Abstract
Purpose
To better understand the needs and experiences of the X-linked carrier community to improve future recognition, diagnosis, and treatment by bringing X-linked carrier voices together.
Methods
An anonymous survey link was distributed to members of Remember the Girls, a non-profit organization for female (XX) carriers of X-linked conditions, through its website, Facebook group, Instagram, and Twitter. The survey was developed to gather data on XX carriers of numerous X-linked conditions.
Results
One hundred and fifty individuals participated in the study. The majority (81/150) of individuals learned about their carrier status by giving birth to a son diagnosed with an X-linked condition. However, over 80% (120/145) believed that they should learn this information before the age of 18. Over 80% of participants (124/148) felt that they either have or may have symptoms attributable to their X-linked condition. Yet, only 10.1% (15/148) felt that they had sufficient access to knowledgeable healthcare providers and/or medical information. Additionally, 46.7% (70/150) of participants reported that healthcare providers did not discuss reproductive options with them. Improving carrier access to medical information, research studies, new treatments, and reproductive methods was found to be the top priority.
Conclusion
Limited information exists on X-linked carriers’ risk for symptoms and there is a lack of available treatments. This study demonstrates the need for more knowledgeable healthcare providers and medical information within the X-linked carrier community.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10815-021-02270-6.
Keywords: Symptomatic female (XX) carrier, X-linked condition, Reproductive genetics, Care management
Introduction
While the majority of genetic conditions are caused by changes or variations in the 22 autosomes, more than 100 genetic conditions can be attributed to changes in the X and Y chromosomes commonly referred to as the sex chromosomes. Of the disorders related to the sex chromosomes, the majority are X-linked, caused by changes in genes on the X chromosome.
A person carrying one X chromosome and one Y chromosome will typically display the phenotype of the X-linked condition, whereas a person with two X chromosomes typically does not. XX individuals heterozygous for X-linked conditions are generally considered to be carriers and are thought to be unaffected or mildly affected [1, 2]. Since XX individuals have two copies of the X chromosome, it is generally believed that the copy with the pathogenic variant tends to be randomly inactivated, while the second copy masks the effect of the pathogenic variant [3]. This process, known as X-inactivation, ensures that genes on the X chromosome are expressed at similar levels in XY and XX individuals [4]. However, when there is skewed or unequal distribution of the X chromosome that is inactivated, carriers may express symptoms and present with a wide spectrum of clinical manifestations that can range between undetectable/mild and severe [5–7].
Historically, carriers of both autosomal recessive and X-linked conditions were commonly believed to be asymptomatic. However, as genetic testing and population screening evolve, research has shown that carriers can be at risk for symptoms [2], underscoring the importance of communicating information and potential risks to individuals identified as carriers. Many medical providers have limited knowledge about the possible symptoms and risks associated with being a carrier, especially of X-linked conditions [8]. This may be attributed to the limited number of studies that address the different phenotypes, disease onset, and progression in XX carriers compared to affected XY individuals [9]. As a result, carriers are often underdiagnosed and have limited access to information regarding how to handle or find a treatment for symptoms. Additionally, carriers are typically not included in clinical trials [10].
Carriers of X-linked conditions often only find out about their carrier status when learning that a XY relative such as a father, brother, uncle, or nephew is affected with a condition or when a XY child is diagnosed. The diagnosis of X-linked adrenoleukodystrophy (X-ALD) in women is rarely made without an affected XY relative, and many symptomatic XX carriers are misdiagnosed until a family history is determined [1]. Carriers of many X-linked conditions, who are often unaware of their carrier status, may experience symptoms and/or complications that warrant medical management. For example, carriers of Duchenne or Becker muscular dystrophy (DMD/BMD) and Fabry disease are at an increased risk for cardiomyopathy and may want to consider routine echocardiograms [5, 11–13]. Knowledge of one’s carrier status for an X-linked condition may impact future reproductive planning; therefore, it is imperative that individuals be provided with counseling regarding the specific X-linked condition, risk to carriers, and reproductive options available. For example, XX premutation carriers of fragile X syndrome have an increased risk for primary ovarian insufficiency and may want to consider embryo and/or oocyte cryopreservation to preserve fertility. Many carriers of fragile X syndrome do not even know of their carrier status until they start having fertility issues, at which time it can be difficult or impossible to begin banking oocytes/embryos [14, 15].
Carriers of more severe X-linked conditions have been found to want to avoid having an affected child. Conditions like Lesch-Nyhan syndrome and Menkes disease are associated with progressive disability during childhood that leads to death by early adulthood [16]. As there is a 50% chance of passing the pathogenic variant to a future child for most X-linked conditions, XX individuals may consider alternative reproductive options such as in vitro fertilization with preimplantation genetic testing (IVF with PGT), use of donor eggs, adoption, and/or diagnostic testing during pregnancy such as chorionic villus sampling/amniocentesis. However, carriers often receive judgment for choosing options such as prenatal diagnostic testing or IVF with PGT since it can be viewed as unethical by some individuals [17]. This can add to the difficulty of the decision-making process for XX carriers. Some carriers, on the other hand, choose to not have more biological children after learning about their carrier status.
