Abstract
The leishmaniases are a group of diseases caused by the protozoan parasite belonging to the genus Leishmania. In the New World, although dogs are considered the main parasite reservoir, in the last two decades, several studies have confirmed the role of cats (Felis catus) in the epidemiology of the disease and feline leishmaniasis (FeL) is now considered to be an emerging disease. The present review summarizes the current knowledge about FeL, focusing on important immunopathological aspects, epidemiology, and diagnostic methods applied for felines in Brazil. Cats are infected with the same species of Leishmania found in dogs (i.e., Leishmania infantum). Like dogs, skin lesions are the most common in cats with clinical FeL, mainly affecting the cephalic region and less frequently the legs which may be accompanied by generalized signs or visceral involvement. Information on the immune response of cats to Leishmania infection is scarce; however, efficient infection control is seen in most cases. For diagnosis, generally, the same methods as those in dogs are used, mainly serological tools. But there is a lack of studies focusing the performance of these methods for diagnosing FeL. The estimated overall prevalence of FeL in Brazil is 8%, with L. infantum being the most prevalent species. However, infections with Leishmania braziliensis and Leishmania amazonensis have also been reported. In conclusion, although there has been an increase in the publication related to FeL in Brazil in recent years, there is a lack of research relating immune response and diagnosis of these animals. Cats have been shown to be competent hosts for Leishmania parasites, and their role in the epidemiology of the disease cannot be underestimated, especially in areas of Brazil where the disease is historically endemic.
Keywords: Diagnosis, Epidemiology, Felis catus, Leishmaniases
Introduction
The leishmaniases are neglected tropical diseases caused by protozoa of the genus Leishmania (Kinetoplastida: Trypanosomatidae), of which more than 20 species infect humans. The main route of transmission to humans and other mammalian hosts is through the inoculation of parasites during the blood meal of the infected sand flies (Burza et al. 2018; WHO 2020).
There are three main forms of manifestation of the disease in humans: cutaneous leishmaniasis (CL), mucocutaneous leishmaniasis (MCL), and visceral leishmaniasis (VL). Depending on the source of infection, from an animal or human reservoir, leishmaniasis can be classified as either zoonotic or anthroponotic, respectively. The World Health Organization (WHO) estimates that about one billion people live in areas at risk for at least one of the clinical forms of the disease, with 556 million people at risk of developing VL (WHO 2016). Nevertheless, in recent years, the global number of human VL has declined substantially, from 200,000 to 400,000 cases in 2012 to approximately 17,000 cases annually in 2018 (Alvar et al. 2012; WHO 2020).
Unlike CL, which has a greater prevalence in rural areas, in Brazil, VL occurs predominantly in peripheral areas of urban centers, associated with environments with poor infrastructure and extremely poor sanitation conditions (Marchi et al. 2019). However, modified disease dynamics in recent years, because of geographic and environmental changes, has resulted in the advancement of VL into areas previously free of the disease, mainly in rural regions of Brazil (Reis et al. 2017).
It is widely known that dogs are the main parasite reservoir for canine and human Leishmania infantum infection (Werneck 2010; Solano-Gallego et al. 2016; Ribeiro et al. 2018). However, other mammals infected with L. infantum have been reported in Brazil (Lima et al. 2013). Wide dispersion of VL suggests new reservoirs of the disease, and probable involvement of synanthropic and domestic animals, such as cats, in parasite biological cycle (Dantas-Torres and Brandão-Filho 2006). The epidemiological role of felines in the disease cycle has been raised worldwide (Pennisi et al. 2013, 2015; Pennisi and Persichetti 2018). In Brazil, felines are confirmed as potential parasite reservoir (Silva et al. 2010; Mendonça et al. 2020), highlighting the importance of discussing the spread of FeL in the country.
Feline leishmaniasis (FeL) is an emerging disease caused primarily by L. infantum and has been globally reported, especially in endemic areas for human and canine leishmaniasis (Soares et al. 2015; Pennisi and Persichetti 2018). In the old world, leishmaniasis in domestic cats (Felis catus) has been mainly reported in Mediterranean countries (Miró et al. 2014; Asfaram et al. 2019; Iatta et al. 2019; Urbani et al. 2020) and recently shown to be an alarming disease in stray cats in Iran (Asgari et al. 2020). In the American continent, records of the disease have been increasing in Central and South America, especially in Brazil (Soares et al. 2015; Asfaram et al. 2019). However, there is still no consensus on the role of cats in maintaining Leishmania transmission in rural and urban areas.
Global emergence of FeL
Over the past 40 years, approximately 80 cross-sectional studies on the prevalence of FeL around the world have shown a worldwide average seroprevalence of 12% (Asfaram et al. 2019). At the same time, the number of published papers on FeL has increased in endemic areas, mainly in Europe and South America, notably in Brazil.
In Europe, most reports of FeL come from southern countries including Italy, Spain, Portugal, and Greece (Asfaram et al. 2019). Recently, the prevalence of FeL in the Northern Italy was shown to be high, with total values ranging from 8.6 to 12.5% in different localities of a non-endemic region, with the presence of L. infantum confirmed by molecular diagnosis (Spada et al. 2020; Urbani et al. 2020). Furthermore, it was seen that the risk of infection may increase depending on the geographical area of the country, as observed in cats in the Southern region of Italy where prevalence values were 10.5% among 645 animals evaluated (Iatta et al. 2019). In Spain, seroprevalence among stray cats was 3.2%, with emphasis on coinfections by zoonotic parasites such as Toxoplasma gondii and Toxocara cati, as shown in a study of 346 animals (Miró et al. 2014). In Greece, FeL infections have also been reported, both in the central and northern regions, with the prevalence ranging from 3.78 to 12.3% (Diakou et al. 2009; Giannakopoulos et al. 2017).
In Portugal, seroprevalence for FeL was 3.7% in a study of 271 cats in the southern region. This prevalence was considered high for the region and the increased contact between the infected vector and the cats is believed to be one of the reasons for the infection values in this study (Maia et al. 2015). In the northern region, the prevalence for 316 animals was lower (2.8%), with rural area cats showing higher positivity than urban area animals (Cardoso et al. 2010). It is important to highlight that the prevalence data on FeL is characterized by a high variability due to different factors such as the diagnostic method used, serological or molecular, the geographical area, and the cat population screened (Miró et al. 2014; Iatta et al. 2019; 2020).
In the Old World, L. infantum is the most prevalent species in infected cats, but Leishmania tropica and Leishmania major have been found in domestic and stray cats in Turkey and L. tropica in stray cats in Iran (Paşa et al. 2015; Can et al. 2016; Akhtardanesh et al. 2020). Worldwide, FeL is not limited to European countries. Several other countries have reported FeL cases including Egypt, Iran, Thailand, Texas (USA), Venezuela, and Mexico (Asfaram et al. 2019). These studies show an increasing number of infected cats and demonstrate the importance of more accurate investigations into the role of cats in the current epidemiology of leishmaniasis.
Emergence of FeL in Brazil
In Brazil, one of the first cases of FeL was reported in Belo Horizonte, Minas Gerais (Passos et al. 1996), in a domestic cat that presented lesions in the interdigital region of the left hind paw, with numerous amastigotes observed in Giemsa staining. Later, through polymerase chain reaction (PCR), the authors confirmed the presence of Leishmania of the subgenus Viannia, but without identifying the species. However, it was only in the year 2000 that the first autochthonous case of FeL was reported in the state of São Paulo, in which L. infantum was identified (Savani et al. 2004). Since then, the importance of the cat in the epidemiology of the disease has become the target of other studies that have reported the presence of the protozoan infecting cats in other Brazilian states (Table 1). The prevalence of FeL in Brazil is estimated to be between 7 and 8% diagnosed via molecular and serological methods, with the most common species being Leishmania braziliensis, L. infantum, and Leishmania amazonensis (Schubach et al. 2004; Souza et al. 2005; Figueiredo et al. 2009; Coura et al. 2018; Asfaram et al. 2019; Carneiro et al. 2020; Costa-Val et al. 2020).
Table 1.
