Abstract
Ascending aortic is an uncommon site for arterial thrombosis and ascending aortic thrombosis is a very rare phenomenon with a high fatality rate. Marijuana is the most commonly used psychoactive drug in the United States and a few cases have been reported on the association of marijuana with vascular thromboembolism. However, the pathophysiology and exact mechanism are still not well studied. Herein, we present a case of a 44-year-old female with active marijuana use presented with ascending aortic thrombus associated with acute arterial occlusion of the right vertebral artery and bilateral renal artery. The unique part of this case is that the patient did not have the classical risk factors for vascular thromboembolic disease. The only risk factor was marijuana smoking. To our best knowledge, this is one of the unique cases of marijuana-associated with ascending aorta thrombosis.
Introduction
Aortic thrombosis is a rare phenomenon with a life-threatening condition because it can cause central and peripheral embolization [1]. The thrombus can form anywhere in the aorta, but it is extremely rare for a thrombus to be formed in the ascending aorta, especially in the absence of other risk factors, such as atherosclerosis, aneurysm, cardio-surgical or traumatic state [2]. Also, because of the rarity of this situation, there is no clear consensus guideline for the management of aortic or arterial thrombosis, and the treatment remained controversial.
Herein, we report a unique diagnostic finding of ascending aortic thrombus associated with embolic stroke and multiple renal parenchymal infarcts. Our case was unique as the patient did not have any of the well-known risk factors and causes that may predispose the patient to thromboembolic disease. Marijuana was the only risk factor and the potential trigger for this case of vascular thromboembolism.
Case report
A 44-year-old African American lady with a no past medical history, except for active marijuana use (last marijuana used was one day prior to the onset of symptoms) presented to the emergency room with the chief complaints of headache, dizziness, right-sided weakness and unsteady gait. The patient reported abdominal discomfort, nausea, vomiting and diarrhea for a two-day duration. Otherwise, the patient denied syncope, seizure activity, loss of consciousness, chest pain and shortness of breath. Initial vital signs were within normal limits. The patient was conscious, alert, and oriented to person, place and time. Physical examinations were unremarkable except for a neurological exam that revealed a 4/5 strength on the upper and lower extremities, a loss of temperature sensation on the left side of the face and a wide-based gait. Also, Romberg's test was positive. Complete blood count showed leukocytosis of 13.1 0 × 103/ul (normal range: 4.4-11.0 × 103/ul), hemoglobin, platelets count, coagulation profiles and comprehensive metabolic panels were within normal limits. Her urine drug screen was positive for cannabinoid. Echocardiogram showed sinus rhythm with possible left atrial enlargement. The chest X-ray was unremarkable. There were no acute ischemic or hemorrhagic stroke in the Computed Tomography (CT) of the head without contrast. CT Angiogram (CTA) of the head and neck was then performed which revealed occlusion of the V4 segment of the right vertebral artery (Fig. 1, Fig. 2, Fig. 3). There was also a slightly decreased or diminished flow within the distal V3 segment of the right vertebral artery and irregular intraluminal thrombus within the visualized distal ascending thoracic aorta. A complete CTA of the chest, abdomen and pelvis was performed and revealed intraluminal thrombus within the ascending thoracic aorta, small bilateral renal infarcts and large right ovarian dermoid (Fig. 4, Fig. 5, Fig. 6). In addition, MRI of the head showed an acute right lateral medullary infarct. As part of the stroke workup, an electrocardiograph was performed which did not show findings suggestive of valvular or cardiac source of embolus. A cardiothoracic surgeon and a hematologist were consulted which started the patient on anticoagulation with heparin initially and transitioned to Apixaban on discharge. A full hypercoagulability workup including DRVVT screening for lupus anticoagulant, anticardiolipin antibodies beta-2-glycoprotein, homocysteine levels, paroxysmal nocturnal hemoglobinuria screening, Protein C and S activity, antithrombin mutations, and factor V Leiden and prothrombin genotyping were unremarkable. Autoimmune workup including antinuclear antibody, antineutrophil cytoplasmic antibody, anti-double-stranded DNA antibody, rheumatoid factor, anti-cyclic citrullinated peptide, anti-histone antibodies, Sjogren antibody, myeloperoxidase antibodies, proteinase 3 autoantibodies, complement levels, Smith antibody, and RNP antibody were also within normal limit. Tumor markers were within normal limits and the patient did not have any nodules or lesions on CT Chest, abdomen and pelvis. Marijuana was believed to be the cause of the ascending aorta thrombosis with the showering emboli to the brain and the kidneys after excluding all other risk factors that may contribute or increase the risk of thrombosis in this patient.