While studies focusing on specific X-linked conditions exist, there are no studies that explore the needs of the X-linked carrier community. In 2019, a survey was conducted by Remember the Girls, a non-profit organization that aims to unite, educate, and empower XX carriers of X-linked conditions. This survey found that 70% of X-linked carriers felt that they either had or likely had physical symptoms attributable to their condition, but only 9% felt that they had sufficient access to medical information concerning those symptoms. Additionally, 85% wanted to know about their carrier status before the age of 18 (Remember the Girls, 2019). While this initial survey was not published, it highlighted the importance of exploring this topic on a larger scale. By bringing many carrier voices together, the goal of this study was to better understand the needs and experiences of the X-linked carrier community to improve future recognition, diagnosis, and treatment.
Methods
Participants
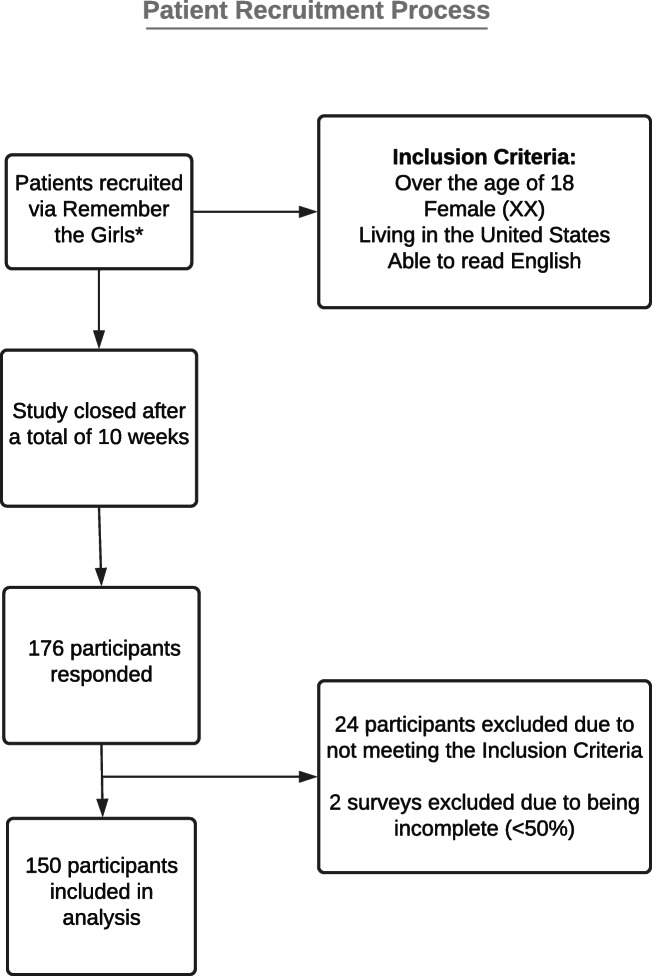
Participants were recruited through Remember the Girls. The organization has over 800 members, and after a recent outreach campaign, most members of specific X-linked condition groups are now also members of Remember the Girls. While only members of Remember the Girls were targeted for this study, a snowball sampling method was utilized to identify other potential participants (Fig. 1).
Fig. 1.
Patient recruitment process. *The survey invitation asked participants to share the survey with other X-linked carriers and their network
In order to be eligible for the study, participants were required to be over the age of 18, XX, living in the USA, and able to read English. Individuals not fitting these parameters were excluded. Participants were also asked to select the condition for which they are a carrier. The main author (JC) reviewed the text entries for all participants who selected “Other” once the survey was closed to confirm that they were carriers of X-linked conditions. Their carrier status was self-reported and not confirmed by laboratory tests.
Procedures
The anonymous online survey was distributed to members of Remember the Girls through their website, Facebook group, Twitter, and Instagram. In the invitation to take the survey, participants were asked to share the survey with other eligible family members or members of their individual X-linked groups. Participants provided consent by agreeing to the first page of the study. A disclaimer was included on the consent form noting that the survey had been distributed to multiple groups and asked participants to only complete the survey once.
The survey was open for a total of 10 weeks beginning on October 10, 2020. Participants who completed the survey were offered a chance to win one of 20 $25 Visa gift cards as an incentive. Contact information for the raffle was collected in a separate form unlinked to their responses.
Instrumentation
A 31-question quantitative survey (Online Resource 1) was developed to gather data on the experiences and needs of XX carriers of numerous X-linked conditions. The survey drew from the initial survey conducted by Remember the Girls and was modified to address the objectives of this study. Survey data was collected through the Qualtrics web application and included multiple choice, Likert scale, and free response questions. Questions addressed X-linked carriers’ experiences with carrier identification, access to medical information such as potential symptoms and/or risks associated with being a carrier, reproductive plans, preferences for reproductive options, and priority of needs. Demographic data such as gender identity, age, ethnicity, religion, education level, employment status, marital status, and household income were included at the end of the survey. The survey took approximately 10 minutes on average to complete.
