Strielkov I, Pak O, Weissmann N. Oxygen sensing and signal transduction in hypoxic pulmonary vasoconstriction. Eur Respir J. 2016;47:288–303. doi: 10.1183/13993003.00945-2015. [DOI] [PubMed] [Google Scholar]
- 15.Smith KA, Schumacker PT. Sensors and signals: The role of reactive oxygen species in hypoxic pulmonary vasoconstriction. J Physiol. 2019;597:1033–43. doi: 10.1113/JP275852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Firth AL, Gordienko DV, Yuill KH, Smirnov SV. Cellular localization of mitochondria contributes to Kv channel-mediated regulation of cellular excitability in pulmonary but not mesenteric circulation. Am J Physiol Lung Cell Mol Physiol. 2009;296:L347–60. doi: 10.1152/ajplung.90341.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaillancourt M, Chia P, Sarji S, Nguyen J, Hoftman N, Ruffenach G, et al. Autonomic nervous system involvement in pulmonary arterial hypertension. Respir Res. 2017;18:201. doi: 10.1186/s12931-017-0679-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shirai M, Tsuchimochi H, Nagai H, Gray E, Pearson JT, Sonobe T, et al. Pulmonary vascular tone is dependent on the central modulation of sympathetic nerve activity following chronic intermittent hypoxia. Basic Res Cardiol. 2014;109:432. doi: 10.1007/s00395-014-0432-y. [DOI] [PubMed] [Google Scholar]
- 19.Brimioulle S, Vachiery JL, Brichant JF, Delcroix M, Lejeune P, Naeije R. Sympathetic modulation of hypoxic pulmonary vasoconstriction in intact dogs. Cardiovasc Res. 1997;34:384–92. doi: 10.1016/s0008-6363(97)00028-x. [DOI] [PubMed] [Google Scholar]
- 20.Gaur P, Saini S, Vats P, Kumar B. Regulation, signalling and functions of hormonal peptides in pulmonary vascular remodelling during hypoxia. Endocrine. 2018;59:466–80. doi: 10.1007/s12020-018-1529-0. [DOI] [PubMed] [Google Scholar]
- 21.Cargill RI, Lipworth BJ. Lisinopril attenuates acute hypoxic pulmonary vasoconstriction in humans. Chest. 1996;109:424–9. doi: 10.1378/chest.109.2.424. [DOI] [PubMed] [Google Scholar]
- 22.Hubloue I, Rondelet B, Kerbaul F, Biarent D, Milani GM, Staroukine M, et al. Endogenous angiotensin II in the regulation of hypoxic pulmonary vasoconstriction in anaesthetized dogs. Crit Care. 2004;8:R163–71. doi: 10.1186/cc2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robin ED, Theodore J, Burke CM, Oesterle SN, Fowler MB, Jamieson SW, et al. Hypoxic pulmonary vasoconstriction persists in the human transplanted lung. Clin Sci (Lond) 1987;72:283–7. doi: 10.1042/cs0720283. [DOI] [PubMed] [Google Scholar]
- 24.Arai TJ, Henderson AC, Dubowitz DJ, Levin DL, Friedman PJ, Buxton RB, et al. Hypoxic pulmonary vasoconstriction does not contribute to pulmonary blood flow heterogeneity in normoxia in normal supine humans. J Appl Physiol (1985) 2009;106:1057–64. doi: 10.1152/japplphysiol.90759.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tawhai MH, Clark AR, Burrowes KS. Computational models of the pulmonary circulation: Insights and the move towards clinically directed studies. Pulm Circ. 2011;1:224–38. doi: 10.4103/2045-8932.83452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naeije R. Pulmonary circulation in hypoxia. Int J Sports Med. 1992;13(Suppl 1):S27–30. doi: 10.1055/s-2007-1024584. [DOI] [PubMed] [Google Scholar]
- 27.National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–75. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 28.Marshall BE, Marshall C, Benumof J, Saidman LJ. Hypoxic pulmonary vasoconstriction in dogs: Effects of lung segment size and oxygen tension. J Appl Physiol Respir Environ Exerc Physiol. 1981;51:1543–51. doi: 10.1152/jappl.1981.51.6.1543. [DOI] [PubMed] [Google Scholar]
