Abstract
Background
A high frequency of BRCA mutations has been established in Nigerian breast cancer (BC) patients. Recently, patients’ and first-degree relatives’ interest have been raised on cancer genetic risk assessment through our awareness activities in Nigeria. This led to the emergence of nurse-led cancer genetic counselling (CGC) and testing aimed at providing standard-of-care for individuals at increased risk of hereditary breast and ovarian cancers.
Methods
In June 2018, CGC and testing of patients with BC and ovarian cancer (OC) commenced in collaboration with Color Genomics Inc. for a 30-panel gene testing. Previously trained nurses in CGC at the University College Hospital, Ibadan offered genetic counselling (GC) to willing patients with BC and gynaecological cancer in four out-patient oncology clinics and departments for the pilot study. Consultation consisted of CGC, patient’s history, pedigree and sample collection for genetic testing (GT).
Results
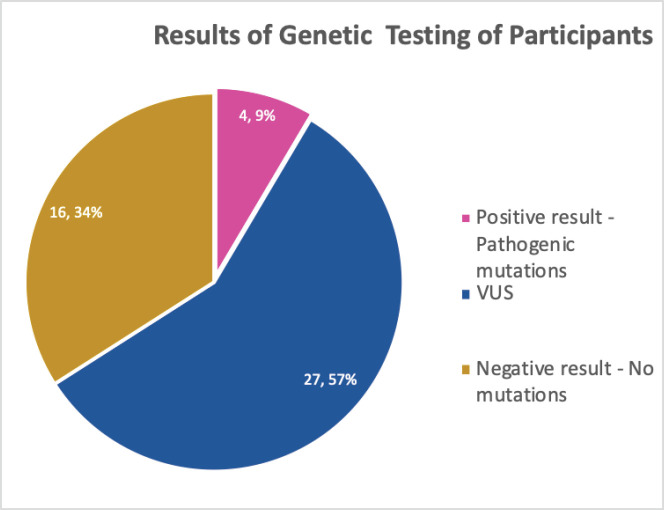
Forty-seven patients – 40 with BC, five with OC and two with endometrial cancer received GC, and all chose to undergo GT. The average age at testing was 48.2 ± 12.1 years. Eight women reported a known family cancer history and there were more perceived benefits than barriers to GT with the patients experiencing the desire for none of their relative to have cancer. Results revealed no mutations in 27 (57.4%), 16 (4.0%) variants of unknown significance and 4 (8.5%) pathogenic mutations.
Conclusion
Personalised cancer care utilises GC and testing for cancer risk assessment towards prevention and early detection in high risk women. The study indicates the necessity of expanded cancer genetic services for integration into patient care and cancer prevention.
Keywords: breast cancer, ovarian cancer, genetic counselling, genetic testing, genetic risk assessment
Introduction
Hereditary cancer syndromes account for approximately 5%–10% of all cancers [1, 2] with breast cancer (BC) and ovarian cancer (OC) association with germline mutations established since the early 1990s [3]. Hereditary breast and ovarian cancer (HBOC) is a syndrome particularly affecting certain populations [4] like the African-American women [5] and African women [6, 7]. Studies in Nigeria, the most populous African country, have reported a high frequency of germline mutations, particularly of BRCA1/2 variant associated with HBOC risk, in the Nigerian women of up to 16% [8, 9]. The implication is that many Nigerian women have up to an 85% and 46% lifetime risk of BC and OCs, respectively. While BC is the leading cause of cancer death in women in Nigeria, OC incidence is increasing and remains the most fatal of all gynaecological cancers [10, 11] particularly due to late presentation of these cancer cases [12, 13] associated with absent effective methods for screening and early diagnosis.
Evaluation of the likelihood of a patient having one of these cancer predisposition syndromes enables physicians to provide individualised assessments of cancer risk, as well as the opportunity to provide tailored screening and prevention strategies such as surveillance, chemoprevention and prophylactic surgery that may reduce the morbidity and mortality associated with these syndromes [14]. This is especially so now that genetic risk assessment is rapidly becoming an expectation in oncology care [15, 16]. A review of service models for provision of genetic healthcare [17] highlighted the effective use of multidisciplinary clinics and services to ensure that patients and families have access to this coordinated care. However as highly proposed and used, BC and OC prevention have not explored this novel opportunity in low- and middle-income countries like Nigeria [18]. There is low awareness of cancer genetics in Nigeria [18] and resources for risk assessment and communication have been lacking. This has led to a growing demand in knowledge for genetic testing (GT) services [19]. The establishment of a cancer risk assessment programme therefore will bridge the knowledge gap about cancer genetics between health professionals and patients [20]. Genetic counseling (GC) and subsequent testing for deleterious gene mutations impacts psychosocial assessment and support, derivation of personalised risks and the likelihood of identifying a mutation with genetic susceptibility testing [14]. This will increase family understanding of testing options and ensure that the most appropriate test is ordered, allowing for informed decision making, and ensuring that families are prepared for the outcomes of testing [21].