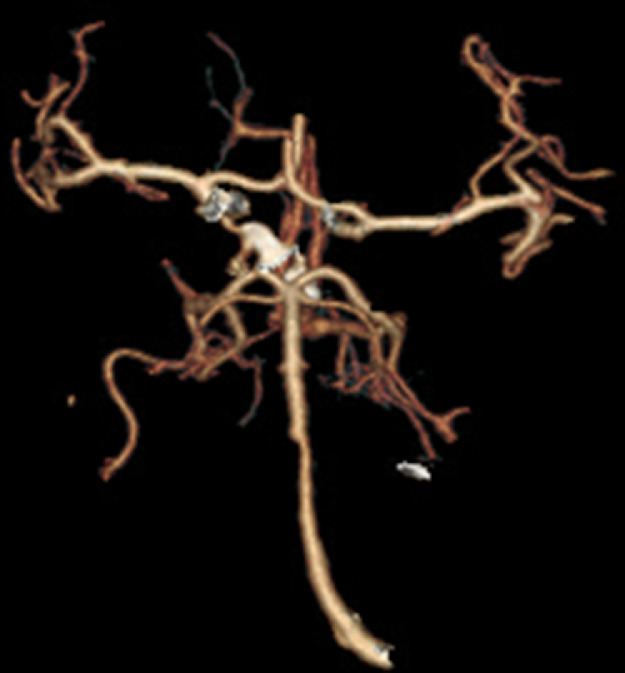
Fig. 1.
CTA of the head, a three-dimensional reconstruction image, showing a complete occlusion of the right vertebral artery, segment V4.
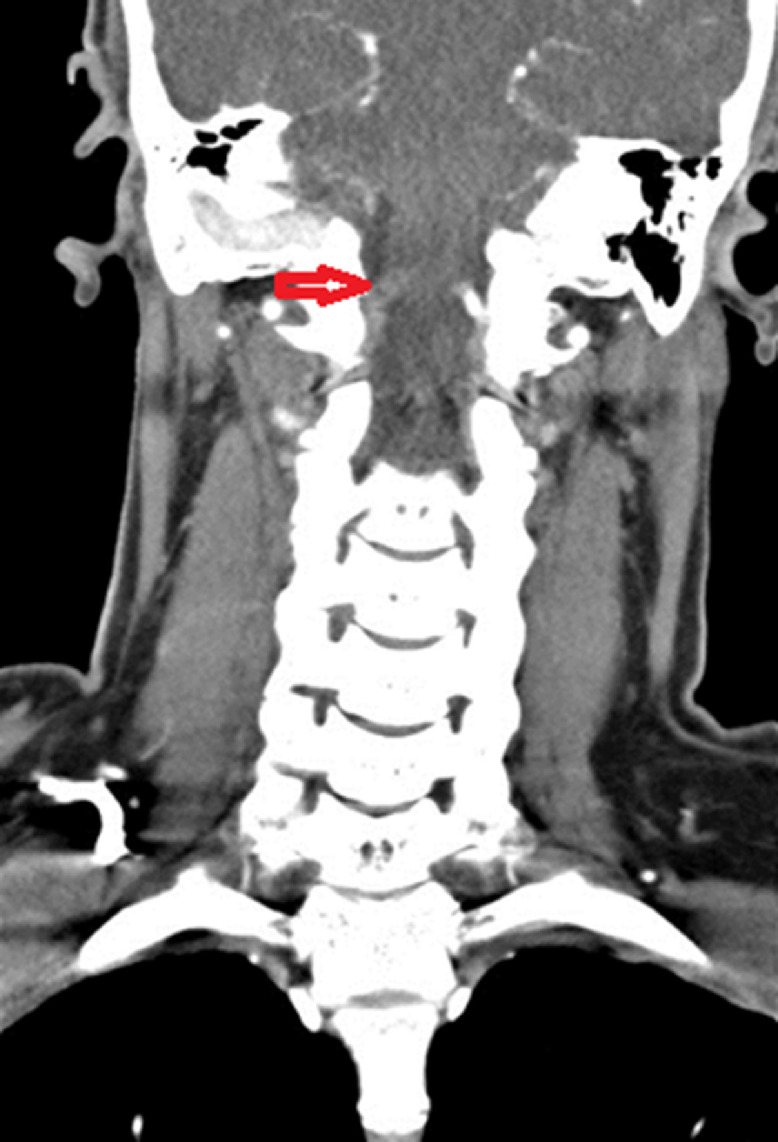
Fig. 2.
