Abstract
Purpose
To evaluate changes in utilization of cardiac imaging—transthoracic, transesophageal, and stress echocardiography (TTE, TEE, and SE), coronary CT angiography (cCTA), cardiac MRI (cMRI), myocardial perfusion imaging (MPI), and cardiac positron emission tomography (cPET).
Materials and Methods
The 2010–2019 Physician/Supplier Procedure Summary files were used to find imaging utilization per 100 000 Medicare beneficiaries. Global and professional claims were aggregated, representing total interpretive services. Specialty codes identified provider specialty. Results were stratified by physician offices, hospital outpatient departments (HOPDs), inpatient setting, and the emergency department.
Results
From 2010 to 2019, there was a partial shift from cardiologist offices to the HOPD for TTE (office: −23%; HOPD: +107%) and SE (office: −44%; HOPD: +11%). Cardiologist cCTA also shifted from the office (−57%) to the HOPD (+211%). Radiologist-performed cCTA grew in all locations but most in the HOPD (+355%), with radiologists performing more cCTA than cardiologists in all settings. cMRI rates remain low but rose in the HOPD for both cardiologists (+209%) and radiologists (+207%). Cardiologist MPI rates dropped dramatically in the office (−52%), with a smaller absolute rate increase in the HOPD (+71%). cPET nearly tripled in the cardiology office (+193%), but rates remained steady for radiologists.
Conclusion
While most cardiologist in-office imaging has shifted to the HOPD, there has been an increase in in-office cPET, likely due to a combination of technological advances, interpretation familiarity, and financial incentives. Radiologist cCTA rates continue to increase, representing a growing opportunity for radiologists to collaborate in cardiac imaging.
Keywords: CT Angiography, Echocardiography, MR Imaging, PET, Radionuclide Studies, SPECT, Cardiac, Work Force Issues
Supplemental material is available for this article.
© RSNA, 2021
Keywords: CT Angiography, Echocardiography, MR Imaging, PET, Radionuclide Studies, SPECT, Cardiac, Work Force Issues
Summary
Cardiologist in-office echocardiography and myocardial perfusion imaging continue to shift to the hospital outpatient department, with increasing in-office cardiac PET utilization.
Key Points
■ From 2010 to 2019, cardiologist in-office myocardial perfusion imaging rates per 100 000 beneficiaries have dropped by 52% (4426 to 2119), with a corresponding rate increase in hospital outpatient departments (935 to 1598; +71%).
■ During this same period, the rates of coronary CT angiography performed by radiologists more than tripled in hospital outpatient departments (28 to 126; +355%), but overall rates remain low compared with myocardial perfusion imaging.
■ Rates of cardiac PET in cardiologist offices nearly tripled during this time (125 to 367; +193%), but rates of cardiac PET performed by radiologists in offices (eight to five; −38%) and hospital outpatient departments (10 to 19; +90%) saw little change.
Introduction
Cardiovascular disease is a prominent source of morbidity and mortality in the United States, and the diagnosis of cardiovascular disease is heavily reliant on diagnostic imaging. Radiologists and cardiologists have long participated in noninvasive cardiac imaging, but now nearly all echocardiography and myocardial perfusion imaging (MPI) is performed by cardiologists (1). As a provider who both orders and performs diagnostic cardiac imaging, cardiologists are in a distinct position that may lead to a conflict of interest in fee-for-service health care models; specifically, it has been suggested that the high volume of in-office echocardiography and MPI has persisted historically because of lucrative reimbursement incentives, despite the limitations of these studies relative to other diagnostic modalities (2). However, following the decreases in reimbursements from the Deficit Reduction Act and MPI code bundling, the rates of in-office MPI began to fall, and examinations began to shift from cardiology offices to hospital outpatient departments (HOPDs) (1). Furthermore, technological advances in competing imaging modalities such as coronary CT angiography (cCTA) and cardiac PET (cPET) may have also resulted in a shift in the preferred cardiac imaging technique (3).
Multiple imaging modalities can be used for cardiac screening and diagnostic studies with various degrees of invasiveness and effectiveness. The purpose of this study was to evaluate changes in utilization of different cardiac imaging modalities, namely echocardiography, CT, MRI, MPI, and PET, in light of rapidly changing technical innovations and the different referral frameworks for cardiologists and radiologists.
