Abstract
Objectives
Increased exposure to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as a result of having an essential job is compounded by factors such as age, race, and ethnicity. We used a cross-sectional study design to describe disparities in the seroprevalence of SARS-CoV-2 immunoglobulin G (IgG) test results by demographic characteristics and clinical roles among a cohort of health care workers employed by the largest Midwestern health care system in the United States.
Methods
We collected 16 233 SARS-CoV-2 IgG serum samples from June 8 through July 10, 2020, from a convenience sample of Illinois- and Wisconsin-based adult health care workers. The research team, in collaboration with ACL Laboratories, used a SARS-CoV-2 IgG assay to detect the presence of SARS-CoV-2 IgG antibodies. Study data included SARS-CoV-2 IgG assay results and demographic characteristics of workers (age, sex, race, ethnicity, clinical role, zip code). We generated crude and adjusted odds ratios (ORs) to describe disparities in seroprevalence distribution among demographic and social factors.
Results
Of 16 233 IgG serum samples tested, 622 (3.8%) test results were positive for SARS-CoV-2. We found significant disparities in SARS-CoV-2 positivity by age, race, ethnicity, and clinical role. Participants aged 32-82 had lower adjusted ORs (aORs) of positive IgG than participants aged 18-31 (aOR range, 0.54-0.66). Odds of positivity were higher among Black (aOR = 3.86), Asian (aOR = 1.42), and mixed-race (aOR = 1.99) workers than among White workers; among Hispanic workers (aOR = 1.80) than among non-Hispanic workers; and among coronavirus disease 2019 (COVID-19) clinical workers (aOR = 1.86) than among nonclinical workers.
Conclusions
Public health efforts should focus on increasing COVID-19 safety messaging, testing, vaccination, and other prevention efforts for people who are young, non-White, Hispanic, and working in COVID-19–clinical units.
Keywords: public health, disparity, communicable diseases, SARS-CoV-2, antibodies, viral
The complete clinical and epidemiological picture of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), is not well understood. As of January 15, 2021, more than 93 million cases of COVID-19 had been confirmed and more than 2 million deaths had been attributed worldwide to COVID-19; more than 389 000 of those deaths had occurred in the United States. 1 Although information so far suggests that most cases of COVID-19 are mild, older age and certain underlying health conditions (eg, obesity, certain cardiovascular disorders, cancer) have been linked to an increased risk of severe illness. 2,3 New and ongoing research has found disparities in COVID-19 distribution, morbidity, and mortality, particularly among racial/ethnic minority groups and urban dwellers as compared with non-Hispanic White people. 3,4
We used a sensitive and specific SARS-CoV-2 immunoglobulin G (IgG) assay (SARS-CoV-2 IgG assay) to test convalescent serum as a reliable method for assessing exposure in a population. 5 Characterizing the magnitude and distribution of the SARS-CoV-2 virus by relying on detection of active SARS-CoV-2 viral RNA shedding has proven to be impractical because of such factors as a lack of symptoms, mild or varying symptoms, and/or limited testing opportunities. 6 Instead, positive IgG status, or seropositivity, indicates antibodies developed from past exposure to SARS-CoV-2, thus providing a better representation of the distribution of COVID-19 than relying on COVID-19 testing alone. To understand the distribution of COVID-19 and SARS-CoV-2, the largest Midwestern health care system collected 16 233 serum samples from clinical and nonclinical health care workers to test for SARS-CoV-2 IgG. IgG tests were provided to health care workers free of charge at their workplace or at a local-affiliated laboratory, which facilitated access to treatment. 7
Disparities exist in COVID-19 distribution among racial/ethnic minority groups, especially Black and Hispanic populations. 8,9 Compared with non-Hispanic White people, non-Hispanic Black people are more likely to contract COVID-19 and are twice as likely to die of COVID-19–related complications. 3,4 Non-Hispanic Black and Hispanic people may be at greater risk of exposure to COVID-19 than non-Hispanic White people because they are more likely to be essential workers and also tend to live in densely populated areas and multigenerational households; examples include Chicago, Illinois, and Milwaukee, Wisconsin,8,9 2 city centers examined in our study. Preliminary COVID-19 research into the causes of disparity primarily indicates social factors rather than medical factors. 8
This study is unique in that it represents a large sample of Midwestern health care employees and examines the demographic representation of health care employees with SARS-CoV-2 IgG-positive status and SARS-CoV-2 IgG-negative status, including people with varying levels of employment-related exposure. We also examined home zip code to assess where in the United States people reside. Most importantly, this study eliminated historic barriers to testing for non-White populations by offering the test free of charge to participating health care employees. This study had 2 objectives: (1) to describe disparities in SARS-CoV-2 IgG seroprevalence by demographic characteristics and clinical role in a large cohort of health care employees and (2) to provide the odds of SARS-CoV-2 IgG seroprevalence, adjusted by demographic characteristics and clinical role, overall and in the 2 states the health care system serves.