CTA of the head and neck, showing a complete occlusion of the right vertebral artery, segment V4 (axial view).
Fig. 3.
CTA of the head and neck, showing a complete occlusion of the right vertebral artery, segment V4 (coronal view).
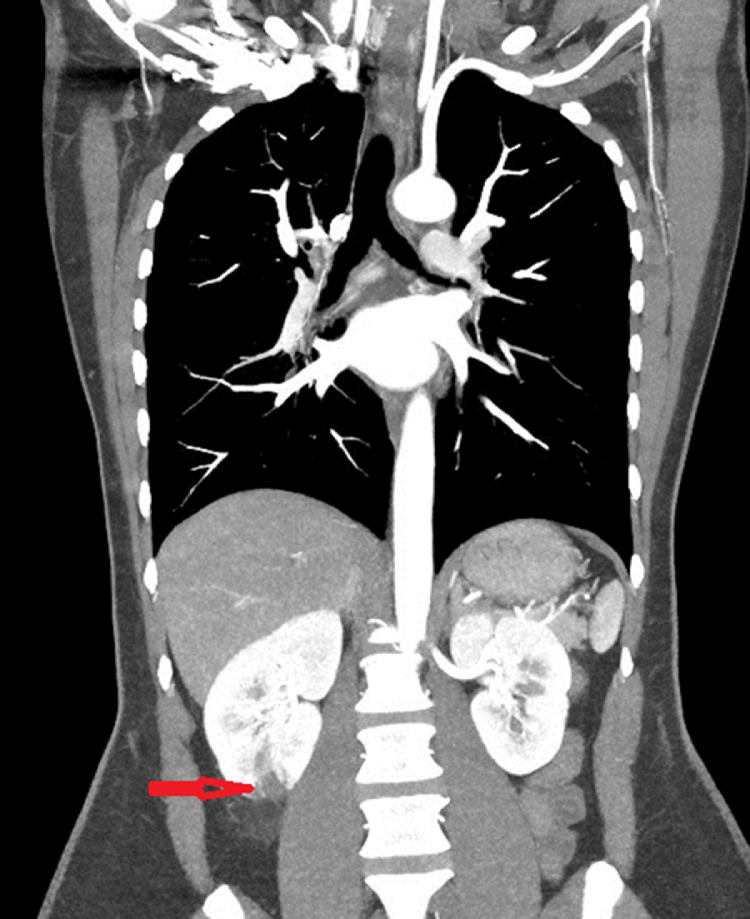
Fig. 4.
CT of the lower abdomen and pelvis showing right lower lobe kidney infarcts (coronal view).
Fig. 5.

CT of the lower abdomen and pelvis showing right lower lobe kidney infarcts (sagittal view).
