Key Features
The Better Outcomes Registry & Network (BORN) Ontario was developed to collect pregnancy, birth and newborn information and outcomes data to facilitate and improve perinatal care in Ontario, Canada. With near-complete capture of all births in Ontario, it has evolved to be an invaluable resource for performance measurement, quality improvement, surveillance and research.
The BORN Information System was launched in 2012 as the amalgamation of data systems from provincial programmes servicing the maternal–newborn population. BORN Ontario also maintains the legacy data sets of its predecessors (2006–2012) and other data holdings have since been added.
Data are submitted regularly by >250 hospitals, fertility clinics, birth centres, midwifery practice groups, primary care organizations, and prenatal- and newborn-screening laboratory and treatment centres. Over 1.3 million maternal–infant records have been captured to date.
Data include maternal demographics, health behaviours, in vitro fertilization assistance, prenatal screening, pregnancy interventions and complications, intrapartum events, peripartum outcomes, intensive-care and newborn-screening information. Record-level data can be linked to a wide range of provincial administrative and clinical data sets to track individuals from conception to birth and across the lifespan.
Aggregate and record-level data are available upon request via the Data Access Request Team. BORN Ontario data dictionaries are openly available to browse online.
Data resource basics
The Better Outcomes Registry & Network (BORN) Ontario collects pregnancy, birth and newborn information and outcomes data for nearly all births in Ontario, Canada. With nearly complete capture of the approximate 140 000 births each year in Ontario—∼40% of births in Canada—BORN Ontario is the largest perinatal registry in the country.1 The origins of BORN Ontario date to the 1980s as a system for tracking regional variation in pregnancy and childbirth outcomes across Eastern Ontario. BORN Ontario was originally named the Niday Perinatal Database in honour of its founder, Dr Patricia Niday, who, as director of one of Ontario’s regional perinatal programmes, advocated tirelessly for its provincial adoption. The regional programme gradually expanded data capture and launched the Ontario Perinatal Surveillance System (OPSS). By 2006, most of the province was contributing data to the OPSS for analysis and reporting.2
In 2009, with funding from the Ontario Ministry of Health and Long-Term Care, OPSS was designated a prescribed registry under the province’s Personal Health Information Protection Act, and rebranded as BORN Ontario. Prescribed registry status granted BORN Ontario the authorization to collect, use and disclose personal health information without consent to facilitate and improve healthcare. The new organization amalgamated the data systems of four programmes servicing the maternal–newborn population: the Prenatal Screening Program, the Fetal Alert Network (high-risk antenatal healthcare for pregnancies complicated by congenital anomalies), the Ontario Midwifery Program and the Niday Perinatal Database. These programmes worked together to normalize their data and build a robust, web-based data-collection and reporting system. In April 2012, the BORN Information System was launched to collect, manage, protect and share critical data about every pregnancy, birth and child in Ontario. Newborn screening test results from Newborn Screening Ontario were also included at launch, representing the first time such information was linked to perinatal data sets in Ontario. A reporting portal for data contributors went live in 2013.
BORN Ontario has evolved to be a secure data platform with multiple data holdings that can be linked to connect individual health records from conception to birth and into early childhood. The Canadian Assisted Reproductive Technologies Registry (CARTR), which collects data on in vitro fertilization (IVF) cycles and birth-outcomes data for fertility clinics across Canada, was added in January 2013 and rebranded CARTR Plus. Other data holdings have since been added, including primary care data on young children and results of standardized screening and assessments of child development through the provincial Healthy Babies Healthy Children programme. BORN Ontario also maintains legacy data sets from the founding five partner programmes (last data entry 31 March 2012) and CARTR (January 2001—December 2012).
The present-day BORN Information System collects data from >250 hospitals, fertility clinics, birth centres, midwifery practice groups, primary-care organizations, and prenatal- and newborn-screening laboratory and treatment centres spanning all levels of care from pre-pregnancy to early childhood. To date, >1.3 million maternal–infant records have been captured. The following sections will focus on the BORN Information System with reference to the Niday Perinatal Database for historical context.
Data collected
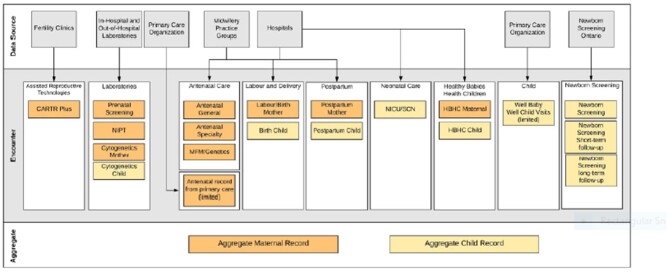
BORN data are collected on a voluntary basis from health-information custodians involved in the care of children, newborns and their mothers. Data are submitted through several mechanisms including manual data entry into a reporting portal by staff in birthing units and midwifery practice groups, Health Level Seven (HL7) data feeds, and automated extraction and uploads from electronic health record systems, where available. Data are submitted in close to real time, or uploaded in batches, and include maternal demographics, health behaviours, any IVF assistance, prenatal screening, pregnancy interventions and complications, intrapartum events, peripartum outcomes, neonatal intensive care unit (NICU) care and newborn-screening data, each of which is classified by the nature of the clinical encounter with the healthcare system (Figure 1). Linkage of data elements and encounters across data sources is facilitated by a robust linking and matching algorithm utilizing unique individual (mother and child), pregnancy and birth identifiers that are assigned upon the first record entry into the BORN Information System. Some data elements are common across encounters, permitting the pre-population of some data fields to reduce duplication of data-entry efforts. This model enables both programme-specific analyses by encounter and analysis of aggregated data by population and health system. A description of the data available in BORN is provided in Table 1.
