Abstract
Background:
Modern oil development frequently occurs in close proximity to human populations. Los Angeles, California is home to the largest urban oil field in the country with thousands of active oil and gas wells in very close proximity to homes, schools and parks, yet little is known about potential health impacts. The neighborhoods along the Las Cienagas oil fields are situated in South LA, densely populated by predominantly low-income Black and Latinx families, many of whom are primarily Spanish-speakers.
Methods:
A cross-sectional community-based study was conducted between January 2017 and August 2019 among residents living <1000 m from two oil wells (one active, one idle) in the Las Cienagas oil field. We collected self-reported acute health symptoms and measured FEV1 (forced expiratory volume in the first second of exhalation) and FVC (forced vital capacity). We related lung function measures to distance and direction from an oil and gas development site using generalized linear models adjusted for covariates.
Results:
A total of 961 residents from two neighborhoods participated, the majority of whom identify as Latinx. Participants near active oil development reported significantly higher prevalence of wheezing, eye and nose irritation, sore throat and dizziness in the past 2 weeks. Among 747 valid spirometry tests, we observe that living near (less than 200m) of oil operations was associated with, on average, −112 mL lower FEV1 (95% CI: −213, -q=10) and −128 mL lower FVC (95% CI: −252, −5) compared to residents living more than 200m from the sites after adjustments for covariates, including age, sex, height, proximity to freeway, asthma status and smoking status. When accounting for predominant wind direction and proximity, we observe that residents living downwind and less than 200m from oil operations have, on average, −414 mL lower FEV1 (95% CI: −636, −191) and −400 mL lower FVC (95% CI: −652, −147) compared to residents living upwind and more than 200m from the wells.
Conclusions:
Living nearby and downwind of urban oil and gas development sites is associated with lower lung function among residents, which may contribute to environmental health disparities.
Keywords: oil drilling, respiratory health, environmental justice, urban health
1. INTRODUCTION
Modern oil development frequently occurs in close proximity to human populations. Globally, there are approximately 40,000 oil fields1 that have the potential to effect over 600 million people living nearby.2 Over the past decade, oil production in the United States (US) has nearly doubled while natural gas production rose 50% reversing a longstanding decline in production.3 An estimated 8.6 million people live less than 1600 m from an active oil extraction site in the US.4 California (CA), together with Texas, North Dakota, and Alaska account for ~60% of all oil produced domestically. Public health concern has accompanied this rapid growth in oil production.5
As oil and gas development is becoming more common near where people live, work and play, there is an increasing potential for human exposure to contaminants associated with drilling and fossil fuel extraction.6,7 Recent research demonstrates multiple health-hazardous air pollutants associated with petroleum extraction, including particulate matter (PM), nitric oxides (NOx), polyaromatic hydrocarbons, benzene, naphthalene, xylenes, toluene, ethylbenzene, formaldehyde, and sulfuric acid.8 Documented health effects from exposure to such chemicals include symptomatic acute physical and respiratory effects, dizziness, headaches, and fatigue along with respiratory system irritation, including difficulty breathing, and impaired lung function.9,10
While, here are few epidemiological studies related to upstream oil extraction, results from three recent health surveys near natural gas extraction and hydraulic fracturing sites reported symptoms of throat and nasal irritation, eye burning, sinus problems, headaches, skin problems, loss of smell, cough, nosebleeds and stress.11–13 These symptoms were more common in individuals living nearby gas facilities compared to those farther away. Elevated incidence of pediatric asthma hospitalization has been observed among nonurban areas with the highest levels of gas drilling activity.14–16 Survey-based studies documented higher rates of headaches, dizziness, and eyes, nose, throat and skin irritation among residents near oil development compared to people living farther away.17,18 Recent studies in CA and Texas identified adverse birth outcomes associated with oil extraction activities.19,20,21
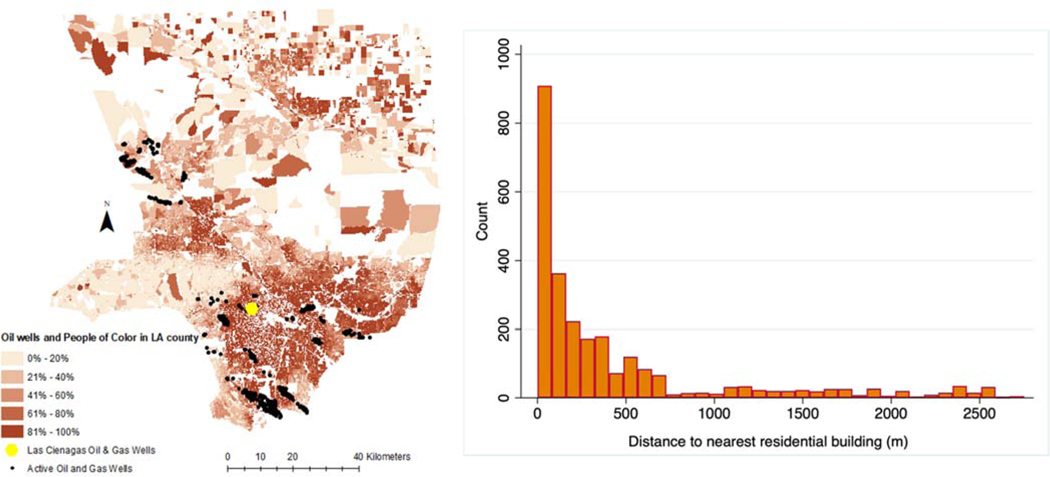
Los Angeles (LA) County, CA, is home to one of the most petroleum-dense basins in the world, with thousands of oil and gas extraction wells spread across multiple oil fields in 70 different communities (Fig 1a).22,23 Approximately 1/3rd of the 10 million LA County residents live <1 mile of an active oil drilling site, and over 500,000 residents live <¼ mile (~400 m).24 Some live as close as 60 feet from active oil operations (Fig 1b).25 Such a dense, diverse population living in close proximity to oil is unmatched across the US.25
Figure 1:
a) Location of active oil wells and people of color (according to 2010 US Census block data) in Los Angeles County. Las Cienagas oil field is shown by the yellow dot. b) Proximity of active oil wells to residential homes in Los Angeles County (graph on right).
The neighborhoods atop the Las Cienagas oil fields are situated in South LA, populated by predominantly low-income Black and Latinx families. Over 90% of residents are people of color (self-identify as Latinx/Hispanic, Black, Asian and/or as a race other than White) and approximately three-quarters of households live below 200% of the federal poverty line.26 According to CalEnviroScreen, CA’s environmental justice screening tool to identify highly vulnerable communities, this area is among the top 10% most disproportionately-environmentally burdened in the state.27 These neighborhoods, when compared to the state, fall into the bottom 20% for educational attainment and among the top 15% for poverty based on CalEnviroScreen metrics. After an upswing in oil production in Las Cienagas oil field, nearby residents began to report adverse acute health symptoms, such as nosebleeds and headaches, ailments that have been described in other areas with oil and gas production.28 Subsequently, one oil and gas development (OGD) site (which consists of multiple production wells) was shuttered by the city of Los Angeles, and is the “idle” site in this study as it was not actively producing oil or gas during the study period. Other sites, including the “active” study site, continued to extract oil from this field. We used community-driven methodology to assess respiratory health among community residents living in two neighborhoods in the Las Cienagas oil field which were within 1000 m of either active or idle OGD sites.
