Abstract
Background
Transplant centers saw a substantial reduction in deceased donor solid organ transplantation since the beginning of the coronavirus 2019 (COVID-19) pandemic in the United States. There is limited data on the impact of COVID-19 on adult and pediatric heart transplant volume and variation in transplant practices. We hypothesized that heart transplant activity decreased during COVID-19 with associated increased waitlist mortality.
Methods
The United Network for Organ Sharing (UNOS) database was used to identify patients at the time of listing for heart transplant from 2017–2020. Patients were categorized as pediatric (<18 years) or adult (≥18 years) and as pre-COVID (2017-2019) or post-COVID (2020). Regional and statewide data were taken from United States Census Bureau. CovidActNow project was used to obtain COVID-19 mortality rates.
Findings
Among pediatric patients, average time on the waiting list decreased by 28 days. Even though the average number of pediatric transplants (n=39 per month) did not change significantly during 2020, there was a temporal decline in the first quarter of 2020 followed by a sharp increase. Overall absolute pediatric waitlist mortality decreased from 5•31 to 4•73, however female mortality increased by 2%. Regional differences in pediatric mortality were observed: Northeast, decreased by 7•5%; Midwest, decreased by 9%; West, increased by 3•5%; and South, increased by 13%. North Dakota (0•55), Oklahoma (0•21) and Hawaii (0•33) showed higher mortality than other states per 100,000. In adults, average time on waiting list increased by 40 days and there was an increase in the number of transplants from 242 to 266. Adult waitlist mortality had a larger decrease, 18•44 to 15•70, with an increase in female mortality of 7%. Regional differences in adult mortality were also observed: Northeast, decreased by 3%; Midwest, increased by 5•5%; West, increased by 4•5% and South, decreased by 5%. Iowa (0•37), Wyoming (0•22), Arkansas (0•18) and Vermont (0•19) had the highest mortality per 100,000 compared to the other states.
Interpretation
Pediatric heart transplant volume declined in early 2020 followed by a later increase, while adult transplant volume increased all year round. Although, overall pediatric waitlist mortality decreased, female waitlist mortality increased for both adults and pediatrics. Regional differences in waitlist mortality were observed for both pediatrics and adults. Future studies are needed to understand this initial correlation and to determine the impact of COVID-19 on heart transplant recipients
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Keywords: COVID-19, Heart transplant, Mortality, Pandemic, Policy
Research in context.
Evidence before this study
In the United States, approximately 40,000 patients receive an organ transplant every year, but 120,000 patients remain on a waiting list for transplantation, with 7600 patients dying annually while waiting for an organ, if one were to look at data from UNOS. The cardiovascular community faces even more challenges as the organ supply is even further limited for hearts. COVID-19 pandemic has had severe implications for patients on the waiting list as they are both at increased risk of acquiring COVID-19 infection and suffering from progression of their original end-organ disease. Many centers in the United States deactivated patients on transplant waiting lists while transplanting patients with severe illness with highest waitlist mortality as evidenced by data obtained from UNOS and earlier institutional reports published.
When we searched PubMed from Jan 2020 till Dec 2020 for published research articles using the terms “COVID-19”, “heart transplantation”, “pediatric heart transplant”, “waiting list mortality”, there was hardly any data that existed. Few (< 5) studies look at very early results of COVID-19 on heart failure and heart transplant practices as the pandemic began but none thereafter. Many centers across United States have adopted new policies and practices that have either changed or evolved to cater for high-risk transplant patients. Therefore, we decided to study the evolution of the initial trend in the heart transplant community and how that applied to adult and pediatric end-stage heart failure patients.
Added value of this study
This study reports that even though pediatric heart transplant volume declined in early 2020, there was an increase towards the latter part of the year implying that centers started to adjust, and developed policies to adapt to the new norm. On the other hand, due to multiple factors, transplant volume in adults continued to increase.
Additionally, our study highlights that overall waitlist mortality decreased for both pediatrics and adults, presumably due to changes in listing status, delays in non-urgent evaluations and decreased in heart failure hospitalizations. Surprisingly, we noticed that there were gender and ethnic differences in waitlist mortality during the pandemic that need to be explored further to better understand as we emerge from this pandemic.
Implications of all the available evidence
The findings in this study shed light on the changing national practice of waitlisting and transplantation in pediatric and adult heart transplant patients. The study highlights how the heart transplantation community has adapted to the new social distancing norms and dealt with the pandemic. Furthermore, it sheds light on gender, ethnic and regional differences in wait list outcomes that would pave the way for future studies. We do hope to learn and better understand these trends as we emerge from this pandemic.
Alt-text: Unlabelled box
1. Introduction
The novel coronavirus 2019 (COVID-19) pandemic of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) brought unprecedented challenges for healthcare systems worldwide. After initially being reported in Wuhan, China in December of 2019, COVID-19 was classified as a pandemic by the World Health Organization on March 11th, 2020. Due to minimal knowledge and absence of treatment, many governments opted for suspension of nonessential services and lockdowns. This included suspension of many nonessential medical procedures, resulting in disruption of numerous medical communities.
