Abstract
The purpose of this study was to explore the differences in anxiety and depressive symptoms between older adult pet owners and non-pet owners after accounting for various correlates. Research findings on the anxiety-relieving and antidepressant effects of late-life pet ownership are mixed and limited. This may be due in part to various characteristics that impact the likelihood of owning a pet. Propensity score matching was used to pair 169 pet owners with 169 non-pet owners aged 70 to 91 years who participated in the University of Alabama at Birmingham Study of Aging. One set of propensity scores was created using age, sex, race, rurality, marital status, and income, as well as self-reported health, difficulty with activities of daily living, and difficulty with instrumental activities of daily living. A second set of scores was created using age, sex, race, rurality, marital status, and income. Multiple linear regression analyses were then used to explore the relation between pet ownership status and anxiety or depressive symptoms, controlling for the other symptoms. Pet ownership was significantly associated with lower self-reported anxiety symptoms (β = −0.14) but not depressive symptoms (β = −0.03) in the data matched without health variables. When propensity score matching included health variables, pet ownership was related to neither symptoms of anxiety (β = −0.08) nor depression (β = 0.05). These results suggest that owning a pet in later life is related to fewer anxiety symptoms, over and above the impact of depressive symptoms, even after accounting for various demographic and economic covariates. However, general and functional health appear to be critical to this relation, but the direction of this relation could not be determined from our analyses (i.e., it is not clear whether the relation between pet ownership and anxiety symptoms is confounded by, mediates, or is mediated by health). This study is the first large-scale analysis to find a significant relation between pet ownership and fewer anxiety symptoms in older adults.
Keywords: Arthritis Impact Measurement Scales 2, human–animal interaction, older adults, propensity score matching, UAB Study of Aging
In the United States, 67% of households own a pet (American Pet Products Association [APPA], 2019). Pet ownership is still common in late life, though less widespread, with the prevalence of pet ownership ranging from 24% to 40%, with prevalence declining with advancing age (Friedmann et al., 2018; Mueller et al., 2018; Research and Markets, 2017).
A large proportion of human–companion animal interaction research is on animal-assisted activities (AAA; brief, informal interactions with an animal administered by a non-therapist), animal-assisted therapies (AAT; brief, structured interactions with an animal administered by a therapist or other professional for treatment purposes), and pet ownership. Pet ownership comes with additional responsibilities that the brief interactions of AAA and AAT do not. Therefore, it is important to not generalize findings from AAA and AAT studies to pet ownership, nor to encourage older adults to own pets owing to the positive benefits provided from AAA and AAT.
The results of research on the psychological consequences of pet ownership for older adults are mixed and limited. Some studies on older adult pet ownership have elucidated benefits of owning a pet. For example, older adults who were current or past dog and/or cat owners in Japan reported greater happiness and fewer depressive symptoms than older adults who never owned these pets (Taniguchi et al., 2018). Further, older adult pet owners were 36% less likely to report loneliness compared with non-pet owners (Stanley et al., 2014), and owning a pet in late life buffered against depressive symptoms and loneliness after the death of a spouse (Carr et al., 2019). In non-older adult samples of military members and veterans, being paired with a service dog has been found to reduce depressive symptoms (O’Haire & Rodriguez, 2018; Yarborough et al., 2017).
There are also findings that suggest owning a pet in older adulthood may be detrimental to one’s mental health. Specifically, older adults without pets have fewer symptoms of depression than dog and cat owners, and cat owners have more symptoms of depression than dog owners and non-pet owners (Enmarker et al., 2015; Parslow et al., 2005). A more recent study, conducted in England, also found that older adult dog owners had more symptoms of depression, but the prevalence of these symptoms did not change over time in relation to pet ownership status (Sharpley et al., 2020). Further, research shows that pet owners aged 50 and older are almost twice as likely to report historical symptoms of depression as non-pet owners (Mueller et al., 2018). Additionally, higher levels of attachment to pets correspond to more symptoms of depression in older adults (Miltiades & Shearer, 2011).
Research on how pet ownership relates to symptoms of anxiety in late life is lacking; a recent systematic review found only two studies on this topic (Gee & Mueller, 2019), with one being a case study (Likourezos et al., 2002) and the other finding no differences in late-life anxiety based on pet ownership among 68 older Australians (Bennett et al., 2015). Further, a study examining older adult physical activity and dog ownership found non-dog owners to report more symptoms of anxiety than dog owners, although this difference was not statistically significant (p = 0.08; Feng et al., 2014). Another analysis of Australians aged 60 to 64 years found no difference in anxiety symptoms between individuals who own/care for pets and those who do not (Parslow et al., 2005). The literature on the relation between anxiety and pet ownership across the lifespan is also sparse, focusing more on stress than anxiety (Bergen-Cico et al., 2018; González Ramírez & Landero Hernández, 2014; Sugawara et al., 2012).
The literature on the association between physical health and pet ownership in late life is also mixed (see Gee & Mueller, 2019, for a review). Some research shows significant associations between better physical health and pet ownership in late life (Netting et al., 1988; Raina et al., 1999). For example, older adult dog owners who regularly walk their dogs report better physical functioning (e.g., housework, climbing stairs, rising from a chair, lifting, etc.) than non-dog owners or dog owners who do not regularly walk their dogs (Gretebeck et al., 2013). Further, older adult dog owners are significantly more active and fit than non-dog owners (Feng et al., 2014; Taniguchi et al., 2018). A small, recent study of older adult pet owners (predominately dog owners) found that pets may prompt engagement in physical activity throughout the day, and on average, this sample of pet owners walked approximately 14,000 steps per day (Peacock et al., 2019). Additionally, owning a pet (either a dog or a cat) in late life helps maintain and/or enhance physical functioning in a one-year span relative to not owning one of these pets (Raina et al., 1999).