IRB approval
This study was submitted to the Northwestern University IRB and was deemed exempt (IRB ID no. STU00213427).
Data analysis
Data analysis was completed using IBM SPSS Statistics (Version 26). Question-specific response rates varied since all questions other than the inclusion criteria questions were voluntary and skip-logic was used. All data was analyzed regardless of the total number of responses for each question. Descriptive statistics were computed for all numerical variables. Chi-square statistics or Fisher’s exact test was used to compare categorical variables, and p-values (p < 0.05) were used to determine if the associations, if any, between responses were statistically significant. Inferential statistics were used to deduce what the broader X-linked carrier community might think about their needs and experiences.
The responses from the open-ended survey question were analyzed as follows: a master list of codes was developed by JC and themes and subthemes were created. An initial analysis was then completed by JC and co-author LP and then reviewed for consistency. Direct quotes from the open-ended survey question were selected to illustrate participants’ experiences (see Online Resource 2).
Results
Demographics
A total of 179 individuals participated in the study. Twenty-nine responses were excluded because they did not meet the inclusion criteria, which left 150 responses to be analyzed. Online Resource 3 includes the detailed demographic features of the participants. The majority of participants were between 30 and 50 years of age (65.8%, n = 96/146), White (non-Hispanic/Latinx) (89.1%, n = 131/147), and have a bachelor’s degree or higher (59.9%, n = 88/147). Of note, 100% (n = 147) identified as female. Twenty-one X-linked conditions were represented, with 46.3% (n = 69/149) of participants being carriers of X-ALD (Table 1).
Table 1.
List of X-linked conditions represented
| Conditions represented | n = 149 |
|---|---|
| Aarskog syndrome | 2 (1.3%) |
| Adrenoleukodystrophy | 69 (46.3%) |
| Alport syndrome | 4 (2.7%) |
| Barth syndrome | 2 (1.3%) |
| Blue cone monochromacy | 11 (7.4%) |
| Choroideremia | 1 (0.7%) |
| Chronic granulomatous disease | 10 (6.7%) |
| Conradi Hunermann | 1 (0.7%) |
| Duchenne/Becker muscular dystrophy | 9 (6.0%) |
| Fragile X syndrome (premutation carrier) | 5 (3.4%) |
| Hemophilia A/B | 6 (4.0%) |
| Kennedy’s disease | 4 (2.7%) |
| L1 syndrome | 2 (1.3%) |
| Lesch-Nyhan syndrome | 3 (2.0%) |
| MECP2-related disorders | 5 (3.4%) |
| Myotubular myopathy | 5 (3.4%) |
| Ornithine transcarbamylase deficiency | 2 (1.3%) |
| X-linked chondrodysplasia punctata type 1 | 1 (0.7%) |
| X-linked hypophosphatemia | 1 (0.7%) |
| X-linked ichthyosis | 5 (3.4%) |
| X-linked severe combined immunodeficiency | 1 (0.7%) |
Experience with carrier identification
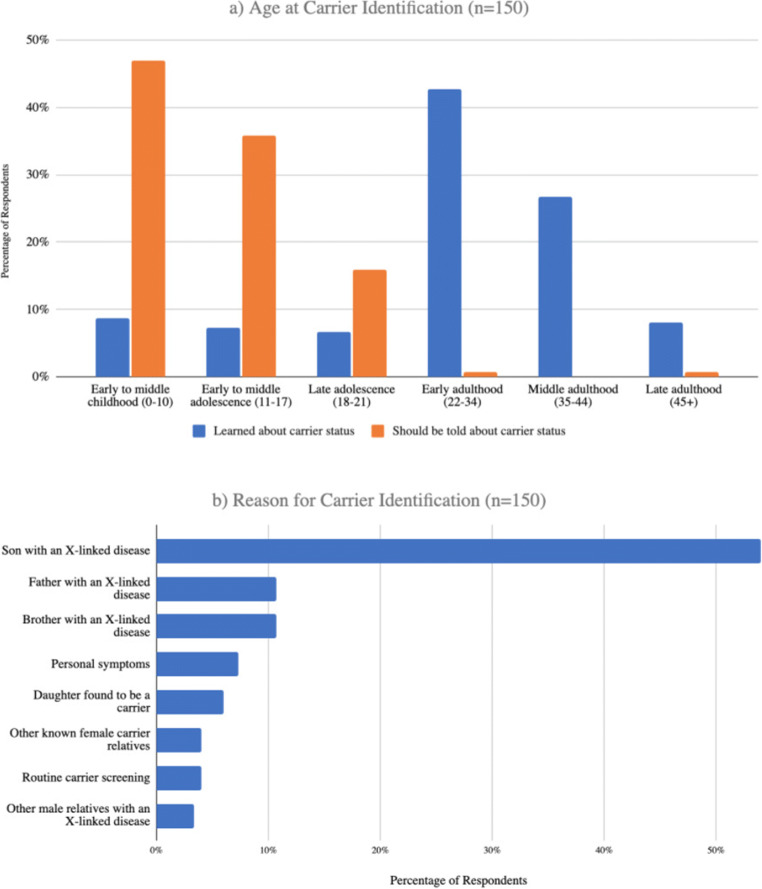
The mean age at which participants learned about their carrier status was 29 years (Fig. 1a). Only 16% (n = 24/150) of participants learned this information before the age of 18. However, the mean age at which participants believed that carriers should be told was 11 years (Fig. 2a). Over 80% (n = 120/145) of participants believe that they should be told before the age of 18. One participant stated, “I may not have fully understood my carrier status when I was 11, however, it did allow me to make informed decisions about future reproduction.” Most participants (54.0%, n = 81/150) initially learned about their carrier status by giving birth to a son diagnosed with an X-linked condition (Fig. 2b).