Materials and Methods
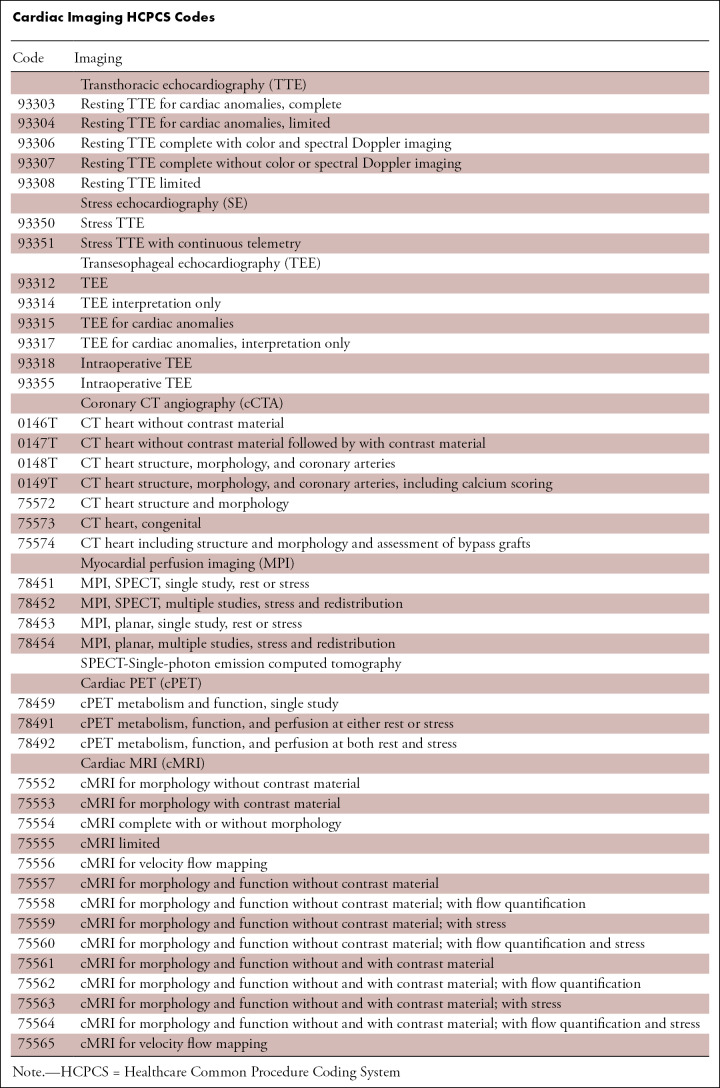
The 2010–2019 Physician/Supplier Procedure Summary (PSPS) files were obtained from the Centers for Medicare & Medicaid Services website (4). The PSPS files contain yearly summaries of the Medicare Part B carrier fee-for-service claims and do not have data on patients covered by Medicare Advantage or private insurers. Healthcare Common Procedure Coding System codes were used to identify imaging studies related to cardiac imaging, including all major noninvasive imaging modalities other than plain radiography, specifically echocardiography, cCTA, nuclear medicine MPI and cPET, and cardiac MRI (cMRI). Given the differences in invasiveness, echocardiography was subdivided into transthoracic echocardiography (TTE), stress echocardiography (SE), and transesophageal echocardiography (TEE) (Table). Because the PSPS files do not contain personal health information, this study was exempt from institutional review board approval.
Cardiac Imaging HCPCS Codes
Imaging claims in the PSPS files may be split into technical (facility and equipment use) and professional (imaging interpretation and report generation) components, or they may be billed globally (technical and professional services are combined). Split claims are identified by having codes for the technical component (code: TC) or professional component (code: 26) in either the initial or second modifier code variables within the PSPS files (4). A simple tabulation of claims will overestimate the number of imaging studies performed due to double-counting imaging studies split into technical claims and professional claims. Because we sought to determine the market share of cardiac imaging among different specialties, we decided to aggregate all professional and global claims and excluded technical claims.