On the other hand, other research shows that older adult pet owners have worse or no different physical health functioning than non-pet owners. For example, Parslow and colleagues (2005) found that pet owners aged 60 to 64 years have worse physical health than non-pet owners. And in an analysis accounting for demographic variables, social support, smoking, and exercise, there was not a significant difference between older adult pet owners’ and non-pet owners’ physical health (Winefield et al., 2008). Further, pet ownership, specifically cat ownership, significantly predicts hospital readmission and/or death in the year following hospitalization for acute coronary syndrome for individuals aged 28 to 92 years (Parker et al., 2010). It is possible that the mixed findings regarding the physical and psychological consequences of owning a pet is confounded by variables that may impact the likelihood of owning a pet, physical health, and mental health.
Numerous factors are associated with pet ownership, and these factors may confound comparisons between pet owners and non-pet owners (Crossman & Kazdin, 2016; Saunders et al., 2017). For example, owning a pet entails completing various pet-care responsibilities, and therefore, individuals who experience difficulty completing activities of daily living (ADLs) or instrumental activities of daily living (IADLs) for themselves may be less likely to own a pet due to the additional burden of caring for a pet (Raina et al., 1999). Further, the prevalence of pet ownership decreases in later adulthood: individuals aged 50 to 84 years are significantly more likely to own pets than individuals aged 85 and older (Mueller et al., 2018). Saunders and colleagues (2017) found other demographic differences between pet owners and non-pet owners: pet owners were more likely to live in more rural areas and be female, White, and married. Further, pet owners report better general health, and dog owners are more likely to have higher household incomes than non-dog owners (Saunders et al., 2017). It is important that research on pet ownership account for differences in physical health as well as demographic and economic factors when attempting to determine the psychological consequences of pet ownership.
The purpose of the current study was to explore the differences in anxiety and depressive symptoms between older adult pet owners and non-pet owners after accounting for covariates that may impact one’s pet ownership status, anxiety, and depressive symptoms. Additionally, this is the first large-scale study we are aware of to examine the association between pet ownership and anxiety in older Americans.
Methods
Participants
Participants were drawn from 522 older adults, aged 70 to 91 years, in the University of Alabama at Birmingham (UAB) Study of Aging (SOA; Allman et al., 2006; Peel et al., 2005). The UAB SOA is a longitudinal study of 1,000 community dwelling Medicare beneficiaries (age 65 years and over at baseline in 1999 to 2001) residing in five central Alabama counties. The UAB SOA oversampled participants who were Black, rural residents, and male in order to ensure a demographically diverse sample. Individuals who resided in nursing homes or were unable to make their own appointments were excluded from participation in the UAB SOA. At baseline, participants were interviewed in their homes using standardized questionnaires, which included assessment of participants’ medical history, physical functioning, demographics, mental health, cognitive functioning, and mobility. Follow-up interviews occurred via telephone every six months for 102 months post-baseline (Allman et al., 2006; Peel et al., 2005). Participants were included in the present, cross-sectional analyses if they had complete data at the fourth- and fifth-year follow-ups (2004 to 2006) as the variables of interest were only measured together in this time frame. The UAB SOA was approved by the UAB Institutional Review Board (X960304001) and the present secondary analyses were granted exemption by the Mississippi State University Institutional Review Board (IRB-19-267).
One set of propensity scores was created using participants’ age, sex, race, rurality, marital status, and income as well as self-reported health, ADLs, and IADLs. Hereafter, this match is referred to as “Match 1 with Health Variables.” A second set of matched participants included the variables of age, sex, race, rurality, marital status, and income. This match is referred to as “Match 2 without Health Variables” hereafter. Theoretically, there are two ways these health variables (defined here as self-reported health, ADLs, and IADLs) and pet ownership may be influencing each other. One possibility is that pet ownership improves health (e.g., increased time walking, more movement within the home); the other possibility is that better health improves the likelihood of owning a pet (e.g., more confidence in one’s ability to take care of the pet). These theoretical possibilities have implications for how health should be included in the matching procedure. If physical health increases the likelihood of pet ownership, the analysis including physical health as a matching factor is most appropriate. However, if pet ownership improves physical health, the analysis matching only on demographic and economic characteristics is most appropriate. As the literature base on the causal relation between pet ownership and physical health is fairly limited, we present both matching options.
Two datasets were created using the nearest-neighbor method and 1:1 matches between 169 pet owners (100% of pet owners) with 169 non-pet owners (48% of non-pet owners). Propensity score matching (PSM) has recently been encouraged in the field of human–animal interaction research (Crossman & Kazdin, 2016; Saunders et al., 2017). PSM was completed in the statistical program R using the MatchIt package (Ho et al., 2011). With this sample size, the analyses were powered to detect effects of 0.31 or larger, which is between a small and medium effect size.
Materials
At the fourth-year follow-up, participants reported demographic information that included their age, sex (0 = male, 1 = female), race (0 = White, 1 = Black), rurality (0 = urban, 1= rural), marital status (1 = married, 2 = widowed, 3 = separated, 4 = divorced, 5 = never married), and annual income range (0 = less than $5,000 to 11 = $150,000 or more). At the fifth-year follow-up, self-reported health was measured on a 5-point Likert scale, with 5 indicating excellent health and 1 indicating poor health. Participants were asked if they had difficulty with six IADLs and nine ADLs, and if so, participants rated the degree of difficulty on a 3-point Likert scale (1 = some, 2 = a lot, 3 = unable to do). These scores were summed to provide total difficulty ratings for both IADLs and ADLs, with higher scores indicating greater difficulty. Pet ownership status was also assessed (0 = no, 1 = yes).