- 29.Ketabchi F, Egemnazarov B, Schermuly RT, Ghofrani HA, Seeger W, Grimminger F, et al. Effects of hypercapnia with and without acidosis on hypoxic pulmonary vasoconstriction. Am J Physiol Lung Cell Mol Physiol. 2009;297:L977–83. doi: 10.1152/ajplung.00074.2009. [DOI] [PubMed] [Google Scholar]
- 30.Sicard D, Haak AJ, Choi KM, Craig AR, Fredenburgh LE, Tschumperlin DJ. Aging and anatomical variations in lung tissue stiffness. Am J Physiol Lung Cell Mol Physiol. 2018;314:L946–55. doi: 10.1152/ajplung.00415.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balanos GM, Pugh K, Frise MC, Dorrington KL. Exaggerated pulmonary vascular response to acute hypoxia in older men. Exp Physiol. 2015;100:1187–98. doi: 10.1113/EP085403. [DOI] [PubMed] [Google Scholar]
- 32.Riley RL, Cournand A. Ideal alveolar air and the analysis of ventilation-perfusion relationships in the lungs. J Appl Physiol. 1949;1:825–47. doi: 10.1152/jappl.1949.1.12.825. [DOI] [PubMed] [Google Scholar]
- 33.West JB. Regional differences in gas exchange in the lung of erect man. J Appl Physiol. 1962;17:893–8. doi: 10.1152/jappl.1962.17.6.893. [DOI] [PubMed] [Google Scholar]
- 34.Grant BJ. Effect of local pulmonary blood flow control on gas exchange: Theory. J Appl Physiol Respir Environ Exerc Physiol. 1982;53:1100–9. doi: 10.1152/jappl.1982.53.5.1100. [DOI] [PubMed] [Google Scholar]
- 35.Nyren S, Radell P, Mure M, Petersson J, Jacobsson H, Lindahl SG, et al. Inhalation anesthesia increases V/Q regional heterogeneity during spontaneous breathing in healthy subjects. Anesthesiology. 2010;113:1370–5. doi: 10.1097/ALN.0b013e3181fc5788. [DOI] [PubMed] [Google Scholar]
- 36.Tokics L, Hedenstierna G, Svensson L, Brismar B, Cederlund T, Lundquist H, et al. V/Q distribution and correlation to atelectasis in anesthetized paralyzed humans. J Appl Physiol (1985) 1996;81:1822–33. doi: 10.1152/jappl.1996.81.4.1822. [DOI] [PubMed] [Google Scholar]
- 37.Duggan M, Kavanagh BP. Pulmonary atelectasis: A pathogenic perioperative entity. Anesthesiology. 2005;102:838–54. doi: 10.1097/00000542-200504000-00021. [DOI] [PubMed] [Google Scholar]
- 38.Wieslander B, Ramos JG, Ax M, Petersson J, Ugander M. Supine, prone, right and left gravitational effects on human pulmonary circulation. J Cardiovasc Magn Reson. 2019;21:69. doi: 10.1186/s12968-019-0577-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bardoczky GI, Szegedi LL, d'Hollander AA, Moures JM, de Francquen P, Yernault JC. Two-lung and one-lung ventilation in patients with chronic obstructive pulmonary disease: The effects of position and F(IO)2. Anesth Analg. 2000;90:35–41. doi: 10.1097/00000539-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Liu TJ, Shih MS, Lee WL, Wang KY, Liu CN, Hung CJ, et al. Hypoxemia during one-lung ventilation for robot-assisted coronary artery bypass graft surgery. Ann Thorac Surg. 2013;96:127–32. doi: 10.1016/j.athoracsur.2013.04.017. [DOI] [PubMed] [Google Scholar]
- 41.Campos JH, Feider A. Hypoxia during one-lung ventilation-A review and update. J Cardiothorac Vasc Anesth. 2018;32:2330–8. doi: 10.1053/j.jvca.2017.12.026. [DOI] [PubMed] [Google Scholar]
- 42.Hambraeus-Jonzon K, Bindslev L, Mellgard AJ, Hedenstierna G. Hypoxic pulmonary vasoconstriction in human lungs. A stimulus-response study. Anesthesiology. 1997;86:308–15. doi: 10.1097/00000542-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Slinger PD, Hickey DR. The interaction between applied PEEP and auto-PEEP during one-lung ventilation. J Cardiothorac Vasc Anesth. 1998;12:133–6. doi: 10.1016/s1053-0770(98)90318-4. [DOI] [PubMed] [Google Scholar]
- 44.Spadaro S, Grasso S, Karbing DS, Fogagnolo A, Contoli M, Bollini G, et al. Physiologic evaluation of ventilation perfusion mismatch and respiratory mechanics at different positive end-expiratory pressure in patients undergoing protective one-lung ventilation. Anesthesiology. 2018;128:531–8. doi: 10.1097/ALN.0000000000002011. [DOI] [PubMed] [Google Scholar]