Fig. 2.
Experiences with carrier identification. a) The age at which carriers learned that they were a carrier of an X-linked condition in comparison to the age at which they believe individuals should be told they are carriers. b) How carriers initially learned about their carrier status
Access to medical information regarding symptoms and treatments
Over 80% of participants (n = 124/149) felt that they either have symptoms or may have symptoms attributable to their X-linked condition (Table 2). In order to assess participants’ awareness regarding risk for symptoms, the X-linked conditions that were represented in this study were categorized into two groups: known symptoms in the carrier population and no known symptoms in the carrier population. Nearly all of those in the “no symptom” group were not aware of a risk to experience symptoms (Table 3). There were only 20.8% (n = 5/24) of participants in the “no symptom” group that felt they experienced symptoms. However, among the “symptom” group, we see that less than half of the cohort (48.8% n = 61/125) was aware that they could be at risk for symptoms but over 65% (n = 82/125) reported being symptomatic. The awareness level between the “symptom” group and “no symptom” group was found to be statistically significant (Fisher’s exact, p < 0.001).
Table 2.
Access to medical information regarding symptoms and treatments. Participants’ experience of symptoms attributable to their X-linked condition
| Yes | No | Maybe | Total | |
|---|---|---|---|---|
| “Symptom” group | 82 | 16 | 27 | 125 |
| “No symptom” group | 5 | 9 | 10 | 24 |
| Total | 87 | 25 | 37 | 149 |
Table 3.
Access to medical information regarding symptoms and treatments. Awareness of risk when participants first learned of their carrier status
| Yes | No | Total | |
|---|---|---|---|
| “Symptom” group | 61 | 64 | 125 |
| “No symptom” group | 2 | 22 | 24 |
| Total | 63 | 86 | 149 |
*p < 0.001
Similarly, the X-linked conditions represented in this study were recategorized into two groups: known treatment for carriers and no known treatment for carriers to assess participants’ awareness of any medications, treatments, or therapies for their symptoms. Among the “no treatment” group, participants were generally not at all aware of any available treatments (69.8%, n = 30/43) (Table 4). Among the “treatment” group, there is more variability in the responses with the most participants somewhat aware to not at all aware (70.8%, n = 75/106). The awareness level between these two groups was found to be statistically significant (p < 0.001).
Table 4.
Awareness of medications/treatments/therapies for symptoms experienced by carriers of the participant’s X-linked condition
| Extremely aware | Moderately aware | Somewhat aware | Slightly aware | Not at all aware | Total | |
|---|---|---|---|---|---|---|
| “Treatment” group | 17 | 14 | 20 | 19 | 36 | 106 |
| “No treatment” group | 1 | 4 | 3 | 5 | 30 | 43 |
| Total | 18 | 18 | 23 | 24 | 66 | 149 |
*p < 0.001
Only 10.1% (n = 15/148) of participants felt that they had sufficient access to knowledgeable healthcare providers and/or medical information concerning possible symptoms and/or risks associated with being a carrier. Several participants expressed that, “Many doctors have not believed me that carriers can have symptoms, the severity of symptoms, or that I could have symptoms at a younger age.”
Reproductive plans and preferences for reproductive options
Participants reported that their healthcare providers did not discuss reproductive options with 46.7% (n = 70/150) of them (Figure 3a). For those who indicated their reproductive options were discussed, prenatal diagnostic testing was discussed the most often (75.0%, n = 60/80), followed by IVF with PGT (68.8%, n = 55/80). Using an oocyte donor was discussed the least often (26.3%, n = 21/80). When analyzing preferred reproductive options when cost is not a barrier, the majority (61.7% n = 71/115) indicated they would prefer IVF with PGT (Figure 3b). Over 22% (n = 34/149) would not choose an alternative reproductive option. One participant stated, “I wish for more understanding and knowledgeable doctors and counselors about options, and not discouragement about having naturally and taking a chance as well.”
Fig. 3.