Figure 1.
Better Outcomes Registry & Network (BORN) Ontario data sources and architecture. BORN Ontario data are submitted on a voluntary basis by health-information custodians from across Ontario servicing the maternal–child population. Data are classified by the nature of the healthcare encounter and are linked to create aggregate records for each woman and child. CARTR, Canadian Assisted Reproductive Technologies Registry; MFM, maternal fetal medicine; NICU, neonatal intensive care unit; NIPT, non-invasive prenatal testing; SCN, special care nursery; HBHC, Healthy Babies Healthy Children.
Table 1.
Summary of data collected by the Better Outcomes Registry & Network (BORN) information system
| Encounter type or data holding | Description |
|---|---|
| Assisted reproductive technology (ART)3,4 |
Collects information on in vitro fertilization treatment cycles from fertility clinics across Canada collected into the Canadian Assisted Reproductive Technology Register (CARTR Plus) Also includes record-level details on any ART treatment cycles from Ontario fertility clinics that result in a pregnancy that is delivered at >20 weeks’ gestation that are automatically linked with other records within the BORN Information System |
| Antenatal general | Captures information relevant to the antenatal period (i.e. obstetrical history, exposures, complications, etc.) |
| Antenatal specialty | Captures maternal, pregnancy and fetal information for women who require specialized care management at a high-risk maternal fetal medicine or prenatal genetic clinic |
| Prenatal screening and follow-up5,6 |
Prenatal screening records for every pregnant individual who receives any form of prenatal screening in Ontario Includes information from laboratory and ultrasound testing, clinical assessment, genetic counselling and diagnostic testing from prenatal screening, as well as screening and diagnostic results |
| Non-invasive prenatal testing7 | Information captured during non-invasive prenatal testing for fetal genetic disorders |
| Cytogenetics | Information related to the clinical indications and results of maternal and child cytogenetic testing |
| Labour and birth |
Captures information relevant to the pregnant person’s spontaneous or induced labour and birth experience through to the first hour postpartum whether this occurs in hospital, at home or in a birth centre Midwifery–client specific data are also captured in the midwifery encounter |
| Birth–child | Documents a child's birth experience through to the first hour postpartum |
| Postpartum mother | Documents the course of care experienced by the mother from 1 hour post birth to discharge from hospital |
| Postpartum child | Documents the course of care experienced by the child from 1 hour post birth to discharge from hospital |
| Newborn screening and diagnostic evaluations |
Screening tests and results from the provincial newborn-screening laboratory (including hearing and congenital heart disease) Information on short-term follow-up, clinical status, diagnostic information and treatment plans for infants who received a positive newborn screen are also available |
| Neonatal intensive care/special care units | Information collected during infant stays in neonatal intensive care units and special care nurseries |
| Midwifery practice group data | Data on prenatal and birth care (home, hospital and birth-centre births) provided by midwives in Ontario |
| Well Baby Well Child visit information |
Information obtained through regular assessments of a baby or child’s development Includes age, height, weight, vaccinations and documentation of developmental milestones using the standardized measures (Rourke Baby Record Ontario, Nipissing District Developmental Screen) |
| Healthy Babies Healthy Children (HBHC) programme |
Information collected from completion of the standardized HBHC Screening Tool, which facilitates identification of risk factors that may affect a child’s healthy development and referral to community programmes and services Screening is voluntary and consent-based BORN facilitates the transfer of this information from hospitals/homes to public-health units who provide the follow-up |
Citations are provided where data elements have been previously validated or described in detail.
Data quality
BORN Ontario data are used to support clinical programme management, benchmarking, evaluation and quality improvement across the province of Ontario. The data may also to be used for research. As such, BORN Ontario upholds a comprehensive framework to promote quality in all aspects of data collection, analysis, use and disclosure of information.8 Five essential dimensions of data quality are upheld (Figure 2).
Figure 2.
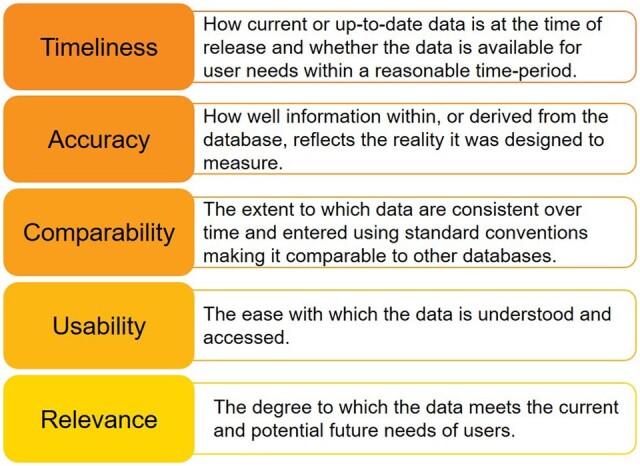
Better Outcomes Registry & Network (BORN) Ontario data-quality framework. The data-quality framework is based on five dimensions to ensure that user decision-making is based on current, valid, reliable and relevant data.