- 45.Benumof JL. Mechanism of decreased blood flow to atelectatic lung. J Appl Physiol Respir Environ Exerc Physiol. 1979;46:1047–8. doi: 10.1152/jappl.1979.46.6.1047. [DOI] [PubMed] [Google Scholar]
- 46.Eisenkraft JB. Effects of anaesthetics on the pulmonary circulation. Br J Anaesth. 1990;65:63–78. doi: 10.1093/bja/65.1.63. [DOI] [PubMed] [Google Scholar]
- 47.Bjertnaes LJ. Hypoxia-induced vasoconstriction in isolated perfused lungs exposed to injectable or inhalation anesthetics. Acta Anaesthesiol Scand. 1977;21:133–47. doi: 10.1111/j.1399-6576.1977.tb01203.x. [DOI] [PubMed] [Google Scholar]
- 48.Nakayama M, Murray PA. Ketamine preserves and propofol potentiates hypoxic pulmonary vasoconstriction compared with the conscious state in chronically instrumented dogs. Anesthesiology. 1999;91:760–71. doi: 10.1097/00000542-199909000-00029. [DOI] [PubMed] [Google Scholar]
- 49.Pang QY, An R, Liu HL. Effects of inhalation and intravenous anesthesia on intraoperative cardiopulmonary function and postoperative complications in patients undergoing thoracic surgery. Minerva Anestesiol. 2018;84:1287–97. doi: 10.23736/S0375-9393.18.12501-6. [DOI] [PubMed] [Google Scholar]
- 50.Volta CA, Alvisi V, Petrini S, Zardi S, Marangoni E, Ragazzi R, et al. The effect of volatile anesthetics on respiratory system resistance in patients with chronic obstructive pulmonary disease. Anesth Analg. 2005;100:348–53. doi: 10.1213/01.ANE.0000140240.83236.AC. [DOI] [PubMed] [Google Scholar]
- 51.Sun B, Wang J, Bo L, Zang Y, Gu H, Li J, et al. Effects of volatile vs.propofol-based intravenous anesthetics on the alveolar inflammatory responses to one-lung ventilation: A meta-analysis of randomized controlled trials. J Anesth. 2015;29:570–9. doi: 10.1007/s00540-015-1987-y. [DOI] [PubMed] [Google Scholar]
- 52.Collins SR, Blank RS, Deatherage LS, Dull RO. Special article: The endothelial glycocalyx: Emerging concepts in pulmonary edema and acute lung injury. Anesth Analg. 2013;117:664–74. doi: 10.1213/ANE.0b013e3182975b85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bjertnaes L, Hauge A, Kriz M. Hypoxia-induced pulmonary vasoconstriction: Effects of fentanyl following different routes of administration. Acta Anaesthesiol Scand. 1980;24:53–7. doi: 10.1111/j.1399-6576.1980.tb01504.x. [DOI] [PubMed] [Google Scholar]
- 54.Gibbs JM, Johnson H. Lack of effect of morphine and buprenorphine on hypoxic pulmonary vasoconstriction in the isolated perfused cat lung and the perfused lobe of the dog lung. Br J Anaesth. 1978;50:1197–201. doi: 10.1093/bja/50.12.1197. [DOI] [PubMed] [Google Scholar]
- 55.Huang SQ, Zhang J, Zhang XX, Liu L, Yu Y, Kang XH, et al. Can dexmedetomidine improve arterial oxygenation and intrapulmonary shunt during one-lung ventilation in adults undergoing thoracic surgery? A meta-analysis of randomized, placebo-controlled trials. Chin Med J (Engl) 2017;130:1707–14. doi: 10.4103/0366-6999.209891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kernan S, Rehman S, Meyer T, Bourbeau J, Caron N, Tobias JD. Effects of dexmedetomidine on oxygenation during one-lung ventilation for thoracic surgery in adults. J Minim Access Surg. 2011;7:227–31. doi: 10.4103/0972-9941.85645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee SH, Kim N, Lee CY, Ban MG, Oh YJ. Effects of dexmedetomidine on oxygenation and lung mechanics in patients with moderate chronic obstructive pulmonary disease undergoing lung cancer surgery: A randomised double-blinded trial. Eur J Anaesthesiol. 