Reproductive options. a) Participants reported that these options were discussed by their healthcare provider. b) Participants preferred these options if cost or insurance were not a barrier. *Participants could select all that apply
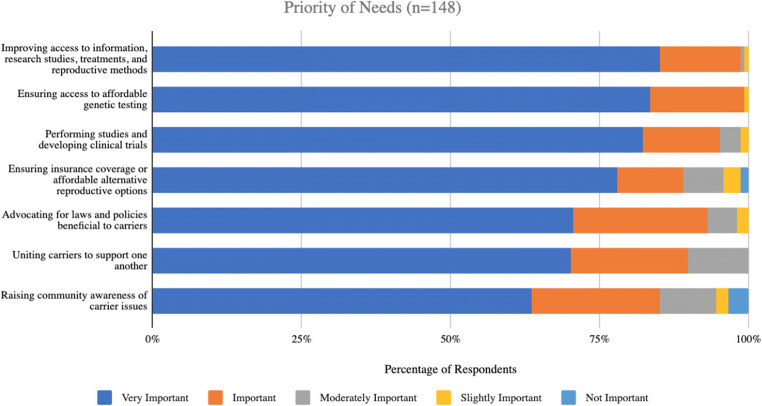
Needs of the X-linked carrier community
In order to assess the needs of the X-linked carrier community, participants were provided with statements and asked how important each statement was to them. The statement that was most commonly seen as “Very Important” was “Improving carrier access to medical information, research studies, new treatments, and reproductive methods,” (85.1%, n = 126/148) (Figure 4). Other commonly selected statements include “Ensuring that all potential carriers have access to affordable genetic testing to determine or confirm carrier status,” (84.1%, n = 122/145) and “Mobilizing the medical community to perform studies and develop clinical trials for XX carriers to help identify treatments/cure” (82.2%, n = 120/146).
Fig. 4.
Priority of needs among X-linked carriers. Participants were asked to select how important certain statements were related to their X-linked disease. *Participants were provided the following options: Very Important, Important, Moderately Important, Slightly Important, and Not Important
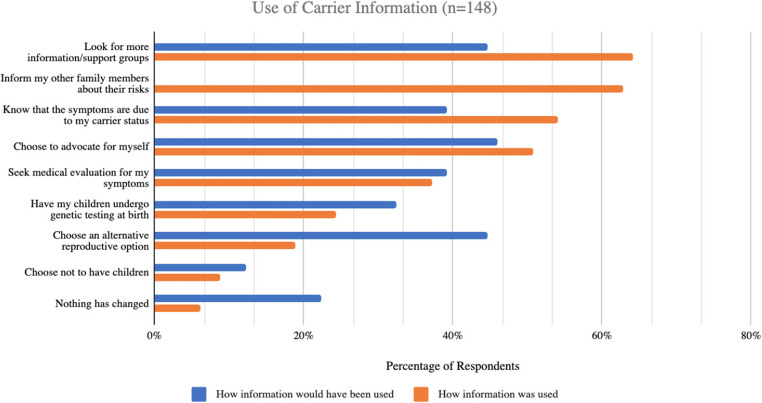
In order to delineate how early knowledge of carrier status impacted decision-making, participants were asked to select various statements describing what action they would have taken with early identification compared to the action they ended up taking once they were actually identified as a carrier. The most commonly selected statements for when participants had early knowledge were “I would have been able to advocate for myself more” (45.9%, n = 68/148), “I would have looked for more information/support groups” (44.6%, n = 66/148), and “I would have considered an alternative reproductive option” (44.6%, n = 66/148) (Figure 4). When describing how learning information about their carrier status impacted them, the most commonly selected statements were “I looked for more information/support groups” (64.2%, n = 95/148), “I was able to or plan to inform my other family members about their risks” (62.8%, n = 93/148), and “I know that the symptoms I am experiencing are due to my carrier status” (54.1%, n = 80/148) (Figure 5). The statements “I would have considered an alternative reproductive option,” “I would have had my children undergo genetic testing at birth,” “I would have chosen not to have children,” and “I would have known that there were associated symptoms with my carrier status and sought out medical evaluation” describe what they would have done differently. Three of those four statements demonstrate that participants would have made changes to their family planning if they had known about their carrier status earlier.
Fig. 5.
How information about X-linked carrier status would have been used if it was known earlier in comparison to the impact of learning information about carrier status
Discussion
This study is the first to bring together carrier voices aimed to better understand the experiences and perspectives of the X-linked carrier community. It establishes that there is a need for more information on X-linked carriers and better access to knowledgeable healthcare providers, research studies, clinical trials, treatments, and alternative reproductive methods.
While historically it was thought that carriers were asymptomatic, the majority of participants in this study experienced symptoms they felt were attributable to their X-linked condition. While they may still be viewed as asymptomatic by medical providers, this is a reflection of the patient experience and the limited information available regarding symptoms associated with being a carrier for an X-linked condition. However, most were not aware that they could be at risk for symptoms when they first learned about their carrier status. This suggests that X-linked carriers are not consistently or thoroughly counseled on their risk for symptoms. As all of these conditions are classified as rare disorders, access to specialty clinics or knowledgeable providers are not readily available to all and could impact patient awareness levels. Even once X-linked carriers find out that their symptoms are attributable to their carrier status, they find it difficult to find a healthcare provider who understands their risks and is able to provide the care that is needed, indicating a lack of providers who are knowledgeable on X-linked conditions and the potential symptoms associated with them. This may be because practice-based guidelines [18] are not available for every X-linked condition so providers do not know how to counsel patients about the risk for symptoms and the availability of treatments.