The heart transplant (HT) community implemented various changes in response to COVID-19 [1]. Due to the overwhelming burden of COVID-19, a substantial negative effect on worldwide organ donation and transplantation followed. Patients active on the waiting list and transplant recipients encountered increased risk of both acquiring COVID-19 and progression to severe disease. Numerous centers across the United States deactivated patients on transplant waiting lists, reserving the organs for the most severe patients with highest risk of waitlist mortality [1]. Simultaneously, hospitalizations for heart failure patients decreased by 50% [2]. This was accompanied by regional changes in health policies further impacting the transplant practices.
In the United States, transplant centers saw a substantial reduction in deceased donor solid organ transplants since the beginning of the COVID-19 pandemic [3]. Heart transplant volumes were significantly affected, even in regions with a lower prevalence of COVID-19 cases [4]. This was accompanied by increased waitlist inactivations, decreased waitlist additions and decreased donor recovery [4]. However, there is limited data on the continued impact of COVID-19 on adult and pediatric heart transplant volume, as well as national and regional variation in transplant practices. The purpose of this study is to highlight the heart transplant waitlist mortality during the pandemic and assess variations in heart transplant volume among adult and pediatric population. We hypothesized that heart transplant activity decreased during COVID-19 with associated increased waitlist mortality.
2. Methods
We conducted a retrospective study of data from the Standard Transplant Analysis and Research (STAR) file, obtained from the United Network for Organ Sharing (UNOS) as the contractor for the Organ Procurement and Transplantation Network (OPTN). The data is accessible from http://optn.transplant.hrsa.gov/data/request-data/ and contains records of solid organ transplants occurring in the United States between 1987 and 2020 [5]. UNOS uses an online database system, called UNet, to collect, store, analyze and publish all OPTN data that pertains to the patient waiting list, organ matching and number of transplants performed. Transplant cases are submitted by 57 Organ Procurement Organizations and over 250 transplant hospitals across the United States.
Data was extracted from the deceased donor dataset and the thoracic dataset. For the mortality calculations, we excluded deceased recipients who required multiple organs or died prior to 2017. For waiting list statistics, we included any patient on the list between 2017-2020, including those added prior to 2017. Only patients whose permanent home was within the United States were included. Patients were then separated into pediatric (< 18 years) and adult (≥18 years) datasets for further analysis. Demographic data included Age, Weight, Sex, Blood type, Race and Ethnicity.
Additional demographic data for states and regions was retrieved from US Census data [6]. Regions were defined based upon US census designation as Northeast, South, Midwest and West. Data from the CovidActNow project, accessible from https://covidactnow.org/, was used for Covid-19 mortality rates [7].
2.1. Statistical Analysis
Descriptive statistics were used to report the specific frequencies and distributions of the demographic factors, along with delta shifts among transplant, waitlist and mortality rates within geographic regions for pediatric and adult populations. More detailed statistical approaches were not pursued due to limitations in the data. The assumption of statistical significance was invalidated due to the different approaches taken by states in handling the pandemic. All statistical analyses were conducted in the IPython environment using Jupyter in Anaconda [8], [9], [10]. Data manipulation was performed using the Numpy and Pandas packages [10], [11], [12]. Graphs were made using Matplotlib [13]. Because of the high quality of the data provided from the registry, extensive data manipulation or other data cleaning techniques were not required.
2.2. Role of the funding source
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
3. Results
3.1. Demographics
Demographics for all registered waiting list members are shown in Table 1. We divided the adult and pediatric populations into Pre-COVID cohort (2017–2019) and COVID cohort (2020). For the adult population, age and weight remained similar. Days on the waiting list during the pandemic were reduced to a third of the pre-pandemic value. Small shifts in gender were observed, with males increasing by ∼1%. Small regional shifts were also observed, with the Northeast and Midwest decreasing slightly, the West increasing slightly, and the South remaining essentially unchanged. Small shifts in blood type were observed, with both O and AB increasing slightly, A decreasing slightly and B remaining essentially unchanged. There was an ∼2% decrease in White population, which was offset by an increase in Black population. Proportion of Hispanic population decreased slightly by ∼0•2%.
Table 1.
Demographic table for all waiting list members divided into adult and pediatric populations and separated by Pre-COVID and COVID. Sex, region, blood type, race and ethnicity are all shown as a percentage of the total population for that group.
