Abstract
Introduction:
Serum cancer antigen 125(SeCA125) has been reported to be increased in patients with heart failure and correlate with both extracellular water (ECW) overload and poor prognosis. Ultrafiltration failure and ECW overload are a major cause of peritoneal dialysis (PD) technique failure. We wished to determine whether SeCA125 could also be a marker of volume status in PD patients.
Methods:
We contemporaneously measured SeCA125, serum N terminal brain natriuretic peptide (NTproBNP) and ECW by bioimpedance in adult PD patients attending for outpatient assessment of peritoneal membrane function.
Results:
The median SeCA125 was 19 (12–33) U/mL in 489 PD patients, 61.3% male, median age 61.5 (interquartile range 50–75) years. SeCA125 was positively associated with the ratio of ECW/total body water (TBW) (r = 0.29, p < 0.001), 4-h peritoneal dialysate to serum creatinine ratio (r = 0.23, p < 0.001), NTproBNP) (r = 0.18, p < 0.001), and age (r = 00.17, p = 0.001) and negatively with 24-h PD ultrafiltration volume (r = −0.28, p < 0.001) serum albumin (r = −0.22, p < 0.001), and echocardiographic left ventricular ejection fraction (r = −0.20, p < 0.001), but not with residual renal function or C-reactive protein. Patients with above the median SeCA125, had greater median ECW/TBW 0.403(IQR 0.394–0.410) vs 0.395(0.387–0.404), p < 0.001 and NTproBNP (6870 (IQR 1936–20096) vs 4069 (1345–12291) vs) pg/mL, p = 0.03.
Conclusion:
Heart failure studies have reported SeCA125 is a marker of ECW overload. Our retrospective analysis suggests that SeCA125 is also associated with ECW volume in PD patients. Further studies are required to determine whether serial measurements of SeCA125 trend with changes in ECW status in PD patients and can be used to aid volume assessments.
Keywords: Bioimpedance, serum CA125, extracellular water, peritoneal dialysis
Introduction
More than 200,000 patients with chronic kidney disease are treated by peritoneal dialysis (PD) world-wide. However, around 35% of PD patients transfer to haemodialysis (HD) annually and few patients remain treated by PD after 5 years.1,2 After peritonitis, technique failure is one of the commonest reasons for patients to switch to HD, and 18% of these cases are associated with ultrafiltration failure and extracellular water (ECW) overload. 2
Achieving optimal fluid balance is important for PD patients, as too little fluid removal can result in hypertension, subcutaneous and pulmonary oedema, left ventricular hypertrophy and pulmonary hypertension, 3 whereas excessive fluid removal can potentially lead to hypotension and loss of residual renal function. ECW expansion may occur as a result of increased fluid intake and ultrafiltration failure, so the use of bio-markers which track changes in ECW could potentially assist the clinician in identifying patients at risk of increasing ECW before the manifestations of ECW overload become clinically manifest.
Serum cancer antigen 125 (CA125) has been recently reported as an emerging biomarker for heart failure, with reports of SeCA125 being used to aid the clinical management of heart failure by guiding diuretic dosages, and as a prognostic marker for mortality. 4 Why CA125 increases in heart failure has not been fully elucidated. Current proposals have included increased lung water and venous congestion leads to increased secretion by pleural mesothelial cells due to increased mechanical pressure, and others have suggested that circulating inflammatory mediators and venous congestion in the skin leads to increased local mesothelial cell CA125 production. 5 We therefore wished to determine whether SeCA125 was also associated with volume status in PD patients.
Material and methods
Serum CA125 was added to our standard order set for PD patients attending for routine outpatient assessment of peritoneal membrane function in 2013, measured using an immune-assay sandwich assay (Roche Cobas, Roche diagnostics, Sussex, UK). No patient had suffered an episode of peritonitis or acute hospital admission in the three months prior to peritoneal equilibration testing (PET) using 2.0 litres 22.7 g/L dextrose. All patients had corresponding 24-h urine and peritoneal dialysate collections to calculate urea clearance (weekly Kt/V), along with standard biochemical tests including N-terminal pro-brain natriuretic peptide (NT-proBNP), and C-reactive protein (CRP). 6 ECW and total body water (TBW) were measured by multifrequency bioimpedance using multifrequency bioelectrical impedance (MFBIA) following a standardised protocol, with the peritoneal dialysate drained out and after voiding (InBody 720, Seoul, South Korea). 7 Bioimpedance equipment was regularly serviced and calibrated. Left ventricular ejection fraction was obtained from two-dimensional M-mode transthoracic echocardiograms (Philips IE33, Philips Medical Systems, Eindhoven, Netherlands).
