Abstract
Background
In 2020, the COVID-19 virus sparked a crisis constituting a nationwide public health emergency that rapidly altered the provision of healthcare services for all Americans. Infectious disease mitigation led to widespread lockdowns of perceived nonessential services, programs, and non-emergent healthcare interventions. This lockdown exacerbated the public health dyad of uncontrolled pain and the opioid epidemic, which was already in a crisis state. Current literature supports the management of uncontrolled pain with a biopsychosocial approach, empowering patients to explore self-care to enhance activities of daily living. Pain Coping Skills Training (PCST) delivers real-life strategies that improve quality of life and strengthen self-efficacy. Self-efficacy has been identified as a patient outcome measure that demonstrates improved patient-perceived function and quality of life despite pain intensity. Studies have shown that nurse practitioners (APRN) are well-positioned to provide PCST to chronic pain sufferers.
Methods
A pretest-posttest design was utilized for this project to enhance pain self- efficacy through an APRN-led community-based intervention.
Intervention
Community-dwelling adults treated in a specialty pain management practice were self-selected to participate in a 6-week telehealth delivered PCST Program. This APRN delivered program presented basic pain education and a broad range of evidence-based nonpharmacologic pain management self-care tools. The primary outcome was improved Pain Self-efficacy measured with the pain self-efficacy questionnaire (PSEQ), with secondary outcomes of improved perceived pain intensity and function measured with the pain, enjoyment, and general activity (PEG) scale tracked weekly.
Results
Baseline PSEQ and weekly PEG scores were obtained and compared to scores after the program. Collateral data points included confidence in using complementary and alternative nonpharmacologic interventions, satisfaction with the program, and a qualitative patient statement regarding pre-and post-intervention participation.
Conclusions
This project concluded that a Nurse Practitioner delivered PCST program via telehealth technology could provide community-dwelling adults with an intervention that improves pain self-efficacy, enhances self-reported PEG measures, and meets the social distancing requirements that continue to impact patients during the COVID-19 pandemic.
Abbreviations: PCST, Pain Coping Skills Training; APRN, Advanced Practice Registered Nurse; DNP, Doctor of Nursing Practice; EBP, Evidence Based Practice; COVID -19, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
Introduction
Problem Description
Chronic pain is a prevalent, complex, and distressing symptom that profoundly impacts individuals and society. Unfortunately, pain management has become increasingly difficult for patients and providers in the wake of the opioid epidemic. As a result, barriers to appropriate and meaningful relief exist at multiple access points. These range from patient expectations and access to evidence-based treatment modalities to provider knowledge of available resources and financial feasibility related to payer restrictions and coverage (National Institute of Health NIH, 2016; National Academies of Sciences, Engineering, and Medicine NASEM; Health and Medicine Division; Board on Health Sciences Policy; Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse, 2017).
Additional barriers may exist at different points in time. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) or COVID -19 pandemic impacted the health care system in the northeast in the spring of 2020 (Coleman et al., 2020). The convergence of the pandemic and epidemic of chronic pain has further challenged communities, health care providers, and health care systems. A dearth of accessible pain treatment options was noted at this time of national crisis, leading to the exploration of accessible, evidence-based treatment alternatives to in-person nonpharmacologic self-management programs that may mitigate pain and its associated suffering.
Comprehensive, patient-centered pain management treatment regimens utilize various nonpharmacologic self-management strategies, opioid and nonopioid medication, and interventional procedures. Individuals with chronic pain may explore complementary and alternative modalities (CAM) to mitigate suffering related to pain. These interventions require hands-on, close contact and are not amenable to social distancing. In the northeast and other areas of the country with high rates of infection, many CAM interventions were suspended, decreasing access to nonpharmacologic therapies (American Society of Regional Anesthesia and Pain Medicine ASRA, 2020; US Pain Foundation, 2020)
Pain management interventions such as epidural steroid injections and large joint injections utilize steroids as a core component of the treatment regimen. However, during the height of the COVID-19 pandemic, pain management guidelines advised against steroids due to an increased risk of adrenal insufficiency and altered immune response. Additionally, surge preparation for the public health crisis led to the cancelation of elective interventions (American Society of Regional Anesthesia and Pain Medicine ASRA, 2020).
Available Knowledge
With the advent of the National Pain Strategy and collaborations across the government, university, and private sector, guidelines, and professional organization position statements have called upon clinicians to engage in patient-centered outcomes and evaluate nonpharmacologic interventions that may enhance self-care for this vulnerable population (Tick et al., 2018). The following is an abbreviated description of literature referenced to explore key components of a nurse practitioner-delivered intervention for community-dwelling adults with chronic pain (Appendix A).
Two recent systematic reviews evaluated studies related to nonpharmacologic interventions for the management of chronic pain. A comparative effectiveness review by the Agency for Healthcare Research and Quality (AHRQ) evaluated 202 randomized controlled trials (RCT) addressing noninvasive nonpharmacological treatments for five common chronic pain conditions (Skelly et al., 2018). The American College of Physicians (ACP), in 2018, reviewed nine RCTs. Both publications endorsed the risk versus benefit of nonpharmacologic interventions over opioid medication with a strong recommendation for a patient-centered approach that includes self-care strategies and noninvasive behavioral interventions such as cognitive-behavioral therapy (CBT). Both groups concluded that behavioral modalities and mind-body interventions are supported by new evidence and should be considered part of a multimodal treatment strategy considering the current opioid epidemic (Qaseem et al., 2017; Skelly et al.,2018).
Feasibility for the implementation of CBT and self-management programs for this population was explicitly addressed in two papers. Scriven et al. (2019) utilized a mixed-method feasibility design to evaluate a multisite group telehealth pain support program. This study demonstrated that access to a pain specialist support program via telehealth enhanced pain self-efficacy (Scriven et al., 2019). Taylor et al. (2016) addressed feasibility in a multicentered pragmatic trial involving 703 adults in 27 general community practices demonstrating cost-effective improved psychological well-being. Both of these works determined CBT and self-management to be feasible and efficacious in enhancing patient-centered outcomes.
The use of telehealth formatted programs was observed in seven of the works reviewed. Study leaders utilized telehealth access to expand the reach and optimize participation in therapy. Heapy et al. (2017) demonstrated in an RCT that CBT delivered remotely was non-inferior to in-person provided therapy and was less burdensome for participants (Heapy et al. 2017). Trudeau et al. (2015) utilized a web-based patient education program guided by CBT. Two hundred and twenty-eight participants accessed the program with improvement noted in self-efficacy and pain catastrophizing. However, this study did not demonstrate improvement in pain intensity. This finding was consistent across other mentioned studies and pain etiologies, including fibromyalgia, chronic back pain, osteoarthritis (OA), and persistent non-specific pain (Nost et al., 2018; Trudeau et al., 2015; Dear et al., 2017; Scriven et al., 2019; Peters et al., 2017; (Bennell et al., 2015); Heapy et al., 2017).
The professionals delivering psychosocial interventions such as CBT varied by study. For example, Broderick et al. (2014) evaluated the effectiveness of a pain coping skills training (PCST) program delivered by a pain management nurse practitioner (NP) for 246 community-dwelling adults with severe knee OA. This study concluded that an NP-delivered PCST protocol produced significant improvements in a range of pain-related variables, including pain intensity, coping, self-efficacy, activity interference, and the use of pain medication when compared with usual care. Originally PCST was developed and delivered by clinical psychologists. This study led the way for an interstate, grant-funded study evaluating NPs in providing PCST to a broad range of patient populations (Broderick & Brunkenthal, 2018). This work demonstrated that advanced practice registered nurses (APRNs), embedded in community medical practices, can achieve comparable clinical outcomes.
