Abstract
Purpose:
To evaluate the correlation between the angle of deviation in different gazes and the amount of head tilt in patients with congenital unilateral superior oblique muscle palsy (SOP).
Methods:
This case series study was performed on 20 consecutive SOP patients with head tilt. Based on the Bielschowsky three-step test, the angle of deviation was measured in different gazes. Furthermore, the hypertropia difference between the two lateral gazes (gaze difference) and the two head tilt sides (bilateral head tilt difference) was calculated. For measuring head tilt, close-up pictures from 40 cm with a habitual abnormal head position were captured and analyzed by the Corel Draw X7 software.
Results:
The mean age of patients was 13 ± 9 years (range, 2.5–31 years). The mean angle of hypertropia in ipsilateral and contralateral head tilt was 24.5 Δ ± 7.1 Δ and 6.5 Δ ± 4.2 Δ, respectively (P < 0.001), and in ipsilateral and contralateral lateral gaze positions, it was 8.2 Δ ± 5.5 Δ and 22.5 Δ ± 6.1 Δ, respectively (P < 0.001). The mean of bilateral head tilt hypertropia difference was 18 Δ ± 5.3 Δ and gaze hypertropia difference was 14.3 Δ ± 6.16 Δ. There was a positive correlation between bilateral head tilt hypertropia difference and the amount of head tilt (R = 0.609, R2 = 0.371, P = 0.004, the amount of head tilt = 0.39 × [Bilateral head tilt hypertropia difference] +1.77). The amount of head tilt also had a positive correlation with the gaze hypertropia difference (R = 0.492, R2 = 0.242, P = 0.028, the amount of head tilt = 0.27 × [gaze hypertropia difference] +4.81).
Conclusion:
In SOP patients, the amount of head tilt had a positive correlation with bilateral head tilt hypertropia difference and also gaze hypertropia difference.
Keywords: Abnormal head position, Head tilt, Hypertropia, Superior oblique palsy
INTRODUCTION
Superior oblique palsy is the most common type of cranial nerve palsy,1,2,3 and it is diagnosed based on the presence of hypertropia in the primary position, which usually increases with adduction in the affected eye.4,5 Previous studies have shown that superior oblique palsy is the most frequent ocular cause of abnormal head posture.6,7,8 Patients with the congenital sources of superior oblique muscle palsy (SOP) are often asymptomatic; however, in acquired superior oblique palsy, the most common symptoms are image tilting, asthenopia, and diplopia.9,10
Abnormal head posture is defined as any deviation of head and face from normal position in x, y, and z axes,11 which is a sign and a manifestation of an underlying disease. The etiology of abnormal head posture may be congenital or acquired and can occur at any age, depending on the cause of the disease.12 The most common sources of abnormal head posture are orthopedic, neurological, and ocular causes.13,14,15 Patients with superior oblique palsy habitually tilt and turn their heads to the contralateral side of the muscle palsy and by eliminating diplopia, abnormal head posture may establish a normal bifoveal fusion.16
Previous studies reported that the most common form of the abnormal head posture in superior oblique palsy patients is pure head tilt to the contralateral side of the eye with muscle palsy.6,17 The severity of head tilt in these patients manifests itself in various degrees. In some patients who have the potential for binocular single vision, they may adjust the amount of head tilt to control the deviation by fusional vergences easily.18 However, the exact cause of the different amount of head tilt in patients with superior oblique palsy has remained unclear.
The main purpose of this study is to evaluate the correlation between the angle of deviation in different gazes and the amount of head tilt in patients with congenital unilateral superior oblique palsy.
METHODS
This study was conducted in Farabi Eye Hospital, Tehran, Iran, from February 2020 to July 2020. The study was performed in accordance with the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences (IR.SBMU.RETECH.REC.1399.228). The aim of the study was explained to the patients and their parents, and then, informed consents were obtained.
This case series study was performed on 20 consecutive patients with congenital unilateral superior oblique palsy. The inclusion criteria were confirmed by the presence of head tilt due to congenital unilateral superior oblique palsy. The exclusion criteria were the presence of other causes of abnormal head posture, which may manifest as head tilt such as nystagmus. In addition, patients who did not have good cooperation for measuring the angle of deviation in different gazes and patients with plagiocephalic syndromes, craniofacial anomalies, and other skeletal and muscular abnormalities and prior history of surgery or trauma to the neck, eye, head, or shoulder area were excluded from the study.