Audits of the Niday Perinatal Database and BORN Information System have demonstrated good agreement with patient charts and clinical administrative hospital databases.9–12 An external audit by Public Health Ontario concluded that the quality of BORN data exceeded that of other sources of reproductive-health information.12 A re-abstraction study of 29 variables from records submitted in 2014–2015 found >90% agreement between BORN records and patient charts for over three-quarters of the audited variables.11 The remaining variables demonstrated fair to moderate agreement. These findings have informed ongoing improvements to BORN data dictionaries, data-entry guidelines and quality-control processes.
The BORN Information System applies a series of validation rules to ensure data quality. Logic rules assess the compliance of data elements collected within a given healthcare encounter. Conformance rules ensure that mandatory elements are completed. Parameter rules compare entered values against reference tables to ensure that they are within acceptable ranges before they are submitted. The system also applies aggregation rules to determine how data elements across multiple encounters (e.g. prenatal screening, general antenatal visits and delivery) are consolidated into a single birth record. Where there is discordance in data elements that are recorded in more than one encounter, aggregation rules provide guidance on which values take precedence. Thus, having some data elements captured multiple times across the pregnancy and birth continuum also helps to increase data accuracy and completeness.
Support mechanisms are in place for submitting organizations to identify and resolve errors in their data entries. The data-validation rules described above facilitate the generation of reports and flags for records identified with missing encounters, possible errors or different data entered for the same element in separate encounters so that errors can be reconciled. All data must be formally acknowledged by the submitting organization and, each month, submitters review their records to ensure that there are no outstanding errors. As a final checkpoint in this process, BORN data analysts conduct additional data checks at the end of each fiscal year.
Finally, online help tips and data-element definitions are available within the data-entry system and regional coordinators are available to answer questions related to data entry, reconciliation and acknowledgement processes, and the implementation of system enhancements. Regional coordinators are distributed throughout the province and work directly and regularly with the data submitters and the regional perinatal networks using the data to improve care. A 24-hour Helpdesk is also available.
Data privacy and security
BORN Ontario is a prescribed registry established under the Ontario Personal Health Information Protection Act, 2004 A.13 As such, personal health information within the BORN network is protected by administrative, physical and technological controls that adhere to industry best practices for privacy and security. BORN Ontario has implemented a rigorous programme to protect personal health information in its custody from theft, loss, unauthorized access, copying, modification, use, disclosure and disposal. Regular audits and investigations are conducted to monitor and manage privacy compliance. BORN Ontario’s information practices and privacy policies are assessed by the Information and Privacy Commissioner of Ontario every 3 years.
Governance and funding
The Children’s Hospital of Eastern Ontario (CHEO) provides the formal governance structure and support for BORN Ontario operations. The BORN Ontario Executive Team works in cooperation with leadership at CHEO to provide medical, scientific and administrative oversight of day-to-day operations. Core funding is provided by the Ontario Ministry of Health and Long-Term Care.
Data resource use
Contributing hospitals, laboratories, clinics and birth centres have access to their own data within the BORN Information System. These data are used locally for practice audits and to support quality-improvement initiatives. In addition, various organizations and external partners may use BORN Ontario data for planning and management of the healthcare-delivery system at organizational, provincial or other regional levels. These efforts have resulted in numerous successful initiatives to enhance the quality of maternal–newborn care delivery in Ontario through data-quality assessments,9–11 the introduction of new health services and programmes14–17 and technology-based interventions.18–22 The BORN Ontario registry is also an invaluable research resource for addressing maternal and child health issues. BORN data have been used extensively to address research topics including the developmental origins of health and disease, complications of pregnancy and childbirth, and evaluating short- and long-term maternal and child health outcomes.
BORN dashboards
BORN has developed two electronic audit and feedback systems that provide hospitals offering maternal, newborn and NICU care with site-specific feedback on a near real-time basis to facilitate practice change on key performance indicators.18–21 The BORN Maternal Newborn Dashboard was launched in 2012 with six key performance indicators and has since become an instrumental tool for decreasing variation in clinical practice and improving patient outcomes across the province. Evaluation of the Maternal Newborn Dashboard 2.5 years after its implementation demonstrated corresponding improvements across several key performance indicators. These include: rates of episiotomy, post-date induction at <41 weeks, repeat caesarean section in low-risk women before 39 weeks and appropriately timed group B streptococcus screening.18 A NICU Dashboard was also launched in 2018 with two key performance indicators to support clinical-practice improvement for neonatal care. Each dashboard displays a hospital’s performance on each key performance indicator relative to provincial benchmarks, provincial-level rates as well as peer-performance data from hospitals providing similar levels of maternal or neonatal care and/or of similar birth volume. Engagement with local health professionals and organizations is ongoing and helps to ensure uptake of these dashboards and meaningful practice change.19,20
Perinatal research
Since its inception, BORN data have been used in Canada and internationally to produce nearly 100 high-impact publications with broad medical and scientific reach. These publications cover a diverse array of topics including, but not limited to, prenatal screening and diagnostic testing7,23; breastfeeding and influencing factors24,25; use and outcomes of assisted reproduction26–30; trends in obstetrical interventions and factors influencing use31–33; and factors influencing maternal and neonatal health outcomes such as environmental exposures,34–36 influenza immunization during pregnancy,37–39 substance use,40,41 hypertension,42,43 diabetes44–47 and obesity/gestational weight gain.48–50 A compendium of published research using BORN data is available online (https://bit.ly/2UXEX3I).
