Abstract
Objective: To evaluate the influence of high-quality care on the psychological well-being, the postoperative complications, and patient satisfaction following a radical mastectomy. Methods: One hundred and eighteen breast cancer patients who underwent radical mastectomies from February, 2017 to May, 2019 in the Cancer Hospital of China Medical University were enrolled. Among them, 56 patients treated with regular care were included in the regular group, while the other 62 patients who underwent high-quality care were included in the high-quality group. The postoperative recoveries and complications were compared between the two groups. The visual analogue scale (VAS), the disabilities of the arm, shoulder and hand (DASH) questionnaire, the self-rating anxiety scale (SAS), the self-rating depression scale (SDS), the quality of life (QOL) assessment scale, and a patient satisfaction questionnaire were used to evaluate the degrees of pain, the upper limb recovery, the negative emotions, the QOL, the patient satisfaction and the two-year survival rate, respectively. Results: The ambulation times, the regression times of upper limb swelling, and the hospital stays in the high-quality group were remarkably shorter than they were in the regular group (P<0.05). The postoperative complications were less frequent in the high-quality group (P<0.05). The VAS scores in the high-quality group were lower than they were in the regular group at 1, 3, and 5 days after surgery, and the DASH scores in the high-quality group were lower at 1 month after discharge (P<0.05). The high-quality group showed lower SAS and SDS scores and higher QOL and patient satisfaction than the regular group (all P<0.05). There was no difference in the two-year survival rates between the two groups after the intervention (P>0.05). Conclusion: High-quality care following a radical mastectomy contributes to postoperative recovery, the relief of negative emotions, the reduction of complications, as well as the enhancement of QOL and patient satisfaction, so it is worthy of clinical promotion.
Keywords: High-quality care, breast cancer, surgery, quality of life
Introduction
Breast cancer is a common malignancy and is responsible for most cancer deaths in women worldwide [1]. In 2008, 2.08 million new cases and more than 600,000 deaths were reported [2]. Radical mastectomy is the first choice for the surgical treatment of breast cancer. However, the removal of the entire breast leads to significant chest deformities, thereby resulting in patients’ lack of confidence and courage. In addition, the occurrence of postoperative complications delays patient recovery [3,4]. Therefore, it is necessary to select reasonable and scientific nursing measures in the process of surgical treatment.
Nowadays, there have been increasing demands and higher requirements for medical services, so nursing care should meet the needs of patients from multiple disciplines [5,6]. High-quality care, a patient-centered nursing mode, focuses on providing comprehensive, high-quality and scientific nursing services according to patients’ needs [7], and it has been widely applied and has achieved significant benefits. It is superior to regular care in improving the mental states, the activities of daily living, and the quality of life (QOL) of patients with liver cancer during radiotherapy, as well as in reducing adverse reactions [8]. There is evidence that high-quality care can enhance the independence and QOL, and reduce the overall medical costs of patients with dementia [9].
The application of high-quality care in patients undergoing a radical mastectomy has not been investigated. Therefore, the effects of regular care and high-quality care in patients undergoing radical mastectomies were compared, aiming to provide them with a premium postoperative intervention.
Data and methods
Participants
In this study, 118 patients with breast cancer who underwent radical mastectomies in the Cancer Hospital of China Medical University from February, 2017 to May, 2019 were retrospectively included as subjects. They were divided into a regular group (n=56) and a high-quality group (n=62) according to the different nursing models the underwent. The inclusion criteria were as follows: primary breast cancer confirmed through a pathological diagnosis; patients aged 18-65 years old; patients with complete clinical data, as well as those who were able to complete each evaluation independently. The exclusion criteria were as follows: patients with severe systemic diseases, communication disorders, or psychological diseases such as anxiety and depression; patients who withdrew from the study. All the patients signed the informed consent, and this study was approved by the Ethics Committee of our hospital (LN163092XX).
Nursing intervention
In the regular group, the patients were administered regular care, mainly explaining the disease-related knowledge and surgical precautions to the patients and their families before the surgery, doing a good job of intraoperative doctor-nurse cooperation and postoperative complication prevention, strengthening the monitoring of vital signs during perioperative period, providing the patients with reasonable diet and exercise, and using drugs to assist in the intervention when necessary.
