Abstract
Objective
To describe the contemporary trends in total, inpatient, and outpatient expenditure on major subtypes of cancer in different classifications of hospitals in mainland China.
Methods
Home page of Inpatient Medical Records (HIMRs) and Hospital Annual Reports (HARs) were used to estimate hospital care expenditure on cancer. Inpatient payments and their share of cancer were calculated with the top-down method. Kriging spatial interpolation methods were used at the county level and summed at the province level. Outpatient expenditure was estimated with inpatient expenditure and the ratios of outpatient to inpatient payments in specialized cancer hospitals, stratified by province. Total expenditure on cancer was the sum of both payments. Log-linear regression was applied to estimate annual percentage change (APC) of expenditure.
Results
Total expenses for cancer of Chinese residents reached up to 304.84 billion Chinese Yuan (CNY) in 2017, accounting for 5.8% of the total health expenses (THE). After adjusting for consumer price index (CPI), medical expenses for cancer have increased from 63.30 billion CNY in 2008 to 249.56 billion CNY in 2017 [APC: 15.2%, 95% confidence interval (95% CI): 13.4%−17.0%]. The APC was slightly higher than THE around 2013, while was lower after 2013. During 2008−2017, the ratio of inpatient to outpatient costs for cancer decreased from 4.3:1 to 3.8:1. The inpatient payments for cancer mainly happened in grade 3 general hospitals, East China, and among lung, colorectal, and stomach cancer; while the fastest increase was found in West China, and among thyroid, prostate, and colorectal cancer.
Conclusions
During 2008−2017, the rapid growth trend of medical expenses for cancer has been effectively controlled with the continuous deepening of medical reform and improvements of residents’ health care. More attention should be paid to potential increases of medical costs caused by technological progress and demand release. Socialized and multi-channel insurance financing modes should be explored in the future.
Keywords: Cancer, payments, expenditure, economic burden
Introduction
To date, cancer has become a major public health concern worldwide, with an estimation of 305.1 million incident cases, 10.1 million deaths, and 251.4 million disability-adjusted life years (DALYs) lost in 2019 (1). As a country of large population, it was considered that approximately 23.7% of the world’s incident cancer cases, 18.4% of prevalent cases, and 30.2% of cancer deaths arose in China (2). According to the China Health Statistics Yearbook, the mortality rate of malignant tumors increased by 26.3% from 128.0/100,000 in 1990 to 161.6/100,000 in 2019 in urban areas of China; the mortality rate in rural areas increased much faster, from 112.4/100,000 to 161.0/100,000 (3). More specifically, the latest data from cancer registries in China indicated a remarkable increase in disease burdens of colorectal cancer, female breast cancer, cervix cancer and thyroid cancer over the last 15 years, and the cancer burden was predicted to continuously increase in China, with the cancer profile containing both features of developing country and developed country (4).
At the same time, with the continuous expansion of the medical insurance coverage and the continuous improvement of the compensation level, the economic burden of cancer was further stimulated. Thus, it is urgently required to estimate the total expenditure of cancer care in China for understanding the impact of cancer on national budgets, and for allocating prevention and research funds optimally. This study used the data of Hospital Annual Reports (HARs) and Home page of Inpatient Medical Records (HIMRs) datasets to estimate the payments of cancer treatment in China systematically, depicting a picture on how the money was spent on cancer treatments.
Materials and methods
Data sources
Data of HIMR
According to the Statistics Law of the People’s Republic of China and the Statistical Regulation of Health, data of HIMR have been collected since 2008. The data collection process can be roughly divided into three stages. During 2008−2012, 820 sample hospitals (consisting of grade 2 and grade 3 hospitals) were required to report the inpatient information extracted from the HIMR, which is uniformly used in hospitals nationwide. Later in 2013−2015, all the hospitals in grade 2 and above (including those with more than 500 beds) were included. Since 2016, all hospitals have been required to report the data of HIMR. The information of HIMR mainly includes patients’ demographic characteristics, diagnostic codes, surgical codes, treatment results, type of medical insurances, inpatient payments, and other personal hospitalization-related information.
According to the data reporting requirements of Statistical Regulation of Health, all the data of HIMR were reported quarterly through the information reporting system of Health Statistics Network, which is in the charge of the Center of Health Statistics and Information, National Health Commission (CHSI, NHC). The data of HIMR reported by each hospital are firstly reviewed by the CHSI at provincial levels, which give feedback to hospitals for revision and re-submission if there are any incomplete or inaccurate data. Then the checked data are submitted to CHSI, NHC, which further verifies the integrity and accuracy of reported data.
Data of HAR
As is regulated by the Statistics Law of the People’s Republic of China and the Statistical Regulation of Health, all hospitals in China are required to report their basic information annually. The basic information mainly includes hospital-related information such as hospital property, grade, number of staff/beds/equipment, outpatient/inpatient volume, outpatient/inpatient income, medical services, and human resources. The above information is also submitted annually through the information reporting system of the Health Statistics Network.
The quality control of annual report data of medical institutions is also hierarchical. The CHSI in provincial levels checks the quality of HARs firstly. Hospitals failing to pass the quality control are asked to submit relevant information again within the allotted time. Then, at the national level, the CHSI, NHC reviews the quality of the data again and informs each province of the results, which further feeds back to hospitals for correction and collects HARs again. In addition, the CHSI, NHC also holds a Data Quality Review Meeting annually, and carries out regular field supervision to inspect the data quality.
Study design
We applied HIMRs and HARs to estimate the expenditure of hospital care on cancer. We calculated the inpatient payments and their share in cancer with the top-down method by calculating the payments at the county level and summed them at the province level (5). Considering, the underreporting could happen at the county level, which could bring bias to the study, we applied the kriging spatial interpolation methods to fill this gap (6). As for the outpatient expenditure, we calculated the ratios of outpatient to inpatient payments in specialized cancer hospitals among every province, and used ratio and inpatient payments to get the outpatient payments. Finally, we summed up both inpatient and outpatient payments, and came to the total expenditure on cancer. Log-linear regression model was used to calculate the annual percentage change (APC) and its confidence interval (7). We used the overall change and APC to describe the contemporary trends in expenditure.
Statistical analysis
Estimation of cancer inpatient payments
The top-down method was adopted to estimate the inpatient payments of various cancers (5). Considering the fully recorded information of HARs and the comparatively incomplete data of HIMRs, we calculated inpatient payments of cancer based on the total inpatient payments derived from HARs and the ratio of cancer inpatient payments from HIMRs.
Specifically, the inpatient payment of cancer was calculated as:
 |
where
 denoted the inpatient payment of cancer,
denoted the inpatient payment of cancer,
 referred to the 31 provinces (municipalities and autonomous regions) in China;
referred to the 31 provinces (municipalities and autonomous regions) in China;
 represented the proportions of cancer inpatient payments in total inpatient payments across different provinces after spatial interpolation, which was calculated through the data from the HIMR; and
represented the proportions of cancer inpatient payments in total inpatient payments across different provinces after spatial interpolation, which was calculated through the data from the HIMR; and
 represented total inpatient payments in different provinces, which were derived from HAR database.
represented total inpatient payments in different provinces, which were derived from HAR database.