Data linkage: long-term follow-up of women and infants
BORN data can be linked with other provincial data resources to facilitate long-term follow-up of women and their children. ICES (www.ices.ca) is a provincial data repository containing longitudinal, coded and linkable clinical and administrative records encompassing nearly all interactions that Ontarians have with the publicly funded healthcare system. Population-based health surveys, research-specific and registry data are also integrated, permitting evaluation of health policy and care delivery as a whole across the province. In 2014, the Niday historical data set (2006/07–2011/12) was transferred to ICES. A 2-year transfer of BORN Information System data spanning 2012/13–2013/14 fiscal years was completed in early 2015; a second data transfer (2014/15–2018/19) took place in 2020. The new data are scheduled for release in 2021. Deterministic and probabilistic linkage of individual maternal and newborn records to master registration files at ICES facilitates linkage of BORN data to all other data sets held by ICES. Thus, linkage of these two repositories provides a unique opportunity to study population-level maternal and infant health outcomes ranging from the fertility treatment and perinatal period to many years after birth. Recent applications of ICES-BORN data include examining the effect of frequent blood donations before pregnancy on maternal and newborn outcomes51; evaluating the association between cannabis exposure in pregnancy and neurodevelopmental outcomes in children52; assessing the 5-year health outcomes of children born to mothers who received the 2009 pandemic H1N1 influenza vaccination during pregnancy38; exploring the link between prenatal and early-life exposures to ambient air pollutants and the development childhood asthma53; the association between intrapartum epidurals and postpartum depression54; and risk of breast cancer following thoracic computed tomography in the perinatal period.55 The potential applications of these linked data include interrupted time-series analyses and using BORN to collect data for clinical trials and other interventions. Given that BORN Ontario is a relatively new entity, the potential use of these linked data will only continue to grow, particularly as other provincial data holdings become available.
Strengths and weaknesses
Ontario, Canada has rich network of health-data repositories that can be used to provide comprehensive insight into population health and healthcare delivery. The BORN Ontario registry is a component of the network, providing the capacity to link pregnancy and newborn health records across multiple health systems and track individuals from conception and birth across their lifespans. The breadth of data held by the BORN Ontario registry makes it a foundational resource for answering perinatal health-related questions. Strengths include: capture of all hospital births in Ontario (>99% of all births in the province) and all midwifery-attended home and birth-centre births; capture of extensive information about maternal and newborn characteristics, health histories and behaviours, outcomes and health-services utilization; integration of multiple data holdings spanning the continuum of maternal–child healthcare delivery; and a nearly 10-year data-collection time frame. Notably, BORN data have been validated and demonstrate consistency with other clinical administrative data sets.
The BORN Ontario birth registry is not without limitations. BORN elements are subject to incomplete or duplicate data entries, misclassification and under-reporting. The BORN Registry is reliant on data sourced from medical records, clinical forms and patient interviews, and, if data are not collected or entered into a patient’s records, they will not be available for abstraction into the BORN Information System. In addition, where manual entry may be performed by clerk staff or nurses, variability in the interpretation of case definitions can affect data quality, and incomplete or duplicate data entry and misclassification are a reality. Data entry errors and duplicate data entries are cleaned when identified. Collection of pre-pregnancy body mass index is limited by early-pregnancy weights or patient self-report, although recent efforts to standardize how this information is collected have improved the data quality for this variable. Information on miscarriage and therapeutic abortions is historically difficult to ascertain, and under-reporting of socially sensitive variables including those related to substance use/abuse, intimate-partner violence and sexually transmitted infections is also likely. Last, socio-economic information at the individual or family level and healthcare-provider identifiers are not available in BORN. Area-level socio-economic information (e.g. education, income, marginalization and deprivation indices) can be obtained, however, through linkage to other resources including Canadian census data.
Data resource access
Access to legacy data sets and the BORN Information System
Data are accessible to contributors through the BORN Information System reporting portal. Each contributor has a designated lead who can grant role-based access for members of their group. Those who do not have access to the reporting portal or who require data that are not available through this mechanism may pursue alternative processes to access BORN Ontario data resources. Legacy data sets and BORN Information System data are available to external requestors to support research, programme evaluation, policy development and surveillance (Table 2). All requests to BORN Ontario are managed in accordance with provincial privacy requirements.
Table 2.