Methods
Using a cross-sectional study design, we recruited health care employees from within a health care system consisting of about 70 000 employees across 26 hospitals and more than 500 sites of care in Illinois and Wisconsin. ACL Laboratories used the SARS-CoV-2 IgG assay to test for seropositivity. We obtained institutional review board approval from the health care system’s internal institutional review board. The health care system’s executive team authorized the enrollment of up to 20 000 participants or complete SARS-CoV-2 IgG testing by July 10, 2020, free of charge to the participant.
Participants
We enrolled and tested a convenience sample of 16 233 participants from June 8 through July 10, 2020. For study inclusion, English- and Spanish-speaking adults aged ≥18 employed by the health care system in full- or part-time roles as of the study initiation date were eligible for study inclusion. Employees who met study inclusion criteria and completed a laboratory blood draw to test for SARS-CoV-2 IgG were included in the study. About 23% of employees participated in the study.
SARS CoV-2 IgG Assay
The research team, in collaboration with ACL Laboratories, collected serum specimens from all participants to detect SARS-CoV-2 IgG using the SARS-CoV-2 IgG Abbott Architect assay (Abbott Diagnostics). 10,11 The qualitative assay was designed to detect IgG antibodies to the nucleocapsid protein of SARS-CoV-2 in serum from patients, with a positive IgG test result indicated by a manufacturer-established cutoff point ≥1.40 Index (signal/cutoff). 11 Because of the pandemic, the assay was made available by the US Food and Drug Administration under the Emergency Use Authorization authority. Performance characteristics of the SARS-CoV-2 IgG assay were validated internally at ACL Laboratories (sensitivity, 98.7%; specificity, 99.2%). 12
Procedures
On June 6, 2020, the health care system’s public affairs and marketing team, under the direction of the research team, sent a recruitment email to all employees’ work email addresses with a detailed description of the study. The email provided instructions for participation in the study, including an alteration of consent and a study-specific registration passcode. Interested employees were instructed to register for and/or log into their active online health portal, an online account for central storage and access of patients’ health records, including appointments, tests, and results. Employees were considered participants in this study once they voluntarily had their blood drawn, not at registration.
Data gathered for this study included SARS-CoV-2 IgG assay result (positive or negative) and demographic characteristic of interest stored in Epic, the health care system’s electronic medical record database. The health care system’s research analytics team acted as an honest broker for the study research team, providing data with no identifiers to the research team other than zip code. A unique patient identification number and associated discrete variable fields were shared in a final analytic data set.
