Hematologic malignancy patients have intrinsic deficits in humoral immunity that are further compounded by cancer-directed therapies, resulting in attenuated antibody responses to COVID-19 vaccination.
Abstract
Coronavirus disease-19 (COVID-19) vaccine response data for patients with hematologic malignancy, who carry high risk for severe COVID-19 illness, are incomplete. In a study of 551 hematologic malignancy patients with leukemia, lymphoma, and multiple myeloma, anti–SARS-CoV-2 spike IgG titers and neutralizing activity were measured at 1 and 3 months from initial vaccination. Compared with healthy controls, patients with hematologic malignancy had attenuated antibody titers at 1 and 3 months. Furthermore, patients with hematologic malignancy had markedly diminished neutralizing capacity of 26.3% at 1 month and 43.6% at 3 months, despite positive seroconversion rates of 51.5% and 68.9% at the respective time points. Healthy controls had 93.2% and 100% neutralizing capacity at 1 and 3 months, respectively. Patients with leukemia, lymphoma, and multiple myeloma on observation had uniformly blunted responses. Treatment with Bruton tyrosine kinase inhibitors, venetoclax, phosphoinositide 3-kinase inhibitors, anti-CD19/CD20–directed therapies, and anti-CD38/B-cell maturation antigen–directed therapies substantially hindered responses, but single-agent immunomodulatory agents did not.
Significance:
Patients with hematologic malignancy have compromised COVID-19 vaccine responses at baseline that are further suppressed by active therapy, with many patients having insufficient neutralizing capacity despite positive antibody titers. Refining vaccine response parameters is critical to guiding clinical care, including the indication for booster vaccines, for this vulnerable population.
See related article by Tamari et al., p. 577.
This article is highlighted in the In This Issue feature, p. 549
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for coronavirus disease-19 (COVID-19), causes respiratory illness ranging from self-limited, mild respiratory tract symptoms to severe pneumonia with acute respiratory distress syndrome, multiorgan failure, and death. Due to their disease and/or associated treatments, patients with cancer are often immunocompromised and at increased risk of severe COVID-19 illness (1,2,3), with fatality rates far exceeding that of the general population (4). Within the cancer population, patients with hematologic malignancy are at greatest risk for COVID-19–related mortality (2,3,5,6,7,8,9,10).
The adverse outcomes of patients with hematologic malignancy to COVID-19 infection stem at least in part from intrinsic immune dysfunction. Patients with indolent B-cell malignancies, including chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and follicular lymphoma, have a high incidence of hypogammaglobulinemia, as well as T-cell dysfunction, which impairs long-term antiviral humoral immunity and response to vaccination (11). Patients with multiple myeloma have compromised humoral and cellular immunity from their plasma cell disorder, its associated hypogammaglobulinemia, and immunosuppression exacerbated by anti–multiple myeloma therapies (12). Patients with myeloid malignancies, including acute myeloid leukemia and high-risk myelodysplastic syndromes, have impaired innate immunity, antigen presentation, and quantitative defects in all immune cells, often at baseline before starting treatment and further exacerbated by therapies, including hematopoietic stem cell transplantation (13, 14).
Given their greater susceptibility to severe COVID-19 illness, patients with hematologic malignancy are a high-priority group for vaccination to mitigate COVID-19–related morbidity and mortality. Effective vaccination would enable receipt of disease-specific therapy and avoid delays in cancer care. There are limited comprehensive data on the efficacy of COVID-19 vaccines in patients with cancer, with many COVID-19 vaccine studies excluding patients with cancer and real-world outcomes for patients with cancer only recently starting to emerge. In this study, we aimed to define how vaccine humoral responses differ by hematologic malignancy subtype and disease-specific therapies across patient cohorts to provide an important metric for optimizing the clinical care of this vulnerable population.
Results
Patient Characteristics
As of August 1, 2021, the study included 551 patients with leukemia (n = 157), lymphoma (n = 173), and multiple myeloma (n = 221), as well as a healthy volunteer control cohort (n = 69; Supplementary Fig. S1—study schema). Supplementary Table S1 lists patient demographics and disease subtypes. Median age was 65 (range, 22–97), with male predominance (56.3%). The most common disease subtypes were symptomatic multiple myeloma (n = 211), CLL/SLL (n = 120), diffuse large B-cell lymphoma (n = 55), follicular lymphoma (n = 42), marginal zone lymphoma (n = 24), Hodgkin lymphoma (n = 14), and mantle cell lymphoma (n = 13). Most patients (75.5%) were on cancer therapy (i.e., treatment received within 6 months of initial COVID-19 vaccination). All patients received two doses of the mRNA-based vaccines, either BNT162b2 (75%) or mRNA-1273 (25%; Table 1). For the healthy controls, the median age was 31 (range, 22–67), with female predominance (78.3%; Supplementary Table S1). All healthy controls also received two doses of the mRNA-based vaccines, BNT162b2 (84.1%) or mRNA-1273 (15.9%; Table 1).
Table 1.