Studies from Brazil reporting Leishmania infection in felines (1996–2020)
| Authors/year | State | Sample size | Leishmania species | Positivity (%) | |||
|---|---|---|---|---|---|---|---|
| IFAT | ELISA | PCR | Parasitologicala | ||||
| Passos et al. (1996) | MG | 1 | Leishmania sp. | - | - | 100 | - |
| Savani et al. (2004) | SP | 1 | L. infantum | 100 | - | 100c | 0 |
| Schubach et al. (2004) | RJ | 2 | L. braziliensis | - | - | - | 100 |
| Souza et al. (2005) | MS | 1 | L. amazonensis | 100 | - | - | 100 |
| Silva et al. (2008) | RJ | 8 | L. infantum | 25 | - | 25.0 | - |
| Figueiredo et al. (2009) | RJ | 43 | L. braziliensis | 0 | 2.4 | - | - |
| Dahroug et al. (2010) | MT | 16 | L. infantum* | - | - | 37.5b | - |
| Coelho et al. (2010) | SP | 1 | L. infantum* | 0 | 100 | 100c | 100 |
| Bresciani et al. (2010) | SP | 283 | Leishmania sp. | 0 | - | - | 0.7 |
| Silva et al. (2010) | MG | 1 | L. infantum | 100 | - | 100c | - |
| Dahroug et al. (2011) | MT | 1 | L. infantum* | - | - | 100b | - |
| Coelho et al. (2011a) | SP | 52 | L. infantum* | - | - | 3.8 | 3.8 |
| Coelho et al. (2011b) | SP | 70 | Leishmania sp. | 0 | 4.2 | - | - |
| Vides et al. (2011) | SP | 55 | L. infantum* | 10.9 | 25.4 | 100bc | 18.2 |
| Neto et al. (2011) | SP | 113 | Leishmania sp. | - | 11.5 | - | - |
| Sobrinho et al. (2012) | SP | 302 | L. infantum | 4.6 | 12.9 | 100bc | 9.9 |
| Morais et al. (2013) | PE | 5 | L. infantum | - | - | 80.0b | - |
| Cardia et al. (2013) | SP | 386 | Leishmania sp. | 0.5 | - | - | - |
| Silva et al. (2014) | PE | 153 | L. infantum | - | 3.9 | - | - |
| Braga et al. (2014a) | MS | 50 | Leishmania sp. | 4.0 | - | - | - |
| Braga et al. (2014b) | SP; MS | 50 | Leishmania sp. | 30.0 | - | 0 | 4.0 |
| Sousa et al. (2014) | MS | 151 | L. infantum | 6.6 | - | - | - |
| Oliveira et al. (2015a) | PA | 443 | Leishmania sp. | 4.0 | - | - | - |
| Oliveira et al. (2015b) | SP | 52 | Leishmania sp. | - | - | 13.5 | - |
| Metzdorf et al. (2017) | MS | 100 | L. infantum | - | - | 6.0b | 4.0 |
| Benassi et al. (2017) | SP | 108 | L. infantum | - | - | 1.8b | - |
| Matos et al. (2018) | PR | 679 | Leishmania sp. | 15.8 | 43.4 | - | - |
| Coura et al. (2018) | MG | 100 | L. infantum | 54.0 | - | 0c | 0 |
| Madruga et al. (2018) | MT | 1 | L. infantum | - | - | 100c | 100 |
| Marcondes et al. (2018) | SP | 90 | L. infantum | - | - | 55.5 | 14.0 |
| Headley et al. (2019) | MT | 2 | Leishmania sp. | - | - | - | 100 |
| Pedrassani et al. (2019) | SC | 30 | L. infantum | 6.6 | - | 0 | - |
| Rocha et al. (2019) | MA | 105 | L. infantum | 30.4 | - | 5.7 | - |
| Bezerra et al. (2019) | RN | 91 | Leishmania sp. | 15.3 | - | 0 | - |
| Tolentino et al. (2019) | MG | 12 | Leishmania sp. | - | 33.3 | - | - |
| Carneiro et al. (2020) | PA | 1 | L. amazonensis | - | - | 100bc | 100 |
| Silva et al. (2020) | PB | 2 | L. infantum | - | 100 | 100 | 100 |
| Costa-Val et al. (2020) | MG | 64 |
L. infantum L. braziliensis |
- | 29.8 | 12.5 | - |
| Berenguer et al. (2020) | PE | 128 | L. infantum | - | - | 0.7 | 0.7 |
| Leonel et al. (2020) | SP | 94 | Leishmania sp. | 29.7 | 31.9 | 0 | - |
- tests not performed, IFAT immunofluorescent antibody test, ELISA enzyme-linked immunosorbent assay, PCR polymerase chain reaction, MG Minas Gerais, MA Maranhão, MS Mato Grosso do Sul, MT Mato Grosso, PA Pará, PB Paraíba, PE Pernambuco, PR Paraná, SC Santa Catarina, SP São Paulo, RJ Rio de Janeiro, RN Rio Grande do Norte
*L. chagasi in the original articles
aCytological, histological or microscopic diagnosis
bBased on quantitative PCR or PCR–RFLP
cMethod used for species identification (In some studies, performed only with part of the study sample)
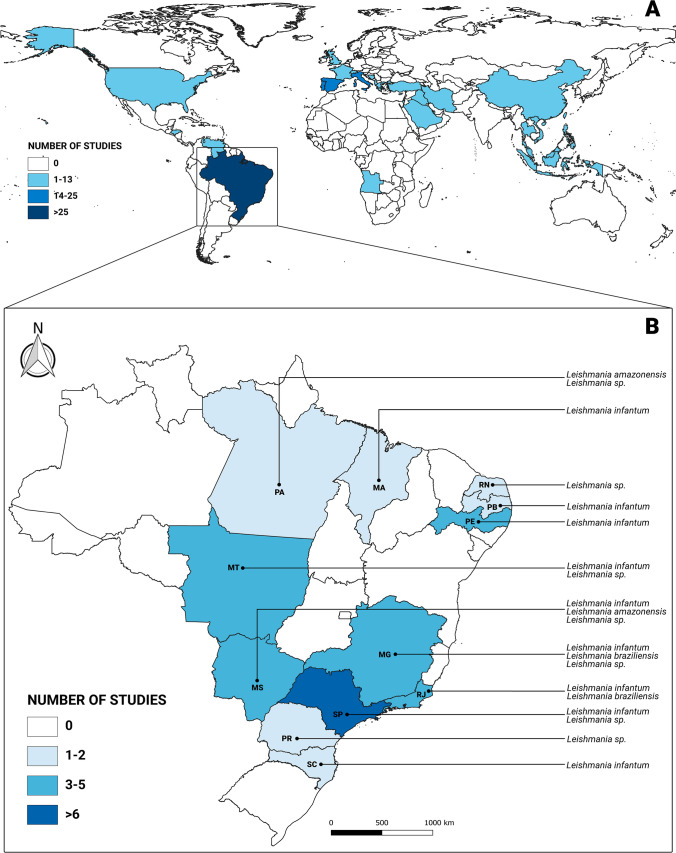
Regarding the geographical location of these species, it was seen that L. braziliensis was restricted to the southeastern region of Brazil, reported both in endemic (Schubach et al. 2004) and non-endemic areas (Figueiredo et al. 2009) of the state of Rio de Janeiro and in endemic municipalities in the state of Minas Gerais (Costa-Val et al. 2020). L. amazonensis has been reported in cats from endemic municipalities in the Midwest, Mato Grosso do Sul state (Souza et al. 2005), and in the North, Pará state (Carneiro et al. 2020). L. infantum, on the other hand, has been reported in 12 of the 27 states of Brazil, with a lesser number in regions not endemic for VL (Savani et al. 2004; Braga et al. 2014b; Benassi et al. 2017; Pedrassani et al. 2019), and mostly in endemic regions (Fig. 1) (Silva et al. 2008; Coelho et al. 2010; Coelho et al. 2011a; Vides et al. 2011; Sobrinho et al. 2012; Morais et al. 2013; Silva et al. 2014; Sousa et al. 2014; Metzdorf et al. 2017; Coura et al. 2018; Marcondes et al. 2018; Rocha et al. 2019; Costa-Val et al. 2020; Berenguer et al. 2020; Silva et al. 2020).
Fig. 1.
Distribution of the number of studies on feline leishmaniasis conducted in the world (A) and Brazil (B) (1996–2020). MG, Minas Gerais; MA, Maranhão; MS, Mato Grosso do Sul; MT, Mato Grosso; PA, Pará; PB, Paraíba; PE, Pernambuco; PR, Paraná; SC, Santa Catarina; SP, São Paulo; RJ, Rio de Janeiro; RN, Rio Grande do Norte
The first report of L. infantum infection transmitted by L. longipalpis in a naturally infected cat was reported in 2010 (Silva et al. 2010). In this study, through xenodiagnosis, promastigotes were visualized in the midgut of the vector, demonstrating its ability to be infected by L. infantum from clinically affected cats during hematophagy. Mendonça et al. (2020) confirmed that cats are capable of infecting L. longipalpis. In this study, eight animals with L. infantum present in the bone marrow and skin were able to infect the vector, and all animals were clinically affected. To verify the possibility of transmission of L. infantum from a clinically affected domestic cat to a healthy domestic dog via the invertebrate vector, a recent study reaffirmed the competence of this transmission route and demonstrated that the dog develops the clinical signs of canine VL such as lymph node enlargement, generalized alopecia, lesions on the ears and face, and weight loss (Batista et al. 2020). These reports not only highlight the possibility of transmission of the disease from cats to dogs, but also draw attention to the possible transmission from cats to humans.
FeL pathogenesis and clinical signs
The mechanism of feline immune function against Leishmania is not yet fully elucidated and much of what is known derives from studies in humans and dogs. Cats, compared to dogs, are known to possess a certain degree of resistance to Leishmania, resulting in a lower prevalence of infection or development and manifestation of characteristic clinical signs of leishmaniasis in these animals (Solano-Gallego et al. 2007; Akhtardanesh et al. 2018). The development of the disease is influenced by the genetic profile of the host, which explains the difference in the immune response in dogs and cats (Day 2016).
Since the sand fly saliva has immunomodulatory properties, after the inoculation of the promastigote forms during hematophagy in the vertebrate host, there is a reduction in the participation of macrophages, which are responsible for inducing pro-inflammatory cytokines such as gamma interferon (IFN-y) and interleukin 2 (IL-2), and the targeting of cellular immunity via T helper 2 (Th2), resulting in infection tolerance (Tomiotto-Pellissier et al. 2018). It is believed that in dogs, the predominant Th2 immune response is one of the factors that determine susceptibility to pathogens (Day 2016; Solano-Gallego et al. 2016).
In this respect, it was recently observed that cats infected with L. infantum, in leishmaniasis endemic areas of Italy and Spain, produced specific IFN-y in response to the parasites. Both clinically affected and apparently healthy felines could stimulate cell-mediated immunity, although clinically affected cats show higher production of pro-inflammatory cytokines (Priolo et al. 2019). As far as the antibody-mediated response is concerned, it does not seem to act in a protective manner in cats. In a follow-up study of 13 female animals for 72 weeks in Brazil (Simões-Mattos et al. 2005), it was seen that immunoglobulin G (IgG) production was detected from the second week post-infection (p.i.) in only 23% of the cats, and the antibody concentration remained low until the 12th week p.i. when seroconversion became evident in 50% of the cats. In addition, in the same study, the peak of antibody production occurred only at the 26th week p.i. with all animals showing positive serology. Even then, only a small correlation between the decrease in nostril lesions and IgG increase was observed. Self-healing occurred in the subsequent months.