Measurement of success for many of the studies reviewed in developing this project looked past numeric pain scores and reduced opioid usage. Assessment of outcomes related to function and self-efficacy were frequent themes. The most commonly used tool observed in this literature search was the pain self-efficacy questionnaire (PSEQ) utilized by 17 studies. Additional clinical outcome measures included the coping strategy questionnaire, Pain Catastrophizing Scale, pain awareness scale, and pain resource utilization measures, such as provider visits and hospital encounters. Matthias et al. (2015) incorporated the pain, enjoyment, and general activity (PEG) scale as an abbreviated version of the Brief Pain Inventory to evaluate pain, enjoyment, and function.
Rationale
COVID-19 caused an insurmountable impact, especially detrimental to marginalized communities, such as individuals who suffer from chronic pain. During and beyond the COVID-19 pandemic, shifts in care delivery have widened the disparity gap in the undertreatment of pain in this at-risk population (Coleman et al., 2020). In addition, state and national authorities expect adverse consequences related to social isolation and inadequate provider interaction for patients with chronic pain (Puntillo et al., 2020). This challenge called for a sense of urgency to address the needs of this vulnerable population.
The PCST intervention described by Broderick et al. (2014) provided an opportunity to implement a self-management program that was anticipated to be amenable to telehealth delivery. This intervention has been successfully implemented by nurse practitioners and aligned with state and national infection prevention mitigation efforts. Additionally, it offered an opportunity for participants to engage with their peers in a group format for social connection.
Specific Aims
This evidence-based practice project aimed to assess the effect of a telehealth delivered PCST program on pain self-efficacy for community-dwelling adults with chronic pain managed by a community pain practice. The primary outcome measure is self-reported pain self-efficacy measured with the PSEQ. Additional data points observed and measured over the 6-week intervention period included measures of PEG, patient confidence in the use of CAM interventions, and patient satisfaction with the overall program.
This pre-test-post-test study design correlated the effect of the 6-week PCST telehealth intervention with a change in self-reported pain self-efficacy utilizing the PSEQ questionnaire. It was hypothesized that empowering patients with knowledge regarding fundamental pain neuroscience and self-care pain mitigation skills in a collaborative, non-threatening environment would enhance their utilization and improve overall perceived pain self-efficacy. Additionally, the correlation between pain self-efficacy and confidence in using modalities that support self-management was explored.
The Patient/Problem Intervention Comparison Outcome (PICOT) question for this nurse-led quality improvement initiative was:
In adult chronic pain patients (P), how does a telehealth delivered Pain Coping Skills Training (PCST) Program (I) compared with usual care (C) affect pain self-efficacy (O) during a six-week period (T)?
Methods
Practice location
This project was conducted in collaboration with a community-based pain clinic in the northeast. This outpatient setting served a wide range of patients from diverse backgrounds. This office was one of a system of pain management offices spread over a sizeable geographic location. It was staffed by eight board-certified pain management physicians and employed three full-time NPs, a licensed acupuncturist, and other support staff to ensure patients had available resources to make functional gains. Patients in this office ranged in age from young adult to elderly. Patients presented with a wide range of pain diagnoses, including chronic neck and back pain, fibromyalgia, chronic regional pain syndrome, cancer pain, neuropathies, and other forms of chronic pain.
Treatment modalities ranged from simple office interventions such as trigger point injections to complex pain management procedures requiring anesthesia. Most patients were managed with a multimodal approach that incorporates opioid and nonopioid medication and interventional treatment modalities. Patients were rarely treated with stand-alone opioid medication. During the COVID 19 pandemic height, all new and existing patients were assessed and treated via telehealth. All nonemergent pain management procedures were postponed. This change in practice for patients and providers was done to comply with state regulations to combat the public health crisis (Cuomo, 2020).
Subjects
All English-speaking adult patients (age 18 or greater) diagnosed with chronic or persistent pain treated in the aforementioned office were considered eligible to enroll. Participants had to be willing to complete the project questionnaires and engage in the weekly sessions via a telehealth platform on a computer or smartphone. Non-English speakers were excluded due to feasibility, with plans for future versions of this program to be augmented to include Spanish and American Sign Language (ASL). Individuals with acute psychiatric conditions such as uncontrolled schizophrenia or paranoia were not considered. Other factors for exclusion were determined by office providers at their discretion.
Intervention
PCST is an evidence-based nonpharmacologic intervention that utilizes the foundation of cognitive-behavioral therapy and motivational interviewing to deliver real-life strategies to improve quality of life and enhance self-efficacy (Broderick & Brunkenthal, 2018). In addition, this program was amenable to delivery in a group format via telehealth to meet the current social distancing requirements and reach patients who would otherwise be unable to attend in-person sessions.
This intervention followed the structure of the PCST program described by Broderick et al. (2014). This project's primary lead and facilitator participated in the grant-funded training program described in this literature. Patients participated in a 6-week, 1-hour PCST session. As this was a patient-centered intervention, participants had the option of engaging with the program synchronously or asynchronously via recorded content sessions. Synchronous participation by all participants was not feasible due to scheduling conflicts and time constraints to the implementation window. Each weekly session was recorded by the project lead and posted to an accessible website to allow participants to engage at a convenient time and provide an opportunity to review content for practice.
Weekly themes and skills incorporated patient-centered education that enhanced self-care. Themes were presented through an educational format and followed with motivational interviewing techniques to empower participants to choose strategies they were likely to practice outside of the weekly session. Additionally, a CBT approach that assisted with goal setting, problem-solving, and plan development for "bad pain days" were woven throughout the program.
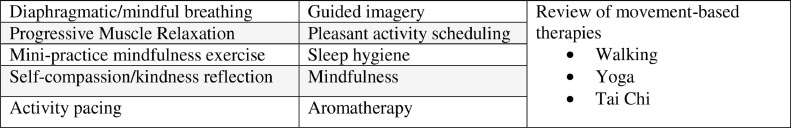
Participants received basic pain neuroscience education such as gate control theory and the chronic pain cycle. In addition, nonpharmacologic interventions were presented with encouragement to self-explore. Finally, participants were coached to identify a strategy and share its use with their providers. A list of the themes and skills can be found in Figure 1 .
Figure 1.
Nonpharmacologic interventions.
A project team was developed to meet the objectives of the current clinical practice problem. The team consisted of the DNP student project leader, project chair, team mentor, project mentors, and clinical office staff. The team leader, a certified pain management NP with previous training in the PCST intervention, provided a foundation to develop the program contents into a version acceptable for telehealth delivery. The project chair and mentors coached the team leader in evidence-based practice, technology, and various obstacles in working through a pandemic. The pain management office staff provided collateral support through patient referral, often connecting with the team lead to query appropriateness for their patients. The PCST intervention was provided by the team lead independent of the clinical practice site.
Study of the Intervention
A convenience sample of self-selected patients from a community-based pain management office was considered for the project intervention. A total of 15 patients expressed interest, inquiring about the program details from the study lead. A total of four patients declined the study intervention for varied reasons. The remaining 11 patients met eligibility and chose to participate in the program. Of these 11 patients, all (n = 11) participated in the study intervention with a 0% attrition rate.
After reviewing current evidence, guidelines, and consideration of the social distancing requirements for the pandemic, a telehealth-delivered version of the PCST was chosen. In addition, the PSEQ, PEG tool, and patient self-report of satisfaction were chosen to evaluate the benefit and impact of the project.