Statistical analysis
Data normality was checked with D’Agostino and Pearson method, and groups compared with student t-test, Mann Whitney U-test, Chi square and univariate analysis by Spearman test. Results were adjusted for multiple testing and small numbers where appropriate. Results are expressed as mean ± standard deviation (SD), median and interquartile range (IQR), or percentage. Statistical analysis was performed using Statistical Package for Social Science version (IBM SPSS 24.0, Armonk, New York, USA). Statistical significance was taken at or below the 5% level.
Ethics
Our retrospective audit complied with the United Kingdom National Health Service Health Research Authority guidelines for clinical audit and service development with all patient data anonymised prior to analysis (https://www.hra.nhs.uk), and was registered with the University College London department of renal medicine.
Results
Serum CA125 was measured in 489 out of a possible 514 PD patients. The cohort comprised 61.3% male, median age 61.5 (50–75) years, with 45.1% diabetics (Table 1). The median Serum CA125 was 19 (interquartile range 12–33) U/mL (normal laboratory reference range < 35 U/mL), NT-proBNP 5033 (1504–18585) pg/mL, serum albumin 37 (33–40) g/L and C-reactive protein (CRP) 5 (2–13) mg/L (Table 1). On univariate analysis serum CA125 was positively associated with the ratio of ECW/TBW ((r = 0.29, p < 0.001), PET 4-hour peritoneal dialysate creatinine to serum creatinine ratio (r = 0.23, p < 0.001), NT-proBNP (r = 0.18, p < 0.001), and age (r = 00.17, p = 0.001), treatment with automated peritoneal dialysis cyclers with a wet day (CCPD), and the use of icodextrin dialysates, and negatively with 4-hour PET ultrafiltration volume (r = −0.28, p < 0.001), serum albumin (r = −0.22, p < 0.001), echocardiographic left ventricular ejection fraction (r = −0.20, p < 0.001), but not with residual renal function, 24-h peritoneal ultrafiltrate volume or CRP.
Table 1.
Patients divided as below and above median serum cancer antigen 125 (SeCa125).
| All N (489) | Serum Ca 125 below median (n = 238) | Serum Ca125 above median (n = 236) | p-Value | |
|---|---|---|---|---|
| Age | 62 (50–75) | 58 (49–72) | 66.5 (52.78) | 0.01 |
| Gender (male) | 295 (60.3%) | 167 (70.2%) | 120 (50.8%) | <0.001 |
| Diabetic (%) | 214/474 (45.1%) | 99 (41.6%) | 115 (48.7%) | 0.12 |
| PD modality | ||||
| APD | 102 (21.4%) | 65 (27.3%) | 33 (14.2%) | <0.001 |
| CAPD | 241 (50.5%) | 125 (52.5%) | 108 (46.4%) | |
| CCPD | 134 (28.1%) | 40 (16.8%) | 92 (39.5%) | |
| PD treatment months | 14 (3–29) | 14 (3–18) | 12 (3–29) | 0.42 |
| PET-UF volume (ml) | 250 (100–400) | 300 (200–400) | 200 (100–300) | <0.001 |
| Icodextrin used | 372 (76.1%) | 166/238 | 196/236 | <0.01 |
| 22.7g/L dextrose used | 268 (54.9%) | 135/238 | 126/235 | 0.49 |
| Weekly Kt/Vurea PD | 1.18 (0.89–1.51) | 1.23 (0.96–1.52) | 1.15 (0.80–1.51) | 0.06 |
| Weekly Kt/Vurea urine | 0.69 (0.17–1.3) | 0.63 (0.16–1.2) | 0.75 (0.20–1.47) | 0.06 |
| 24-hour peritoneal ultrafiltration (mL) | 676 (314–1073) | 676 (355–1134) | 674 (291–1003) | 0.25 |
| PET transporter status | ||||
| Slow | 37/462 (8%) | 23/227 (10.1%) | 13/222 (5.9%) | 0.04 |
| Medium | 274/462 (59.3%) | 148/227 (65.2%) | 117/222 (52.7%) | |
| Fast | 151/462 (32.7%) | 56/227 (24.7%) | 92/222 (41.4%) | |
| Haemoglobin (g/dL) | 10.9 (9.8–11.9) | 10.9 (9.9–11.9) | 10.9 (9.8–11.9) | 0.24 |
| Albumin (g/L) | 37 (33–40) | 38 (35–41) | 36 (32–39) | <0.001 |
| NT-proBNP (pg/mL) | 5032.6 (1504.3–18585.1) | 4069 (1344.7–12291.0) | 6870.0 (1936.6–20096.2) | 0.03 |
| CRP mg/L | 5 (2–13) | 5 (1–11) | 5 (2–17.5) | 0.03 |
| ECW/ TBW ratio | 0.399 (0.38–0.407) | 0.395 (0.387–0.407) | 0.403 (0.394–0.410) | <0.001 |
| LV ejection fraction | 57.0% (47.5–57.5%) | 57.0% (52.5–57.5%) | 55 (42.5–57.5%) | 0.01 |
PD: peritoneal dialysis; APD: automated peritoneal dialysis with dry day; CAPD: continuous ambulatory peritoneal dialysis; CCPD: automated peritoneal dialysis with wet day; PET: peritoneal equilibrium test; UF: ultrafiltration volume; NT-proBNP: N-terminal brain natriuretic peptide; CRP: C-reactive protein; ECW/TBW: ratio of extracellular to total body water; LV: echocardiogram left ventricular; ejection fraction.