Enquiries are made by patients and their relatives on cancer genetic risk assessment through our recent awareness activities on cancer genetics in Nigeria. This led to the emergence of a nurse-led cancer genetic counselling (CGC) and testing. This study aimed to explore the feasibility of GT for risk assessment programme in Nigeria in making CGC and testing standard-of-care for individuals at increased risk of HBOCs by introducing the services to cancer care at the University College Hospital, Ibadan.
Methods
We conducted a pilot study testing the feasibility of integrating systematic cancer risk assessment and GC as a standard and routine component of oncology management at the University College Hospital (UCH) , Ibadan, Nigeria between July and August 2018. Nurses who received a 1 week abridged intensive training in CGC at the UCH, Ibadan in 2014–2015 offered GC to willing patients with BC, OC and endometrial cancer, but without prior genetic counselling and testing (GCT) in four out-patient oncology clinics and departments of the hospital. The nurses’ training was based on the Cancer Genetics and Risk Management training which the lead nurse and the coordinating nurse had received from the University of Iowa, The University of Chicago and the City of Hope, United States of America from 2013 to 2016. Counselling and interview session discussions included educating about genetics of hereditary breast and gynaecological cancers, benefits and risks of GC; documentation of personal and family history with pedigree drawing; determination of cancer mutation risk, GT methods and meaning of results. Consenting patients were, subsequently, tested with 30 cancer susceptibility gene panel in the Color® Genomics kit which include BAP1, MITF, CDK4, CDKN2A, ATM, CDH1, NBN, CHEK2, PTEN, BRCA1, BRCA2, PALB2, BARD1, BRIP1, TP53, STK11, MLH1, MSH2, EPCAM, MSH6, PMS2, RAD51C, RAD51D, APC, BMPR1A, SMAD4, GREM1, MUTYH, POLD1, POLE using targeted sequencing panel. Sequencing was done on an Illumina NextSeq 500/550 instrument for 150 bp paired-end sequencing. The genetic variants were reviewed, discussed and classified as likely pathogenic, or pathogenic and variants of uncertain significance, according to the American College of Medical Genetics and Genomics 2015 guidelines.
After testing, patients completed a semi-standardised questionnaire assessing their socio-demographic information, family cancer history and perceived benefits and barriers to GT. Ethical approval for the study was obtained from the University of Ibadan (UI)/UCH Ethics Committee with the number UI/EC/18/0251. Institutional support was obtained, based on the awareness previously raised on CGC.
Results
Forty-seven women with cancers (BC = 40 (85.1%), OC = 5 (10.0%) and endometrial = 2 (4.3%)) who consented to participate were recruited from the oncology clinics and departments of the selected hospital. The women received GC and subsequently, had GT. The mean age at the time of testing was 48.2 (± 12.1 years; Range: 28–70) years. Family history of cancer was reported by eight (17.0%) of the women (Table 1).
Table 1. Participants’ sociodemographic characteristics N = 47.
| Characteristics | Frequency | % |
|---|---|---|
|
Type of cancer Breast Ovarian Endometrial |
40 5 2 |
85.1 10.6 4.3 |
|
Gender Female |
47 |
100.0 |
|
Marital status Single Married Separated/divorced Widowed |
1 36 3 7 |
2.1 76.5 6.4 14.9 |
|
Religion Christianity Islamic |
35 12 |
74.5 25.5 |
|
Ethnicity Yoruba Ibo Others |
33 9 5 |
70.2 19.1 10.6 |
|
Highest educational qualification Elementary Secondary Diploma /National Certificate of Education B.Sc. M.Sc. Ph.D. |
7 7 13 (27.7) 17 (36.2) 2 (4.3) 1 (2.1) |
14.9 14.9 27.7 36.2 4.3 2.1 |
|
Any family had cancer Yes No |
8 39 |
17.0 83.0 |
| Mean age: 48.2 ± 12.1 years; Range: 28–70 years | ||
| Mean income: N51,542 ± N46,007; ($136 ± 121.07) Range: N2,000–N180,000 (Equivalent to – $474) | ||
Perceived personal risk of cancer recurrence and the lifetime risk of their relatives showed that 42.8% believed that they cannot have cancer again while 17.2% agreed to a risk of 50% and above. A considerable proportion of participants had a view that their children (24.0%), siblings (25.5%) and parents (13.5%) have above 50% risk of developing cancer (Table 2).