First, demographic information such as the age of patients, sex, and duration of strabismus was collected by a questionnaire. Then, uncorrected and best corrected distance visual acuity were measured. The amount of refractive error was determined by Topcon RM-8900 auto refractometer (Topcon Medical Systems, Tokyo, Japan), and the results were confirmed using Heine Beta 200 retinoscope (Herrsching, Germany). Also, fundoscopy examinations were performed for all patients.
Eye movements, overaction, and underaction of extraocular muscles were tested by version and duction tests. Inferior oblique muscle overaction was defined as over-elevation of the eye in adduction upgaze, and it was recorded from +1 to +4 by version test, as previously described.19
Horizontal and vertical deviations in different gaze positions were measured by alternate prism-cover test. The angle of deviation was neutralized by holding appropriate prisms in front of the paretic eye with full correction of refractive errors.20 By unmasked expert examiners, based on the maneuver of Bielschowsky three-step,21 angles of deviation were measured in six different gaze positions as follows; 1 – far (6 m) in primary position, 2 – near (40 cm) in primary position, 3 – lateral gaze toward the contralateral side of the eye with muscle palsy, 4 – lateral gaze toward the ipsilateral side, 5 – head tilt to the contralateral side, and 6 – head tilt to the ipsilateral side. The hypertropia difference between the contralateral and ipsilateral head tilt positions was measured and defined as “bilateral head tilt difference”. In addition, “gaze difference” was defined as the difference in the angle of hypertropia between ipsilateral and contralateral lateral gaze positions.22,23 All measurements were first obtained by an optometrist and then confirmed by an expert pediatric ophthalmologist and strabismus surgeon (MR. A.).
A diagnosis of superior oblique palsy was made based on the Parks–Bielschowsky three-step test, with hypertropia in the primary gaze that increased in ipsilateral head tilt and on contralateral gaze.4,5 Other clinical conditions that may have a positive Bielschowsky three-step test or conditions mimicking unilateral superior oblique palsy were considered and excluded from this study.24 A congenital etiology for superior oblique palsy was confirmed based on the patient's childhood photographs, absence of diplopia, presence of facial asymmetry, and long-term history of strabismus.25
The head tilt form of the abnormal head posture in patients with unilateral superior oblique palsy was determined based on direct observation during measuring best corrected distance visual acuity from different angles. Besides, close-up pictures from 40 cm with habitual abnormal head posture were captured from all patients. For evaluation of the severity of abnormal head posture and measurement of head tilt, these pictures were analyzed by the Corel Draw X7 software (version 17.0.0.491 for Windows, USA).26 As shown in Figure 1, the angle between the line that connects the center of the eyebrows to the center of the lip and the vertical line is measured as the angle of the head tilt.
Figure 1.
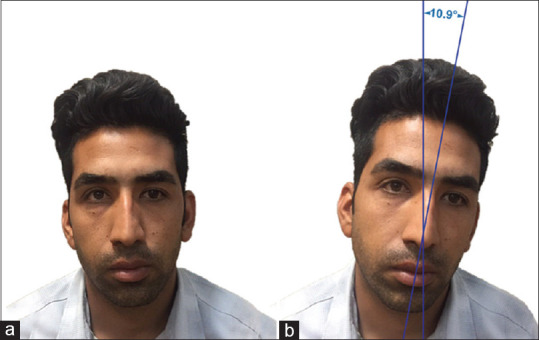
A patient with congenital right superior oblique palsy. (a): The head in the straight position by force, indicating right hypertropia (b) Habitual left head tilt (10.9°) due to right superior oblique palsy. The angle between the vertical line and the line that connects the center of the eyebrows to the center of the lip is calculated as the angle of the head tilt
SPSS 24 (IBM Corp, Armonk, New York, USA) software was used for data analysis. Normal data distribution was tested by Shapiro–Wilk, and according to normal distribution of the data, a two-independent sample t-test was applied to determine statistically significant differences in some variables such as the mean of hypertropia between different gazes. The Wilcoxon test was performed to compare the parameters between the eye with superior oblique palsy and another eye. Spearman correlation was applied to investigate the relationship between the amount of the head tilt and the angle of hypertropia in different gazes. Linear regression was applied to determine possible associations between the amount of head tilt and bilateral head tilt hypertropia difference or gaze hypertropia difference. Graphs were drawn using the Microsoft Excel 2019 (Office 365; Microsoft Corporation, Redmond, WA) software. P < 0.05 was considered statistically significant.