2. METHODS
To examine the possible chronic deleterious effects of oil drilling operations in close proximity to neighborhoods in urban Los Angeles, we analyzed the relationship between OGD sites’ proximity with self-reported acute symptoms and pulmonary function test results among diverse residents. A cross-sectional community-based study was conducted between January 2017 and August 2019 near two oil sites in the Las Cienagas oil field in South Los Angeles, CA. One OGD well site (in the North University Park neighborhood) housed 21 wells which were idle, that is, not actively producing any oil or gas, during the study period. The second OGD well site (in the Jefferson Park neighborhood) had 28 wells at the time of the study and was actively producing oil during the entire study period. The USC research team and Esperanza Community Housing collaborated to train Promotores de Salud (community health workers) in recruitment and research methods. A Promotor de Salud is a community member who is uniquely linked to the cultural and regional connections in the neighborhood and this local, networked approach offers an innovative model that provides culturally accessible health education for low-income communities of color and supports changes for improved health.29–32 We partnered with skilled community promotores for recruitment in this neighborhood-based study. USC researchers and community partners went to local elementary schools, churches and door to door to distribute recruitment flyers, answer questions and invite residents to participate in the study. Flyers were posted in apartment buildings and distributed to school children when permission was granted. To be eligible, participants were at least 6 years old, spoke English, Spanish or Korean, and lived within 1000 m of one of the OGD sites of interest for at least two years. Multiple participants per household were eligible to participate if they met the inclusion criteria. Among the potential eligible participants that spoke a community promotor, 74% agreed to participate in the study. Written informed consent was obtained from all participants 18 years of age or older, assent and parental consent were obtained from all participants younger than 18 years. All protocols, consent forms, and survey materials were approved by the University of Southern California Institutional Review Board. Participants who provided written consent completed a baseline demographic and health questionnaire, reported acute symptoms over the past two weeks, and provided physiological measurements.
2.1. Health Questionnaire.
If participants were under the age of 13, the parent/guardian completed the questionnaire. The questions were based on validated questionnaires from the Southern CA respiratory health study33 and adapted for accessibility and cultural relevance based on input from the promotores and Esperanza. The questionnaire was administered in the participant’s preferred language (Spanish, English or Korean) and asked sociodemographic information, race/ethnicity, sex, age, tobacco exposure (e.g. smoking history, current smoking practices, presence of indoor environmental tobacco smoke), occupation and residential history. We collected information about disease history, including if the participant ever had a doctor-diagnosis of asthma. The participant was considered to have allergic rhinitis if answered affirmative to the question “Have you ever had hay fever?”.
2.2. Acute symptoms survey.
We asked questions regarding acute irritant and physical symptoms experienced during the previous two weeks, leveraging survey tools developed in partnerships with communities near nuisance industries.34,35 We considered the following acute symptoms: respiratory (wheezing or whistling of the chest, coughing every morning, sleep disturbed by wheezing, sore throat, chest tightness, or runny nose), mucous-membrane irritation (burning, tearing, or irritated eyes, burning or irritated nose), neurological (dizziness, headache, fatigue, ringing of the ears, seizure), gastrointestinal (nausea or vomiting, diarrhea), and as well as others (nosebleeds, backache, rash). Some symptoms that we considered to be unrelated to airborne emissions (e.g. backache, vomiting, diarrhea, cold/flu) were included to address the possibility that residents might report excessive symptoms due to possible negative feelings about the well sites. These questions were collected on a scale with 4 categories within the past two weeks (“not at all”, “once or twice”, “a few times per week”or “daily”). We dichotomized the response into any symptom (Yes) or not at all (No) categories for interpretability and analysis purposes.
2.3. Lung function measurements.
Lung function was assessed using a commercially available spirometer (ndd Easy-On PC, Andover MA) by trained study staff. Maximal-effort spirometry was overseen by trained personnel following American Thoracic Society criteria. Three to 7 blows were performed by each participant to establish consistency, representativeness, and performance credibility. Multiple variables were automatically collected and logged using the ndd software; FEV1 (forced expiratory volume in the first second of exhalation), FVC (forced vital capacity), and MMEF (maximal mid-expiratory flow). We focused on FEV1 and FVC as both measures are established as strong and independent predictors of respiratory disease, cardiovascular mortality and all-cause mortality.36–39 Each participant’s height (to nearest 0.1 cm) and weight (0.1 lbs) was also measured. Finally, each participant was asked if they had cold or flu symptoms within the past 72 hours (defined as the presence of cough, fever, sore throat, and/or runny or stuffy nose).
2.4. Statistical Analysis.
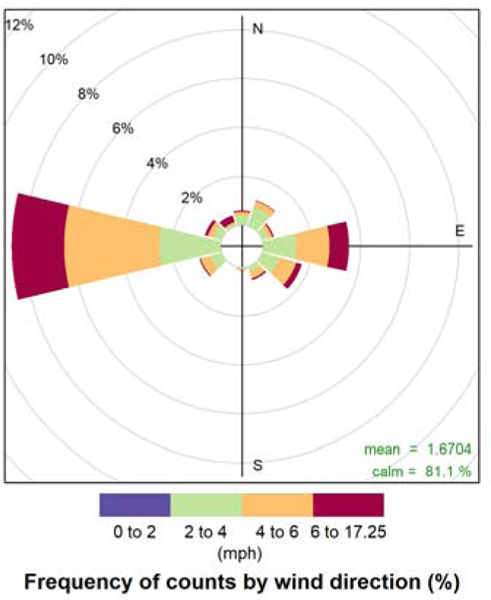
We evaluated participant characteristics by neighborhood and variable distributions. We found the continuous spirometry data to approximate a normal distribution and proceeded with untransformed variables for subsequent analyses. Various representations of oil-well related exposures were then constructed. We assessed differences based on neighborhood (Model 1) and then distance from the oil well using a binary indicator of whether the participants’ home was near (<200 m) versus farther (200–1000m) from an oil well (Model 2). The selection of 200m for the main analysis was chosen based on a changing relationship observed between distance and lung function among study participants (Figure S1). Then, we constructed a 4-level categorical exposure variable accounting for predominant wind direction and distance from the well site: living upwind and more than 200 m from OGD wells (reference); living upwind and within 200 m; living downwind and more than 200 m; and living downwind and within 200 m (Model 3). In addition, we considered models with distance modeled as a continuous variable using a lognormal transformation (Model 4). Predominant wind direction in the LA basin is from the west to the east which we confirmed using 5 years (Jan 2015 – Jan 2020) of wind speed and direction data from a nearby meteorological station (see Figure 3). Prior studies have observed high pollution concentrations and gradients on the east side of freeways40,41 and downwind (east) of the OGD facilities.42 Sensitivity analysis for lung function outcomes was also assessed at 150m and 400m.
Figure 3:
Wind rose showing wind direction and speed based on 5 years of data (Jan 2015 – Jan 2020) from a meteorological station located at the USC University Park Campus, <5 km from the study sites. Direction was reported when wind speeds were >0 mph.
A list of potential confounders was determined a priori from the available survey variables based on previous literature and biological plausibility.43 Logistic models for the presence of acute respiratory symptoms were adjusted for sex (male/female), age group (<18, 18–60, >60), race/ethnicity (Hispanic/Latinx, Black or Asian), dichotomized residential distance to freeway (<200 m), season (winter, spring, summer or fall), baseline asthma status (yes/no), ever smoker (yes/no), reported indoor environmental tobacco smoke (yes/no), recent flu or cold symptoms (yes/no) and neighborhood. A random effect for household (based on address) was included to account for multiple participants from the same residential address. Using generalized linear models, we examined the relationship between lung function and proximity to oil wells adjusted for age (polynomial spline with 3 degrees of freedom), sex (male/female), race/ethnicity, baseline asthma status (yes/no), ever smoker (yes/no), reported indoor environmental tobacco smoke (yes/no), recent flu or cold symptoms (yes/no), dichotomized residential distance to freeway (<200 m), height (m), weight (lbs), neighborhood and interactions between age and height, and age and sex. We further examined the effect of distance and direction from the oil well site (using the 4-level categorical exposure variable) on measured FEV1 and FVC in a model stratified by neighborhood.
Finally, we conducted a subgroup analysis based on age groups, sex, race/ethnicity and asthma status. All analyses assumed a 2-sided alternative hypothesis at a 0.05 level of significance. All statistical analyses were conducted using R statistical computing language (R Core Team, 2020) version 3.6.2.
3. RESULTS
3.1. Characteristics of the Study Population.
A total of 972 residents participated in this study to measure lung function and self-reported acute mental and physical health symptoms from 488 distinct addresses (Table 1). 11 participants were subsequently excluded for living outside of the study area after subsequent confirmation of residential address. The mean age of the participants was 39 years with 29% of the participants being children (<18 years) and 22% over the age of 60. The majority (62%) were female and 100% identified as people of color including 792 Hispanic/Latinx, 115 Black/ African Americans, and 54 Asians/ Asian Americans (51 identified as Korean and 3 as South Asian). On average, participants had lived in the neighborhood for 19 years. 68% of the participants completed the survey in Spanish. Overall, 15% of participants reported a doctor diagnosis of asthma. 21% of participants were ever smokers and 6% reported environmental tobacco smoke inside of the home. More than 70% of participants were nonworkers (e.g. students, homemaker, retired or unemployed). The median distance from the respective well sites to residences was 291 meters. Participants living near the neighborhood with the active drill site were, on average, slightly older and more diverse in terms of race/ethnicity as well as more likely to have ever smoked cigarettes. A total of 288 people lived near (<200m) an oil well site.