Variables
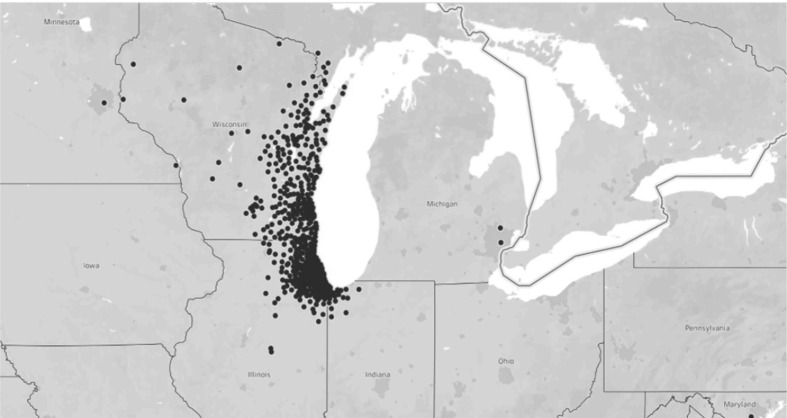
Data on age were collected as a continuous variable and grouped into quantiles (18-31, 32-40, 41-52, 53-82) for analysis. Because age is an important factor in COVID-19 risk, age was grouped into quantiles to evaluate risk by increasing age and to avoid underrepresentation of the oldest participants, who are less likely than younger people to work in health care. Race was categorized as White, Black, Asian, American Indian, or mixed race (for participants who identified as ≥2 races); 399 (2.5%) participants had missing data on race. Race and ethnicity are categorized separately in the electronic medical record; as such, race is not necessarily exclusive of being non-Hispanic. Sex was categorized as male and female; 2 participants were missing data on race. Clinical role was categorized as COVID-19–clinical (participants working in a clinical capacity on COVID-19–designated units), clinical (participants working in a clinical capacity on non–COVID-19–designated units), or nonclinical (participants in nonclinical roles such as administration and hospital support staff). Finally, data on state and zip code represented participants’ home locations and were used to group participants as city dwellers or non–city dwellers (Figure).
Figure.
Map of distribution of health care workers at a large Midwestern health care system (N = 16 233) who received testing for severe acute respiratory syndrome coronavirus 2, June 8–July 10, 2020, Illinois and Wisconsin.
Statistical Methods
We managed data and conducted analyses using SAS version 9.4 (SAS Institute, Inc). We described the overall sample, including demographic characteristics, clinical role, and SARS-CoV-2 IgG status (outcome), as numbers and percentages, means and SDs, or medians and interquartile ranges, as appropriate. Bivariate analyses highlight variables across IgG status. Corresponding measures of association included mean difference for continuous age and odds ratios (ORs) for age quantiles, sex, race, ethnicity, and clinical role. We determined the odds of seroprevalence for each variable relative to the reference group. We used the Pearson χ2 test to determine overall differences in seroprevalence and the Fisher exact test when cell sizes were <5. We used the Wald χ2 test to determine differences between each variable and its reference group, with P < .05 considered significant.
Finally, we calculated logistic regressions to determine the crude ORs and adjusted ORs (aORs) of seroprevalence in the overall sample and in the Illinois and Wisconsin cohorts. Since the beginning of the COVID-19 pandemic in the United States, Illinois and Wisconsin had markedly different peaks and demographic patterns of disease; as such, we performed separate models to highlight similar types of disparities in demographic characteristics and clinical roles between the 2 states. We adjusted all 3 logistic regressions for age quantiles, race, ethnicity, and clinical role.
Results
Overall, participants had a mean (SD) age of 41.8 (12.3), and most were female (13 890 of 16 231, 85.6%), White (13 500 of 15 842, 85.2%), and non-Hispanic (n = 15 265, 94.0%); had a clinical role in the health care system (n = 9308, 57.3%); and lived in Wisconsin (n = 9988, 61.5%). Of the 16 233 participants, 622 (3.8%) had a positive IgG test result (Table 1).
Table 1.