Measures
General demographics collected included age, gender, source and duration of chronic pain, previous use, and confidence in CAM modalities. A data set for all independent and dependent variables was developed and collected via a web-based form completed by the participant. The data collected from the form was converted into an excel spreadsheet uploaded into Intellectus Statistics® for analysis. As this health crisis was unexpected, preliminary data were not available to guide program planning.
The primary outcome for this project was perceived self-efficacy measured by the PSEQ (Appendix B). The PSEQ is a 10-item questionnaire developed by Michael Nicholas to assess the confidence people with ongoing pain have in performing activities while in pain (Nicholas, 2007). Participants rate each item in the survey on a 7-point scale ranging from 0 "not at all confident" to 6 "completely confident." Higher scores reflect stronger self-efficacy beliefs. The PSEQ applies to all persisting pain presentations. It covers a range of functions, including work, household chores, socializing, and the ability to deal with pain without pain medication. This brief tool may be completed in under 2 minutes and is available free of charge to assess treatment planning and outcome evaluation (Nicholas, 2007). A score >40 represents high pain self-efficacy.
The internal consistency of the PSEQ is excellent (0.92 Cronbach's α), and test-retest reliability is high over 3 months (Asghari & Nicholas, 2001). Validity is reflected in high correlations with pain-related disability measures, varied coping strategies, and activity-specific measures of self-efficacy beliefs (Kaivanto et al.,1995). In addition, high PSEQ scores are strongly associated with clinically significant functional gains and provide a valuable gauge for evaluating outcomes in chronic pain patients (Nicholas, 2007).
Secondary measures included weekly assessment of PEG utilizing an ultra-brief pain measure derived from the Brief Pain Inventory (BPI). The PEG tool (Appendix C) is a valuable and practical measure to track progress over time. This tool has been validated in clinical and research settings (Krebs et al., 2009). Patients respond to a three-item questionnaire that reflects the participant's perception of pain intensity, interference of pain with the enjoyment of life, and interference of pain with general activity. Items are scored on a 0-10 scale. A total of 0-30 points is divided by 3 to obtain the PEG score. Participants were asked to complete the PEG scale weekly as they logged on for participation in the PCST module. Results were tracked by individual questions and total scores by the week. After the six-session program, results were compared for overall change.
Baseline scores for the PSEQ were compared with the post-intervention scores. In addition, weekly PEG scores were observed for consistent changes and to identify any participant setbacks during the program. It was hypothesized that participants would demonstrate an increased PSEQ score by the program conclusion and a gradual decrease in the PEG score over the 6-week implementation window. Finally, additional data were collected related to the participant's confidence in the use of CAM modalities. Confidence rating on a six-point Likert scale measured the impact this training program may have on the future use of CAM interventions to manage pain.
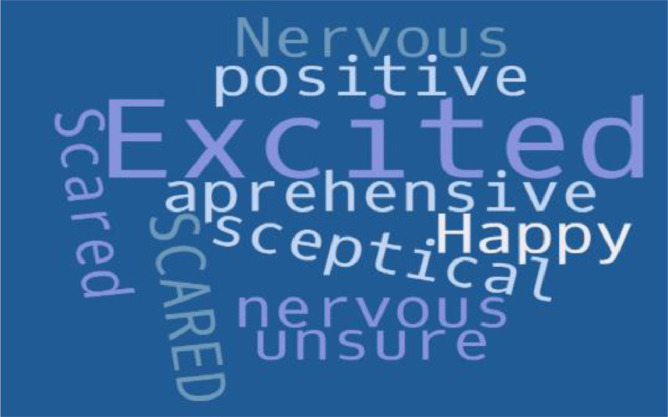
Patient satisfaction and compliance with participation were measured with the final patient questionnaire, which provided insight into the program's value. This feedback was intended to guide future changes to the course outline, content, and presentation style. In addition, pre-study expectation and post-study feedback were collected and presented in a word cloud pictogram to highlight patient response (Figure 7). Finally, the word cloud was shared with participants along with their PCST “diploma” as a memento of their participation.
Figure 7.

Post-intervention participant comments.
Analysis
A two-tailed paired samples t test was conducted to examine whether the mean difference of the PSEQ baseline assessment (Pre-PSEQ) and PSEQ post-intervention assessment (Post-PSEQ) was significantly different from zero. In addition, the mean of Pre-PSEQ was compared with the mean of Post-PSEQ. A repeated measure analysis of variance (ANOVA) with one within-subjects factor was conducted to determine whether significant differences exist among baseline total PEG score and PEG scores collected at week 3 through the program's conclusion at week 6. PEG scores were collected in week 2; however, the statistical software could not accommodate 6 weeks of data. Finally, a two-tailed paired samples t test was conducted to examine whether the mean difference of confidence in CAM before the study intervention (Prior CAM) and confidence in CAM after the intervention (Post CAM) was significantly different from zero. In addition, the mean of prior CAM confidence ratings was compared to the mean of Post CAM confidence ratings.
Ethical Considerations
This project was reviewed and approved by a Human Subjects Review Committee and received exempt status. The team lead completed the Health Professions Human Subjects Research training, the Collaborative Institutional Training Initiative (CITI) program. Project participants were screened based on predetermined inclusion and exclusion criteria. Participation was voluntary and caused no financial burden to the participant. No payment or reimbursement for participation was provided. Demographic data and study tools were de-identified and assigned a random number to ensure data collection confidentiality and continuity. Patient names were not utilized, only the randomly assigned number. Participants had the option to participate in the group experience with or without video during group interaction. There was no conflict of interests identified.
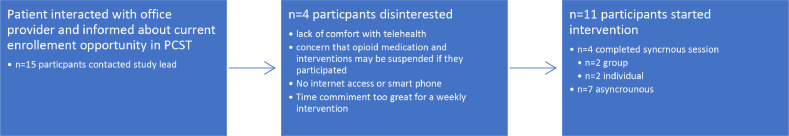
Results
Fifteen community-dwelling adults diagnosed with chronic pain, treated in a community interventional pain practice, were referred and inquired about participation in this evidence-based practice quality improvement project. Of the 15, four declined, and a convenience sample of eleven (n = 11) enrolled and completed the intervention with a 0% attrition rate (Fig. 2). Reasons for declining to participate varied from lack of accessible technology, comfort with telehealth, and concern for possible changes to a prescribed pain regimen if they participated.
Figure 2.
Patient enrollment.
Descriptive statistics were used to analyze the participant demographics. Frequency and percent were conducted for each demographic variable. The final sample consisted of women (n = 9) and men (n = 2) for a total sample size of (n = 11) patients with chronic pain who agreed to complete the program surveys and engage in the weekly PCST modules. The average age was 60.27 (SD 10.61). Frequencies and percentages were calculated for pain history. The most frequently observed category of chronic pain condition was degenerative disc disease (n = 6, 55%). The most frequently reported category related to the length of time with chronic pain was "More than 10 years" (n = 5, 45%) (Tables 1 & 2 ).
Table 1.
Frequency Table for Demographics
| Variable | n | % | Cumulative % |
|---|---|---|---|
| Gender | |||
| Female | 9 | 81.82 | 81.82 |
| Male | 2 | 18.18 | 100.00 |
| Prefer not to answer | 0 | 0.00 | 100.00 |
| Length of time with chronic pain | |||
| 0-3 months | 2 | 18.18 | 45.45 |
| 4-6 months | 2 | 18.18 | 45.45 |
| 1-3 years | 1 | 9.09 | 27.27 |
| 4-6 years | 1 | 9.09 | 54.55 |
| More than ten years | 5 | 45.45 | 100.00 |
| Missing | 0 | 0.00 | 100.00 |
Due to rounding errors, percentages may not equal 100%.
Table 2.
