Abstract
Background:
During the COVID-19 pandemic of Spring 2020, Belfast City Hospital functioned as Belfast’s Nightingale facility. Evidence published during this time focused mainly on the acute management of the condition. Guidance on follow up and long-term management for patients recovering from COVID-19 was sparse. A specialist COVID-19 follow up service was devised in Belfast City Hospital led by a respiratory physician with physiotherapy and psychology input.
Methods:
Data was collected on all patients admitted to Belfast Nightingale unit. Patients admitted to Intensive Care at any stage in their admission were followed up separately by Intensive Care. Initial consultation was via telephone call for all eligible patients six weeks post discharge, followed by face-to-face consultation for those with symptoms at next available appointment, and a further face-to-face consultation at twelve weeks post hospital discharge. Patients were seen by respiratory physician, physiotherapy and psychology at each appointment. All patients who had initial changes on chest radiograph had 12 week follow up radiograph requested as per British Thoracic Society guidelines.
Results:
29 patients were followed up after hospitalisation with COVID-19. Of these, 10 were brought for face-to-face consultations. Patients at clinic were all functionally independent with a median Medical Research Council dyspnoea score of 2 and a subjective assessment of their current health of median 50, on a visual analogue scale 0-100. Fatigue was common with all patients. Depression, anxiety and post-traumatic stress disorder were all reported from psychological review. Chest radiograph showed signs of improvement in 100% of clinic attendees. 90% of patients seen in clinic had normal or chronic obstructive patterns on spirometry, with one patient having a reduced transfer factor.
Conclusion:
Majority of patients did not require face-to-face review and were recovering well. Of the 10 patients seen in the respiratory led clinic, the main issues reported were fatigue and psychological issues. Respiratory symptoms were significantly improving in 9 out of the 10 patients seen. All patients have been introduced to psychology service whilst at clinic and will continue to receive necessary support.
Introduction
At the time of writing, there have been 33,722,075 confirmed cases of infection with SARS-CoV-2 (severe acute respiratory syndrome – coronavirus - 2), otherwise referred to as COVID-19, worldwide1, with 11,952 of these in Northern Ireland2. While a lot of focus has been on logistical and clinical management of the pandemic, there has been little guidance on follow up of patients with COVID-19 after they have been discharged from hospital.
Given the extent of respiratory involvement during the peak of the illness, a clear concern lay around the potential for chronic respiratory illness as a result. The clinical severity across those infected with the SARS-CoV-2 virus was broad, ranging from those who remained asymptomatic to those who required critical care support for multi-organ failure. Due to this, there will also be a range of psychological and rehabilitation needs following discharge from hospital. This greatly differs from typical respiratory discharges and so a new follow up service was developed specifically for this patient cohort.
During the COVID-19 pandemic, Belfast City Hospital (BCH) was restructured to function as Belfast’s Nightingale Hospital. This was required for a 7 week period over April – May 2020. Each patient initially presented to another hospital within the Belfast Health and Social Care Trust, where they had a confirmed positive SARS-CoV-2 nasopharyngeal and / or oral swab, and were transferred to the Nightingale facility. In total, 113 patients were admitted under the Nightingale Medical team.
Methods
A database was compiled and maintained on all patients admitted to the Nightingale facility. Data was collected on patient demographics, smoking history, co-morbidities, clinical frailty score3, ventilation requirements, need for renal replacement therapy, and incidence of delirium and mortality.
Conference calls facilitated discussion between the respiratory, intensive care, psychology and physiotherapy departments across the trust to devise a structured approach for the COVID-19 follow up clinic. The six week follow up approach was designed across respiratory and intensive care to facilitate appropriate care for all patients, allow comparisons of outcomes and to enable safe transfer of care from intensive care to respiratory if required following the initial follow up period. Patients admitted to intensive care at any stage in their admission were followed up by the intensive care team for 12 weeks following discharge and any patients not admitted to intensive care were followed up by the respiratory team. This article focuses on the initial 12 week respiratory follow up service. Assessments were carried out virtually with a holistic approach to cover not only medical needs, but also addressing need for psychological and physical rehabilitation requirements.