Vaccine responses
| Healthy control | Leukemia | Lymphoma | Multiple myeloma | All patients | ||
|---|---|---|---|---|---|---|
| Total individuals | 69 | 157 | 173 | 221 | 551 | |
| Vaccine subtype | BNT162b2 | 58 (84.1%) | 105 | 136 | 172 | 413 (75%) |
| mRNA-1273 | 11 (15.9%) | 52 | 37 | 49 | 138 (25%) | |
| SARS-CoV-2 spike IgG antibody response: Prior COVID-19 illness | 1 mo seropositive rate | 8/9 (88.9%) | 1/1 (100%) | 5/5 (100%) | 6/6 (100%) | 12/12 (100%) |
| 1 mo Ab titer (AU/mL): mean ± SD | 16,881 ± 8,302 | 719.9 ± 0 | 13,748 ± 11,792 | 21,881 ± 4,984 | 16,729 ± 10,182 | |
| 1 mo Ab titer (AU/mL): median (IQR) | 16,850 (12,763–24,672) | 719.9 (719.9–719.9) | 15,536 (1,602–25,000) | 25,000 (16,607–25,000) | 21,286 (5,787–25,000) | |
| 3 mo seropositive rate | 9/9 (100%) | 5/7 (71.4%) | 10/10 (100%) | 10/11 (90.9%) | 25/28 (89.3%) | |
| 3 mo Ab titer (AU/mL): mean ± SD | 17,737 ± 6,327 | 14,617 ± 12,973 | 19,003 ± 9,006 | 17,817 ± 8,492 | 17,441 ± 9,704 | |
| 3 mo Ab titer (AU/mL): median (IQR) | 16,748 (11,566–25,000) | 25,000 (4.9–25,000) | 24,798 (12,669–25,000) | 21,749 (11,244–25,000) | 24,798 (10,604–25,000) | |
| SARS-CoV-2 spike IgG antibody response: No prior COVID-19 illness | 1 mo seropositive rate | 59/59 (100%) | 10/34 (29.4%) | 18/38 (47.4%) | 58/95 (61.1%) | 86/167 (51.5%) |
| 1 mo Ab titer (AU/mL): mean ± SD | 2,620 ± 5,104 | 1,137 ± 4,598 | 1,481 ± 4,015 | 1,716 ± 4,889 | 1,545 ± 4,624 | |
| 1 mo Ab titer (AU/mL): median (IQR) | 886.2 (502.3–2,240) | 4.5 (1.8–86.33) | 46 (4.9–329.9) | 96.6 (8.3–571.4) | 55.7 (4–465.7) | |
| 3 mo seropositive rate | 54/54 (100%) | 73/131 (55.7%) | 74/132 (56.1%) | 167/193 (86.5%) | 314/456 (68.9%) | |
| 3 mo Ab titer (AU/mL): mean ± SD | 7,656 ± 4,701 | 3,827 ± 7,217 | 4,241 ± 7,752 | 4,176 ± 6,775 | 4,095 ± 7,182 | |
| 3 mo Ab titer (AU/mL): median (IQR) | 7,720 (3,885–9,746) | 187 (5–3,632) | 127 (6.5–3,592) | 1,218 (180.4–4,424) | 517.7 (18.2–3,779) |
| Healthy control | Patients with hematologic malignancies | |||||
|---|---|---|---|---|---|---|
| Neutralizing antibody | 1 mo positive inhibition | 55/59 (93.2%) | 21/80 (26.3%) | |||
| 1 mo: mean % inhibition ± SD | 62.8 ± 20.3 | 22.8 ± 26.3 | ||||
| 1 mo: median % inhibition (IQR) | 63.6 (51.3–78.4) | 11.3 (4.9–30.6) | ||||
| 3 mo positive inhibition | 21/21 (100%) | 17/39 (43.6%) | ||||
| 3 mo: mean % inhibition ± SD | 94 ± 4.2 | 36 ± 40.4 | ||||
| 3 mo: median % inhibition (IQR) | 95.6 (93.8–95.9) | 9.3 (1–86.7) | ||||
Abbreviations: Ab, antibody; AU/mL, artificial units/milliliter; IQR, interquartile range; mo, month; SD, standard deviation.
Quantitative Antibody Response to Vaccination
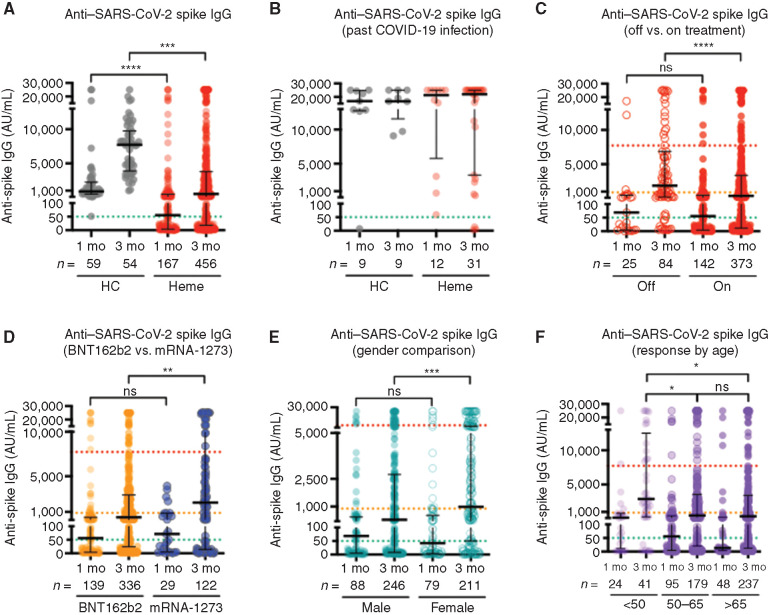
Quantification of anti–SARS-CoV-2 antibody titers to assess humoral response after vaccination was determined using a chemiluminescent enzyme immunoassay at 1 and 3 months from initial vaccine (NB: “1 month” time point = 3 weeks from the first BNT162b2 vaccine and 4 weeks from the first mRNA-1273 vaccine). Individuals with a history of COVID-19 infection before vaccination were analyzed separately because of the likelihood of mounting extreme responses that would obscure the interpretation of the responses of those without prior infection. Based on a cutoff value of 50.0 AU/mL as the threshold for a positive result, postvaccination seroconversion rates and median antibody titers for patients with hematologic malignancy were 51.5% and 55.7 AU/mL [interquartile range (IQR) 4–465.7] at 1 month (n = 167) and 68.9% and 517.7 AU/mL (IQR 18.2–3,779) at 3 months (n = 456), with patients with multiple myeloma possessing the highest conversion rates of 61.1% and 86.5% at 1 and 3 months, respectively (Table 1). For most individuals, antibody titers peaked at 3 months (Supplementary Fig. S2), but when compared with healthy controls, patients with hematologic malignancy had markedly lower seroconversion rates and degree of response at both time points (Fig. 1A and Table 1). Patients and healthy controls with previous COVID-19 infection had robust responses, with notable exceptions of three patients on treatment with a