While the presence of antibodies against Leishmania in felines demonstrates that these animals can be infected by these protozoa (Bezerra et al. 2019), the absence of anti-Leishmania antibody titers in cats experimentally infected has also been reported (Akhtardanesh et al. 2018). Low antibody titers in cats with a positive parasitological diagnosis indicate that cats may not develop an intense humoral immune response (Sobrinho et al. 2012).
In dogs with severe clinical signs and infected with L. donovani, low IFN-y production was observed, and despite having higher antibody titers, these animals demonstrated high parasitemia (Solano-Gallego et al. 2016). Recently, using the PCR technique, it was observed that the mean Leishmania parasite load in cats, unlike dogs, is significantly lower in the positive blood samples. This could be associated, in part, with the decreased antibody titers in these cats, possibly due to the prevalence of the Th1 immune response profile (Priolo et al. 2019; Baneth et al. 2020).
Coinfection with other parasites has been reported significantly in some studies. Cats with L. infantum in leishmaniasis endemic areas have coinfections with Toxoplasma gondii, feline coronavirus, and especially with feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV), which could partly explain the success of Leishmania infection in these animals (Sobrinho et al. 2012; Spada et al. 2016; Iatta et al. 2019). Retroviruses such as FIV and FeLV have a large impact on domestic cat health worldwide. Due to the suppressive effects on the immune system of these animals caused by FIV and FeLV, there is an increased risk of opportunistic infections such as vector-borne diseases (VBDs) (Hartmann 2012). As seen in a recent study in Iran, FIV- and FeLV-infected cats have a higher risk of testing positive for L. infantum (Akhtardanesh et al. 2020). However, further studies on the presence of coinfections with FIV and FeLV need to be performed to present more consistent information on the role of leishmaniasis in this type of coinfection (Bezerra et al. 2019). In this regard, there is research showing that although FIV coinfection is frequently reported, there is no association between the presence of FIV and or FeLV with Leishmania infection in cats, making the association between retroviral infections and FeL uncertain (Sousa et al. 2014; Miró et al. 2014; Poffo et al. 2017; Marcondes et al. 2018; Bezerra et al. 2019; Baneth et al. 2020). Also, VBDs may become even more frequent in cats living in geographically confined environments. For example, island-dwelling cats in Italy were reported to have an increased incidence of L. infantum infection after a season of exposure to sand flies (Otranto et al. 2017). Less common coinfections in cats with L. infantum have also been reported in Brazil, such as the presence of Mycoplasma spp. and Neospora caninum (Sousa et al. 2014; Marcondes et al. 2018). Although there has been an increase in research with FeL in the recent years, including in Brazil, data on coinfection is still scarce (Marcondes et al. 2018).
Regarding the age of the animals, it is believed that adult cats are more likely to be infected by protozoa than young cats. Toxoplasma infections, for example, were significantly higher in cats older than one year (Cardia et al. 2013). To date, no Leishmania infections have been reported in young cats; however, further investigations are needed about genetic differences among cats to elucidate mechanisms of susceptibility, as well as to clarify the higher prevalence in adult animals (Pennisi and Persichetti 2018).
Although there are positive L. infantum cats without apparent clinical manifestations (Figueiredo et al. 2009; Morais et al. 2013; Braga et al. 2014a; Oliveira et al. 2015b; Coura et al. 2018; Pedrassani et al. 2019), in recent years, case reports have recorded the main pathological clinical signs associated with the manifestation of FeL (Brianti et al. 2019). The most common clinical signs are skin lesions, which are usually the only signs available for physical examination, showing mainly ulcerative dermatitis, eventually crusted; nodular or scaly dermatitis, especially in the head and neck region; followed by alopecia, thinning coat and lacerations (Pennisi et al. 2013). Skin lesions accompanied by lymph node enlargement have been described in more than half of clinical cases. The dermatological lesions can be single or multiple and are usually located in the cephalic region, the pinna, and the tip of the nose, in addition to generalized involvement, especially in the legs (Vides et al. 2011; Pennisi et al. 2013; 2015; Pennisi and Persichetti 2018; Rivas et al. 2018; Rocha et al. 2019; Fernandez-Gallego et al. 2020).
Eye diseases, especially uveitis, nodular blepharitis, and panophthalmitis, may also be present, which is usually the reason for consulting the veterinarian (Pennisi et al. 2013). Similarly, corneal edema or perforation, ulcerative or non-ulcerative keratitis with intense neovascularization, and conjunctivitis have been described. Cases with exclusively ocular manifestations and the presence of pseudotumors in the iris have also been recently reported both in Brazil and in Europe (Madruga et al. 2018; Fernandez-Gallego et al. 2020).
In addition, there are several non-specific signs that can appear in infected cats, such as weight loss, anorexia, dehydration, and decreased appetite. Visceral and sporadic signs are also present, including membrane paleness, cachexia, fever, diarrhea, hepatomegaly, splenomegaly, enlarged lymph nodes, vomiting, dyspnea, hypothermia, kidney disease, and even abortion. Among the laboratory abnormalities, hyperglobulinemia, hypoalbuminemia, proteinuria, renal azotemia, and leukopenia may be present (Chatzis et al. 2014; Pennisi et al. 2015; Pennisi and Persichetti 2018). All these signs have also been reported in dogs, and they can be general or localized, symmetric or asymmetric, with diffuse or focal distribution, and also coexist with mucocutaneous lesions (Pennisi et al. 2015).
Diagnostic methods for FeL
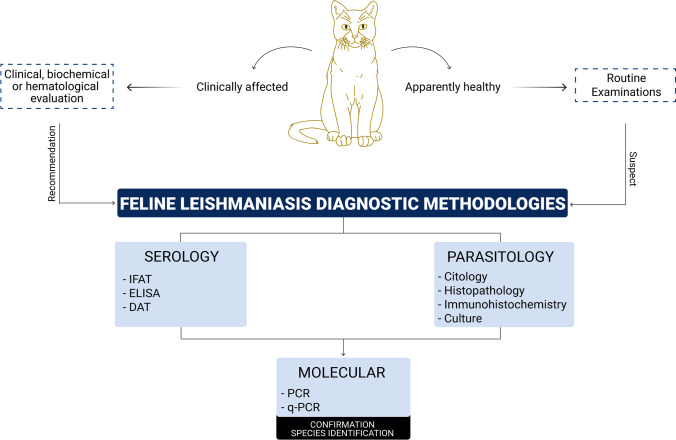
For the diagnosis of an infected animal, several techniques can be employed, with the methodologies applied in dogs generally also being used in cats (Fig. 2). Leishmania amastigotes infecting mainly macrophages, and sporadically neutrophils, of the host can be found in various tissues such as lymph nodes, bone marrow, peripheral blood, skin, mucous membranes, and the eyes (Schubach et al. 2004; Souza et al. 2005; Bresciani et al. 2010; Coelho et al. 2010, 2011a; Vides et al. 2011; Sobrinho et al. 2012; Metzdorf et al. 2017; Madruga et al. 2018; Marcondes et al. 2018; Carneiro et al. 2020). Usually, the diagnosis begins with an anamnesis, regarding the geographical area where the animal lives, the risk of exposure to sand flies, use of repellents, etc. This follows a clinical and biochemical evaluation, analyzing the characteristic clinical signs of leishmaniasis as well as potential variations in the blood count, which provide support for more specific investigations. Main laboratory diagnostic methods include parasitological analysis, followed by serological and molecular methods, notably PCR (Soares et al. 2015; Pennisi et al. 2013, 2015; Brianti et al. 2017) (Fig. 2).
Fig. 2.
Feline leishmaniasis diagnostic methodologies. IFAT, immunofluorescent antibody test; ELISA, enzyme-linked immunosorbent assay; DAT, direct agglutination test; PCR, polymerase chain reaction; qPCR, quantitative PCR
Direct observation of the parasite is done through parasitological diagnosis (Soares et al. 2015). Cytological preparations of the spleen, liver, bone marrow, and lymph nodes (organs classically affected by the amastigote forms), usually stained with Giemsa, are most frequently used (Savani et al. 2004; Coelho et al. 2011a). The presence of amastigotes in lymphoid tissues is probably associated with clinical-pathological conditions in felines, which highlight the importance of investigating these tissues to increase the sensitivity of parasitological diagnosis (Bresciani et al. 2010; Coelho et al. 2010, 2011a; Vides et al. 2011; Sobrinho et al. 2012; Marcondes et al. 2018).
In clinically affected cats, it has been observed that among the lymphoid organs, the lymph nodes and bone marrow provide a more sensitive diagnosis compared to the spleen and liver. However, there is still no consensus on which organ is the best for cytological diagnosis (Coura et al. 2018). In cats with dermatologic lesions, the sensitivity of cytology tests may be enhanced (Sobrinho et al., 2012). In addition, cytology is recommended in symptomatic cases because it is a technique with relatively simple implementation and fast results, and should, therefore, be part of the set of methods used by veterinarians during examinations for FeL, especially in cats previously diagnosed with a negative result but with clinical signs (Vides et al. 2011; Metzdorf et al. 2017).
