Background:
Although HIV antiretroviral treatment (ART) access and uptake have increased among racial/ethnic minority individuals, lower rates of ART adherence and viral suppression persist, especially among Black men who have sex with men (BMSM) compared with their White counterparts.
Setting:
Black men who have sex with men living with HIV (BMSM+) residing in Los Angeles County (N = 124) were recruited in-person (eg, clinic) and online (eg, social networking apps).
Methods:
Participants completed a cross-sectional survey measuring demographic characteristics, structural syndemics (poverty, criminal justice involvement, and housing instability), and psychosocial syndemics (mental health and substance use). A text message survey assessed missed doses of ART over the past week. Zero-inflated Poisson regression models were used to evaluate variables associated with the number of missed doses of ART.
Results:
On average, participants missed 1.30 doses of ART (SD = 2.09) and reported structural syndemics: poverty (56.1%), criminal justice involvement (36.6%), housing instability (26.3%), and psychosocial syndemics: childhood sexual abuse (51.8%), intimate partner violence (16.9%), depression (39%), and problem alcohol use (15.5%). After controlling for employment, age, education, and psychosocial syndemics, participants with a one-point increase in structural syndemic indicators were found to be 1.63 times more likely to have missed a dose of ART.
Conclusions:
Structural syndemic were associated with ART nonadherence among BMSM+ after adjusting for demographic and psychosocial factors. HIV treatment interventions that incorporate financial incentives, legal support, and housing may help improve ART adherence among BMSM+. Findings suggest that key priorities to ending the HIV epidemic must include structural interventions that alleviate poverty, eliminate disproportionate policing and criminalization, and end homelessness.
Key Words: HIV, ART, MSM, Black men, syndemics
INTRODUCTION
HIV Treatment Adherence Among Black MSM
Rapid initiation into HIV medical care is crucial to the national plan for “Ending the HIV Epidemic: A Plan for America,” which aims to reduce new infections by 75% in 2025 and by 90% in 2030.1 If adherent to antiretroviral therapy (ART) as prescribed, people living with HIV (PLWH) benefit from fewer opportunistic infections and lower hospitalization, mortality, and morbidity rates.2 High adherence suppresses viremia among PLWH, which helps curb forward HIV transmission. This process is often referred to as treatment as prevention for public health.3,4 National surveillance data indicate that HIV care outcomes, such as viral suppression and linkage to care within a month of diagnosis, for racial/ethnic minority people have been improving.5–7 Lower rates of engagement in care, ART adherence, and viral suppression persist, however, especially among Black PLWH compared with their White counterparts.8–10
Psychosocial and structural factors are implicated in treatment as prevention.11 Psychosocial factors include risk behaviors such as substance use and problem drinking, which are associated with lower ART adherence particularly among young Black men who have sex with men (BMSM).12,13 A study with young adult Black men receiving HIV care, 72% of whom was identified as gay, found that those with depressive symptoms had higher odds of reporting lower ART adherence.14 Experiences of trauma from physical or sexual assault or exposure to extreme violence were also associated with lower adherence among men in a South Carolina sample of 337 PLWH, of whom 77% was Black and 65% was men.15 Structural factors tied to lower adherence among BMSM include homelessness and economic insecurity broadly.16 In a large study of MSM, of whom 289 participants (26%) were Black, financial difficulty was significantly associated with nonadherence.17 A review focused on BMSM with a history of criminal justice involvement considered care continuum outcomes in penal institutions to be a relative success.18 This aligns with an earlier review, examining ART adherence among incarcerated and recently released populations, which found that low rates of engagement in HIV care and viral suppression at entry improved considerably during incarceration.19 Another study found that young BMSM in Chicago with previous criminal justice involvement, relative to counterparts with no such history, had more success along the HIV care continuum, including ART adherence and viral suppression, relative to counterparts with no such history. However, repeated episodes of detainment were associated with worse outcomes.20 Finally, a forthcoming article seems to show that PLWH in Florida with recent incarceration history were least likely to report high medication adherence, compared with those never or distally incarcerated.21
Psychosocial and Structural Syndemic Factors Related to HIV Treatment Engagement
The concept of syndemics, defined by the Centers for Disease Control and Prevention as 2 or more afflictions that interact synergistically and contribute to the excess burden of disease in a population,22 emerged in the mid-1990s when researchers identified closely linked conditions related to increased HIV infection among residents in low-income urban areas.23 Investigators have recently focused their attention toward MSM living with HIV and the impact of psychological syndemic conditions on ART adherence and viral suppression.24–28 These studies demonstrated that an increasing number of psychosocial syndemic factors experienced by MSM was associated with higher odds of ART nonadherence and detectable viral load, even after adjusting for demographic variables such as race, age, and educational level. Of these studies, only one study25 noted differences in viral load values and number of syndemic conditions by race/ethnicity. In this study, Black and Latino MSM had poorer HIV-related health outcomes and higher number of syndemic experiences compared with their White counterparts.25