Table 1.
Characteristics of participants by neighborhood and well proximity.
| North University Park (idle) N=441 |
Jefferson Park (active) N=520 |
Near Well (<200 m) N=288 |
Farther from Well (>200 – 1000m) N=673 |
|
|---|---|---|---|---|
| Age categories, N (%): | ||||
| 9 – 18 | 138 (31.3%) | 136 (26.2%) | 56 (19.4%) | 218 (32.4%) |
| 18–60 | 243 (55.1%) | 212 (40.8%) | 133 (46.2%) | 322 (47.8%) |
| 60 < | 60 (13.6%) | 172 (33.1%) | 99 (34.4%) | 133 (19.8%) |
| Gender, N (%): | ||||
| Female | 286 (64.9%) | 310 (59.5%) | 180 (62.5%) | 416 (61.7%) |
| Male | 155 (35.1%) | 210 (40.5%) | 108 (37.5%) | 257 (38.2%) |
| Race/Ethnicity, N (%): | ||||
| Asian/ Asian American | 2 (0.4%) | 52 (10.0%) | 48 (16.7%) | 6 (0.9%) |
| Black/ African American | 6 (1.4%) | 109 (21.0%) | 40 (13.9%) | 75 (11.1%) |
| Hispanic or Latinx | 433(98.2%) | 359 (69.0%) | 200 (69.4%) | 592 (88.0%) |
| Employed, N (%) | 132 (29.9%) | 144 (27.7%) | 74 (25.7%) | 202 (30.0%) |
| Duration (years) of residence in the neighborhood, Median [25th;75th] | 10.0 [5.0;17.0] | 24.5 [12.0;40.0] |
14.0 [7.0;27.0] |
14.0 [7.0;33.0] |
| Ever smoker, N (%) | 70 (15.9%) | 138 (26.5%) | 74 (25.7%) | 134 (19.9%) |
| Current smoker, N (%) | 19 (4.3%) | 35 (6.7%) | 16 (5.6%) | 38 (5.6%) |
| Exposed to environmental tobacco smoke, N (%) | 38 (8.6%) | 21 (4.0%) | 17 (5.9%) | 42 (6.2%) |
| Allergic rhinitis / Hay fever, N (%) | 71 (16.1%) | 132 (25.4%) | 78 (27.1%) | 125 (18.6%) |
| Doctor diagnosis of asthma, N (%) | 57 (12.9%) | 85 (16.3%) | 50 (17.4%) | 92 (13.7%) |
| Distance to the closest freeway, N (%): | ||||
| ≥ 200m – 1000m | 235 (53.3%) | 480 (92.3%) | 228 (79.2%) | 487 (72.4%) |
| < 200m | 206 (46.9%) | 40 (7.7%) | 60 (20.8%) | 186 (27.6%) |
| Distance from well, m, Mean (SD) | 308 (224) | 380 (238) | 162 (42) | 396 (156) |
| Distance from well, categorial, N (%) | ||||
| ≥ 200m – 1000m | 268 (60.8%) | 405 (77.9%) | -- | 673 (100%) |
| < 200m | 173 (39.2%) | 115 (22.1%) | 288 (100%) | -- |
| Direction from well, N (%) | ||||
| Upwind | 174 (39.5%) | 175 (33.3%) | 55 (19.1%) | 294 (43.4%) |
| Downwind | 267 (60.5%) | 345 (66.3%) | 233 (80.9%) | 379 (56.3%) |
|
| ||||
| Households, N | 205 | 283 | 163 | 325 |
3.2. Self Reported Acute Symptoms.
Participants living in the neighborhood with the active OGD wells reported significantly higher prevalence of recent wheeze, daily morning cough, eye irritation, dizziness, fatigue, backache and rash in the past 2 weeks (Table 2) compared to participants living near the idle OGD wells (n=960). However, we did not observe differences in respiratory symptoms based on proximity to wells, with the exception of sneezing/running nose. Other symptoms unlikely to be related to oil drilling, showed no difference (e.g. trouble hearing, diarrhea) or higher prevalence among the neighborhood with the idle site (e.g. flu or cold symptoms).
Table 2.
Self-reported acute symptoms among participants by neighborhood and well proximity.
| North University Park (idle) |
Jefferson Park (active) |
Near Well (<200m) |
Farther from Well (>200–1000m) |
|
|---|---|---|---|---|
|
|
|
|
|
|
| N = 442 | N = 518 | N = 288 | N = 672 | |
| Wheeze & Bronchitic Symptoms | ||||
| Wheezing/whistling in the chest | 57 (12.9%) | 95 (18.3%) | 50 (17.4%) | 102 (15.2%) |
| Morning cough, eveiy day | 110 (24.9%) | 105 (20.3%)* | 67 (23.2%) | 148 (22.0%) |
| Sleep disturbed by wheeze | 43 (9.7%) | 69 (13.3%) | 39 (13.5%) | 73 (10.9%) |
| Other | ||||
| Respiratory Symptoms | ||||
| Sore throat | 157 (35.5%) | 181 (34.9%) | 91 (31.6%) | 247 (36.8%) |
| Chest tightness | 76 (17.2%) | 112 (21.6%) | 56 (19.4%) | 132 (19.6%) |
| Sneezing or runny nose | 175 (40.0%) | 207 (40.0%) | 132 (45.8%) | 250 (37.2%)* |
| Recent cold or flu symptoms during spirometry | 151 (34.2%) | 98 (18.9%)* | 79 (27.4%) | 170 (25.2%) |
| Mucous-membrane irritation | ||||
| Irritation of the eyes | 184 (41.6%) | 276 (53.3%)* | 144 (50.0%) | 316 (47.0%) |
| Irritation of the nose | 168 (38.0%) | 213 (41.1%) | 117 (40.6%) | 264 (39.3%) |
| Neurological | ||||
| Dizziness | 114 (25.8%) | 176 (34.0%)* | 91 (31.6%) | 199 (29.6%) |
| Headache | 222 (50.2%) | 242 (47.1%) | 130 (45.1%) | 334 (49.7%) |
| Fatigue | 177 (40.0%) | 241 (46.7%)* | 144 (50.0%) | 274 (40.1%)* |
| Ringing of the ears | 125 (26.5%) | 156 (30.1%) | 87 (30.2%) | 194 (28.9%) |
| Seizure | 8 (1.8%) | 6 (1.2%) | 4 (1.4%) | 10 (1.4%) |
| Gastrointestinal | ||||
| Diarrhea | 43 (9.7%) | 78 (15.1%)* | 39 (13.5%) | 82 (12.2%) |
| Nausea or Vomiting | 40 (9.0%) | 53 (10.2%) | 19 (6.6%) | 61 (9.1%) |
| Other | ||||
| Nosebleeds | 45 (10.2%) | 67 (12.9%) | 22 (7.6%) | 90 (13.4%)* |
| Backache | 188 (42.5%) | 251 (48.5%)* | 144 (50.0%) | 295 (43.8%) |
| Rash | 47 (10.6%) | 84 (16.2%)* | 43 (14.9%) | 88 (13.1%) |
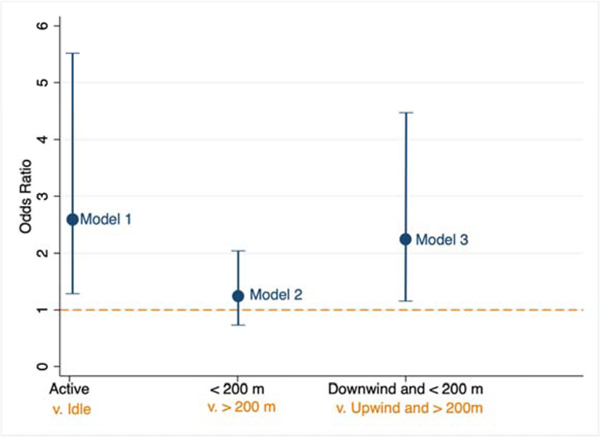
In multivariable logistic regression models, we observe that the participants living in the neighborhood with active oil production wells have 2.6 times higher odds (OR 2.58; 95% CI: 1.19, 5.59) of reporting wheezing in the past two weeks compared to participants living in the neighborhood with idle wells. Living near compared to farther from an oil drill site was not statistically significant (OR 1.20; 95% CI 0.69, 2.13) in the model, although living near and downwind was associated with higher odds of recent wheeze (OR 2.26; 95% CI: 1.14, 4.49, Figure 4, Table S1). In the multivariable models we did not observe consistent significant differences by neighborhood or distance for morning cough (Table S2). We did observe that participants living downwind of the well sites had higher odds of reporting sleep disturbance due to wheezing over the past two weeks (downwind and <200m: OR 2.91, 95% CI 1.20, 7.06, Table S3).