Cardiac imaging is most commonly performed by cardiologists, followed by radiologists (2). To determine the market share of cardiac imaging performed by these specialties, we identified cardiologists using the specialty codes for cardiologists (code: 06), electrophysiologists (code: 21), interventional cardiologists (code: C3), and heart failure specialists (code: C7). Radiologists were identified using the codes for diagnostic radiology (code: 30), interventional radiology (code: 94), and nuclear medicine (code: 36). We tallied claims issued by multispecialty practices (code: 70) and independent diagnostic testing facilities (code: 47) as a separate category because the provider’s specialty performing the imaging study cannot be determined in these cases. The remaining specialty codes were combined to form an “other provider” category. As previously mentioned, patients with cardiac disease may undergo one of many different possible imaging modalities, and the setting where the imaging is performed may affect the type of imaging modality that is ordered, the reimbursement level, and, ultimately, financial incentives. With this in mind, we used the place of service variable in the PSPS files to identify imaging claims performed in physician offices (code: 11), the HOPD (codes: 19, 22), the emergency department (ED) (code: 23), and the inpatient setting (code: 0). The remaining imaging claims were combined to represent an “other place of service.”
The annual Medicare imaging volumes may vary not only because of changes in physician utilization but also because of changes in the number of Medicare Part B enrollees. As a result, we converted the yearly imaging volumes into rates per 100 000 beneficiaries by dividing the aggregate imaging volumes by the annual Medicare Part B population, which is publicly available on the Centers for Medicare & Medicaid Services website (5). The PSPS files represent the total number of imaging services per year for Medicare Part B enrollees; because the entire Medicare population is represented in the PSPS files, inferential statistics are not appropriate for this analysis. Data analysis was performed by using IBM SPSS Statistics for Windows, version 27.0.
Results
Echocardiography
Transthoracic echocardiography.—From 2010 to 2019, the rate of TTE performed by cardiologists decreased in the office (8299 to 6365; −23%) and saw a corresponding growth in the HOPD (2869 to 5944; +107%; Fig 1). Cardiologist TTE rates fell slightly in the inpatient setting (7249 to 6863; −5%). In the ED, TTE rates grew for both cardiologists (94 to 128; +36%) and other nonradiologist providers (34 to 131; +284%). Of the TTE performed in 2019, cardiologists performed 89% (6365 of 7163) in physician offices, 95% (5944 of 6279) in the HOPD, and 94% (6863 of 7268) in inpatient settings. However, by 2019, cardiologists performed only 49% (128 of 261) of TTE in the ED, with 50% (131 of 261) being performed by other nonradiologist providers. Radiologists performed less than 1% of all TTE in all settings.
Figure 1:
Transthoracic echocardiography (TTE) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, ED = emergency department, HOPD = hospital outpatient department, Rad = radiologist.
Stress echocardiography.—From 2010 to 2019, rates of SE performed by cardiologists decreased in the office (723 to 406; −44%), inpatient (98 to 25; −74%), and ED (11 to five; −52%) settings (Fig 2). From 2010 to 2014, there was a small increase in SE performed by cardiologists in the HOPD (365 to 454; +24%), but by 2019, the rates fell to nearly 2010 levels (overall 2010–2019 growth: 365 to 406; +11%). Radiologists performed less than 1% of SE in all four imaging locations.
Figure 2:
Stress echocardiography (SE) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, ED = emergency department, HOPD = hospital outpatient department, Rad = radiologist.
Transesophageal echocardiography.—From 2010 to 2019, TEE rates remained relatively low in comparison with those of TTE and SE, but cardiologist rates doubled in the HOPD during this time (201 to 402, +100%; Fig E1 [supplement]). Radiologists performed less than 1% of TEE in all locations.