The first step of follow up consisted of a telephone call with screening questions to assess patients and determine the need for a subsequent face-to-face consultation at post COVID-19 follow up clinic. We aimed to complete phone calls by six weeks following hospital discharge.
Any patient requiring critical care support on Intensive Care Unit during their admission was contacted by an intensive care physician for their 6 week virtual review. Patients who had not required intensive care were contacted by a member of the respiratory team at 6 weeks. Following Electronic Care Record (ECR) review, patients were excluded if aged 90 years or older, or if they had a clinical frailty score of greater than5. Excluded patients’ notes were then passed to our respiratory specialist nurse to review and assess if any additional support would be required. Asymptomatic incidental presentations with normal chest radiograph at presentation were also excluded.
A proforma was drawn up for the phone call to ensure key questions were asked and phone calls all made by a member of the respiratory team.
Following the telephone discussion, outcome options were clinic appointment arranged or no follow up required. If the patient reported persisting symptoms from any section of telephone screen, they were offered a clinic appointment. If, however, they were recovering well with no symptoms but had changes on chest x-ray (CXR) during admission, then as per British Thoracic Society (BTS) guidelines, they were offered a 12 week follow up CXR. For the patients with no lasting symptoms and no CXR changes during admission, no follow up was arranged4.
For those requiring face-to-face respiratory consultation, they were invited to a multidisciplinary post COVID-19 clinic where they had follow up CXR, lung function tests, ECG, blood tests to include full blood count, kidney function and NT-proBNP. Each patient was assessed by respiratory team, physiotherapy and psychology. Degree of breathlessness was measured using the Medical Research Council (MRC) Breathlessness Scale5. Physiotherapy assessment consisted of the Fatigue Impact Scale (FIS)6; The QOL EQ5DL7, a quality of life questionnaire; The Duke Activity Status Index (DASI)8; Post-COVID-19 Functional Status (PCFS) Scale9 and the 30 second sit to stand test in which the heart rate and oxygen saturation was taken pre- and post-testing. The EQ-59 score includes a visual analogue scale by which patients rated their perceived current health compared to their best score, on a 0-100 scale.
Questionnaires were sent to patients to complete prior to clinic attendance to allow calculation of various symptomatology scoring systems. Psychology questionnaires sent included the PHQ9 score for depression10, the 7-item Generalised Anxiety Disorder Scale GAD-7 for anxiety11 and the Posttraumatic Stress Disorder (PTSD) Checklist PCL-5 score12.
Results
This patient cohort totalled 113 patients, comprised of 69 male patients (61%) and 44 female patients (39%), with a median age of 66 years(IQR 53.5 – 78). 98 patients (86%) were of white Northern Irish ethnicity, with the remaining 14% comprising 7 different ethnicities. Only 2 patients were current smokers, 31 ex-smokers and 61 patients had never smoked. Smoking status was unknown in 19 cases. 79 patients (70%) were direct admissions from home via an Emergency Department,13 (11%) were admitted from 24-hour care facilities and the remaining 21 (19%) were transferred from other hospitals following positive swabs for SARS-CoV-2. The median length of hospital stay was 10 days (IQR 5 – 21).