At the fifth-year follow-up, anxiety symptoms were measured using five items from the Arthritis Impact Measurement Scales 2 (AIMS2; Meenan et al., 1992) that assess participants’ level of tension. The AIMS2 Level of Tension scale is a revision of the Arthritis Impact Measurement Scales 1 Anxiety scale (Meenan et al., 1980), which itself is an adaptation of the anxiety measure used in Rand’s Health Insurance Study (Brook et al., 1979). Sample items on the AIMS2 include “How often have you felt tense or high strung?” and “How often have you been bothered by nervousness or your nerves?” Each item is scored on a 5-point Likert scale, and total scores range from 5 (no tension or anxiety) to 25 (very high tension and anxiety), although no clinical cut-off has been established for this measure. It should be noted that one item from the AIMS2 Level of Tension scale (How often have you felt calm and peaceful?) was presented to participants as a 6-point Likert scale (1 = all of the time, 2 = most of the time, 3 = a good bit of the time, 4 = some of the time, 5 = a little bit of the time, 6 = none of the time). In order to conform to AIMS2 scoring guidelines, the 6-point scale was recoded into the AIMS2 5-point scale (1 = all of the time became 5 = always, 2 = most of the time and 3 = a good bit of the time became 4 = very often, 4 = some of the time became 3 = sometimes, 5 = a little bit of the time became 2 = almost never, and 6 = none of the time became 1 = never).
Depressive symptoms were measured at the fifth-year follow-up using the Geriatric Depression Scale – Short Form (GDS-SF; Sheikh & Yesavage, 1986). The GDS-SF is a validated 15-item questionnaire comprised of yes/no questions used to screen for depression in older adults. Scores above 5 are suggestive of depression and scores above 10 are highly indicative of depression, though scores on the GDS-SF were treated as continuous for the present analyses.
Data Analyses
PSM using the nearest neighbor method was used to match pet owners and non-pet owners on several variables. Two matches were conducted: Match 1 with Health Variables and Match 2 without Health Variables. Data from the matched participants were then analyzed using multiple linear regressions to examine the relation between pet ownership status, depressive symptoms, and symptoms of anxiety while controlling for the overlap between these two symptom clusters.
Results
Match 1 with Health Variables
Match 1 with Health Variables included 169 pet owners and 169 non-pet owners for a final sample size of 338. Thus, 184 non-pet owners were not included in the regression analyses. Overall, PSM was successful in that matched variables were not significantly different between groups (see Table 1), and the distribution of propensity scores is depicted in Figure 1. Of this matched sample, 80.5% endorsed being in good to excellent health, 51.2% endorsed earning $16,000 to $19,999 or less annually, and participants were predominately married (53.0%) or widowed (39.4%). Relative to excluded participants, included participants (matched pet owners and non-pet owners combined) were more likely to be male (47.9% vs 42.4%), rural residents (60.1% vs 33.7%), and White (60.1% vs 34.2%). Bivariate correlations indicated no significant associations between pet ownership and symptoms of anxiety (r = −0.08, p = 0.17) or depressive symptoms (r = 0.02, p = 0.70; Table 2 above diagonal). In the linear regression analysis controlling for depressive symptoms (Table 3), pet ownership was not significantly associated with anxiety symptoms (b = −0.32, p = 0.09). Controlling for anxiety symptoms (Table 4), pet ownership was not significantly associated with depressive symptoms (b = 0.14, p = 0.30).
Table 1.
Descriptive statistics of covariate and outcome variables.
| MPO | MNPO | UNPO | ||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Category | M (SD) or % | M (SD) or % | M (SD) or % | p-value | |||
|
| ||||||||
| M1 & M2 | M1 | M2 | M1 | M2 | M1 | M2 | ||
|
|
||||||||
| Age | – | 78.05 (5.18) | 77.97 (5.40) | 78.67 (5.54) | 79.02 (5.67) | 78.38 (5.59) | 0.89 | 0.29 |
| Race | White | 59.8% | 60.4% | 58.0% | 34.2% | 36.4% | 0.91 | 0.74 |
| Sex | Female | 50.3% | 53.9% | 49.7% | 57.6% | 61.4% | 0.52 | 0.91 |
| Rurality | Rural | 60.4% | 59.8% | 61.0% | 33.7% | 32.6% | 0.91 | 0.91 |
| Income | Less than $20k | 51.5% | 50.9% | 46.7% | 64.1% | 67.9% | 0.32 | 0.30 |
| $20k–$49,999 | 33.7% | 36.1% | 40.8% | 29.9% | 25.6% | |||
| $50k or more | 14.8% | 13.0% | 12.4% | 6.0% | 6.5% | |||
| MS | Married | 54.4% | 51.5% | 53.3% | 39.1% | 37.5% | 0.99 | 0.99 |
| Widowed | 37.9% | 40.8% | 39.6% | 48.4% | 49.5% | |||
| Separated | 1.8% | 1.8% | 1.8% | 2.7% | 2.7% | |||
| Divorced | 3.6% | 3.6% | 3.6% | 6.0% | 6.0% | |||
| Never married | 2.4% | 2.4% | 1.8% | 3.8% | 4.4% | |||
| Health | – | 3.04 (0.65) | 2.97 (0.65) | – | 2.71 (0.78) | – | 0.93 | – |
| ADLs | – | 1.39 (3.05) | 0.75 (1.99) | – | 2.28 (3.48) | – | 0.35 | – |
| IADLs | – | 1.53 (3.12) | 1.44 (3.04) | – | 4.27 (4.84) | – | 0.78 | – |
| GDS-SF | – | 0.94 (1.41) | 0.88 (1.28) | 1.27 (1.78) | 1.59 (1.82) | 1.24 (1.47) | 0.69 | 0.06 |
| AIMS2 | – | 7.75 (1.88) | 8.04 (1.92) | 8.59 (2.67) | 8.61 (2.68) | 8.10 (2.02) | 0.17 | 0.001 |
Note: Total n = 522 with 169 pet owners matched (MPO) with 169 non-pet owners (MNPO) and 184 unmatched non-pet owners (UNPO) excluded from the analyses for each match. MS = marital status, Health = self-reported health, ADLs = activities of daily living, IADLs = instrumental activities of daily living, GDS-SF = Geriatric Depression Scale – Short Form, AIMS2 = Arthritis Impact Measurement Scales 2 Level of Tension, M1 = PSM 1 with health variables, M2 = PSM 2 without health variables. M1 and M2 matched pet-owners are the same participants in each group. P-value indicates difference between matched pet owners and non-pet owners on each variable.