However, researchers have identified structural factors to be critical in understanding syndemics and their impact on HIV treatment engagement, particularly within communities often left vulnerable to societal forces such as poverty, homelessness, and unemployment.29,30 Yet only a handful of studies have examined these relations directly.22 A qualitative study examining HIV treatment engagement among 23 Black men who have sex with men living with HIV (BMSM+) found that poverty, depression, substance use, and intersectional stigma, defined in this study as the overlapping stigmas associated with race, gender, sexual orientation, HIV status, and other marginalized identities, affected HIV treatment engagement decisions of young BMSM+.31 Quantitative studies assessing the role of multiple structural factors in treatment behaviors focused on select populations of PLWH, including women of color,32 young people,33 injection drug users,34 and men of color who have sex with men.30 These studies broadened the examination of syndemics to include previously defined psychosocial factors and structural factors, including unemployment, poverty, incarceration history, housing instability, and HIV stigma. Structural indicators, counted alongside psychosocial factors, were found to be associated with poor ART adherence, detectable viral load,33,35 and being interrelated, demonstrating a syndemic relationship.36,37 A study of people living with HIV who inject drugs found lower odds of adherence to HIV medication when participants reported 3 or more psychosocial problems and lower likelihood of being virally suppressed when reporting 4 or more psychosocial problems.34 For this study, psychosocial problems encompassed both structural (ie, housing instability and incarceration history) and behavioral (ie, experiences of abuse and psychological distress) factors, which were used to develop a count score by adding the number of experienced psychosocial problems and later examined in association with HIV treatment adherence outcomes.34 Similarly, a recent study among men of color who have sex with men living in Los Angeles County that focused only on structural syndemic conditions, such as current unemployment, housing instability, incarceration history, and remote contact with health care providers, demonstrated that the number of structural syndemic factors experienced were associated with higher odds of sexual HIV transmission risk behaviors and having a detectable viral load for participants living with HIV.30
There is strong evidence that psychosocial syndemics are associated with treatment behaviors and a growing understanding of the role that structural conditions might play in these relations. Yet the differentiation between psychosocial factors and structural conditions, along with its effect on HIV outcomes, is limited.29,30 Therefore, a better understanding of the prevalent structural conditions and psychosocial factors that affect the HIV treatment engagement of BMSM+ is warranted. This study hypothesizes that psychosocial and structural factors would be negatively associated with ART adherence among BMSM+ in LA County.
METHODS
Participants and Procedures
Data for this study come from self-reported responses to a cross-sectional baseline interview from LINX LA, a prospective, randomized comparison trial of a web-based mobile application, which is described in detail elsewhere.38 Participants (N = 124) were recruited using a variety of in-person and virtual strategies, including flyers at HIV and Lesbian, Gay, Bisexual, and Transgender-friendly clinics and postings on social media platforms. To be eligible for the study, participants had to meet the following criteria: (1) be at least 18 years or older; (2) identify as male individual; (3) identify as Black or African American; (4) identify as gay, bisexual, or another sexual minority; (5) own a smartphone; (6) be living with HIV; (7) reside in Los Angeles County; and (8) be able to provide informed consent. Eligibility criteria did not specify cisgender or transgender identity. Participants received $30 for completing the baseline interview. By answering weekly text message surveys about ART adherence, participants were also entered into a monthly raffle, with a chance to win a $100 US Dollars e-gift card. The LINX LA study was approved by the North Campus Institutional Review Board at the University of California, Los Angeles (IRB#17-001615).
Measures
As part of the baseline interview, interviewers guided participants through an online questionnaire, which included items related to demographic characteristics, including age, educational attainment, income, employment status, and place of birth. All participants also completed a Medication Adherence Assessment, 1 week after their baseline assessment. This consisted of a brief text message survey asking, “During the past week, on how many days did you miss taking your medications?” Participants indicated the number of days they missed taking their HIV medication in the past week (range: 0–7).
Structural syndemic factors included poverty, criminal justice involvement, and housing instability. This composite measure was constructed emulating a previous study with similar indicators.39 Poverty was measured using a single binary item and coded “yes” for participants with an annual income below the federal poverty level (FPL; $12,000 US Dollars). FPL is a measure of income issued every year by the Department of Health and Human Services. FPL levels are used to determine eligibility for certain programs and benefits, including savings on Marketplace Health Insurance, Medicaid, and children's health insurance program coverage. Criminal justice involvement was measured using responses to the single item, “In the past 5 years, have any of the following happened to you?” Answer choices included the following: “you were accused of committing a crime”; “you were arrested”; “you were charged with a crime in court or in a hearing before a judge”; and “you received a sentence or probation related to being accused of committing a crime.” Participants who responded affirmatively to any of these answer choices were coded as having involvement with the criminal justice system. Housing instability was measured using a single item asking, “Where have you lived in the past year?” If participants indicated they either were homeless or lived in a shelter, they were coded as being unstably housed. A sum of these items was created to measure structural syndemics (range: 0–3).
Psychosocial syndemic factors included alcohol-related problems, drug-related problems, intimate partner violence (IPV), depression, and childhood sexual abuse (CSA). Problem alcohol use was measured using the 10-item Alcohol Use Disorders Identification Test scale.40 A score of 8 and above indicated alcohol-related problems. Other drug use was measured using the 11-item Drug Use Disorders Identification Test scale.41 A score of 6 and above indicated drug-related problems. IPV was measured using a 4-item scale, with scores ranging from 0 to 20.42 A cutoff of 11 was used to positively code for an experience of IPV. Depression was measured using the Patient Health Questionaire-9, where a score >10 indicated depressive symptoms.43 CSA was measured using the items: “Between the ages of 12 and 16 did you have any sexual experiences with an adult or someone at least 5 years older?” or “Between the ages of 12 and 16 did you have any unwanted sexual experiences?” or “Before the age of 12 years, was the person you had the sexual experience with an adult or someone at least 5 years older than you?” 42 If participants indicated that they had either of the experiences above, then they were coded as having a history of CSA. A sum of these items was created to measure psychosocial syndemics (range: 0–5).
