Abstract
Background
for shared decision-making, it is important to discuss of the patients’ priorities in order to align treatment decisions with these priorities.
Objective
to assess the most important health outcome for older patients on the verge of making a treatment decision, using the Outcome Prioritization Tool (OPT). Secondary objectives were the feasibility of the OPT and patient variables associated with prioritising different health outcomes.
Design
retrospective cohort study.
Setting and subjects
at the University Medical Hospital Groningen, the Netherlands, 350 patients were included who visited the geriatric outpatient clinic during the work-up regarding a complex treatment decision (such as cancer treatment or heart valve replacement).
Methods
during geriatric assessment, patients prioritised between four health outcomes, using the OPT.
Results
median age was 78.5 years, 172 (49.1%) were referred regarding a treatment decision for a malignant disease. Cognitive impairment was present in 23.6%. Most patients (55.2%) prioritised maintaining independence as their most important goal, followed by extending life in 21.1%. Only cognitive impairment was significantly associated with prioritising extending life as the most important health outcome. For 107 patients (30.6%), the OPT was not feasible; these patients more often had malnutrition and assisted living.
Conclusions
the main health outcome of older patients on the verge of making a treatment decision was maintaining independence, followed by extending life. Patients with cognitive impairment more often prioritised extending life. The OPT was feasible as a decision aid for most patients. For optimal shared decision-making, it is crucial to take patient preferences into account.
Keywords: health outcome prioritiszation, Outcome Prioritization Tool (OPT), patient preferences, decision-making, older patients, older people
Key Points
Using the Outcome Prioritization Tool (OPT) can support shared decision-making.
Maintaining independence was the most important health outcome for older patients.
Only patients with cognitive impairment prioritised ‘extending life’ more often.
The OPT was feasible for most patients facing complex decisions.
Introduction
Assessing patient’s goals and preferences is an important aspect of shared decision-making. However, it has been shown that healthcare professionals often have limited knowledge of these goals and preferences [1–3]. A decision aid might support engaging a conversation about goals and preferences.
The Outcome Prioritization Tool (OPT) is such a decision aid. It assesses universal health outcomes and is thereby neither disease nor treatment specific. This makes the tool usable in different settings [4]. The health outcomes used in the OPT are extending life, maintaining independence, reducing pain or reducing other symptoms (such as dyspnoea or nausea). The OPT uses a trade-off principle for competing outcomes, i.e. the notion that reaching a certain outcome can have negative impact on another outcome [5]. Using the OPT, the patient is invited to prioritise and rate the health outcomes in order of importance [6]. The OPT has mostly been studied in older patients with multimorbidity [6, 7]. Little is known about the use of the OPT in clinical decision-making regarding intensive treatments (such as cancer therapy or surgery).
This study assesses the main health outcome prioritised by older patients on the verge of making a complex treatment decision, using the OPT.
Methods
Setting
This retrospective study was performed at the Department of Geriatric Medicine at the University Medical Center Groningen (UMCG). All patients referred to the geriatric outpatient clinic for co-assessment in treatment decision-making between April 2018 and October 2019 were included. There were no other inclusion or exclusion criteria. Patient and disease characteristics were extracted from the patient’s medical records.
Patients
There were three groups of patients referred for co-assessment: (i) patients aged ≥65 years with an aortic valve stenosis eligible for transcatheter aortic valve implantation (TAVI), (ii) patients with cancer, who were considered frail, based on a nurse-led geriatric assessment, [8] and (iii) patients referred based on the clinical judgement of the treating physician.
Comprehensive geriatric assessment
At the geriatric outpatient clinic, a Comprehensive Geriatric Assessment (CGA) was performed and patient preferences were assessed using the OPT. During the CGA, four geriatric domains were assessed (somatic, psychological, social and functional) [9–15] (Figure 1). Based on the results of CGA, the level of frailty was determined, defined as an accumulation of deficits on the geriatric domains [16].
Figure 1 .