Bruton tyrosine kinase (BTK) inhibitor (n = 1), venetoclax (n = 1), and belantamab mafodotin (n = 1; Fig. 1B and Table 1). Patients on active treatment had reduced responses at 3 months compared with patients on observation (Fig. 1C). Although seropositivity rates after two vaccine doses were similar for BNT162b2 (70.3%) and mRNA-1273 (67.7%), median antibody titer at 3 months was 389.2 AU/mL (IQR 24–2,896) for BNT162b2 (n = 336) and 2,042 AU/mL (IQR 14.3–10,632) for mRNA-1273 (n = 122; Fig. 1D). Female patients developed higher antibody titers than male patients, with median antibody titer at 3 months of 981.8 AU/mL (IQR 50–6,573) for women (n = 211) and 276.7 AU/mL (IQR 7.98–2,737) for men (n = 246; Fig. 1E). Younger patients generated higher antibody titers than older patients. Specifically, for patients age <50, median antibody titers were 147.2 AU/mL (IQR 10.3–787) at 1 month (n = 24) and 2,902 AU/mL (IQR 287–12,499) at 3 months (n = 41), compared with patients age 50 to 65, with median antibody titers 55.9 AU/mL (IQR 4.3–439.6) at 1 month (n = 95) and 496.1 AU/mL (IQR 20.9–3,553) at 3 months (n = 179) and patients age >65, with median antibody titers 12.6 AU/mL (IQR 3.2–186.7) at 1 month (n = 48) and 373.5 AU/mL (IQR 12.7–3,423) at 3 months (n = 237; Fig. 1F).
Figure 1.
Quantitative antibody responses to COVID-19 vaccines. Anti–SARS-CoV-2 spike IgG antibody titers were measured at 1 and 3 months after initial COVID-19 vaccination and summarized using scatter plots with median and interquartile range. Note: “1 month” time point = 3 weeks from the first BNT162b2 vaccine and 4 weeks from the first mRNA-1273 vaccine. mo, month. A, Patients with hematologic malignancy (Heme; red dots) compared with healthy controls (HC; gray dots), excluding those with previous COVID infection. B, Heme and HC with history of COVID-19 infection. C, Heme off (open circles) and on (filled red circles) cancer treatment. D, Heme responses after receiving BNT162b2 (orange circles) and mRNA-1273 (blue circles). E, Heme responses by gender (male = filled teal circles; female = open teal circles). F, Heme responses by age. For all plots, green dashed line denotes the threshold for a positive result (50.0 AU/mL), orange dashed line denotes the median value at 1 month for HC (886 AU/mL), and red dashed line denotes the median value at 3 months for HC (7,720 AU/mL). *, P < 0.05; **, P < 0.01; ***, P < 0.001; ****, P < 0.0001; ns = not significant. n = number of individuals per category.
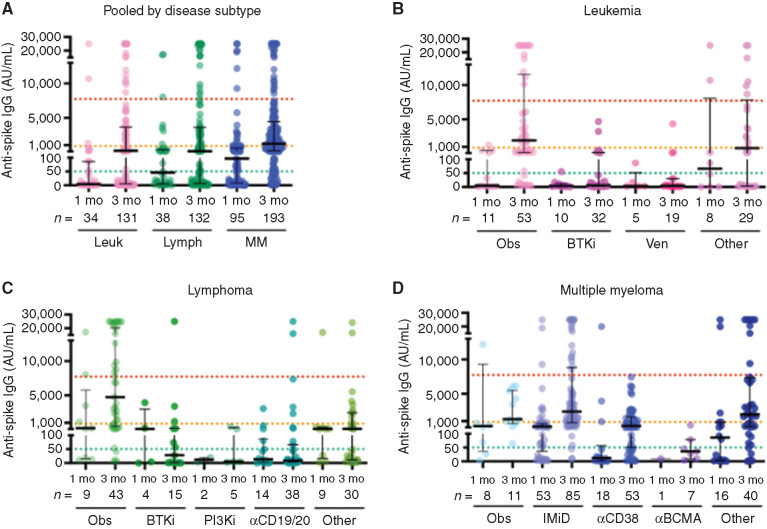
To account for the biological and treatment heterogeneity of the different hematologic malignancies, antibody responses were assessed by disease subcategory (Fig. 2A). Figure 2B and Table 1 summarize leukemia patient responses, including the following categories: (i) observation: median antibody titer 5.3 AU/mL (IQR 2–465.7) at 1 month (n = 11) and 1,945 AU/mL (IQR 176.2–11,556) at 3 months (n = 53); (ii) BTK inhibitors: median antibody titer 3.5 AU/mL (IQR 0.7–12.9) at 1 month (n = 10) and 6.2 AU/mL (IQR 3–189) at 3 months (n = 32); and (iii) venetoclax: median antibody titer 2.9 AU/mL (IQR 2.6–51.5) at 1 month (n = 5) and 4.3 AU/mL (IQR 1.4–29.5) at 3 months (n = 19). As expected from underlying disease pathology and B-cell–directed therapies, patients with CLL/SLL, who constituted 76.4% of patients in the leukemia cohort, had extremely blunted responses at 3 months with median antibody titer 20.5 AU/mL (IQR 3.6–1,863; n = 105) compared with myeloid leukemia patient responses with median antibody titer 2,555 AU/mL (IQR 214.3–5,843; n = 23; Supplementary Fig. S3). Figure 2C and Table 1 summarize lymphoma patient responses, including the following categories: (i) observation: median antibody titer 219 AU/mL (IQR 15.9–5,763) at 1 month (n = 9) and 4,743 AU/mL (IQR 496.1–20,251) at 3 months (n = 43); (ii) BTK inhibitors: median antibody titer 105.3 AU/mL (IQR 1.1–2,997) at 1 month (n = 4) and 28 AU/mL (IQR 1.5–172.1) at 3 months (n = 15); (iii) phosphoinositide 3-kinase (PI3K) inhibitors: median antibody titer 11.7 AU/mL (IQR 3.6–19.8) at 1 month (n = 