Demographic characteristics of health care workers at a large Midwestern health care system (N = 16 233), overall and by SARS-CoV-2 IgG-positive status, Illinois and Wisconsin, June 8–July 10, 2020
| Characteristic | Total a | IgG positive | IgG negative | Measure of association (95% CI) | P value b |
|---|---|---|---|---|---|
| Total | 16 233 (100.0) | 622 (3.8) | 15 611 (96.2) | ||
| Age, y | <.001 | ||||
| Mean (SD) | 41.8 (12.3) | 39.5 (12.5) | 41.9 (12.3) | −2.39 (−3.37 to −1.40) | |
| Median (IQR) | 40.0 (21.0) | 38.0 (22.0) | 40.0 (20.0) | ||
| 18-31 | 4073 (25.1) | 226 (5.5) | 3847 (94.5) | 1.0 [Reference] | |
| 32-40 | 4124 (25.4) | 126 (3.1) | 3998 (96.9) | 0.54 (0.43 to 0.67) | |
| 41-52 | 4122 (25.4) | 147 (3.6) | 3975 (96.4) | 0.63 (0.51 to 0.78) | |
| 53-82 | 3914 (24.1) | 123 (3.1) | 3791 (96.9) | 0.55 (0.44 to 0.69) | |
| Sex (n = 16 231) | .88 | ||||
| Male | 2341 (14.4) | 91 (3.9) | 2250 (96.1) | 1.0 [Reference] | |
| Female | 13 890 (85.6) | 531 (3.8) | 13 359 (96.2) | 0.98 (0.78 to 1.23) | |
| Race (n = 15 842) | <.001 | ||||
| White | 13 500 (85.2) | 423 (3.1) | 13 077 (96.9) | 1.0 [Reference] | |
| Black | 587 (3.7) | 62 (10.6) | 525 (89.4) | 3.65 (2.76 to 4.83) | |
| Asian | 787 (5.0) | 46 (5.8) | 741 (94.2) | 1.92 (1.40 to 2.63) | |
| American Indian | 56 (0.4) | 2 (3.6) | 54 (96.4) | 1.15 (0.28 to 4.72) | |
| Mixed | 912 (5.8) | 60 (6.6) | 852 (93.4) | 2.18 (1.65 to 2.88) | |
| Ethnicity | <.001 | ||||
| Non-Hispanic | 15 265 (94.0) | 556 (3.6) | 14 709 (96.4) | 1.0 [Reference] | |
| Hispanic | 968 (6.0) | 66 (6.8) | 902 (93.2) | 1.94 (1.49 to 2.52) | |
| Clinical role c | <.001 | ||||
| Nonclinical | 4576 (28.2) | 139 (3.0) | 4437 (97.0) | 1.0 [Reference] | |
| Clinical | 9308 (57.3) | 330 (3.5) | 8978 (96.5) | 1.17 (0.96 to 1.44) | |
| COVID-19–clinical | 2349 (14.5) | 153 (6.5) | 2196 (93.5) | 2.20 (1.76 to 2.81) | |
| State | <.001 | ||||
| Wisconsin | 9988 (61.5) | 226 (2.3) | 9762 (97.7) | 1.0 [Reference] | |
| Illinois | 6245 (38.5) | 396 (6.3) | 5849 (93.7) | 2.90 (2.48 to 3.46) | |
| Illinois (n = 6245) | .02 | ||||
| Non-Chicago | 4962 (79.5) | 297 (6.0) | 4665 (94.0) | 1.0 [Reference] | |
| Chicago | 1283 (20.5) | 99 (7.7) | 1184 (92.3) | 1.31 (1.04 to 1.66) | |
| Wisconsin (n = 9988) | <.001 | ||||
| Non-Milwaukee | 7532 (75.4) | 135 (1.8) | 7397 (98.2) | 1.0 [Reference] | |
| Milwaukee | 2456 (24.6) | 91 (3.7) | 2365 (96.3) | 2.11 (1.61 to 2.76) |
Abbreviations: COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; IQR, interquartile range; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
aPercentages represent column percentages, and percentages across IgG groups represent row percentages.
bSignificance was determined using the Pearson χ2 test for overall differences in associations between variables by exposure, with the Fisher exact test interpreted if any cell was <5. P < .05 was considered significant.
cClinical role was categorized as COVID-19–clinical (participants working in a clinical capacity on COVID-19–designated units), clinical (participants working in a clinical capacity on non–COVID-19–designated units), or nonclinical (participants in nonclinical roles such as administration and hospital support staff).
Participants with a positive IgG test result were significantly younger than participants with a negative IgG test result (mean difference = –2.39; 95% CI, −3.37 to −1.40; P < .001; Table 1). We found a significant association between age quantiles and IgG positivity. The odds of IgG positivity were 0.46 times lower for participants aged 32-40, 0.37 times lower for participants aged 41-52, and 0.45 times lower for participants aged 53-82 compared with participants aged 18-31 (P < .001). We found no significant association between IgG positivity status and sex.