| Adult (N=15489) | Pediatric (N=2596) | |||
| 2017-2019 (N=11883) Mean (SD) | 2020 (N=3606) Mean (SD) | 2017-2019 (N=1989) Mean (SD) | 2020 (N=607) Mean (SD) | |
| Age (yrs.) | 52•97 (12.77) | 53•18 (12•74) | 6•04 (6•24) | 5•82 (6•28) |
| Weight (kg) | 85•11 (19.04) | 85•45 (18•65) | 25•71 (25•90) | 26•09 (27•26) |
| Days on Waiting List | 244•81 (298.53) | 70•17 (85•17) | 176•41 (241•29) | 84•65 (79•89) |
| Sex | ||||
| Male | 8685 (73•09%) | 2675 (74•18%) | 1095 (55•05%) | 338 (55•68%) |
| Female | 3198 (26•91%) | 931 (25•82%) | 894 (44•95%) | 269 (44•32%) |
| Region | ||||
| Northeast | 2277 (19•16%) | 659 (18•28%) | 248 (12•47%) | 62 (10•21%) |
| South | 4662 (39•23%) | 1429 (39•63%) | 846 (42•53%) | 261 (43•00%) |
| Midwest | 2740 (23•06%) | 825 (22•88%) | 483 (24•28%) | 153 (25•21%) |
| West | 2204 (18•55%) | 693 (19•22%) | 412 (20•71%) | 131 (21•58%) |
| Blood Type | ||||
| O | 5186 (43•64%) | 1595 (44•23%) | 953 (47•91%) | 289 (47•61%) |
| A | 4441 (37•37%) | 1301 (36•08%) | 693 (34•84%) | 216 (35•58%) |
| B | 1715 (14•43%) | 517 (14•34%) | 263 (13•22%) | 76 (12•52%) |
| AB | 541 (4•55%) | 193 (5•35%) | 80 (4•02%) | 26 (4•28%) |
| Race | ||||
| White | 7398 (62•26%) | 2165 (60•04%) | 1032 (51•89%) | 294 (48•43%) |
| Black | 2896 (24•37%) | 940 (26•07%) | 408 (20•51%) | 150 (24•71%) |
| Hispanic | 1062 (8•94%) | 314 (8•71%) | 391 (19•66%) | 117 (19•28%) |
| Asian | 392 (3•30%) | 140 (3•88%) | 65 (3•27%) | 20 (3•29%) |
| American Native | 37 (0•31%) | 8 (0•22%) | 12 (0•60%) | 5 (0•82%) |
| Pacific Native | 35 (0•29%) | 17 (0•47%) | 13 (0•65%) | 3 (0•49%) |
| Multiracial | 63 (0•53%) | 22 (0•61%) | 68 (3•42%) | 18 (2•97%) |
| Ethnicity | ||||
| Hispanic | 1075 (9•05%) | 319 (8•85%) | 405 (20•36%) | 123 (20•26%) |
| Non-Hispanic | 10808 (90•95%) | 3287 (91•15%) | 1584 (79•64%) | 484 (79•74%) |
Similar trends for age, weight and wait list time in the adult population were also observed in the pediatric population. A slight shift towards males was observed. Decreases in waiting list participants from the Northeast (∼2%) were offset by increases in all other regions. Blood type composition did not markedly change, with only a small increase in A and AB, offset by decrease in O ad B. White population decreased by ∼3%, which was offset by an increase in the Black population. Other populations remained essentially unchanged. Ethnicity remained essentially unchanged for pediatric population.
3.2. Waitlist mortality
Demographics for waitlist mortality are shown in Table 2. For adult population, age and weight was similar between Pre-COVID and COVID eras. Average days on waiting list increased by ∼40 days. Shifts in mortality demographics were observed at the onset of Covid-19. Mortality increased in the female population by ∼1%. Mortality decreased in the Northeast and South for adults, while mortality remained constant in the Midwest and West. Mortality for Type B increased by ∼0.5%, with decreased in mortality for all other blood types. White, Asian and Multiracial mortality all decreased. Black, Hispanic and Pacific Islander mortality remained effectively unchanged. Native American mortality increased. No multiracial deaths were recorded in 2020. Mortality changes decreased in non-Hispanic population, while remaining unchanged in the Hispanic population.
Table 2.
Demographic table for waiting list fatalities divided into adult and pediatric populations and separated by Pre- COVID and COVID. Sex, region, blood type, race and ethnicity are all shown as a percentage of the total population for that group on the waiting list.