Estimation of outpatient payments
The total outpatient payments in different provinces were estimated as the provincial-specific total inpatient payments multiplied by the provincial-specific ratio of outpatient income to inpatient income, which was estimated according to HARs of cancer specialized hospitals. We simply considered these ratios as ratios of outpatient payments to inpatient payments of cancer treatments among all the hospitals.
To evaluate temporal trends in inpatient and outpatient expenditure for cancer, we estimated APC and its 95% confidence interval (95% CI) by fitting log-linear regression models:
 |
where Yα denoted the inpatient and outpatient expenditure for cancer α, and X was the calendar year between 2008 and 2017.
Thus, the APC of Yα was calculated as:
 |
We calculated APC and the confidence interval with the Joinpoint Regression Program Statistical Software (Desktop Version 4.9.0.0, https://surveillance.cancer.gov/joinpoint/) (7).
Kriging spatial interpolation methods
Considering the significant advantages on approximation degree, extrapolation ability, calculation speed and application scope comparing to other spatial interpolation methods, kriging spatial interpolation method was used to avoid the impact of non-random underreporting at the county level (6). The formula of the kriging method was as follows:
 |
where
 represented the value of counties with hospitals but without the data of HIMRS;
represented the value of counties with hospitals but without the data of HIMRS;
 represented the value of counties having the data of HIMRS;
represented the value of counties having the data of HIMRS;
 represented the number of counties having the data of HIMRS; and
represented the number of counties having the data of HIMRS; and
 represented the weight of
represented the weight of
 th sample point, which was calculated by the covariance function or variance function.
th sample point, which was calculated by the covariance function or variance function.
The kriging interpolation was used to estimate the proportion of cancer inpatient payments in total inpatient payments within those unknown areas at county level. To generate the proportions at the provincial level, the estimates of proportions at county level multiplied by the weighting coefficients were summed up. The weighting coefficients were calculated from the number of hospitals in every county divided by the total number of hospitals in every province. The entire process of interpolation was performed with the ArcGIS software (Version 10.3; Redlands, CA: Environmental Systems Research Institute, Inc.).
Results
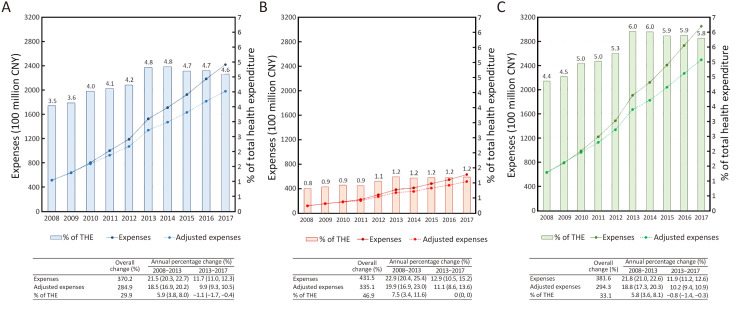
The total expense of cancer in 2017 has reached 304.8 billion Chinese Yuan (CNY) (Table 1 , Figure 1 ). From 2008 to 2017, the overall change of the total expense of cancer was 381.6%, after being adjusted by CPI, the overall change decreased to 294.3%. The percentage of total expense of cancer in total health expenditure (THE) increased from 4.4% in 2008 to 5.8% in 2017 nonlinearly, reaching its maximum value of 6.0% during 2013−2014. Before 2013, the APC (95% CI) of cancer expenses [21.8% (21.0%, 22.6%)] was higher than that of THE [15.7% (14.2%, 17.3%)] (P<0.05); however, after 2013, the APC of cancer expense [11.9% (11.2%, 12.6%)] tended to be similar with that of THE [12.9% (11.9%, 13.8%)] (P=0.10).
Table 1. Total, inpatient, and outpatient expenses of cancer in China during 2008−2017.
| Variables | Expenses of cancer (×100 million) (CNY) | Overall change (%) | APC (95% CI) (%) | ||||||||||
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2008−2013 | 2013−2017 | ||
| THE, total health expenditure; CNY, Chinese Yuan; APC, annual percentage change; 95% CI, 95% confidence interval. | |||||||||||||
| THE | |||||||||||||
| Crude | 14,535.4 | 17,541.9 | 19,980.4 | 24,345.9 | 28,119.0 | 31,669.0 | 35,312.4 | 40,974.6 | 46,344.9 | 52,598.3 | 261.9 | 15.7 (14.2, 17.3) | 12.9 (11.9, 13.8) |
| Adjusted | 14,535.4 | 17,663.0 | 19,468.6 | 22,502.1 | 25,319.1 | 27,785.0 | 30,377.5 | 34,747.6 | 38,526.7 | 43,058.7 | 196.2 | 12.8 (10.8, 14.7) | 11.1 (10.1, 12.2) |
| Inpatient expenses | |||||||||||||
| Crude | 514.6 | 637.4 | 804.3 | 1,002.2 | 1,190.1 | 1,526.4 | 1,710.9 | 1,926.0 | 2,185.0 | 2,419.4 | 370.2 | 21.5 (20.3, 22.7) | 11.7 (11.0, 12.3) |
| Adjusted | 514.6 | 641.8 | 783.7 | 926.3 | 1,071.6 | 1,339.2 | 1,471.8 | 1,633.3 | 1,816.4 | 1,980.6 | 284.9 | 18.5 (16.9, 20.2) | 9.9 (9.3, 10.5) |
| % of THE | 3.5 | 3.6 | 4.0 | 4.1 | 4.2 | 4.8 | 4.8 | 4.7 | 4.7 | 4.6 | 29.9 | 5.9 (3.8, 8.0) | −1.1 (−1.7, −0.4) |
| Outpatient expenses | |||||||||||||
| Crude | 118.4 | 153.0 | 185.0 | 220.5 | 297.5 | 381.6 | 410.6 | 481.5 | 546.3 | 629.0 | 431.5 | 22.9 (20.4, 25.4) | 12.9 (10.5, 15.2) |
| Adjusted | 118.4 | 154.0 | 180.3 | 203.8 | 267.9 | 334.8 | 353.2 | 408.3 | 454.1 | 515.0 | 335.1 | 19.9 (16.9, 23.0) | 11.1 (8.6, 13.6) |
| % of THE | 0.8 | 0.9 | 0.9 | 0.9 | 1.1 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 | 46.9 | 7.5 (3.4, 11.6) | 0 (0, 0) |
| Total expenses | |||||||||||||
| Crude | 633.0 | 790.4 | 989.3 | 1,222.7 | 1,487.6 | 1,908.0 | 2,121.5 | 2,407.5 | 2,731.3 | 3,048.4 | 381.6 | 21.8 (21.0, 22.6) | 11.9 (11.2, 12.6) |
| Adjusted | 633.0 | 795.8 | 964.0 | 1,130.1 | 1,339.5 | 1,674.0 | 1,825.0 | 2,041.6 | 2,270.5 | 2,495.6 | 294.3 | 18.8 (17.3, 20.3) | 10.2 (9.4, 10.9) |
| % of THE | 4.4 | 4.5 | 5.0 | 5.0 | 5.3 | 6.0 | 6.0 | 5.9 | 5.9 | 5.8 | 33.1 | 5.8 (3.6, 8.1) | −0.8 (−1.4, −0.3) |
Figure 1.