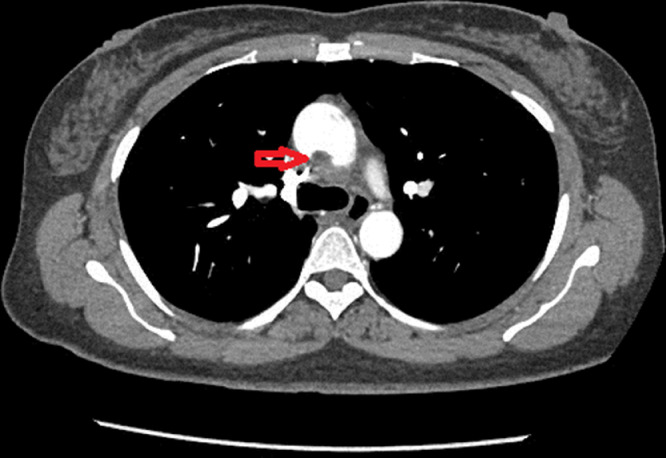
Fig. 6.
CTA of the chest showing an intramural thrombus of the ascending aorta (axial view).
Discussion
Ascending aorta thrombosis is very rare, with no well-documented incidence and prevalence. It is very uncommon for a thrombus to form in the ascending aorta, mainly due to the high blood flow and shear stress [3]. Due to its function in supplying blood to the rest of the body, ascending aorta thrombosis can be complicated by showering emboli to the rest of the vital organs leading to serious and life-threatening conditions. The mechanism of thrombus formation in the ascending aorta remains unclear. We do not have a thorough understanding of the pathophysiology of the formation of an aortic thrombus especially in relatively young patients without any of the typical risk factors for cardiovascular disease. However, there are several factors that may increase the risk of ascending aortic thrombus formation, namely coagulation disorders, oral contraceptive pills, hormone replacement therapy or pregnancy [4]. Our case is unique given that the patient had no well-known risk factors that predispose or increase the probability of developing thromboembolic disease. After excluding all the common risk factors, marijuana use could be the potential trigger that increased the risk of vascular thromboembolism in this patient.
Marijuana is the most commonly used psychoactive drug in the United States. There is a steadily-increasing prevalence in its usage and abuse over the past decade, especially among adolescents [5]. There are two known cannabinoid receptors (inhibitory G-protein linked receptor): CB1 in the central nervous system and CB2 found peripherally in the immune system, peripheral nerve terminals and vas deferens. There are many strains of marijuana, the most commonly used for recreational purposes is Cannabis Sativa which consist of more than 500 different natural and chemical compounds, and over 60 known cannabinoids [6]. The recreational use of marijuana includes smoking the dried flower in the form of cigarettes (joints) and water bongs. In addition to its psychoactive effects, marijuana has multiple adverse effects on the human body, including cardiovascular and cerebrovascular events. Many reports have linked marijuana use to heart attack, cardiac arrests, arrhythmias, and strokes [7], [8].
Marijuana can acutely increase the sympathetic activity and suppress the parasympathetic activity, leading to catecholamine's surge, tachycardia, vasodilation, increase in the cardiac output and the myocardium oxygen demand which can cause myocardial infarction [9]. Marijuana can also cause transient ischemic attacks and stroke via orthostatic hypotension, diminished circulatory response to exercise, cerebral vasoconstriction, intracranial stenosis, increased cerebrovascular resistance and reduced cerebrovascular perfusion [10]. As for vascular thromboembolism, the pathophysiology and the exact mechanism of how marijuana induces hypercoagulability and thrombosis are still not well studied. Different theories have emerged in the literature. Some studies reported that Cannabinoids, the active component of marijuana, causes the disruption of endothelial cells, leading to vascular thrombosis [11]. Other studies, like Al-Hweish et al., described an association between marijuana and secondary lupus anticoagulant [3]. In that study, they reported a patient with multiple renal infarcts after heavy marijuana smoking. The patient had a positive anticardiolipin and beta-2-glycoprotein on presentation, which came to be negative six months after marijuana usage was stopped. Rezkalla and Kloner, on the other hand, proposed that marijuana abuse is associated with an increased risk of paroxysmal atrial fibrillation in young patients without organic heart disease, which can cause arterial thrombosis [4]. Paroxysmal atrial fibrillation can occur acutely after marijuana smoking and most of the patients will have a favorable outcome after marijuana cessation, which can explain the sinus rhythm observed in the ECG of our patient [12].