Coronary CT Angiography
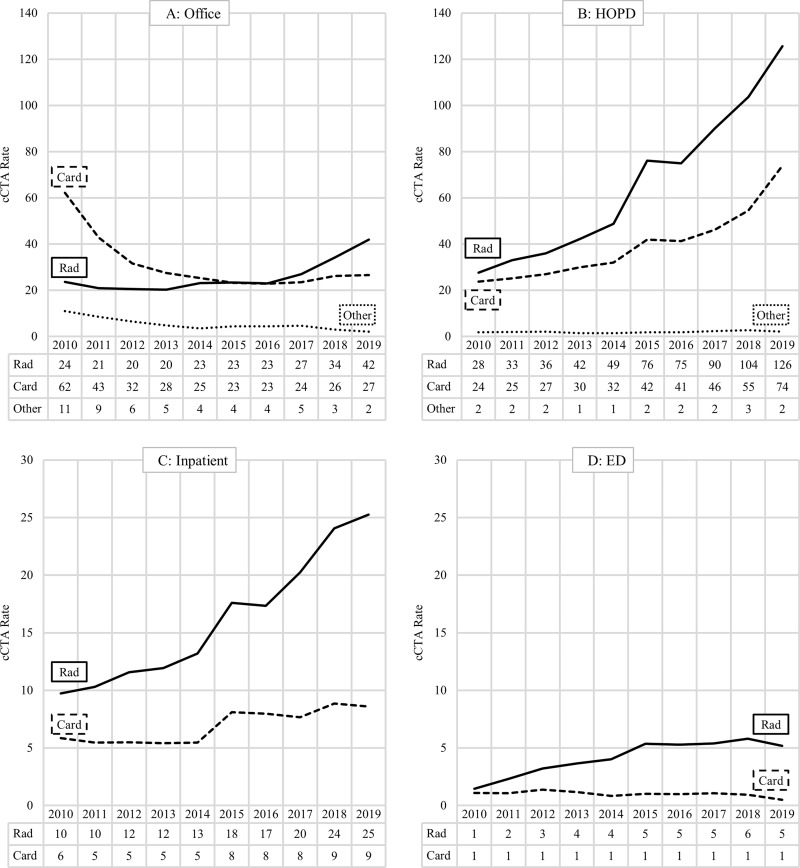
From 2010 to 2019, the rate of in-office cCTA for cardiologists fell (62 to 27; −57%), with a corresponding increase in the HOPD (24 to 74; +211%) (Fig 3). In comparison, the rates of cCTA performed by radiologists increased in all locations, but the growth was most substantial in the HOPD (28 to 126; +355%). In 2017, radiologists began to administer more cCTA in the office setting than cardiologists (27 vs 24), and by 2019, radiologists performed 59% (42 of 71) of all in-office cCTA. In 2019, most cCTA was performed by radiologists in all four locations, with radiologists performing the greatest proportion of inpatient cCTA (25 of 34 or 74%). Other nonradiologist providers performed fewer than one cCTA per 100 000 beneficiaries per any year in the inpatient and ED settings (data not shown).
Figure 3:
Coronary CTA (cCTA) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, ED = emergency department, HOPD = hospital outpatient department, Rad = radiologist.
Cardiac MRI
From 2010 to 2019, cMRI grew in the HOPD for both cardiologists (15 to 48; +209%) and radiologists (12 to 37; +207%) (Fig 4). However, the rate of cMRI performed in cardiologist offices fell by half (six to three; −50%), while cMRI in radiology offices nearly doubled (five to seven; +40%); although, overall office-based cMRI rates remained low compared with the HOPD (10 vs 85 in 2019). In 2019, cardiologists performed 55% (48 of 88) of cMRI in the HOPD, with radiologists performing 42% (37 of 88). Other nonradiologist providers performed fewer than one cMRI per 100 000 beneficiaries per year in all settings, and fewer than one cMRI was performed per any year in the ED setting (data not shown).
Figure 4:
Cardiac MRI (cMRI) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, ED = emergency department, HOPD = hospital outpatient department, Rad = radiologist.
Myocardial Perfusion Imaging
From 2010 to 2019, MPI performed by cardiologists decreased in the office (4426 to 2119; −52%) and inpatient (471 to 291; −38%) settings (Fig 5). However, MPI rates in the HOPD increased from 2010 to 2015 (935 to 1679; +80%) and then stabilized from 2015 to 2019 (overall 2010–2019 gain: 935 to 1598; +71%). Over this time frame, the rate of MPI performed by radiologists fell in all locations but most dramatically for the inpatient setting (502 to 215; −57%). In 2019, cardiologists performed 92% (2119 of 2293) of office, 75% (1598 of 2133) of HOPD, and 56% (291 of 519) of inpatient MPI, but in the ED, radiologists performed 81% (38 of 47) of MPI, albeit an overall low volume compared with the three other locations. Other nonradiologists performed no more than one MPI per 100 000 beneficiaries per any year in the ED setting (data not shown).
Figure 5:
Myocardial perfusion imaging (MPI) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, ED = emergency department, HOPD = hospital outpatient department, Rad = radiologist.