Inpatient (A); outpatient (B); and total (C) expenses of cancer in China during 2008−2017. THE, total health expenditure.
In 2017, the inpatient expense of cancer has reached 241.9 billion CNY and the outpatient expense of cancer has reached 62.9 billion CNY. From 2008 to 2017, the overall change of the inpatient expense was 370.2% and that of the outpatient expense was 431.5%. Adjusted by CPI, the overall change of inpatient expense decreased to 284.9% and that of outpatient expense change decreased to 335.1%. The ratios of inpatient expenses over outpatient expenses have changed from 4.3 to 3.8.
In different classifications of hospitals (including grade 2 general hospitals, grade 3 general hospitals and cancer specialized hospitals), the inpatient expenses of cancer in 2017 were 23.0, 155.9 and 41.9 billion CNY, the overall changes from 2008 to 2017 were 147.4%, 449.4%, and 378.2%, respectively (Table 2 ). The APC growth of inpatient expenses of cancer was slower in 2013−2017 compared with 2008−2013 in all kinds of hospitals. In all hospitals, grade 3 general hospitals take up the most proportion of inpatient expenses of cancer. The overall change from 2008 to 2017 is also the fastest in grade 3 general hospitals.
Table 2. Inpatient expenses of cancer in China during 2008−2017.
| Variables | Inpatient expenses (×100 million) (CNY) | Overall
change (%) |
APC (95% CI) (%) | ||||||||||
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2008−2013 | 2013−2017 | ||
| CNY, Chinese Yuan; APC, annual percentage change; 95% CI, 95% confidence interval. | |||||||||||||
| Overall | 514.6 | 637.4 | 804.3 | 1,002.2 | 1,190.1 | 1,526.4 | 1,710.9 | 1,926.0 | 2,185.0 | 2,419.4 | 370.2 | 21.5 (20.3, 22.7) | 11.7 (11.0, 12.3) |
| By subtypes | |||||||||||||
| Nasopharynx cancer | 9.5 | 13.0 | 17.1 | 21.3 | 23.9 | 28.5 | 29.3 | 35.2 | 31.4 | 31.1 | 227.4 | 21.5 (16.5, 26.6) | 2.4 (−5.9, 10.8) |
| Esophagus cancer | 34.9 | 41.3 | 57.9 | 73.9 | 86.0 | 113.0 | 124.0 | 126.6 | 139.8 | 149.7 | 328.9 | 23.8 (20.6, 26.9) | 6.8 (4.8, 8.8) |
| Stomach cancer | 55.0 | 76.2 | 91.4 | 114.4 | 134.2 | 181.6 | 185.6 | 193.8 | 222.6 | 238.4 | 333.5 | 22.6 (19.4, 25.7) | 7.3 (3.5, 11.0) |
| Colorectal cancer | 62.0 | 79.4 | 98.4 | 124.6 | 158.0 | 197.7 | 225.7 | 256.5 | 287.4 | 323.3 | 421.5 | 23.1 (22.7, 23.6) | 12.3 (11.5, 13) |
| Liver cancer | 44.9 | 53.8 | 64.2 | 80.5 | 92.8 | 144.6 | 176.6 | 164.7 | 178.3 | 202.9 | 351.9 | 22.0 (16.3, 27.7) | 6.9 (0, 13.8) |
| Gallbladder carcinoma | 3.6 | 4.6 | 5.5 | 7.8 | 8.1 | 10.9 | 11.8 | 12.9 | 14.3 | 16.0 | 344.4 | 21.7 (17.3, 26.1) | 9.6 (8.4, 10.8) |
| Pancreatic cancer | 11.8 | 14.4 | 18.2 | 22.9 | 26.5 | 33.8 | 36.1 | 39.4 | 47.2 | 52.9 | 348.3 | 20.9 (19.3, 22.5) | 11.6 (7.9, 15.4) |
| Lung cancer | 89.0 | 109.9 | 142.2 | 174.8 | 208.8 | 281.2 | 313.6 | 355.9 | 395.6 | 460.3 | 417.2 | 22.5 (20.6, 24.5) | 12.2 (10.8, 13.5) |
| Breast cancer | 32.8 | 38.6 | 51.3 | 62.9 | 75.1 | 95.1 | 107.3 | 115.7 | 135.6 | 144.9 | 341.8 | 21.5 (19.6, 23.4) | 10.8 (8.4, 13.1) |
| Cervical cancer | 14.5 | 18.3 | 21.9 | 28.5 | 35.2 | 56.0 | 59.1 | 70.0 | 89.7 | 83.7 | 477.2 | 25.7 (19.9, 31.4) | 12.2 (3.5, 20.9) |
| Ovarian cancer | 8.8 | 10.7 | 14.0 | 17.3 | 20.2 | 27.8 | 29.5 | 33.2 | 38.7 | 40.8 | 363.6 | 22.5 (19.9, 25) | 10.4 (7.3, 13.4) |
| Prostatic cancer | 7.1 | 9.3 | 10.7 | 14.1 | 17.8 | 21.5 | 27.1 | 33.9 | 36.5 | 42.1 | 493.0 | 22.2 (20.0, 24.3) | 16.4 (10.6, 22.3) |
| Bladder cancer | 10.5 | 13.6 | 15.3 | 19.3 | 23.9 | 27.9 | 32.8 | 39.8 | 43.5 | 50.1 | 377.1 | 19.5 (17.3, 21.6) | 14.5 (11.5, 17.6) |
| Brain cancer | 13.5 | 15.9 | 18.6 | 22.4 | 25.0 | 37.3 | 41.1 | 43.8 | 56.3 | 67.0 | 396.3 | 18.9 (13.7, 24.2) | 14.9 (8.5, 21.2) |
| Thyroid cancer | 8.6 | 10.8 | 10.7 | 15.5 | 22.0 | 33.5 | 46.8 | 56.2 | 70.3 | 89.5 | 940.7 | 26.6 (16.7, 36.4) | 23.7 (19.6, 27.8) |
| Leukemia | 38.2 | 50.2 | 51.4 | 63.7 | 71.5 | 111.8 | 124.5 | 126.5 | 168.0 | 169.2 | 342.9 | 19.0 (11.6, 26.4) | 11.3 (4.1, 18.5) |
| Others | 69.9 | 77.6 | 115.6 | 138.3 | 161.1 | 124.3 | 140.2 | 221.9 | 229.9 | 257.7 | 268.7 | 15.0 (2.2, 27.8) | 19.5 (7.4, 31.6) |
| By types of hospital | |||||||||||||
| General, grade 2 | 93.0 | 115.2 | 143.5 | 163.4 | 166.8 | 198.7 | 209.5 | 218.2 | 215.6 | 230.1 | 147.4 | 14.4 (9.8, 19.0) | 3.2 (1.2, 5.3) |