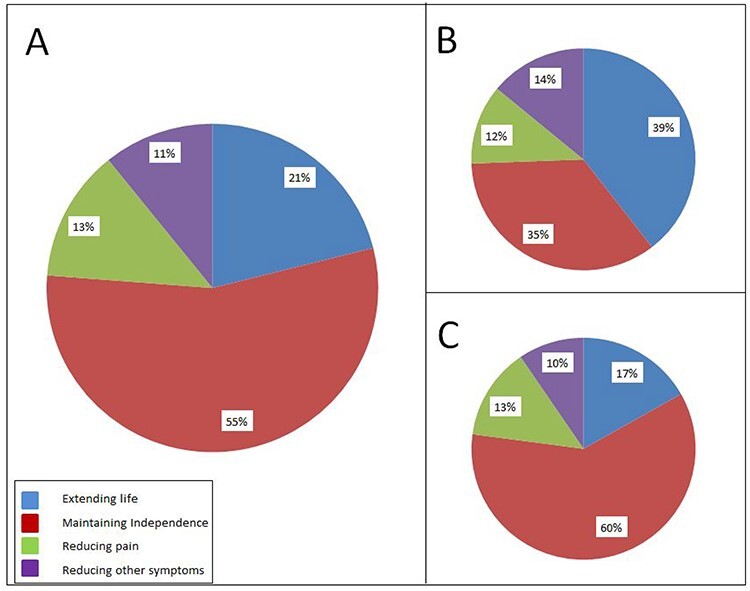
Main health outcomes, using the OPT. Main health outcome for (A) the total group (n = 223) and for the subgroup (B) with cognitive impairment (n = 43) and (C) without cognitive impairment (n = 179).
Patients’ preferences
The patients’ preferred health outcomes were assessed using the OPT [6]. On a VAS from 0–100, The patient is invited to prioritise and rank the four health outcomes. Due to the principle of trade-offs, no two health outcomes can have an equal score. For the analysis, the most important health outcome was registered. If, despite instructions, patients ranked two outcomes the same, these data were left out of the analysis of the main OPT goals.
Outcome measures
The primary outcome was the main health outcome as prioritised by the patient. The secondary outcomes were the feasibility of the OPT and the associations between patient- and disease characteristics with the main OPT goal and with the feasibility of the OPT.
Statistical analysis
Baseline characteristics, feasibility and main health outcome were analysed using descriptive statistics. To assess the association between patient and disease characteristics and 1. main health outcome prioritisation and 2. feasibility, univariate logistic regression was performed, followed by multivariate analyses for variables with a p < 0.1. A p-value smaller than 0.05 was considered significant. Statistical analysis was performed using IBM SPSS Statistics 23.
Statement of ethics
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. Permission was granted by the local medical ethical committee. A waiver of consent was obtained from the relevant institutional review board.
Results
Patients
Table 1 shows the characteristics of the 350 included patients. Median age was 78.5 years; the majority were male. Most patients with a benign disease were referred with an indication for transcatheter aortic valve replacement (TAVI). Other benign diseases included other heart and vessel disease, benign tumours, cochlear implant, hip/knee replacement and kidney failure. Most patients with a malignant disease suffered from head and neck cancer.
Table 1 .
Baseline characteristics and CGA for the total group and association of the variables with feasibility of the OPT
| Baseline characteristics and CGA (n = 350) | Log regression for the OPT not being feasible (n = 107) | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis** | |||||||
| Variable | N (%)* | OR | 95% CI | P | OR | 95% CI | P | |
| BASELINE CHARACTERISTICS | ||||||||
| Age | ||||||||
| Median (IQR) | 78.5 (73.0–82.25) | |||||||
| >70 | 305 (87.1) | 1.24 | 0.62–2.52 | 0.54 | ||||
| Gender | ||||||||
| Male | 195 (55.7) | 0.97 | 0.61–1.53 | 0.89 | ||||
| Reason for referral | ||||||||
| Benign | 178 (50.9) | |||||||
| TAVI | 137 (77.0) | |||||||
| Cochlear implant placement | 12 (6.7) | |||||||
| Other benign diseasea | 29 (16.3) | |||||||
| Malignant | 172 (49.1) | 1.49 | 0.95–2.36 | 0.09 | 1.10 | 0.64–1.90 | 0.74 | |
| Head and neck tumour | 85 (49.4) | |||||||
| Gastrointestinal tumour | 29 (16.9) | |||||||
| Skin tumour | 27 (15.7) | |||||||
| Urogenital tumour | 15 (8.7) | |||||||
| Other malignancyb | 16 (9.3) | |||||||
| Tumour stage (n = 172) | ||||||||
| I | 15 (8.7) | |||||||
| II | 28 (16.3) | |||||||
| III | 39 (22.7) | |||||||
| IV | 55 (32.0) | |||||||
| Missing, not applicable or unknownc | 35 (20.3) | |||||||
| GERIATRIC ASSESSMENT | ||||||||
| Somatic | Charlson Comorbidity Index | |||||||
| Median (IQR) | ||||||||
| ≥3 points | 190 (54.3) | 1.38 | 0.87–2.19 | 0.17 | ||||
| Malnutrition (Mini Nutritional Assessment, Short Form) | ||||||||
| Risk of malnutrition | 137 (40.5) | 2.39 | 1.48–3.87 | <0.001 | 1.78 | 1.04–3.07 | 0.04 | |