2) and 5 AU/mL (IQR 3.5–286.9) at 3 months (n = 5); and (iv) anti-CD19/anti-CD20–directed therapies: median antibody titer 13.6 AU/mL (IQR 1.4–87.6) at 1 month (n = 14) and 8.4 AU/mL (IQR 3.7–66.8) at 3 months (n = 38). Figure 2D and Table 1 summarize multiple myeloma patient responses, including the following categories: (i) observation: median antibody titer 282.2 AU/mL (IQR 36.8–9,305) at 1 month (n = 8) and 1,298 AU/mL (IQR 664.3–5,459) at 3 months (n = 11); (ii) immunomodulatory agents: median antibody titer 198.8 AU/mL (IQR 36.85–624.5) at 1 month (n = 53) and 2,397 AU/mL (IQR 798.1–8,816) at 3 months (n = 85); (iii) anti-CD38–directed therapies: median antibody titer 12.3 AU/mL (IQR 1.7–56.7) at 1 month (n = 18) and 318 AU/mL (IQR 50.1–1,594) at 3 months (n = 53); and (iv) anti–B-cell maturation antigen (BCMA)–directed therapies: median antibody titer 9.6 AU/mL (IQR 9.6–9.6) at 1 month (n = 1) and 36.4 AU/mL (IQR 9.4–78.7) at 3 months (n = 7). Overall, patients with lymphoma on observation, the group with the largest fraction of patients in remission, had the highest median antibody response at 3 months. Patients on BTK inhibitors, venetoclax, PI3K inhibitors, anti-CD19/CD20–directed therapies, and anti-CD38/BCMA–directed therapies had markedly attenuated seroconversion rates and absolute antibody titers. In contrast, patients with multiple myeloma on maintenance therapy with immunomodulatory agents (lenalidomide or pomalidomide) had relatively intact responses, with median antibody titers at 3 months approaching that of patients with lymphoma on observation.
Figure 2.
Disease-specific antibody responses to COVID-19 vaccines. Anti–SARS-CoV-2 spike IgG antibody titers measured at 1 and 3 months after initial COVID-19 vaccination grouped by disease subtype and summarized using scatter plots with median and interquartile range. Note: “1 month” time point = 3 weeks from the first BNT162b2 vaccine and 4 weeks from the first mRNA-1273 vaccine. A, Patients with leukemia (Leuk), lymphoma (Lymph), and multiple myeloma (MM). mo, month. B, Patients with leukemia on observation (Obs) and patients receiving BTK inhibitors (BTKi), venetoclax (ven), and other therapies. C, Patients with lymphoma on Obs and patients receiving BTKi, phosphoinositide 3-kinase (PI3K) inhibitors, anti-CD19/CD20–directed therapies (αCD19/20), and other therapies. D, Patients with multiple myeloma on Obs and patients receiving immunomodulatory agents (IMiD), anti-CD38–directed therapy (αCD38), anti–B-cell maturation antigen-directed therapies (αBCMA), and other therapies. For all plots, green dashed line denotes the threshold for a positive result (50.0 AU/mL), orange dashed line denotes the median value at 1 month for healthy controls (886 AU/mL), and red dashed line denotes the median value at 3 months for healthy controls (7,720 AU/mL). n = number of individuals per category.
Qualitative Antibody Response to Vaccination
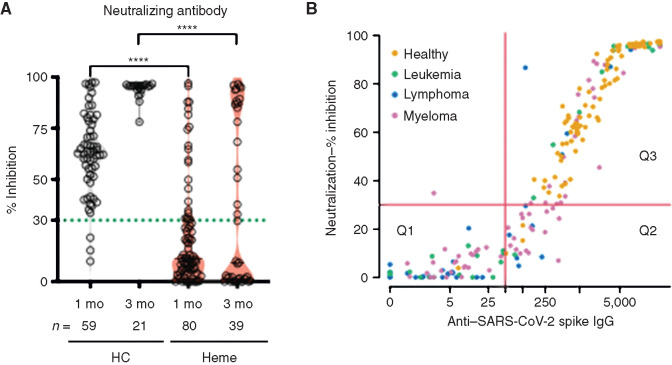
Because neutralizing antibody levels against SARS-CoV-2 are predictive of protection from symptomatic COVID-19 (15), we analyzed available samples for neutralizing activity at 1 and 3 months from initial vaccine, with at least 30% inhibition required as a positive result per assay standardization against a plaque-reduction neutralization test. For patients with hematologic malignancy, the percentage of individuals with positive neutralizing activity and the median percentage inhibition were 26.3% and 11.3% (IQR 4.9–30.6) at 1 month (n = 80) and 43.6% and 9.3% (IQR 1–86.7) at 3 months (n = 39; Fig. 3A; Table 1). Furthermore, median percentage inhibition at both 1 and 3 months was lowest for patients with leukemia, all of whom had CLL/SLL, and highest for patients with multiple myeloma, the majority of whom were on lenalidomide maintenance therapy (Supplementary Fig. S4). In contrast, the percentage of healthy controls with positive neutralizing activity and the median percentage inhibition were 93.2% and 63.6% (IQR 51.3–78.4) at 1 month (n = 59) and 100% and 95.6% (IQR 93.8–95.9) at 3 months (n = 21; Fig. 3A and Table 1).