Cytology is the most commonly used diagnostic method for skin lesions, but when amastigotes are not visualized by this technique, histological, immunohistochemical, or PCR-based diagnostics of the lesion samples are usually used (Abramo et al. 2021). Lesion fragments are cultured in Novy-MacNeal-Nicolle (NNN) medium in search of promastigotes (Schubach et al. 2004; Souza et al. 2005; Simões-Mattos et al. 2005). However, diagnosis by culture is slow to produce results and presents low sensitivity, even in endemic areas, which is a disadvantage when using this technique (Soares et al. 2015; Coura et al. 2018). Biopsy fragments taken from skin lesions can have amastigotes detected by histology (Abramo et al. 2021), and the tissue can also be homogenized and inoculated into hamsters to analyze the development of lesions in these animals and reinforce the diagnosis result, as recently demonstrated in the first report of L. amazonensis in a cat in the Amazon region of Brazil (Carneiro et al. 2020). Finally, immunohistochemistry can be used to increase the possibility of finding parasites when they are in low numbers in tissues. Due to its high sensitivity, this test can be used as a complementary method to increase the sensitivity of the diagnostic result (Vides et al. 2011; Headley et al. 2019).
Serological methods are the most used diagnostic methods worldwide for the diagnosis of Leishmania infection. Among these techniques, immunofluorescent antibody test (IFAT) and enzyme-linked immunosorbent assay (ELISA) are the preferred options (Pennisi and Persichetti 2018; Asfaram et al. 2019). In Brazil, IFAT followed by ELISA are the techniques most frequently used for diagnosis of both dogs and cats (Trevisan et al. 2015). Although Western Blot (WB), generally used in academic surveys, has demonstrated better sensitivity and specificity compared to IFAT and ELISA (Persichetti et al. 2017), a recent study showed that the WB has a low agreement when compared to the results of these two serological tests, as well as compared to molecular diagnosis (Alcover et al. 2021).
IFAT has shown to be the most sensitive methodology for identifying subclinical or early infections in felines and has revealed a relatively high prevalence in endemic areas of Brazil (Silva et al. 2008; Persichetti et al. 2017). An important issue to be defined in this methodology is the choice of the optimal cutoff point. The cutoff at the 1:80 dilution, like that used in dogs, is believed to have the best sensitivity in cats (Pennisi et al. 2015; Pennisi and Persichetti 2018). However, in Brazil, most published studies have used values equal to or above 1:40, ranging from low (Silva et al. 2008, 2010; Cardia et al. 2013) to high serological prevalence, as seen in studies using data from the states of Mato Grosso, Pará, and São Paulo (Braga et al. 2014a; Oliveira et al. 2015a; Leonel et al. 2020). Some studies reported up to 54% positivity for this titration, as seen in a study from the state of Minas Gerais (Coura et al. 2018). On the other hand, some studies have not shown positive results with these dilutions, even in endemic areas (Figueiredo et al. 2009; Bresciani et al. 2010; Coelho et al. 2010; 2011b; Vides et al. 2011; Sobrinho et al. 2012). In the study from Araçatuba (state of São Paulo, Brazil), the 1:40 cutoff showed higher sensitivity compared to the 1:80 dilution, with 5/55 and 1/55 cats diagnosed with leishmaniasis in the above dilutions respectively (Vides et al. 2011). In a study from São Luís (state of Maranhão, Brazil), however, the 1:80 dilution proved to be more sensitive (15/105 positive), compared to 4/105 seropositive in the 1:40 dilution. The total seroprevalence reported in this study was 30.48% (Rocha et al. 2019). Thus, there is still no consensus on the best cutoff for diagnosing FeL by IFAT. For dogs, the Brazilian Ministry of Health considers as seroreagent samples that have antibody dilution titers equal to or greater than the 1:40 dilution (cutoff) (Brasil 2014). The lack of standardization, associated with low antibody titers, could explain, in part, the discrepancy in the positivity of this technique compared to other serological methods such as ELISA utilized in the country (Coelho et al. 2011b).
The ELISA technique has been widely used for the detection of anti-Leishmania antibodies that may represent an infection or a history of exposure to the parasite in Brazil (Trevisan et al. 2015). This methodology demonstrates greater sensitivity in clinically affected felines (Persichetti et al. 2017). In several studies around the country a higher seroprevalence of FeL was found by ELISA when compared to IFAT (Figueiredo et al. 2009; Coelho et al. 2011b; Vides et al. 2011; Sobrinho et al. 2012; Matos et al. 2018). Although FeL seroprevalence in Brazil is relatively low, some studies have shown high positive results in endemic areas of the country, as seen in Londrina, Paraná state, Brazil, recording a seroprevalence of 43.4% (295/679) (Matos et al. 2018) and in Ilha Solteira, São Paulo state, Brazil showing a seroprevalence of 31.91% (30/94) (Leonel et al. 2020). Even so, the seroprevalence measured by ELISA diagnosis may be influenced by methodological variation and the antigen used in the test (Neto et al. 2011). Therefore, it is recommended to use ELISA in combination with other techniques to increase the sensitivity of the diagnoses (Silva et al. 2014).
It is important to note that in case of the whole parasite being used as an antigen in areas endemic for other parasites (like Trypanosoma spp.), the possibility of false positive result should be considered (Sobrinho et al. 2012; Braga et al. 2014b; Iatta et al. 2020). Since Leishmania spp. are phylogenetically very close to other trypanosomatids, employing only serological diagnostics is not recommended (Braga et al. 2014b). Cross-reactions between Leishmania spp. and Trypanosoma cruzi have already been reported in cats from an endemic area (Pará state, Northern region) for CL in Brazil (Matos et al. 2018).
Few reports using recombinant antigens for FeL diagnosis have been published to date. Two of the limited number of studies used the antigens k39 and rKDDR (recombinant kinesin degenerated derived repeat), with both ELISA and rapid immunochromatography tests. These antigens offer the possibility of increased binding specificity with Leishmania-specific antibodies, although there is still the possibility of cross-reaction with members of the Trypanosomatidae (Neto et al. 2011; Tolentino et al. 2019).
Since peak antibody production is not reached during Leishmania infection in cats until around the 26th week, serology may not be a good marker for the diagnosis of Leishmania infection (Simões-Mattos et al. 2005). Therefore, this factor, combined with differences in the natural genetic background of these animals, may induce false-negative results during serology, requiring confirmation with another more sensitive and specific technique for FeL, such as molecular methods (Silva et al. 2008; Pennisi et al. 2015; Day 2016; Persichetti et al. 2017). Few broad seroepidemiological surveys have been conducted in endemic areas of Brazil, and most cases are diagnosed only when cats show clinical signs or during vaccination programs. This leads to a delay in correct diagnosis and favors the spread of infection in these regions (Silva et al. 2008).
There are several types of molecular tests for the detection of Leishmania in humans and animals. Among the molecular methods, conventional PCR (cPCR) is the most widely used, acting as a confirmatory diagnosis for FeL (Pennisi and Persichetti 2018). In Brazil, there are variations in molecular results depending on the type of tissue used for analysis. In this regard, some studies report negative PCR results in blood tissue even in animals with confirmed antibody presence by one or more serological tests (Braga et al. 2014b; Bezerra et al. 2019; Leonel et al. 2020), while others have shown higher PCR positivity with bone marrow compared to blood (Marcondes et al. 2018). However, negative PCR results for Leishmania DNA have also been seen in investigations using bone marrow samples (Coura et al. 2018). According to Oliveira et al. (2015b), PCR with samples from the ocular conjunctiva can detect felines positive for Leishmania, also being a less invasive and stressful alternative.
Some studies use molecular analyses only to discriminate parasite species after a positive serological or parasitological test result, using cPCR (Coelho et al. 2010, 2011a; Oliveira et al. 2015b; Madruga et al. 2018; Marcondes et al. 2018; Rocha et al. 2019; Costa-Val et al. 2020), qPCR (Vides et al. 2011; Sobrinho et al. 2012; Benassi et al. 2017) and less frequently PCR–RFLP (PCR-restriction fragment length polymorphism) (Dahroug et al. 2010; Metzdorf et al. 2017). In Brazil, the most prevalent species diagnosed by molecular methods both domestic and wild cats is L. infantum (Coelho et al. 2010; Dahroug et al. 2010; Vides et al. 2011; Sobrinho et al. 2012; Metzdorf et al. 2017). PCR has also allowed the identification of other Leishmania spp. in cats in the country, such as L. braziliensis and more recently L. amazonensis, species related to cutaneous leishmaniasis in humans (Schubach et al. 2004; Simões-Mattos et al. 2005; Carneiro et al. 2020). Thus, in Brazil, cats infected with at least three of the five Leishmania spp., found in felines around the world, have been identified by molecular methods (Asfaram et al. 2019).
By using small amounts of biological material and distinguishing polymorphic differences in genetic material, different PCR-based techniques have been developed and employed for detection and identification of Leishmania (Veasey et al. 2020). Several genes are used as target sequences for Leishmania-specific identification, such as the glucose-6-phosphate dehydrogenase enzyme gene (g6pd), ribosomal DNA (rDNA) and especially kinetoplast DNA (kDNA) (Reimão et al. 2020; Veasey et al. 2020). In blood samples from dogs, it is well established that kDNA has better sensitivity compared to nuclear DNA and, for this reason, has been widely used for the detection of parasite DNA in these animals (Lachaud et al. 2002). kDNA has also been widely used as a target for diagnosis and species identification for cats in Brazil (Silva et al. 2008; Coelho et al. 2011a; Morais et al. 2013; Metzdorf et al. 2017; Benassi et al. 2017; Coura et al. 2018; Pedrassani et al. 2019; Costa-Val et al. 2020). However, it is necessary to pay attention to the selection of the best primers for a better performance of molecular diagnosis (Lachaud et al. 2002; Spada et al. 2020).