| General, grade 3 | 283.8 | 353.9 | 453.6 | 574.2 | 703.2 | 924.1 | 1,046.0 | 1,197.6 | 1,402.1 | 1,559.3 | 449.4 | 23.4 (22.4, 24.5) | 13.4 (12.1, 14.7) |
| Cancer specialized | 87.7 | 108.0 | 132.9 | 170.8 | 213.3 | 261.1 | 305.6 | 350.0 | 389.3 | 419.4 | 378.2 | 22.1 (21.2, 23.0) | 11.9 (8.9, 14.9) |
| Others | 50.1 | 60.3 | 74.3 | 93.8 | 106.8 | 142.5 | 149.8 | 160.2 | 178.0 | 210.6 | 320.4 | 20.5 (18.3, 22.7) | 9.5 (5.2, 13.9) |
| By regions | |||||||||||||
| East China | 333.6 | 403.1 | 509.0 | 620.8 | 719.5 | 884.9 | 1,004.9 | 1,147.7 | 1,326.0 | 1,443.4 | 332.7 | 19.5 (18.0, 21.0) | 12.6 (10.8, 14.3) |
| Middle China | 123.4 | 158.7 | 200.5 | 258.6 | 327.6 | 427.0 | 470.5 | 522.4 | 577.8 | 664.2 | 438.2 | 24.7 (24.1, 25.2) | 10.9 (9.5, 12.3) |
| West China | 57.5 | 75.6 | 94.8 | 122.9 | 142.9 | 214.5 | 235.5 | 255.9 | 281.2 | 311.8 | 442.3 | 25.0 (21.2, 28.8) | 9.3 (8.6, 9.9) |
Inpatient expenses of cancer are 144.34, 66.42 and 31.18 billion CNY in East, Middle and West China, respectively, in 2017. Also, a decline in the growth rate of APC is observed in each region of China when we compare between 2008−2013 and 2013−2017. Inpatient expenses of cancer in East China are the highest among all three regions, while the fastest overall change of inpatient expenses of cancer appears in West China.
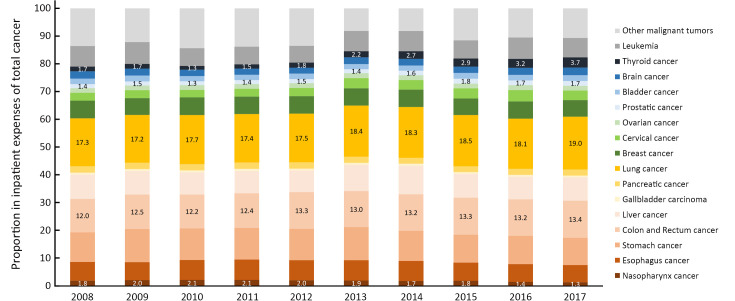
Significant disparity of inpatient expenses was observed across subtypes of cancer, both in levels and in temporal trends. Among all the major subtypes, lung cancer (from 8.90 billion CNY in 2008 to 46.03 billion CNY in 2017), colorectal cancer (from 6.20 billion CNY in 2008 to 32.33 billion CNY in 2017), and stomach cancer (from 5.50 billion CNY in 2008 to 23.84 billion CNY in 2017) remained the top 3 contributors to cancer inpatient payments during 2008−2017, which in total accounted for more than 40% of the entire expenses (Figure 2 ). Subtypes including liver cancer, leukemia, esophagus cancer, and breast cancer also attained a meaningful share of total inpatient expenses, while the proportions belonging to gallbladder carcinoma and nasopharynx cancer were relatively limited across the study period. In addition, it should be noted that although the thyroid cancer was not a major contributor to the inpatient expenses, it increased rapidly by 940.7% during the observation time, from 0.86 billion CNY (1.7%) in 2008 to 8.95 billion CNY (3.7%) in 2017. Inpatient payments of prostatic cancer (493.0%), colorectal cancer (421.5%), and lung cancer (417.2%) also increased much faster than average during the entire study period. In general, the APC (95% CI) of overall cancer inpatient payments slowed down from 21.8% (21.0%, 22.6%) per year before 2013 to 11.9% (11.2%, 12.6%) per year after 2013. The largest fluctuation in annual growth rates was found for nasopharynx cancer, of which the APC declined from 21.5% (16.5%, 26.6%) per year to 2.4% (−5.9%, 10.8%) per year. Similarly, the increasing rates of inpatient expenses for esophagus cancer, stomach cancer, and liver cancer also significantly slowed down after 2013.
Figure 2.
Proportion of different subtypes in total inpatient expenses of cancer during 2008−2017.
Although most cancer inpatient expenses have generally happened in grade 3 general hospitals, the relative proportion of payments spent in different classes of hospitals varied across cancer subtypes (Supplementary Table S1 ). In 2017, the inpatient expense of cervical cancers happened in cancer specialized hospitals held a significantly larger share (39.6%) than average (18.2%), along with breast cancer (28.5%), ovarian cancer (28.5%), nasopharynx cancer (37.9%) and thyroid cancer (23.8%). On the other hand, the inpatient payments of prostatic and bladder cancers spent in cancer specialized hospitals only accounted for about 9% of total costs. The proportion was even more limited for leukemia (1.3%), of which over 85% of inpatient expenses have happened in grade 3 general hospitals. In addition, more than 25.0% of inpatient payments of gallbladder carcinoma (28.9%), stomach cancer (25.2%) and bladder cancer (25.0%) were spent in grade 2 general hospitals, which were relatively larger than general (19.7%).