Figure 3.
Neutralizing antibody levels after COVID-19 vaccines. Circulating neutralizing antibodies against SARS-CoV-2 were assessed at 1 and 3 months after initial COVID-19 vaccination. Note: “1 month” time point = 3 weeks from the first BNT162b2 vaccine and 4 weeks from the first mRNA-1273 vaccine. A, Violin plots comparing patients with hematologic malignancy (Heme; red fill) with healthy controls (HC; gray fill). Green dashed line denotes the threshold for a positive result (30% inhibition). ****, P < 0.0001. mo, month; n = number of individuals per category. B, Scatter plot of anti–SARS-CoV-2 spike IgG antibody titers and neutralizing antibodies assessed at 1 and 3 months after initial COVID-19 vaccination. Red horizontal line denotes threshold for the positive neutralizing result (30% inhibition). Red vertical line denotes threshold for the positive antibody result (50.0 AU/mL). Q1 = negative antibody titer and negative neutralizing activity. Q2 = positive antibody titer and negative neutralizing activity. Q3 = positive antibody titer and positive neutralizing activity.
Figure 3B shows the correlation between anti–SARS-CoV-2 antibody titers and neutralizing activity, demarcating responses into quadrants based on test results. For individuals (patients and healthy controls) with negative antibody titers and negative neutralizing activity (n = 60; group Q1 in Fig. 3B), the median antibody titer was 5.4 AU/mL (IQR 1.8–12) with median percentage inhibition 2.2% (IQR 0–6.5). For individuals with positive antibody titers but negative neutralizing activity (n = 27; group Q2 in Fig. 3B), the median antibody titer was 101.7 AU/mL (IQR 78–150.4) with median percentage inhibition 17.5% (IQR 9.9–24.3). For individuals with positive antibody titers and positive neutralizing activity (n = 44; group Q3 in Fig. 3B), the median antibody titer was 1,891 AU/mL (IQR 557.2–8,733) with median percentage inhibition 84.9% (IQR 51.8–95.2). Overall, every individual with an antibody titer of at least 500 AU/mL (n = 113) had positive neutralizing activity with median percentage inhibition 87.9% (IQR 65.4–95.9), whereas only 1 of 61 individuals with an antibody titer <50 AU/mL had positive neutralizing activity. For individuals with positive antibody titers but negative neutralizing activity after one vaccine (n = 23; group Q2 in Fig. 3B), the median antibody titer after receiving a second vaccine increased to 2,121 AU/mL (IQR 991.4–4,680), an antibody level with a high likelihood of adequate neutralizing capacity (i.e., antibody titer ≥500). In contrast, for individuals with negative antibody titers and negative neutralizing activity after one vaccine (n = 45; group Q1 in Fig. 3B), the median antibody titer after receiving a second vaccine increased incrementally to 15.7 AU/mL (IQR 2.1–345.6), an antibody level with low likelihood of adequate neutralizing capacity (i.e., antibody titer <50). Of the patients in the Q1 subgroup who failed to mount positive antibody titers after receiving a second vaccine (n = 29; Fig. 3B), perivaccine treatments included anti-CD19/CD20–directed therapies (n = 11), PI3K inhibitors (n = 5), anti-CD38–directed therapy (n = 4), BTK inhibitors (n = 3), anti-BCMA–directed therapies (n = 2), venetoclax (n = 2), lenalidomide (n = 1), and prednisone (n = 1).
Discussion
Hematologic malignancies are biologically heterogeneous with a spectrum of inherent immune impairment that is further exacerbated by disease-directed therapies. Understanding the impact of hematologic malignancy subtype and treatments on immune responses to COVID-19 vaccines is essential for optimizing vaccination strategies for this vulnerable population. To address this vital issue, we show that patients with hematologic malignancy have compromised COVID-19 vaccine humoral responses at baseline that are further suppressed in the setting of active therapy and, importantly, that antibody titers alone are an imperfect measure of immunity, as many patients with positive anti–SARS-CoV-2 antibody titers have insufficient neutralizing capacity.
A growing series of studies from multiple groups using various testing methods have reported blunted COVID-19 vaccine responses in patients with cancer, including those with hematologic malignancies (16,17,18,19,20,21,22). In addition to confirming impaired humoral capacity of patients receiving B-cell–directed treatments targeting CD20, CD38, and BCMA, as well as BTK inhibitors, our results show impaired responses in the setting of PI3K inhibitors and venetoclax. Further illustrating the profound dampening effect of therapy on vaccine responses was a subset of patients in our study with past COVID-19 infection who failed to mount robust responses after two vaccine doses, contrasting with the amplified antibody titers expected after a single vaccine dose in healthy individuals with prior COVID-19 infection (23). Our findings also highlight preserved humoral responses for patients with multiple myeloma on maintenance therapy with immunomodulatory agents. Insights into the underlying mechanisms of therapies that diminish or enhance responses to COVID-19 vaccines will aid the future development and refinement of vaccination and/or therapeutic strategies to control the current and future pandemics.