Summary Statistics Table for Interval and Ratio Variables
| Variable | M | SD | N | SEM | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|---|
| Age | 60.27 | 10.61 | 11 | 3.20 | 47.00 | 75.00 | 0.05 | -1.67 |
Note: '-' indicates the statistic is undefined due to constant data or insufficient sample size.
Of the 11 participants, seven (n = 7) interacted via asynchronous access, opting to listen to pre-recorded sessions, and four (n = 4) participated via synchronous "live" sessions. Of the four (n = 4) in the synchronous group, two (n = 2) participants engaged as a group, participating in a session scheduled at the same time every week, and two (n = 2) participants engaged individually due to scheduling conflicts. Patient enrollment is depicted in Figure 2 .
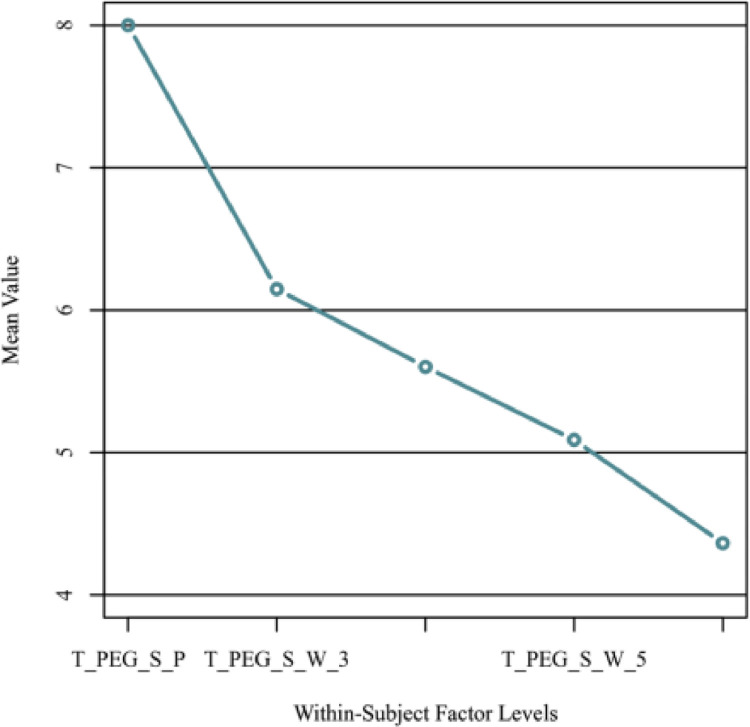
Figure 4.
Means Graph for Within-Subjects Variables for PEG Scale Scores.
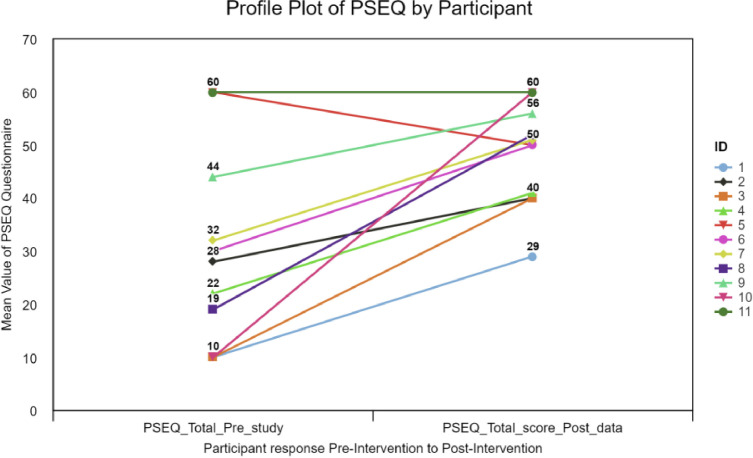
The result of this project reflected the intended goal. The target population of adults with chronic pain in a community pain management office provided a 6-week evidence-based practice intervention to enhance pain self-efficacy. The data collected demonstrated a statistically significant increase in patient-reported pain self-efficacy from baseline, as evidenced by the preintervention mean score of 29.55 (SD 18.40) and a post-intervention mean score of 48.09 (SD 9.61) (Fig. 5 & Table 3). Additional supporting data demonstrated that participants reported improvement in their perception of Pain, Enjoyment of Life, and General Activity reported using the PEG scale, showing a baseline of a mean of 8.00 (SD 1.30) to a mean of 4.36 (SD 1.09) at week 6. The results were examined based on an alpha of 0.05. The within-subjects factor's main effect was significant, F (4, 40) = 18.32, p < .001, indicating significant differences between the values of baseline total PEG Score and PEG scores collected at weeks 3 through the conclusion of the program at week 6. Table 4 presents the ANOVA results.
Figure 6.
Pre-intervention participant comments.
Figure 5.
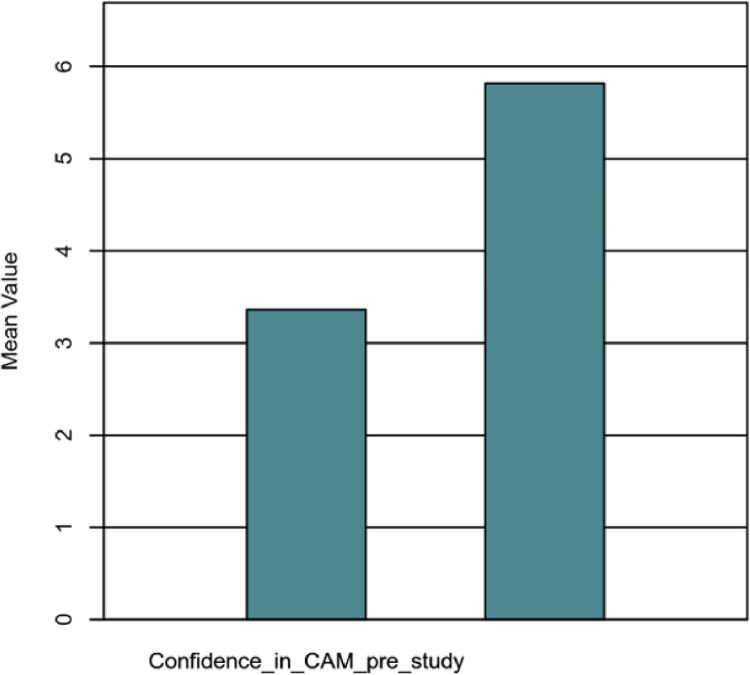
Pre and Post CAM confidence.
Table 3.
PSEQ Mean Score
| Pre-PSEQ |
Post-PSEQ |
|||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t | p | d |
| 29.55 | 18.40 | 48.09 | 9.61 | -3.83 | .003 | 1.16 |
Note: N = 11. Degrees of freedom for the t-statistic = 10. d represents Cohen's d.
Table 4.
Repeated Measure ANOVA PEG Score Over Time
| Source | df | SS | MS | F | p | ηp2 |
|---|---|---|---|---|---|---|
| Within-subjects | ||||||
| Within factor | 4 | 83.16 | 20.79 | 18.32 | < .001 | 0.65 |
| Residuals | 40 | 45.39 | 1.13 |
Participants endorsed greater confidence in the use of CAM interventions with a mean confidence level of 3.36 (SD = 2.25) at baseline and a mean of 5.82 (SD = 0.60) after completing the program. High satisfaction rates were represented by 91 % of the participants reporting they were extremely satisfied with the program, and 100% of the participants reported they would recommend the program to a friend or family member with chronic pain.