2016;33:275–82. doi: 10.1097/EJA.0000000000000405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y, Liu Y, Huang H, Zhu Y, Zhang Y, Lu F, et al. Dexmedetomidine inhibits inflammatory reaction in lung tissues of septic rats by suppressing TLR4/NF-kappaB pathway? Mediators Inflamm. 2013;2013:562154. doi: 10.1155/2013/562154. doi: 10.1155/2013/562154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xia R, Xu J, Yin H, Wu H, Xia Z, Zhou D, et al. Intravenous infusion of dexmedetomidine combined isoflurane inhalation reduces oxidative stress and potentiates hypoxia pulmonary vasoconstriction during one-lung ventilation in patients? Mediators Inflamm. 2015;2015:238041. doi: 10.1155/2015/238041. doi: 10.1155/2015/238041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Weir EK, McMurtry IF, Tucker A, Reeves JT, Grover RF. Prostaglandin synthetase inhibitors do not decrease hypoxic pulmonary vasoconstriction. J Appl Physiol. 1976;41:714–8. doi: 10.1152/jappl.1976.41.5.714. [DOI] [PubMed] [Google Scholar]
- 61.Su CL, Yuan DW, Chiang LL, Lee HL, Chen KH, Wang D. Inducible cyclooxygenase expression mediating hypoxia/reoxygenation-induced pulmonary vasoconstriction is attenuated by a cyclooxygenase inhibitor in rats. Transplant Proc. 2012;44:929–32. doi: 10.1016/j.transproceed.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 62.Kylhammar D, Radegran G. The principal pathways involved in the in vivo modulation of hypoxic pulmonary vasoconstriction, pulmonary arterial remodelling and pulmonary hypertension. Acta Physiol (Oxf) 2017;219:728–56. doi: 10.1111/apha.12749. [DOI] [PubMed] [Google Scholar]
- 63.Bryan TL, van Diepen S, Bhutani M, Shanks M, Welsh RC, Stickland MK. The effects of dobutamine and dopamine on intrapulmonary shunt and gas exchange in healthy humans. J Appl Physiol (1985) 2012;113:541–8. doi: 10.1152/japplphysiol.00404.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tanaka M, Dohi S. Effects of phenylephrine and ephedrine on pulmonary arterial pressure in patients with cervical or lumbar epidural anesthesia, or enflurane anesthesia. J Anesth. 1994;8:125–31. doi: 10.1007/BF02514698. [DOI] [PubMed] [Google Scholar]
- 65.Doering EB, Hanson CW, 3rd, Reily DJ, Marshall C, Marshall BE. Improvement in oxygenation by phenylephrine and nitric oxide in patients with adult respiratory distress syndrome. Anesthesiology. 1997;87:18–25. doi: 10.1097/00000542-199707000-00004. [DOI] [PubMed] [Google Scholar]
- 66.Tal A, Pasterkamp H, Leahy F. Arterial oxygen desaturation following salbutamol inhalation in acute asthma. Chest. 1984;86:868–9. doi: 10.1378/chest.86.6.868. [DOI] [PubMed] [Google Scholar]
- 67.Kiely DG, Cargill RI, Lipworth BJ. Angiotensin II receptor blockade and effects on pulmonary hemodynamics and hypoxic pulmonary vasoconstriction in humans. Chest. 1996;110:698–703. doi: 10.1378/chest.110.3.698. [DOI] [PubMed] [Google Scholar]
- 68.Stanek EJ, Nara AR, Strohl KP, Nair RN, Decker MJ, Munger MA. Effect of long-term angiotensin-converting enzyme inhibitor therapy on arterial oxygen saturation in patients with mild to moderate heart failure. Pharmacotherapy. 1994;14:321–9. [PubMed] [Google Scholar]
- 69.Vincent JL, Lignian H, Gillet JB, Berre J, Contu E. Increase in PaO2 following intravenous administration of propranolol in acutely hypoxemic patients. Chest. 1985;88:558–62. doi: 10.1378/chest.88.4.558. [DOI] [PubMed] [Google Scholar]
- 70.Pellett AA, Cairo JM, Levitzky MG. Hypoxemia and hypoxic pulmonary vasoconstriction: Autonomic nervous system versus mixed venous PO2. Respir Physiol. 1997;109:249–60. doi: 10.1016/s0034-5687(97)00055-8. [DOI] [PubMed] [Google Scholar]
- 71.Gorecka D, Sliwinski P, Palasiewicz G, Pachocki R, Zielinski J Almitrine Study Group. Effects of almitrine bismesylate on arterial blood gases in patients with chronic obstructive pulmonary disease and moderate hypoxaemia: A multicentre, randomised, double-blind, placebo-controlled study. Respiration. 2003;70:275–83. doi: 10.1159/000072009. [DOI] [PubMed] [Google Scholar]