We found a significant association between race and IgG positivity. Of 622 participants with a positive IgG test result, 10.6% were Black, 6.6% were mixed race, 5.8% were Asian, 3.6% were American Indian, and 3.1% were White (Table 1). In the bivariate analysis, the odds of IgG positivity were 3.65 times higher among Black participants, 1.92 times higher among Asian participants, and 2.18 times higher among mixed-race participants than among White participants (P < .001). We found no significant differences in seropositivity between American Indian and White participants. Hispanic participants had 1.94 times higher odds of seropositivity than non-Hispanic participants (P < .001).
The association between clinical role and IgG positivity was significant (P < .001), driven by large differences in seropositivity between COVID-19–clinical and nonclinical participants (Table 1). COVID-19–clinical participants had 2.22 times higher odds of IgG seropositivity than nonclinical participants.
A total of 396 (6.3%) Illinois participants and 226 (2.3%) Wisconsin participants had a positive IgG test result. Illinois participants had 2.92 times higher odds of being seropositive than Wisconsin participants (P < .001). Workers who lived in Chicago and Milwaukee had 1.31 and 2.11 times higher odds, respectively, of seropositivity than their non–urban-dwelling counterparts (P < .001; Table 1).
Overall Sample Models
In the adjusted model, all 3 older age groups (32-40, 41-52, 53-82) had significantly lower odds of seroprevalence than participants aged 18-31: age 32-40 (aOR = 0.52; 95% CI, 0.43-0.68; P < .001), age 41-52 (aOR = 0.66; 95% CI, 0.53-0.83; P < .001), and age 53-82 (aOR = 0.65; 95% CI, 0.51-0.83; P < .001). Odds of seroprevalence were also significantly higher among Black, Asian, and mixed-race participants than among White participants: Black (aOR = 3.86; 95% CI, 2.91-5.12), Asian (aOR = 1.87; 95% CI, 1.37-2.57), and mixed race (aOR = 1.99; 95% CI, 1.50-2.63). Hispanic participants had 1.80 (95% CI, 1.34-2.42) times higher odds of seroprevalence than non-Hispanic participants (P < .001). Furthermore, COVID-19–clinical participants had 1.86 (95% CI, 1.45-2.40) times higher odds of seroprevalence than nonclinical participants (P < .001); however, we found no significant difference in odds of seroprevalence between clinical and nonclinical participants.
Illinois Cohort
In the Illinois cohort, odds of seroprevalence were similar to the overall model by age and clinical role. However, Black participants had significantly higher odds of seroprevalence than White participants (aOR = 2.54; 95% CI, 1.76-3.66; P < .001), but these odds were attenuated to the null compared with the overall sample. Although Hispanic participants had 1.44 (95% CI, 0.99-2.10) times higher odds of seroprevalence than non-Hispanic participants, the finding was not significant.
Wisconsin Cohort
In the adjusted model for the Wisconsin cohort, findings on age were similar to findings in the overall and Illinois models. Although COVID-19–clinical participants had 1.47 (95% CI, 0.94-2.29) times higher odds of seroprevalence than nonclinical participants, the finding was not significant (Table 2). The odds of seroprevalence were significantly higher among Black participants than among White participants (aOR = 4.79; 95% CI, 3.04-7.55; P < .001). Hispanic participants had significantly higher odds of seroprevalence than non-Hispanic participants (aOR = 2.12; 95% CI, 1.30-3.45; P = .003).
Table 2.