Consistent with other reports, our findings emphasize the importance of a two-dose approach when administering mRNA-based vaccines for patients with hematologic malignancy due to the extremely low response rates and absolute antibody titers after a single vaccine. Interestingly, at 3 months after receiving two vaccine doses, hematologic malignancy recipients of mRNA-1273 generated higher median antibody titers (2,042 AU/mL) than recipients of BNT162b2 (389.2 AU/mL), which was also noted in another study (20). However, our sample size and cross-sectional observation preclude determination of clinical significance. It has been posited that the higher amount of mRNA encoding the SARS-CoV-2 spike protein in mRNA-1273 (100 μg for mRNA-1273 vs. 30 μg for BNT162b2) may account for the difference in antibody titers between the two vaccines (20). Thus, similar to influenza vaccine efficacy in older individuals, administration of a higher mRNA total dose to increase antigen delivery may be required to optimize responses of individuals immunocompromised by disease and/or therapy. In addition, because germinal center reactions in response to mRNA vaccination last up to 12 weeks (24), the delayed timing of the second dose of mRNA-1273 (28 days for mRNA-1273 vs. 21 days for BNT162b2) may induce higher spike-specific antibody levels from the positive effects of delayed boosting following the priming dose, a strategy used early in the COVID-19 pandemic in the United Kingdom.
In this study, we evaluated antibody neutralization capacity using a surrogate ACE-2/receptor binding domain (RBD) inhibition assay, which provides results comparable to conventional live virus or pseudovirus neutralization assays (25). Although the various antibody neutralization assays have not been validated specifically in patients with cancer, significant variation in assay accuracy for patients with cancer, as compared with noncancer populations, is unlikely. Importantly, regardless of the neutralization assay platform, there are known deficiencies of each regarding their true representation of activity in vivo, as none of the assays measure actual effector function mediated by the Fc fragment of the antibody. In addition, viral clearance is only partially related to neutralization, as has been demonstrated for many viruses including SARS-CoV-2 (26). Our results also demonstrate a threshold effect between absolute antibody titers and neutralizing activity, thus supporting strategies to augment responses including consideration of booster vaccines. Although our current study evaluated neutralization capacity against the SARS-CoV-2 wild-type variant, further investigation into neutralization capacity against the B.1.617.2 (delta) variant, as well as other new variants of concern, in the setting of booster vaccination is warranted.
Vaccine efficacy requires the induction of vigorous and durable antibody and cellular responses (27). Although humoral immunity is a key measure of vaccine response, inadequate antiviral antibody titers and/or neutralizing activity do not necessarily signify absence of vaccine benefit. In one study, patients with cancer with impaired B-cell responses but preserved CD8 T-cell responses during COVID-19 infection had lower viral loads and mortality than patients without T-cell responses (28), underscoring the contribution of the adaptive arm of immunity in conferring immune protection. Although B-cell targeting therapies like anti-CD20 antibodies or BTK inhibitors may allow for adequate T-cell immunity, others like anti-CD38–directed therapies have broader effects, including targeting activated T-cell subsets. Studies evaluating the qualitative and quantitative aspects of cellular immune responses to COVID-19 vaccines for our study population are ongoing.
An important caveat to our study is that response assessments were specific for the original SARS-CoV-2 strain. The breadth and depth of antibody responses, as well as other aspects of vaccine efficacy, in the context of cancer therapy require additional investigation, especially as SARS-CoV-2 variants arise in the community. A strength of this study is the inclusion of a vaccinated healthy volunteer cohort, with the provision that the healthy volunteer pool skewed younger with female predominance. However, the overall vaccine responses of this cohort were consistent with those seen in adults for other studies (29, 30). More diverse, age-matched control groups will be important moving forward as data emerge on waning immunity in those age >65 and the role for booster vaccination. Another limitation of this study is the relative underrepresentation of some of the hematologic malignancy subsets, which merits follow-up studies of additional patients to confirm response outcomes. Finally, because virtually all patients in the study received mRNA-based vaccines, the applicability of our findings to alternative vaccine platforms is unknown.
In conclusion, intrinsic deficits in humoral immunity, further compounded by cancer-directed therapies, hinder antibody responses of patients with hematologic malignancy to COVID-19 vaccines. Because antibody titers alone are an imperfect surrogate of immunity, comprehensive evaluation of other parameters of response are warranted to define the role of booster vaccines and other adjunctive approaches to optimize vaccination strategies and clinical care for these patients.
Methods
Patients
Patients at Memorial Sloan Kettering Cancer Center (MSKCC) with leukemia, lymphoma, and multiple myeloma participated in this observational study and received their initial mRNA-based vaccines between December 2020 and April 2021, with vaccine responses measured at 1 and 3 months from initial vaccination (NB: “1 month” time point = 3 weeks from the first BNT162b2 vaccine and 4 weeks from the first mRNA-1273 vaccine). Any patient with a response assessment from at least one of the time points was included in the data analysis. Parallel assessments from a healthy volunteer cohort provided controls. The study was conducted through the Division of Hematologic Malignancies at MSKCC in accordance with the Declaration of Helsinki guidelines. Informed consent was waived under a retrospective research protocol (protocol 20-390) approved by the Institutional Review and Privacy Board of Memorial Hospital/MSKCC.
Anti–SARS-CoV-2 Spike IgG Assay
A chemiluminescent microparticle immunoassay (AdviseDx SARS-CoV-2 IgG II assay; Abbott) detected anti–SARS-CoV-2 spike IgG antibody titers. Briefly, serum samples were combined with paramagnetic particles coated with recombinant SARS-CoV-2 protein specific for the RBD of the S1 protein, followed by incubation, washing, and addition of a conjugate and chemiluminescent substrate. The resulting chemiluminescent reaction was measured as a relative light unit (RLU), with a direct relationship between the amount of IgG antibodies to SARS-CoV-2 in the sample and the RLU detected by the system optics (Architect i2000 analyzer). The assay uses a 4-Parameter Logistic Curve fit data reduction method (4PLC, Y-weighted) to generate a calibration. The cutoff is 50.0 AU/mL.