Table 2. Participants’ perceived risk of personal and relative cancer risk.
| Perceived lifetime risk of relatives developing cancer (0 is the lowest perceived risk, 10 highest perceived risk) |
Frequency | % |
|---|---|---|
|
Risk of developing cancer again n = 35 0 1 2 3 5 7 8 10 |
15 1 8 5 2 1 2 1 |
42.8 2.9 22.8 14.3 5.7 2.9 5.7 2.9 |
|
Lifetime risk of children n = 25 0 1 2 3 4 5 6 8 |
16 5 5 2 3 2 1 |
4.0 24.0 20.0 20.0 8.0 12.0 8.0 4.0 |
|
Lifetime risk of any siblings n = 43 0 1 2 3 4 5 6 8 9 |
17 5 5 4 1 8 1 1 1 |
39.5 11.6 11.6 9.3 2.3 18.6 2.3 2.3 2.3 |
|
Lifetime risk of any of parents n = 37 0 1 2 3 4 5 6 9 |
18 5 5 2 2 2 1 2 |
48.6 13.5 13.5 5.4 5.4 5.4 2.7 5.4 |
More participants (75.6%) had concerns about their families developing cancer and they identified such as not wanting their relatives to develop cancer like them (67.6%) and desiring that the relatives will know how cancer can be prevented (Table 3). To this effect, most of the participants (93.5%, 91.3% and 93.3%) would like their relatives to have GC, discuss their risks with a specialist and undergo GT, respectively (Table 3).
Table 3. Participants’ concerns about their relatives’ risks of cancer.
| Concerns about relatives’ cancer risk | Frequency | % |
|---|---|---|
|
Do you have concern about other relatives getting cancer n = 45 Yes No |
34 11 |
75.6 24.4 |
|
Concerns n = 34 I don’t want them to develop cancer I will like them to know that cancer can be prevented |
23 11 |
67.6 32.4 |
|
Will you like for your relative to have GC? n = 46 Yes No |
43 3 |
93.5 6.5 |
|
Will you like your relative to discuss their risks with a specialist n = 46 Yes No |
42 4 |
91.3 68.7 |
|
Will you like your relatives to have GT n = 45 Yes No |
42 3 |
93.3 6.7 |
GT for risk assessment was perceived by the participants to be beneficial Top three of their perceived benefits of cancer GCT were, cancer prevention (89.4%), early detection of cancer (70.2%), motivation for self-examination (61.7%). The most mentioned barriers to GC and testing services were cost (80.9%), accessing testing centres (55.3%) and availability of test (38.9%) (Table 4).
Table 4. Participants’ perceived benefits and barriers of GT N = 47.
| Perceived benefits | Frequency | % |
|---|---|---|
| Motivate self-exam | 29 | 61.7 |
| Helps family and children | 25 | 53.2 |
| Reduces concern about cancer | 24 | 51.1 |
| Reduces uncertainty | 20 | 42.5 |
| Provides sense of personal control | 22 | 46.8 |
| Helps plan the future | 27 | 57.4 |
| Helps make important life decisions | 24 | 51.1 |
| Helps with cancer prevention | 42 | 89.4 |
| Early detection of BC | 33 | 70.2 |
| Perceived barriers | ||
| Cultural perception | 11 | 23.4 |
| Cost | 38 | 80.9 |
| Access to the testing centre | 26 | 55.3 |
| Availability of test | 18 | 38.3 |
| Anticipated worry about offspring/relative if result is positive | 13 | 27.7 |
| Anticipated personal emotion if result is positive | 18 | 38.3 |
| Worry that other would find out | 12 | 25.5 |
| Time | 7 | 14.9 |
| Not wanting blood taken | 9 | 19.1 |
| Lack of interest | 9 | 19.1 |
| Worry about increased risk | 10 | 21.3 |
| Worry about discomfort | 7 | 14.9 |
All the participants planned to disclose and discuss their test results with their relatives who were mostly children (Daughters – 72.3%, sons – 68.1%) and siblings (sisters – 74.5%, brothers 55.3%) as shown in Table 5. As all the participants tested for genetic mutations, the result showed about 9.0% pathologic gene mutation which were in BRCA 1, BRCA 2 and ATM, negative result showing no mutations were 34.0% while more than half, 57.0% turned out to be variance of uncertain significance (VUS) (Figure 1). Details of the mutations are as follows: BRCA 1 variant c.5095C>T (p.