Of all the X-linked conditions that were represented in this study, only DMD/BMD, Fabry disease, and fragile X syndrome have professional guidelines. In order for more guidelines to be created, additional research studies and clinical trials on X-linked carriers are needed. Critically, this is a need that the X-linked carrier community recognizes. On top of creating more guidelines for how to treat the carrier population, it is important for healthcare providers to counsel carriers on communicating with their extended families about the risks and heredity patterns of the X-linked condition they are affected by. Many studies show that carriers do not disclose to their families for numerous reasons, indicating that it is critical they are advised of the importance of and ways to initiate these conversations [19]. Additionally, as we learn more about the risks associated with individuals who are heterozygotes, currently referred to as “carriers” for these X-linked conditions, we also need to consider re-evaluating the language and terminology that is being used as carrier is not the most appropriate term for these individuals.
Another barrier faced by the X-linked carrier community is that they often do not know about their carrier status until they have an affected son. While most participants found out about their carrier status in early to middle adulthood, they felt that carriers should learn about their carrier risk by middle adolescence. These findings are consistent with previous research studies on when X-linked carriers are made aware of their carrier risk and when they would be able to cope with the result [20]. Knowing this information ahead of time by having access to affordable testing allows carriers to make informed reproductive decisions [17]. Participants agree that if they had found out about their carrier status earlier, they would have had reproductive options that were not available to them previously. The 2015 expanded carrier screening joint statement states that “the goal of preconception and prenatal carrier screening is to provide couples with information to optimize pregnancy outcomes based on their personal values and preferences” [21]. However, if X-linked carriers want information about their carrier status but do not currently have an avenue to receive this information, it raises questions about whether we are accomplishing this goal and providing appropriate healthcare to patients. Furthermore, most genetic testing laboratories in the US currently do not test minors unless they are pregnant due to ethical concerns about patient autonomy [22]. While carrier screening focuses on reproductive risks, X-linked carriers have a risk to develop symptoms. For this reason, it may be appropriate to develop a system in which a gene panel of X-linked conditions be offered at primary care offices during routine visits for XX individuals between ages 11 and 18 years.
Some X-linked conditions such as Alport syndrome and Ornithine transcarbamylase deficiency have childhood onset symptoms for XX carriers [23, 24]. This raises the question of whether XX individuals with a known family history of an X-linked condition should have the option to get genetic testing at a younger age. However, more information is needed on whether and how genetic testing could change the management of symptoms for X-linked carriers in order to change the testing guidelines and allow patients to be tested before the age of 18 [25]. Additionally, over the years, the types of conditions included on newborn screening programs have expanded to include certain X-linked conditions such as X-ALD and DMD [26]. At the moment, results are generally only returned for affected XY individuals but not XX carriers. As more and more research shows that these X-linked carriers can be symptomatic themselves, additional consideration and evaluation should be given to returning results for them as well.
Most participants reported that a healthcare provider had not discussed any alternative reproductive options with them. Those who did have an alternative reproductive option discussed were told about prenatal diagnostic testing the most often, which was the second to least preferred option. This highlights the need for healthcare providers to discuss all available options to carriers, including natural conception [3]. When given the option to choose any alternative reproductive option, the vast majority of participants chose IVF with PGT. Unfortunately, cost for these services is a barrier for most individuals and cost plays a vital role in the decision-making process. Many insurance companies will financially cover or reimburse IVF for infertile couples but will not solely for X-linked carriers [27]. Interestingly, using an oocyte donor was the least preferred alternative reproductive option by participants even though using an oocyte donor is one way to almost guarantee not passing down an X-linked condition, assuming the oocyte donor had negative expanded carrier screening including the specific X-linked condition. While participants did not cite specific reasons for not wanting to use an oocyte donor, previous studies indicate that the absent genetic connection varies in significance between mothers. Many women reported the child felt like theirs, while others struggled with the idea that their child was not genetically related to them [28].
The study was limited by a survey that was not validated and a small sample size. While this study was the first IRB-approved study to our knowledge that examined the experiences of the X-linked carrier community and brought together many voices of the X-linked carrier community, it is not generalizable. In addition, this study surveyed a targeted population—members of an advocacy group. Many individuals in advocacy groups have an affected child or are symptomatic themselves. This may have skewed the data towards those who are more information-seeking. The cohort was also skewed towards the X-ALD carrier community as the founder of Remember the Girls is an X-ALD carrier. The use of the snowball sampling method may have led to the overrepresentation of this group. In addition, our sample consisted of primarily White individuals which is not representative of the experiences of the whole X-linked carrier community.