Data reported as integer, percentage, mean ± standard deviation, median (interquartile range).
Patients were divided into 2 subgroups according to the median serum CA125 (Table 1). Patients with higher serum CA125 were more likely to be female, older, have increased ECW/TBW, NT-proBNP and CRP, be faster peritoneal transporters with lower PET ultrafiltration, and have lower echocardiograph left ventricular ejection fraction, and serum albumin. More patients with higher serum CA125 used icodextrin and were treated with CCPD. Patients with higher serum CA125cocentrations had both higher ECW/TBW ratios and NT-proBNP (Figures 1 and 2).
Figure 1.
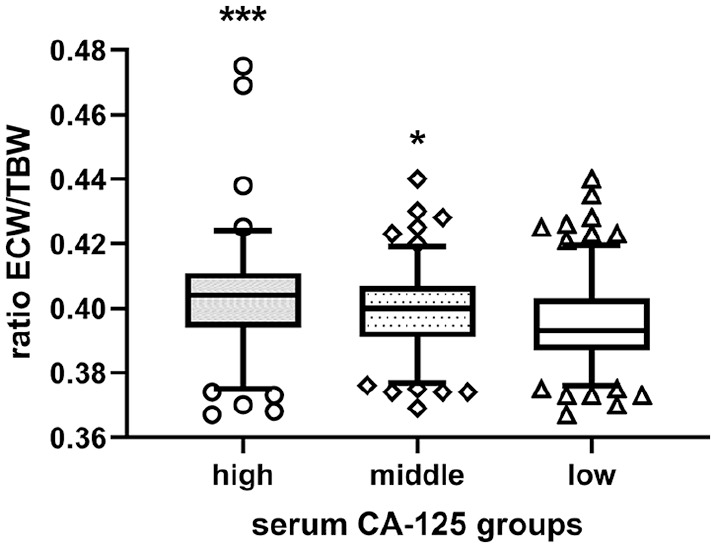
Extracellular water to total body water ratios (ECW/TBW) in peritoneal patients divided into three groups according to serum cancer antigen 125 (CA125) concentrations. Median, interquartile and 95% confidence limits box and whisker plot.
*p < 0.05, *** < 0.001 versus lowest serum CA125 tertile.
Figure 2.
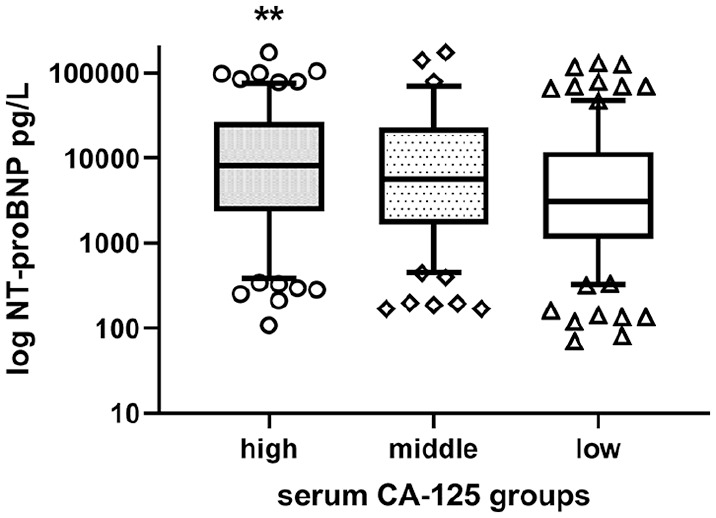
Log N terminal brain natriuretic peptide (NTproBNP) in peritoneal patients divided into three groups according to serum cancer antigen 125 (CA125) concentrations. Median, interquartile and 95% confidence limits box and whisker plot.