Table 1. Patient demographics.
| Total (n=113) | ICU | Non-ICU | |
|---|---|---|---|
| Age (years) | 66 (53.5 – 78) | 55 (49 – 63) | 74 (64 – 86) |
| Sex | |||
| Male | 69 (61.06%) | 33 (80.49%) | 36 (50%) |
| Female | 44 (38.93%) | 8 (19.51%) | 36 (50%) |
| Smoking | |||
| Current smoker | 2 (1.77%) | 0 (0%) | 2 (2.78%) |
| Ex-smoker | 31 (27.43%) | 11 (26.83%) | 20 (27.78%) |
| Never smoker | 61 (53.98%) | 21 (51.22%) | 40 (55.56%) |
| Unknown | 19 (16.82%) | 9 (21.95%) | 10 (13.88%) |
| Length of stay | 10 (5 – 21) | 22 (12 – 39) | 7 (3 – 12.5) |
Data are n (%), or median (IQR)
Out of a total of 113 patients admitted to the Nightingale facility at BCH, 29 met eligibility criteria for follow up under respiratory team. We had a 19% mortality rate, excluding 21 patients from follow up. 36 patients were admitted to intensive care and had initial follow up with the intensive care team. Frail, elderly (>90years) patients (n=24) were not reassessed at clinic but were offered a follow up CXR if changes on initial scan. Any incidental cases of positive SARS-CoV-2 swabs who were asymptomatic with normal CXR were not contacted for follow up (n=5).
We aimed to complete initial telephone call for these 29 patients within 6 weeks of discharge. We were able to contact 28 (97%) patients (Figure 1). The median time from hospital discharge to initial telephone conversation was 42 days and median time to initial face-to-face consultation 56 days.
Figure 1.
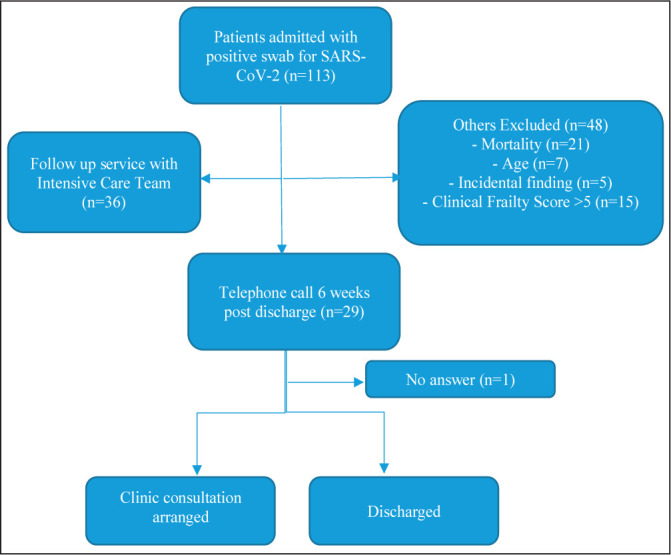
Flowchart showing COVID-19 follow-up pathway
Of the 28 patients contacted for virtual respiratory telephone review, 9 patients (32%) reported persisting breathlessness,4 (14%), ongoing cough and 3 (11%) had chest pains. 12 patients (43%) were off their baseline mobility with reduced exercise tolerance.7 patients (25%) reported low mood since discharge from hospital,5(18%) reported anxiety or panic attacks and 5(18%) reported a disrupted sleep pattern or nightmares.2 patients had new cognitive decline – 1 patient had new memory impairment and 1 patient, currently a nursing home resident, had new fluctuating mild confusion.
In total, 12 patients were identified as requiring face-to-face consultation. 2 patients remain inpatients in a rehabilitation facility and so have had their initial face-to-face consultation arranged for 12weeks post discharge so a total of 10 patients were reviewed in the multi-disciplinary six week follow up clinic. 16 patients are listed for a 12 week CXR. 7 patients reported good recovery and have not required follow up at this time.
Of patients brought to clinic, 40% were obese with a median BMI of 30.2 (27.2 – 33.55kg/m2). The median dyspnoea score was 2.