Infections by different Leishmania spp. in humans are known to result in different clinical signs, with L. infantum being associated with VL and L. braziliensis and L. amazonensis mainly related to cutaneous leishmaniasis (Burza et al. 2018). Although in cats the immune response pattern may interfere with the clinical signs of the disease (Day 2016), the response pattern to different Leishmania spp. seen in humans also appears to occur in felines in Brazil. Cats naturally infected with L. amazonensis and L. braziliensis exhibited nodular lesions of different sizes mainly on the face, notably on the ears (Carneiro et al. 2020; Schubach et al. 2004), followed by the nose and the digital regions of the paws (Souza et al. 2005). In another study from Brazil, in cats experimentally infected with L. braziliensis, no amastigotes in the bone marrow or visceral signs were observed. Dermatological signs such as nodules and papules on the ears and the nose were cured in 32 and 40 week p.i., respectively, and all animals produced antibodies against the parasite (Simões-Mattos et al. 2005). However, it is impossible to characterize the species of Leishmania using only the dermatological signs manifested in clinically affected animals, but they can be used together with other diagnostic tools for differential diagnosis for FeL in endemic areas.
Recently, using molecular and phylogenetic analyses, a study from Portugal showed the presence of the same L. infantum strain found in cats also isolated from humans, dogs, and sand flies (Pereira et al. 2020). Similarly, a recent study in Teresina, Piauí state, Brazil, showed that nucleotide sequences found in L. infantum from a clinically affected cat displayed 100% identity to sequences of L. infantum found in dogs and 98% similarity to sequences of L. infantum found in humans (Batista et al. 2020). This data further supports the argument that cats play an important role in the epidemiology of VL.
Conclusions
Studies on FeL in Brazil reveal widespread infections, but these numbers may be underestimated due to scarce data from other macroregions of the country. Many questions still need to be answered for a better understanding of FeL dynamics and its relationship to canine and human VL. Therefore, the tracking and identification of infections in cats (at the level of species) using the most effective epidemiological and diagnostic methods are extremely important for a better understanding of their the role in disease and transmission cycle in Brazil, especially in localities that are historically endemic for human and canine leishmaniasis but have few or no recorded cases of FeL.
Acknowledgements
RTF is a research fellow (Bolsa de Produtividade em Pesquisa) from the Brazilian National Council of Research (CNPq).
Author contribution
LFJN: conceptualization, investigation, methodology, writing — original draft. TMC: investigation, methodology, writing — original draft. DSG: investigation, methodology, writing — original draft. ACAG: writing — original draft. VFSL: writing — review and editing. RS: writing — review and editing. SJ: writing — review and editing. RTF: conceptualization, writing — review and editing. SSD: conceptualization, writing — review and editing. All authors read and approved the final manuscript.
Funding
Financial support was received from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior — Brasil (CAPES—Finance Code 001) and FAPITEC/SE — Fundação de Apoio à Pesquisa e Inovação Tecnológica do Estado de Sergipe (Grant CAPES/FAPITEC 11/2016 — PROEF, Processo 88881.157453/2017–01).
Declarations
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ricardo T. Fujiwara, Email: rtfujiwara@gmail.com
Silvio S. Dolabella, Email: dolabellaufs@gmail.com
References
- Abramo F, Albanese F, Gattuso S, Randone A, Fileccia I, Dedola C, Ibba F, Ottaianoo P, Brianti E. Skin lesions in Feline leishmaniosis: a systematic review. Pathogens. 2021;10:472. doi: 10.3390/pathogens10040472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhtardanesh B, Kheirandish R, Sharifi I, Mohammadi A, Mostafavi A, Mahmoodi T, Primeiro-Luiz Ebrahimi M. Low susceptibility of domestic cats to experimental Leishmania infantum infection. J Vector Borne Dis. 2018;55:230–234. doi: 10.4103/0972-9062.249481. [DOI] [PubMed] [Google Scholar]
- Akhtardanesh B, Moeini E, Sharifi I, Saberi M, Sadeghi B, Ebrahimi M, Otranto D. Leishmania infection in cats positive for immunodeficiency virus and feline leukemia virus in an endemic region of Iran. Vet Parasitol Reg Stud Reports. 2020;20:100387. doi: 10.1016/j.vprsr.2020.100387. [DOI] [PubMed] [Google Scholar]
- Alcover MM, Basurco A, Fernandez A, Riera C, Fisa R, Gonzalez A, Verde M, Garrido AM, Ruíz H, Yzuel A, Villanueva-Saz S. A cross-sectional study of Leishmania infantum infection in stray cats in the city of Zaragoza (Spain) using serology and PCR. Parasit Vectors. 2021;14:1–14. doi: 10.1186/s13071-021-04682-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, Boer M. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7:e35671. doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asfaram S, Fakhar M, Teshnizi SH. Is the cat an important reservoir host for visceral leishmaniasis? A systematic review with meta-analysis. J Venom Anim Toxins Incl Trop Dis. 2019;25:1–10. doi: 10.1590/1678-9199-JVATITD-2019-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asgari Q, Mohammadpour I, Bozorg-Ghalati F, Motazedian MH, Kalantari M, Hosseini S. Alarming: high prevalence of Leishmania infantum infection in cats from southern Iran based on molecular and serological methods. Ann Parasitol. 2020;66:143–156. doi: 10.17420/ap6602.249. [DOI] [PubMed] [Google Scholar]
- Baneth G, Nachum-Biala Y, Zuberi A, Zipori-Barki N, Orshan L, Kleinerman G, Shmueli-Goldin A, Bellaiche M, Leszkowicz-Mazuz M, Salant H, Yasur-Landau D. Leishmania infection in cats and dogs housed together in an animal shelter reveals a higher parasite load in infected dogs despite a greater seroprevalence among cats. Parasit Vectors. 2020;13:4–11. doi: 10.1186/s13071-020-3989-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batista JF, Neto FDCRM, Lopes KSPDP, Sato MO, Costa CHN, Mendonça IL. Transmission of Leishmania infantum from cats to dogs. Rev Bras Parasitol Vet. 2020;29:1–11. doi: 10.1590/S1984-29612020099. [DOI] [PubMed] [Google Scholar]
- Benassi JC, Benvenga GU, Ferreira HL, Pereira VF, Keid LB, Soares R, Oliveira TMFS. Detection of Leishmania infantum DNA in conjunctival swabs of cats by quantitative real-time PCR. Exp Parasitol. 2017;177:93–97. doi: 10.1016/j.exppara.2017.04.004. [DOI] [PubMed] [Google Scholar]
- Berenguer LKAR, Gomes CFCA, Nascimento JO, Bernardi JCM, Lima VFS, Oliveira JB, Ramos CAN, Ramos RAN, Alves LC. Leishmania infantum infection in a domestic cat: a real threat or an occasional finding? Acta Parasitol. 2020;66:673–676. doi: 10.1007/s11686-020-00294-z. [DOI] [PubMed] [Google Scholar]
- Bezerra JAB, Oliveira IVPM, Yamakawa AC, Nilsson MG, Tomaz KLR, Oliveira KDS, Rocha CS, Calabuig CIP, Fornazari F, Langoni H, Antunes JMAP. Serological and molecular investigation of Leishmania spp. infection in cats from an area endemic for canine and human leishmaniasis in northeast Brazil. Rev Bras Parasitol Vet. 2019;28:790–796. doi: 10.1590/S1984-29612019082. [DOI] [PubMed] [Google Scholar]
- Brianti E, Falsone L, Napoli E, Gaglio G, Giannetto S, Pennisi MG, Priolo V, Latrofa MS, Taralloo VD, Basano FS, Nazzari R, Deuster K, Pollmeier M, GulottaL Colella V, Dantas-Torres F, Capelli G, Otranto D. Prevention of feline leishmaniosis with an imidacloprid 10%/flumethrin 4.5% polymer matrix colar. Parasit Vectors. 2017;10:334. doi: 10.1186/s13071-017-2258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brianti E, Celi N, Napoli E, Arfuso AJM, F, Gaglioo G, Iatta R, Giannetto S, Gramiccia M, Otranto D, Treatment and long-term follow-up of a cat with leishmaniosis. Parasit Vectors. 2019;12:121. doi: 10.1186/s13071-019-3388-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga ARC, Corrêa APFL, Camossi LG, Silva RCD, Langoni H, Lucheis SB. Coinfection by Toxoplasma gondii and Leishmania spp. in domestic cats (Felis catus) in State of Mato Grosso do Sul. Rev Soc Bras Med Trop. 2014;47:796–797. doi: 10.1590/0037-8682-0041-2014. [DOI] [PubMed] [Google Scholar]