| Adult (N=833) | Pediatric (N=244) | |||
| 2017-2019 (N=664) Mean (SD) | 2020 (N=169) Mean (SD) | 2017-2019 (N=191) Mean (SD) | 2020 (N=53) Mean (SD) | |
| Age (yrs.) | 53•75 (12•35) | 53•58 (12•38) | 3•17 (4•97) | 3•67 (5•38) |
| Weight (kg) | 88•11 (20•39) | 88•60 (18•51) | 15•10 (20•51) | 14•93 (17•31) |
| Days on Waiting List | 438•48 (671•37) | 473•97 (691•48) | 144•21 (278•59) | 116•83 (176•05) |
| Sex | ||||
| Male | 524 (6•03%) | 121 (4•52%) | 101 (9•22%) | 27 (7•99%) |
| Female | 140 (4•38%) | 48 (5•16%) | 90 (10•07%) | 26 (9•67%) |
| Region | ||||
| Northeast | 158 (6•94%) | 34 (5•16%) | 29 (11•69%) | 4 (6•45%) |
| South | 283 (6•07%) | 64 (4•48%) | 80 (9•46%) | 29 (11•11%) |
| Midwest | 137 (5•00%) | 43 (5•21%) | 49 (10•14%) | 9 (5•88%) |
| West | 86 (3•90%) | 28 (4•04%) | 33 (8•01%) | 11 (8•40365%) |
| Blood Type | ||||
| O | 365 (7•04%) | 99 (6•21%) | 90 (9•44%) | 22 (7•61%) |
| A | 196 (4•41%) | 39 (3•00%) | 67 (9•67%) | 18 (8•33%) |
| B | 81 (4•72%) | 27 (5•22%) | 29 (11•03%) | 9 (11•84%) |
| AB | 22 (4•07%) | 4 (2•07%) | 5 (6•25%) | 4 (15•38%) |
| Race | ||||
| White | 433 (5•85%) | 99 (4•57%) | 87 (8•43%) | 21 (7•14%) |
| Black | 153 (5•28%) | 47 (5•00%) | 46 (11•27%) | 13 (8•67%) |
| Hispanic | 52 (4•90%) | 16 (5•10%) | 40 (10•23%) | 12 (10•26%) |
| Asian | 16 (4•08%) | 5 (3•57%) | 6 (9•23%) | 4 (20•00%) |
| American Native | 3 (8•11%) | 1 (12•50%) | 2 (16•67%) | 0 (0%) |
| Pacific Islander | 2 (5•71%) | 1 (5•88%) | 3 (23•08%) | 1 (33•33%) |
| Multiracial | 5 (7•94%) | 0 (0%) | 7 (10•29%) | 2 (11•11%) |
| Ethnicity | ||||
| Hispanic | 53 (4•93%) | 16 (5•02%) | 44 (10•86%) | 13 (10•57%) |
| Non-Hispanic | 611 (5•65%) | 153 (4•65%) | 147 (9•28%) | 40 (8•26%) |
For pediatric population, age increased by 0•5 years and days on the waiting list decreased by ∼28 days. Shifts in sex demographics showed a decrease in male mortality offset by an increase in female mortality. Regional differences were also observed. Pediatric mortality decreased by approximately half from ∼11•7% to ∼6•5% in the Northeast. A decrease was also observed in the Midwest, with a drop-in mortality of almost 5%. Mortality in the West remained effectively unchanged, while the South had an increase of ∼1.5%. Trends for O, A and B blood types in pediatrics mirrored trends observed in adult population. Blood type AB approximately tripled in the pediatric population. Mortality decreased for white, black and American Native pediatric populations. Hispanic mortality remained essentially unchanged. Asian, Pacific Islander and Multiracial mortality all increased. Deaths by ethnicity followed similar trends to the adult population.
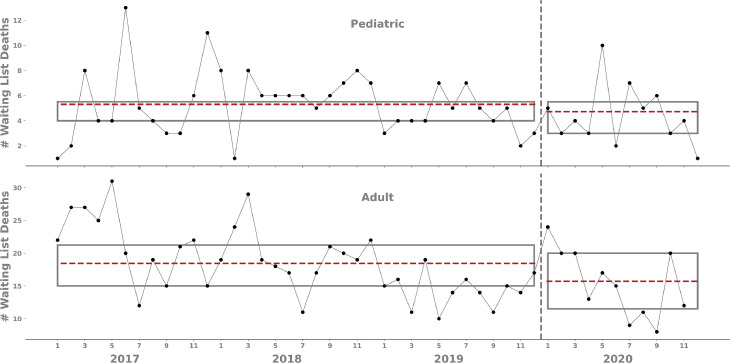
Deaths on the waiting list for pediatric and adult populations are shown in Figure 1. Decreases in the average deaths Pre-COVID and COVID are observed for both pediatric and adult populations. Average number of pediatric deaths decreased from 5•31 to 4•73 per month. A larger decrease was observed for adults, decreasing from 18•44 to 15•70 per month. Additionally, the average number of discarded hearts Pre-COVID and during COVID were calculated and found to have increased from 2•67 to 3•38. However, this would not have significantly contributed to the observed wait list mortality rate.
Figure 1.
Number of waiting list deaths for pediatric and adult populations separated into Pre- COVID data (Jan. 2017 – Dec. 2019) and COVID data (Jan. 2020 – Nov. 2020) shown by a dashed line. Means are shown by the dashed red line, while the box shows the interquartile range.
3.3. Transplant volume and regional variation
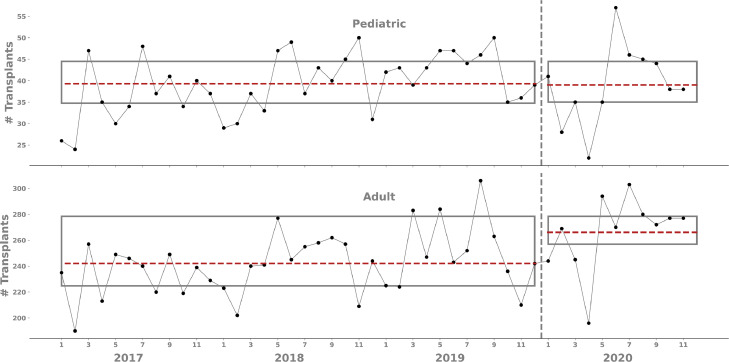
The average number of monthly pediatric transplants did not change after COVID onset (39 versus 39; Fig. 2). However, there was an increase in the average number of monthly transplants in adults from 242 to 266 after the onset of COVID-19. For both populations, an initial decrease in the number of transplants after COVID-19 onset was followed by an increase in the number of transplants performed.