All patients who attended clinic were functionally independent with no physical limitations to strength or balance. However, fatigue was common with all patients seen and this was reflected in the FIS questionnaire scores. Patients reported a fatigue impact score median 65 out of total 160 and DASI score median 21.4 points METS 5.38, demonstrating moderate impairment of functional status. Of the patients who were seen on a second review and re-tested, the FIS scores had shown an improvement of 19% and the DASI functional impact score showed an improvement of 54%. Physiotherapy assessment included 30 second sit to stand with patients managing a median result of 13 in this time frame. Post-COVID-19 Functional Status (PCFS) Scale showed an improvement in the second review of 37.5%. EQ-5D-5L Visual Analogue Scale showed an improvement in the second review of 27.2%.
Psychological assessment showed overall moderate severity depression with median PHQ9 score of 10 (4 -15) and mild severity anxiety with GAD7 median 7 (2 -11). The median PCL-5 score, the screening tool used for PTSD, had a median score of 28.5 (3 – 33.75), which would not meet criteria for PTSD clinical caseness. Cognitive assessment was completed using the Montreal Cognitive Assessment (MoCA) tool in 4 patients with a median result of 24.5 (23 – 26), which is in normal range. However, it is important to note that there was considerable variation in responses to the psychological questionnaires. On review of the data there were 3 clear outliers, which consistently differed significantly across all questionnaire responses thus deflating the other scores.
Patients graded their current health on day of clinic as a median of 65 (56.25 – 71.25) on a virtual analogue scale of 0-100, 100 being their best health.
At presentation, 111/113 (98%) patients had a CXR. Of these, 66 (59%) showed changes typically seen with SARS-CoV-2, 25 (23%) had a radiograph showing changes unlikely to be due to SARS-CoV-2 infection and 20 (18%) were normal. At this stage, we have repeated CXRs in patients brought for face-to-face consultation, however the remainder of patients with abnormal CXRs on admission will have their CXR arranged at twelve weeks post discharge. CXRs showed significant improvement by time of clinic review in 100% (n=10).
10 patients had spirometry and transfer factor measured. These were in normal range for 6 patients. Out of remaining four, three patients had obstructive spirometry with known history of chronic obstructive respiratory conditions and one patient had new reduced transfer factor. This patient has had further investigations and follow up arranged with the respiratory team.
ECG was reviewed with no abnormalities detected, in sinus rhythm for eight of the ten patients seen in clinic and was not performed in the remaining two patients. NT-ProBNP blood test was in normal range for seven patients, high in one patient and test not performed for two patients.
Discussion
We have reviewed the design and outcomes of the first stage of ongoing follow up in the care for patients discharged from hospital following infection with SARS-CoV-2.
Data will continue to be collected on lasting physical and psychological symptoms, chest radiography and lung function following hospitalisation. Patients who were not discharged following 6 week face-to-face review will be seen again at the twelve week post discharge point, and patients assessed by intensive care teams at six weeks have been invited for a face-to-face review.
At this early stage, it is good to see that 54% of patients did not require face-to-face review and report they are recovering well from COVID-19. Of the 10 patients seen in the respiratory-led clinic, the main issues reported were fatigue and psychological issues. Respiratory symptoms were significantly improving in 9 out of the 10 patients seen. All patients have been introduced to the psychology service whilst at clinic and will continue to receive necessary support.
Patients presented with expected and normative distress given both their personal experiences and the ongoing wider societal perceived risks and ongoing restrictions and concerns. Many reported being very grateful for having survived and for the care they received and potentially this may have reduced initial reporting of psychological symptoms. All those seen at clinic reported feeling very reassured in having the opportunity to discuss and normalise their feelings and some preliminary, lower level psychological advice was given. All will be reviewed at 12 weeks.
There was no physiotherapy follow up needed for any patients seen with most given advice with pacing their activities to help with fatigue with home exercises programs as needed. The participants were shown the COVIDcare NI APP which has information and guidance on recovering from COVID-19 amongst other advice.