Figure 4:
The odds ratio and 95% confidence interval for recent wheeze for Model 1) participants living in the neighborhood with the active compared to the idle OGD well sites; Model 2) participants living near (<200 m) the OGD well sites compared to those living farther away (200–1000 m); and Model 3) participants living both near (<200 m) and downwind of an OGD well site compared to those living farther (200–1000m) and upwind. All models are adjusted for age, sex, race/ethnicity, asthma diagnosis, recent flu/cold, season, ever smoker, recent exposure to environmental tobacco smoke and living near a freeway. Models include a random effect for residential household.
Among other symptoms analyzed with the adjusted logistic models, we identify significantly higher odds of sore throat (OR 2.04; 95% CI 1.19, 3.51), chest tightness (OR 3.16; 95% CI 1.54, 6.48), irritation of the eyes (OR 3.08; 95% CI 1.775.30), irritation of the nose (OR 2.23; 95% CI 1.31, 3.82), dizziness (OR 3.01; 95% CI 1.53, 5.90) and ringing of the ears (OR 1.74, 95% CI 1.05, 2.88) among residents in the neighborhood with the active drill site. The other symptoms were not statistically significant for neighborhood site in multivariable models, including symptoms thought to be unrelated to the well activity (e.g. backache and trouble hearing) (Table S4). We do not observe proximity alone to be a significant predictor of self-reported acute symptoms after adjusting for neighborhood and other covariates.
3.3. Pulmonary Function Results.
Of the study participants, 919 performed at least one spirometry test. 172 participants were excluded because of restrictions in age (included only participants ages 10 to 85, n=26) or due to invalid/outlier pulmonary function measurements that did not meet the ATS criteria (n=146). Mean FEV1 and FVC for males were 2773 mL and 3654 mL, respectively, and the corresponding means for females were 2220 mL and 2875 mL.
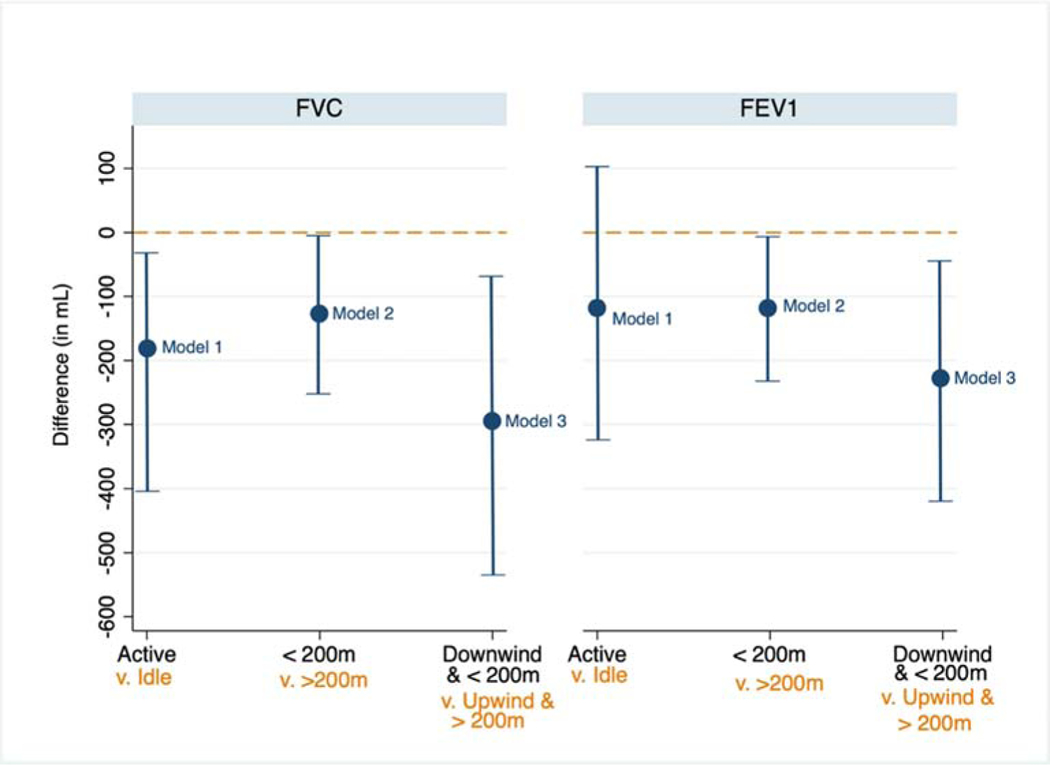
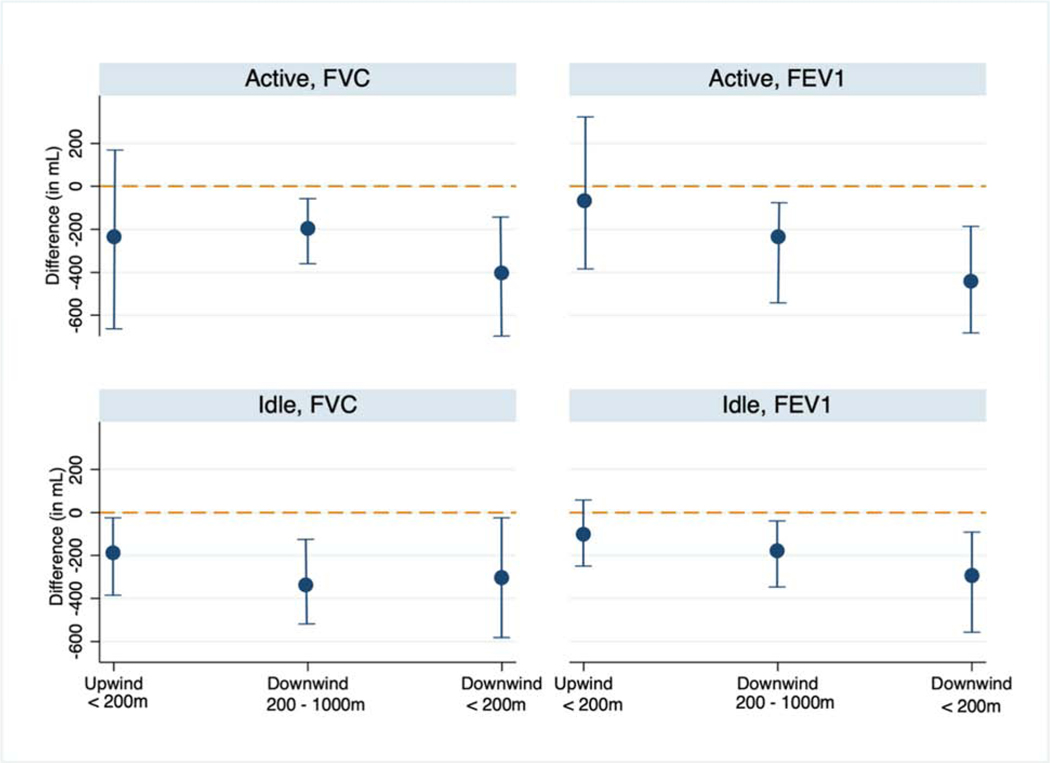
In multivariable linear models, participants living near the active oil wells had, on average, a −188 mL FVC (95% CI: −405, −28) and −110 mL FEV1 (95% CI: −286, 66) difference compared to the idle site suggesting significantly lower FVC values among residents near the active site. After considering proximity, we observe that residents living near (<200m) oil well sites had, on average, −128 mL lower FVC (95% CI: −282, −5) and −112 mL lower FEV1 (95% CI: −213, −10) compared to residents living more than 200m from the wells (Figure 4). When accounting for predominant wind direction and proximity, we observe that residents living downwind and less than 200m from oil operations had, on average, −296 mL lower FVC (95% CI: −525, −67) and −236 mL lower FEV1 (95% CI: −425, −48) compared to residents living upwind and more than 200m from the wells (Figure 5, Table S6). Participants living downwind 200–1000m from the site also had, on average, significantly lower FVC (β = −253mL, 95% CI: −384, −123) and FEV1 (β = −207mL, 95% CI: −314, −100) than those upwind and farther away. Further, living upwind and close (<200m) from the well sites was also associated with a significantly reduced FEV1 and FVC lung function measurements (Table S6). Examining distance from the well site using a continuous log transformed metric per 100 m, we find that a twofold increase in the distance away from the site improves FVC by 92 mL (β = 133 95% CI: 30.3, 236.2); FEV1 values are positively associated with an increase in the distance from the OGD site but not statistically significant (β = 72; 95% CI: −13.9, 157.1) (Table S7).