Table S1. Inpatient expenses of cancer subtypes in different types of hospitals during 2008−2017.
| Subtypes of cancer | Types of hospitals | Inpatient expenses (×100 million) (CNY) | Overall change (%) | APC (95% CI) (%) | ||||||||||
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2008−2013 | 2013−2017 | |||
| CNY, Chinese Yuan; APC, annual percentage change; 95% CI, 95% confidence interval. | ||||||||||||||
| All cancers | General,
grade 2 |
93.0 | 115.2 | 143.5 | 163.4 | 166.8 | 198.7 | 209.5 | 218.2 | 215.6 | 230.1 | 147.4 | 14.4 (9.8, 19.0) | 3.2 (1.2, 5.3) |
| General,
grade 3 |
283.8 | 353.9 | 453.6 | 574.2 | 703.2 | 924.1 | 1046.0 | 1,197.6 | 1,402.1 | 1,559.3 | 449.4 | 23.4 (22.4, 24.5) | 13.4 (12.1, 14.7) | |
| Cancer specialized | 87.7 | 108.0 | 132.9 | 170.8 | 213.3 | 261.1 | 305.6 | 350.0 | 389.3 | 419.4 | 378.2 | 22.1 (21.2, 23.0) | 11.9 (8.9, 14.9) | |
| Nasopharynx cancer | General,
grade 2 |
1.1 | 1.4 | 1.8 | 2.2 | 2.0 | 2.8 | 2.4 | 2.9 | 2.1 | 2.1 | 90.9 | 17.0 (9.7, 24.2) | −7.1 (−19.3, 5.1) |
| General,
grade 3 |
4.8 | 7.1 | 8.7 | 10.9 | 13.0 | 15.4 | 16.3 | 19.0 | 17.7 | 17.3 | 260.4 | 22.5 (17.6, 27.4) | 3.2 (−4.1, 10.4) | |
| Cancer specialized | 3.4 | 4.2 | 6.4 | 8.1 | 9.1 | 10.4 | 11.2 | 12.2 | 11.4 | 11.7 | 244.1 | 23.3 (16.3, 30.3) | 2.5 (−2.5, 7.6) | |
| Esophagus cancer | General,
grade 2 |
7.9 | 9.7 | 12.5 | 14.3 | 13.0 | 20.2 | 19.1 | 18.7 | 18.5 | 19.8 | 150.6 | 16.3 (8.2, 24.4) | −0.7 (−4.9, 3.4) |
| General,
grade 3 |
17.0 | 19.3 | 29.5 | 38.3 | 48.6 | 61.0 | 67.0 | 70.5 | 82.2 | 87.2 | 412.9 | 26.9 (22.5, 31.3) | 9.2 (6.6, 11.8) | |
| Cancer specialized | 7.5 | 9.5 | 12.2 | 16.9 | 19.9 | 23.5 | 29.4 | 30.9 | 30.7 | 33.8 | 350.7 | 23.6 (20, 27.1) | 7.7 (0.7, 14.7) | |
| Stomach cancer | General,
grade 2 |
11.7 | 18.8 | 21.0 | 23.6 | 21.9 | 27.8 | 28.6 | 27.8 | 28.3 | 31.2 | 166.7 | 14.0 (3.8, 24.2) | 2.2 (−1.6, 6.0) |
| General,
grade 3 |
30.2 | 40.8 | 49.4 | 64.2 | 80.3 | 111.8 | 114.3 | 123.0 | 146.1 | 155.5 | 414.9 | 25.3 (22.8, 27.7) | 9.1 (4.6, 13.5) | |
| Cancer specialized | 8.4 | 10.3 | 12.9 | 17.1 | 20.5 | 25.1 | 30.5 | 33.7 | 35.2 | 38.4 | 357.1 | 22.3 (20.6, 24.1) | 9.9 (5.0, 14.9) | |
| Colorectal cancer | General,
grade 2 |
12.1 | 15.9 | 19.0 | 22.0 | 21.3 | 25.7 | 28.5 | 31.0 | 30.8 | 34.3 | 183.5 | 13.7 (7.7, 19.7) | 6.5 (3.2, 9.9) |
| General,
grade 3 |
33.8 | 43.4 | 53.9 | 70.4 | 96.0 | 125.0 | 143.6 | 161.8 | 191.0 | 214.3 | 534.0 | 26.3 (24.3, 28.2) | 13.6 (12.4, 14.9) | |
| Cancer specialized | 9.3 | 11.5 | 13.8 | 17.2 | 21.6 | 26.9 | 33.2 | 38.1 | 41.7 | 46.3 | 397.8 | 21.2 (20.2, 22.2) | 13.1 (8.8, 17.5) | |
| Liver cancer | General,
grade 2 |
6.7 | 8.3 | 10.4 | 11.8 | 11.4 | 13.8 | 15.0 | 15.7 | 14.8 | 15.6 | 132.8 | 13.4 (7.7, 19.1) | 2.3 (−1.9, 6.6) |
| General,
grade 3 |
21.9 | 25.9 | 34.7 | 43.2 | 50.1 | 71.4 | 71.0 | 81.4 | 96.3 | 109.6 | 400.5 | 23.2 (19.8, 26.6) | 11.6 (5.9, 17.4) | |
| Cancer specialized | 4.3 | 5.3 | 6.3 | 9.8 | 10.1 | 12.9 | 14.1 | 16.6 | 19.4 | 20.6 | 379.1 | 22.5 (16.8, 28.2) | 12.6 (9.3, 15.8) | |
| Gallbladder carcinoma | General,
grade 2 |
0.8 | 1.2 | 1.3 | 2.1 | 1.4 | 1.7 | 1.8 | 1.7 | 1.8 | 2.1 | 162.5 | 13.5 (−2.2, 29.1) | 4.2 (−2.2, 10.6) |
| General,
grade 3 |
1.8 | 2.1 | 2.7 | 3.6 | 4.4 | 5.8 | 6.6 | 7.2 | 8.3 | 9.3 | 416.7 | 23.9 (21.4, 26.3) | 11.7 (10.4, 13.1) | |
| Cancer specialized | 0.3 | 0.4 | 0.5 | 0.7 | 0.8 | 1.0 | 1.1 | 1.1 | 1.4 | 1.4 | 366.7 | 24.1 (20.6, 27.6) | 9.1 (2.8, 15.5) | |
| Pancreatic cancer | General,
grade 2 |
1.9 | 2.6 | 3.4 | 3.8 | 3.9 | 4.8 | 4.8 | 4.8 | 5.0 | 5.5 | 189.5 | 17.0 (10.2, 23.8) | 3.1 (−0.6, 6.9) |
| General,
grade 3 |
6.6 | 7.9 | 10.0 | 12.7 | 14.9 | 19.6 | 21.5 | 24.4 | 29.3 | 34.1 | 416.7 | 21.7 (19.9, 23.5) | 14.2 (11.1, 17.2) | |
| Cancer specialized | 1.6 | 2.0 | 2.4 | 2.8 | 3.4 | 4.1 | 5.0 | 6.1 | 8.4 | 8.9 | 456.3 | 18.4 (17.3, 19.6) | 20.7 (14.2, 27.1) | |
| Lung cancers | General,
grade 2 |
15.9 | 20.0 | 26.9 | 30.8 | 31.4 | 40.1 | 42.6 | 43.3 | 42.8 | 43.2 | 171.7 | 17.5 (11.8, 23.1) | 1.5 (−0.8, 3.9) |
| General,
grade 3 |
38.9 | 47.3 | 65.8 | 80.5 | 103.7 | 124.1 | 155.6 | 170.2 | 207.9 | 240.0 | 517.0 | 23.9 (21.3, 26.5) | 16.1 (12.8, 19.4) | |
| Cancer specialized | 15.0 | 18.6 | 22.6 | 29.5 | 37.8 | 46.6 | 51.1 | 54.8 | 64.1 | 69.6 | 364.0 | 23.0 (21.6, 24.5) | 10.3 (7.9, 12.6) | |
| Breast cancer | General,
grade 2 |
7.4 | 7.0 | 9.4 | 10.8 | 10.0 | 12.6 | 14.4 | 14.2 | 14.2 | 14.8 | 100 | 11.1 (4.5, 17.6) | 3.1 (−1.4, 7.5) |
| General,
grade 3 |