Future areas of study include exploring the experience of X-linked carriers of more diverse backgrounds and those living outside of the US. Experiences may be different for individuals living in other countries since their healthcare system, systems of support, and regulations surrounding genetic testing may differ. It was not possible to determine whether the experiences and needs of X-linked carriers were truly the same from one X-linked condition group to the other. Additional exploration to examine possible differences between various X-linked groups is also important. Future studies should expand upon these findings by increasing the cohort size and reaching out to targeted groups that have symptoms and targeted groups that do not have symptoms to see how their experiences may differ. Another future area of study involves a longitudinal project in which teens are offered a gene panel consisting of X-linked conditions. Subjects’ attitudes and reproductive actions could be studied and assessed over time.
Conclusion
This study begins to describe the experience of the X-linked carrier community. Currently, there is limited information available on their risk for symptoms and the availability of treatments, and there is a need for more knowledgeable healthcare providers and medical information. This study suggests that healthcare providers should inform XX carriers that they could be at risk for symptoms, be receptive to patients who express having symptoms, and recommend them to the necessary specialists. Healthcare providers should also present all available reproductive options to X-linked carriers regardless of cost/insurance coverage. In order to make these changes, there needs to be guidelines and education so that healthcare providers can be informed.
Supplementary Information
(PDF 100 kb)
(PDF 133 kb)
(PDF 113 kb)
Acknowledgements
The research was conducted as part of a Master’s thesis project for the Northwestern University Graduate Program in Genetic Counseling. Funding for the study was provided by Northwestern University. We thank the members of Remember the Girls for participating in the survey and sharing it with other X-linked carriers.
Code availability
Not applicable.
Funding
The Northwestern University Graduate Program in Genetic Counseling provided funding for this Master’s thesis project.
Data availability
The data that support the findings of this study are available upon request from the corresponding author.
Declarations
Ethics approval
This study was reviewed and approved by the Northwestern University Institutional Review Board (STU00213427).
Consent to participate
Informed consent was obtained from all participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
Aishwarya Arjunan and Jamie Kostialik are former employees of Myriad Women’s Health. Lauren Propst is an employee of BillionToOne. Taylor Kane is the founder of Remember the Girls. Authors Jennifer Choi and Sara Spencer declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lourenço CM, Simão GN, Santos AC, Jr WM. X-linked adrenoleukodystrophy in heterozygous female patients: women are not just carriers. Arq Neuropsiquiatr. 2012;70(7):487–91. 10.1590/s0004-282x2012000700003. [DOI] [PubMed]
- 2.Barba-Romero MÁ, Serena J, Puig JM, C VV, Climent V, Herrero JA, et al. Clinical profile of women diagnosed with Fabry disease non receiving enzyme replacement therapy. Med Clin. 2019;153(2):47–55. doi: 10.1016/j.medcli.2018.10.039. [DOI] [PubMed] [Google Scholar]
- 3.den Veyver V, Ignatia B. Skewed X Inactivation in X-linked disorders. Semin Reprod Med. 2001;19(2):183–191. doi: 10.1055/s-2001-15398. [DOI] [PubMed] [Google Scholar]
- 4.Shvetsova E, Sofronova A, Monajemi R, Gagalova K, Draisma H, White S, et al. Skewed X-inactivation is common in the general female population. Eur J Hum Genet. 2019;27:455–465. doi: 10.1038/s41431-018-0291-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finsterer J, Stöllberger C, Freudenthaler B, Simoni D, Höftberger R, Wagner K. Muscular and cardiac manifestations in a Duchenne-carrier harboring a dystrophin deletion of exons 12-29. Intractable & rare diseases research. 2018;7(2):120–125. doi: 10.5582/irdr.2018.01003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webb K, Patel H, Bowne S, Sullivan L, Fahim A, Daiger S, Hoffman D, Birch D, Wheaton D. Among female carriers of X-linked retinitis pigmentosa (xIRP) due to RPGR mutations. Invest Ophthalmol Vis Sci. 2011;52(14):4981. [Google Scholar]
- 7.Battersby AC, Braggins H, Pearce MS, Mckendrick F, Campbell M, Burns S, et al. Health-related quality of life and emotional health in X-linked carriers of chronic granulomatous disease in the United Kingdom. J Clin Immunol. 2019;39(2):195–199. doi: 10.1007/s10875-019-00607-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelen M, Barbier M, Dijkstra IME, Schür R, Bie RMAD, Verhamme C, et al. X-linked adrenoleukodystrophy in women: a cross-sectional cohort study. Brain. 2014;137(3):693–706. doi: 10.1093/brain/awt361. [DOI] [PubMed] [Google Scholar]