Crude and adjusted odds of SARS-CoV-2 IgG-positive status among health care workers at a large Midwestern health care system (N = 16 233), by demographic characteristics, Illinois and Wisconsin, June 8–July 10, 2020
| Characteristic | Overall | Illinois | Wisconsin | |||
|---|---|---|---|---|---|---|
| OR (95% CI) [P value] a | aOR (95% CI) [P value] a | OR (95% CI) [P value] a | aOR (95% CI) [P value] a | OR (95% CI) [P value] a | aOR (95 CI%) [P value] a | |
| Age, y | ||||||
| 18-31 | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] |
| 32-40 | 0.54 (0.43-0.67) [<.001] | 0.54 (0.43-0.68) [<.001] | 0.54 (0.41-0.72) [<.001] | 0.52 (0.39-0.71) [<.001] | 0.54 (0.32-0.78) [.001] | 0.56 (0.38-0.81) [.002] |
| 41-52 | 0.63 (0.51-0.78) [<.001] | 0.66 (0.53-0.83) [<.001] | 0.61 (0.46-0.80) [<.001] | 0.62 (0.47-0.83) [.001] | 0.68 (0.48-0.95) [.03] | 0.70 (0.49-1.00) [.047] |
| 53-82 | 0.55 (0.44-0.69) [<.001] | 0.65 (0.51-0.83) [<.001] | 0.48 (0.36-0.64) [<.001] | 0.53 (0.39-0.73) [<.001] | 0.62 (0.43-0.89) [.01] | 0.71 (0.48-1.04) [.08] |
| Race | ||||||
| White | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] |
| Black | 3.65 (2.76-4.83) [<.001] | 3.86 (2.91-5.12) [<.001] | 2.34 (1.63-3.36) [<.001] | 2.54 (1.76-3.66) [<.001] | 4.58 (2.91-7.19) [<.001] | 4.79 (3.04-7.55) [<.001] |
| Asian | 1.12 (1.40-2.63) [<.001] | 1.87 (1.37-2.57) [<.001] | 1.42 (1.01-2.01) [.046] | 1.39 (0.98-1.98) [.06] | 0.97 (0.40-2.39) [.95] | 0.97 (0.40-2.39) [.95] |
| American Indian | 1.15 (0.28-4.71) [.85] | 0.85 (0.20-3.55) [.82] | 1.15 (0.27-4.85) [.84] | 0.93 (0.22-4.04) [.92] | — b | — b |
| Mixed | 2.18 (1.65-2.88) [<.001] | 1.99 (1.50-2.63) [<.001] | 1.34 (0.99-1.81) [.05] | 1.27 (0.94-1.72) [.12] | 1.20 (0.38-3.80) [.76] | 1.11 (0.32-3.26) [.97] |
| Ethnicity | ||||||
| Non-Hispanic | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] |
| Hispanic | 1.94 (1.49-2.52) [<.001] | 1.80 (1.34-2.42) [<.001] | 1.49 (1.08-2.05) [.01] | 1.44 (0.99-2.10) [.06] | 2.06 (1.27-3.33) [.003] | 2.12 (1.30-3.45) [.003] |
| Clinical role c | ||||||
| Nonclinical | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] | 1.0 [Ref] |
| Clinical | 1.17 (0.96-1.44) [.12] | 1.09 (0.88-1.35) [.41] | 1.18 (0.91-1.54) [.21] | 1.09 (0.82-1.44) [.57] | 1.21 (0.88-1.66) [.25] | 1.13 (0.82-1.57) [.46] |
| COVID-19–clinical | 2.22 (1.76-2.81) [<.001] | 1.86 (1.45-2.40) [<.001] | 2.10 (1.57-2.81) [<.001] | 1.76 (1.28-2.42) [.001] | 1.69 (1.11-2.58) [.02] | 1.47 (0.94-2.29) [.09] |
Abbreviations: aOR, adjusted odds ratio; COVID-19, coronavirus disease 2019; IgG, immunoglobulin G; IQR, interquartile range; OR, odds ratio; ref, reference group; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
aSignificance was determined using the Wald χ2 test for direct differences between a variable level relative to the reference level of the same variable, with P < .05 considered significant.
bAt least one category count for this level of race was 0, inhibiting the calculating of ORs.
cClinical role was categorized as COVID-19–clinical (participants working in a clinical capacity on COVID-19–designated units), clinical (participants working in a clinical capacity on non–COVID-19–designated units), or nonclinical (participants in nonclinical roles such as administration and hospital support staff).