Cardiac PET
From 2010 to 2019, the rate of cPET performed by cardiologists grew in the office (125 to 367, +193%) (Fig 6) and the HOPD (25 to 72; +189%). However, the overall HOPD rates remained small compared with office rates (72 vs 367 in 2019). The rates of cPET performed by radiologists remained relatively steady over this time frame, with cardiologists performing 97% (367 of 380) of office and 78% (72 of 93) of HOPD cPET in 2019. Other nonradiologist specialties administered fewer than 14 cPET per 100 000 beneficiaries per any year in all imaging settings, and cumulatively, fewer than 18 cPET per 100 000 beneficiaries were performed per any year in the inpatient and ED settings among all specialties (data not shown).
Figure 6:
Cardiac PET (cPET) rates per 100 000 Medicare beneficiaries by specialty and place of service. Card = cardiologist, HOPD = hospital outpatient department, Rad = radiologist.
Overall Cardiac Imaging Utilization
Overall imaging rates, aggregated by place of service and specialty are described in Figure 7. Since 2010, the combined rates of TTE, TEE, and SE ("Echo" line in Fig 7) have decreased by 3% (23 911 to 23 188), and MPI has also decreased by 36% (7817 to 4996). However, cPET has risen by 146% (202 to 496), cCTA has risen by 84% (169 to 312), and cMRI has risen by 125% (53 to 119).
Figure 7:

Overall cardiac imaging rates per 100 000 Medicare beneficiaries by noninvasive imaging modality. A log10 scale was used for rates to separate the differences between the cPET, cCTA, and cMRI trendlines. TTE, TEE, and SE were combined (Echo) given the small numbers of TEE and SE. The 2010 to 2019 percentage changes per modality are listed. SE = stress echocardiography, TEE = transesophageal echocardiography, TTE = transthoracic echocardiography.
Discussion
The purpose of this study was to evaluate noninvasive cardiac imaging utilization among radiologists and cardiologists in four primary imaging locations. As noted in other recent studies, we continue to observe a shift of cardiac imaging from the cardiologist’s office to the HOPD for nearly all modalities (6); however, cPET is an exception that demonstrates increased utilization in cardiology offices since 2012. Cardiologists continue to dominate almost every aspect of cardiac imaging except for cCTA, where radiologists hold an increasing market share across all sites of service. Similarly, other nonradiologist providers (ED providers) are now performing more TTE in the ED than cardiologists, likely due to the growing adoption of point-of-care US (7).
Following the combined effects of the Deficit Reduction Act of 2005 and code bundling in echocardiography in 2009 that decreased reimbursements by 22%, there was a shift of echocardiography from the office to the HOPD (8–10). The reasons for this shift during this time are multifactorial: (a) many cardiologist offices consolidated their practices with hospital networks, shifting imaging studies that would have been performed in the office to the HOPD, (b) increased utilization of electronic medical records, allowing for easier transmission of health information and imaging examinations, decreasing the incentive for cardiologists to perform in-office imaging, and (c) decreased reimbursements, making in-office imaging financially untenable. Since that time, we showed that in-office TTE rates have plateaued, but TTE rates performed in the HOPD continue to increase (Fig 1). Although bundling events intend to reduce overall Medicare payments, this may increase overall expenditures if they merely shift care into higher-cost facilities, such as the HOPD.
Prior work has suggested that in-office imaging may result in increased utilization, possibly driven by lucrative reimbursement incentives (1,11–14). Petersen et al found that in 2015, the noninvasive cardiac imaging rates in the United States were 3.1 times higher than in England, dominated by a higher rate of MPI in the United States (15); this difference is presumed to be due to differences between the fee-for-service and salary models of the United States and England, respectively. Code bundling in 2010 resulted in a decline in in-office MPI by nonradiologist providers, suggesting that many of these imaging studies may have not been medically necessary (16); despite this change, MPI utilization remains much higher than cCTA, a diagnostic study that has been shown to have as much or even greater utility than MPI in at least several clinical trials (2,17). Although MPI rates continue to decline, there has been a smaller, nonproportional growth in cCTA (Fig 3 vs Fig 5). Because CT equipment is cumbersome to own and maintain, cCTA may not be profitable in the office setting when the equipment is used exclusively for cardiac imaging. The issues of equipment expense and maintenance present a likely explanation as to why radiologists have absorbed much of the growing demand for in-office cCTA. In addition, cardiologists may be less inclined to adopt cCTA because they receive less training than radiologists on the management of incidental findings, such as lung nodules. However, the discrepancy between the relatively slow growth of in-office cCTA compared with the decreased utilization of MPI in our study implies that higher MPI utilization in the past likely represented overutilization (16).