**p < 0.01 versus lowest serum CA125 tertile.
We then analysed data from 152 of our patients who had repeat serum CA125 measurements six months or longer apart (Table 2). Blood pressure was similar, and there were no changes in the number of classes of antihypertensive medications prescribed. Patients who had an increase in serum CA125, had an increase in NTproBNP, and ECW/TBW compared to those with no change or a decrease in serum CA125. CRP and change in CRP were not different, but there was a reduction in serum albumin in those patients who had an increase in serum CA125. On Univariate analysis the percentage change in serum CA125 was positively associated with the change in NTproBNP (Spearman rho 0.33, p < 0.0001), ECW/TBW rho 0.25 p = 0.006) and negatively with the change in serum albumin (rho −0.26, p = 0.0012). There was no association between the change in serum CA125 and either urine output or 24-h urinary creatinine clearance.
Table 2.
Peritoneal Dialysis (PD) patients with follow-up measurement of serum cancer antigen (CA125) divided into those with no increase in serum CA125 and those with an increase in serum CA125.
| No increase in CA125 | Increase in CA125 | |
|---|---|---|
| Male/female | 37/34 | 53/28 |
| Age years | 64 (56–76) | 67 (55–77) |
| Months of PD | 10 (3–25) | 13 (3–27) |
| Follow-up | 7 (6–13) | 8 (6–13) |
| Initial serum CA 125 U/mL | 27 (16–40) | 18 (12–24) |
| Urine output mL/day | 586 (306–1245) | 854 (291–1504) |
| Change in urine output mL/day | −75 (−357 to 0) | −129 (−464 to +76) |
| Mean arterial blood pressure mmHg | 101.7 (87–111.7) | 97 (89.7–106) |
| Change in blood pressure (%) | −2.2 (−15.2 to 8.3) | 0 (−9.8 to 11.5) |
| NTpro BNP pg/mL | 2027 (347–13034) | 1198 (196–8907) |
| Change in NTproBNP (%) | −4.2 (−33.1 to 5.6) | 47.9 (8.7 to 135.7)*** |
| ECW/TBW | 0.402 (0.391–0.405) | 0.402 (0.394–0.414) |
| Change in ECW/TBW | 0 (−0.007 to 0.005) | 0.004 (−0.003 to 009)** |
| Serum albumin g/L | 36 (32–39) | 38 (35–40) |
| Change in serum albumin g/L | 0 (−2 to 3) | −2 (−5 to 11)** |
| C reactive protein mg/L | 5 (2–13) | 6 (1–18) |
| Change in C reactive protein mg/L | 0 (−4 to 3) | 1 (−3 to 5) |
N terminal pro brain natriuretic peptide (NTproBNP), ratio extracellular water to total body water (ECW/TBW). Data expressed as integer or percentage, median and interquartile range.
p < 0.01, *** < 0.001 versus no increase in CA125.
Discussion
Serum CA125 has been reported to be a biomarker for heart failure and ECW overload in the cardiology field, and has prognostic value.4,8 We therefore wished to determine whether serum CA125 was similarly associated with ECW and heart failure in PD patients. Our results in a cross sectional study of more than 400 PD patients demonstrate that serum Ca125 correlates with markers of increased ECW and heart failure including ECW/ TBW, NT-proBNP, reduced left ventricular ejection fraction and faster peritoneal transport. In a smaller sub-group of around 150 patients, longitudinal changes in serum CA125 were also associated with corresponding changes in ECW/TBW and NTproBNP.
After peritonitis, failure to achieve adequate control of ECW is a major cause of PD technique failure. Unlike haemodialysis patients who attend dialysis centres 2–3 times a week, PD is a home-based treatment, and especially in the era of Covid-19, PD patients are much less frequently reviewed in face to face assessments. Therefore, clinical assessment of volume status is less frequently performed, and as such there is a clinical need to search for biomarkers which can provide guidance as to volume status. Although NT-proBNP is a biomarker of heart failure, it is cleared by the kidney, so affected by changes in residual renal function. However, we found no effect of peritoneal urea clearance or residual renal function on serum CA125. Serum CA125 has been shown to be a biomarker for heart failure, and serial measurements have been used to direct diuretic dosages. 8 Other studies in the cardiology field have reported an association between serum CA125 and echocardiographic findings. 9 It has been suggested that CA125 can be increased by inflammation, 5 and in our cross-sectional study CRP concentrations were marginally greater in patients with higher serum CA125. Although, in the follow-up cohort there was no association between the change in CA125 and CRP. Serum albumin was both lower in the cross-sectional study and fell in those who had an increase in serum CA125 in our longitudinal cohort. Although albumin may be a nutritional marker, and a negative acute phase protein, in PD patients a lower serum albumin may equally reflect volume overload and dilution. 10 As the increase in serum CA125 was associated with an increase in NTproBNP and ECW/TBW, 11 we postulate that the fall in albumin was due to an increase in volume and a dilutional effect.