Figure 1.
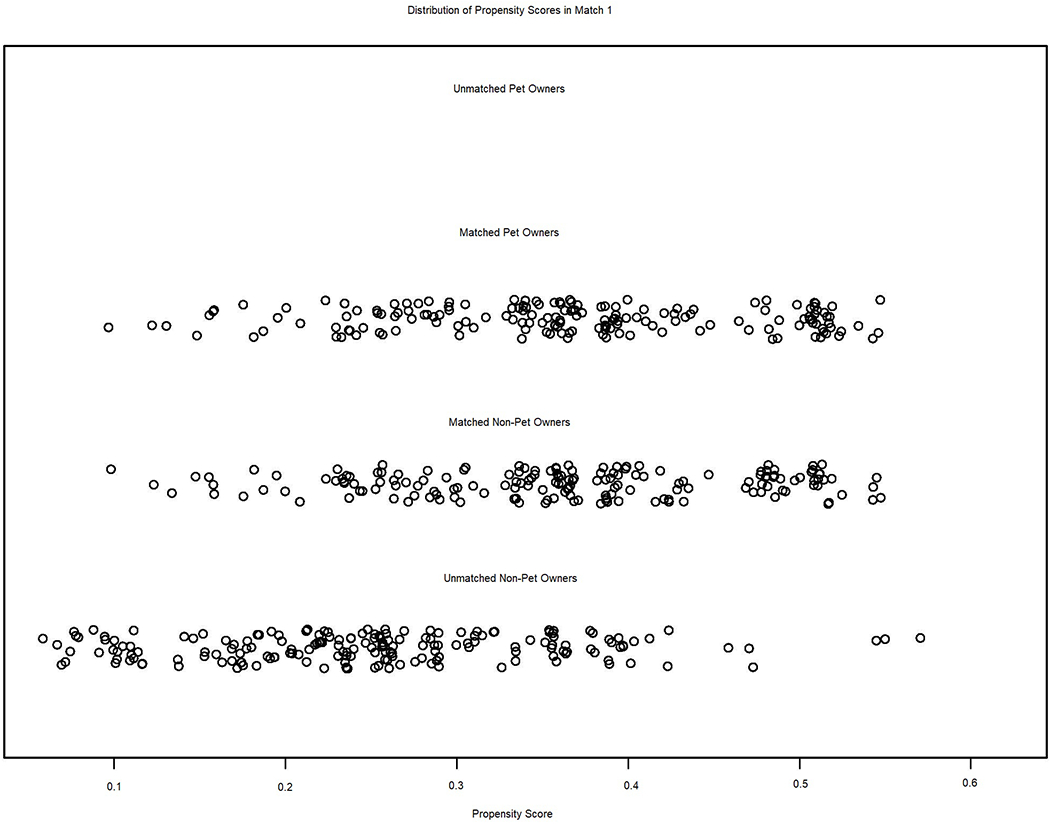
Illustrates propensity scores from Match 1 with Health Variables, including the concordance between matched pet owners’ (n = 169) and non-pet owners’ (n = 169) propensity scores as well as the propensity scores for non-pet owners who were excluded from analyses (n = 184) due to inadequate matching with a pet owner. All pet owners were matched with a non-pet owner who shared a similar propensity score.
Table 2.
Pearson correlations of variables for matched participants.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | – | 0.01 | 0.02 | −0.14* | 0.03 | −0.44** | −0.09 | 0.15** | 0.20*** | −0.04 | 0.19*** | 0.13* |
| 2. Age | 0.01 | – | 0.07 | −0.18** | 0.10 | −0.19** | −0.13* | 0.07 | 0.14** | 0.01 | −0.08 | 0.08 |
| 3. Race | 0.03 | 0.12* | – | −0.45*** | 0.10 | −0.19** | −0.02 | 0.03 | 0.01 | 0.01 | −0.14* | 0.05 |
| 4. Income | −0.12* | −0.19** | −0.47*** | – | −0.27*** | 0.45*** | 0.18** | −0.15** | −0.20*** | 0.01 | 0.00 | −0.23*** |
| 5. Rurality | 0.03 | 0.09 | 0.13* | −0.32*** | – | −0.04 | −0.15** | 0.08 | 0.07 | 0.01 | 0.06 | 0.11* |
| 6. Marital status | −0.42*** | −0.19*** | −0.24*** | 0.41*** | −0.05 | – | 0.11* | −0.17** | −0.23*** | 0.03 | −0.05 | −0.13* |
| 7. Health | −0.11* | −0.19*** | −0.01 | 0.20*** | −0.18** | 0.11 | – | −0.32*** | −0.33*** | −0.01 | −0.33*** | −0.37*** |
| 8. ADL | 0.15** | 0.12* | 0.07 | −0.19*** | 0.04 | −0.19*** | −0.35*** | − | 0.80*** | 0.05 | 0.24*** | 0.46*** |
| 9. IADL | 0.23*** | 0.20*** | 0.05 | −0.25*** | 0.05 | −0.24*** | −0.43*** | 0.77*** | – | 0.02 | 0.30*** | 0.47*** |
| 10. Pet owner | 0.01 | −0.06 | −0.02 | −0.01 | −0.01 | 0.01 | 0.07 | −0.11* | −0.17** | – | −0.08 | 0.02 |
| 11. AIMS2 | 0.25*** | −0.02 | −0.08 | −0.03 | −0.01 | −0.06 | −0.38*** | 0.29*** | 0.42*** | −0.18** | – | 0.41*** |
| 12. GDS-SF | 0.12* | 0.14** | 0.04 | −0.22*** | 0.09 | −0.11* | −0.39*** | 0.46*** | 0.52*** | −0.10 | 0.43*** | – |
Note: n = 388.
p < 0.05,
p < 0.01,
p < 0.001 two-tailed.