- 72.Roch A, Hraiech S, Dizier S, Papazian L. Pharmacological interventions in acute respiratory distress syndrome. Ann Intensive Care. 2013;3:20. doi: 10.1186/2110-5820-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bermejo S, Gallart L, Silva-Costa-Gomes T, Valles J, Aguilo R, Puig MM. Almitrine fails to improve oxygenation during one-lung ventilation with sevoflurane anesthesia. J Cardiothorac Vasc Anesth. 2014;28:919–24. doi: 10.1053/j.jvca.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 74.Silva-Costa-Gomes T, Gallart L, Valles J, Trillo L, Minguella J, Puig MM. Low- vs high-dose almitrine combined with nitric oxide to prevent hypoxia during open-chest one-lung ventilation. Br J Anaesth. 2005;95:410–6. doi: 10.1093/bja/aei194. [DOI] [PubMed] [Google Scholar]
- 75.Dalibon N, Moutafis M, Liu N, Law-Koune JD, Monsel S, Fischler M. Treatment of hypoxemia during one-lung ventilation using intravenous almitrine. Anesth Analg. 2004;98:590–4. doi: 10.1213/01.ane.0000099715.40831.2a. table of contents. [DOI] [PubMed] [Google Scholar]
- 76.Freise H, Van Aken HK. Risks and benefits of thoracic epidural anaesthesia. Br J Anaesth. 2011;107:859–68. doi: 10.1093/bja/aer339. [DOI] [PubMed] [Google Scholar]
- 77.Licker M, Spiliopoulos A, Tschopp JM. Influence of thoracic epidural analgesia on cardiovascular autonomic control after thoracic surgery. Br J Anaesth. 2003;91:525–31. doi: 10.1093/bja/aeg212. [DOI] [PubMed] [Google Scholar]
- 78.Garutti I, Quintana B, Olmedilla L, Cruz A, Barranco M, Garcia de Lucas E. Arterial oxygenation during one-lung ventilation: Combined versus general anesthesia. Anesth Analg. 1999;88:494–9. doi: 10.1097/00000539-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 79.Jung SM, Cho CK, Kim YJ, Cho HM, Kim CW, Kwon HU, et al. The effect of thoracic epidural anesthesia on pulmonary shunt fraction and arterial oxygenation during one-lung ventilation. J Cardiothorac Vasc Anesth. 2010;24:456–62. doi: 10.1053/j.jvca.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 80.Ozcan PE, Senturk M, Sungur Ulke Z, Toker A, Dilege S, Ozden E, et al. Effects of thoracic epidural anaesthesia on pulmonary venous admixture and oxygenation during one-lung ventilation. Acta Anaesthesiol Scand. 2007;51:1117–22. doi: 10.1111/j.1399-6576.2007.01374.x. [DOI] [PubMed] [Google Scholar]
- 81.Casati A, Mascotto G, Iemi K, Nzepa-Batonga J, De Luca M. Epidural block does not worsen oxygenation during one-lung ventilation for lung resections under isoflurane/nitrous oxide anaesthesia. Eur J Anaesthesiol. 2005;22:363–8. doi: 10.1017/s0265021505000621. [DOI] [PubMed] [Google Scholar]
- 82.Xu Y, Tan Z, Wang S, Shao H, Zhu X. Effect of thoracic epidural anesthesia with different concentrations of ropivacaine on arterial oxygenation during one-lung ventilation. Anesthesiology. 2010;112:1146–54. doi: 10.1097/ALN.0b013e3181d40347. [DOI] [PubMed] [Google Scholar]
- 83.Licker M. Anaesthetic management and unplanned admission to intensive care after thoracic surgery. Anaesthesia. 2019;74:1083–6. doi: 10.1111/anae.14741. [DOI] [PubMed] [Google Scholar]
- 84.Jiao XF, Lin XM, Ni XF, Li HL, Zhang C, Yang CS, et al. Volatile anesthetics versus total intravenous anesthesia in patients undergoing coronary artery bypass grafting: An updated meta-analysis and trial sequential analysis of randomized controlled trials. PLoS One. 2019;14:e0224562. doi: 10.1371/journal.pone.0224562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Landoni G, Lomivorotov VV, Nigro Neto C, Monaco F, Pasyuga VV, Bradic N, et al. Volatile anesthetics versus total intravenous anesthesia for cardiac surgery. N Engl J Med. 2019;380:1214–25. doi: 10.1056/NEJMoa1816476. [DOI] [PubMed] [Google Scholar]