Data Analysis
Zero-inflated Poisson (ZIP) regression models were used to evaluate variables associated with number of missed ART doses among the participants. Because we were interested in understanding the differences between participants who did not miss doses at all (ie, true zeroes and chance zeroes) versus participants who missed at least one dose, a ZIP model was warranted. In addition to the excess zeroes, we also adjusted for overdispersion, comparing a traditional Poisson model with a ZIP model. We used as model selection criteria a lower Akaike Information Criterion/Bayesian Information Criterion in addition to the Vuong test,44 which indicated that the ZIP model fit our data better than a traditional Poisson model. First, independent variables were entered with the outcome variable. Next, we conducted adjusted analyses with the structural syndemic sum as the primary predictor, adjusting for psychosocial syndemics and demographic characteristics. None of the variables were highly correlated with each other, which allowed us to generate the most parsimonious model for our analysis.
RESULTS
Of the 124 participants who completed the baseline interview, 98 (79%) were currently receiving ART, completed the follow-up text message adherence survey, and were included in subsequent analysis. On average, participants missed 1.30 doses of ART (SD = 2.09). Participants ranged in age between 18 and 67 years (mean = 37.5, median = 35, SD = 12.2), and 43.9% was born in Los Angeles. Although we enrolled BMSM, 28.8% of our participants endorsed multiple ethnicities including “Black/African.” More than half (56.1%) reported an annual household income below the FPL, and participants with any form of employment (full-time, part-time, or self-employed) comprised 41.9% of our sample. More than half (51.6%) resided in the urban core of Los Angeles County. Nearly all (95.9%) had access to health insurance at the time of enrollment, and 88.8% of the participants had regular access to a primary care physician (Table 1).
TABLE 1.
Demographic Characteristics of BMSM+ in Los Angeles County on ART Who Responded to Text Message Adherence Survey at 1-Week Postenrollment, 2018–2019 (N = 98)*
| N | % | |
| Born in Los Angeles | 43 | 43.9 |
| Age group | ||
| 18–29 | 28 | 28.9 |
| 30–39 | 34 | 35.1 |
| 40–49 | 15 | 15.5 |
| 50–59 | 14 | 14.4 |
| 60+ | 6 | 6.2 |
| Race/ethnicity† | ||
| Black/African American | 61 | 67.8 |
| Black/African + other ethnicity | 26 | 28.8 |
| Educational attainment | ||
| 9–11 grade | 10 | 10.2 |
| Bachelor’s degree | 15 | 15.3 |
| High-school graduate/GED | 24 | 24.5 |
| Master’s degree | 1 | 1.0 |
| Some college credit but no degree | 36 | 36.7 |
| Technical/vocational or associates | 11 | 11.2 |
| Income below FPL | 55 | 56.1 |
| Employment status†‡ | ||
| Employed—full-time | 13 | 13.3 |
| Employed—part-time | 19 | 19.4 |
| Self-employed | 9 | 9.2 |
| Retired | 4 | 4.1 |
| Unable to work because of disability | 31 | 31.6 |
| Out of work | 20 | 20.4 |
| Student | 7 | 7.1 |
| Access to a health care facility | ||
| Yes, there are 1 or more places | 87 | 88.8 |
| There is NO place | 6 | 6.1 |
| Decline to answer | 5 | 5.1 |
| Current access to health insurance | 94 | 95.9 |
Totals may not add to 100 because of missing data.
Multiple responses accepted, and percentages may exceed 100.
Employment status was assigned by giving preference to any type of employment when multiple other responses were chosen. Students with other positions were included in the respective groups. Individuals who were out of work and had a disability were included in both the groups.
Participants endorsed multiple psychosocial syndemics, including CSA (51.8%), IPV (16.9%), depression (39%), problem alcohol use (15.5%), and problem drug abuse (41%). Our sample also endorsed structural syndemics, including poverty (56.1%), criminal justice involvement (36.6%), and housing instability (26.3%). Bivariate correlations between structural syndemics and psychosocial syndemics were statistically significant (r = 0.27; P = 0.008). Figure 1 depicts the number of psychosocial and structural syndemics reported among the study sample. Nearly one-third (31.7%) of participants reported 2 or more structural syndemic factors; 43.3% of the participants reported 2 or more psychosocial syndemic factors (Table 2).
FIGURE 1.