Match 1 with Health Variables is presented above the diagonal and Match 2 without Health Variables is presented below the diagonal. Marital Status was dichotomized such that 0 includes participants who selected widowed, separated, divorced, or never married and 1 = married, Health = self-reported health, ADLs = activities of daily living, IADLs = instrumental activities of daily living, AIMS2 = Arthritis Impact Measurement Scales 2 Level of Tension, GDS-SF = Geriatric Depression Scale – Short Form.
Table 3.
Summary of linear regression analyses for outcome of anxiety symptoms.
| Match 1 with Health Variables |
Match 2 without Health Variables |
|||||
|---|---|---|---|---|---|---|
| Variable | B | β | t | B | β | t |
| GDS-SF | 0.58 | 0.41 | 8.17*** | 0.60 | 0.41 | 8.38*** |
| Pet ownership | −0.32 | −0.08 | −1.68 | −0.65 | −0.14 | −2.81** |
| R2 | 0.17 | 0.20 | ||||
| F for R2 | 34.46*** | 41.86*** | ||||
Note: n = 338 with 169 pet owners matched with 169 non-pet owners in each match.
p < 0.05.
p < 0.01.
p < 0.001.
GDS-SF = Geriatric Depression Scale-Short Form.
Table 4.
Summary of linear regression analyses for outcome of depressive symptoms.
| Match 1 with Health Variables |
Match 2 without Health Variables |
|||||
|---|---|---|---|---|---|---|
| Variable | B | β | t | B | β | t |
| AIMS2 | 0.29 | 0.41 | 8.17*** | 0.29 | 0.42 | 8.38*** |
| Pet ownership | 0.14 | 0.05 | 1.05 | −0.08 | −0.03 | −0.51 |
| R2 | 0.16 | 0.18 | ||||
| F for R2 | 33.43*** | 37.21*** | ||||
Note: n = 338 with 169 pet owners matched with 169 non-pet owners in each match.
p < 0.05.
p < 0.01.
p < 0.001.
AIMS2 = Arthritis Impact Measurement Scales 2 Level of Tension.
Match 2 without Health Variables
In Match 2 without Health Variables, 169 pet owners were again matched with 169 non-pet owners for a final sample size of 338, excluding 184 non-pet owners from the regression analyses. PSM of Match 2 without Health Variables was also successful in that matched variables were not significantly different between groups (see Table 1), and the distribution of propensity scores is depicted in Figure 2. Of this matched sample, 49.1% endorsed earning $16,000 to $19,999 or less annually and participants were predominately married (53.8%) or widowed (38.8%). Compared with excluded participants, included participants were more likely to be male (50.0% vs 38.6%), rural residents (60.7% vs 32.6%), and White (58.9% vs 36.4%). Point biserial correlations demonstrated that in this dataset, pet ownership was significantly associated with anxiety symptoms at a small effect size (r = −0.18, p = 0.001) but not depressive symptoms (r = −0.10, p = 0.06; Table 2 below diagonal). In the linear regression analysis controlling for depressive symptoms (Table 3), pet ownership was significantly associated with fewer symptoms of anxiety (b = −0.65, p = 0.01, partial r = −0.15), though this was a small effect. Controlling for anxiety symptoms (Table 4), pet ownership was not significantly associated with depressive symptoms (b = −0.08, p = 0.61).
Figure 2.
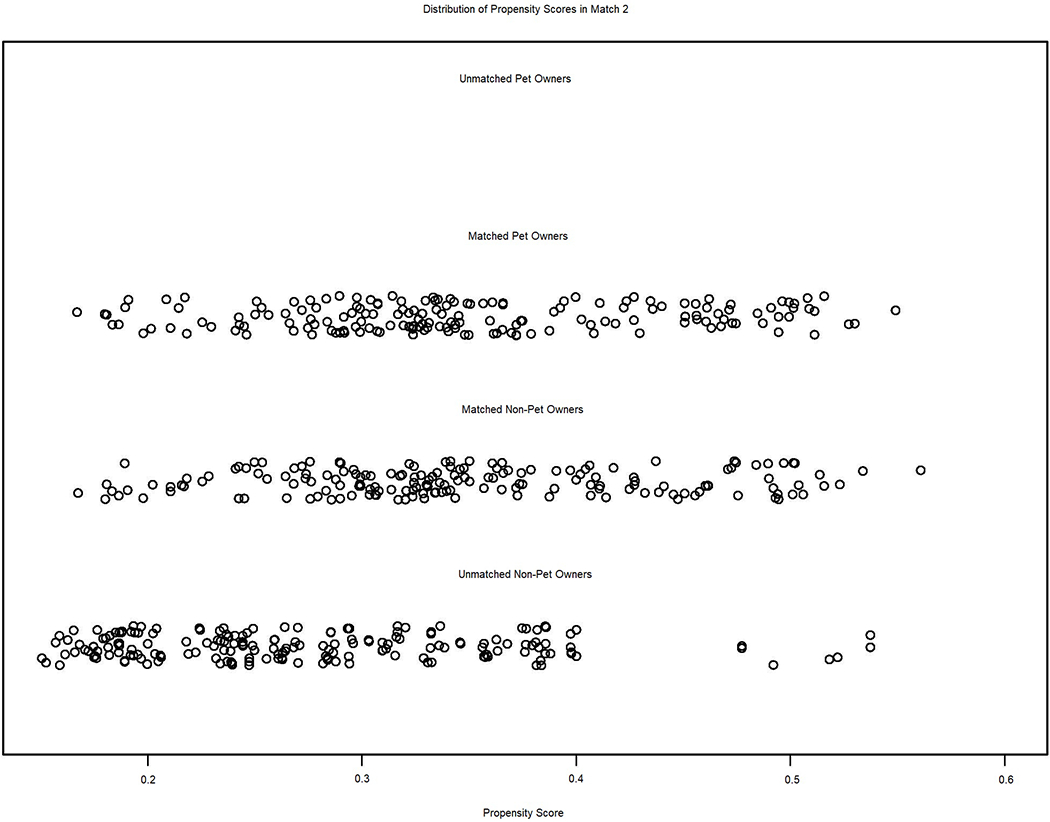
Illustrates propensity scores from Match 2 without Health Variables, including the concordance between matched pet owners’ (n = 169) and non-pet owners’ (n = 169) propensity scores as well as the propensity scores for non-pet owners who were excluded from analyses (n = 184) due to inadequate matching with a pet owner. All pet owners were matched with a non-pet owner who shared a similar propensity score.