Our retrospective observational report also demonstrates an association between serum CA125 and markers of increased ECW in PD patients, and as such is in keeping with reports from cardiology.4,5,8 We therefore suggest that serum CA125 be considered as an adjunct to clinical assessments and other currently used techniques including bioimpedance and cardiac bio-markers for ECW assessment and that patients with greater values may be at increased risk of ultrafiltration failure. Several authors have suggested that serial estimations of serum CA125 can be used to guide therapy in patients with heart failure. 10 Covid-19 has changed clinical practice world-wide, with a reduction in face-to-face assessments of patients, and, as such, there is a need to review and develop newer biomarkers associated with in an increased ECW, that could allow changes in PD prescription, without regular physical patient review. Further studies are required to evaluate the role of serial CA125 measurements in determining changes in ECW, and whether increasing serum CA125 concentrations can have an additional prognostic value in PD patients, alerting physicians to increasing fluid retention and thus allowing patients developing or at risk of ultrafiltration failure to timely transfer to haemodialysis.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics: Our retrospective audit complied with the United Kingdom National Health Service Health Research Authority guidelines for clinical audit and service development with all patient data anonymised prior to analysis (https://www.hra.nhs.uk),and was registered with the University College London department of renal medicine.
ORCID iD: Andrew Davenport  https://orcid.org/0000-0002-4467-6833
https://orcid.org/0000-0002-4467-6833
References
- 1. Afolalu B, Troidle L, Osayimwen O, et al. Technique failure and center size in large cohort of peritoneal dialysis patients in a defined geographic area. Perit Dial Int 2009; 29(3): 292–296. [PubMed] [Google Scholar]
- 2. Guo A, Mujais S. Patient and technique survival on peritoneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int 2003; 64(88): S3–S12. [DOI] [PubMed] [Google Scholar]
- 3. Ronco C, Rosner MH, Crepaldi C. (eds.) Peritoneal dialysis–state-of-the-art 2012. Contributions to nephrology. Vol. 178, Basel: Karger, 2012, pp.164–168. [Google Scholar]
- 4. Yoon JY, Yang DH, Cho HJ, et al. Serum levels of carbohydrate antigen 125 in combination with N-terminal pro-brain natriuretic peptide in patients with acute decompensated heart failure. Korean J Intern Med 2019; 34(4): 811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu HB, Shao K, Wang YC, et al. Research progress of CA125 and BDNF in serum of patients with acute myocardial infarction for predicting acute heart failure. Clin Hemorheol Microcirc 2020; 75(1): 99–106. [DOI] [PubMed] [Google Scholar]
- 6. Papakrivopoulou E, Lillywhite S, Davenport A. Is N-terminal probrain-type natriuretic peptide a clinically useful biomarker of volume overload in peritoneal dialysis patients? Nephrol Dial Transplant 2012; 27(1): 396–401 [DOI] [PubMed] [Google Scholar]
- 7. Davenport A. Does peritoneal dialysate affect body composition assessments using multi-frequency bioimpedance in peritoneal dialysis patients? Eur J Clin Nutr 2013; 67(2): 223–225. [DOI] [PubMed] [Google Scholar]
- 8. Llàcer P, Bayés-Genís A, Núñez J. Carbohydrate antigen 125 in heart failure. New era in the monitoring and control of treatment. Med Clin (Barc) 2019; 152(7): 266–273. [DOI] [PubMed] [Google Scholar]
- 9. Kouris NT, Zacharos ID, Kontogianni DD, et al. The significance of CA125 levels in patients with chronic congestive heart failure. Correlation with clinical and echocardiographic parameters. Eur J Heart Fail 2005; 7(2): 199–203. [DOI] [PubMed] [Google Scholar]
- 10. Jones CH, Wells L, Stoves J, et al. Can a reduction in extracellular fluid volume result in increased serum albumin in peritoneal dialysis patients? Am J Kidney Dis 2002; 39(4): 872. [DOI] [PubMed] [Google Scholar]
- 11. Davies SJ, Davenport A. The role of bioimpedance and biomarkers in helping to aid clinical decision-making of volume assessments in dialysis patients. Kidney Int 2014; 86(3): 489–496. [DOI] [PubMed] [Google Scholar]