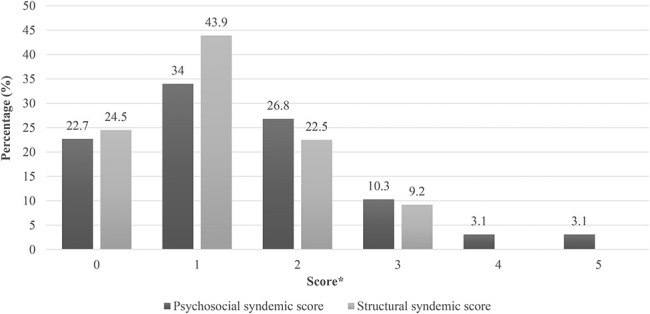
Number of psychosocial and structural syndemics among BMSM living with HIV, 2018–2019. *Scores: psychosocial syndemic scores were measured between 0 and 5, and structural syndemic scores were measured between 0 and 3.
TABLE 2.
Syndemic Conditions Among BMSM+ in Los Angeles County, 2018–2019 (N = 98)*
| N | % | x̄ (σ) | |
| Psychosocial syndemics | 1.4 (1.23) | ||
| Problem alcohol use | 13 | 15.5 | — |
| Other drug use | 34 | 41 | — |
| IPV | 15 | 16.85 | — |
| Depression | 37 | 39 | — |
| CSA | 43 | 51.8 | — |
| Structural syndemics | 1.17 (0.90) | ||
| Poverty | 55 | 56.1 | — |
| Criminal justice involvement | 34 | 36.6 | — |
| Unstable housing | 25 | 26.3 | — |
| Syndemic sum scores | — | ||
| Psychosocial syndemic score | — | ||
| 0 | 22 | 22.7 | — |
| 1 | 33 | 34 | — |
| 2 | 26 | 26.8 | — |
| 3 | 10 | 10.3 | — |
| 4 | 3 | 3.1 | — |
| 5 | 3 | 3.1 | — |
| Structural syndemic score | — | ||
| 0 | 24 | 24.5 | — |
| 1 | 43 | 43.9 | — |
| 2 | 22 | 22.5 | — |
| 3 | 9 | 9.2 | — |
Totals may not add to 100 because of missing data.
ZIP models are summarized in Table 3 and examine the effects of demographic characteristics and syndemic indicators as correlates of treatment adherence (number of missed doses) in the week after enrollment into the study. Bivariate associations between the count outcome variable (number of missed doses) and demographic characteristics and syndemic variables are reported. Unstable housing (count portion of the ZIP model) was statistically significantly associated with the number of missed doses [internal rate of return = 1.68, 95% confidence interval (CI) = 1.12 to 2.53, P = 0.012] and structural syndemic indicators (count portion of the ZIP model) were statistically significantly associated with the number of doses missed (internal rate of return = 1.31, 95% CI = 1.06 to 1.63, P = 0.013).
TABLE 3.
Zero-Inflation Poisson Distribution Assessing Independent Associations Between Treatment Adherence and Demographic and Syndemic Predictors Among BMSM in Los Angeles County, 2018–2019 (N = 98)
| Predictors | Missed Doses in 1-wk Postenrollment | |||
| Unadjusted Model | Adjusted Model | |||
| Exponentiated Count Estimate (95% CI) | Zero-Inflation Exponentiated Coefficients (95% CI) | Exponentiated Count Estimate (95% CI) | Zero-Inflation Exponentiated Coefficients (95% CI) | |
| Demographics | ||||
| Age | 0.98 (0.97 to 1.01) | 1 (0.96 to 1.04) | 1.01 (0.97 to 1.03) | 1.01 (0.95 to 1.077) |
| Educational attainment* | 0.74 (0.5 to 1.08) | 0.88 (0.36 to 2.12) | 0.77 (0.49 to 1.18) | 0.66 (0.23 to 1.93) |
| Employment status† | 1.08 (0.72 to 1.64) | 1.14 (0.47 to 2.76) | 1.39 (0.79 to 2.48) | 1.83 (0.43 to 7.7) |
| Psychosocial syndemics | ||||
| Problem alcohol use | 0.55 (0.29 to 1.04) | 0.21 (0.03 to 1.49) | — | — |
| Other drug use | 0.79 (0.52 to 1.21) | 0.38 (0.14 to 1.01) | — | — |
| IPV | 1.3 (0.85 to 2.0) | 0.39 (0.12 to 1.3) | — | — |
| Depression | 1.17 (0.79 to 1.75) | 0.66 (0.275 to 1.61) | — | — |
| CSA | 1.07 (0.7 to 1.63) | 0.75 (0.3 to 1.89) | — | — |
| Structural syndemics | ||||
| Poverty | 1.36 (0.91 to 2.03) | 1.1 (0.46 to 2.62) | — | — |
| Criminal justice involvement | 1.27 (0.84 to 1.91) | 0.54 (0.21 to 1.33) | — | — |
| Unstable housing‡ | 1.68‡ (1.12 to 2.53) | 1.3 (0.49 to 3.4) | — | — |
| Structural syndemic score‡ | 1.31‡ (1.06 to 1.63) | 0.96 (0.59 to 1.55) | 1.63‡ (1.17 to 2.25) | 1.5 (0.63 to 3.6) |
| Psychosocial syndemic score | 0.99 (0.87 to 1.14) | 0.72 (0.49 to 1.03) | 0.86 (0.71 to 1.04) | 0.56 (0.32 to 0.99) |
Employment status compares individuals with any kind of employment with unemployed individuals.
Educational attainment compares individuals with high school + education with those with or below high-school education.
Indicates P < 0.05.