In the high-quality group, the patients were given high-quality care, which included the following measures: (1) Psychological support: Introduce the procedure and precautions of radical mastectomy to the patients to eliminate their doubts, anxieties and fears; Strengthen the interactions with the patients (entertainment programs, chatting, music) to divert their attention, ease their negative emotions and build confidence in their recoveries. Actively communicate with their family members, inform them of the patients’ specific conditions and surgical knowledge to keep them positive and optimistic in order to reduce their psychological pressure. (2) Prevention of complications: Closely monitor the postoperative changes in the patients for the early treatment of complications, so as to reduce the harm caused by the complications. (3) Pain care: Monitor and record the location, severity, and duration of any pain, guide the patients to use drugs scientifically and reasonably for analgesia. Divert the patients’ attention by means of communication or music. (4) Training guidance: Assess the patients’ physiological conditions regularly, formulate targeted training programs, adjust them promptly (frequency, intensity, and duration). Make a demonstration before training and correct the patients’ mistakes during training. (5) Discharge guidance: Use lectures, texts, and videos to explain the relationship between mental health and breast cancer, information on sexual life during rehabilitation, and breast self-examinations and methods of wearing breast prostheses, so as to enhance the postoperative QOL of patients.
Outcome measures
The recovery times of the indicators of physiological function were recorded, including the ambulation times after surgery, the sleep times within 72 h after the surgery and the regression times of upper limb swelling. The postoperative complications (upper limb edema, skin flap necrosis, subcutaneous effusion, and incisional surgical site infections) were recorded in the two groups.
The visual analogue scale (VAS) [10] was used to evaluate the patients’ pain on the 1st, 3rd, and 5th days after the surgery, with a highest possible score of 10 (the higher the score, the more severe the pain).
The upper limb function was evaluated using the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire [11]. There were 11 items related to upper limb function in this questionnaire, with a total score of 55. A higher score indicated a more severe dysfunction of the upper limb.
The self-rating anxiety scale (SAS) and the self-rating depression scale (SDS) [12] were employed to determine the patients’ mental health. The SAS has a maximum score of 100 points and indicates mild anxiety with scores of 50-70 points, moderate anxiety with scores of 71-90 points, and severe anxiety with scores of more than 90 points. A higher score indicates a severer anxiety. The SDS also has a maximum score of 100 points and indicates mild depression with scores of 50-70 points, moderate depression with scores of 71-90 points, and severe depression with scores of more than 90 points. A higher score indicates a severer depression.
After undergoing the nursing for 2 months, the treatment compliance of the patients in the two groups was evaluated using the self-made “treatment compliance questionnaire”. The questionnaire included five aspects, including reasonable diet, regular exercise, standardized medication, living habits and regular return visits, with a total score of 100 points. According to the scores, the patients’ compliance was divided into non-compliance (<70 points), basic compliance (70-85 points), compliance (>85 points). Total compliance rate = (cases with basic compliance + cases with compliance)/total number of cases × 100%.
The quality of life (QOL) assessment scale [13], including items covering general health, role-physical, physical functioning, social functioning, role-emotional and mental health, was administered at one month after discharge, Each dimension was scored out of 100 points, and the higher the score, the better the quality of life.
A patient satisfaction questionnaire developed by our hospital was used to evaluate the patient satisfaction in terms of environment, attitude and quality of medical staff. There were 20 questions in all, each worth 5 points (<70= dissatisfied, 70-89= moderately satisfied, ≥90= satisfied). Satisfaction rate = (satisfied cases + moderately satisfied cases)/total cases × 100%.
The postoperative 2-year survival rates of the two groups were observed, and 118 patients were followed up by telephone and interviews. The overall survival was defined as the period from the date of the surgery to the date of death. The patients were followed up once every three months for two years, and there were no lost cases.
Statistical processing
SPSS 19.0 (IBM Corp, Armonk, NY, USA) was used for the statistical analyses, and GraphPad Prism 7 was used to prepare the figures. The categorical data were compared using chi-square tests, and the measurement data were compared using independent samples t-tests. The intra-group comparisons were carried out using paired t-tests, and the inter-group comparisons were carried out using one-way ANOVA and verified using post-hoc tests. Kaplan-Meier was used to plot the OS of the breast cancer patients, and log-rank tests were used for the comparisons. P<0.05 was considered statistically significant.
Results
Comparison of the general data
Comparing the general clinical data of the two groups, it was found that there were no significant differences in terms of age, weight, residence, educational level, marital status, menopause, tumor location, or tumor staging (P>0.05) (Table 1).
Table 1.