Available data sets at Better Outcomes Registry & Network (BORN) Ontario
| Legacy data holdings | BORN Information System | |
|---|---|---|
| Description | Includes record-level data from:
|
Includes record-level data from birthing hospitals, midwifery practice groups, birthing centres, fertility clinics, prenatal- and newborn-screening laboratories, follow-up clinics, clinical programmes and primary-care organizations |
| Time frame | April 2006–March 2012 | April 2012–present |
| Data dictionary | https://bit.ly/2whlSRu | https://bit.ly/2I55jec |
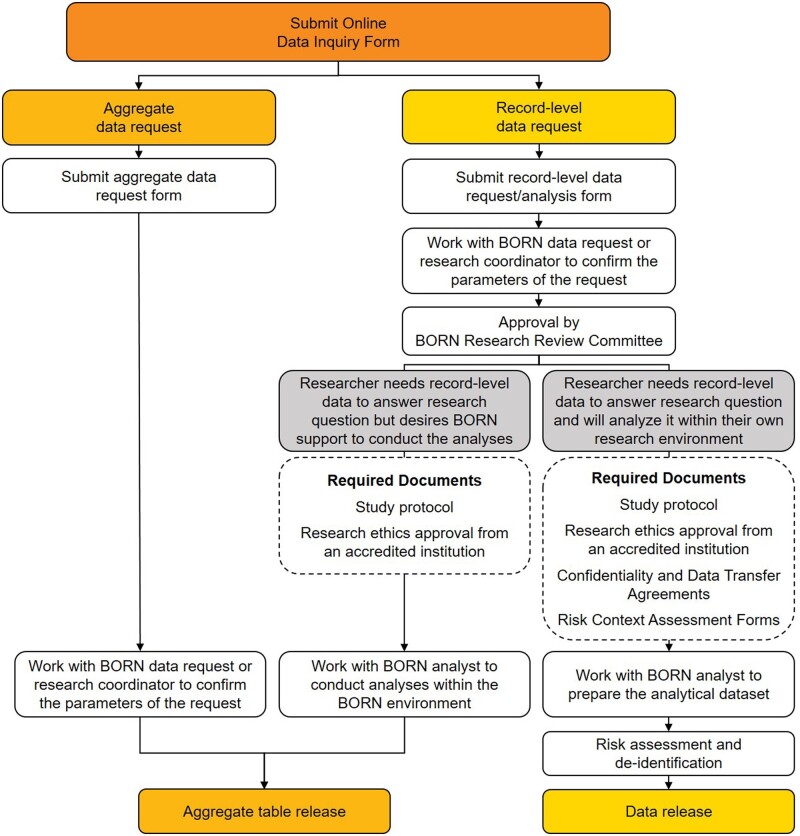
Data requests can be made to the BORN Data Analysis & Request Team and initiated through submission of a data request inquiry form (https://forms.bornontario.ca/Data-Inquiry-Form). From here, the application process varies, depending on the type of information requested (aggregate tables or record-level data) and the support required (Figure 3). BORN coordinators and data analysts work closely with external requestors to navigate data access approval processes, prepare analytical data sets and conduct analyses. At present, BORN Ontario does not provide a platform through which external requestors can interact with the data for research purposes. Research data sets are securely and electronically transferred to external requestors following completion of all of the necessary approval processes.
Figure 3.
Accessing Better Outcomes Registry & Network (BORN) Ontario data. External parties may submit requests for aggregate or record-level data. Requests can be initiated through submission of an online form. Turnaround times and data access fees may vary, depending on the nature and complexity of the request. Requests to access record-level data from BORN Ontario data holdings may be subject to additional approvals.
Data dictionaries for legacy data elements are available for download. The BORN Information System data dictionary is available online as an interactive library and may also be downloaded in portable document form. A data dictionary improvement project is currently underway. Notably, the data dictionary and data elements available from the legacy data sets and the BORN Information System differ. New data elements and updated terminology were added to the BORN Information System in 2012 and may not be available in the historical data. It is not always possible to link some of the older data elements to the new BORN Information System.
Access to data relating to Indigenous peoples in Canada
Data on pregnant individuals and newborns with a postal code where the majority of the population identifies with an Indigenous Nation (First Nation, Inuit and Métis peoples) are only available for public-health activities or research analysis when there is evidence of stakeholder engagement and consent of the Indigenous Nation(s). BORN Ontario has a responsibility to ensure that the information it collects is managed in a culturally appropriate and respectful manner, and thus adheres to the principles of ownership, control, access and possession (OCAP®) and other similar Indigenous frameworks for conducting research pertaining to Indigenous people. The decision to suppress Indigenous data in BORN is based on guidance from Indigenous stakeholders on the collection, interpretation and governance of data related to their community members and communities as a whole.56 Resources are dedicated to facilitating data release to Indigenous stakeholders for programme planning and delivery of maternal, newborn and early-childhood services and does not otherwise release information without evidence of engagement and consent by a community stakeholder.
Data access fees
Costs associated with preparing aggregate data and record-level data sets for external requestors depend on the nature and complexity of the request. Following consultation and an assessment of the project needs, cost estimates can be provided for research-funding applications, for funded research projects and other quality initiative and policy work. Data access fees include consultation, risk assessment and de-identification, data analyst time for file preparation and verification, and an administration fee.
Summary
BORN Ontario is a primary and authoritative resource for reproductive health information and data in Ontario, Canada. The BORN Information System is an accurate and trusted tool for evaluating care delivery and health outcomes of mothers and their newborns. It can further be used to support data-driven change-management strategies in perinatal healthcare policy and programming. Importantly, BORN Ontario data are accessible to local, national and international investigators looking to address research questions relevant to maternal, newborn and paediatric populations.
Acknowledgements
The authors would like to thank Barbara Chapman, Yanfang (Mary) Guo, Sarah McKenna, Cathy Yang and other individuals who have contributed significantly to BORN Ontario since its inception. We acknowledge the epidemiologists, data analysts, data-request and research coordinators, and knowledge-translation specialists at BORN Ontario who coordinate efforts across the province to facilitate and improve care for mothers, children and families, and to provide scientific and technical leadership for Ontario’s health system. In addition, we recognize the important contributions of the technical and regional coordinator teams who support the data platform and the users contributing data.