- Braga ARC, Langoni H, Lucheis SB. Evaluation of canine and feline leishmaniasis by the association of blood culture, immunofluorescent antibody test and polymerase chain reaction. J Venom Anim Toxins Incl Trop Dis. 2014;20:1–7. doi: 10.1186/1678-9199-20-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brasil (2014) Manual de vigilância e controle da leishmaniose visceral. Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Vigilância Epidemiológica. Brasília: Editora do Ministério da Saúde. https://www.paho.org/bra/index.php?option=com_docman&view=document&slug=manual-vigilancia-e-controle-da-leishmaniose-visceral-2&layout=default&alias=1462-manual-vigilancia-econtrole-da-leishmaniose-visceral-2&category_slug=leishmanioses-978&Itemid=965. Accessed 30 Jul 2020
- Bresciani KDS, Serrano ACM, Matos LVS, Savani ESMM, D’Auria SRN, Perri SHV, Bonello FL, Coelho WMD, Aoki CG, Costa AJ. Occurrence de Leishmania spp. in domestic cats from Araçatuba. SP Rev Bras Parasitol Vet. 2010;19:127–129. doi: 10.4322/rbpv.01902012. [DOI] [PubMed] [Google Scholar]
- Burza S, Croft SL, Boelaert M. Leishmaniasis Lancet. 2018;392:951–970. doi: 10.1016/S0140-6736(18)31204-2. [DOI] [PubMed] [Google Scholar]
- Can H, Doskaya M, Ozdemir HG, Sahar EA, Karakavuk M, Pektas B, Karakus M, Toz S, Caner A, Doskaya AD, Iz SG, Ozbel Y, Guruz Y. Seroprevalence of Leishmania infection and molecular detection of Leishmania tropica and Leishmania infantum in stray cats of İzmir, Turkey. Exp Parasitol. 2016;167:109–114. doi: 10.1016/j.exppara.2016.05.011. [DOI] [PubMed] [Google Scholar]
- Cardia DFF, Camossi LG, Neto LS, Langoni H, Bresciani KDS. Prevalence of Toxoplasma gondii and Leishmania spp. infection in cats from Brazil. Vet Parasitol. 2013;197:634–637. doi: 10.1016/j.vetpar.2013.07.017. [DOI] [PubMed] [Google Scholar]
- Cardoso L, Lopes AP, Sherry K, Schallig H, Solano-Gallego L. Low seroprevalence of Leishmania infantum infection in cats from northern Portugal based on DAT and ELISA. Vet Parasitol. 2010;174:37–42. doi: 10.1016/j.vetpar.2010.08.022. [DOI] [PubMed] [Google Scholar]
- Carneiro LA, Santos TV, Lima LVR, Ramos PKS, Campos MB, Silveira FT. First report on feline leishmaniasis caused by Leishmania (Leishmania) amazonensis in Amazonian Brazil. Vet Parasitol Reg Stud Reports. 2020;19:100360. doi: 10.1016/j.vprsr.2019.100360. [DOI] [PubMed] [Google Scholar]
- Chatzis MK, Andreadou M, Leontides L, Kasabalis D, Mylonakis M, Koutinas AF, Rallis T, Ikonomopoulos J, Saridomichelakis MN. Cytological and molecular detection of Leishmania infantum in different tissues of clinically normal and sick cats. Vet Parasitol. 2014;202:217–225. doi: 10.1016/j.vetpar.2014.02.044. [DOI] [PubMed] [Google Scholar]
- Coelho WMD, Lima VMF, Amarante AFT, Langoni H, Pereira VBR, Abdelnour A, Bresciani KDS. Occurrence of Leishmania (Leishmania) chagasi in a domestic cat (Felis catus) in Andradina, São Paulo, Brazil: case report. Brazilian Journal of Vet Parasitol. 2010;19:256–258. doi: 10.1590/s1984-29612010000400013. [DOI] [PubMed] [Google Scholar]
- Coelho WMD, Richini-Pereira VB, Langoni H, Bresciani KDS. Molecular detection of Leishmania sp. in cats (Felis catus) from Andradina Municipality, São Paulo State. Brazil Vet Parasitol. 2011;176:281–282. doi: 10.1016/j.vetpar.2010.10.052. [DOI] [PubMed] [Google Scholar]
- Coelho WMD, Amarante AFT, Apolinário JC, Coelho NMD, Lima VMF, Perri SHV, Bresciani KDS. Seroepidemiology of Toxoplasma gondii, Neospora caninum, and Leishmania spp. infections and risk factors for cats from Brazil. Parasitol Res. 2011;109:1009–1013. doi: 10.1007/s00436-011-2461-. [DOI] [PubMed] [Google Scholar]
- Costa-Val APD, Coura FM, Barbieri JM, Diniz L, Sampaio A, Reis JKP, Bueno BL, Gontijo CMF. Serological study of feline leishmaniasis and molecular detection of Leishmania infantum and Leishmania braziliensis in cats (Felis catus) Rev Bras Parasitol Vet. 2020;29:e003520. doi: 10.1590/S1984-29612020023. [DOI] [PubMed] [Google Scholar]
- Coura FM, Passos SKP, Pelegrino MOF, Leme FOP, Paz GF, Gontijo CMF, Costa-Val AP. Serological, molecular, and microscopic detection of leishmania in cats (Felis catus) in Belo Horizonte, Minas Gerais State, Brazil. Rev Bras Parasitol Vet. 2018;27:570–574. doi: 10.1590/S1984-296120180052. [DOI] [PubMed] [Google Scholar]
- Dahroug MAA, Almeida ABPF, Sousa VRF, Dutra V, Turbino NCMR, Nakazato L, Souza RL. Leishmania (Leishmania) chagasi in captive wild felids in Brazil. Trans R Soc Trop Med Hyg. 2010;104:73–74. doi: 10.1016/j.trstmh.2009.08.003. [DOI] [PubMed] [Google Scholar]
- Dahroug MAA, Almeida ABPF, Sousa VRF, Dutra V, Guimarães LD, Soares C, Nakazato L, Souza RL. The first case report of Leishmania (leishmania) chagasi in Panthera leo in Brazil. Asian Pac J Trop Biomed. 2011;1:249–250. doi: 10.1016/S2221-1691(11)60036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dantas-Torres F, Brandão-Filho SP. Visceral leishmaniasis in Brazil: Revisiting paradigms of epidemiology and control. Rev Inst Med Trop Sao Paulo. 2006;48:151–156. doi: 10.1590/s0036-46652006000300007. [DOI] [PubMed] [Google Scholar]
- Day MJ. Cats are not small dogs: Is there an immunological explanation for why cats are less affected by arthropod-borne disease than dogs? Parasit Vectors. 2016;9:507. doi: 10.1186/s13071-016-1798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diakou A, Papadopoulos E, Lazarides K. Specific anti-Leishmania spp. antibodies in stray cats in Greece. J Feline Med Surg. 2009;11:728–730. doi: 10.1016/j.jfms.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Gallego A, Bernabe LF, Dalmau A, Esteban-Saltiveri D, Font A, Leiva M, Ortuñez-Navarro A, Peña MT, Tabar MD, Real-Sampietro L, Saló F, Lloret A, Bardagí M. Feline leishmaniosis: diagnosis, treatment and outcome in 16 cats. J Feline Med Surg. 2020;22:993–1007. doi: 10.1177/1098612X20902865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueiredo FB, Bonna ICF, Nascimento LD, Costa T, Baptista C, Pacheco TMV, Amendoeira MRR, Madeira MDF. Serological evaluation for detection of anti-Leishmania antibodies in dogs and cats in the district of Santa Rita de Cássia, municipality of Barra Mansa, State of Rio de Janeiro. Rev Soc Bras Med Trop. 2009;42:141–145. doi: 10.1590/s0037-86822009000200009. [DOI] [PubMed] [Google Scholar]
- Giannakopoulos A, Tsokana CN, Papadopoulos E, Chatzopoulos DC, Valiakos G, Touloudi A, Athanasiou LV, Billinis C. Molecular investigation and geographical distribution of Leishmania spp. infection in stray and owned cats (Felis catus) in Thessaly, central Greece. J Hellenic Vet Med Soc. 2017;68:027–034. doi: 10.12681/jhvms.15553. [DOI] [Google Scholar]
- Hartmann K. Clinical aspects of feline retroviruses: a review. Viruses. 2012;4:2684–2710. doi: 10.3390/v4112684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headley SA, Pimentel LA, Amorim IFG, Amude AM, Viana NE, Muraro LS, Tafuri WL, Santos MD. Immunohistochemical characterization of cutaneous leishmaniasis in cats from central-west Brazil. Vet Parasitol Reg Stud Reports. 2019;17:100290. doi: 10.1016/j.vprsr.2019.100290. [DOI] [PubMed] [Google Scholar]
- Iatta R, Furlanello T, Colella V, Tarallo VD, Latrofa MS, Brianti E, Trerotoli P, Decaro N, Lorusso E, Schunack B, Mirò G, Dantas-Torres F, Otranto D. A nationwide survey of Leishmania infantum infection in cats and associated risk factors in Italy. PLoS Negl Trop Dis. 2019;13:e0007594. doi: 10.1371/journal.pntd.0007594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iatta R, Trerotoli P, Lucchese L, Natale A, Buonavoglia C, Nachum-Biala Y, Baneth G, Otranto D. Validation of a new immunofluorescence antibody test for the detection of Leishmania infantum infection in cats. Parasitol Res. 2020;119:1381–1386. doi: 10.1007/s00436-020-06627-1. [DOI] [PubMed] [Google Scholar]
- Lachaud L, Marchergui-Hammami S, Chabbert E, Dereure J, Luix UM, Debet JP, Bastien P. Comparison of six PCR methods using peripheral blood for detection of canine visceral leishmaniasis. J Clin Microbiol. 2002;40:210–215. doi: 10.1128/JCM.40.1.210-215.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonel JAF, Vioti V, Alves ML, Benassi JC, Silva DT, Spada JCP, Ruiz VLA, Starke-Buzetti WA, Soares RM, Oliveira TMFS. Leishmaniasis in cat shelters: a serological, molecular and entomological study. Trans Emer Dis. 2020;00:1–7. doi: 10.1111/tbed.13544. [DOI] [PubMed] [Google Scholar]