Table 5. Relatives that participants would discuss result of GT with.
| Relatives to discuss result with | Frequency | % | |
|---|---|---|---|
| Father | 7 | 14.9 | |
| Mother | 17 | 36.2 | |
| Brother(s) | 26 | 55.3 | |
| Sister(s) | 35 | 74.5 | |
| Daughter(s) | 34 | 72.3 | |
| Son(s) | 32 | 68.1 | |
| Spouse | 18 | 38.3 | |
| Others | Step parents | 1 | 2.1 |
| Aunts | 8 | 17.0 | |
| Uncles | 2 | 4.3 | |
| Cousin(s) | 3 | 6.4 | |
| Daughters-in-law | 1 | 2.1 | |
Figure 1. Results of GT undergone by the participants.
Arg1699Trp) alternate names, g.41215948G>A, BIC: R1699W; BRCA 2 c.7900delA (p.Met2634Trpfs*14) alternate names, g.32936754delA, BIC: 8128delA; ATM variant c.1066-2A>T, alternate name, g.108119658A>T, ATM variant c.72+1G>A alternate name, g.108098424G>A. All mutations are of heterozygous.
Discussion
This study set out to explore the feasibility of an integrated CGC and testing in the care of individuals with cancers and their hereditary cancer at-risk relatives in UCH, Nigeria. With the advent of more targeted and personalised approaches to cancer prevention and treatment, it has become imperative to understand the genetic basis of BC and gynaecological cancer such as OC and endometrial cancer. This is vital in providing patients with the needed effective preventive and/or management strategies towards improvement of outcomes. The causes of hereditary susceptibility to some women cancers have been documented to include hereditary cancer susceptibility genes, BRCA1 or BRCA2, associated with HBOC syndrome [22, 23], DNA mismatch repair genes, MLH1, MSH2, MSH6, or PMS2, in Lynch/Hereditary Non-Polyposis Colorectal Cancer in endometrial, colorectal and OC [24, 25], Cowden syndrome in endometrial and BC [26, 27] and Li-Fraumeni syndrome in BC [28, 29]. In this study, the patients’ personal and relatives’ perceived lifetime cancer risk was explored. The perceived personal risk of developing cancer of 17.2% is a pointer to the fact that the belief system still plays a role in the aetiology of the disease as cancer is generally perceived as a taboo among the people of African descent [30, 31]. This further shows a gap that needs to be filled by providing appropriate cancer genetic risk assessment education and cancer care practice in this era of personalised care. However, 63% concerns the women communicated in the study about their relatives developing cancer is an indication for their ardent need for interventions in the area of CGC and service provision. This has also been shown in studies that positive perceptions of the public towards GT and its beneficial function in the healthcare as a factor in its uptake [32, 33]. This understanding of patients’ perceived risk is salient to the establishment of cancer genetic risk assessment and management services as the risk of a second primary BC in BRCA 1 or 2 mutation carriers, particularly those diagnosed with BC at a younger age, is much higher (upwards of 50%) than in non-carriers [34]. Also, with this knowledge, it is now paramount to identify women who carry mutations which can lead to the utilisation of the targeted medical advances in prevention, early detection and treatment [35, 36].
With the evidence that 5%–10% of BCs and 10%–15% of OCs are hereditary [37], the result of gene testing from this pilot study is not implausible. Moreover, up to 16% germline mutations have been reported in the Nigerian women with BC [9, 38]. The authors believe that with the concerns of the patients about their relatives; possibility of getting cancer, the pooling of multiple generations with BC, OC and other related cancers is possible. Efforts at cancer prevention and early detection have of recent been expanded towards pre-cancer/pre-symptomatic interventions [36]. These can be tailored to individual care given to women at increased risk for hereditary breast and gynaecological cancers.