- 9.Jangouk P, Zackowski KM, Naidu S, Raymond GV. Adrenoleukodystrophy in female heterozygotes: underrecognized and undertreated. Mol Genet Metab. 2012;105(2):180–185. doi: 10.1016/j.ymgme.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Huffnagel IC, Dijkgraaf MGW, Janssens GE, Weeghel MV, Geel BMV, Poll-The BT, et al. Disease progression in women with X-linked adrenoleukodystrophy is slow. Orphanet Journal of Rare Diseases. 2019;14(1):30. doi: 10.1186/s13023-019-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cardiovascular health supervision for individuals affected by Duchenne or becker muscular dystrophy PEDIATRICS. 2005;116(6):1569–1573. doi: 10.1542/peds.2005-2448. [DOI] [PubMed] [Google Scholar]
- 12.Cho YN, Choi Y. Female carriers of Duchenne muscular dystrophy. Journal of Genetic Medicine. 2013;10(2):94–98. doi: 10.5734/JGM.2013.10.2.94. [DOI] [Google Scholar]
- 13.Pavlu L, Kocourkova L, Taborsky M, Petrkova J. Ventricular tachycardia: a presentation of Fabry disease case report. European Heart Journal - Case Reports. 2018;3(1). 10.1093/ehjcr/yty154. [DOI] [PMC free article] [PubMed]
- 14.Monaghan K, Lyon E, Spector E. ACMG Standards and Guidelines for fragile X testing: a revision to the disease-specific supplements to the Standards and Guidelines for Clinical Genetics Laboratories of the American College of Medical Genetics and Genomics. Genet Med. 2013;15:575–586. doi: 10.1038/gim.2013.61. [DOI] [PubMed] [Google Scholar]
- 15.Fink DA, Nelson LM, Pyeritz R, Johnson J, Sherman SL, Cohen Y, et al. Fragile X associated primary ovarian insufficiency (FXPOI): case report and literature review. Front Genet. 2018;9. 10.3389/fgene.2018.00529. [DOI] [PMC free article] [PubMed]
- 16.Kay E, Kingston H. Feelings associated with being a carrier and characteristics of reproductive decision making in women known to be carriers of x-linked conditions. J Health Psychol. 2002;7(2):169–181. doi: 10.1177/1359105302007002456. [DOI] [PubMed] [Google Scholar]
- 17.Summary of professional guidelines. (n.d.). Retrieved February 24, 2021, from https://www.ncbi.nlm.nih.gov/medgen/docs/guideline/
- 18.Gallo AM, Angst DB, Knafl KA. Disclosure of genetic information within families. Am J Nurs. 2009;109(4):65–69. doi: 10.1097/01.NAJ.0000348607.31983.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldman A, Metcalfe A, Macleod R. The process of disclosure: mothers’ experiences of communicating X-linked carrier risk information to at-risk daughters. J Genet Couns. 2018;27(5):1265–1274. doi: 10.1007/s10897-018-0251-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwards JG, Feldman G, Goldberg J, Gregg AR, Norton ME, Rose NC, Schneider A, Stoll K, Wapner R, Watson MS. Expanded carrier screening in reproductive medicine—points to consider. Obstet Gynecol. 2015;125(3):653–662. doi: 10.1097/AOG.0000000000000666. [DOI] [PubMed] [Google Scholar]
- 21.Biesecker BB. Predictive genetic testing of minors: evidence and experience with families. Genetics in medicine : official journal of the American College of Medical Genetics. 2016;18(8):763–764. doi: 10.1038/gim.2015.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pridmore CL, Clarke JTR, Blaser S. Ornithine transcarbamylase deficiency in females: an often overlooked cause of treatable encephalopathy. J Child Neurol. 1995;10(5):369–374. doi: 10.1177/088307389501000506. [DOI] [PubMed] [Google Scholar]
- 23.Savige J, Colville D, Rheault M, Gear S, Lennon R, Lagas S, Finlay M, Flinter F. Alport syndrome in women and girls. Clinical journal of the American Society of Nephrology : CJASN. 2016;11(9):1713–1720. doi: 10.2215/CJN.00580116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bester J, Sabatello M, Van Karnebeek CD, Lantos, J. D. Please test my child for a cancer gene, but don’t tell her. Pediatrics. 2018;141(4):e20172238. doi: 10.1542/peds.2017-2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiens K, Berry SA, Choi H, Gaviglio A, Gupta A, Hietala A, et al. A report on state-wide implementation of newborn screening for x-linked adrenoleukodystrophy. Yearbook of Paediatric Endocrinology. 2019. 10.1530/ey.16.8.14. [DOI] [PMC free article] [PubMed]
- 26.Reumkens K, van Oudheusden A, Gietel-Habets J, Tummers M, de Die-Smulders C, van Osch L. Reproductive decision support: preferences and needs of couples at risk for hereditary cancer and clinical geneticists. J Genet Couns. 2018;27(4):920–926. doi: 10.1007/s10897-017-0204-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Imrie S, Jadva V, Golombok S. “Making the child mine”: mothers’ thoughts and feelings about the mother-infant relationship in egg donation families. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2020;34(4):469–479. doi: 10.1037/fam0000619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ray PF. Ethics and genetics of carrier embryos. Hum Reprod. 2006;21(10):2722–2723. doi: 10.1093/humrep/del237. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 100 kb)
(PDF 133 kb)
(PDF 113 kb)
Data Availability Statement
The data that support the findings of this study are available upon request from the corresponding author.