Comparison of the general data ([n (%)], x±sd)
| Group | General group (n=56) | High-quality group (n=62) | χ2/t | P |
|---|---|---|---|---|
| Average age (years) | 47.28±6.88 | 48.67±7.12 | 1.076 | 0.284 |
| Average weight (kg) | 60.81±5.69 | 61.56±6.35 | 0.673 | 0.502 |
| Residence | 1.314 | 0.252 | ||
| Urban | 33 (58.93) | 30 (48.39) | ||
| Rural | 23 (41.07) | 32 (51.61) | ||
| Education level | 0.123 | 0.726 | ||
| ≤ high school | 28 (50.00) | 33 (53.23) | ||
| > high school | 28 (50.00) | 29 (46.77) | ||
| Marital status | 0.537 | 0.464 | ||
| Married | 48 (85.71) | 50 (80.65) | ||
| Unmarried | 8 (14.29) | 12 (19.35) | ||
| Menopause | 0.134 | 0.714 | ||
| Yes | 38 (67.86) | 44 (70.97) | ||
| No | 18 (32.14) | 18 (29.03) | ||
| Tumor location | 1.303 | 0.521 | ||
| Left | 24 (43.86) | 33 (53.23) | ||
| Right | 26 (46.43) | 23 (37.10) | ||
| Bilateral | 6 (10.71) | 6 (9.68) | ||
| Tumor staging | 0.279 | 0.870 | ||
| I | 22 (39.29) | 26 (41.94) | ||
| II | 27 (48.21) | 27 (43.55) | ||
| III | 7 (12.50) | 9 (14.52) |
Comparison of the postoperative recovery
The evaluations of the postoperative recoveries revealed that the ambulation times, the regression times of upper limb swelling, and the hospital stays in the high-quality group were remarkably shorter than they were in the regular group (P<0.05). Comparing the incidences of postoperative complications between the two groups, it was found that the total incidence of postoperative complications in the high-quality group was lower than it was in the regular group (6.45% VS. 19.64%, P<0.05) (Table 2).
Table 2.
Comparison of the postoperative recovery (x±sd)/[n (%)]
| Group | Regular group (n=56) | High-quality group (n=62) | χ2 | P |
|---|---|---|---|---|
| Ambulation time (h) | 24.62±4.51 | 19. 87±4.33 | 2.622 | 0.105 |
| Regression time of upper limb swelling (d) | 16. 21±3.29 | 10.35±2.89 | 3.276 | 0.070 |
| Hospital stay (d) | 29.25±4.77 | 23.28±3.82 | 4.053 | 0.044 |
Comparison of pain levels and the upper limb function
The VAS scores in the high-quality group were lower than they were in the regular group on the 1st, 3rd, and 5th days after the surgery (P<0.05). The evaluation of the upper limb function showed that the DASH scores in both groups decreased one month after discharge, but the DASH scores in the high-quality group were lower than they were in the regular group (P<0.05) (Figure 1).
Figure 1.
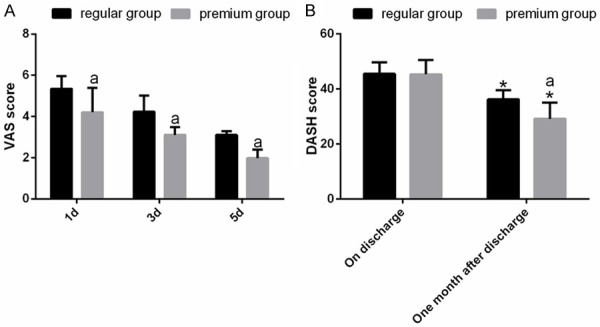
Comparison of pain levels and upper limb function. A. Comparison of VAS scores between the two groups. B. Comparison of the DASH scores between two groups. Note: aP<0.05 vs. regular group; *P<0.05 vs. at discharge.
Comparison of the negative emotions
There were no significant differences in the SAS and SDS scores between the two groups before admission (P>0.05). However, one month after discharge, the scores decreased significantly in both groups, and the scores in the high-quality group were lower than the scores in the regular group (P<0.05) (Figure 2).
Figure 2.
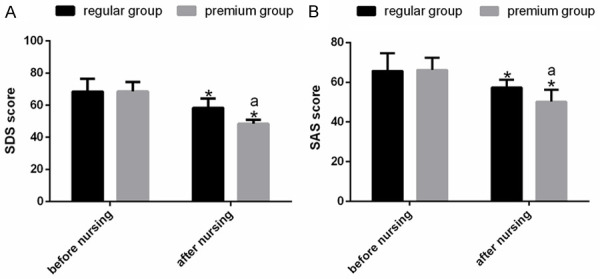
Comparison of the negative emotion scores. A. Comparison of the SAS scores between the two groups before and after the nursing. B. Comparison of the SDS scores between the two groups before and after the nursing. Note: *P<0.05 vs. before the nursing; aP<0.05 vs. the regular group.
Comparison of treatment compliance
After the nursing for 3 months, the treatment compliance of the patients was evaluated in the two groups. The results showed that there were 18 cases of compliance (32.14%), 20 cases of basic compliance (35.71%) and 18 cases of non-compliance (32.14%) in the conventional group, for a total compliance rate was 67.86%. In the high-quality group, there were 30 cases of compliance (48.39%), 23 cases of basic compliance (37.10%) and 9 cases of non-compliance (14.52%), for a total compliance rate of 85.48%. The total compliance rate in the high-quality group was higher than the rate in the regular group (P<0.05) (Table 3).