Surrogate Virus Neutralization Assay
The SARS-CoV-2 surrogate virus neutralization test kit (Genescript) measured circulating neutralizing antibodies against SARS-CoV-2 that block the interaction between the RBD of the viral spike glycoprotein with the ACE2 cell-surface receptor. Briefly, serum samples were preincubated with the horseradish peroxidase (HRP)–conjugated recombinant SARS-CoV-2 RBD fragment (HRP-RBD, wild-type variant) to allow binding of circulating neutralization antibodies to HRP-RBD, then added to a capture plate precoated with the human ACE2 receptor (hACE2) protein, followed by additional incubation and washing steps before addition of a stop solution for endpoint reaction reading on a microplate reader at 450 nm. The absorbance of the sample is inversely dependent on the titer of the anti–SARS-CoV-2 neutralizing antibodies. Percentage inhibition was calculated per manufacturer's instructions with a positive cutoff value of 30% and validated with a panel of confirmed COVID-19 patient and healthy control sera. This value was determined from a comparator plaque-reduction neutralization test (PRNT) assay performed per World Health Organization guidelines, showing 100% agreement with PRNT50 and PRNT90 levels.
Statistical Analyses
Descriptive analyses included mean ± standard deviation (SD) and median with the IQR. The Wilcoxon signed rank test and the Wilcoxon rank-sum test compared anti–SARS-CoV-2 neutralizing antibody titers and neutralizing activity across groups. Statistical analyses were calculated using Prism 8 software (GraphPad) and R 4.1.0 (R Core Team), with statistical significance requiring P < 0.05.
Supplementary Material
Acknowledgments
The authors thank the patients and healthy volunteers for participating in the trial. They also thank the nurses, advanced practice providers, research staff, and physicians of the Laboratory Medicine, Leukemia, Lymphoma, and Multiple Myeloma Services. Supplementary Figure S1 was created with BioRender.com. This study was supported by The Society of Memorial Sloan Kettering (D.J. Chung), NIH/NCI 5K08CA248966–02 (D.A. Knorr), Leukemia & Lymphoma Society (S.A. Vardhana), Pershing Square Sohn Cancer Research Alliance (S.A. Vardhana), and Conrad Hilton Foundation (S.A. Vardhana). This study was also funded in part through the NIH/NCI Cancer Center Support Grant P30 CA008748 and NIH P01 CA23766.
Footnotes
Note: Supplementary data for this article are available at Blood Cancer Discovery Online (https://bloodcancerdiscov.aacrjournals.org/).
#S.A. Vardhana and D.A. Knorr contributed equally to this article.
Blood Cancer Discov 2021;2:568–76
Authors' Disclosures
G.L. Shah reports other support from Janssen and Amgen outside the submitted work. G.A. Papanicolaou reports grants and personal fees from Merck & Co. outside the submitted work. A.R. Mato reports grants from Pfizer during the conduct of the study, as well as grants and personal fees from Loxo, Genentech/AbbVie, J & J, PCYC, AstraZeneca, Octopharma, and TG Therapeutics, personal fees from Curio, Dava, Medscape, and PER, and grants from Nurix, DTRM, and GenMab outside the submitted work. L.E. Roeker reports personal fees from AbbVie, AstraZeneca, Vaniam Group, Janssen, Loxo Oncology, Pharmacyclics, and TG Therapeutics, grants and personal fees from Pfizer, and other support from Abbott Laboratories outside the submitted work. M. Hultcrantz reports other support from Intellisphere LLC, Curio Science LLC, GlaxoSmithKline, Daiichi Sankyo, and Amgen outside the submitted work. S. Mailankody reports other support from Juno/Bristol Myers Squibb, Fate Therapeutics, Takeda Oncology, Allogene Therapeutics, and Janssen Oncology and personal fees from Evicore, Legend Biotech, and Plexus Communications during the conduct of the study. A.M. Lesokhin reports grants and personal fees from Pfizer and personal fees from Trillium, GenMab, Iteos, and Janssen outside the submitted work. S.A. Vardhana reports personal fees from Immunai and ADC Therapeutics outside the submitted work. No disclosures were reported by the other authors.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Authors' Contributions
D.J. Chung: Conceptualization, resources, data curation, formal analysis, supervision, funding acquisition, validation, investigation, visualization, methodology, writing–original draft, project administration, writing–review and editing. G.L. Shah: Conceptualization, visualization, project administration, writing–review and editing. S.M. Devlin: Formal analysis, visualization, writing–review and editing. L.V. Ramanathan: Investigation, writing–review and editing. S. Doddi: Investigation, writing–review and editing. M.S. Pessin: Writing–review and editing. E. Hoover: Project administration, writing–review and editing. L.T. Marcello: Investigation, writing–review and editing. J.C. Young: Investigation, writing–review and editing. S.R. Boutemine: Investigation, writing–review and editing. E. Serrano: Investigation, writing–review and editing. S. Sharan: Investigation, writing–review and editing. S. Momotaj: Investigation, writing–review and editing. L. Margetich: Investigation, writing–review and editing. C.D. Bravo: Project administration, writing–review and editing. G.A. Papanicolaou: Writing–review and editing. M. Kamboj: Writing–review and editing. A.R. Mato: Writing–review and editing. L.E. Roeker: Writing–review and editing. M. Hultcrantz: Writing–review and editing. S. Mailankody: Writing–review and editing. A.M. Lesokhin: Writing–review and editing. S.A. Vardhana: Conceptualization, supervision, funding acquisition, visualization, project administration, writing–review and editing. D.A. Knorr: Conceptualization, supervision, funding acquisition, visualization, project administration, writing–review and editing.