Discussion
The seroprevalence of SARS-CoV-2 IgG was only 3.8% among 16 233 participants, which is in line with similar studies. 13 -15 Our study documented and described disparities in SARS-CoV-2 IgG seroprevalence in mostly unmodifiable factors (eg, age, race, ethnicity) across 2 states that had different outbreak histories and trajectories. Our findings support growing evidence that certain groups are being disproportionately exposed to SARS-CoV-2, regardless of geographic location.
Seroprevalence varied significantly by state, with 6.3% seropositivity in Illinois and 2.3% seropositivity in Wisconsin. We found that state-specific seropositivity was largely driven by the 2 population centers—Chicago and Milwaukee—suggesting that urban dwellers are more generally affected by COVID-19 than non–urban dwellers, regardless of the timing, size, or severity of the outbreak in the state.
The odds of SARS-CoV-2 seroprevalence were significant by race, ethnicity, age, and clinical role. Seropositivity was generally higher among participants who were non-White (Black and Asian) rather than White, Hispanic rather than non-Hispanic, and younger (aged 18-31) rather than older (aged 32-82). These findings were supported among the overall cohort and within-state analyses, albeit to slightly different degrees. These findings reinforce mounting evidence that racial, ethnic, and age disparities in exposure to SARS-CoV-2 exist, regardless of geography. 3,4,7 -9
We found no significant differences in seroprevalence between clinical and nonclinical participants, indicating that clinical exposure can be mitigated by protective measures taken in health care systems. Overall and within each state, participants working in COVID-19–clinical departments had the highest seroprevalence compared with participants working in clinical and nonclinical departments. This finding was predictable, because frequent exposure to SARS-CoV-2, even with protection and/or at low consistent levels, could lead to the development of SARS-CoV-2 IgG antibodies. 16,17 However, our study raises new questions about factors that contribute to SARS-CoV-2 exposure and subsequent COVID-19 disease. Although it is not surprising that SARS-CoV-2 seroprevalence was more common among people who worked in COVID-19–clinical departments than among people who did not, people who worked in COVID-19–clinical departments were also more likely to be non-White, Hispanic, and younger than workers in other non–COVID-19 and nonclinical units.
Our study responds to the Centers for Disease Control and Prevention’s call for research to better understand potential COVID-19 risk factors of certain occupations, age, and race/ethnicity. 18 Although our study describes demographic and social disparities in SARS-CoV-2 exposure, it also highlights that increased risk of morbidity and mortality due to clinical role may be compounded by factors such as age, race, and ethnicity. Increased exposure to SARS-CoV-2 as a result of having an essential job is compounded by the social and living factors that are more common among young, non-White, and Hispanic people, resulting in disproportionate odds of exposure.
Strengths and Limitations
This study has several strengths. First, this study provides data on SARS-CoV-2 IgG prevalence from the largest Midwestern health care employee cohort to date and offers critical and novel information on demographic characteristics associated with seroprevalence. Second, because this study was offered free and at convenient locations for all employees, testing barriers for marginalized groups (eg, non-White, Hispanic, urban dwelling) were eliminated, providing a more accurate accounting of the prevalence and distribution of SARS-CoV-2 than by relying on COVID-19 testing alone. 8 Third, aggregated data were collected via electronic health record with minimal missing data points.
However, this study also had several limitations. First, the study was limited by the use of a convenience sample. Although the research team attempted to mitigate selection issues, the use of employee email for primary study advertisement may have limited the inclusion of some workers. Second, the short period between the initial study-related advertisement email on June 6, 2020, and the last day of data collection on July 10, 2020, may also have contributed to selection bias. Third, information on lifestyle and social habits of health care employees may have provided critical insight into differences between workers with a positive or negative IgG test result. Lastly, although regression models could have used interactions to describe between-state differences, stratified analyses were used for easier interpretation and to maintain focus on disparities by characteristics and not by state.
Conclusion
This study adds to the literature by highlighting disparities in demographic characteristics among health care workers with SARS-CoV-2 infection. Further studies should examine lifestyle and social factors among health care workers to fill gaps in disparity research.