Funding
Core funding for BORN Ontario is provided by the Ontario Ministry of Health and Long-Term Care.
Conflict of interest
None declared.
Contributor Information
Malia S Q Murphy, OMNI Research Group, Clinical Epidemiology Program, Ottawa Hospital Research, Institute, Ottawa, Canada.
Deshayne B Fell, School of Epidemiology and Public Health, University of Ottawa, Ottawa, Canada; CHEO Research Institute, Ottawa, Canada.
Ann E Sprague, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada; School of Nursing, University of Ottawa, Ottawa, Canada.
Daniel J Corsi, OMNI Research Group, Clinical Epidemiology Program, Ottawa Hospital Research, Institute, Ottawa, Canada; School of Epidemiology and Public Health, University of Ottawa, Ottawa, Canada; CHEO Research Institute, Ottawa, Canada; BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Shelley Dougan, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Sandra I Dunn, OMNI Research Group, Clinical Epidemiology Program, Ottawa Hospital Research, Institute, Ottawa, Canada; CHEO Research Institute, Ottawa, Canada; BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada; School of Nursing, University of Ottawa, Ottawa, Canada.
Vivian Holmberg, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Tianhua Huang, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada; Genetics Program, North York General Hospital, Toronto, Canada; Department of Obstetrics and Gynaecology, University of Toronto, Toronto, Canada.
Moya Johnson, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Michael Kotuba, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Lise Bisnaire, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Pranesh Chakraborty, Department of Pediatrics, University of Ottawa, Ottawa, Canada; Newborn Screening Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Susan Richardson, BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Mari Teitelbaum, Children’s Hospital of Eastern Ontario, Ottawa, Canada.
Mark C Walker, OMNI Research Group, Clinical Epidemiology Program, Ottawa Hospital Research, Institute, Ottawa, Canada; School of Epidemiology and Public Health, University of Ottawa, Ottawa, Canada; BORN Ontario, Children’s Hospital of Eastern Ontario, Ottawa, Canada; Department of Obstetrics, Gynecology & Newborn Care, The Ottawa Hospital, Ottawa, Canada; Department of Obstetrics and Gynecology, University of Ottawa, Ottawa, Canada.
References
- 1. Dunn S, Bottomley J, Ali A, Walker M. 2008 Niday perinatal database quality audit: report of a quality assurance project. Chronic Dis Inj Can 2011;32:21–32. [PubMed] [Google Scholar]
- 2. Public Health Agency of Canada. The Ontario Perinatal Surveillance System Report. Ottawa; 2008. https://www.canada.ca/en/public-health/services/reports-publications/canadian-perinatal-health-report-2008-edition.html (23 March 2020, date last accessed).
- 3. Bacal V, Fell DB, Shapiro H et al. The Canadian Assisted Reproductive Technologies Register (CARTR) Plus database: a validation study. Hum Reprod Open 2020;2020:hoaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lanes A, Fell DB, Teitelbaum M et al. CARTR Plus: the creation of an assisted reproductive technologies registry in Canada. Hum Reprod Open 2020;2020:hoaa22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Huang T, Dougan S, Walker M, Armour CM, Okun N. Trends in the use of prenatal testing services for fetal aneuploidy in Ontario: a descriptive study. Cmajo 2018;6:E436–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang T, Meschino WS, Teitelbaum M, Dougan S, Okun N. Enhanced first trimester screening for trisomy 21 with contingent cell-free fetal DNA: a comparative performance and cost analysis. J Obstet Gynaecol Canada 2017;39:742–49. [DOI] [PubMed] [Google Scholar]
- 7. Bellai-Dussault K, Meng L, Huang T et al. A 2-year review of publicly funded cell-free DNA screening in Ontario: utilization and adherence to funding criteria. Prenat Diagn 2019;40:164–72. [DOI] [PubMed] [Google Scholar]
- 8. Promoting Data Quality—BORN Ontario. https://www.bornontario.ca/en/data/promoting-data-quality.aspx (21 February, 2020, date last accessed).
- 9. Miao Q, Fell DB, Dunn S, Sprague AE. Agreement assessment of key maternal and newborn data elements between birth registry and clinical administrative hospital databases in Ontario. Arch Gynecol Obstet 2019;300:135–43. [DOI] [PubMed] [Google Scholar]
- 10. Dunn S, Bottomley J, Ali A, Walker M. 2008 Niday Perinatal Database quality audit: report of a quality assurance project. Chronic Dis Inj Can 2011;32:32–42. [PubMed] [Google Scholar]
- 11. Dunn S, Lanes A, Sprague AE et al. Data accuracy in the Ontario birth Registry: a chart re-abstraction study. BMC Health Serv Res 2019;19:1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ontario Agency for Health Protection and Promotion (Public Health Ontario). BORN Information System: A Data Quality Assessment for Public Health Monitoring. Toronto, 2016. https://www.publichealthontario.ca/-/media/documents/born-data-quality-assessment.pdf?la=en (1 March 2021, date last accessed).