A positive inclination in the patients’ perceptions on the benefits of cancer genetic assessment services especially to their relatives was also noted. Studies found that members of families with identified BRCA 1 and 2 mutations were more likely to have GT when the genetic test results are shared [39, 40]. In these families, cancer-specific distress and worry play a significant role in the choice to test for BRCA1 mutations as does a greater perceived risk of being a mutation carrier and of developing BC or OC, and the perception that the advantages of BRCA testing outweigh the disadvantages [41]. The family serves as a vital communication nexus for information exchange [42] and may be an avenue for sharing information on cancer risk and prevention strategies. The intention to disclose and discuss the genetic test result to close relatives such as siblings and children is an indication of the assertion in other studies [40, 42].
Cancer risk assessment and associated GT are essential services in cancer risk prevention and are therefore important to be integrated to cancer care. This is, therefore, a right step in the right direction as the findings indicate its feasibility. This is crucial for a greater degree of personalised and yet comprehensive cancer care including GT for cancer risk assessment programme in Nigeria.
Limitation of the study
There is need for more data on a larger population for increased level of generalisation. Color Genomics® is the only laboratory engaged in this study which although have variants tested for African American population, is being engaged for the first time in the Nigerian population.
However, multi gene panels including Color Genomics® 30 gene panel have been used extensively among African Americans. This advancement in sequencing panels for hereditary BC, OC and prostate cancer has shown that people of African descent tend to have more rare multiple variants and VUS than Caucasians [43, 44]. Also, Color Genomics® 30 gene panel has been used among Africans in Uganda and Cameroon [7]; therefore, this study relies on the result to provide population relevant data.
Conclusion
Cancer GC and testing are perceived by patients in this study as beneficial for providing risk assessment for personalised patient care, early detection and prevention in women with high BC’s and gynaecological cancers’ risk. These results are important as GC and testing are expected to be offered to newly diagnosed BC, OC and endometrial cancer patients with increasing frequency in order to inform these women and their relatives about the possibility of a familial/hereditary nature of their disease to influence both their treatment and prevention for their family members. Proper education of the patients and their relatives on cancer genetic risk management will facilitate the required attention for maximal utilisation of cancer genetic services.
Authors’ disclosures of potential conflicts of interest
Olufunmilayo I Olopade is an equity stock holder of CancerIQ. The other authors declare no conflicts of interest.
Funding declaration
This project was supported by National Institutes of Health grants from Susan G. Komen for the Cure (OIO) and Breast Cancer Research Foundation (OIO) the Color Genomics® Foundation.
References
- 1.Rahner N, Steinke V. Hereditary cancer syndromes. Dtsch Arztebl Int. 2008;105(41):706–714. doi: 10.3238/arztebl.2008.0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsaousi GN, Papadopoulou E, Apessos A, et al. Analysis of hereditary cancer syndromes by using a panel of genes: novel and multiple pathogenic mutations. BMC Cancer. 2019;19:535. doi: 10.1186/s12885-019-5756-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Somasundaram K. BRCA1 and BRCA1 genes and inherited breast and/or ovarian cancer: benefits of genetic testing. Indian J Surg Oncol. 2010;1(3):245–249. doi: 10.1007/s13193-011-0049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenthal E, Moyes K, Arnell C, et al. Incidence of BRCA1 and BRCA2 non-founder mutations in patients of Ashkenazi Jewish ancestry. Breast Cancer Res Treat. 2015;149(1):223–227. doi: 10.1007/s10549-014-3218-x. [DOI] [PubMed] [Google Scholar]
- 5.Palmer JR, Hart S, et al. Recurrent BRCA1 and BRCA2 mutations in breast cancer patients of African ancestry. Breast Cancer Res Treat. 2012;134(2):889–894. doi: 10.1007/s10549-012-2136-z. [DOI] [PubMed] [Google Scholar]