| Psychological | Leven of educationd | |||||||
| Low | 218 (64.9) | 1.10 | 0.67–1.79 | 0.71 | ||||
| Cognition | ||||||||
| Cognitive impairmente | 82 (23.6) | 2.05 | 1.22–3.42 | 0.006 | 1.76 | 0.97–3.17 | 0.06 | |
| Mood | ||||||||
| Signs of depressionf | 33 (9.6) | 2.14 | 1.03–4.43 | 0.04 | 1.49 | 0.66–3.38 | 0.34 | |
| Social | Marital status | |||||||
| No partner | 132 (37.8) | 1.45 | 0.91–2.30 | 0.12 | ||||
| No children | 48 (13.7) | 1.44 | 0.76–2.71 | 0.26 | ||||
| Living situation | ||||||||
| Assisted | 32 (9.2) | 3.83 | 1.81–8.09 | <0.001 | 2.88 | 1.22–6.75 | 0.02 | |
| Home care | 1.72 | 1.01–2.90 | 0.04 | 0.19 | 1.52–0.82 | 2.84 | ||
| Functional | (i)ADLg | |||||||
| ADL dependent | 189 (54.9) | 1.14 | 0.72–1.81 | 0.59 | ||||
| IADL dependent | 221 (64.2) | 1.59 | 0.97–2.62 | 0.07 | 0.96 | 0.53–1.74 | 0.88 | |
| Mobility | ||||||||
| Timed Up and Go test > 15 s | 61 (20.5) | 1.25 | 0.67–2.33 | 0.49 | ||||
| Walking aid | 144 (41.4) | 0.98 | 0.61–1.55 | 0.92 | ||||
| Frailty | ||||||||
| Frail based on CGAh | 209 (59.7) | 1.34 | 0.83–2.14 | 0.23 | ||||
| VAS EQ5Di (median) | 70 (50–80) | 1.01 | 0.99–1.02 | 0.46 | ||||
Liver or kidney transplantation, vascular surgery, orthopaedic surgery, benign head and neck surgery, benign neurosurgery, benign abdominal surgery.
Sarcoma, breast cancer, hepatobiliary cancer, Merkel cell carcinoma, haematological malignancy, unknown primary, suspected malignancy, but no definite diagnosis.
Haematological malignancy, no pathological diagnosis, unknown primary, no staging.
Education level according to Verhage.
Cognitive impairment as determined by the internist geriatrician based on the CGA.
PHQ-2: Patients Health Questionnaire-2.
(i)ADL: (instrumental) activities of daily living, assessed by the KATZ-15, a score of one or higher on the ADL and iADL subscale was considered as being dependent.
Frailty as determined by the internist geriatrician based on the CGA.
Self-assessed health based on the EQ5D VAS.
*All values are given as N(%) unless otherwise specified.
**Variables with a P < 0.1 in univariate analysis were entered in the multivariable model.
Bold: variables with a p value <0.05.
Comprehensive geriatric assessment
Comorbidity was common (54.3%). Eighty-two patients (23.4%) were diagnosed with cognitive impairment based on the CGA and most patients were dependent in ADL and iADL. More than half of the patients were considered frail by the geriatrician (Table 1).
Patients’ main health outcome
For 243 patients (69.4%), preferences could be assessed using the OPT, of which 20 ranked two or more outcomes equally. Of the 223 patients who prioritised one health outcome, more than half prioritised maintaining independence, followed by extending life, reducing pain and reducing other symptoms (Figure 1).
In univariate analysis, a low education level, having a malignancy, cognitive impairment and frailty were associated with higher odds of prioritising ‘life extension’ as the main goal. High comorbidity, cognitive impairment, ADL deficits and frailty were associated with lower odds of prioritising ‘maintaining independence’ as a main goal. In multivariate analysis, having cognitive impairment was the only variable significantly associated with prioritising ‘extending life’ (odds ratio (OR) 2.78, 95% confidence interval (CI) 1.22–6.33, P = 0.02) as well as with prioritising ‘maintaining independence’ less often (OR 0.46, 95%CI 0.22–0.97, P = 0.04).
Feasibility
In 107 patients (30.6%), the OPT could not be assessed. The results of the univariate and multivariate analyses are shown in Table 1. In multivariate analysis, assisted living and a high risk of malnourishment were significantly associated with not using the OPT.