This approach is in keeping with BTS guidance for early integration with ICU follow up and the requirements of a ‘post-COVID-19’ holistic assessment, however we did decide to facilitate earlier follow up for all patients than the suggested 12 weeks4. In those still symptomatic, it offered early opportunity for referral to appropriate services. Patients were reassured knowing they weren’t alone in the problems they were facing and that support was available. We feel this will affect long term outcomes and overall patient satisfaction. We have now developed a patient satisfaction questionnaire which we will email to patients following 12 week review to address if they found this helpful.
We continue to run separate intensive care and respiratory follow up clinics until 12 weeks post discharge with frequent communication between teams to address any issues encountered and update on progress. Following the 12 week review, a follow up pathway has been designed for further follow up needs. If symptoms are improving as expected for a patient following a severe viral pneumonia, no evidence of lasting CXR changes and/or physiological impairment, they will be discharged from medical follow up. Other members of the multidisciplinary team will arrange follow up as required. If the patient has an abnormal CXR or physiological impairment, defined as abnormal lung function tests, raised NT-ProBNP, or symptoms out of keeping with resolving pneumonia, they will have further investigations arranged based on suspected diagnosis. Based on investigation results, patients will be triaged by an allocated respiratory/intensive care consultant to follow up. New interstitial lung disease cases will be seen at a respiratory physician led clinic and follow up of chronic thromboembolic disease / pulmonary hypertension at a pulmonary vascular disease clinic.
The COVID-19 outbreak is posing considerable challenges to healthcare systems worldwide. Throughout the pandemic, understanding of the acute phase of the disease has rapidly expanded, however, there is still little known about the long-term consequences following clinical remission. Information on the long-term effects of other coronavirus diseases is limited, and we still do not know to what extent this data can be applied to COVID-1913 14.
It is possible that the COVID-19 pandemic may result in ongoing psychological distress for many survivors with the potential for some to develop significant mental health issues. Post trauma symptoms and, in the longer term, development of PTSD, can be a common pathological outcome of a wide variety of traumatic events, from natural disasters to road traffic accidents15. Core symptoms of PTSD, as defined by the Diagnostic and Statistics of Mental Disorders, the fifth edition (DSM-5) of the American Psychiatric Association, include persistent avoidance of stimuli, persistent intrusion symptoms, negative alterations in mood or cognition, and marked alterations in arousal and reactivity, all associated with the experienced traumatic event16. PTSD results in clinically significant distress to the individual, as well as impairment in normal functioning. Epidemiological data indicate that the median time for PTSD to recover is 36 months for individuals who sought help for any mental health problem and about 64 months for individuals who never sought help for a mental health problem17.
Infectious disease epidemics result in a psychological trauma. While most of these mental health problems will fade out after the epidemic, symptoms of PTSD may last for a prolonged time and result in serious disability. Issues such as a pre-morbid history of mental health difficulties, physical morbidity sequelae and wider life impacts (such as impact on employment) and admission to ICU can all be contributing factors in ongoing distress. A systematic review of psychological consequences of infectious disease outbreak indicates that the average prevalence of PTSD among health professionals was approximately 21%18. A study of the long-term psychiatric morbidities among SARS survivors revealed that PTSD was the most prevalent longterm psychiatric condition. 47.8% of SARS patients were diagnosed with PTSD, and 25.5% of these patients continued to meet PTSD criteria at 30 months post-SARS19.
An already large and still increasing number of people have been exposed to COVID-19. It remains a cause of increased social anxiety, with high visibility in terms of media coverage and strong public health messaging, some of which is promoting increased vigilance and increased safety behaviours (which post traumatic event could be interpreted as trauma reactions). It is very important, therefore, to gain an understanding of the ongoing natural progression of expected psychological distress, normative psychological impact and the longer term likelihood of developing PTSD and other mental health issues. This will allow better understanding of the workforce needs and service developments needed to best support individuals and families during and in the aftermath of the pandemic.