References
- 1.Assaad S, Avrillon V, Fournier M-L, Mastroianni B, Russias B, Swalduz A, et al. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur J Cancer 2020;135:251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, et al. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov 2020;10:783–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rugge M, Zorzi M, Guzzinati S.SARS-CoV-2 infection in the Italian Veneto region: adverse outcomes in patients with cancer. Nat Cancer 2020;1:784–8. [DOI] [PubMed] [Google Scholar]
- 4.Saini KS, Tagliamento M, Lambertini M, McNally R, Romano M, Leone M, et al. Mortality in patients with cancer and coronavirus disease 2019: a systematic review and pooled analysis of 52 studies. Eur J Cancer 2020;139:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, et al. Case fatality rate of cancer patients with COVID-19 in a New York Hospital System. Cancer Discov 2020;10:935–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee LYW, Cazier JB, Starkey T, Briggs SEW, Arnold R, Bisht V, et al. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol 2020;21:1309–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mato AR, Roeker LE, Lamanna N, Allan JN, Leslie L, Pagel JM, et al. Outcomes of COVID-19 in patients with CLL: a multicenter international experience. Blood 2020;136:1134–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hultcrantz M, Richter J, Rosenbaum CA, Patel D, Smith EL, Korde N, et al. COVID-19 infections and clinical outcomes in patients with multiple myeloma in New York City: a cohort study from five academic centers. Blood Cancer Discov 2020;1:234–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chari A, Samur MK, Martinez-Lopez J, Cook G, Biran N, Yong K, et al. Clinical features associated with COVID-19 outcome in multiple myeloma: first results from the International Myeloma Society data set. Blood 2020;136:3033–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharafeldin N, Bates B, Song Q, Madhira V, Yan Y, Dong S, et al. Outcomes of COVID-19 in patients with cancer: report from the National COVID Cohort Collaborative (N3C). J Clin Oncol 2021;39:2232–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamboj M, Shah MK.Vaccination of the stem cell transplant recipient and the hematologic malignancy patient. Infect Dis Clin North Am 2019;33:593–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schütt P, Brandhorst D, Stellberg W, Poser M, Ebeling P, Müller S, et al. Immune parameters in multiple myeloma patients: influence of treatment and correlation with opportunistic infections. Leuk Lymphoma 2006;47:1570–82. [DOI] [PubMed] [Google Scholar]
- 13.Le Dieu R, Taussig DC, Ramsay AG, Mitter R, Miraki-Moud F, Fatah R, et al. Peripheral blood T cells in acute myeloid leukemia (AML) patients at diagnosis have abnormal phenotype and genotype and form defective immune synapses with AML blasts. Blood 2009;114:3909–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fozza C, Crobu V, Isoni MA, Dore F.The immune landscape of myelodysplastic syndromes. Crit Rev Oncol Hematol 2016;107:90–9. [DOI] [PubMed] [Google Scholar]
- 15.Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat Med 2021;27:1205–11. [DOI] [PubMed] [Google Scholar]
- 16.Terpos E, Gavriatopoulou M, Ntanasis-Stathopoulos I, Briasoulis A, Gumeni S, Malandrakis P, et al. The neutralizing antibody response post COVID-19 vaccination in patients with myeloma is highly dependent on the type of anti-myeloma treatment. Blood Cancer J 2021;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parry H, McIlroy G, Bruton R, Ali M, Stephens C, Damery S, et al. Antibody responses after first and second Covid-19 vaccination in patients with chronic lymphocytic leukaemia. Blood Cancer J 2021;11:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lim SH, Campbell N, Johnson M, Joseph-Pietras D, Collins GP, O'Callaghan A, et al. Antibody responses after SARS-CoV-2 vaccination in patients with lymphoma. Lancet Haematol 2021;8:e542–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ehmsen S, Asmussen A, Jeppesen SS, Nilsson AC, Østerlev S, Vestergaard H, et al. Antibody and T cell immune responses following mRNA COVID-19 vaccination in patients with cancer. Cancer Cell 2021;39:1034–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL.Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies. Cancer Cell 2021;39:1031–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roeker LE, Knorr DA, Thompson MC, Nivar M, Lebowitz S, Peters N, et al. COVID-19 vaccine efficacy in patients with chronic lymphocytic leukemia. Leukemia 2021;35:2703–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Oekelen O, Gleason CR, Agte S, Srivastava K, Beach KF, Aleman A, et al. Highly variable SARS-CoV-2 spike antibody responses to two doses of COVID-19 RNA vaccination in patients with multiple myeloma. Cancer Cell 2021;39:1028–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anichini G, Terrosi C, Gandolfo C, Gori Savellini G, Fabrizi S, Miceli GB, et al. SARS-CoV-2 antibody response in persons with past natural infection. N Engl J Med 2021;385:90–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner JS, O'Halloran JA, Kalaidina E, Kim W, Schmitz AJ, Zhou JQ, et al. SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses. Nature 2021;596:109–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tan CW, Chia WN, Qin X, Liu P, Chen MIC, Tiu C, et al. A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2–spike protein–protein interaction. Nat Biotechnol 2020;38:1073–8. [DOI] [PubMed] [Google Scholar]
- 26.Winkler ES, Gilchuk P, Yu J, Bailey AL, Chen RE, Chong Z, et al. Human neutralizing antibodies against SARS-CoV-2 require intact Fc effector functions for optimal therapeutic protection. Cell 2021;184:1804–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pulendran B, Ahmed R.Immunological mechanisms of vaccination. Nat Immunol 2011;12:509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang A, Bange E, Han N, Wileyto EP, Kim J, Gouma S, et al. CD8 T cells compensate for impaired humoral immunity in COVID-19 patients with hematologic cancer. Res Sq 2021:rs.3.rs-162289. [Google Scholar]
- 29.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med 2020;383:2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2020;384:403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.