Figure 2.
Number of transplants for pediatric and adult populations separated into pre-COVID era (Jan. 2017 – Dec. 2019) and COVID era (Jan. 2020 – Nov. 2020) shown by a dashed line. Means are shown by the dashed red line, while the box shows the interquartile range.
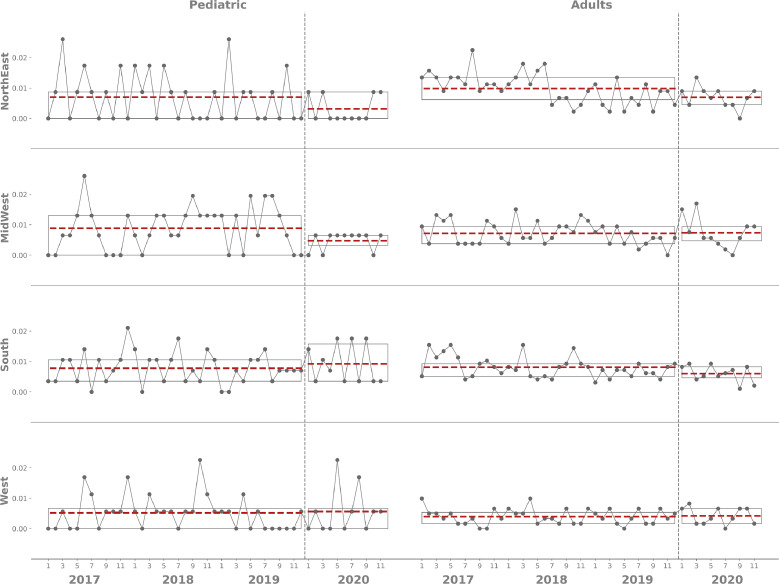
Mortality rate by region for both pediatric and adult populations are shown in Fig 3. For pediatric populations, the mortality rate decreased in the Northeast and Midwest, while increasing in the South. The West remained effectively unchanged. For the adult population, both the Northeast and South experienced a decreased mortality rate. Both the Midwest and the West however experienced no effective change.
Figure 3.
Mortality rate per 100,000 residents by census region for pediatric and adult populations divided into pre-COVID era (Jan. 2017 – Dec. 2019) and COVID era (Jan. 2020 – Nov. 2020) shown by a dashed line. Means are shown by the dashed red line, while the box shows the interquartile range.
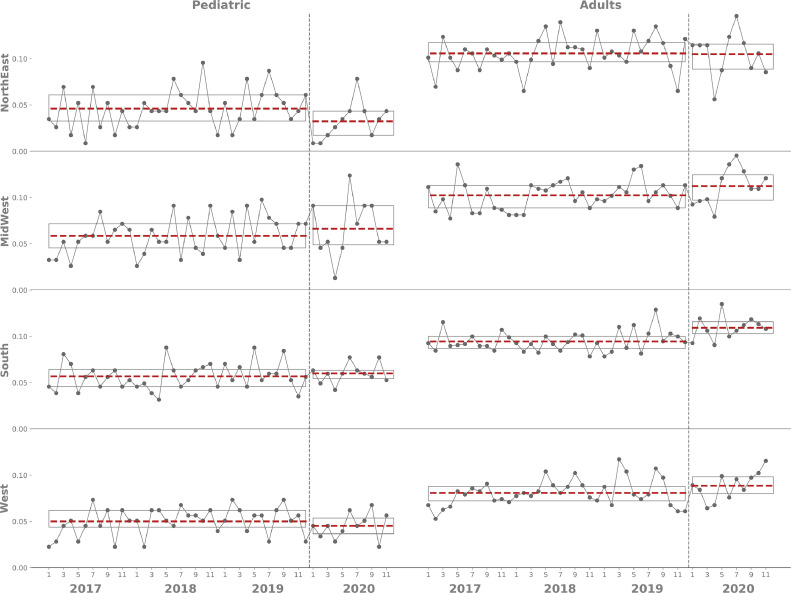
Transplant rate per 100,000 by region (Fig. 4) revealed a decrease in the number of pediatric transplants for the Northeast and the West, while the Midwest and the South had increases in the transplant rate. For the adult population, the Northeast remained effectively unchanged, while the transplant rate for all other regions increased. The South in particular had the largest increase in transplants, while the West and Midwest had smaller increases.
Figure 4.
Transplant rate per 100,000 residents by census region for pediatric and adult populations divided into pre-COVID era (Jan. 2017 – Dec. 2019) and COVID era (Jan. 2020 – Nov. 2020) shown by a dashed line. Means are shown by the dashed red line, while the box shows the interquartile range.
Changes from the Pre- COVID to COVID era are summarized in Table 3. For the adult population, waiting list deaths decreased by ∼15%, while transplants increased by ∼10%. Regionally this was reflected by a decrease in the Northeast and the South, with smaller increases in the Midwest and the West. Transplant rates remained effectively unchanged for the Northeast, while increasing in all other regions. For the pediatric population, the mortality rate decreased in both the Northeast and the Midwest, while increasing in the South and the West. Transplant rates decreased for the Northeast and the West, while increasing in the Midwest and the South.