Figure 5:
The difference in average FEV1 and FVC (in mL) and 95% confidence interval for Model 1) participants living near the neighborhood with the active compared to the idle OGD sites; Model 2) participants living near (<200 m) the OGD sites compared to those living farther away (200–1000 m); and Model 3) participants living both near (<200 m) and downwind of an OGD site compared to those living farther (200–1000m) and upwind. All models are adjusted for age, height, age-height interaction, sex, race/ethnicity, weight, asthma diagnosis, recent flu/cold, ever smoker, indoor exposure to environmental tobacco smoke, living near a freeway, season, spirometry technician and a random effect for residential household.
Among the multivariable linear regression models stratified by neighborhood, we found that living within 200 m of the active wells (Jefferson Park, Table S8) was associated with significantly lower mean FVC (β = −278mL, 95% CI: −502, −55) and FEV1 (β = −240mL, 95% CI: −439, −42) compared to more than 200 m away from the wells. A similar pattern was observed when examining downwind participants, where those living downwind and near (< 200m) the active oil wells had significantly lower mean FVC (β = −399 mL, 95% CI: −652, −147) and FEV1 (β = −414mL, 95% CI: −636, −191) compared to living upwind and more than 200m away from the wells after adjusting for covariates (Figure 6). The pattern largely persistent among participants in the neighborhood with the idle wells (Figure 6, Table S9). Among participants in the neighborhood near the idle wells, which is impacted by multiple freeways, we found that residents living downwind and close to the idle wells was associated with lower lung function (FVC: β = −297mL, 95% CI: −577, −18; FEV1: β = −284mL, 95% CI: −490, −76).
Figure 6.
Average difference in FEV1 (left) and FVC (right) in mL compared to participants living upwind and 200–1000m from the OGD site stratified by neighborhood. Top row show results for participants living near the active OGD site (Jefferson Park neighborhood) and bottom row is among participants living near the idle OGD site (North University Park). The reference category is living upwind and more than 200m from an OGD site. Models are adjusted for age, height, age-height interaction, sex, race/ethnicity, weight, asthma diagnosis, recent flu/cold, ever smoker, indoor exposure to environmental tobacco smoke, living near a freeway, season, spirometry technician and a random effect for residential household.
3.4. Sensitivity Analyses.
We assessed lung function using two additional proximity distances: 150m and 400m. The associations observed with lung function persists in similar direction (Table S10 and S11). The difference in FEV1 among participants living <150m from the well site are similar (β = −187mL, 95% CI: −332, −42) when compared to the results using the <200m distance. We observe the difference attenuate for FEV1 at the 400m distance (β = −21mL, 95% CI: −119, 82). Across both analyses, a significantly lower lung function was observed among those living nearby and downwind of the oil well facilities.
In addition, significant effects with respect to distance and direction from oil operations and lung function were seen across subgroups (Table 3), including among participants without asthma. In an analysis restricted to participants without asthma, the difference in the effect of living near and downwind of an OGD well site was similar to that of the entire study population (−271 mL lower FEV1 and −326 mL lower FVC on average). We observed the effects of oil and gas wells on FEV1 lung function, on average, to be significant among adults, Latinx residents and participants over 60 if living downwind and <200m from a well site.
Table 3:
Multivariate subgroup analyses of oil site distance and direction effects ond differences in FEV1 and FVC (reported in mL).
| FVC* | FEV1* | |||||
|---|---|---|---|---|---|---|
| Subgroups | Downwind <200m | Downwind 200–1000m | Upwind <200m | Downwind <200m | Downwind 200–1000m | Upwind <200m |
| Age | ||||||
| 9- <18 | −234 (−495, 37) | −292 (−495, −89) | −8 (−396, 379) | −163 (−378, 51) | −180 (−347, −13) | −51 (−369, 266) |
| 18–60 | −225 (−419, −32) | −157 (−334, 20) | −251 (−566, 63) | −290 (−570, −8) | −169 (−327, −12) | −219 (−394, −45) |
| >60 | −303 (−669, 62) | −339 (−734, 55) | −275 (−806, 256) | −303 (−266, −40) | −284 (−569, −0.5) | −170 (−552, 212) |
| Sex | ||||||
| Female | −158 (−335, 19) | −158 (−335, −46) | −162 (−449, 114) | −194 (−332, −55) | −161 (−283, −39) | −170 (−390, 50) |
| Male | −435 (−863, −7) | −276 (−393, 3) | −313 (−589, −37) | −236 (−603, 131) | −224 (−457, −32) | −160 (−395, 75) |
| Race/Ethnicity | ||||||
| Latinx | −298 (−544, −54) | −271 (−412, −125) | −208 (−373, −42) | −264 (−459, −69) | −205 (−319, −91) | −176 (−308, −44) |
| Black | −305 (−717, 108) | −476 (−1015, 61) | 367 (−823,1557) | −330 (−681, 20) | −397 (−854, 61) | 438 (−574,1450) |
| Asthma status | ||||||
| Yes | −263 (−591, 72) | −69 (−378, 239) | −122 (−591, 346) | −380 (−662, −99) | −276 (−558, 5) | 77 (−350, 504) |
| No | −326 (−601, −52) | −271 (−420, 123) | −232 (−401, −63) | −271 (−498, −46) | −191 (−313, −69) | −171 (−331, −32) |
Models were adjusted for age, height, age-height interaction, sex, race/ethnicity, weight, asthma diagnosis, recent flu/cold, smoking, exposure to indoor environmental tobacco smoke, site, living near a freeway, season and spirometry technician. A random effect was included for residential household. Stratifying variables were excluded from their respective model runs.
4. DISCUSSION
Although petroleum extraction is increasingly common in urbanized areas, few studies exist on the health consequences for nearby residents.44–46 In this community-driven epidemiological study, we report both self-reported acute symptoms and pulmonary function measurements of a diverse cohort of residents living near both an active and idle drill site that draw from Las Cienagas oil field in urban South Los Angeles. We identify that residents living near the active drill site report more acute symptoms, including wheezing, sore throat, chest tightness, dizziness and eye or nose irritation compared to their counterparts living near the idle wells. Furthermore, residents living closer to the OGD operations have, on average, lower lung function compared to the residents farther away. While this pattern is more pronounced near the actively producing site, we see persistent effects in both neighborhoods and among non-asthmatics. The impacts on lung function were further observed among non-asthmatic participants, indicating that oil-related activity may have adverse effects on otherwise healthy people. This study provides evidences of potential adverse relationship between respiratory health and oil drilling activities in an urban context.