14.8 | 18.8 | 25.0 | 30.7 | 40.5 | 53.1 | 60.3 | 65.3 | 77.7 | 83.2 | 462.2 | 25.4 (24.1, 26.7) | 11.5 (8.9, 14.1) | |
| Cancer specialized | 8.5 | 10.3 | 13.7 | 17.6 | 20.5 | 24.6 | 28.0 | 29.7 | 34.2 | 37.2 | 337.6 | 21.8 (18.9, 24.7) | 10.3 (8.2, 12.3) | |
| Cervical cancer | General,
grade 2 |
1.8 | 2.1 | 2.7 | 3.3 | 3.0 | 4.6 | 4.3 | 4.9 | 4.5 | 4.9 | 172.2 | 17.0 (9.7, 24.4) | 1.7 (−4.0, 7.5) |
| General,
grade 3 |
5.4 | 7.1 | 9.8 | 12.7 | 17.5 | 24.2 | 27.6 | 30.3 | 46.4 | 40.9 | 657.4 | 29.9 (28.6, 31.2) | 15.7 (2.5, 28.9) | |
| Cancer specialized | 5.6 | 7.0 | 8.2 | 11.3 | 13.8 | 17.0 | 22.0 | 23.9 | 25.0 | 25.6 | 357.1 | 22.6 (20.2, 25) | 9.5 (1.1, 17.9) | |
| Ovarian cancer | General,
grade 2 |
1.7 | 1.8 | 2.5 | 2.7 | 2.7 | 3.2 | 3.8 | 4.0 | 4.1 | 4.1 | 141.2 | 12.7 (7.0, 18.4) | 5.7 (−0.3, 11.8) |
| General,
grade 3 |
3.8 | 4.9 | 6.3 | 7.9 | 10.1 | 13.6 | 14.8 | 17.1 | 19.7 | 21.9 | 476.3 | 25.1 (23.8, 26.3) | 12.4 (10.5, 14.3) | |
| Cancer specialized | 2.1 | 2.6 | 3.5 | 4.7 | 5.5 | 6.8 | 7.3 | 8.0 | 8.6 | 9.3 | 342.9 | 24.0 (20.9, 27.2) | 7.9 (7.4, 8.4) | |
| Prostatic cancer | General,
grade 2 |
1.3 | 1.8 | 2.1 | 2.5 | 2.8 | 3.1 | 3.5 | 4.1 | 3.8 | 4.5 | 246.2 | 16.7 (11.7, 21.7) | 8.3 (1.5, 15.1) |
| General,
grade 3 |
3.9 | 5.0 | 6.1 | 8.1 | 10.0 | 13.1 | 17.6 | 20.5 | 24.4 | 28.1 | 620.5 | 24.1 (22.7, 25.4) | 18.5 (13.4, 23.6) | |
| Cancer specialized | 0.6 | 0.7 | 0.8 | 1.0 | 1.4 | 1.8 | 2.3 | 2.7 | 3.3 | 3.8 | 533.3 | 22.3 (17.1, 27.4) | 18.6 (15.5, 21.6) | |
| Bladder cancer | General,
grade 2 |
2.2 | 3.1 | 3.4 | 3.8 | 3.6 | 4.0 | 4.4 | 4.7 | 4.8 | 5.2 | 136.4 | 10.1 (2.5, 17.8) | 6.1 (4.0, 8.3) |
| General,
grade 3 |
6.0 | 7.7 | 8.9 | 11.4 | 15.0 | 17.4 | 21.2 | 24.5 | 29.1 | 34.1 | 468.3 | 21.6 (19.2, 24.1) | 16.6 (15.3, 18.0) | |
| Cancer specialized | 0.9 | 1.1 | 1.3 | 1.7 | 2.1 | 2.6 | 3.2 | 3.8 | 4.4 | 4.8 | 433.3 | 21.5 (19.8, 23.1) | 15.4 (11.3, 19.6) | |
| Brain tumor | General,
grade 2 |
1.1 | 1.7 | 2.7 | 2.5 | 2.7 | 2.9 | 3.2 | 3.3 | 3.2 | 3.4 | 209.1 | 17.6 (3.6, 31.6) | 3.2 (−0.6, 6.9) |
| General,
grade 3 |
8.5 | 9.5 | 11.9 | 14.6 | 16.4 | 20.9 | 23.8 | 27.7 | 32.4 | 36.2 | 325.9 | 18.1 (15.7, 20.5) | 14.1 (12.7, 15.4) | |
| Cancer specialized | 1.2 | 1.6 | 1.9 | 2.5 | 2.8 | 3.9 | 3.9 | 4.3 | 4.9 | 5.4 | 350.0 | 22.4 (19.1, 25.8) | 8.8 (4.5, 13.1) | |
| Thyroid cancer | General,
grade 2 |
1.1 | 1.5 | 1.6 | 2.0 | 2.3 | 2.9 | 3.8 | 4.0 | 4.8 | 6.0 | 445.5 | 18.1 (14.6, 21.7) | 16.9 (11.2, 22.6) |
| General,
grade 3 |
4.3 | 5.4 | 6.1 | 9.4 | 13.2 | 21.5 | 28.9 | 36.9 | 48.0 | 61.7 | 1,334.9 | 31.9 (23.4, 40.4) | 26.2 (24.7, 27.6) | |
| Cancer specialized | 3.0 | 3.6 | 2.4 | 3.6 | 5.8 | 7.6 | 11.8 | 14.0 | 16.2 | 18.9 | 530.0 | 18.5 (−0.1, 37.2) | 21.4 (10.7, 32.1) | |
| Leukemia | General,
grade 2 |
3.4 | 4.2 | 5.3 | 5.7 | 5.9 | 6.7 | 5.9 | 5.8 | 5.9 | 6.4 | 88.2 | 12.8 (7.6, 18.0) | −0.9 (−8.0, 6.2) |
| General,
grade 3 |
22.7 | 31.4 | 33.1 | 40.9 | 42.5 | 68.5 | 66.1 | 79.3 | 92.0 | 98.9 | 335.7 | 19.0 (11.2, 26.8) | 10.7 (4.4, 16.9) | |
| Cancer specialized | 0.4 | 0.4 | 0.5 | 0.7 | 1.0 | 1.0 | 1.6 | 2.3 | 2.7 | 2.8 | 600.0 | 21.9 (13.6, 30.2) | 25.8 (9.2, 42.5) | |
| Others | General,
grade 2 |
15.0 | 14.2 | 17.5 | 19.5 | 27.3 | 22.0 | 23.2 | 27.3 | 26.2 | 27.1 | 80.7 | 11.4 (2.4, 20.4) | 5.4 (−0.2, 11.0) |
| General,
grade 3 |
59.4 | 70.4 | 91.7 | 114.8 | 127.0 | 157.9 | 189.9 | 238.7 | 253.6 | 286.8 | 382.8 | 19.7 (16.8, 22.5) | 14.8 (9.3, 20.3) | |
| Cancer specialized | 15.5 | 19.0 | 23.4 | 25.6 | 37.3 | 45.5 | 50.0 | 67.6 | 77.6 | 80.9 | 421.9 | 21.4 (17.0, 25.8) | 15.9 (8.3, 23.5) | |
Discussion
Globally, expenditure of cancer health care in a country often accounts for a significant part of its THE. In Europe, the expenditure on cancer health care in 31 countries ranged from 4% to 7% of THE in 2018 (8). For instance, the proportion was reported to be 6.8% in Germany. Evidence was relatively limited in China. According to the study of Zhang et al., health care expenditure for cancer in 2011 took up about 7.35% of that for overall chronic diseases, and about 5.14% of THE (9). The proportion was similar to findings in Europe, while it was a little bit higher than our results (ranged from 3.5% to 4.6%). The possible reason for the difference is that the health care expenditure in Zhang’s study included expenditures on prevention, inpatient, outpatient, medicine, and health management, while our study only included expenditures on inpatient and outpatient.