We entered structural syndemics as a score (0–3) in our adjusted model. The association between structural syndemics remained statistically significant after adjusting for employment, age, education, and psychosocial syndemics in the count portion of the model in the expected direction, indicating that structural syndemics increase the odds of missed doses among our participants. However, psychosocial syndemics did not predict the number of missed doses either independently or in the adjusted model. The estimated rate ratio for a one-unit increase in structural syndemic score, given the other variables are held constant in the model, was 1.63. This means that as participants' syndemic score increased by one point, the mean number of missed doses would be expected to increase by a factor of 1.63 while holding constant psychosocial syndemics, age, and employment (P < 0.05).45
DISCUSSION
Results from our study add to the limited but growing literature examining psychosocial and structural syndemics associated with HIV adherence among MSM,25,29 particularly BMSM+.30 Although previous research has focused largely on psychosocial factors as drivers of elevated rate of HIV among BMSM,46 this study uses syndemics theory, which follows the tenet that disease clustering may be derived from structural conditions of inequity, poverty, and stigmatization and not just from psychosocial experiences.23,30 As such, this study builds on recent literature in which structural conditions are examined separately from psychosocial conditions to better understand the pathways to differential biological and psychological outcomes among populations left vulnerable to various social conditions.23,29,30,39
Studies using syndemics theory center on interrelated psychosocial factors, including CSA, anxiety disorders, depression, alcohol, and substance use, to examine HIV treatment engagement among MSM.25,47 Previous studies demonstrate a marked decline in HIV treatment engagement among MSM as the number of psychosocial syndemics increased.25,27 Previous research also indicates that psychosocial syndemics negatively affect BMSM because trauma and oppression may reduce the ability of BMSM to build supportive interpersonal and community networks.31,48 Our study results differ from these findings in that we did not find psychosocial syndemic factors to be associated with worse HIV treatment adherence. Although the sample size of this study may account for the nonsignificant association (see limitations), these results may be indicative of the relative importance of structural forces (eg, poverty, criminal justice involvement, and housing instability) in the lives of study participants compared with that of psychosocial factors. After adjusting for employment, age, education, and psychosocial syndemic factors, we found that the structural syndemic factors of poverty, criminal justice involvement, and housing instability increased the odds of missed ART doses among participants. These results support the findings of others that interrelated structural factors, such as unemployment, limited health care access, incarceration history, poverty, and housing instability, are associated with poorer HIV treatment engagement among MSM,30,31,35 particularly BMSM+.14,49 Previous research demonstrates that BMSM+ may delay resource help-seeking.50,51 The intersecting stigma of HIV serostatus, race/ethnicity, and sexual orientation may play a role in reducing HIV care engagement among BMSM+ because they are shown to limit the utilization of social support networks and increase depressive symptoms in this population.51,52 Low health care engagement among BMSM+ has been associated with anticipated HIV stigma after diagnosis, and prejudicial sentiments before diagnosis is predictive of HIV stigma.53 Additional reasons for reduced ART adherence may include stigma associated with disability54 and stigma associated with accessing disability benefits because it is seen as a form of welfare fraud.55
Our research findings are subject to several limitations. First, the sample size is small and may have prevented the detection of statistically significant effects. This is one possible explanation for not finding statistically significant associations between psychosocial syndemics and ART adherence, which has been demonstrated in the previous literature.24 The data are cross-sectional; we cannot make causal inference as to the direction of the associations described earlier. In addition, all data are based on self-report, which is less desirable for measuring ART medication adherence than other methodologies.56,57 Interviewer-administrated surveys may also have introduced social desirability bias into the data.58 Using text message surveys to measure adherence 1 week after the baseline assessment may have introduced bias, priming participants to overreport medication adherence. That said, this methodology has been shown to improve recall bias, which may arise when PLWH are asked to describe medication adherence retrospectively over longer periods of time.59,60 We also recognize that structural syndemic factors used in our analyses are captured through documenting individual outcomes. A more nuanced approach to measuring structural syndemic factors may be warranted; in addition, future research may benefit from examining HIV stigma as part of the analyses. Despite these limitations, our data contribute to a growing body of literature on syndemics and ART medication adherence among BMSM+.
Policy Implications and Future Research Directions
In the United States, events in the past year related to racial justice movements and the global COVID-19 pandemic have exposed useful pillars to framing our work in addressing HIV treatment engagement among BMSM+ and other communities disproportionately affected by HIV. First, we recognized that the negative impact of structural racism often falls on individuals. The burden of dismantling institutionalized racism, however, should lay in the hands of those in power who can address its structural manifestations. Second, we recognized that protecting individuals from homelessness during the COVID-19 crisis, including measures to halt evictions and increase resources to fund public social safety net and housing programs, was politically feasible because these measures were framed as key public health interventions to address the spread of COVID-19.61 This is instructive in our goal to reach our nation's Ending the HIV Epidemic goals. We must frame and further document how helping individuals achieve and/or maintain housing stability is not only a form of health care but also critical to maintaining public health. Disparities in HIV related to intersections of race/ethnicity offer proof that racism is a public health emergency that requires structural intervention. If we fail to learn, grow, and integrate key lessons, PLWH and especially people most vulnerable to disparities in treatment outcomes will face greater risk of morbidity and mortality.