Before 2007, technical claim reimbursements may have partially incentivized clinicians to perform advanced diagnostic imaging studies in the office setting, primarily MRI. However, the Deficit Reduction Act decreased reimbursements for many MRI and CT examinations, eliminating the reimbursement gap between the office and HOPD, a change that reduced the in-office imaging incentive (16,18,19). cMRI rates continue to grow, although substantial volumes are not present in the Medicare population (Fig 4). This slow growth is partly due to the limited indications for cMRI compounded by the inherent difficulties in obtaining a high-quality diagnostic examination. Similar to our previous discussion regarding cCTA, marginal reimbursement rates also make office-based MRI less tenable for many cardiologists. Furthermore, lesser familiarity with cMRI by cardiologists than other modalities may also partially explain the relatively slow adoption rate. cMRI rates are higher for cardiologists in the HOPD, although both specialties’ utilization is low, with a recent study showing that less than 1% of radiologists and 0.2% of cardiologists perform cMRI (20).
The continued growth of cPET in cardiologist offices is distinct because it is the only in-office imaging modality that has continued to grow over this time and has nearly tripled in volume in cardiology offices while utilization has remained unchanged for radiologists. Many factors likely underpin this observation, which relate to shifting from SPECT to cPET: (a) technological advances in cPET have made this modality superior to cardiac SPECT, with greater specificity and sensitivity for detecting coronary artery disease (21), (b) the rubidium 82 (82Rb) radionuclide used in cPET is more office-friendly than the often used thallium 201 (201Tl) agent, because 82Rb can be created in a generator whereas 201Tl is created in a cyclotron, (c) cPET is less subject to imaging artifacts seen in SPECT, such as attenuation artifacts, and cPET has a higher spatial resolution, (d) cPET studies are much shorter than SPECT, increasing patient throughput, and (e) cPET results in lower radiation dose to the patient compared with SPECT and cCTA (22,23). Furthermore, given the similarities between cPET and SPECT, it is reasonable for cardiologists to choose to upgrade to cPET over less familiar competing imaging studies such as cCTA or cMRI. It should be noted that there is a strong financial incentive to convert MPI studies to cPET, which are reimbursed at a higher rate. The Centers for Medicare & Medicaid Services recently had their sights set on reducing cPET technical claim reimbursements, but this decision has been delayed (24). Because radiologist cPET claims have remained nearly constant over the period of our study (Fig 6), the growth of cPET in cardiologists’ offices suggests a shift from in-office MPI to in-office cPET within cardiology offices. The observation that MPI performed by cardiologists has not continued to grow in the HOPD since 2015 (Fig 5), while cPET volumes have assumed an accelerated growth rate over this time (Fig 6), further suggests a conversion from cardiologist office MPI to cPET. Although the trends demonstrated for MPI and cPET suggest a shifting referral pattern, the methods used in this study do not provide definitive conclusions regarding the importance of financial incentives. At this point, the future of in-office cPET reimbursements is still uncertain because the Centers for Medicare & Medicaid Services has yet to make any further determinations for future code bundling or reimbursement cuts. These future determinations will be essential for both cardiologists and nuclear medicine specialists and will also affect radiologists as changes that may disincentivize in-office cPET are likely to influence the utilization of other modalities.
This study had several notable limitations. First, the PSPS file does not contain information to evaluate the appropriateness for any cardiac imaging examination. However, because decreased in-office utilization has led to an overall decrease in imaging rates rather than an equal increase in other locations, the utilization data suggest that at least some imaging studies previously performed in office settings were not medically necessary. Second, some cardiologists and radiologists may be part of a multispecialty practice and were therefore excluded from the analysis, resulting in a slight underestimation of each specialty’s utilization rates. Finally, the PSPS only captures information on Medicare Part B beneficiaries, resulting in a skewed view of overall cardiac imaging. For instance, congenital cardiac anomalies are frequently diagnosed with echocardiography or cMRI, but pediatric patients are not captured in the PSPS files. Nonetheless, the large number of patients recorded in the PSPS data of more than 45 million beneficiaries suggests that the trends we reported are essential determinants of medical imaging expenditures (5).