- 6.Cherbal F, Bakour R, Adane S, et al. BRCA1 and BRCA2 germline mutations screening in Algerian breast/ovarian cancer families. Dis Markers. 2010;28(6):377–384. doi: 10.1155/2010/585278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adedokun B, Zheng Y, Ndom P, et al. Prevalence of inherited mutations in breast cancer predisposition genes among Uganda and Cameroon women. Cancer Epidemiol Biomarkers Prev. 2019;29(2):359–367. doi: 10.1158/1055-9965.EPI-19-0506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang J, Fackenthal J, King MC, et al. Inherited predisposition to breast cancer among African American women breast cancer. Res Treat. 2015;149(1):31–9. doi: 10.1007/s10549-014-3195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng Y, Walsh T, Gulsuner S, et al. Inherited breast cancer in Nigerian women. J Clin Oncol. 2018;36(28):2820–2825. doi: 10.1200/JCO.2018.78.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torre LA, Trabert B, DeSantis CE, et al. Ovarian cancer statistics 2018. CA Cancer J Clin. 2018;68(4):284–296. doi: 10.3322/caac.21456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 12.Torre LA, Islami F, Siegel RL, et al. Global cancer in women: burden and trends. Cancer Epidemiol Biomarkers Prev. 2017;26(4):444–457. doi: 10.1158/1055-9965.EPI-16-0858. [DOI] [PubMed] [Google Scholar]
- 13.Rivera-Franco MM, Leon-Rodriguez E. Delays in breast cancer detection and treatment in developing countries. Breast Cancer Basic Clin Res. 2018;12:1178223417752677. doi: 10.1177/1178223417752677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nelson HD, Pappas M, Zakher B, et al. Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: a systematic review to update the U.S. preventive services task force recommendation. Ann Intern Med. 2014;160(4):255–266. doi: 10.7326/M13-1684. [DOI] [PubMed] [Google Scholar]
- 15.Chan IS, Ginsburg GS. Personalized medicine: progress and promise. Annu Rev Genomics Hum Genet. 2011;12:217–244. doi: 10.1146/annurev-genom-082410-101446. [DOI] [PubMed] [Google Scholar]
- 16.Lopez V. Genetic testing: do cancer care nurses have a role? Asia-Pac J Oncol Nurs. 2018;5(4):391–393. doi: 10.4103/apjon.apjon_23_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Battista RN, Blancquaert I, Laberge AM, et al. Genetics in health care: an overview of current and emerging models. Public Health Genomics. 2012;15:34–45. doi: 10.1159/000328846. [DOI] [PubMed] [Google Scholar]
- 18.Adejumo PO, Aniagwu TI, Oluwatosin OA, et al. Knowledge of genetic counselling among patients with breast cancer and their relatives at a Nigerian teaching hospital. J Glob Oncol. 2018;4:1–8. doi: 10.1200/JGO.17.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen SA, Bradbury A, Henderson V, et al. Genetic counseling and testing in a community setting: quality, access, and efficiency. Am Soc Clin Oncol Educ Book. 2019;39:e34–e44. doi: 10.1200/EDBK_238937. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald DJ, Blazer KR, Weitzel JN. Extending comprehensive cancer center expertise in clinical cancer genetics and genomics to diverse communities: the power of partnership. J Natl Compr Cancer Netw. 2010;8(5):615–624. doi: 10.6004/jnccn.2010.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Druker H, Zelley K, McGee RB, et al. Genetic counselor recommendations for cancer predisposition evaluation and surveillance in the pediatric oncology patient. Clin Cancer Res. 2017;23(13):e91–e97. doi: 10.1158/1078-0432.CCR-17-0834. [DOI] [PubMed] [Google Scholar]
- 22.Kobayashi H, Ohno S, Sasaki Y, et al. Hereditary breast and ovarian cancer susceptibility genes. Oncolo Rep. 2013;30:1019–1029. doi: 10.3892/or.2013.2541. [DOI] [PubMed] [Google Scholar]
- 23.Saam J, Moyes K, Landon M, et al. Hereditary cancer-associated mutations in women diagnosed with two primary cancers: an opportunity to identify hereditary cancer syndromes after the first cancer diagnosis. Oncol. 2015;88:226–233. doi: 10.1159/000368836. [DOI] [PubMed] [Google Scholar]
- 24.Banno K, Kisu I, Yanokura M, et al. Hereditary endometrial cancer: Lynch syndrome. Curr Obstet Gynecol Rep. 2013;2:11–18. doi: 10.1007/s13669-012-0029-0. [DOI] [Google Scholar]