Discussion
Overall, we found that pet ownership was significantly related to anxiety symptoms after controlling for several demographic characteristics that may relate to pet ownership status and the overlap between anxiety and depressive symptoms, although this effect was small. However, controlling for health variables attenuated this association. The same result was not found for depressive symptoms, however, as pet ownership was not significantly related to depressive symptoms after controlling for covariates and anxiety symptoms in either matched sample.
These results suggest that owning a pet in later life may be related to fewer symptoms of anxiety but not depression. This finding adds to the sparse literature on late-life pet ownership and anxiety (Bennett et al., 2015; Feng et al., 2014; Likourezos et al., 2002; Parslow et al., 2005) and prompts the need for further research to be conducted to examine the anxiety-relieving aspects of owning a pet in older adulthood. Further, the significant relation between owning a pet and fewer symptoms of anxiety was blunted after matching pet owners and non-pet owners on health variables (i.e., self-reported health and difficulty with ADLs and IADLs). This suggests that one’s health status may play an important role in owning a pet or that owning a pet may improve one’s health. Therefore, this relation is important to consider when examining mental health outcomes in older adulthood. However, post-hoc analyses indicate that the reverse is not true and that controlling for pet ownership does not significantly affect the association between health and anxiety symptoms (analyses not shown).
Our results do not support owning a pet in late life is associated with fewer depressive symptoms. This is in opposition to findings that companionship provided by pets, and owning a pet in general, may reduce feelings of loneliness (McConnell et al., 2011; Stanley et al., 2014). The lack of a significant relation between pet ownership and depressive symptoms may be due in part to pets being beneficial for some older adults and not others, although examination of this was beyond the scope of the present study. Unpleasant aspects of pet ownership that may negatively impact depressive symptoms in older adults include feelings of frustration, anger, guilt, grief, rejection, financial burden, and interference with social relationships (Chandler et al., 2015). On the other hand, the lack of a significant relation between pet ownership and depressive symptoms may also be explained by the low prevalence of depressive symptoms in our sample or a lack of power to detect a small effect. Regardless of statistical significance, the difference in depressive symptoms in the current sample was also not clinically significant (i.e., the mean GDS-SF score for pet owners was less than half a point different than the mean GDS-SF score for non-pet owners).
These findings are limited by the use of a non-clinical, healthy sample. On one hand, this allows generalization of our findings to the general older adult population, but on the other hand, we cannot generalize our findings to older adults with higher illness burden. However, given the size and how well-characterized the sample is, our findings still significantly add to the literature in this area. Further, participants reported very low average levels of anxiety and depressive symptoms, with means being approximately one standard deviation from the lowest possible scores. This homogeneity likely reduced the ability of the analyses to determine significant relations to pet ownership, thus introducing a conservative bias. Because of this, the fact that significant differences in symptoms of anxiety were found is that much more notable. Additionally, the data included in the present analyses were collected in 2004 to 2006, and changes in older adult pet ownership may have occurred in the time since these data were collected. Further, the assessment measures used in this study have shortcomings as the AIMS2 Level of Tension scale used to measure participants’ symptoms of anxiety has yet to be validated for clinical purposes, and this study only assessed participants’ current pet ownership status. Consideration of the type of pet owned may enhance the present findings as older adult dog owners may be more physically active than owners of cats or other pet species (Thorpe et al., 2006). Despite these methodological limitations, the present study is the strongest utilized to date to test the relation between pet ownership and anxiety symptoms in older Americans as previous studies have been conducted outside of the United States (Bennett et al., 2015; Feng et al., 2014; Parslow et al., 2005) or have used a case study design (Likourezos et al., 2002). These studies, with the exception of the case study, did not find a significant relation between late-life pet ownership and anxiety symptoms. Therefore, the current study is a notable advance to the field. Examination of the relationship between pet ownership, anxiety symptoms, and symptoms of depression in late life using a contemporary clinical sample, validated anxiety measures, and additional variables related to pet ownership (e.g., type of pet, length of ownership, recent losses of pets, history of pet ownership, and specific responsibilities associated with ownership) is warranted to further this area of research. Also, it would be beneficial to probe the relationship between late-life pet ownership, symptoms of anxiety, and depressive symptoms by testing various moderators. This would help uncover circumstances in which owning a pet is detrimental or beneficial to older adults. Additionally, further research on the specific mechanisms or qualities of pet ownership that are related to mental health is needed to identify what functions pet ownership serves that benefit mental health, and anxiety symptoms in particular. Exploration of the causal pathways between physical health, mental health, and pet ownership would also greatly advance this area of research.