- Lima BS, Dantas-Torres F, Carvalho MR, Marinho-Junior JF, Almeida EL, Brito MEF, Gomes F, Brandão-Filho SP. Small mammals as hosts of Leishmania spp. in a highly endemic area for zoonotic leishmaniasis in north-eastern Brazil. Trans R Soc Trop Med Hyg. 2013;107:592–597. doi: 10.1093/trstmh/trt062. [DOI] [PubMed] [Google Scholar]
- Madruga G, Ribeiro AP, Ruiz T, Sousa VRF, Campos CG, Almeida ABPF, Pescador CA, Dutra V. Ocular manifestations of leishmaniasis in a cat: first case report from Brazil. Arq Bras Med Vet Zootec. 2018;70:1514–1520. doi: 10.1590/1678-4162-9244. [DOI] [Google Scholar]
- Maia C, Ramos C, Coimbra M, Cardoso L, Campino L. Prevalence of Dirofilaria immitis antigen and antibodies to Leishmania infantum in cats from southern Portugal. Parasitol Int. 2015;64:154–156. doi: 10.1016/j.parint.2014.11.006. [DOI] [PubMed] [Google Scholar]
- Marcondes M, Hirata KY, Vides JP, Sobrinho LSV, Azevedo JS, Vieira TSWJ, Vieira RFC. Infection by Mycoplasma spp., feline immunodeficiency virus and feline leukemia virus in cats from an area endemic for visceral leishmaniasis. Parasit Vectors. 2018;11:131. doi: 10.1186/s13071-018-2716-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchi MNA, Caldart ET, Martins FDC, Freire RL. Spatial analysis of leishmaniasis in Brazil: a systematized review. Rev Inst Med Trop Sao Paulo. 2019;61:e68. doi: 10.1590/S1678-9946201961068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matos AMRN, Caldart ET, Ferreira FP, Monteiro KC, Souza M, Brunieri DTSC, Hilst CLS, Mascarenhas NMF, Mitsuka-Breganó R, Freire RL, Navarro IT. Antibodies anti-trypanosomatides in domestic cats in Paraná: who is at highest risk of infection? Rev Bras Parasitol Vet. 2018;27:232–236. doi: 10.1590/s1984-296120180033. [DOI] [PubMed] [Google Scholar]
- Mendonça IL, Batista JF, Lopes KSPP, Magalhães-Neto FCR, Alcântara DS, Merigueti YFFB, Costa CHN. Infection of Lutzomyia longipalpis in cats infected with Leishmania infantum. Vet Parasitol. 2020;280:109058. doi: 10.1016/j.vetpar.2020.109058. [DOI] [PubMed] [Google Scholar]
- Metzdorf IP, Costa-Lima MS, Matos FCM, Souza-Filho AF, Souza-Tsujisaki RA, Franco KG, Shapiro JT, Almeida-Borges F. Molecular characterization of Leishmania infantum in domestic cats in a region of Brazil endemic for human and canine visceral leishmaniasis. Acta Trop. 2017;166:121–125. doi: 10.1016/j.actatropica.2016.11.013. [DOI] [PubMed] [Google Scholar]
- Miró G, Rupérez C, Checa R, Gálvez R, Hernández L, García M, Canorea I, Marino V, Montoya A. Current status of L. infantum infection in stray cats in the Madrid region (Spain): implications for the recent outbreak of human leishmaniosis? Parasit Vectors. 2014;7:112. doi: 10.1186/1756-3305-7-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morais RCS, Gonçalves SC, Costa PL, Silva KG, Silva FJ, Silva RP, Brito MEF, Brandão-Filho SP, Dantas-Torres F, Paiva-Cavalcanti M. Detection of Leishmania infantum in animals and their ectoparasites by conventional PCR and real time PCR. Exp Appl Acarol. 2013;59:473–481. doi: 10.1007/s10493-012-9611-4. [DOI] [PubMed] [Google Scholar]
- Neto LS, Sobrinho LSV, Martins CO, Machado RZ, Marcondes M, Lima VMF. Use of crude, FML and rK39 antigens in ELISA to detect anti-Leishmania spp. antibodies in Felis catus. Vet Parasitol. 2011;177:374–377. doi: 10.1016/j.vetpar.2010.11.055. [DOI] [PubMed] [Google Scholar]
- Oliveira GC, Paiz LM, Menozzi BD, Lima MS, Moraes CCG, Langoni H. Antibodies to Leishmania spp. in domestic felines. Rev Bras Parasitol Vet. 2015;24:464–470. doi: 10.1590/S1984-29612015071. [DOI] [PubMed] [Google Scholar]
- Oliveira TMF, Pereira VF, Benvenga GU, Martin MFA, Benassi JC, Silva DT, Starke-Buzetti WA. Conjunctival swab PCR to detect Leishmania spp. in cats. Rev Bras Parasitol Vet. 2015;24:220–222. doi: 10.1590/S1984-29612015016. [DOI] [PubMed] [Google Scholar]
- Otranto D, Napoli E, Latrofa MS, Annoscia G, Tarallo VD, Greco G, Lorusso E, Gulotta L, Falsone L, Basano FS, Pennisi MG, Deuster K, Capelli G, Dantas-Torres F, Brianti E. Feline and canine leishmaniosis and other vector-borne diseases in the Aeolian Islands: pathogen and vector circulation in a confined environment. Vet Parasitol. 2017;236:144–151. doi: 10.1016/j.vetpar.2017.01.019. [DOI] [PubMed] [Google Scholar]
- Passos VM, Lasmar EB, Gontijo CM, Fernandes O, Degrave W. Natural infection of a domestic cat (Felis domesticus) with Leishmania (Viannia) in the metropolitan region of Belo Horizonte, State of Minas Gerais, Brazil. Mem Inst Oswaldo Cruz. 1996;91:19–20. doi: 10.1590/s0074-02761996000100003. [DOI] [PubMed] [Google Scholar]
- Paşa S, Tetik Vardarlı A, Erol N, Karakuş M, Töz S, Atasoy A, Balcıoğlu İC, Emek Tuna G, Ermiş ÖV, Ertabaklar H, Özbel Y. Detection of Leishmania major and Leishmania tropica in domestic cats in the Ege Region of Turkey. Vet Parasitol. 2015;212:389–392. doi: 10.1016/j.vetpar.2015.07.042. [DOI] [PubMed] [Google Scholar]
- Pedrassani D, Biolchi J, Gonçalves LR, Mendes NS, Zanatto DCS, Calchi AC, Machado RZ, André MR. Molecular detection of vector-borne agents in cats in Southern Brazil. Rev Bras Parasitol Vet. 2019;28:632–643. doi: 10.1590/S1984-29612019077. [DOI] [PubMed] [Google Scholar]
- Pennisi MG, Hartmann K, Lloret A, Addie D, Belák S, Boucraut-Baralon C, Egberink H, Frymus T, Gruffydd-Jones T, Hosie MJ, Lutz H, Marsilio F, Möstl K, Radford AD, Thiry E, Truyen U, Horzinek MC. Leishmaniosis in cats: ABCD guidelines on prevention and management. J Feline Med Surg. 2013;15:638–642. doi: 10.1177/1098612X13489229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennisi MG, Cardoso L, Baneth G, Bourdeau P, Koutinas A, Miró G, Oliva G, Solano-Gallego L. LeishVet update and recommendations on feline leishmaniosis. Parasit Vectors. 2015;8:1–18. doi: 10.1186/s13071-015-0909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennisi MG. Leishmaniosis of companion animals in Europe: an update. Vet Parasitol. 2015;208:35–47. doi: 10.1016/j.vetpar.2014.12.023. [DOI] [PubMed] [Google Scholar]
- Pennisi MG, Persichetti MF. Feline leishmaniosis: is the cat a small dog? Vet Parasitol. 2018;251:131–137. doi: 10.1016/j.vetpar.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira A, Parreira R, Cristóvão JM, Castelli G, Bruno F, Vitale F, Campino L, Maia C. Phylogenetic insights on Leishmania detected in cats as revealed by nucleotide sequence analysis of multiple genetic markers. Infect Genet Evol. 2020;77:104069. doi: 10.1016/j.meegid.2019.104069. [DOI] [PubMed] [Google Scholar]
- Persichetti MF, Solano-Gallego L, Vullo A, Masucci M, Marty P, Delaunay P, Vitale F, Pennisi MG. Diagnostic performance of ELISA, IFAT and Western blot for the detection of anti-Leishmania infantum antibodies in cats using a Bayesian analysis without a gold standard. Parasit Vectors. 2017;10:119. doi: 10.1186/s13071-017-2046-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poffo D, Almeida ABPF, Nakazato L, Dutra V, Correa SHR, Mendonça AJ, Sousa VRF. Feline immunodeficiency virus (FIV), feline leukaemia virus (FeLV) and Leishmania sp. in domestic cats in the Midwest of Brazil. Pesq Vet Bras. 2017;37:491–494. doi: 10.1590/S0100-736X2017000500011. [DOI] [Google Scholar]
- Priolo V, Martínez-Orellana P, Pennisi MG, Masucci M, Prandi D, Ippolito D, Bruno F, Castelli G, Solano-Gallego L. Leishmania infantum-specific IFN-γ production in stimulated blood from cats living in areas where canine leishmaniosis is endemic. Parasit Vectors. 2019;12:133. doi: 10.1186/s13071-019-3386-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimão JQ, Coser EM, Lee MR, Coelho AC. Laboratory diagnosis of cutaneous and visceral leishmaniasis: current and future methods. Microorganisms. 2020;8:1–30. doi: 10.3390/microorganisms8111632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis LL, Balieiro AAS, Fonseca FR, Gonçalves MJF. Changes in the epidemiology of visceral leishmaniasis in Brazil from 2001 to 2014. Rev Soc Bras Med Trop. 2017;50:638–645. doi: 10.1590/0037-8682-0243-2017. [DOI] [PubMed] [Google Scholar]