Taken together, this research supports the need for more broad-based HIV treatment interventions to support BMSM+, including those that tackle poverty, disproportionate rates in policing and criminalization, and housing instability. In theory, eligible PLWH have access to additional safety net programs to address poverty and housing instability. They include federally funded disability benefits (eg, financial assistance) for individuals whose conditions are disabling62 and wraparound services for low-income PLWH funded by the Ryan White Care Act.63 Benefits include a panoply of social services (eg, health care, social support, food programs, and legal services), coverage for drug costs, and health, behavioral health, and substance use services. In addition, federal, state, and local funding facilitate access to emergency, transitional, permanent housing, and long-term housing subsidies (eg, Section 8) for eligible participants.64–67 When theory meets reality, however, problems arise. The costs (ie, time and effort) associated with seeking assistance from social welfare programs are disproportionately high because eligibility guidelines remain strict and applicants must engage with problematic bureaucracy within administrating institutions.68 The reality, too, is that available benefits are often substandard because they fail to lift people out of poverty and into stable and habitable housing environments. Barring significant changes to these trends, however, greater investment in understanding the specific needs of PLWH who are justice involved is a clear direction for future work. Recent efforts to eliminate disproportionate policing and the criminalization of communities of color are a starting point for structural change.
ACKNOWLEDGMENTS
The authors acknowledge the contributions of the community advisory board (CAB) members, many of whom are Black LGBTQ individuals. They also thank their community partners, including APLA Health and the AMAAD Institute for their assistance in coordinating the study. They also thank UCLA staff and affiliates for their assistance in coordinating the study and assisting with manuscript preparation, including Robert Gamboa, Kelly Gluckman, Maynard Hearns, Shellye Jones, Gregory Victorianne, Giselle Ruballos, Elizabeth S. C. Wu, Nina Young, Rosalia Alvarado, Sidra Rashid, Christian Paneda, Rae Jones, Sharon Lau, Tiffany Luu, Heliud Garcia, Arthur Sun, Paulette Orhii, and Jack Hjerpe.
Footnotes
Supported by the California HIV/AIDS Research Program (HD15-LA-061) and the Center for HIV Identification, Prevention, and Treatment Services (CHIPTS). R. Beltran is supported by the National Institutes of Health (T32MH080634). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors have no conflicts of interest to disclose.
Contributor Information
Raiza Beltran, Email: rmbeltran@mednet.ucla.edu.
Saanchi V. Shah, Email: saanchi_shah@icloud.com.
Luisita Cordero, Email: luisitacordero@gmail.com.
Gerald Garth, Email: gerald@amaad.org.
Terry Smith, Email: tsmith@apla.org.
Bianca D. M. Wilson, Email: wilsonb@law.ucla.edu.
Ayako M. Ochoa, Email: amochoa@luskin.ucla.edu.
REFERENCES
- 1.U.S. Department of Health & Human Services. What is “Ending the HIV Epidemic: A Plan for America?” HIV.gov; 2021. Available at: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed March 24, 2021. [Google Scholar]
- 2.Oguntibeju OO. Quality of life of people living with HIV and AIDS and antiretroviral therapy. HIV AIDS (Auckl). 2012;4:117–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV [fact sheet]. 2020. Available at: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf. Accessed March 24, 2021.
- 4.U.S. Department of Health & Human Services. HIV Treatment as Prevention. HIV.gov; 2020. Available at: https://www.hiv.gov/tasp. Accessed March 24, 2021. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2014. 2016. Available at: http://www.cdc.gov/hiv/library/reports/surveillance/. Accessed May 29, 2021.
- 6.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2015. 2017. Available at: http://www.cdc.gov/hiv/library/reports/surveillance/. Accessed May 29, 2021.
- 7.Centers for Disease Control and Prevention. Core indicators for monitoring the ending the HIV Epidemic initiative, data reported through December 2019. 2020. Available at: https://www.cdc.gov/hiv/library/reports/surveillance-data-tables/vol-1-no-1/index.html. Accessed May 29, 2021.