In summary, the present study found that pet ownership in late life was significantly related to symptoms of anxiety, but not depressive symptoms, independent of several covariates. This relation was reduced when health variables were considered when matching older adult pet owners and non-pet owners. The results of the current study highlight the importance of general and functional health for the association between pet ownership and mental health symptoms in late life as models controlling for general and functional health indicated non-significant associations between pet ownership and both depression and anxiety symptoms. However, models not matching on general and functional health indicated significant associations between pet ownership and anxiety symptoms, but the cross-sectional nature of the current investigation precludes determining how pet ownership and health relate to each other. These results contribute to a growing literature on the potential benefits of pet ownership for older adults’ psychological health, and symptoms of anxiety in particular.
Acknowledgements
We thank Carolyn E. Adams-Price, PhD for introducing the first author to the University of Alabama at Birmingham’s Study of Aging, as well as her comments on portions of this work presented in poster form.
Funding
The University of Alabama at Birmingham Study of Aging was funded in part by National Institute on Aging grants R01-AG015062, P30AG031054, and 5UL1 RR025777. The content is solely the responsibility of the authors and does not necessarily reflect the policy of the National Institute on Aging or the National Institutes of Health.
Footnotes
Disclosure Statement
No potential conflict of interest was reported by the authors.
References
- Allman RM, Sawyer P, & Roseman JM (2006). The UAB Study of Aging: Background and insights into life-space mobility among older Americans in rural and urban settings. Aging Health, 2(3), 417–429. 10.2217/1745509X.2.3.417 [DOI] [Google Scholar]
- American Pet Products Association. (2019). APPA releases findings from new 2019-2020 national pet owners survey. https://www.americanpetproducts.org/press_releasedetail.asp?id=192
- Bennett PC, Trigg JL, Godber T, & Brown C (2015). An experience sampling approach to investigating associations between pet presence and indicators of psychological wellbeing and mood in older Australians. Anthrozoös, 28(3), 403–420. 10.1080/08927936.2015.1052266 [DOI] [Google Scholar]
- Bergen-Cico D, Smith Y, Wolford K, Gooley C, Hannon K, Woodruff R, Spicer M, & Gump B (2018). Dog ownership and training reduces post-traumatic stress symptoms and increases self-compassion among veterans: Results of a longitudinal control study. The Journal of Alternative and Complementary Medicine, 24(12), 1166–1175. 10.1089/acm.2018.0179 [DOI] [PubMed] [Google Scholar]
- Brook RH, Ware JE, & Davies-Avery A (1979). Overview of adult health status measures fielded in Rand’s health insurance study. Medical Care, 17(Suppl. 7). [PubMed] [Google Scholar]
- Carr DC, Taylor MG, Gee NR, & Sachs-Ericsson N (2019). Psychological health benefits of companion animals following a social loss. The Gerontologist, 60(3), 1–11. 10.1093/geront/gnz109 [DOI] [PubMed] [Google Scholar]
- Chandler CK, Fernando DM, Barrio Minton CA, & Portrie-Bethke TL (2015). Eight domains of pet-owner wellness: Valuing the owner-pet relationship in the counseling process. Journal of Mental Health Counseling, 37(3), 268–282. 10.17744/mehc.37.3.06 [DOI] [Google Scholar]
- Crossman MK, & Kazdin AE (2016). Additional evidence is needed to recommend acquiring a dog to families of children with Autism Spectrum Disorder: A response to Wright and colleagues. Journal of Autism and Developmental Disorders, 46(1), 332–335. 10.1007/s10803-015-2542-2 [DOI] [PubMed] [Google Scholar]
- Enmarker I, Hellzén O, Ekker K, & Berg AGT (2015). Depression in older cat and dog owners: The Nord-Trøndelag Health Study (HUNT)-3. Aging and Mental Health, 19(4), 347–352. 10.1080/13607863.2014.933310 [DOI] [PubMed] [Google Scholar]
- Feng Z, Dibben C, Witham MD, Donnan PT, Vadiveloo T, Sniehotta F, Crombie IK, & McMurdo MET (2014). Dog ownership and physical activity in later life: A cross-sectional observational study. Preventive Medicine, 66, 101–106. 10.1016/j.ypmed.2014.06.004 [DOI] [PubMed] [Google Scholar]
- Friedmann E, Gee NR, Simonsick E, & Simonsick S (2018). Pet ownership patterns in community-living older adults. Innovation in Aging, 2(S1), 974. [Google Scholar]
- Gee NR, & Mueller MK (2019). A systematic review of research on pet ownership and animal interactions among older adults. Anthrozoös, 32(2), 183–207. 10.1080/08927936.2019.1569903 [DOI] [Google Scholar]
- González Ramírez MT, & Landero Hernández R (2014). Benefits of dog ownership: Comparative study of equivalent samples. Journal of Veterinary Behavior, 9(6), 311–315. 10.1016/j.jveb.2014.08.002 [DOI] [Google Scholar]
- Gretebeck KA, Radius K, Black DR, Gretebeck RJ, Ziemba R, & Glickman LT (2013). Dog ownership, functional ability, and walking in community-dwelling older adults. Journal of Physical Activity and Health, 10(5), 646–655. 10.1123/jpah.10.5.646 [DOI] [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, & Stuart EA (2011). MatchIt: Nonparametric preprocessing for parametric causal inference. Journal of Statistical Software, 42(8), 1–28. http://www.jstatsoft.org/v42/i08/ [Google Scholar]
- Likourezos A, Burack OR, & Lantz MS (2002). The therapeutic use of companion animals. Clinical Geriatrics, 10(4), 31–33. [Google Scholar]