- Ribeiro RR, Michalick MSM, Silva ME, Santos CCP, Frézard FJG, Silva SM. Canine leishmaniasis: an overview of the current status and strategies for control. Biomed Res Int. 2018;2018:3296893. doi: 10.1155/2018/3296893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivas AK, Alcover M, Martínez-Orellana P, Montserrat-Sangrà S, Nachum-Biala Y, Bardagí M, Fisa R, Riera C, Baneth G, Solano-Gallego L. Clinical and diagnostic aspects of feline cutaneous leishmaniosis in Venezuela. Parasit Vectors. 2018;11:141. doi: 10.1186/s13071-018-2747-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha AVVO, Moreno BFS, Cabral AD, Louzeiro NM, Miranda LM, Santos VMB, Costa FB, Nogueira RMS, Marcili A, Sperança MA, Costa AP. Diagnosis and epidemiology of Leishmania infantum in domestic cats in an endemic area of the Amazon region, Brazil. Vet Parasitol. 2019;273:80–85. doi: 10.1016/j.vetpar.2019.08.007. [DOI] [PubMed] [Google Scholar]
- Savani ESMM, Oliveira-Camargo MCG, Carvalho MR, Zampieri RA, Santos MG, D’Áuria SRN, Shaw JJ, Floeter-Winter LM. The first record in the Americas of an autochthonous case of Leishmania (Leishmania) infantum chagasi in a domestic cat (Felix catus) from Cotia County, São Paulo State, Brazil. Vet Parasitol. 2004;120:229–233. doi: 10.1016/j.vetpar.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Schubach TMP, Figueiredo FB, Pereira SA, Madeira MF, Santos IB, Andrade MV, Cuzzi T, Marzochi MCA, Schubach A. American cutaneous leishmaniasis in two cats from Rio de Janeiro, Brazil: first report of natural infection with Leishmania (Viannia) braziliensis. Trans R Soc Trop Med Hyg. 2004;98:165–167. doi: 10.1016/s0035-9203(03)00040-3. [DOI] [PubMed] [Google Scholar]
- Silva RCN, Ramos RAN, Pimentel DS, Oliveira GMA, Carvalho GA, Santana MA, Faustino MAG, Alves LC. Detection of antibodies against Leishmania infantum in cats (Felis catus) from the state of Pernambuco, Brazil. Rev Soc Bras Med Trop. 2014;47:108–109. doi: 10.1590/0037-8682-0005-2012. [DOI] [PubMed] [Google Scholar]
- Silva AVM, Souza-Cândido CD, Pita-Pereira D, Brazil RP, Carreira JCA. The first record of American visceral leishmaniasis in domestic cats from Rio de Janeiro, Brazil. Acta Trop. 2008;105:92–94. doi: 10.1016/j.actatropica.2007.09.001. [DOI] [PubMed] [Google Scholar]
- Silva RBS, Portela RA, Arruda LFB, Ferreira JS, Souto EPF, Araújo AL, Madeira MF, Dantas AFM, Melo MA. Natural Infection by Leishmania infantum in domestic cats (Felis catus) in a municipality of moderate transmission in the Brazilian semi-arid region. Rev Bras Parasitol Vet. 2020;29:e016620. doi: 10.1590/S1984-29612020102. [DOI] [PubMed] [Google Scholar]
- Silva SM, Rabelo PFB, Gontijo NF, Ribeiro RR, Melo MN, Ribeiro VM, Michalick MSM. First report of infection of Lutzomyia longipalpis by Leishmania (Leishmania) infantum from a naturally infected cat of Brazil. Vet Parasitol. 2010;174:150–154. doi: 10.1016/j.vetpar.2010.08.005. [DOI] [PubMed] [Google Scholar]
- Simões-Mattos L, Mattos MRF, Teixeira MJ, Oliveira-Lima JW, Bevilaqua CML, Prata RC, Holanda CM, Rondon FCM, Bastos KMS, Coêlho ZCB, Coêlho ICB, Barral A, Pompeu MML. The susceptibility of domestic cats (Felis catus) to experimental infection with Leishmania braziliensis. Vet Parasitol. 2005;127:199–208. doi: 10.1016/j.vetpar.2004.10.008. [DOI] [PubMed] [Google Scholar]
- Soares CSA, Duarte SC, Sousa SR. What do we know about feline leishmaniosis? J Feline Med Surg. 2015;18:435–442. doi: 10.1177/1098612X15589358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobrinho LSV, Rossi CN, Vides JP, Braga ET, Gomes AAD, Lima VMF, Perri SHV, Generoso D, Langoni H, Leutenegger C, Biondo AW, Laurenti MD, Marcondes M. Coinfection of Leishmania chagasi with Toxoplasma gondii, feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV) in cats from an endemic area of zoonotic visceral leishmaniasis. Vet Parasitol. 2012;187:302–306. doi: 10.1016/j.vetpar.2012.01.010. [DOI] [PubMed] [Google Scholar]
- Solano-Gallego L, Rodríguez-Cortés A, Iniesta L, Quintana J, Pastor J, Espada Y, Portús M, Alberola J. Cross-sectional serosurvey of feline leishmaniasis in ecoregions around the Northwestern Mediterranean. Am J Trop Med Hyg. 2007;76:676–680. doi: 10.4269/ajtmh.2007.76.676. [DOI] [PubMed] [Google Scholar]
- Solano-Gallego L, Montserrrat-Sangrà S, Ordeix L, Martínez-Orellana P. Leishmania infantum-specific production of IFN-γ and IL-10 in stimulated blood from dogs with clinical leishmaniosis. Parasit Vectors. 2016;9:317. doi: 10.1186/s13071-016-1598-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa KCM, Herreira HM, Domingos IH, Campos JBV, Santos IMC, Neves HH, Machado RZ, André MR (2014) Serological detection of Toxoplasma gondii, Leishmania infantum and Neospora caninum in cats from an area endemic for leishmaniasis in Brazil. Rev Bras Parasitol Vet 23:449–455. 10.1590/S1984-29612014078 [DOI] [PubMed]
- Souza AI, Barros EMS, Ishikawa E, Novaes-Ilha IM, Barbosa-Marin GR, Brandão-Nunes VL. Feline leishmaniasis due to Leishmania (Leishmania) amazonensis in Mato Grosso do Sul State, Brazil. Vet Parasitol. 2005;128:41–45. doi: 10.1016/j.vetpar.2004.11.020. [DOI] [PubMed] [Google Scholar]
- Spada E, Canzi I, Baggiani L, Perego R, Vitale F, Migliazzo A, Proverbio D. Prevalence of Leishmania infantum and co-infections in stray cats in northern Italy. Comp Immunol Microbiol Infect Dis. 2016;45:53–58. doi: 10.1016/j.cimid.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spada E, Perego R, Vitale F, Bruno F, Castelli G, Tarantola G, Baggiani L, Magistrelli S, Proverbio D. Feline Leishmania spp. infection in a non-endemic area of northern Italy. Animals. 2020;10:817. doi: 10.3390/ani10050817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolentino N, Pinheiro GRG, Ottino J, Oliveira AR, Coelho CM, Tinoco HP, Fujiwara RT, Santos RL, Ribeiro VM. Serological evidence of Leishmania infection by employing ELISA and rapid tests in captive felids and canids in Brazil. Vet Parasitol Reg Stud Reports. 2019;17:100308. doi: 10.1016/j.vprsr.2019.100308. [DOI] [PubMed] [Google Scholar]
- Tomiotto-Pellissier F, Bortoleti BTS, Assolini JP, Gonçalves MD, Carloto ACM, Miranda-Sapla MM, Conchon-Costa I, Bordignon J, Pavanelli WR. Macrophage polarization in leishmaniasis: broadening horizons. Front Immunol. 2018;9:2529. doi: 10.3389/fimmu.2018.02529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trevisan DAC, Lonardoni MVC, Demarchi IG. Diagnostic methods to cutaneous leishmaniasis detection in domestic dogs and cats. An Bras Dermatol. 2015;90:868–872. doi: 10.1590/abd1806-4841.20153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbani L, Tirolo A, Salvatore D, Tumbarello M, Segatore S, Battilani M, Balboni A, Dondi F. Serological, molecular and clinicopathological findings associated with Leishmania infantum infection in cats in Northern Italy. J Feline Med Surg. 2020;22:935–943. doi: 10.1177/1098612X19895067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veasey JV, Zampieri RA, Lellis RF, Freitas THP, Winter LMF. Identification of Leishmania species by high-resolution DNA dissociation in cases of American cutaneous leishmaniasis. An Bras Dermatol. 2020;4:459–468. doi: 10.1016/j.abd.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vides JP, Schwardt TF, Sobrinho LSV, Marinho M, Laurenti MD, Biondo AW, Leutenegger C, Marcondes M. Leishmania chagasi infection in cats with dermatologic lesions from an endemic area of visceral leishmaniosis in Brazil. Vet Parasitol. 2011;178:22–28. doi: 10.1016/j.vetpar.2010.12.042. [DOI] [PubMed] [Google Scholar]
- Werneck GL. Geographic spread of visceral leishmaniasis in Brazil. Cad Saúde Pública. 2010;26:644–645. doi: 10.1590/s0102-311x2010000400001. [DOI] [PubMed] [Google Scholar]
- WHO (2016) Leishmaniasis in high-burden countries: an epidemiological update based on data reported in 2014. Geneva: World Health Organization. Weekly Epidemiological Record 91:285–296. https://www.who.int/publications/i/item/who-wer9122. Accessed 30 Oct 2020 [PubMed]
- WHO (2020) Global leishmaniasis surveillance, 2017–2018, and first report on 5 additional indicators. Geneva: World Health Organization. Weekly Epidemiological Record 25:265–280. https://www.who.int/publications/i/item/who-wer9525. Accessed 23 Nov 2020