Discussion
Summary
Due to the subjective nature of chronic pain, quality improvement outcome measurements need to be patient-centered U.S. Department of Health and Human Services (HHS) 2019. Current literature has demonstrated that enhanced pain self-efficacy is a quantitative outcome measure for this qualitative experience. A score of 40 on the PSEQ questionnaire is consistent with better patient outcomes regardless of independent numeric pain scores (Nicholas, 2007). This score became the benchmark for this project.
The participants reported a mean pre-intervention PSEQ score of 29.55. The mean post score of 48.09 at the conclusion represented an 18.54 point mean improvement for the group. In terms of individual gains, 91% (n = 10) of participants reported a PSEQ ≥40, with the outlier (n = 1) showing an improvement of 19 points (Figure 3, Figure 5).
Figure 3.
Change in PSEQ by Participant.
These results were pertinent to the overall project aim, rationale, and goal. The data yielded a statistically significant difference in pre and post PSEQ responses by the target patient population. This project's key finding suggests that a NP-delivered intervention, such as PCST, effectively improves pain self-efficacy for the community-dwelling adult in a community pain office.
Providing an evidence-based nonpharmacologic intervention that met the needs of chronic pain patients during a global pandemic was the primary aim of this project. The impact of COVID 19 on chronic pain patients is well documented in the current literature. Containment strategies for the pandemic have amplified anxiety and depression, with greater than one in three adults in the US reporting anxiety or depressive disorder symptoms during the pandemic (Panchal et al., 2021). These symptoms are known to exacerbate chronic pain (US Pain Foundation, 2020). In the pain management field, leaders released position papers and clinical practice guidelines to support front-line clinicians in caring for this population (Puntillo et al., 2020; Shanthanna et al., 2020; Cohen et al.,2020). National clinical practice pain management guidelines call for nonpharmacologic interventions as a foundation for pain palliation (Tick et al., 2018). Through the PCST program, participants engaged in learning self-management skills and nonpharmacologic pain interventions that enhanced self-efficacy. Based on the foundation of Orem's theory of self-care, participants were empowered with self-management tools and real-life skills in an easily accessible format. Through weekly education that allowed participants to learn the rationale for each skill and reinforce skills from the previous week, confidence was enhanced. This was demonstrated through the participant's rating of their confidence in CAM modalities pre (3.36/6) and post (5.82/6) intervention with an increased mean confidence rating of 2.46 points on a six-point Likert scale . This confidence results in buy-in, which is necessary for patient engagement.
A literature review by Gobeil-Lavoie et al. (2019) found that patients are more likely to engage in self-care activities that they consider beneficial (Gobeil-Lavoie et al., 2019). Due to the multiple priorities that individuals with chronic conditions face, conflicts arise in using self-care practices. The change in both confidence in using CAM interventions for managing chronic pain and a statistically significant increase in pain self-efficacy scores demonstrated that the PCST program met the intended aim and aligned with the project's rationale.
All participants reported satisfaction in the program and improved confidence in the use of self-management nonpharmacologic CAM modalities. Self-management interventions are a vital component of the overall reduction in national health care expenditures for chronic disease. However, these interventions may have a more significant impact when providers clearly outline the benefits of self-management behaviors for the patient (Gobeil-Lavoie et al., 2019). PCST creates a framework to deliver nonpharmacologic pain management strategies to underserved populations while maintaining social distancing.
Project strengths
This project's primary strength is applying advanced nursing practice to identify an immediate need and rapidly implement an evidence-based, outcome-driven intervention in a narrow window of time. This project was implemented amid an unprecedented outbreak and delivered statistically significant results with high patient satisfaction ratings. Additional strengths include the ease of delivery and use of a group intervention that is effective both as a synchronous or asynchronous program. This flexibility allows for a patient-centered approach to the delivery of self-management skills training. Through empowering patients to maximize their autonomy, programs such as this carry the potential to decrease reliance on the health care system, thus reducing the overall financial burden of this and other chronic conditions. Patients endorsed their satisfaction with this program, with 91% expressing "completely satisfied" (n = 10). Additionally, comments related to a qualitative aspect were collected and shared via a word cloud.
Interpretation
Association between intervention, outcome, and similar studies
The statistical analysis of the results demonstrated a strong association between the patient-reported survey responses and the intervention. In addition, the pre- and post-study design suggest that the intervention's effect was the key driver for the statistically significant results. Multiple large-scale and small pragmatic trials have attempted to correlate patient-centered programs with improved pain outcomes such as pain self-efficacy.
Studies demonstrating similar results include Scriven et al. (2019), (Li and Tse, 2020), Bunzli et al. (2016), and Nost et al. (2018), citing clinically significant improvements in overall function, mood, physical activity, and pain levels. (Jinnouchi et al., 2021) conducted a community-based RCT for the management of chronic low back pain (CLBP), revealing that an individualized self-exercise program and low-frequency 100-minute direct teaching did not show additional improvement in pain intensity compared with material-based education but did enhance functional limitation, self-efficacy (PSEQ), and quality of life. This aligns with similar published studies reporting improved clinical significance despite a lack of statistical significance. Dear et al. (2018) published a study demonstrating long-term outcome data for an RCT (n = 490) of an internet-delivered pain management program for adults with chronic pain. The clinical improvements observed were maintained per their examination of the 12- and 24-month follow-up data. This study indicates that patient-centered pain education programs, such as the PCST, may have a lasting clinical effect.
The most closely aligned current literature is described by Broderick et al. (2014), providing a successful pain coping skills training program delivered by nurse practitioners in an RCT of 256 patients with osteoarthritis. Participants were randomized into treatment (N = 129) and control (N = 127). The intervention was delivered over ten in-person sessions versus the six sessions telehealth sessions described in this paper. The study team used the Arthritis Self-Efficacy Scale, an 8-item instrument that measures patients' perceived ability to perform specific behaviors to control arthritis pain and disability. While similar in concept to the PSEQ, responses were averaged to yield a score ranging from 1 to 10 (higher = greater self-efficacy). The team concluded that PCST is a viable and effective intervention that NPs can deliver to enhance self-efficacy for OA patients.
These studies reflect a small sample of recent similar studies that sought to engage patients through education and self-management both in-person and via telehealth. The PCST program presented in this paper demonstrates a more remarkable improvement in pain self-efficacy scores than other available studies. This may be due to the small sample size and personalized attention provided to participants in the synchronous program. In addition, due to the current climate of anxiety and depression related to COVID-19, this patient-centered program may have had a more significant impact on those who participated than previously published projects.
Opportunity cost and strategic trade-offs
There was no recognized loss of opportunity during the provision of this program. As a DNP student, the team lead engaged in all project activities as part of the doctoral program's clinical engagement hours. Future versions of this program should weigh the time of program delivery with the time required to educate and counsel individual patients about nonpharmacologic interventions, self-care, and self-management. The use of a group intervention delivered via telehealth may provide an opportunity to decrease overall individual office visit length or frequency, thus decreasing the cost of delivering evidence-based care. Using one NP to oversee the group, the program delivery format may have an opportunity to generate revenue through CPT codes for group psychological interventions or education. Additional value may be added related to enhanced patient outcomes. As previously discussed, self-management is predicted to decrease health care costs long term. Future areas of study may consider examining the time and cost per patient on a larger scale compared with usual care.
Impact of the project on people and systems
As with many chronic conditions, optimum chronic pain self-management may only be achieved when patients and professionals develop effective partnerships that integrate best practice resources, knowledge sharing, and practical skills in self-care interventions. Empowering pain sufferers with these tools cannot be accomplished during a brief office visit. Self-care strategies that have been reviewed in the context of this paper require education and coaching that requires a component of time that office providers may not have. The utilization of group activities that engage patients to learn self-management skills outside of the office visit has been explored in the literature as a feasible option to empower patients with tools and resources (Cameron et al., 2018).