Footnotes
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.WHO Coronavirus Disease (COVID-19) Dashboard, [Online] [Accessed 01 10 20]. Available: https://covid19.who.int/
- 2.Department of Health COVID-19 Testing Overview [Online] [Accessed 01 10 20]. Available: https://app.powerbi.com/view?r=eyJrIjoiZGYxNjYzNmUtOTlmZS00ODAxLWE1YTEtMjA0NjZhMzlmN2JmIiwidCI6IjljOWEzMGRlLWQ4ZDctNGFhNC05NjAwLTRiZTc2MjVmZjZjNSIsImMiOjh9.
- 3.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.BTS Guidance on Respiratory Follow Up of Patients with a Clinico-Radiological Diagnosis of COVID-19 Pneumonia v1.2 11 5 2020. [Online] Available: https://www.brit-thoracic.org.uk/document-library/quality-improvement/covid-19/resp-follow-up-guidance-post-covid-pneumonia/
- 5.MRC Dyspnoea Scale. [last accessed 20/06/20]. Available at: https://mrc.ukri.org/research/facilities-and-resources-for-researchers/mrc-scales/mrc-dyspnoea-scale-mrc-breathlessness-scale/
- 6.Learmonth YC, Dlugonski D, Pilutti LA, Sandroff BM, Klaren R, Motl RW. Psychometric properties of the Fatigue Severity Scale and the Modified Fatigue Impact Scale. J Neurol Sci. 2013;331(1-2):102–107. doi: 10.1016/j.jns.2013.05.023. [DOI] [PubMed] [Google Scholar]
- 7.Balestroni G, Bertolotti G. L’EuroQol-5D (EQ-5D): uno strumento per la misura della qualita della vita [EuroQol-5D (EQ-5D): an instrument for measuring quality of life] Monaldi Arch Chest Dis. 2012;78(3):155–159. doi: 10.4081/monaldi.2012.121. [DOI] [PubMed] [Google Scholar]
- 8.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64(10):651–4. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 9.Klok FA, Boon GJAM, Barco S, Endres M, Geelhoed JJM, Knauss S, et al. The Post-COVID-19 Functional Status (PCFS) Scale: a tool to measure functional status over time after COVID-19. Eur Res J. 2020 Jul 2;56(1):2001494. doi: 10.1183/13993003.01494-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levis B, Benedetti A, Thombs BD, DEPRESsion Screening Data (DEPRESSD) Collaboration Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis [published correction appears in BMJ. 2019 Apr 12;365:l1781] BMJ. 2019;365:l1476. doi: 10.1136/bmj.l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, Herzberg PY. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 12.Blevins C, Weathers F, Davis M, Witte T, Domino J. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 13.Wu X, Dong D, Ma D. Thin-Section Computed Tomography Manifestations During Convalescence and Long-Term Follow-Up of Patients with Severe Acute Respiratory Syndrome (SARS) Med Sci Monit. 2016;22:2793–9. doi: 10.12659/MSM.896985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou X, Li Y, Li T, Zhang W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect. 2020;26(7):957–959. doi: 10.1016/j.cmi.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shalev AY, Marmar CR. Posttraumatic stress disorder. In: Sadock BJ, Sadock AV, Ruiz, editors. Kaplan and Sadock’s comprehensive textbook of psychiatry. 10th ed. Philadelphia: Wolters Kluwer; 2017. [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and statistical manual of mental disorder. 5th edition DSM-5. Washington: American Psychiatric Publishing; 2013. [Google Scholar]
- 17.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vyas KJ, Delaney EM, Webb-Murphy JA, Johnston SL. Psychological impact of deploying in support of the U.S. response to Ebola: a systematic review and meta-analysis of past outbreaks. Mil Med. 2016;181(11):1515–31. doi: 10.7205/MILMED-D-15-00473. [DOI] [PubMed] [Google Scholar]
- 19.Mak IWC, Chu CM, Pan PC, Yiu MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. 2009;31(4):318–26. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