Acknowledgments
The authors thank the many people at Advocate Aurora Health who supported this study, especially the executive team who financially supported staff testing, without which this study would not be possible: Public Affairs and Marketing, Andy Marek and Chris Blumberg in Analytics, ACL leadership and staff, the Health Informatics Technology team, Advocate Aurora Research Institute, Institutional Review Board, and Maureen Shields for early work on this project.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Veronica Fitzpatrick, DrPH https://orcid.org/0000-0002-0509-3475
References
- 1. Coronavirus Resource Center . COVID-19 United States cases. Updated August 7, 2020. Accessed August 8, 2020. https://coronavirus.jhu.edu/us-map
- 2. Havers FP., Reed C., Lim T. et al. Seroprevalence of antibodies to SARS-CoV-2 in 10 sites in the United States, March 23–May 12, 2020 [online ahead of print July 21, 2020]. JAMA Intern Med. 10.1001/jamainternmed.2020.4130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Selden TM., Berdahl TA. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood). 2020;39(9):1624-1632. 10.1377/hlthaff.2020.00897 [DOI] [PubMed] [Google Scholar]
- 4. Brown IM., Khan A., Slocum J., Campbell LF., Lacey JR., Landry AM. COVID-19 disparities and the Black community: a health equity–informed rapid response is needed. Am J Public Health. 2020;110(9):1350-1351. 10.2105/AJPH.2020.305804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. US Food and Drug Administration . EUA authorized serology test performance. Updated August 7, 2020. Accessed August 7, 2020. https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/eua-authorized-serology-test-performance
- 6. Robbiani DF., Gaebler C., Muecksch F. et al. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature. 2020;584(7821):437-442. 10.1038/s41586-020-2456-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention . COVID-19: health equity considerations and racial and ethnic minority groups. Updated July 24, 2020. Accessed August 16, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html
- 8. Holmes L Jr., Enwere M., Williams J. et al. Black–White risk differentials in COVID-19 (SARS-CoV-2) transmission, mortality and case fatality in the United States: translational epidemiologic perspective and challenges. Int J Environ Res Public Health. 2020;17(12):4322. 10.3390/ijerph17124322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Figueroa JF., Wadhera RK., Lee D., Yeh RW., Sommers BD. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood). 2020;39(11):1984-1992. 10.1377/hlthaff.2020.01040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lieberman JA., Pepper G., Naccache SN., Huang M-L., Jerome KR., Greninger AL. Comparison of commercially available and laboratory-developed assays for in vitro detection of SARS-CoV-2 in clinical laboratories. J Clin Microbiol. 2020;58(8):e00821-20. 10.1128/JCM.00821-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. US Food and Drug Administration . SARS-CoV-2 IgG for use with Architect. Revised June 2020. Accessed December 2020. Accessed January 13, 2021. https://www.fda.gov/media/137383/download
- 12. Bryan A., Pepper G., Wener MH. et al. Performance characteristics of the Abbott Architect SARS-CoV-2 IgG assay and seroprevalence in Boise, Idaho. J Clin Microbiol. 2020;58(8):e00941-20. 10.1128/JCM.00941-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pollán M., Pérez-Gómez B., Pastor-Barriuso R. et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide population-based seroepidemiological study. Lancet. 2020;396(10250):535-544. 10.1016/S0140-6736(20)31483-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stringhini S., Wisniak A., Piumatti G. et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet. 2020;396(10247):313-319. 10.1016/S0140-6736(20)31304-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oran DP., Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362-367. 10.7326/M20-3012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leung GM., Lim WW., Ho L-M. et al. Seroprevalence of IgG antibodies to SARS-coronavirus in asymptomatic or subclinical population groups. Epidemiol Infect. 2006;134(2):211-221. 10.1017/S0950268805004826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Suthar MS., Zimmerman MG., Kauffman RC. et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep Med. 2020;1(3):100040. 10.1016/j.xcrm.2020.100040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention . Assessing risk factors for severe COVID-19 illness. Updated November 30, 2020. Accessed January 13, 2021. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/assessing-risk-factors.html [PubMed]