Our findings in this study in an urban context suggest that resident self-reported health symptoms are similar to those reported through surveys nearby natural gas and hydraulic fracturing sites in more rural settings. Results from three recent health surveys in the US observed symptoms of throat and nasal irritation, eye burning, sinus problems, headaches, skin problems, loss of smell, cough, nosebleeds and stress as more common among individual living closer to extraction sites compared to those living farther away.11–13 Survey-based studies documented higher rates of headaches, dizziness, and eyes, nose, throat and skin irritation among residents in oil producing regions compared to people living farther away in Ecuador17 and Nigeria.18 Elevated incidence of pediatric asthma hospitalization has also been observed in nonurban areas with the highest levels of drilling activity, suggesting an association between extraction activity and respiratory health.14
A single well typically operates for decades (often more than 60 years in CA) with neighbors facing impacts from construction, production, processing and transportation. Such operations produce a complex mixtures of pollutants including carcinogens, mutagens, reproductive, developmental toxins and endocrine disruptors.47–50 Hazardous compounds can be volatilized or aerosolized during extraction via active evaporating pits, flares, surface spills, processing, and transportation.51 Research near Las Cienagas oil field identified both combusted (e.g. traffic) and volatilized hydrocarbons were affecting air quality throughout the community and revealed episodic peaks of methane and VOCs likely attributable to local oil and gas operations.52 Studies of acute inhalation exposures to petroleum hydrocarbons in occupational settings as well as among residents living near refineries, oil spills or gas stations have found increased risks of eye irritation and headaches53,54 and asthma symptoms.55–57 In additional reviews of non-occupational exposures to ambient levels of benzene and other petroleum hydrocarbons found adverse impacts to the respiratory health of children58 and respiratory dysfunction and endocrine disruption among adults.10
Occupational exposure in the petroleum industry is associated with a higher prevalence of respiratory and nasal symptoms, and lung function impairment.59 Decrease in lung function has been documented among children living near petrochemical industries60 and among children living near gas-flares and oil spills61 compared to those in a reference communities. In a community-based study across five states, multiple volatile organic compounds (VOCs) were measured at concentrations exceeding a chronic risk level threshold.50 Evidence suggests that exposure to VOCs may adversely affect pulmonary function.62–64 Stagnant air patterns have also been associated with health impacts in regions with unconventional natural gas development.65 While the mechanisms of VOC toxicity are still being understood, some research indicates oxidative stress having a role.66–68 Reduced lung function has been associated with subsequent increased risk of overall mortality including coronary artery disease and respiratory disease.69–71 A small study in rural Colorado found preliminary evidence of adverse cardiovascular impacts, including higher augmentation index and blood pressure, among adults near the most drilling activity in this cross-sectional community study.72
Los Angeles houses a dense, diverse population living in close proximity to oil extraction.25 Nonetheless, oil extraction in LA has long been obfuscated from public view even as extraction sites operate within residential zones, hidden by tall walls or landscaped hedges.25 In recent years, as oil production increased, low-income neighborhoods have raised health concerns. The City of LA requires no buffers or setbacks between oil extraction and homes, and approximately 75% of active oil or gas wells are located within a 500 m distance from “sensitive land uses”, such as a home, school, childcare facility, park, or senior residential facility. Recent research leveraging a community air monitoring network in South Los Angeles identified ambient methane concentrations were higher within 500 m of the OGD sites.73 Such elevated concentrations were present at the idle well suggesting fugitive emissions occur even when oil production has ceased.73 There are ~970 active oil or gas wells within 200m of a residential property in LA County as of 2019 (Figure 1b). Nonetheless, a prior door to door survey in the Las Cienagas neighborhoods found that 63% of residents would not know how to contact local regulatory authorities in case of a pollution or health concern.74 45% of respondents in this same survey were unaware of the oil and gas operations in the neighborhood.74
To our knowledge, this is the first study to examine the relationship between lung function in urban communities and oil well sites. To date the limited health research on oil and gas development in the US is based in rural and majority non-Hispanic White communities. Our study involves a predominantly low-income community of color living in an historically underserved and environmental justice community. Very limited data is available on the impacts of oil drilling in an urban environment.42,74 In this study we identify proximity to urban oil drilling sites as a factor associated with reduced lung function among nearby residents. To date, researchers have largely relied on assessing health impacts near oil and gas development, such as birth outcomes or hospitalization, using secondary data.75 While limited by a cross-sectional design, our study contributes novel pulmonary function measurements to the epidemiology on health effects of urban oil drilling. However, this analysis faces several limitations. We cannot rule out potential confounding by unmeasured covariates or differential participation rates based on concerns about neighborhood health or environmental quality. We cannot account for lifetime residential history, individual household characteristics nor occupational exposures. Self-reported household income data was not reliable (30% of the data was missing or reported as “I don’t know”); therefore this information was not considered in the analysis. Multiple participants per household were allowed as long as they met the inclusion criteria and our modeling only accounted for such differences based on a random effect by residential address. As we only collected address information, and as multiple families often live in one household (or one common address), we could not distinguish unique families. Wind direction and proximity is used as a proxy for exposure to pollution associated with the well sites and may not represent true oil-related exposure. Future work will include assessing neighborhood scale air pollution to better understand potential spatiotemporal patterns of regional, freeway and oil drilling related exposures.
5. CONCLUSIONS
Together, our findings suggest that living near urban oil drilling sites is significantly associated with reduced lung function in South Los Angeles. This community-academic research improves understanding of impacts from living nearby drilling operations on the health and welfare of this community, which is critical to inform public health relevant strategies to address community concerns. We observe a similar pattern among those living near the active and idle sites suggesting potential chronic impacts of exposures. As a community of predominantly low-income residents of color, these impacts raise environmental justice concerns about the effects of urban oil drilling. Reducing emissions, increasing the distance between oil operations and residents, and investments in renewable energy and energy efficiency measures that reduce reliance on fossil fuels overall—could protect the lung health of residents near oil wells.
Supplementary Material
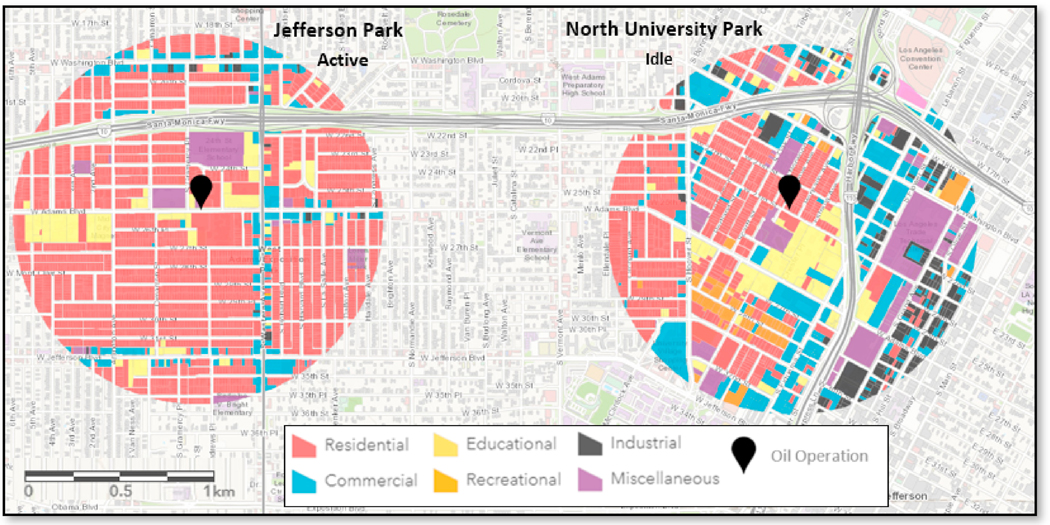
Figure 2:
Oil operation locations and land-use around the two neighborhoods in South Los Angeles, California.
Highlights.
Urban oil and gas development occurs in close proximity to homes in Los Angeles
Residents living near an active oil well reported more wheezing symptoms
Living near oil develop was associated with lower lung function
Oil development activities may contribute to respiratory health problems
ACKNOWELDGEMENTS
This work was supported in part by a grant from the National Institute of Environmental Health Sciences (ES027695). Thank you to all our partners at Esperanza Community Housing and Redeemer Community Partnership, along with Ruth Andrade, Alejandra Castillo, Deisy Gutierrez, Amanda Jimenez, Kelly Koh, Esther Lim, Leticia Ortiz, Veronica Ponce de Leon, Toby Rodriguez, Sandra Serrano, Blanca Valdez and Nicole Wong.
Additional Information: This work was funded in part by National Institute of Environmental Health Sciences (ES027695). All research was approved by the Institutional Review Board at the University of Southern California.