Limitations
Limits to the generalizability of work
This small study represented a snapshot in time in a small cohort of participants. The impact of COVID-19 and health care delivery changes related to containment strategies prevented a comprehensive needs assessment and gap analysis of the individual outpatient practice. Ideally, the pain office staff and patients may have been assessed for baseline data collection and current practice related to the provision of nonpharmacologic interventions.
The sample size and length of the enrollment period impacted the overall results of this program. The COVID-19 pandemic and its impact on higher education and student engagement led to a shorter than expected time frame for this intervention. A 2-week participant recruitment window yielded 11 participants who wished to engage in the intervention. The program's original goal of 25 participants was not achieved due to this time restriction.
Although most enrolled participants felt confident in their ability to access the telehealth intervention or recording, technology malfunction and connection issues hindered a smooth delivery of program content at several points in the program timeline. Issues ranged from the inability to input the program website's web address to sound and connectivity malfunctions. These technology barriers led to program content being delayed or accessed as a recording instead of a live session on several occasions.
This project intended to incorporate a group dynamic. Scheduling conflicts between the participants and the project lead led to participants choosing the asynchronous option when they verbalized preferring the synchronous platform. Due to these conflicts, only two participants were able to engage as a group consistently. Two participants engaged in private sessions, and the remaining seven participants utilized the asynchronous video content. Future presentations of this content should seek to engage a more significant number of participants in a synchronous group program to assess the benefit of social interaction and peer support.
Factors limiting internal validity
The Hawthorne effect relates to study participants and the consequence of their awareness of being studied. This creates a potential impact on their behavior. This widely used term suggests that participants may not answer survey questions with the same response as if they were not involved in a program where their responses were being examined. This phenomenon may also impact a participant's engagement with a study intervention and other study participants (McCambridge et al., 2014). This phenomenon should be considered when analyzing and presenting data that rely solely on patient self-report, as is the case with this study.
Self-selection bias results when survey respondents decide entirely for themselves whether they will participate in a program. The participant's propensity for participating in the program correlates with the substantive topic the study team is trying to evaluate. Self-selection bias may impact resulting data as the respondents who choose to participate will not represent the entire target population (Lavrakas, 2008). Participants were self-selected in this program by the nature of their willingness to enroll. Self-management programs require a level of participant engagement. Individuals who were not interested in devoting weekly time to interact with the group visit or weekly recordings were excluded from the program due to their lack of willingness to be contacted by the project lead or proceed with the enrollment process. This excludes those who were unwilling to participate, leaving a gap in the data for this group.
The willing participants have determined there may be a benefit to the proposed intervention. This is assumed by the act of enrolling in an optional program. This self-determination may result in a placebo effect at some level. The placebo effect, however, is not a negative consequence. This dynamic psychoneurobiologic tool can be helpful in daily clinical practice for illness and symptom management within a wide variety of specialties and health care practices (Rossettini et al., 2020; Peiris et al., 2018). The impact of placebo and nocebo responses related to subjective symptoms is powerful in the context of self-management programs (Blasini et al., 2017). This potential limitation should be considered for other practitioners attempting to recreate a similar program.
Efforts made to minimize and adjust for limitations
As a small pilot project, the availability of options to avoid the limitations discussed was impeded. Participants were self-selected due to the desire to create a patient-centered intervention. The number of participants enrolled made it challenging to assess this project's impact on specific types of pain syndrome, length of time patients have been suffering from chronic pain, previous use of CAM interventions, age, gender, and other co-existing factors. The project team did not collect data on the participants' use and frequency of pharmaceutical interventions utilized. To ensure privacy, the participants' identity was not shared with the pain practice who referred them. Future programs may benefit from a more collaborative approach whereby office staff familiar with the participant run the weekly program. Additional value for this intervention may be obtained by collecting data on pre- and post-pharmaceutical utilization.
Conclusions
Usefulness of Work
Despite limitations and small sample size, this project demonstrated a NP-delivered program's impact on a vulnerable population. Chronic pain patients lack access to evidence-based nonpharmacologic intervention due to many factors, as previously described. The current global pandemic and state mandate on social distancing further amplify this disparity. The national epidemic of chronic pain and the immediate need to enhance the care of vulnerable patients required a timely implementation of telehealth-delivered programming that can enhance the quality of life for the local populations. The utilization of programs such as PCST, whereby patients are empowered to engage in self-management, can profoundly impact clinical and patient-centered outcomes. Management of persistent pain may be a lifelong task for many individuals. Self-management skills can provide a more sustainable solution to symptom management and can be personalized to reflect patient preferences and values (Dineen-Griffin et al., 2019).
Sustainability
The literature suggests a gap of adequately prepared community providers and resources to manage chronic pain individuals. Primary care providers lack pain management education and are ill-prepared to meet the needs of this patient population (Webster et al., 2019). Additional gaps exist for the provision of nonpharmacologic pain management options. This gap leads to unfavorable outcomes for patients with chronic pain (Tick et al., 2018). Nurse-led interventions such as this program carry the potential to partner with community-based practices and fill the need for specialist care through telehealth and education. It does not require physical space and has minimal requirements in terms of staffing. Therefore, it is well suited to be incorporated into a community primary care practice or chronic pain management office setting.
Potential for Spread to Other Contexts
This program may be considered in another context, most notably, primary care practices that care for patients with chronic pain. As the number of senior citizens grows, an increase in chronic pain from age-related degenerative changes such as osteoarthritis will increase (Barbour et al., 2017). A national population-based study found that 55.7% of all US adults reported some pain in the prior 3 months, of which 31.7% reported moderate to severe pain (Nahin, 2015). This population typically presents to their primary care practice to manage pain that interferes with quality of life. It is common for this population to seek treatment from a pain provider when the primary care office has exhausted all available pharmacologic and accessible nonpharmacologic interventions. Although an interdisciplinary pain management program is the evidence-based recommendation for managing this population, barriers such as lack of education in pain management, lack of time, and resources impede this model of care (Lincoln et al., 2013). APRN-directed programs such as PCST may provide a bridge to narrow the gap for this practice issue. Access to a referral resource may lessen the burden for the primary care provider and allow both patients and providers to improve the pain management experience.
Implications for Practice and Further Study in the Field
The current global focus on implementing innovative strategies to enhance health care delivery to vulnerable populations makes this work of particular significance. Recommendations of the 2011 National Academies of Science report, The Future of Nursing, delineate the APRN role to be pertinent to health promotion and patient populations' management, including prescribing pharmacologic and nonpharmacologic interventions (Altman et al., 2016). This abbreviated list of APRN competencies creates a strong foundation for PCST and its curriculum.
Practicing APRNs and pain management nurses are uniquely positioned to engage health care stakeholders by demonstrating outcome-producing interventions to change the health care delivery paradigm. APRNs are gaining expanded practice privileges to work to the full extent of their license and education. The impact of COVID-19 on APRN practice regulations allowed APRNs an expanded opportunity to showcase their clinical skills (Diez-Sampedro et al., 2020). As the advanced practice nurse engages in evidence-based care delivery implementation and dissemination, they will expand their reach to impact research, policy, advocacy, and enhanced patient care delivery models. Opportunities are abundant to provide enhanced care and reduce disparities across the lifespan.
Suggested Next Steps
Research is needed to identify more clinically applicable outcomes data for the patient with chronic pain. The availability of standardized clinical benchmarks that provide a meaningful evaluation of a qualitative experience may ensure that providers can advocate for payor support and resources. Numerous studies reviewed in this paper's creation call for further research into guidelines for a specific frequency and dosing of patient education, self-management strategies, and provider education.