- 86.Grabitz SD, Farhan HN, Ruscic KJ, Timm FP, Shin CH, Thevathasan T, et al. Dose-dependent protective effect of inhalational anesthetics against postoperative respiratory complications: A prospective analysis of data on file from three hospitals in New England. Crit Care Med. 2017;45:e30–9. doi: 10.1097/CCM.0000000000002015. [DOI] [PubMed] [Google Scholar]
- 87.Wigmore TJ, Mohammed K, Jhanji S. Long-term survival for patients undergoing volatile versus IV anesthesia for cancer surgery: A retrospective analysis. Anesthesiology. 2016;124:69–79. doi: 10.1097/ALN.0000000000000936. [DOI] [PubMed] [Google Scholar]
- 88.Sekandarzad MW, van Zundert AAJ, Lirk PB, Doornebal CW, Hollmann MW. Perioperative anesthesia care and tumor progression. Anesth Analg. 2017;124:1697–708. doi: 10.1213/ANE.0000000000001652. [DOI] [PubMed] [Google Scholar]
- 89.Longhini F, Bruni A, Garofalo E, De Sarro R, Memeo R, Navalesi P, et al. Anesthetic strategies in oncological surgery: Not only a simple sleep, but also impact on immunosuppression and cancer recurrence. Cancer Manag Res. 2020;12:931–40. doi: 10.2147/CMAR.S237224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xu Y, Pan S, Jiang W, Xue F, Zhu X. Effects of propofol on the development of cancer in humans. Cell Prolif. 2020;53:e12867. doi: 10.1111/cpr.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Beilin B, Rusabrov Y, Shapira Y, Roytblat L, Greemberg L, Yardeni IZ, et al. Low-dose ketamine affects immune responses in humans during the early postoperative period. Br J Anaesth. 2007;99:522–7. doi: 10.1093/bja/aem218. [DOI] [PubMed] [Google Scholar]
- 92.Yap A, Lopez-Olivo MA, Dubowitz J, Hiller J, Riedel B Global Onco-Anesthesia Research Collaboration Group. Anesthetic technique and cancer outcomes: A meta-analysis of total intravenous versus volatile anesthesia. Can J Anaesth. 2019;66:546–61. doi: 10.1007/s12630-019-01330-x. [DOI] [PubMed] [Google Scholar]
- 93.Eichhorn JH. Effect of monitoring standards on anesthesia outcome. Int Anesthesiol Clin. 1993;31:181–96. doi: 10.1097/00004311-199331030-00012. [DOI] [PubMed] [Google Scholar]
- 94.Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation: Prediction, prevention, and treatment. Anesthesiology. 2009;110:1402–11. doi: 10.1097/ALN.0b013e31819fb15d. [DOI] [PubMed] [Google Scholar]
- 95.Zhang W, Chen M, Li H, Yuan J, Li J, Wu F, et al. Hypoxia preconditioning attenuates lung injury after thoracoscopic lobectomy in patients with lung cancer: A prospective randomized controlled trial. BMC Anesthesiol. 2019;19:209. doi: 10.1186/s12871-019-0854-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Feiner JR, Weiskopf RB. Evaluating pulmonary function: An assessment of PaO2/FIO2. Crit Care Med. 2017;45:e40–8. doi: 10.1097/CCM.0000000000002017. [DOI] [PubMed] [Google Scholar]
- 97.Benatar SR, Hewlett AM, Nunn JF. The use of iso-shunt lines for control of oxygen therapy. Br J Anaesth. 1973;45:711–8. doi: 10.1093/bja/45.7.711. [DOI] [PubMed] [Google Scholar]
- 98.Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, et al. Lung-protective ventilation for the surgical patient: International expert panel-based consensus recommendations. Br J Anaesth. 2019;123:898–913. doi: 10.1016/j.bja.2019.08.017. [DOI] [PubMed] [Google Scholar]
- 99.Jung DM, Ahn HJ, Jung SH, Yang M, Kim JA, Shin SM, et al. Apneic oxygen insufflation decreases the incidence of hypoxemia during one-lung ventilation in open and thoracoscopic pulmonary lobectomy: A randomized controlled trial. J Thorac Cardiovasc Surg. 2017;154:360–6. doi: 10.1016/j.jtcvs.2017.02.054. [DOI] [PubMed] [Google Scholar]