RESULTS
This case series study was performed on 20 patients with congenital unilateral superior oblique palsy [Table 1] with the mean age of 13 ± 9 years (range, 2.5–31 year), of which 5 (25%) were female and 15 (75%) were male. Superior oblique palsy was observed in the right eye of 11 (55%) patients, and in the left eye of 9 (45%) cases.
Table 1.
Summary of patients with unilateral congenital unilateral superior oblique muscle palsy
| n | Age | Sex | Tilt side | Head tilt (°) | IOOA | Primary position (Δ) | |||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Far | Near | ||||||||
|
|
|
||||||||
| Hypertropia | Exo-deviation | Hypertropia | Exo-deviation | ||||||
| 1 | 11 | Female | Left | 9.4 | +2 | 3 | 0 | 5 | 0 |
| 2 | 18 | Male | Left | 8 | +2 | 20 | 18 | 16 | 14 |
| 3 | 31 | Female | Left | 3.3 | +2 | 18 | 10 | 18 | 14 |
| 4 | 30 | Male | Right | 8.5 | +2 - +3 | 25 | 4 | 20 | 4 |
| 5 | 5 | Male | Right | 2 | +2 | 10 | 10 | 10 | 12 |
| 6 | 2.5 | Male | Right | 17.5 | +2 - +3 | 18 | 6 | 18 | 0 |
| 7 | 8 | Male | Right | 11.2 | +2 - +3 | 30 | 0 | 33 | 0 |
| 8 | 27 | Male | Left | 10.9 | +2 | 9 | 4 | 9 | 4 |
| 9 | 12 | Female | Right | 7.1 | +2 | 18 | 0 | 14 | 0 |
| 10 | 2.5 | Female | Right | 11.6 | +3 | 22 | 0 | 20 | 0 |
| 11 | 28 | Male | Left | 6.6 | +3 | 20 | 4 | 18 | 4 |
| 12 | 14 | Male | Right | 7.4 | +2 | 12 | 0 | 14 | 8 |
| 13 | 13 | Male | Left | 6.2 | +2 | 14 | 16 | 10 | 18 |
| 14 | 29 | Male | Left | 9.8 | +2 - +3 | 23 | 0 | 17 | 0 |
| 15 | 12 | Female | Left | 8.5 | +2 | 12 | 5 | 9 | 6 |
| 16 | 19 | Male | Left | 9 | +2 | 27 | 10 | 25 | 0 |
| 17 | 5 | Male | Right | 6.4 | +3 | 4 | 0 | 9 | 0 |
| 18 | 9 | Male | Right | 8.1 | +3 | 8 | 6 | 8 | 12 |
| 19 | 11 | Male | Left | 9.5 | +2 - +3 | 22 | 14 | 17 | 16 |
| 20 | 4 | Male | Left | 14.2 | +2 - +3 | 22 | 5 | 15 | 10 |
|
| |||||||||
| n | Lateral gaze (Δ) | Head tilt (Δ) | |||||||
|
|
|
||||||||
| Ipsilateral | Contralateral | Ipsilateral | Contralateral | ||||||
|
|
|
|
|
||||||
| Hypertropia | Exo-deviation | Hypertropia | Exo-deviation | Hypertropia | Exo-deviation | Hypertropia | Exo-deviation | ||
|
| |||||||||
| 1 | 1 | 0 | 20 | 0 | 16 | 0 | 0 | 0 | |
| 2 | 8 | 8 | 25 | 16 | 25 | 14 | 10 | 14 | |
| 3 | 14 | 6 | 20 | 10 | 20 | 8 | 10 | 10 | |
| 4 | 20 | 0 | 25 | 0 | 25 | 0 | 5 | 0 | |
| 5 | 8 | 6 | 12 | 6 | 14 | 8 | 4 | 8 | |
| 6 | 6 | 0 | 22 | 8 | 30 | 0 | 8 | 7 | |
| 7 | 20 | 0 | 37 | 0 | 40 | 0 | 12 | 0 | |
| 8 | 5 | 0 | 17 | 0 | 24 | 0 | 6 | 0 | |
| 9 | 6 | 0 | 16 | 0 | 22 | 0 | 3 | 0 | |
| 10 | 13 | 0 | 27 | 0 | 30 | 0 | 12 | 0 | |
| 11 | 5 | 0 | 30 | 0 | 30 | 0 | 14 | 0 | |
| 12 | 7 | 0 | 20 | 0 | 20 | 0 | 4 | 0 | |