- 13. Personal Health Information Protection Act. Canada: Legislative Assembly of Ontario. 2004. https://www.ontario.ca/laws/statute/04p03 (1 March 2021, date last accessed).
- 14. Reszel J, Sidney D, Peterson WE et al. The integration of Ontario birth centers into existing maternal-newborn services: health care provider experiences. J Midwifery Womens Health 2018;63:541–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sprague AE, Sidney D, Darling EK et al. Outcomes for the first year of Ontario’s birth center demonstration project. J Midwifery Womens Health 2018;63:532–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Reszel J, Weiss D, Sprague AE et al. A mixed-methods evaluation of the MOREOB program in Ontario hospitals: Participant knowledge, organizational culture, and experiences. BMC Health Serv Res 2019;19:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Weiss D, Fell DB, Sprague AE et al. Effect of implementation of the MOREOB program on adverse maternal and neonatal birth outcomes in Ontario, Canada: a retrospective cohort study. BMC Pregnancy Childbirth 2019;19:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dunn S, Sprague AE, Grimshaw JM et al. A mixed methods evaluation of the maternal-newborn dashboard in Ontario: dashboard attributes, contextual factors, and facilitators and barriers to use: a study protocol. Implement Sci 2016;11:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Weiss D, Dunn SI, Sprague AE et al. Effect of a population-level performance dashboard intervention on maternal-newborn outcomes: an interrupted time series study. BMJ Qual Saf 2018;27:425–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reszel J, Dunn SI, Sprague AE et al. Use of a maternal newborn audit and feedback system in Ontario: a collective case study. BMJ Qual Saf 2019;28:635–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sprague AE, Dunn SI, Fell DB et al. Measuring quality in maternal-newborn care: developing a clinical dashboard. J Obstet Gynaecol Can 2013;35:29–38. [DOI] [PubMed] [Google Scholar]
- 22. Atkinson KM, El-Khatib Z, Barnum G et al. Using mobile apps to communicate vaccination records: a city-wide evaluation with a national immunization app, maternal child registry and public health authorities. Healthc Q 2017;20:41–46. [DOI] [PubMed] [Google Scholar]
- 23. Hayeems RZ, Campitelli M, Ma X, Huang T, Walker M, Guttmann A. Rates of prenatal screening across health care regions in Ontario, Canada: a retrospective cohort study. CMAJ Open 2015;3:E236–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Leclair E, Robert N, Sprague AE, Fleming N. Factors associated with breastfeeding initiation in adolescent pregnancies: a cohort study. J Pediatr Adolesc Gynecol 2015;28:516–21. [DOI] [PubMed] [Google Scholar]
- 25. Lutsiv O, Giglia L, Pullenayegum E et al. A population-based cohort study of breastfeeding according to gestational age at term delivery. J Pediatr 2013;163:1283–88. [DOI] [PubMed] [Google Scholar]
- 26. Dayan N, Joseph KS, Fell DB et al. Infertility treatment and risk of severe maternal morbidity: a propensity score–matched cohort study. CMAJ 2019;191:E118–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sun L-M, Walker MC, Cao H-L, Yang Q, Duan T, Kingdom JCP. Assisted reproductive technology and placenta-mediated adverse pregnancy outcomes. Obstet Gynecol 2009;114:818–24. [DOI] [PubMed] [Google Scholar]
- 28. El-Chaar D, Yang Q, Gao J et al. Risk of birth defects increased in pregnancies conceived by assisted human reproduction. Fertil Steril 2009;92:1557–61. [DOI] [PubMed] [Google Scholar]
- 29. White PM, Commercialization A. Clinical practice: seeking explanation for similarities and differences in Californian and Canadian gestational surrogacy outcomes. Women’s Health Issues 2018;28:239–50. [DOI] [PubMed] [Google Scholar]
- 30. Chen XK, Wen SW, Bottomley J, Smith GN, Leader A, Walker MC. In vitro fertilization is associated with an increased risk for preeclampsia. Hypertens Pregnancy 2009;28:1–12. [DOI] [PubMed] [Google Scholar]
- 31. Yasseen Iii AS, Bassil K, Sprague A, Urquia M, Maguire JL. Late preterm birth and previous cesarean section: a population-based cohort study. J Matern Neonatal Med 2019;32:2400–07. [DOI] [PubMed] [Google Scholar]
- 32. Bassil KL, Yasseen AS, Walker M et al. The association between obstetrical interventions and late preterm birth. Am J Obstet Gynecol 2014;210:538.e1-538–e9. [DOI] [PubMed] [Google Scholar]
- 33. Liu N, Wen SW, Manual DG, Katherine W, Bottomley J, Walker MC. Social disparity and the use of intrapartum epidural analgesia in a publicly funded health care system. Am J Obstet Gynecol 2010;202:273.e1-273–e8. [DOI] [PubMed] [Google Scholar]
- 34. Zhai D, Guo Y, Smith G, Krewski D, Walker M, Wen SW. Maternal exposure to moderate ambient carbon monoxide is associated with decreased risk of preeclampsia. Am J Obstet Gynecol 2012;207:57. [DOI] [PubMed] [Google Scholar]
- 35. Lavigne E, Lima I, Hatzopoulou M et al. Spatial variations in ambient ultrafine particle concentrations and risk of congenital heart defects. Environ Int 2019;130:104953. [DOI] [PubMed] [Google Scholar]