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mead W. Crude oil supply and demand. The Environment of Oil 1993:43–83. [Google Scholar]
- 2.O’Callaghan-Gordo C, Orta-Martinez M, Kogevinas M. Health effects of non-occupational exposure to oil extraction. Environmental health : a global access science source 2016;15:56-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petroleum & Other Liquids: Crude Oil Production. U.S. Department of Energy, 2018. (Accessed 2/28/2018, at https://www.eia.gov/dnav/pet/pet_crd_crpdn_adc_mbblpd_a.htm.) [Google Scholar]
- 4.Czolowski ED, Santoro RL, Srebotnjak T, Shonkoff SBC. Toward Consistent Methodology to Quantify Populations in Proximity to Oil and Gas Development: A National Spatial Analysis and Review. Environmental health perspectives 2017;125:086004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotton M, Charnley-Parry I. Beyond opposition and acceptance: examining public perceptions of the environmental and health impacts of unconventional oil and gas extraction. Current Opinion in Environmental Science & Health 2018;3:8–13. [Google Scholar]
- 6.Adgate JL, Goldstein BD, McKenzie LM. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environmental Science & Technology 2014;48:8307–20. [DOI] [PubMed] [Google Scholar]
- 7.Finkel M, Hays J, Law A. The shale gas boom and the need for rational policy. American Journal of Public Health 2013;103:1161–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field RA, Soltis J, Murphy S . Air quality concerns of unconventional oil and natural gas production. Environ Sci Process Impacts 2014;16:954–69. [DOI] [PubMed] [Google Scholar]
- 9.Atsdr. Toxicological Profile for Total Petroleum Hydrocarbons (TPH). Agency for Toxic Substances and Disease Registry, US Department of Health and Human Services; 1999:315–. [PubMed] [Google Scholar]
- 10.Bolden AL, Kwiatkowski CF, Colborn T. New look at BTEX: are ambient levels a problem? Environmental Science & Technology 2015;49:5261–76. [DOI] [PubMed] [Google Scholar]
- 11.Steinzor N, Subra W, Sumi L. Investigating links between shale gas development and health impacts through a community survey project in Pennsylvania. New Solutions: A Journal of Environmental and Occupational Health Policy 2013;23:55–83. [DOI] [PubMed] [Google Scholar]
- 12.Rabinowitz PM, Slizovskiy IB, Lamers V, et al. Proximity to natural gas wells and reported health status: results of a household survey in Washington County, Pennsylvania. Environmental health perspectives 2015;123:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferrar KJ, Kriesky J, Christen CL, et al. Assessment and longitudinal analysis of health impacts and stressors perceived to result from unconventional shale gas development in the Marcellus Shale region. International Journal of Occupational and Environmental Health 2013;19:104–12. [DOI] [PubMed] [Google Scholar]
- 14.Willis MD, Jusko TA, Halterman JS, Hill EL. Unconventional natural gas development and pediatric asthma hospitalizations in Pennsylvania. Environmental research 2018;166:402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willis M, Hystad P, Denham A, Hill E. Natural gas development, flaring practices and paediatric asthma hospitalizations in Texas. International Journal of Epidemiology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rasmussen SG, Ogburn EL, McCormack M, et al. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA internal medicine 2016;176:1334–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.San Sebastián M, Armstrong B, Stephens C. [Health of women living near oil wells and oil production stations in the Amazon region of Ecuador]. Revista panamericana de salud publica = Pan American journal of public health 2001;9:375–84. [DOI] [PubMed] [Google Scholar]
- 18.Kponee KZ, Chiger A, Kakulu II, Vorhees D, Heiger-Bernays W. Petroleum contaminated water and health symptoms: a cross-sectional pilot study in a rural Nigerian community. Environ Health 2015;14:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran KV, Casey JA, Cushing LJ, Morello-Frosch R. Residential Proximity to Oil and Gas Development and Birth Outcomes in California: A Retrospective Cohort Study of 2006–2015 Births. Environmental health perspectives 2020;128:067001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonzalez DJX, Sherris AR, Yang W, et al. Oil and gas production and spontaneous preterm birth in the San Joaquin Valley, CA: A case–control study. Environmental Epidemiology 2020;4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cushing LJ, Vavra-Musser K, Chau K, Franklin M, Johnston JE. Flaring from Unconventional Oil and Gas Development and Birth Outcomes in the Eagle Ford Shale in South Texas. Environmental Health Perspectives 2020;128:077003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chilingar GV, Endres B. Environmental hazards posed by the Los Angeles Basin urban oilfields: An historical perspective of lessons learned. Environmental Geology 2005;47:302–17. [Google Scholar]
- 23.Gamache MT, Frost PL. Urban development of oil fields in the Los Angeles Basin Area: 1983–2001. Sacramento, 2003. [Google Scholar]
- 24.Sadd JL, Shamasunder B. Oil Extraction in Los Angeles: Health, Land Use, and Environmental Justice Consequences. Los Angeles, CA 2015. Report No.: 9788578110796. [Google Scholar]
- 25.Elkind SS. Oil in the City: The Fall and Rise of Oil Drilling in Los Angeles. Journal of American History 2012;99:82–90. [Google Scholar]
- 26.Shamasunder B, Collier-Oxandale A, Blickley J, et al. Community-based health and exposure study around urban oil developments in South Los Angeles. International journal of environmental research and public health 2018;15:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Office of Environmental Health Hazard Assessment (OEHHA). CalEnviroScreen 3.0: Update to the California Communities Environmental Health and Screening Tool: California Environmental Protection Agency, Office of Environmental Health; 2017. [Google Scholar]
- 28.Lohah T. What it’s like to have 30 oil & gas wells as neighbors. Grist 2014. October 24, 2014. [Google Scholar]
- 29.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American Journal of Preventive Medicine 2007;33:418–27. [DOI] [PubMed] [Google Scholar]
- 30.Dominguez K, Penman-Aguilar A, Chang MH, et al. Vital signs: leading causes of death, prevalence of diseases and risk factors, and use of health services among hispanics in the United States - 2009–2013. MMWRMorbidity and mortality weekly report 2015;64:469–78. [PMC free article] [PubMed] [Google Scholar]
- 31.Ingram M, Schachter KA, Sabo SJ, et al. A community health worker intervention to address the social determinants of health through policy change. The journal of primary prevention 2014;35:119–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pérez LM, Martinez J. Community health workers: social justice and policy advocates for community health and well-being. American journal of public health 2008;98:11–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peters JM, Avol E, Navidi W, et al. A study of twelve Southern California communities with differing levels and types of air pollution. I. Prevalence of respiratory morbidity. Am J Respir Crit Care Med 1999;159:760–7. [DOI] [PubMed] [Google Scholar]
- 34.Tajik M, Muhammad N, Lowman A, Thu K, Wing S, Grant G. Impact of odor from industrial hog operations on daily living activities. New Solut 2008;18:193–205. [DOI] [PubMed] [Google Scholar]
- 35.Schinasi L, Horton RA, Guidry VT, Wing S, Marshall SW, Morland KB. Air pollution, lung function, and physical symptoms in communities near concentrated Swine feeding operations. Epidemiology 2011;22:208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baughman P, Marott JL, Lange P, et al. Combined effect of lung function level and decline increases morbidity and mortality risks. European journal of epidemiology 2012;27:933–43. [DOI] [PubMed] [Google Scholar]
- 37.Beaty T, Cohen B, Newill C, Menkers H, Diamond E, Chen C. Impaired pulmonary function as a risk factor for mortality. American journal of epidemiology 1982;116:102–13. [DOI] [PubMed] [Google Scholar]
- 38.Mannino D, Buist AS, Petty T, Enright P, Redd S. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax 2003;58:388–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schünemann HJ, Dorn J, Grant BJ, Winkelstein W, Trevisan M. Pulmonary function is a long-term predictor of mortality in the general population. Chest 2000;118:656–64. [DOI] [PubMed] [Google Scholar]