| 13 | 6 | 14 | 15 | 16 | 22 | 18 | 8 | 16 | |
| 14 | 7 | 0 | 23 | 0 | 25 | 0 | 6 | 0 | |
| 15 | 4 | 0 | 17 | 0 | 16 | 0 | 5 | 0 | |
| 16 | 16 | 8 | 28 | 10 | 35 | 8 | 12 | 12 | |
| 17 | 8 | 0 | 18 | 0 | 16 | 0 | 0 | 0 | |
| 18 | 2 | 0 | 22 | 10 | 18 | 6 | 2 | 0 | |
| 19 | 5 | 10 | 30 | 10 | 33 | 10 | 2 | 5 | |
| 20 | 4 | 0 | 27 | 0 | 30 | 0 | 8 | 0 | |
n: Number of patients, IOOA: Inferior oblique muscle overaction
The means of uncorrected distance visual acuity in the cases that cooperated with visual acuity measurement in the paretic and nonparetic eyes were 0.071 (range, 0–0.9 logMAR) and 0.043 (range, 0–0.5 logMAR), respectively (P = 0.317), and best corrected distance visual acuity were 0.015 and 0.08, respectively (range, 0–0.1 logMAR in both eyes) (P = 0.317). There were not any pathological findings in the fundoscopic examinations other than fundus extorsion. The mean of spherical equivalent in the eye with superior oblique palsy and another eye was +0.01 ± 1.28 diopter (D) and +0.21 ± 0.55 D, respectively (P = 0.414). All patients had ipsilateral inferior oblique muscle overaction with the mean of +2.3 ± 0.3 (range, +2 to + 3).
The mean angle of hypertropia and exo-deviation in patients with congenital unilateral superior oblique palsy in the different gazes are shown in Table 2. The mean angle of hypertropia in ipsilateral head tilt was 24.5 Δ ± 7.1 Δ (range, 14 Δ to 40 Δ), and in the contralateral head tilt was 6.5 Δ ± 4.2 Δ (range, 0 Δ to 14 Δ), (P <.001).
Table 2.
The mean angle of hypertropia and exo-deviation in patients with congenital unilateral superior oblique muscle palsy in different gazes
| Deviation | Gaze | Mean±SD (Δ) | Minimum (Δ) | Maximum (Δ) | P |
|---|---|---|---|---|---|
| Hypertropia | Primary position | ||||
| Far | 16.8±7.5 | 3 | 30 | 0.043* | |
| Near | 15.2±6.6 | 5 | 33 | ||
| Lateral gaze | |||||
| Contralateral | 22.5±6.1 | 12 | 37 | <0.001* | |
| Ipsilateral | 8.2±5.5 | 1 | 20 | ||
| Head tilt | |||||
| Contralateral | 6.5±4.2 | 0 | 14 | <0.001* | |
| Ipsilateral | 24.5±7.1 | 14 | 40 | ||
| Exo-deviation | Primary position | ||||
| Far | 5.7±5.8 | 0 | 18 | 0.503† | |
| Near | 6.1±6.3 | 0 | 18 | ||
| Lateral gaze | |||||
| Contralateral | 4.3±5.8 | 0 | 16 | 0.027† | |
| Ipsilateral | 2.6±4.4 | 0 | 14 | ||
| Head tilt | |||||
| Contralateral | 3.6±5.5 | 0 | 16 | 1.000 | |
| Ipsilateral | 3.6±5.6 | 0 | 18 |
SD: Standard deviation, * Independent Samples Test, † Mann-Whitney U
The mean amount of bilateral head tilt difference was 18 Δ ± 5.3 Δ (range, 10 Δ to 31 Δ). Furthermore, the hypertropia gaze difference was 14.3 Δ ± 6.16 Δ (range, 4 Δ to 25 Δ).