- 25.Nakamura K, Banno K, Yanokura M, et al. Features of ovarian cancer in Lynch syndrome. Mol Clin Oncol. 2014;2:909–916. doi: 10.3892/mco.2014.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gammon A, Jasperson K, Champine M. Genetic basis of Cowden syndrome and its implications for clinical practice and risk management. Appl Clin Genet. 2016;9:83–92. doi: 10.2147/TACG.S41947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minamiguchi K, Takahama J, Uchiyama T, et al. Uterine endometrial carcinoma with DNA mismatch repair deficiency: magnetic resonance imaging findings and clinical features. Jpn J Radiol. 2018;36:429–436. doi: 10.1007/s11604-018-0741-4. [DOI] [PubMed] [Google Scholar]
- 28.Neto N, Cunha TM. Do hereditary syndrome-related gynecologic cancers have any specific features? Insights Imaging. 2015;6(5):545–552. doi: 10.1007/s13244-015-0425-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Penkert J, Schmidt G, Hofmann W, et al. Breast cancer patients suggestive of Li-Fraumeni syndrome: mutational spectrum, candidate genes, and unexplained heredity. Breast Cancer Res. 2018;20:87. doi: 10.1186/s13058-018-1011-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ehiwe E, McGee P, Thomson K, et al. How black West African migrants perceive cancer. Divers Equal Health Care. 2013;10:115–21. [Google Scholar]
- 31.Tetteh DA, Faulkner SL. Sociocultural factors and breast cancer in sub-Saharan Africa: implications for diagnosis and management. Women's health (Lond) 2016;12(1):147–156. doi: 10.2217/whe.15.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haga SB, Barry WT, Mills R, et al. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomarkers. 2013;17(4):327–35. doi: 10.1089/gtmb.2012.0350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Etchegar H. Public attitudes toward genetic risk testing and its role in healthcare. Personalized Med. 2014;11(5):509–22. doi: 10.2217/pme.14.35. [DOI] [PubMed] [Google Scholar]
- 34.Pal T, Vadaparampil ST. Genetic risk assessments in individuals at high risk for inherited breast cancer in the breast oncology care setting. Cancer Control. 2012;19(4):255–266. doi: 10.1177/107327481201900402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olopade OI, Grushko T, Nanda R, et al. Advances in breast cancer: pathways to personalized medicine. Clin Cancer Res. 2008;14(24):7988–7999. doi: 10.1158/1078-0432.CCR-08-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loomans-Kropp HA, Umar A. Cancer prevention and screening: the next step in the era of precision medicine. Npj Precis Oncol. 2019;3:3. doi: 10.1038/s41698-018-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lynch JA, Berse VVB. Genetic tests to identify risk for breast cancer. Semin Oncol Nurs. 2015;31(2):100–107. doi: 10.1016/j.soncn.2015.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fackenthal JD, Zhang J, Zhang B, et al. High prevalence of BRCA1 and BRCA2 mutations in unselected Nigerian breast cancer patients. Int J Cancer. 2012;131(5):1114–1123. doi: 10.1002/ijc.27326. [DOI] [PubMed] [Google Scholar]
- 39.Biesecker BB, Ishibe N, Hadley DW, et al. Psychosocial factors predicting BRCA1/BRCA2 testing decisions in members of hereditary breast and ovarian cancer families. Am J Med Genet. 2000;93(4):257–63. doi: 10.1002/1096-8628(20000814)93:4<257::AID-AJMG1>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 40.Vadaparampil ST, Malo T, Cruz C, et al. Do breast cancer patients tested in the oncology care setting share BRCA mutation results with family members and health care providers? J Cancer Epidemiol. 2012;2012:10. doi: 10.1155/2012/498062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schlich-Bakker K, Kroode H, Wárlám-Rodenhuis C, et al. Barriers to participating in genetic counseling and BRCA testing during primary treatment for breast cancer. Genet Med. 2007;9:766–777. doi: 10.1097/GIM.0b013e318159a318. [DOI] [PubMed] [Google Scholar]
- 42.Chopra I, Kelly KM. Cancer risk information sharing: the experience of individuals receiving genetic counseling for BRCA1/2 mutations. J Health Commun. 2017;22(2):143–152. doi: 10.1080/10810730.2016.1258743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Neben CL, Zimmer AD, Stedden W, et al. Multi-Gene panel testing of 23,179 individuals for hereditary cancer risk identifies pathogenic variant carriers missed by current genetic testing guidelines. J Mol Diagn. 2019;21(4):646–657. doi: 10.1016/j.jmoldx.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Bishop MR, Omeler-Fenaud SM, Huskey ALW, et al. Gene panel screening for insight towards breast cancer susceptibility in different ethnicities. PLoS One. 2020;15(8):e0238295. doi: 10.1371/journal.pone.0238295. [DOI] [PMC free article] [PubMed] [Google Scholar]