In conclusion, cardiologists have performed the bulk of in-office cardiac imaging over the years, but we are now witnessing declining MPI utilization with more slowly rising rates of cCTA, cMRI, and cPET. The growth in cCTA and cMRI has been shared by cardiologists and radiologists and represents a growing opportunity for interdisciplinary collaboration in cardiac imaging. Although MPI rates in cardiologist offices have dramatically decreased, only a minority of these studies have shifted to the HOPD, suggesting that many of these studies have represented overutilization of a test that was not medically necessary. In contrast to the decreased in-office utilization of most cardiac imaging modalities by cardiologists, the rates of in-office and HOPD cPET nearly tripled from 2010 to 2019, likely related to a combination of technological advances and financial incentives. Rather than eliminating in-office imaging, reduced reimbursements, code bundling, and technological advances have shifted the utilization of cardiac imaging from one modality to another. Both radiologists and cardiologists have vested interests in increasing referrals for cPET, although this pattern may change with reductions for cPET reimbursements in the future.
Authors declared no funding for this work.
Disclosures of Conflicts of Interest: R.A.R. disclosed no relevant relationships. E.J.H. disclosed no relevant relationships. V.M.R. former board member of RSNA.
Abbreviations:
- cCTA
- coronary CT angiography
- cMRI
- cardiac MRI
- cPET
- cardiac PET
- ED
- emergency department
- HOPD
- hospital outpatient department
- MPI
- myocardial perfusion imaging
- PSPS
- Physician/Supplier Procedure Summary
- SE
- stress echocardiography
- TEE
- transesophageal echocardiography
- TTE
- transthoracic echocardiography
References
- 1. Kamel SI , Intenzo CM , Parker L , Rao V , Levin DC . Recent trends suggest possible inappropriate utilization of myocardial perfusion imaging . J Am Coll Radiol 2019. ; 16 ( 8 ): 1013 – 1017 . [DOI] [PubMed] [Google Scholar]
- 2. Levin DC , Parker L , Halpern EJ , Rao VM . Recent trends in imaging for suspected coronary artery disease: what is the best approach? J Am Coll Radiol 2016. ; 13 ( 4 ): 381 – 386 . [DOI] [PubMed] [Google Scholar]
- 3. Ohira H , Mc Ardle B , Cocker MS , deKemp RA , Dasilva JN , Beanlands RS . Current and future clinical applications of cardiac positron emission tomography . Circ J 2013. ; 77 ( 4 ): 836 – 848 . [DOI] [PubMed] [Google Scholar]
- 4. Physician Supplier Procedure Summary . Centers for Medicare and Medicaid; . https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Physician-Supplier-Procedure-Summary. Published 2019. Accessed September 27, 2020 . [Google Scholar]
- 5. Medicare Enrollment . Centers for Medicare & Medicaid Services Program Statistics; . https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/2017/2017_Enrollment. Published 2020. Accessed March 30, 2020 . [Google Scholar]
- 6. Levin DC , Parker L , Halpern EJ , Rao VM . Coronary CT angiography: reversal of earlier utilization trends . J Am Coll Radiol 2019. ; 16 ( 2 ): 147 – 155 . [DOI] [PubMed] [Google Scholar]
- 7. Birch MS , Marin JR , Liu RB , Hall J , Hall MK . Trends in Diagnostic Point-of-Care Ultrasonography Reimbursement for Medicare Beneficiaries Among the US Emergency Medicine Workforce, 2012 to 2016 . Ann Emerg Med 2020. ; 76 ( 5 ): 609 – 614 . [DOI] [PubMed] [Google Scholar]
- 8. Levin DC , Parker L , Halpern EJ , Rao VM . The diversion of outpatient echocardiography from private offices to higher cost hospital facilities: an unanticipated effect of code bundling . J Am Coll Radiol 2014. ; 11 ( 5 ): 477 – 480 . [DOI] [PubMed] [Google Scholar]