In our case, the patient had a negative hypercoagulability workup including normal antiphospholipid workup. The patient had normal ECG (sinus rhythm), though the possibility of paroxysmal atrial fibrillation cannot be excluded, which may be the underlying mechanism leading to marijuana-associated arterial thrombosis. Nonetheless, the exact mechanism and pathophysiology of how marijuana can be associated with thrombosis and increases the risk of arterial thrombosis remain unclear and warrants further studies.
There are several approaches in treating the ascending aortic thrombosis associated with showering emboli causing ischemic stroke and distal organ infarcts. The commonly used methods include anticoagulation therapy, thrombolytic therapy, aortic stent placement, aspiration thrombectomy, and open surgical thrombectomy [5,13]. Choukroun et al., suggested a strategy of beginning with anticoagulation, followed by a surgical thrombus removal only when anticoagulation alone is not effective [14]. In our case, the patient on her presentation had an ischemic stroke with total occlusion of the V4 segment of the vertebral artery, and after scanning the abdomen, multiple distal small renal infarcts were found. A multidisciplinary team, consisting of cardiology, neurology, cardiothoracic surgery, vascular surgery and hematology, were involved in the management. The decision was to treat medically without surgical intervention. The patient started on anticoagulation with heparin drip initially and was transitioned to Apixiaban on discharge. Apixaban is a direct oral anticoagulant that works via direct factor Xa inhibition. Food and Drug Administration approved the drug for multiple uses including for non-valvular atrial fibrillation, prevention of venous thromboembolism, treatment and prevention of pulmonary embolisms, and deep vein thrombosis [15]. The role of the newer oral anticoagulant in treating arterial thrombosis, in general, is not well established despite being used in many clinical trials [16], [17], [18]. There is a theoretical possibility that anticoagulation could cause fragmentation of thrombus with massive embolism and significant neurologic sequelae, hence patients should be closely monitored [19].
Conclusion
The patient described in this case is an exceptional and unusual case presented with ascending aortic thrombus complicated by ischemic stroke and bilateral renal infarcts without having the classical risk factors for thrombosis. After a thorough workup and very extensive evaluation, marijuana-induced paroxysmal atrial fibrillation was the only explanation for having an ascending aortic thrombosis in our patient. The research of the area is sparse, possibily because of the Drug Enforcement Administration classification of marijuana as schedule I. In addition to that, because of the uncommonness of the aortic thrombosis and the lack of a standardized guideline for the management of this condition, some studies recommended aggressive management to prevent the risk of thrombus recurrence and arterial embolization while others recommended a more conservative, less invasive medical management. We recommend a multidisciplinary approach for the management and treatment with close monitoring and follow-ups.
Footnotes
Competing interests: All authors including: Iyad Farouji, Kok Hoe Chan, Arwa Battah, Hossam Abed, Theodore DaCosta, Joaquim Correia, Addi Suleiman, declare no competing conflict of interest
References
- 1.Alaeddini J, Ilercil A, Shirani J. Thoraco-abdominal aortic thrombosis and superior mesenteric artery embolism. Tex Heart Inst J. 2000;27:318–319. [PMC free article] [PubMed] [Google Scholar]
- 2.Fayad ZY, Semaan E, Fahoum B, Briggs M, Tortolani A, D'Ayala M. Aortic mural thrombus in the normal or minimally atherosclerotic aorta. Ann Vasc Surg. 2013;27:282–290. doi: 10.1016/j.avsg.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Al-Hwiesh AK, Bahbhani H, Alhwiesh A, Saad I, AlMohama F. Acute renal infarction induced by heavy marijuana smoking. Saudi J Kidney Dis Transpl. 2018;29:971–975. doi: 10.4103/1319-2442.239652. [DOI] [PubMed] [Google Scholar]