The trifecta of chronic pain, the opioid epidemic, and uncertainties surrounding the COVID pandemic have generated a tsunami that has revealed great suffering and highlighted global disparities in identifying and treating pain. Nevertheless, as bleak as this may sound, a shining light is visible through this darkness. Hope created by advocates and innovators such as pain management clinical and advanced practice nurses can mitigate the impact of this storm. Seeking financial and programmatic support to develop, create, and implement pragmatic solutions for patient-centered care, pain management nurses have the power to soften suffering, hold space for healing, and guide patients with the light of hope that only a nurse can shine.
Declarations of Competing Interest
None.
Acknowledgments
The author would like to acknowledge the support and encouragement of the Wilmington University Doctor of Nursing Practice faculty, specifically Dr. Denise Lyons, and Dr. Aaron Sebach.
Appendix A

Appendix B
Appendix C

References
- Altman S.H., Butler A.S., Shern L, Change, Committee for Assessing Progress on Implementing the Recommendations of the Institute of Medicine Report the Future of Nursing: Leading Change, Advancing Health, Institute of Medicine, National Academies of Sciences, Engineering, and Medicine . National Academies Press; Washington, D.C.: 2016. Removing barriers to practice and care. [PubMed] [Google Scholar]
- Asghari A., Nicholas M.K. Pain self-efficacy beliefs and pain behaviour. A prospective study. Pain. 2001;94(1):85–100. doi: 10.1016/S0304-3959(01)00344-X. [DOI] [PubMed] [Google Scholar]
- Barbour K.E., Helmick C.G., Boring M., Brady T.J. Vital signs: Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation—United States, 2013-2015. MMWR. Morbidity and Mortality Weekly Report. 2017;66(9):246–253. doi: 10.15585/mmwr.mm6609e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennell K.L., Rini C., Keefe F., French S., Nelligan R., Kasza J., Forbes A., Dobson F., Abbott J.H., Dalwood A., Vicenzino B., Harris A., Hinman R.S. Effects of adding an internet-based pain coping skills training protocol to a standardized education and exercise program for people with persistent hip pain (HOPE Trial): Randomized controlled trial protocol. Physical Therapy. 2015;95(10):1408–1422. doi: 10.2522/ptj.20150119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasini M., Corsi N., Klinger R., Colloca L. Nocebo and pain: An overview of the psychoneurobiological mechanisms. Pain Reports. 2017;2(2):e585. doi: 10.1097/PR9.0000000000000585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Society of Regional Anesthesia and Pain Medicine (ASRA) (2020) Recommendations on chronic pain practice during the COVID-19 pandemic. Retrieved Month XX, XXXX, from https://www.asra.com/news-publications/asra-updates/blog-landing/legacy-b-blog-posts/2020/03/27/recommendations-on-chronic-pain-practice-during-the-covid-19-pandemichttps://www.nursingworld.org/∼495e9b/globalassets/docs/ana/ethics/theethicalresponsibilitytomanagepainandthesufferingitcauses2018.pdf, Accessed April 1, 2020
- Broderick J.E., Keefe F.J., Bruckenthal P., Junghaenel D.U., Schneider S., Schwartz J.E., Kaell A.T., Caldwell D.S., McKee D., Reed S., Gould E. Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: A randomized, controlled trial. Pain. 2014;155(9):1743–1754. doi: 10.1016/j.pain.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunzli S., McEvoy S., Dankaerts W., O'Sullivan P., O'Sullivan K. Patient perspectives on participation in cognitive functional therapy for chronic low back pain. Physical Therapy. 2016;96(9):1397–1407. doi: 10.2522/ptj.20140570. [DOI] [PubMed] [Google Scholar]
- Cameron J.E., Voth J., Jaglal S.B., Guilcher S.J.T., Hawker G., Salbach N.M. In this together”: Social identification predicts health outcomes (via self-efficacy) in a chronic disease self-management program. Social Science & Medicine. 2018;208:172–179. doi: 10.1016/j.socscimed.2018.03.007. [DOI] [PubMed] [Google Scholar]
- Cohen S.P., Baber Z.B., Buvanendran A., McLean B.C., Chen Y., Hooten W.M., Laker S.R., Wasan A.D., Kennedy D.J., Sandbrink F., King S.A., Fowler I.M., Stojanovic M.P., Hayek S.M., Phillips C.R. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Medicine. 2020;21(7):1331–1346. doi: 10.1093/pm/pnaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman B., Kean J., Brandt C., Peduzzi P., Kerns R. Adapting to disruption of research during the COVID-19 pandemic while testing nonpharmacological approaches to pain management. Translational Behavioral Medicine. 2020;10(4):827–834. doi: 10.1093/tbm/ibaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broderick, J. E., & Brunkenthal, P. (2018). Expanding access to pain coping skills training (PCST), a proffessional certification program to enable advanced practice nurses (APRN) to fill the gap (proposal to Pfizer). Retrieved Month XX, XXXX, from https://cdn.pfizer.com/pfizercom/funded_initiative_proposal/16004615%20-%20University%20of%20Southern%20California.pdf?fgUf0Wk6P_Pt6v8p3eZk_mdmm62V2WLu=., Accessed April 1, 2020
- Cuomo, A. (2020). Continuing Temporary Suspension and Modification of Laws Relating to the Disaster Emergency; Number 202.6
- Dear B.F., Gandy M., Karin E., Ricciardi T., Fogliati V.J., McDonald S., Staples L.G., Perry K.N., Sharpe L., Nicholas M.K., Titov N. The pain course: A randomized controlled trial comparing a remote-delivered chronic pain management program when provided in online and workbook formats. Pain. 2017;158(7):1289–1301. doi: 10.1097/j.pain.0000000000000916. [DOI] [PubMed] [Google Scholar]
- Dear B.F., Gandy M., Karin E., Fogliati R., Fogliati V.J., Staples L.G., Wootton B.M., Sharpe L., Titov N. The pain course: 12- and 24-month outcomes from a randomized controlled trial of an internet-delivered pain management program provided with different levels of clinician support. Journal of Pain. 2018;19(12):1491–1503. doi: 10.1016/j.jpain.2018.07.005. [DOI] [PubMed] [Google Scholar]
- Diez-Sampedro A., Gonzalez A., Delgado V., Flowers M., Maltseva T., Olenick M. COVID-19 and advanced practice registered nurses: Frontline update. Journal for Nurse Practitioners. 2020;16(8):551–555. doi: 10.1016/j.nurpra.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dineen-Griffin S., Garcia-Cardenas V., Williams K., Benrimoj S.I. Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PloS One. 2019;14(8) doi: 10.1371/journal.pone.0220116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gobeil-Lavoie A.P., Chouinard M.C., Danish A., Hudon C. Characteristics of self-management among patients with complex health needs: A thematic analysis review. BMJ Open. 2019;9(5) doi: 10.1136/bmjopen-2018-028344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heapy A.A., Higgins D.M., Goulet J.L., LaChappelle K.M., Driscoll M.A., Czlapinski R.A., Buta E., Piette J.D., Krein S.L., Kerns R.D. Interactive voice response-based self-management for chronic back pain: The COPES noninferiority randomized trial. JAMA Internal Medicine. 2017;177(6):765–773. doi: 10.1001/jamainternmed.2017.0223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinnouchi H., Matsudaira K., Kitamura A., Kakihana H., Oka H., Hayama-Terada M., Yamagishi K., Kiyama M., Iso H. Effects of brief self-exercise education on the management of chronic low back pain: A community-based, randomized, parallel-group pragmatic trial. Modern Rheumatology. 2021;31(4):890–898. doi: 10.1080/14397595.2020.1823603. [DOI] [PubMed] [Google Scholar]