- 40.Zhu Y, Hinds WC, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc 2002;52:1032–42. [DOI] [PubMed] [Google Scholar]
- 41.Zhu Y, Kuhn T, Mayo P, Hinds WC. Comparison of daytime and nighttime concentration profiles and size distributions of ultrafine particles near a major highway. Environ Sci Technol 2006;40:2531–6. [DOI] [PubMed] [Google Scholar]
- 42.Garcia-Gonzales DA, Shamasunder B, Jerrett M. Distance decay gradients in hazardous air pollution concentrations around oil and natural gas facilities in the city of Los Angeles: A pilot study. Environmental research 2019;173:232–6. [DOI] [PubMed] [Google Scholar]
- 43.Peters JM, Avol E, Gauderman WJ, et al. A Study of Twelve Southern California Communities with Differing Levels and Types of Air Pollution. American Journal of Respiratory and Critical Care Medicine 1999;159:768–75. [DOI] [PubMed] [Google Scholar]
- 44.Colborn T, Kwiatkowski C, Schultz K, Bachran M. Natural gas operations from a public health perspective. Human and Ecological Risk Assessment: An International Journal 2011;17:1039–56. [Google Scholar]
- 45.McKenzie LM, Witter RZ, Newman LS, Adgate JL. Human health risk assessment of air emissions from development of unconventional natural gas resources. The Science of the total environment 2012;424:79–87. [DOI] [PubMed] [Google Scholar]
- 46.Werner AK, Vink S, Watt K, Jagals P. Environmental health impacts of unconventional natural gas development: A review of the current strength of evidence. Science of the Total Environment 2015;505:1127–41. [DOI] [PubMed] [Google Scholar]
- 47.Garcia-Gonzales DA, Shonkoff SBC, Hays J, Jerrett M. Hazardous Air Pollutants Associated with Upstream Oil and Natural Gas Development: A Critical Synthesis of Current Peer-Reviewed Literature. Annual review of public health 2019;40:283–304. [DOI] [PubMed] [Google Scholar]
- 48.Johnston JE, Lim E, Roh H. Impact of upstream oil extraction and environmental public health: A review of the evidence. Science of the Total Environment 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Colborn T, Schultz K, Herrick L, Kwiatkowski C. An Exploratory Study of Air Quality near Natural Gas Operations. Human and Ecological Risk Assessment: An International Journal 2014;20:86–105. [Google Scholar]
- 50.Macey GP, Breech R, Chernaik M, et al. Air concentrations of volatile compounds near oil and gas production: a community-based exploratory study. Environ Health 2014;13:82-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Colborn T, Schultz K, Herrick L, Kwiatkowski C. An Exploratory Study of Air Quality near Natural Gas Operations. Human and Ecological Risk Assessment: An International Journal 2013;20:86–105. [Google Scholar]
- 52.Collier-Oxandale A, Wong N, Navarro S, Johnston J, Hannigan M. Using gas-phase air quality sensors to disentangle potential sources in a Los Angeles neighborhood. Atmospheric Environment 2020;233:117519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kim BM, Park E-K, LeeAn S-Y, et al. BTEX exposure and its health effects in pregnant women following the Hebei spirit oil spill. J Prev Med Public Health Yebang Uihakhoe Chi 2009;42:96–103. [DOI] [PubMed] [Google Scholar]
- 54.Tunsaringkarn T, Ketkaew P, Siriwong W, Rungsiyothin A, Zapuang K. Benzene exposure and its association with sickness exhibited in gasoline station workers. Int J Environ Pollut Solutions 2013;1:1–8. [Google Scholar]
- 55.White N, van der Walt A, Ravenscroft G, Roberts W, Ehrlich R. Meteorologically estimated exposure but not distance predicts asthma symptoms in schoolchildren in the environs of a petrochemical refinery: a cross-sectional study. Environmental Health 2009;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rovira E, Cuadras A, Aguilar X, et al. Asthma, respiratory symptoms and lung function in children living near a petrochemical site. Environmental research 2014;133:156–63. [DOI] [PubMed] [Google Scholar]
- 57.Wichmann FA, Müller A, Busi LE, et al. Increased asthma and respiratory symptoms in children exposed to petrochemical pollution. Journal of Allergy and Clinical Immunology 2009;123:632–8. [DOI] [PubMed] [Google Scholar]
- 58.Ferrero A, Íñiguez C, Esplugues A, Estarlich M, Ballester F. Benzene exposure and respiratory health in children: a systematic review of epidemiologic evidences. Journal of Pollution Effects & Control 2014:1–13. [Google Scholar]
- 59.Stoleski S, Karadzinska-Bislimovska J, Minov J, Mijakoski D, Risteska-Kuc S, Trajceva L. Respiratory symptoms, lung function tests and bronchial hyperresponsiveness among workers in petroleum industry. Eur Respiratory Soc; 2011. [Google Scholar]
- 60.Rusconi F, Catelan D, Accetta G, et al. Asthma Symptoms, Lung Function, and Markers of Oxidative Stress and Inflammation in Children Exposed to Oil Refinery Pollution. Journal of Asthma 2011;48:84–90. [DOI] [PubMed] [Google Scholar]
- 61.Aweto H, Saro-Bakpo M, Aiyegbusi A. Cardiopulmonary functions of school children in oil-spilled and gas-flared Niger-Delta and rural-Riverine Lagos Communities. Journal of Applied Sciences and Environmental Management 2019;23:1529–34. [Google Scholar]
- 62.Elliott L, Longnecker MP, Kissling GE, London SJ. Volatile organic compounds and pulmonary function in the Third National Health and Nutrition Examination Survey, 1988–1994. Environmental health perspectives 2006;114:1210–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yoon HI, Hong Y-C, Cho S, et al. Exposure to volatile organic compounds and loss of pulmonary function in the elderly. European Respiratory Journal 2010;36:1270–6. [DOI] [PubMed] [Google Scholar]
- 64.Cakmak S, Dales RE, Liu L, et al. Residential exposure to volatile organic compounds and lung function: Results from a population-based cross-sectional survey. Environmental Pollution 2014;194:145–51. [DOI] [PubMed] [Google Scholar]
- 65.Brown DR, Lewis C, Weinberger BI. Human exposure to unconventional natural gas development: A public health demonstration of periodic high exposure to chemical mixtures in ambient air. Journal of Environmental Science and Health, Part A 2015;50:460–72. [DOI] [PubMed] [Google Scholar]
- 66.Garçon G, Dagher Z, Zerimech F, et al. Dunkerque City air pollution particulate matter-induced cytotoxicity, oxidative stress and inflammation in human epithelial lung cells (L132) in culture. Toxicology in vitro 2006;20:519–28. [DOI] [PubMed] [Google Scholar]
- 67.Coleman CA, Hull BE, McDougal JN, Rogers JV. The effect of m-xylene on cytotoxicity and cellular antioxidant status in rat dermal equivalents. Toxicology letters 2003;142:133–42. [DOI] [PubMed] [Google Scholar]
- 68.Röder-Stolinski C, Fischäder G, Oostingh GJ, et al. Styrene induces an inflammatory response in human lung epithelial cells via oxidative stress and NF-κB activation. Toxicology and applied pharmacology 2008;231:241–7. [DOI] [PubMed] [Google Scholar]
- 69.Islam T, Gauderman WJ, Berhane K, et al. Relationship between air pollution, lung function and asthma in adolescents. Thorax 2007;62:957–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Knuiman MW, James AL, Divitini ML, Ryan G, Bartholomew HC, Musk A. Lung function, respiratory symptoms, and mortality: results from the Busselton Health Study. Annals of epidemiology 1999;9:297–306. [DOI] [PubMed] [Google Scholar]
- 71.Sin DD, Wu L, Man SP. The relationship between reduced lung function and cardiovascular mortality: a population-based study and a systematic review of the literature. Chest 2005;127:1952–9. [DOI] [PubMed] [Google Scholar]
- 72.McKenzie LM, Crooks J, Peel JL, et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in Northeastern Colorado. Environmental research 2019;170:56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Okorn K, Jimenez A, Collier-Oxandale A, Johnston J, Hannigan M. Characterizing methane and total non-methane hydrocarbon levels in Los Angeles communities with oil and gas facilities using air quality monitors. Science of The Total Environment 2021:146194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shamasunder B, Collier-Oxandale A, Blickley J, et al. Community-Based Health and Exposure Study around Urban Oil Developments in South Los Angeles. International journal of environmental research and public health 2018;15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Johnston J, Cushing L. Chemical Exposures, Health, and Environmental Justice in Communities Living on the Fenceline of Industry. Current Environmental Health Reports 2020;7:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.