- 4.Rezkalla S., Kloner R.A. Cardiovascular effects of marijuana. Trends Cardiovasc. Med. 2018;21:452–455. doi: 10.1016/j.tcm.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Soleimani A, Marzban M, Sahebjam M, Shirani S, Sotoudeh-Anvari M, Abbasi A. Floating thrombus in the aortic arch as an origin of simultaneous peripheral emboli. J Cardiac Surg. 2008;23(6):762–764. doi: 10.1111/j.1540-8191.2008.00694.x. [DOI] [PubMed] [Google Scholar]
- 6.Soo A, Marley D, McGrath-Soo L, Herron B, Parissis H. Ascending aorta thrombus: a diagnostic and treatment dilemma. Asian Cardiovasc Thorac Ann. 2013;22(6):731–733. doi: 10.1177/0218492313481969. [DOI] [PubMed] [Google Scholar]
- 7.Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103(23):2805–2809. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- 8.Hackam DG. Cannabis and stroke: systematic appraisal of case reports. Stroke. 2015;46(3):852–856. doi: 10.1161/STROKEAHA.115.008680. [DOI] [PubMed] [Google Scholar]
- 9.Pacher P., Steffens S., Haskó G., Schindler T.H., Kunos G. Cardiovascular effects of marijuana and synthetic cannabinoids: the good, the bad, and the ugly. Nat Rev Cardiol. 2018;15:151–166. doi: 10.1038/nrcardio.2017.130. [DOI] [PubMed] [Google Scholar]
- 10.Eguchi K, Ohtaki E, Misu K, et al. Acute myocardial infarction caused by embolism of thrombus in the right coronary sinus of Valsalva: a case report and review of the literature. J Am Soc Echocardiogr. 2004;17(2):173–177. doi: 10.1016/j.echo.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Tatli E, Yilmaztepe M, Altun G, Altun A. Cannabis-induced coronary artery thrombosis and acute anterior myocardial infarction in a young man. Int J Cardiol. 2007;120(3):420–422. doi: 10.1016/j.ijcard.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 12.Korantzopoulos P, Liu T, Papaioannides D, Li G, Goudevenos JA. Atrial fibrillation and marijuana smoking. Int J Clin Pract. 2008;62:308–313. doi: 10.1111/j.1742-1241.2007.01505.x. [DOI] [PubMed] [Google Scholar]
- 13.Choi JB, Choi SH, Kim NH, Jeong JW. Floating thrombus in the proximal aortic arch. Tex Heart Inst J. 2004;31(4):432–434. [PMC free article] [PubMed] [Google Scholar]
- 14.Choukroun EM, Labrousse LM, Madonna FP, Deville C. Mobile thrombus of the thoracic aorta: diagnosis and treatment in 9 cases. Ann Vasc Surg. 2002;16(6):714–722. doi: 10.1007/s10016-001-0314-2. [DOI] [PubMed] [Google Scholar]
- 15.Kjerpeseth LJ, Ellekjær H, Selmer R, Ariansen I, Furu K, Skovlund E. Trends in use of warfarin and direct oral anticoagulants in atrial fibrillation in Norway, 2010 to 2015. Eur J Clin Pharmacol. 2017;73(11):1417–1425. doi: 10.1007/s00228-017-2296-1. [DOI] [PubMed] [Google Scholar]
- 16.Chan NC, Eikelboom JW, Weitz JI. Evolving treatments for arterial and venous thrombosis: role of the direct oral anticoagulants. Circ Res. 2016;118(9):1409–1424. doi: 10.1161/CIRCRESAHA.116.306925. [DOI] [PubMed] [Google Scholar]
- 17.Houmsse M, McDavid A, Kilic A. Large de novo ascending aortic thrombus successfully treated with anticoagulation. J Cardiovasc Thorac Res. 2018;10(2):113–114. doi: 10.15171/jcvtr.2018.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Toyama M, Nakayama M, Hasegawa M, Yuasa T, Sato B, Ohno O. Direct oral anticoagulant therapy as an alternative to surgery for the treatment of a patient with a floating thrombus in the ascending aorta and pulmonary embolism. J Vasc Surg Cases Innov Tech. 2018;4(2):170–172. doi: 10.1016/j.jvscit.2018.03.002. Published 2018 Apr 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mando R, Gemayel R, Chaddha A, Barbat JJ, Cami E. Peripherally Embolizing Aortic Thrombus: The Work-Up, Management, and Outcome of Primary Aortic Thrombus. Case Rep Cardiology. 2019 doi: 10.1155/2019/8132578. Article ID 8132578, 6 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]