- 9. Moser JW . The deficit reduction act of 2005: policy, politics, and impact on radiologists . J Am Coll Radiol 2006. ; 3 ( 10 ): 744 – 750 . [DOI] [PubMed] [Google Scholar]
- 10. Levin DC , Rao VM , Parker L , Frangos AJ , Sunshine JH . Bending the curve: the recent marked slowdown in growth of noninvasive diagnostic imaging . AJR Am J Roentgenol 2011. ; 196 ( 1 ): W25 – W29 . [DOI] [PubMed] [Google Scholar]
- 11. Levin DC , Rao VM . The effect of self-referral on utilization of advanced diagnostic imaging . AJR Am J Roentgenol 2011. ; 196 ( 4 ): 848 – 852 . [DOI] [PubMed] [Google Scholar]
- 12. Hillman BJ , Goldsmith J . Imaging: the self-referral boom and the ongoing search for effective policies to contain it . Health Aff (Millwood) 2010. ; 29 ( 12 ): 2231 – 2236 . [DOI] [PubMed] [Google Scholar]
- 13. Hughes DR , Bhargavan M , Sunshine JH . Imaging self-referral associated with higher costs and limited impact on duration of illness . Health Aff (Millwood) 2010. ; 29 ( 12 ): 2244 – 2251 . [DOI] [PubMed] [Google Scholar]
- 14. Degnan AJ , Yi PH , Kim N , Swietlik J , Huh E , Nguyen JC . Diagnostic and interventional imaging services are significant sources of medicare revenue for highly reimbursed nonradiologist providers . Curr Probl Diagn Radiol 2020. ; 49 ( 1 ): 17 – 22 . [DOI] [PubMed] [Google Scholar]
- 15. Petersen SE , Friebel R , Ferrari V , et al . Recent Trends and Potential Drivers of Non-invasive Cardiovascular Imaging Use in the United States of America and England . Front Cardiovasc Med 2021. ; 7 617771 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Levin DC , Parker L , Rao VM . The Percent Share of All Medicare Payments to Physicians That Is Attributable to Noninvasive Diagnostic Imaging . J Am Coll Radiol 2018. ; 15 ( 5 ): 721 – 725 . [DOI] [PubMed] [Google Scholar]
- 17. Hulten EA , Carbonaro S , Petrillo SP , Mitchell JD , Villines TC . Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis . J Am Coll Cardiol 2011. ; 57 ( 10 ): 1237 – 1247 . [DOI] [PubMed] [Google Scholar]
- 18. Levin DC , Rao VM , Parker L , Frangos AJ . The disproportionate effects of the Deficit Reduction Act of 2005 on radiologists’ private office MRI and CT practices compared with those of other physicians . J Am Coll Radiol 2009. ; 6 ( 9 ): 620 – 625 . [DOI] [PubMed] [Google Scholar]
- 19. Levy F , Rosen MP . How radiologists are paid: an economic history, part IV: end of the bubble . J Am Coll Radiol 2020. ; 17 ( 9 ): 1080 – 1085 . [DOI] [PubMed] [Google Scholar]
- 20. Goldfarb JW , Weber J . Trends in Cardiovascular MRI and CT in the U.S. Medicare Population from 2012 to 2017 . Radiol Cardiothorac Imaging 2021. ; 3 ( 1 ): e200112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Danad I , Raijmakers PG , Driessen RS , et al . Comparison of coronary CT angiography, SPECT, PET, and hybrid imaging for diagnosis of ischemic heart disease determined by fractional flow reserve . JAMA Cardiol 2017. ; 2 ( 10 ): 1100 – 1107 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Klein R , Celiker-Guler E , Rotstein BH , deKemp RA . PET and SPECT tracers for myocardial perfusion imaging . Semin Nucl Med 2020. ; 50 ( 3 ): 208 – 218 . [DOI] [PubMed] [Google Scholar]
- 23. Lu M , Wang S , Sirajuddin A , Arai AE , Zhao S . Dynamic stress computed tomography myocardial perfusion for detecting myocardial ischemia: A systematic review and meta-analysis . Int J Cardiol 2018. ; 258 ( 325 ): 331 . [DOI] [PubMed] [Google Scholar]
- 24. Thompson RC . Cardiac PET reimbursement policy: Success when we come together . J Nucl Cardiol 2020. ; 27 ( 2 ): 345 – 347 . [DOI] [PubMed] [Google Scholar]