- 36. Lavigne É, Bélair M-A, Rodriguez Duque D et al. Effect modification of perinatal exposure to air pollution and childhood asthma incidence. Eur Respir J 2018;51:1701884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fell DB, Sprague AE, Liu N; for Better Outcomes Registry & Network (BORN) Ontario et al. H1N1 influenza vaccination during pregnancy and fetal and neonatal outcomes. Am J Public Health 2012;102:e33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Walsh LK, Donelle J, Dodds L et al. Health outcomes of young children born to mothers who received 2009 pandemic H1N1 influenza vaccination during pregnancy: retrospective cohort study. BMJ 2019;366:14151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fell DB, Wilson K, Ducharme R et al. Infant respiratory outcomes associated with prenatal exposure to maternal 2009 A/H1N1 influenza vaccination. Ye Z, ed. PLoS One 2016;11:e0160342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Corsi DJ, Walsh L, Weiss D et al. Association between self-reported prenatal cannabis use and maternal, perinatal, and neonatal outcomes. JAMA 2019;322:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Corsi DJ, Hsu H, Weiss D, Fell DB, Walker M. Trends and correlates of cannabis use in pregnancy: a population-based study in Ontario, Canada from 2012 to 2017. Can J Public Health 2019;110:76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ram M, Berger H, Geary M et al. Timing of delivery in women with chronic hypertension. Obstet Gynecol 2018;132:669–77. [DOI] [PubMed] [Google Scholar]
- 43. Dayan N, Lanes A, Walker MC, Spitzer KA, Laskin CA. Effect of chronic hypertension on assisted pregnancy outcomes: a population-based study in Ontario. Canada Fertil Steril 2016;105:1003–09. [DOI] [PubMed] [Google Scholar]
- 44. Hiersch L, Berger H, Okby R; for DOH-NET (Diabetes, Obesity and Hypertension in Pregnancy Research Network) and SOON (Southern Ontario Obstetrical Network) Investigators™ et al. Incidence and risk factors for gestational diabetes mellitus in twin versus singleton pregnancies. Arch Gynecol Obstet 2018;298:579–87. [DOI] [PubMed] [Google Scholar]
- 45. Melamed N, Ray JG, Geary M et al. Induction of labor before 40 weeks is associated with lower rate of cesarean delivery in women with gestational diabetes mellitus. Am J Obstet Gynecol 2016;214:364.e1–8. [DOI] [PubMed] [Google Scholar]
- 46. Peticca P, Keely EJ, Walker MC, Yang Q, Bottomley J. Pregnancy outcomes in diabetes subtypes: how do they compare? A province-based study of Ontario, 2005-2006. J Obstet Gynaecol Canada 2009;31:487–96. [DOI] [PubMed] [Google Scholar]
- 47. Berger H, Melamed N, Murray-Davis B et al. Prevalence of pre-pregnancy diabetes, obesity, and hypertension in Canada. J Obstet Gynaecol Canada 2019;41:1579–88.e2. [DOI] [PubMed] [Google Scholar]
- 48. Murray-Davis B, Berger H, Melamed N et al. Weight gain during pregnancy: Does the antenatal care provider make a difference? A retrospective cohort study. Cmajo 2019;7:E283–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Guo Y, Miao Q, Huang T et al. Racial/ethnic variations in gestational weight gain: a population-based study in Ontario. Can J Public Health 2019;110:657–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McDonald SD, Woolcott C, Chapinal N, Guo Y, Murphy P, Dzakpasu S. Interprovincial variation in pre-pregnancy body mass index and gestational weight gain and their impact on neonatal birth weight with respect to small and large for gestational age. Can J Public Health 2018;109:527–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chassé M, Tinmouth A, Goldman M et al. Evaluating the clinical effect of female blood donors of child-bearing age on maternal and neonatal outcomes: a cohort study. Transfus Med Rev 2020;34:117–23. [DOI] [PubMed] [Google Scholar]
- 52. Corsi DJ, Donelle J, Sucha E et al. Maternal cannabis use in pregnancy and child neurodevelopmental outcomes. Nat Med 2020;26:1536–40. [DOI] [PubMed] [Google Scholar]
- 53. Lavigne E, Donelle J, Hatzopoulou M et al. Spatiotemporal variations in ambient ultrafine particles and the incidence of childhood asthma. Am J Respir Crit Care Med 2019;199:1487–95. [DOI] [PubMed] [Google Scholar]
- 54. Wu Y(M), McArthur E, Dixon S, Dirk JS, Welk BK. Association between intrapartum epidural use and maternal postpartum depression presenting for medical care: a population-based, matched cohort study. Int J Obstet Anesth 2018;35:10–16. [DOI] [PubMed] [Google Scholar]
- 55. Burton KR, Park AL, Fralick M, Ray JG. Risk of early-onset breast cancer among women exposed to thoracic computed tomography in pregnancy or early postpartum. J Thromb Haemost 2018;16:876–85. [DOI] [PubMed] [Google Scholar]
- 56. Better Outcomes Registry & Network (BORN) Ontario. BORN Engagement with Indigenous Stakeholders: 2012-2013. Ottawa, 2016. https://www.bornontario.ca/en/publications/resources/Documents/Indigenous-stakeholder-feedback-to-BORN-Report_2016-Final2.pdf (1 December 2020, last date accessed).