- 8.Nance RM, Delaney JAC, Simoni JM, et al. HIV viral suppression trends over time among HIV-infected patients receiving care in the United States, 1997 to 2015: a cohort study. Ann Intern Med. 2018;169:376–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beer L, Mattson CL, Bradley H, et al. Understanding cross-sectional racial, ethnic, and gender disparities in antiretroviral use and viral suppression among HIV patients in the United States. Medicine (Baltimore). 2016;95:e3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simoni JM, Huh D, Wilson IB, et al. Racial/ethnic disparities in ART adherence in the United States: findings from the MACH14 study. J Acquir Immune Defic Syndr. 2012;60:466–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maulsby C, Millett G, Lindsey K, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18:10–25. [DOI] [PubMed] [Google Scholar]
- 12.Voisin DR, Quinn K, Kim DH, et al. A longitudinal analysis of antiretroviral adherence among young Black men who have sex with men. J Adolesc Health. 2017;60:411–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mutchler MG, Bogart LM, Klein DJ, et al. Age matters: differences in correlates of self-reported HIV antiretroviral treatment adherence between older and younger Black men who have sex with men living with HIV. AIDS Care. 2019;31:965–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hightow-Weidman L, LeGrand S, Choi SK, et al. Exploring the HIV continuum of care among young black MSM. PLoS One. 2017;12:e0179688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brown MJ, Harrison SE, Li X. Gender disparities in traumatic life experiences and antiretroviral therapy adherence among people living with HIV in South Carolina. AIDS Behav. 2019;23:2904–2915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Creasy SL, Henderson ER, Bukowski LA, et al. HIV testing and ART adherence among unstably housed Black men who have sex with men in the United States. AIDS Behav. 2019;23:3044–3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oh DL, Sarafian F, Silvestre A, et al. Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among White, Hispanic, and Black men in the MACS cohort. J Acquir Immune Defic Syndr. 2009;52:290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harawa NT, Brewer R, Buckman V, et al. HIV, sexually transmitted infection, and substance use continuum of care interventions among criminal justice-involved Black men who have sex with men: a systematic review. Am J Public Health. 2018;108:e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105:e5–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider JA, Kozloski M, Michaels S, et al. Criminal justice involvement history is associated with better HIV care continuum metrics among a population-based sample of young black MSM. AIDS. 2017;31:159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ibañez GE, Zhou Z, Algarin AB, et al. Incarceration history and HIV care among individuals living with HIV in Florida, 2014–2018. AIDS Behav. 2021;25:3137–3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson PA, Nanin J, Amesty S, et al. Using syndemic theory to understand vulnerability to HIV infection among Black and Latino men in New York City. J Urban Health. 2014;91:983–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singer M, Bulled N, Ostrach B, et al. Syndemics and the biosocial conception of health. Lancet. 2017;389:941–950. [DOI] [PubMed] [Google Scholar]
- 24.Blashill AJ, Bedoya CA, Mayer KH, et al. Psychosocial syndemics are additively associated with worse ART adherence in HIV-infected individuals. AIDS Behav. 2015;19:981–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Friedman MR, Stall R, Plankey M, et al. Effects of syndemics on HIV viral load and medication adherence in the multicenter AIDS cohort study. AIDS. 2015;29:1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harkness A, Bainter SA, O'Cleirigh C, et al. Longitudinal effects of syndemics on ART non-adherence among sexual minority men. AIDS Behav. 2018;22:2564–2574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pantalone DW, Valentine SE, Woodward EN, et al. Syndemic indicators predict poor medication adherence and increased health care utilization for urban HIV-positive men who have sex with men. J Gay Lesbian Ment Health. 2018;22:71–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walters SM, Braksmajer A, Coston B, et al. A syndemic model of exchange sex among hiv-positive men who have sex with men. Arch Sex Behav. 2020;49:1965–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsai AC, Venkataramani AS. Syndemics and health disparities: a methodological note. AIDS Behav. 2016;20:423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quinn B, Gorbach PM, Okafor CN, et al. Investigating possible syndemic relationships between structural and drug use factors, sexual HIV transmission and viral load among men of colour who have sex with men in Los Angeles County. Drug Alcohol Rev. 2020;39:116–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quinn KG, Reed SJ, Dickson-Gomez J, et al. An exploration of syndemic factors that influence engagement in HIV care among Black men. Qual Health Res. 2018;28:1077–1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan KA, Messer LC, Quinlivan EB. Substance abuse, violence, and HIV/AIDS (SAVA) syndemic effects on viral suppression among HIV positive women of color. AIDS Patient Care STDs. 2015;29(suppl 1):S42–S48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kuhns LM, Hotton AL, Garofalo R, et al. An index of multiple psychosocial, syndemic conditions is associated with antiretroviral medication adherence among HIV-positive youth. AIDS Patient Care STDs. 2016;30:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mizuno Y, Purcell DW, Knowlton AR, et al. Syndemic vulnerability, sexual and injection risk behaviors, and HIV continuum of care outcomes in HIV-positive injection drug users. AIDS Behav. 2015;19:684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glynn TR, Safren SA, Carrico AW, et al. High levels of syndemics and their association with adherence, viral non-suppression, and biobehavioral transmission risk in Miami, a U.S. city with an HIV/AIDS epidemic. AIDS Behav. 2019;23:2956–2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee JS, Safren SA, Bainter SA, et al. Examining a syndemics network among young Latino men who have sex with men. Int J Behav Med. 2020;27:39–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Turpin R, Slopen N, Boekeloo B, et al. Testing a syndemic index of psychosocial and structural factors associated with HIV testing among black men. J Health Care Poor Underserved. 2020;31:455–470. [DOI] [PubMed] [Google Scholar]
- 38.Miyashita Ochoa A, Paneda CC, Wu ESC, et al. A community-developed, web-based mobile app intervention addressing social work and legal needs of Black sexual minority men living with HIV: protocol for a randomized comparison trial. JMIR Res Protoc. 2021;10:e19770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blashill AJ, Brady JP, Rooney BM, et al. Syndemics and the PrEP cascade: results from a sample of young Latino men who have sex with men. Arch Sex Behav. 2020;49:125–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction. 1993;88:791–804. [DOI] [PubMed] [Google Scholar]
- 41.Berman AH, Bergman H, Palmstierna T, et al. DUDIT: The Drug Use Disorders Identification Test Manual Version 1.0. Karolinska Institute Department of Clinical Neuroscience; 2003. Available at: https://paihdelinkki.fi/sites/default/files/duditmanual.pdf. Accessed October 8, 2021. [Google Scholar]
- 42.Williams JK, Wilton L, Magnus M, et al. Relation of childhood sexual abuse, intimate partner violence, and depression to risk factors for HIV among Black men who have sex with men in 6 US cities. Am J Public Health. 2015;105:2473–2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–359. [DOI] [PubMed] [Google Scholar]
- 44.Vuong QH. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica. 1989;57:307–333. [Google Scholar]
- 45.UCLA Institute for Digital Research & Education Statistical Consulting. Poisson regression. Available at: https://stats.idre.ucla.edu/stata/dae/poisson-regression/. Accessed May 23, 2021.