Table 3.
Changes in rate from Pre- COVID to COVID for waiting list (WL) deaths, transplants, mortality rate and transplant rate. Mean values are provided with standard deviations given in parentheses.
| Adult | Pediatric | |||||
| Pre-COVID | COVID | % Diff | Pre-COVID | COVID | % Diff | |
| Waitlist mortality | 18•44 | 15•70 | -14•86% | 5•31 | 4•3 | -10•92% |
| Transplants | 242•06 | 266•09 | 9•93% | 39•31 | 39•00 | -0•79% |
| Mortality Rate x 10−3 | ||||||
| Northeast | 9•87 (4•98) | 6•95 (3•38) | -29•58% | 7•00 (7•89) | 3•16 (4•18) | -54•86% |
| Midwest | 7•18 (3•66) | 7•38 (4•93) | 2•79% | 8•87 (7•06) | 4•74 (2•90) | -46•56% |
| South | 8•10 (3•43) | 5•99 (2•66) | -26•05% | 7•80 (5•04) | 9•26 (6•04) | 18•72% |
| West | 3•94 (2•50) | 4•20 (2•67) | 6•60% | 5•17 (5•55) | 5•65 (7•22) | 9•28% |
| Transplant Rate x 10−2 | ||||||
| Northeast | 10•57 (1•78) | 10•51 (2•29) | -0•57% | 4•61 (2•06) | 3•24 (1•93) | -29•72% |
| Midwest | 10•23 (1•52) | 11•24 (1•91) | 9•87% | 5•86 (1•98) | 6•63 (2•94) | 13•14% |
| South | 9•45 (1•09) | 10•93 (1•21) | 15•66% | 5•67 (1•42) | 6•00 (1•01) | 5•82% |
| West | 8•08 (1•41) | 8•86 (1•47) | 9•65% | 5•00 (1•46) | 4•52 (1•32) | -9•60% |
Mortality rate by state shows more localized differences (SI Fig. 1). States are descending order by COVID-19 death rate. For pediatric populations, ND, OK and HI show higher increase in mortality than counterparts. Other states with increases are FL, GA, AR and LA. In the adult population, IA, WY, OK, VT and ME have highest mortality increases. SD, ND, MI, AL, UT, OR and HI also had increases in adult mortality rate.
4. Discussion
This study describes the regional and national variation in adult and pediatric heart transplant activity and waitlist mortality during the COVID-19 pandemic for the year 2020 as compared to the previous three years. Findings indicate that waitlist mortality decreased more for adults than pediatric population with regional variations. The total number of pediatric heart transplants did not change, albeit there was an earlier downward trend, and adult transplant volume increased throughout the year, with associated gender and racial differences.
4.1. Waitlist Mortality
Overall, COVID-19 waitlist mortality for pediatric heart transplant decreased by 10% during 2020 versus Pre- COVID mortality rates (Table 3). Initially, there was a gradual decline in the first four months of 2020, followed by an increase in months four to six, and then subsequently followed by a progressive decline through November (Fig. 1). Regional differences (Fig. 3, Table 3) that resulted in this finding came primarily from Northeast region (decrease by 7•5%) and Midwest region (decrease by 9%). We surmise that contributing factors include a decrease in waitlist additions likely due to delays in non-urgent evaluations along with a decrease in heart failure hospitalizations [2]. This was reflected in our data analyses as well, by comparing waiting list time from Table 1 and Table 2. Furthermore, decrease in mortality rate in Midwest could be due to more transplant centers being inactivated. However, our study was not designed to look at practice patterns of individual centers. Patients who expired in 2020 remained on the waiting list longer than the average waiting list population for both adult (473•97 Table 2 vs. 70•17 Table 1) and pediatric populations (116•83 Table 2 vs. 84•65 Table 1). We identified differences in mortality outcomes by race, with waitlist mortality for White population decreasing, Black mortality remaining unchanged, and mortality in Hispanics increasing. This could be partly explained by a greater decrease in the number of waitlist additions among Whites as well as severe heart failure (higher level) status in Blacks and Hispanics. The study by DeFilippis [1] looked at centers in New York, NY and found that most of the patients were inactivated on the transplant list except those that had the highest mortality risk, thus limiting active patients to Status 1 and 2 on the new heart allocation policy. Highly-sensitized patients requiring higher acuity of care and prolonged immunosuppression were also restricted. We also identified a higher female mortality rate during this time suggesting that women may have been disproportionally affected. Comparatively, a larger decrease of 15% was seen among adult waitlist mortality. The Northeast and South regions were key drivers for that decrease in adult wait-list mortality. We postulate that since these were the main regions affected early in the pandemic, stringent criteria were set by adult transplant centers to prioritize highly acute transplant patients and hence we see that difference. Restrictions on children and the prevalence of COVID in children was not appreciated in the early days and may have resulted in the comparative increase in the number of waitlist mortality in pediatrics. In adults, both Blacks and Hispanics had an increase in mortality.