In the present study, the mean amount of head tilt was 8.7° ± 3.4° (range, 2.0° to 17.5°). As shown in Figure 2, there was a positive correlation between the amount of head tilt and the bilateral head tilt hypertropia difference (R = 0.609, R2 = 0.371, P = 0.004). The equation of the amount of head tilt was determined as follows: the amount of head tilt = 0.39 × (bilateral head tilt hypertropia difference) + 1.77.
Figure 2.

The correlation between the amount of the head tilt and the bilateral head tilt difference. The hypertropia difference between the contralateral and ipsilateral head tilt positions was measured and defined as “Bilateral head tilt difference”
Figure 3 illustrates that the amount of head tilt also had a positive correlation with the gaze difference (R = 0.492, R2 = 0.242, P = 0.028). The equation of the amount of the head tilt was determined as follows: the amount of the head tilt = 0.27 × (hypertropia difference) + 4.81.
Figure 3.

The correlation between the amount of head tilt and gaze difference. “Gaze difference” was defined as the hypertropia difference between ipsilateral and contralateral side gaze positions
DISCUSSION
In this case series study, we found a weak positive correlation between the amount of head tilt and the angle of hypertropia difference between the two tilt sides. Furthermore, the amount of head tilt had a weak positive correlation with the angle of hypertropia difference between two lateral gazes. Indeed, in patients with higher bilateral head tilt difference or higher gaze difference, head tilt was manifested with a higher degree.
This study was conducted in patients with congenital unilateral superior oblique palsy, whose abnormal head posture was manifested as pure head tilt. In one study by Turan et al., they reported that abnormal head posture in 87% of patients with superior oblique palsy manifested as head tilt.6 In another study by Nucci et al., from 12 patients with abnormal head posture due to superior oblique palsy, 10 (83%) patients had head tilt.17 Therefore, according to the results of previous studies, the most common form of the abnormal head posture in patients with superior oblique palsy is the head tilt to the contralateral side of palsy without a head turn or chin down.
In this study, the mean angle of deviation in the primary position in both far and near was 16.8 Δ and 15.2 Δ, respectively, which was the same as previous studies.23,27 Furthermore, the mean amount of hypertropia in bilateral head tilt difference was 18 Δ, which was the same as Lee et al.'s study.23
The most common sign in patients with congenital unilateral superior oblique palsy is abnormal head posture, which is due to the induced hypertropia and excyclotorsion effect.28 In the present study, the mean amount of head tilt was 8.7°, which was the same as Bagheri and Eshaghi29 (8.4°) and Greenberg and Pollard30 (9.3°) studies and lower than Kekunnaya and Isenberg28 (17°) findings. Head tilt in patients with superior oblique palsy plays a role as a compensatory mechanism by holding their eyes away from the field of action of the paretic muscle. Therefore, this compensatory mechanism leads to regaining bifoveal fusion.15 Based on the results of this study, different severities of head tilt in patients with SOP were observed. Although the exact cause of different severity of head tilt in these patients is unknown, some researchers reported that a higher amount of head tilt would help some patients to control their deviation more easily by fusional vergences.17 Thus, the amount of head tilt in patients with superior oblique palsy manifests itself in various degrees.
To the best of the authors’ knowledge, the present study, for the first time, finds a positive correlation between the amount of head tilt and the bilateral head tilt hypertropia difference.
In patients with a higher amount of bilateral head tilt hypertropia difference, the amount of head tilt as a compensatory mechanism tends to increase in order to regain bifoveal fusion because, in comparison to patients with a lower amount of bilateral head tilt hypertropia difference, the angle of deviation in the field of action of the paretic muscle is much higher than other gazes. In contrast, in patients with a lower amount of bilateral head tilt hypertropia difference, bifoveal fusion is achieved easily with a lower amount of head tilt because the angle of deviation in the field of action of the paretic muscle is not much higher than other gazes. Therefore, this could be the main reason for finding a positive correlation between the amount of head tilt and the bilateral head tilt hypertropia difference.
The correlation between the amount of head tilt and the bilateral head tilt hypertropia difference was stronger than the correlation between the amount of head tilt and the hypertropia difference between two lateral gazes. This finding would be explained with the primary action of the superior oblique muscle, which is intorsion.