Discussion
This study shows that most older patients facing a complex treatment decision regarding intensive treatments prioritised maintaining independence as their most important health outcome, using the OPT. Since the intensive treatments are often aimed at life extension, this is an important finding. This is in line with previous research, that has shown that older patients facing a trade-off in decision-making often value retaining of independence, function and cognition over extending life per se [17]. Assessment of patients’ preferences is considered an important aspect in shared decision-making [18, 19]. However, research has shown that preference misdiagnoses are frequent [2, 20] emphasising the importance of discussing goals and preferences [20, 21]. Using the OPT to discuss health outcome preferences was feasible for 7 out of 10 patients.
As far as we know, this is the first large cohort of patients in which the OPT was used in complex treatment decision-making. Only one previous study describes incorporating the OPT in treatment decision-making in older patients with cancer [8]. The OPT has mostly been studied in older patients with multimorbidity and regarding decision-making on polypharmacy [6]. Assessment of patient priorities in cancer patients, using other tools, has been shown to have a positive effect on communication, shared decision-making and patient satisfaction [22]. In a recent study, the use of the OPT by general practitioners in patients with non-curable cancer was associated with less anxiety and fatigue [23]. Priorities-aligned care might also improve patient outcomes by minimising harm and treatment burden [24].
There were a higher number of patients prioritising extending life when cognitive impairment was present. Patients with cognitive impairment might find it more difficult to oversee different health outcomes and understand the trade-off principle. A study by Fazel et al. showed that patients with dementia more often indicate a preference for treatment interventions on realistic clinical vignettes [25]. It has also been shown that a decline in health status can lead to accepting a further decline more easily [26]. This might be explained by an adaptation to increased dependency, leading to a reprioritisation response shift [27]. Furthermore, it is known that treatment-specific preferences can change over time as well as with a change in health status [28].
The OPT is a decision aid that in our sample was feasible for most older patients. Even if a patient is not able to prioritise the four health outcomes, introducing the tool might facilitate discussing preferences and trade-offs in order to align decision-making. The OPT was less feasible for patients in assisted living and with malnourishment. This might be due to the fact that these patients were more ill and did not have the concentration to fill in the OPT, or this was perceived as such by the healthcare professional.
There are some limitations to our study. This was a selected group of patients with a high level of (suspected) frailty. Only the TAVI patients were unselected. The analysis was retrospective, and we were limited to information noted in the patient’s files. It was therefore not always possible to assess the exact reason for not assessing the OPT. Furthermore, not using the OPT could be due to a selection bias of the doctor deciding not to use the OPT, for instance when the patient had cognitive impairment. Still, this reflects a real life setting in a heterogeneous geriatric population.
Conclusions and implications
The OPT is a decision aid feasible for most patients facing complex treatment decision-making regarding intensive treatment. Maintaining independence was considered the most important health outcome by the majority of older patients, which is relevant to consider in treatment decisions. In order to align care to patients’ preferences, it is important to explicitly discuss these goals and preferences. Future research should be aimed at how priorities-aligned care improves decision-making and patient outcomes.
Acknowledgements
We thank H.J. van der Zaag for advice on the analysis and on the article text. We thank D.J. Bosold for text editing. Data from this research have been submitted and accepted as a poster presentation at the Dutch Geriatrics Society (geriatriedagen NVKG) meeting in February 2021.
Contributor Information
Suzanne Festen, University Center for Geriatric Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Yvette Z van Twisk, University Center for Geriatric Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Barbara C van Munster, University Center for Geriatric Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Pauline de Graeff, University Center for Geriatric Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
None.