4.2. Transplant Volume
The average number of pediatric heart transplants (n=39•3 per month over a 36-month range Pre-COVID) did not change significantly for the year 2020 (n=39•0 per month over an 11-month range). These values are in line with previous findings [14]. However, there was a sharp decrease in transplant volume in the first four months followed by a rapid increase from months four to six, with a return to baseline towards the end of the year. One could attribute the earlier yearly decline to seasonal variation similar to pre-COVID years, although the decline was more marked in 2020 than other years due likely to changes from COVID-19. These changes include concerns regarding COVID-19 positive donors, lack of intensive care unit beds, as well as limitations in the ability to procure organs as a result of personnel limitations and travel restrictions. It appears that May 2020 was the beginning of the reactivation phase (Fig. 2) where programs probably adjusted to the new social distancing norms. This is also when we see an upward trend in the waitlist mortality for pediatrics and to a lesser degree adult. Most institution-specific guidelines started to emerge, as did consensus documents from national and international specialty societies regarding COVID-19 protocols. Strategies to minimize contact between patients and health care workers were developed and resource optimization and prioritization of patients was also instituted. For adults, however, the average number of transplants increased (n=266 per month during COVID from n=242 per month pre-COVID). There was an earlier, sharper downward trend but that was short-lasting, and the curve started to rise more steeply than pediatric patients and continued to stay higher for the remainder of the year. This finding is understandable as there are relatively more adults on the waiting list and programs started reactivation after the first quarter with presumptive increase in the number of organ donations due to unexpected deaths as has been reported in earlier COVID related studies [3].
4.3. Policy Implications
The data provided help elucidate potential policy guidelines for future pandemics. The transplant community should strive to be proactive and equip ourselves with improved preparation, organized systems and put a systematic process in place for the next pandemic. Considerations for donor offers must include detailed travel history and related exposures, identification of high-risk behaviors of contracting and/or transmitting a lethal and highly contagious infection. Education for not only clinicians, but other transplant team members, and most importantly, patients and their families who may fear reaching out to medical facilities is paramount to handling future pandemics. Decline in heart failure hospitalizations has been reported with COVID-19 as a result of a ‘weathering-the-storm’ mentality .1 This obviously adds an enormous burden on the healthcare system when either these patients get sick at home or present to the hospital in a dire clinical state, as they become worse transplant candidates. For a future approach, the transplant community needs to pay particular attention to this and innovate with systems such as telemonitoring, improved accessibility, dedicated intensive care unit beds to house these fragile patients. Immediate post-transplant management may include selecting a core group of nurses, midlevel providers and clinicians that are assigned to only immunosuppressed patients, preventing excessive turnover with infected patients. Limited family and visitor contact also helps reduce spread, and should be put in place from the beginning of any future outbreaks. How we need to adapt and change immunosuppressive and induction treatment continues to be an ongoing discussion, and we will have more information as studies look specifically at transplant recipient immune response to COVID-19 infection as well as response post-vaccination. Even though stable outpatient adult patients on the transplant waiting list may be temporarily inactivated, this option does not always exist for pediatric heart failure patients. The majority of these patients are in-hospital or on mechanical assist devices that have not reached a suitable point for outpatient management. With new devices such as HeartMate III now being approved by the FDA for pediatric use as durable strategy, this may change for a few selected patients, the majority of whom will continue to require higher level in-hospital care [15,16]. Legislation and policymaking, both at federal and state level have to be well thought out early in the process. Even though the federal government started applying travel and social distancing restrictions, disparate policies were instituted on a state-by-state basis. While the federal government took steps to recommend providing and receiving care through telehealth, additional steps allowing HIPAA flexibility, modifying Medicare and Medicaid policies, interstate licenses and prescription of controlled substances are necessary [17,18] Lastly, as shown in our supplemental data (SI Fig. 1), states such as North Dakota, Oklahoma and Hawaii had higher pediatric waitlist mortality, and Iowa, Alabama, Wyoming, Virginia, Arkansas and Vermont had higher adult waitlist mortality. This does not coincide with COVID-19 related mortality rates and does not correlate with the mortality trends in the previous three years. While the underlying cause for this trend is unclear, there are several potential explanations for this observation. One is a decrease in access to healthcare workers. A second is a change in available healthcare resources at the height of COVID-19 due to travel and visitation limitations. A third is healthcare workers travelling to high pandemic areas to provide care resulting in a loss of local resources. Resource limitations for these states could have been further affected by the growing COVID-19 related cases as all resources were diverted to take care of these patients limiting availability for other cases. COVID-19 cases are now on the decline in the United States with widespread vaccination. As the healthcare system returns to normal or adjusts to a new normal, will waiting list mortality return to previous levels? This question will be answered in an ongoing study currently being conducted by our team.
Our study has inherent limitations of the descriptive approach. This approach does not allow us to assess causality, correlations or inferences to provide a deeper statistical understanding. However, we argue that this still provides valuable information that in some form is self-evident. A second limitation is derived from the UNOS dataset. The waitlist data and transplant volume information does not have associated COVID-19 data for the first half of the year and direct associations could not be made. COVID-19 data and deaths were obtained from the COVID Act Now Project which provides real time data. However, it is not supervised by a governmental or healthcare organization and is completely volunteer based.