- Kaivanto K.K., Estlander A.M., Moneta G.B., Vanharanta H. Isokinetic performance in low back pain patients: The predictive power of the Self-Efficacy Scale. Journal of Occupational Rehabilitation. 1995;5(2):87–99. doi: 10.1007/BF02109912. [DOI] [PubMed] [Google Scholar]
- Krebs E.E., Lorenz K.A., Bair M.J., Damush T.M., Wu J., Sutherland J.M., Asch S.M., Kroenke K. Development and initial validation of the PEG, a three-item scale assessing pain intensity and interference. Journal of General Internal Medicine. 2009;24(6):733–738. doi: 10.1007/s11606-009-0981-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavrakas P.J. Sage Publications, Inc; Thousand Oaks, CA: 2008. Encyclopedia of survey research methods (Vols. 1-0) [Google Scholar]
- Lincoln L.E., Pellico L., Kerns R., Anderson D. Barriers and facilitators to chronic non-cancer pain management in primary care: A qualitative analysis of primary care providers’ experiences and attitudes. Journal of Palliative Care & Medicine. 2013;S3:3–7. [Google Scholar]
- Li Y., Tse M.Y.M. An online pain education program for working adults: Pilot randomized controlled trial. Journal of Medical Internet Research. 2020;22(1):e15071. doi: 10.2196/15071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthias M.S., McGuire A.B., Kukla M., Daggy J., Myers L.J., Bair M.J. A brief peer support intervention for veterans with chronic musculoskeletal pain: A pilot study of feasibility and effectiveness. Pain Medicine. 2015;16(1):81–87. doi: 10.1111/pme.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCambridge J., Witton J., Elbourne D.R. Systematic review of the Hawthorne effect: New concepts are needed to study research participation effects. Journal of Clinical Epidemiology. 2014;67(3):267–277. doi: 10.1016/j.jclinepi.2013.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin R.L. Estimates of pain prevalence and severity in adults: United States, 2012. Journal of Pain. 2015;16(8):769–780. doi: 10.1016/j.jpain.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine (NASEM) Health and Medicine Division. Board on Health Sciences Policy. Committee on Pain Management and Regulatory Strategies to Address Prescription Opioid Abuse . In: Pain management and the opioid epidemic: Balancing societal and individual benefits and risks of prescription opioid use. Phillips J.K., Ford M.A., Bonnie R.J., editors. National Academies Press; Washington, D.C.: 2017. Retrieved January 15, 2020, from https://www.ncbi.nlm.nih.gov/books/NBK458655/ [PubMed] [Google Scholar]
- National Institute of Health (NIH) NIH; Washington, DC: 2016. National pain strategy: A comprehensive population health-level strategy for pain. Retrieved January 15, 2020, from https://iprcc.nih.gov/docs/HHSNational_Pain_Strategy.pdf. [Google Scholar]
- Nicholas M.K. The pain self-efficacy questionnaire: Taking pain into account. European Journal of Pain. 2007;11(2):153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- Nøst T.H., Steinsbekk A., Bratås O., Grønning K. Twelve-month effect of chronic pain self-management intervention delivered in an easily accessible primary healthcare service - A randomised controlled trial. BMC Health Services Research. 2018;18(1):1012. doi: 10.1186/s12913-018-3843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchal, N., Kamal, R., Muñana, C., Chidambaram, P., Orgera, K., Cox, C., Rachel Garfield, & Hamel, L. (2021). The Implications of COVID-19 for Mental Health and Substance Use. Retrieved September 27, 2020, from https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/.
- Peiris N., Blasini M., Wright T., Colloca L. The placebo phenomenon: A narrow focus on psychological models. Perspectives in Biology & Medicine. 2018;61(3):388–400. doi: 10.1353/pbm.2018.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M.L., Smeets E., Feijge M., van Breukelen G., Andersson G., Buhrman M., Linton S.J. Happy despite pain: A randomized controlled trial of an 8-week internet-delivered positive psychology intervention for enhancing well-being in patients with chronic pain. Clinical Journal of Pain. 2017;33(11):962–975. doi: 10.1097/AJP.0000000000000494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puntillo F., Giglio M., Brienza N., Viswanath O., Urits I., Kaye A.D., Pergolizzi J., Paladini A., Varrassi G. Impact of COVID-19 pandemic on chronic pain management: Looking for the best way to deliver care. Best Practice & Research. Clinical Anaesthesiology. 2020;34(3):529–537. doi: 10.1016/j.bpa.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qaseem A., Wilt T.J., McLean R.M., Forciea M.A., Clinical Guidelines Committee of the American College of PhysiciansDenberg T.D., Barry M.J.…Vijan S. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of internal medicine. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- Rossettini G., Camerone E.M., Carlino E., Benedetti F., Testa M. Context matters: The psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Archives of Physiotherapy. 2020;10(1):1–11. doi: 10.1186/s40945-020-00082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scriven H., Doherty D.P., Ward E.C. Evaluation of a multisite telehealth group model for persistent pain management for rural/remote participants. Rural Remote Health. 2019;19(1):4710. doi: 10.22605/RRH4710. [DOI] [PubMed] [Google Scholar]
- Shanthanna H., Strand N.H., Provenzano D.A., Lobo C.A., Eldabe S., Bhatia A., Wegener J., Curtis K., Cohen S.P., Narouze S. Caring for patients with pain during the COVID-19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia. 2020;75(7):935–944. doi: 10.1111/anae.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skelly A.C., Chou R., Dettori J.R., Turner J.A., Friedly J.L., Rundell S.D., Fu R., Brodt E.D., Wasson N., Winter C., Ferguson A.J.R. Noninvasive nonpharmacological treatment for chronic pain: A systematic review. AHRQ Comparative Effectiveness Reviews. 2018 Report No: 18-EHC013-EF. [PubMed] [Google Scholar]
- Taylor S.J.C., Carnes D., Homer K., Kahan B.C., Hounsome N., Eldridge S., Spencer A., Pincus T., Rahman A., Underwood M. Novel three-day, community-based, nonpharmacological group intervention for chronic musculoskeletal pain (COPERS): A randomized clinical trial. PLoS Medicine. 2016;13(6) doi: 10.1371/journal.pmed.1002040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tick H., Nielsen A., Pelletier K.R., Bonakdar R., Simmons S., Glick R., Ratner E., Lemmon R.L., Wayne P., Zador V., Pain Task Force of the Academic Consortium for Integrative Medicine and Health Evidence-based nonpharmacologic strategies for comprehensive pain care: The Consortium Pain Task Force white paper. Explore (N.Y.) 2018;14(3):177–211. doi: 10.1016/j.explore.2018.02.001. [DOI] [PubMed] [Google Scholar]
- Trudeau K.J., Pujol L.A., DasMahapatra P., Wall R., Black R.A., Zacharoff K. A randomized controlled trial of an online self-management program for adults with arthritis pain. Journal of Behavioral Medicine. 2015;38(3):483–496. doi: 10.1007/s10865-015-9622-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) (2019). Pain management best practices inter-agency task force report: Updates, gaps, inconsistencies, and recommendations. from https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf (Accessed 1 September 2020).
- Webster F., Rice K., Katz J., Bhattacharyya O., Dale C., Upshur R. An ethnography of chronic pain management in primary care: The social organization of physicians' work in the midst of the opioid crisis. PloS One. 2019;14(5) doi: 10.1371/journal.pone.0215148. [DOI] [PMC free article] [PubMed] [Google Scholar]