- 46.Millett GA, Flores SA, Peterson JL, et al. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–2091. [DOI] [PubMed] [Google Scholar]
- 47.Harkness A, Bainter SA, O'Cleirigh C, et al. Longitudinal effects of syndemics on HIV-positive sexual minority men’s sexual health behaviors. Arch Sex Behav. 2019;48:1159–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reed SJ, Miller RL. Thriving and adapting: resilience, sense of community, and syndemics among young Black gay and bisexual Men. Am J Community Psychol. 2016;57:129–143. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan PS, Knox J, Jones J, et al. Understanding disparities in viral suppression among Black MSM living with HIV in Atlanta Georgia. J Int AIDS Soc. 2021;24:e25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miyashita Ochoa A, Hasenbush A, Wilson BDM, et al. The Legal Needs of People Living With HIV: Evaluating Access to Justice in Los Angeles. The Williams Institute, UCLA School of Law; 2015. Available at: https://williamsinstitute.law.ucla.edu/publications/legal-needs-people-living-hiv/. Accessed October 8, 2021. [Google Scholar]
- 51.Quinn K, Dickson-Gomez J, Broaddus M, et al. “It's almost like a crab-in-a-barrel situation”: stigma, social support, and engagement in care among Black men living with HIV. AIDS Educ Prev. 2018;30:120–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bogart LM, Wagner GJ, Galvan FH, et al. Perceived discrimination and mental health symptoms among Black men with HIV. Cultur Divers Ethnic Minor Psychol. 2011;17:295–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Eaton LA, Earnshaw VA, Maksut JL, et al. Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. J Behav Med. 2018;41:458–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc Sci Med. 2014;103:1–6. [DOI] [PubMed] [Google Scholar]
- 55.Hansen H, Bourgois P, Drucker E. Pathologizing poverty: new forms of diagnosis, disability, and structural stigma under welfare reform. Soc Sci Med. 2014;103:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Martin S, Elliott-DeSorbo DK, Calabrese S, et al. A comparison of adherence assessment methods utilized in the United States: perspectives of researchers, HIV-infected children, and their caregivers. AIDS Patient Care STDs. 2009;23:593–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Samet JH, Sullivan LM, Traphagen ET, et al. Measuring adherence among HIV-Infected persons: is MEMS consummate technology? AIDS Behav. 2001;5:21–30. [Google Scholar]
- 58.Latkin CA, Mai NVT, Ha TV, et al. Social desirability response bias and other factors that may influence self-reports of substance use and HIV risk behaviors: a qualitiative study of drug users in Vietnam. AIDS Educ Prev. 2016;28:417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Crankshaw T, Corless IB, Giddy J, et al. Exploring the patterns of use and feasibility of using cellular phones for clinic appointment reminders and adherence messages in an antiretroviral treatment clinic, Durban, South Africa. AIDS Patient Care STDs. 2010;24:729–734. [DOI] [PubMed] [Google Scholar]
- 60.Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25:825–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention. Interim guidance for homeless service providers to plan and respond to Coronavirus disease 2019 (COVID-19). 2021. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/homeless-shelters/plan-prepare-respond.html. Accessed March 24, 2021.
- 62.Social Security Administration. Overview of our disability programs. Available at: https://www.ssa.gov/redbook/eng/overview-disability.htm. Accessed March 25, 2021.
- 63.Health Resources and Services Administration. About the ryan white HIV/AIDS program. 2020. Available at: https://hab.hrsa.gov/about-ryan-white-hivaids-program/about-ryan-white-hivaids-program. Accessed March 24, 2021.
- 64.US Department of Housing and Urban Development. Housing Oppportunities for Persons With AIDS. HUD Exchange; 2021. Available from: https://www.hudexchange.info/programs/hopwa/. Accessed March 24, 2021. [Google Scholar]
- 65.California Department of Social Services. Project Roomkey/Housing and homelessness COVID response. 2021. Available at: https://www.cdss.ca.gov/inforesources/cdss-programs/housing-programs/project-roomkey. Accessed March 24, 2021.
- 66.Health Services Los Angeles County. Whole person care—Los Angeles. Available at: https://dhs.lacounty.gov/whole-person-care/. Accessed March 24, 2021.
- 67.Alliance for Housing and Healing. Emergency financial assistance. 2019. Available at: https://alliancehh.org/programs/emergencyfinancialassistance/. Accessed March 24, 2021.
- 68.Whittle HJ, Palar K, Ranadive NA, et al. “The land of the sick and the land of the healthy”: disability, bureaucracy, and stigma among people living with poverty and chronic illness in the United States. Soc Sci Med. 2017;190:181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]