This study revealed the extent of the impact of the COVID-19 pandemic on cardiac transplant waitlist, cardiac transplant waitlist mortality and cardiac transplant volume in pediatric and adult populations in the United States.
Contributors
AA conceived the study idea. AA, JC, LA and AK contributed to the protocol and design of the study. JC coordinated data request through UNOS for data collection. GG, LA, EA and MR undertook data gathering and statistical analysis. AA, GG, JC, LA, EA, MR, JQ, MP, AS and AK contributed to the preparation of the report. AA, GG, JC and AK verified the data from the UNOS. AA, GG, LA, EA, MR and AK analyzed the data for reporting. All authors were responsible for the decision to submit the manuscript. All authors critically reviewed and approved the final version of the manuscript.
Declaration of interests
The authors declare no competing interests in any form.
Data sharing statement
Data from UNOS is available to all participating institutions and is not publicly available. Proposals from interested participants are reviewed and approved by the investigators and collaborators on the basis of scientific merit. After approval of proposal, data can be shared after signing a data access agreement. Data used in this study from US Census and CovidActNow project are publicly available for anyone to access.
Acknowledgments
Acknowledgements
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100060.
Appendix. Supplementary materials
References
- 1.DeFilippis EM, Farr MA, Givertz MM. Challenges in Heart Transplantation in the Era of COVID-19. Circulation. 2020 Jun 23;141(25):2048–2051. doi: 10.1161/CIRCULATIONAHA.120.047096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez GA, Moore CK, Lennep BW, Mcmullan MR, Butler J. Reductions in heart failure hospitalizations during the COVID-19 pandemic. Journal of cardiac failure. 2020 Jun 1;26(6):462–463. doi: 10.1016/j.cardfail.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C. Organ procurement and transplantation during the COVID-19 pandemic. The Lancet. 2020 May 23;395(10237):e95–e96. doi: 10.1016/S0140-6736(20)31040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeFilippis EM, Sinnenberg L, Reza N, Givertz MM, Kittleson MM, Topkara VK, Farr MA. Trends in US heart transplant waitlist activity and volume during the coronavirus disease 2019 (COVID-19) pandemic. JAMA cardiology. 2020 Sep 1;5(9):1048–1052. doi: 10.1001/jamacardio.2020.2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Network for Organ Sharing Data - UNOS. 2020. http://optn.transplant.hrsa.gov/data.
- 6.US Census Bureau Data - US Census. 2020. https://data.census.gov/.
- 7.Covid ActNow - Data. 2021. https://covidactnow.org/.
- 8.Kluyver T, Ragan-Kelley B, Pérez F, Granger BE, Bussonnier M, Frederic J, Kelley K, Hamrick JB, Grout J, Corlay S, Ivanov P. Jupyter Notebooks-a publishing format for reproducible computational workflows. 2016 May 26.
- 9.Anaconda Software Distribution. (2020). Anaconda Documentation. Anaconda Inc. Retrieved from https://docs.anaconda.com/.
- 10.Pérez F, Granger BE. IPython: a system for interactive scientific computing. 2007 Jun 18;9(3):21–29. Computing in science & engineering. [Google Scholar]
- 11.Harris CR, Millman KJ, van der Walt SJ, Gommers R, Virtanen P, Cournapeau D, Wieser E, Taylor J, Berg S, Smith NJ, Kern R. Array programming with NumPy. Nature. Sep 2020;585(7825):357–362. doi: 10.1038/s41586-020-2649-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McKinney W. Data structures for statistical computing in python. InProceedings of the 9th Python in Science Conference. Jun 28 2010;445:51–56. [Google Scholar]
- 13.Hunter JD. Matplotlib: A 2D graphics environment. Computing in science & engineering. May 1 2007;9(03):90–95. [Google Scholar]
- 14.Colvin M, Smith JM, Hadley N, Skeans MA, Uccellini K, Lehman R, Robinson AM, Israni AK, Snyder JJ, Kasiske BL. OPTN/SRTR 2017 annual data report: heart. American Journal of Transplantation. Feb 2019;19:323–403. doi: 10.1111/ajt.15278. [DOI] [PubMed] [Google Scholar]
- 15.O'Connor MJ, Lorts A, Davies RR, Fynn-Thompson F, Joong A, Maeda K, Mascio CE, McConnell PI, Mongé MC, Nandi D, Peng DM. Early experience with the HeartMate 3 continuous-flow ventricular assist device in pediatric patients and patients with congenital heart disease: a multicenter registry analysis. The Journal of Heart and Lung Transplantation. Jun 1 2020;39(6):573–579. doi: 10.1016/j.healun.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 16.Abbott Laboratories. 2020. https://abbott.mediaroom.com/2020-12-17-FDA-Approves-Labeling-Update-for-Abbotts-HeartMate-3-Heart-Pump-for-use-in-Pediatric-Patients.
- 17.U.S. States and Territories Modifying Requirements for Telehealth in Response to COVID-19. Federation of State Medical Boards.
- 18.Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency [Internet].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.