With the remarkable epidemiological and demographic transition in China, DALYs of cancer have remarkably increased during the last decades in China. Moreover, the great improvements in screening, diagnosis, and medical treatments of cancer, which greatly helped better identify patients at earlier stages and prolong their survival time with diseases, have further exacerbated the burden of cancer in China (1). Accordingly, our study indicated a remarkable increase (294.3% from 2008 to 2017) in the health care expenditure of cancer in China.
At the same time, the expenditures of cancer health care have increased significantly worldwide. Cancer health care expenditures had increased by 233% from 35.7 billion euro in 1995 to 83.2 billion euro in 2014 in the EU, and this growth is foreseeable to continue (10). Not only in Europe, but also in the United States (US), the expenditure on cancer health care also increased significantly. Based on the report from the Agency for Healthcare Research and Quality, the total expenditure on cancer health care was approximately
 57 billion in 2001, whereas in 2011, the total expenditure on cancer health care has increased to approximately
57 billion in 2001, whereas in 2011, the total expenditure on cancer health care has increased to approximately
 88.3 billion (11). Cancer health care expenditure had increased by 154.91% in that decade.
88.3 billion (11). Cancer health care expenditure had increased by 154.91% in that decade.
In order to control the excessive growth of THE, a series of health expenditure control policies were promulgated in China in 2012, including Opinions on Carrying out Total Control of Basic Medical Insurance Payments issued by the Ministry of Human Resources and Social Security, Ministry of Finance, National Health Commission (previously the Ministry of Health), and Opinions of Carrying out Controlling the Total Payment of Basic Medical Insurance issued by Ministry of Human Resources and Social Security, Ministry of Finance, National Health Commission. Several months after these policies issued, significant changes in annual growth rates of expenditures were observed (e.g. from 2008 to 2013 the APC of the total expenditure of cancer was 21.8% (21.0%, 22.6%), while from 2013 to 2017 it decreased to 11.9% (11.2%, 12.6%), which to some extent reflected the policy effect. A similar influence of policy reform was observed in other studies. In the US, studies also showed that once the government introduced a fee control policy, the expenditure on cancer treatment was greatly impacted. The reform could improve the efficiency of health resources through adjustment in medical insurance and hospital finances, leading to a reduction in the profit of cancer treatment (12). Data from the World Bank also indicated a slight decline in the proportion of THE in GDP in the US after 2010 due to the cost control policy of the Affordable Care Act.
Inpatient payments of cancer were observed to be mainly concentrated on grade 3 hospitals and continued to pour into grade 3 hospitals from 2008 to 2017. In consideration of the complication of cancer treatments and its high equipment requirements, the large share of grade 3 hospitals in total cancer payments was reasonable. In addition, this tendency was also rational under the strengthening hierarchical diagnosis and treatment program in China, since both the Service Capacity Standards of Community Health Service Centers and the Service Capacity Standards of Township Health Centers launched by the government in 2018 did not recommend the cancer treatment as s a basic medical and health service.
The ratio of outpatient expenditure to inpatient expenditure for cancer treatments generally remained stable, with a slight increase observed from 0.22 in 2011 to 0.26 in 2017. This nearly 1:4 ratio was consistent with our previous findings and its modest increase partially indicated the improvement of outpatient service for cancer treatments in China (13). Studies in the US showed that with the improving technology of cancer treatment, the ratio would increase further. Studies of the expenditure of cancer treatments in the US showed that ambulatory care visits treatments (similar to the outpatient treatments in China) account for 41% of health care expenditures and is the largest part of expenditures, followed by inpatient treatments accounting for about 27%, anti-cancer drugs accounting for about 21%, and the rest of services accounting for about 10% (14). Similar results were also reported in a recently published regional study conducted in Southwest China in 2016, which showed that payments incurred in hospitalization accounted for 82.18% of the total direct medical expenses for cancers and the outpatient expenses accounted for the remaining 17.82%. The corresponding ratio of 0.22 was a bit lower in comparison with the national level of 0.25 in 2016 observed in our analyses.
Along with other upper-middle income countries, lung cancer, gastric cancer, and colorectal cancer have remained the top-three-ranking causes of DALYs in China. In 2015, lung cancer was estimated as the most common cancer diagnosed in China, followed by gastric and colorectal cancer, in total accounting for over 40% of overall new cancer cases in China (15). Accordingly, we found that lung cancer was also the leading contributor to the expenditure of cancer health care, which generated 460.3 billion CNY inpatient payments (19% of total inpatient payments) in 2017. Besides, gastrointestinal cancers including gastric and colorectal cancers also contributed substantially to the cancer inpatient payments. Consistent with our findings, lung cancer and colorectal cancer were proved to be the costliest cancer among US adults (14). Despite the prevalence, the difference in stage at diagnosis, survival duration, intensity of treatment, and comorbidity also contributed to disparity in economic burdens for cancer subtypes (16). For instance, most lung cancer patients were diagnosed at advanced stages and often had higher comorbidity burdens, which led to greater demand for intensive care and higher spending on inpatient services (17).