This study had some limitations. First, the diagnosis of superior oblique palsy was based on clinical examinations without confirming by neuroimaging. Second, this study was performed on superior oblique palsy patients whose abnormal head posture was only manifested as head tilt. Third, the sample size of superior oblique palsy patients was small, and finally, the present study was carried out only on congenital superior oblique palsy cases for uniformity within the study sample. So further studies, including acquired and congenital superior oblique palsy patients with all forms of abnormal head posture, might be needed for better proving the correlation between the angle of deviation in different gazes and the amount of various forms of the abnormal head posture.
In summary, in superior oblique palsy patients, the amount of head tilt had a weak positive correlation with the bilateral head tilt hypertropia difference and gaze hypertropia difference. This finding indicated that in patients with a higher angle of hypertropia difference between two tilt sides or two lateral gazes, the severity of head tilt was manifested with a higher degree.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Mr. Ali Pazoki (Faculty of Science, York University, Toronto, Canada) for his help in editing this article.
REFERENCES
- 1.Ellis FD, Helveston EM. Superior oblique palsy: Diagnosis and classification. Int Ophthalmol Clin. 1976;16:127–35. [PubMed] [Google Scholar]
- 2.von Noorden GK, Murray E, Wong SY. Superior oblique paralysis.A review of 270 cases. Arch Ophthalmol. 1986;104:1771. doi: 10.1001/archopht.1986.01050240045037. [DOI] [PubMed] [Google Scholar]
- 3.Khorrami-Nejad M, Akbari MR, Khosravi B. The prevalence of strabismus types in strabismic Iranian patients. Clin Optom (Auckl) 2018;10:19–24. doi: 10.2147/OPTO.S147642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akbari MR, Sadrkhanlou S, Mirmohammadsadeghi A. Surgical outcome of single inferior oblique myectomy in small and large hypertropia of unilateral superior oblique palsy. J Pediatr Ophthalmol Strabismus. 2019;56:23–7. doi: 10.3928/01913913-20180925-03. [DOI] [PubMed] [Google Scholar]
- 5.Akbari M, Nikdel M, Moghimi S, Subramanian PS, Fard MA. Effect of foveal location on retinal nerve fiber layer thickness profile in superior oblique palsy eyes. J Glaucoma. 2019;28:916–21. doi: 10.1097/IJG.0000000000001347. [DOI] [PubMed] [Google Scholar]
- 6.Erkan Turan K, Taylan ŞaylanKc H, Koy İ, Vural E, Karakaya J, Ş rak EC, et al. Ocular causes of abnormal head position: Strabismus clinic data. Turk J Ophthalmol. 2017;47:211–5. doi: 10.4274/tjo.42068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kushner BJ. Ocular causes of abnormal head postures. Ophthalmology. 1979;86:2115–25. doi: 10.1016/s0161-6420(79)35301-5. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell PR. Ocular torticollis. Trans Am Ophthalmol Soc. 1999;97:697–769. [PMC free article] [PubMed] [Google Scholar]
- 9.Kawai M, Goseki T, Ishikawa H, Hoshina M, Shoji N. Causes, background, and characteristics of binocular diplopia in the elderly. Jpn J Ophthalmol. 2018;62:659–66. doi: 10.1007/s10384-018-0617-2. [DOI] [PubMed] [Google Scholar]
- 10.Diora JR, Plager DA. Sudden-onset trochlear nerve palsy: Clinical characteristics and treatment implications. J AAPOS. 2019;23:321. doi: 10.1016/j.jaapos.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 11.Krewson 3rd WE. Ocular torticollis. Am Orthopt J. 1957;7:151–61. [PubMed] [Google Scholar]
- 12.Nucci P, Kushner BJ, Serafino M, Orzalesi N. A multi-disciplinary study of the ocular, orthopedic, and neurologic causes of abnormal head postures in children. Am J Ophthalmol. 2005;140:65–8. doi: 10.1016/j.ajo.2005.01.037. [DOI] [PubMed] [Google Scholar]