References
- 1. Bruera E, Sweeney C, Calder K, Palmer L, Benisch-Tolley S. Patient preferences versus physician perceptions of treatment decisions in cancer care. J Clin Oncol 2001; 19: 2883–5. [DOI] [PubMed] [Google Scholar]
- 2. Mulley AG, Trimble C, Elwyn G. Stop the silent misdiagnosis: patients’ preferences matter. BMJ 2012; 345: e6572. [DOI] [PubMed] [Google Scholar]
- 3. Montgomery AA, Fahey T. How do patients' treatment preferences compare with those of clinicians? Qual Health Care 2001 Sep;10; Suppl 1: i39–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fried TR, Tinetti M, Agostini J, Iannone L, Towle V. Health outcome prioritization to elicit preferences of older persons with multiple health conditions. Patient Educ Couns 2011; 83: 278–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Case SM, O'Leary J, Kim N, Tinetti ME, Fried TR. Older adults’ recognition of trade-offs in healthcare decision-making. J Am Geriatr Soc 2015; 63: 1658–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stegmann ME, Festen S, Brandenbarg D et al. Using the Outcome Prioritization Tool (OPT) to assess the preferences of older patients in clinical decision-making: a review. Maturitas 2019; 128: 49–52. [DOI] [PubMed] [Google Scholar]
- 7. Fried TR, Tinetti ME, Iannone L, O'Leary JR, Towle V, Van Ness PH. Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med 2011; 171: 1854–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Festen S, Kok M, Hopstaken JS et al. How to incorporate geriatric assessment in clinical decision-making for older patients with cancer. An implementation study. J Geriatr Oncol 2019; 10: 951–9. [DOI] [PubMed] [Google Scholar]
- 9. Kaiser MJ, Bauer JM, Ramsch C et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging 2009; 13: 782–8. [DOI] [PubMed] [Google Scholar]
- 10. Rijnen SJM, Meskal I, Emons WHM et al. Evaluation of normative data of a widely used computerized neuropsychological battery: applicability and effects of sociodemographic variables in a Dutch sample. Assessment 2020 Mar; 27: 373–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer 2004; 4: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41: 1284–92. [DOI] [PubMed] [Google Scholar]
- 13. Laan W, Zuithoff NP, Drubbel I et al. Validity and reliability of the Katz-15 scale to measure unfavorable health outcomes in community-dwelling older people. J Nutr Health Aging 2014; 18: 848–54. [DOI] [PubMed] [Google Scholar]
- 14. Huisman MG, van Leeuwen BL, Ugolini G et al. ``Timed Up & Go'': a screening tool for predicting 30-day morbidity in onco-geriatric surgical patients? A multicenter cohort study. PLoS One 2014; 9: e86863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kristensen MT, Bloch ML, Jønsson LR, Jakobsen TL. Interrater reliability of the standardized Timed Up and Go Test when used in hospitalized and community-dwelling older individuals. Physiother Res Int 2019; 24: e1769. [DOI] [PubMed] [Google Scholar]
- 16. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381: 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fried TR, Bradley EH. What matters to seriously ill older persons making end-of-life treatment decisions? A qualitative study. J Palliat Med 2003; 6: 237–44. [DOI] [PubMed] [Google Scholar]
- 18. Bomhof-Roordink H, Gärtner FR, Stiggelbout AM, Pieterse AH. Key components of shared decision making models: a systematic review. BMJ Open 2019; 9: e031763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fried TR. Shared decision making--finding the sweet spot. N Engl J Med 2016; 374: 104–6. [DOI] [PubMed] [Google Scholar]
- 20. Ramer SJ, McCall NN, Robinson-Cohen C et al. Health outcome priorities of older adults with advanced CKD and concordance with their nephrology providers' perceptions. J Am Soc Nephrol 2018; 29: 2870–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tinetti ME, Naik AD, Dindo L et al. Association of patient priorities-aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: a nonrandomized clinical trial. JAMA Intern Med 2019; 179: 1688–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Frey MK, Ellis A, Shyne S, Kahn R, Chapman-Davis E, Blank SV. Bridging the gap: a priorities assessment tool to support shared decision making, maximize appointment time, and increase patient satisfaction in women with ovarian cancer. JCO Oncol Pract 2020; 16: e148–54. [DOI] [PubMed] [Google Scholar]
- 23. Stegmann ME, Brandenbarg D, Reyners AK, van Geffen WH, Hiltermann TJN, Berendsen AJ. Prioritisation of treatment goals among older patients with non-curable cancer: the OPTion randomised controlled trial in Dutch primary care. Br J Gen Pract 2020; 70: e450–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hargraves IG, Montori VM. Aligning care with patient values and priorities. JAMA Intern Med 2019; 179: 1697–98. [DOI] [PubMed] [Google Scholar]
- 25. Fazel S, Hope T, Jacoby R. Effect of cognitive impairment and premorbid intelligence on treatment preferences for life-sustaining medical therapy. Am J Psychiatry 2000; 157: 1009–11. [DOI] [PubMed] [Google Scholar]
- 26. Fried TR, Byers AL, Gallo WT et al. Prospective study of health status preferences and changes in preferences over time in older adults. Arch Intern Med 2006; 166: 890–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schwartz CE, Merriman MP, Reed GW, Hammes BJ. Measuring patient treatment preferences in end-of-life care research: applications for advance care planning interventions and response shift research. J Palliat Med 2004; 7: 233–45. [DOI] [PubMed] [Google Scholar]
- 28. Jansen SJ, Otten W, Baas-Thijssen MC, VAN DE Velde CJ, Nortier HW, Stiggelbout AM. Stability of preferences with regard to adjuvant chemotherapy: impact of treatment decision, experience and the passing of time. Eur J Cancer Care (Engl) 2008; 17: 74–83. [DOI] [PubMed] [Google Scholar]