- McConnell AR, Brown CM, Shoda TM, Stayton LE, & Martin CE (2011). Friends with benefits: On the positive consequences of pet ownership. Journal of Personality and Social Psychology, 101(6), 1239–1252. 10.1037/a0024506 [DOI] [PubMed] [Google Scholar]
- Meenan RF, Gertman PM, & Mason JH (1980). Measuring health status in arthritis: The Arthritis Impact Measurement Scales. Arthritis & Rheumatism, 23(2), 146–152. [DOI] [PubMed] [Google Scholar]
- Meenan RF, Mason JH, Anderson JJ, Guccione AA, & Kazis LE (1992). AIMS2: The content and properties of a revised and expanded arthritis impact measurement scales health status questionnaire. Arthritis & Rheumatism, 35(1), 1–10. [DOI] [PubMed] [Google Scholar]
- Miltiades H, & Shearer J (2011). Attachment to pet dogs and depression in rural older adults. Anthrozoös, 24(2), 147–154. 10.2752/175303711X12998632257585 [DOI] [Google Scholar]
- Mueller MK, Gee NR, & Bures RM (2018). Human–animal interaction as a social determinant of health: Descriptive findings from the health and retirement study. BMC Public Health, 18(305), 1–7. 10.1186/s12889-018-5188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netting EF, Wilson CC, & Fruge C (1988). Pet ownership and nonownership among elderly in Arizona. Anthrozoös, 2(2), 125–132. 10.2752/089279389787058154 [DOI] [Google Scholar]
- O’Haire ME, & Rodriguez KE (2018). Preliminary efficacy of service dogs as a complementary treatment for posttraumatic stress disorder in military members and veterans. Journal of Consulting and Clinical Psychology, 86(2), 179–188. 10.1037/ccp0000267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker GB, Gayed A, Owen CA, Hyett MP, Hilton TM, & Heruc GA (2010). Survival following an acute coronary syndrome: A pet theory put to the test. Acta Psychiatrica Scandinavica, 121(1), 65–70. 10.1111/j.1600-0447.2009.01410.x [DOI] [PubMed] [Google Scholar]
- Parslow RA, Rodgers B, Jorm AF, Jacomb P, & Christensen H (2005). Pet ownership and health in older adults: Findings from a survey of 2,551 community-based Australians aged 60–64. Gerontology, 51(1), 40–47. 10.1159/000081433 [DOI] [PubMed] [Google Scholar]
- Peacock M, Netto J, Yeung P, McVeigh J, & Hill A-M (2019). Understanding the relationship between pet ownership and physical activity among older community-dwelling adults—A mixed methods study. Journal of Aging and Physical Activity, 28(1), 131–139. 10.1123/japa.2019-0056 [DOI] [PubMed] [Google Scholar]
- Peel C, Sawyer Baker P, Roth DL, Brown CJ, Brodner EV, & Allman RM (2005). Assessing mobility in older adults: The UAB Study of Aging Life-Space Assessment. Physical Therapy, 85(10), 1008–1119. 10.1093/ptj/85.10.1008 [DOI] [PubMed] [Google Scholar]
- Raina P, Waltner-Toews D, Bonnett B, Woodward C, & Abernathy T (1999). Influence of companion animals on the physical and psychological health of older people: An analysis of a one-year longitudinal study. Journal of the American Geriatrics Society, 47(3), 323–329. 10.1111/j.1532-5415.1999.tb02996.x [DOI] [PubMed] [Google Scholar]
- Research and Markets. (2017). Pet population and ownership trends in the U.S.: Dogs, cats, and other pets, 2nd ed. Retrieved November 14, 2019, from https://www.researchandmarkets.com/research/f9ws72/pet_population.
- Saunders J, Parast L, Babey SH, & Miles JV (2017). Exploring the differences between pet and non-pet owners: Implications for human–animal interaction research and policy. PLoS ONE, 12(6), 1–15. 10.1371/journal.pone.0179494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpley C, Veronese N, Smith L, López-Sánchez GF, Bitsika V, Demurtas J, Celotto S, Noventa V, Soysal P, Isik AT, Grabovac I, & Jackson SE (2020). Pet ownership and symptoms of depression: A prospective study of older adults. Journal of Affective Disorders, 264(November), 35–39. 10.1016/j.jad.2019.11.134 [DOI] [PubMed] [Google Scholar]
- Sheikh JI, & Yesavage JA (1986). Geriatric Depression Scale (GDS) recent evidence and development of a shorter version. Clinical Gerontologist, 5(1–2), 165–173. [Google Scholar]
- Stanley IH, Conwell Y, Bowen C, & Van Orden KA (2014). Pet ownership may attenuate loneliness among older adult primary care patients who live alone. Aging & Mental Health, 18(3), 394–399. 10.1080/13607863.2013.837147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugawara A, Masud MM, Yokoyama A, Mizutani W, Watanuki S, Yanai K, Itoh M, & Tashiro M (2012). Effects of presence of a familiar pet dog on regional cerebral activity in healthy volunteers: A positron emission tomography study. Anthrozoös, 25(1), 25–34. 10.2752/175303712X13240472427311 [DOI] [Google Scholar]
- Taniguchi Y, Seino S, Nishi M, Tomine Y, Tanaka I, Yokoyama Y, Amano H, Kitamura A, & Shinkkai S (2018). Physical, social, and psychological characteristics of community-dwelling elderly Japanese dog and cat owners. PLoS ONE, 13(11), 1–11. 10.1371/journal.pone.0206399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe RJ, Kreisle RA, Glickman LT, Simonsick EM, Newman AB, & Kritchevsky S (2006). Physical activity and pet ownership in year 3 of the Health ABC study. Journal of Aging and Physical Activity, 14(2), 154–168. 10.1123/japa.14.2.154 [DOI] [PubMed] [Google Scholar]
- Winefield HR, Black A, & Chur-Hansen A (2008). Health effects of ownership of and attachment to companion animals in an older population. International Journal of Behavioral Medicine, 15(4), 303–310. 10.1080/10705500802365532 [DOI] [PubMed] [Google Scholar]
- Yarborough BJH, Owen-Smith AA, Stumbo SP, Yarborough MT, Perrin NA, & Green CA (2017). An observational study of service dogs for veterans with posttraumatic stress disorder. Psychiatric Services, 68(7), 730–734. 10.1176/appi.ps.201500383 [DOI] [PubMed] [Google Scholar]