- 13.Teodorescu L. Anomalous head postures in strabismus and nystagmus diagnosis and management. Rom J Ophthalmol. 2015;59:137–40. [PMC free article] [PubMed] [Google Scholar]
- 14.Halachmi-Eyal O, Kowal L. Assessing abnormal head posture: A new paradigm. Curr Opin Ophthalmol. 2013;24:432–7. doi: 10.1097/ICU.0b013e3283644f17. [DOI] [PubMed] [Google Scholar]
- 15.Akbari MR, Khorrami Nejad M, Askarizadeh F, Farahbakhsh Pour F, Pazooki MR, Moeinitabar MR. Facial asymmetry in ocular torticollis. J Curr Ophthalmol. 2015;27:4–11. doi: 10.1016/j.joco.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel CK, Bahl RS. Practical Management of Pediatric Ocular Disorders and Strabismus. New York, NY: Springer; 2016. [Google Scholar]
- 17.Nucci P, Curiel B, Lembo A, Serafino M. Anomalous head posture related to visual problems. Int Ophthalmol. 2015;35:241–8. doi: 10.1007/s10792-014-9943-7. [DOI] [PubMed] [Google Scholar]
- 18.Kushner BJ. Abnormal Head Postures. In: Kushner BJ, editor. Strabismus. Cham: Springer; 2017. pp. 241–5. [Google Scholar]
- 19.Wu SQ, Xu QB, Sheng WY, Zhu LW. Unilateral inferior oblique anterior transposition for markedly asymmetric dissociated vertical deviation with unilateral inferior oblique over-action. BMC Ophthalmol. 2019;19:196. doi: 10.1186/s12886-019-1205-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Irsch K. Optical issues in measuring strabismus. Middle East Afr J Ophthalmol. 2015;22:265–70. doi: 10.4103/0974-9233.159691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Von Noorden GK. Binocular Vision and Ocular Motility. 5th ed. Philadelphia: Mosby Company; 1995. [Google Scholar]
- 22.Kono R, Okanobu H, Ohtsuki H, Demer JL. Absence of relationship between oblique muscle size and bielschowsky head tilt phenomenon in clinically diagnosed superior oblique palsy. Invest Ophthalmol Vis Sci. 2009;50:175–9. doi: 10.1167/iovs.08-2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JE, Yang HK, Kim JH, Hwang JM. Quantitative analysis of structure-function relationship between ocular motility and superior oblique muscle hypoplasia in unilateral superior oblique palsy. Br J Phthalmol. 2019;103:1253–8. doi: 10.1136/bjophthalmol-2018-312560. [DOI] [PubMed] [Google Scholar]
- 24.Kushner BJ. Errors in the three-step test in the diagnosis of vertical strabismus. Ophthalmology. 1989;96:127–32. doi: 10.1016/s0161-6420(89)32933-2. [DOI] [PubMed] [Google Scholar]
- 25.Straumann D, Steffen H, Landau K, Bergamin O, Mudgil AV, Walker MF, et al. Primary position and listing's law in acquired and congenital trochlear nerve palsy. Invest Ophthalmol Vis Sci. 2003;44:4282–92. doi: 10.1167/iovs.02-1181. [DOI] [PubMed] [Google Scholar]
- 26.Akbari MR, Khorrami-Nejad M, Aghazadeh Amiri M, Akbarzadeh Baghban A, Khosravi B, Nourizad S. Facial asymmetry in unilateral duane retraction syndrome. Optom Vis Sci. 2019;96:920–4. doi: 10.1097/OPX.0000000000001452. [DOI] [PubMed] [Google Scholar]
- 27.Akbari MR, Sadeghi AM, Ghadimi H, Nikdel M. Outcome of inferior oblique disinsertion versus myectomy in the surgical treatment of unilateral congenital superior oblique palsy. J AAPOS. 2019;23:77. doi: 10.1016/j.jaapos.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 28.Kekunnaya R, Isenberg SJ. Effect of strabismus surgery on torticollis caused by congenital superior oblique palsy in young children. Indian J Ophthalmol. 2014;62:322–6. doi: 10.4103/0301-4738.116468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bagheri A, Eshaghi M. Botulinum toxin injection of the inferior oblique muscle for the treatment of superior oblique muscle palsy. J AAPOS. 2006;10:385–8. doi: 10.1016/j.jaapos.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg MF, Pollard ZF. Treatment of inferior oblique paresis with superior oblique silicone tendon expander. J AAPOS. 2005;9:341–5. doi: 10.1016/j.jaapos.2005.04.003. [DOI] [PubMed] [Google Scholar]