In addition, we observed a much faster increase in inpatient expenditure for thyroid cancer, along with the rapid rise in incidence and moderate growth in mortality of thyroid cancer in current China (18). Apart from higher prevalence of risk factors like obesity, the improved sensitivity of diagnostic tools might also be an important explanation for this increase, as previous studies have reported (19). Similar situations were also observed for cervical cancer among females and prostatic cancer among males (20-22). Moreover, the inpatient expense for colorectal cancer was found to be increased much faster than average, along with a significant growth in incidence due to westernization of lifestyle and aged tendency of population in China. Meanwhile, advances in treatment including surgical techniques, liver metastasis therapy, and targeted therapy remarkably improved survival rates of patients and prolonged their survival duration, which unavoidably added to the hospitalization expenditure of colorectal cancer currently (23). Early prevention strategies could help reduce the cancer expenditure in hospitals (24,25).
Conclusions
This study estimates the total payments of cancer treatments in China from 2008 to 2017, which would provide information for decision making on the allocation of resources to service provisioning, prevention strategies and research funding. What is more, our results showed that after 2013, the APC (95% CI) of cancer health care expenditure dropped from 21.8% (21.0%, 22.6%) to 11.9% (11.2%, 12.6%), from higher than APC of THE to lower than APC of THE. This study may provide scientific evidence to evaluate whether our government can afford the economic burden of cancer in the future.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Acknowledgements
This study was supported by the National Key Research and Development Program of China (No. 2018YFC1311704).
Contributor Information
Shiyong Wu, Email: wusy99@126.com.
Jinghua Li, Email: jhli@jlu.edu.cn.
References
- 1.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. 2020. Available online: http://www.healthdata.org/gbd/2019
- 2.Sung H, Ferlay J, Siegel RL, et al Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.National Health Commission of the People’s Republic of China. China Health Statistical Yearbook, 2020. Beijing: Peking Union Medical College Press, 2021.
- 4.Zhang S, Sun K, Zheng R, et al Cancer incidence and mortality in China, 2015. J Natl Cancer Center. 2021;1:2–11. doi: 10.1016/j.jncc.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carey K, Burgess JF Hospital costing: experience from the VHA. Financial Accountability & Management. 2000;16:289–308. doi: 10.1111/1468-0408.00109. [DOI] [Google Scholar]
- 6.Li J, Li Z, Yin Z ArcGIS based Kriging interpolation and its application. Ce Hui Tong Bao. 2013;0:87–90. [Google Scholar]
- 7.Kim HJ, Fay MP, Feuer EJ, et al Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 8.Hofmarcher T, Lindgren P, Wilking N, et al The cost of cancer in Europe 2018. Eur J Cancer. 2020;129:41–9. doi: 10.1016/j.ejca.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Y, Wan Q, Zhai T, et al Results and analysis of total health expenditure in China in 2011. Zhongguo Wei Sheng Jing Ji. 2013;32:5–9. [Google Scholar]
- 10.Wilking N, Lopes G, Meier K, et al Can we continue to afford access to cancer treatment. Eur Oncol Haematol. 2017;13:114–9. doi: 10.17925/EOH.2017.13.02.114. [DOI] [Google Scholar]
- 11.Soni A. Trends in use and expenditures for cancer treatment among adults 18 and older, U. S. Civilian Noninstitutionalized Population, 2001 and 2011. In: Statistical Brief [Medical Expenditure Panel Survey (US)]. Rockville (MD): Agency for Healthcare Research and Quality (US), 2001.
- 12.Ferris LW, Farber M, Guidi TU, et al Impact of health care reform on the cancer patient: a view from cancer executives. Cancer J. 2010;16:600–5. doi: 10.1097/PPO.0b013e3181feeba1. [DOI] [PubMed] [Google Scholar]
- 13.Cai Y, Xue M, Chen W, et al Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. 2017;29:253–62. doi: 10.21147/j.issn.1000-9604.2017.03.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park J, Look KA Health care expenditure burden of cancer care in the United States. Inquiry. 2019;56:46958019880696. doi: 10.1177/0046958019880696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao M, Li H, Sun D, et al Cancer burden of major cancers in China: A need for sustainable actions. Cancer Commun (Lond) 2020;40:205–10. doi: 10.1002/cac2.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yabroff KR, Lamont EB, Mariotto A, et al Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst. 2008;100:630–41. doi: 10.1093/jnci/djn103. [DOI] [PubMed] [Google Scholar]
- 17.Bluethmann SM, Mariotto AB, Rowland JH Anticipating the “Silver Tsunami”: Prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25:1029–36. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang J, Yu F, Shang Y, et al Thyroid cancer: incidence and mortality trends in China, 2005-2015. Endocrine. 2020;68:163–73. doi: 10.1007/s12020-020-02207-6. [DOI] [PubMed] [Google Scholar]
- 19.Grodski S, Brown T, Sidhu S, et al Increasing incidence of thyroid cancer is due to increased pathologic detection. Surgery. 2008;144:1038. discussion 1043. doi: 10.1016/j.surg.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 20.Xu Y, Zhang Z Evaluation on PSA screening status of prostate cancer. Xian Dai Mi Niao Sheng Zhi Zhong Liu Za Zhi. 2012;4:371–3. doi: 10.3870/j.issn.1674-4624.2012.06.016. [DOI] [Google Scholar]
- 21.Wei L, Shen D, Zhao F, et al Expert Consensus on Cervical Cancer Screening and Abnormal Management in China (part II) Zhongguo Fu Chan Ke Lin Chuang Za Zhi. 2017;18:286–8. doi: 10.13390/j.issn.1672-1861.2017.03.041. [DOI] [Google Scholar]
- 22.Wei L, Zhao Y, Shen D, et al Expert Consensus on Cervical Cancer Screening and Abnormal Management in China (part I) Zhongguo Fu Chan Ke Lin Chuang Za Zhi. 2017;18:190–2. doi: 10.13390/j.issn.1672-1861.2017.02.032. [DOI] [Google Scholar]
- 23.Siegel RL, Miller KD, Goding Sauer A, et al Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70:145–64. doi: 10.3322/caac.21601. [DOI] [PubMed] [Google Scholar]
- 24.Shi J, Liu G, Wang H, et al Medical expenditures for colorectal cancer diagnosis and treatment: A 10-year high-level-hospital-based multicenter retrospective survey in China, 2002-2011. Chin J Cancer Res. 2019;31:825–37. doi: 10.21147/j.issn.1000-9604.2019.05.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lei H, Lei L, Shi J, et al No expenditure difference among patients with liver cancer at stage I-IV: Findings from a multicenter cross-sectional study in China. Chin J Cancer Res. 2020;32:516–29. doi: 10.21147/j.issn.1000-9604.2020.04.09. [DOI] [PMC free article] [PubMed] [Google Scholar]