Table 3.
Comparison of the treatment compliance [n (%)]
| Group | Compliance | Basic compliance | Non-compliance | Total compliance rate |
|---|---|---|---|---|
| Regular group (n=56) | 18 (32.14) | 20 (35.71) | 18 (32.14) | 38 (67.86) |
| High-quality group (n=62) | 30 (48.39) | 23 (37.10) | 9 (14.52) | 53 (85.48) |
| χ2 | - | - | - | 5.181 |
| P | - | - | - | 0.023 |
Comparison of the postoperative QOL
The high-quality group showed higher general health, role-physical, physical functioning, social functioning, role-emotional, and mental health scores than the regular group after the intervention (P<0.05) (Figure 3).
Figure 3.
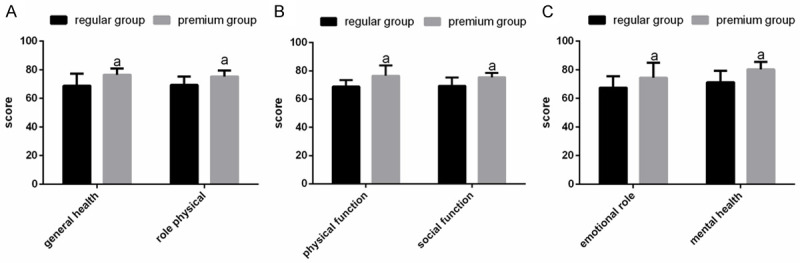
Comparison of the postoperative QOL. A. Comparison of the general health and role-physical scores. B. Comparison of the physical functioning and social functioning scores. C. Comparison of the role-emotional and mental health scores. Note: aP<0.05 vs. the regular group.
Comparison of the patient satisfaction levels
The patients’ satisfaction levels with the nursing care were evaluated before their discharge. In the regular group, 12 patients were highly satisfied, 28 were moderately satisfied, 16 were unsatisfied, for a total satisfaction rate of 71.43%. In the high-quality group the corresponding scores were 22, 33, and 7, for a total satisfaction rate of 88.87%. Therefore, the patients in the high-quality group were more satisfied with the care they received (P<0.05) (Table 4).
Table 4.
Comparison of the patient satisfaction rates [n (%)]
| Group | Satisfied | Moderately satisfied | Dissatisfied | Satisfaction rate |
|---|---|---|---|---|
| Regular group (n=56) | 12 (21.43) | 28 (50.00) | 16 (28.57) | 40 (71.43) |
| High-quality group (n=62) | 22 (35.48) | 33 (53.23) | 7 (11.29) | 55 (88.71) |
| χ2 | - | - | - | 5.600 |
| P | - | - | - | 0.018 |
Comparison of two-year survival rates between the two groups after the intervention
After intervention, the two-year survival rates of the two groups were evaluated, and the results showed that there was no significant difference between the high-quality group and the regular group (96.77% VS. 94.64%, P>0.05) (Figure 4).
Figure 4.
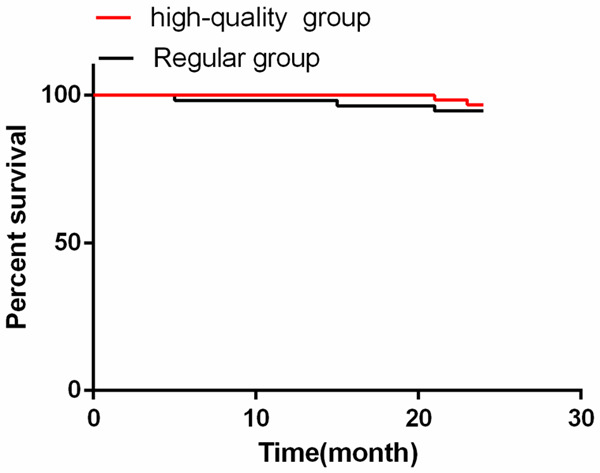
Comparison of the two-year survival rates between the two groups after the intervention. There was no difference in the two-year survival rates between the quality group and the conventional group (96.77% vs. 94.64%).
Discussion
The study was designed to analyze the implications of high-quality care in patients undergoing breast cancer surgery. It turned out that it is superior to regular care in terms of the postoperative recovery, the relief of negative emotions, the reduction of complications, as well as the enhancement of QOL and patient satisfaction, so it is worthy of clinical promotion.
Due to its high incidence and mortality, breast cancer has posed a serious threat to people’s health [14]. Radical mastectomy, a preferred option for its treatment, involves resecting the breast, an important female symbol, resulting in enormous psychological pressure on patients. Furthermore, the fear of surgery and illness may lead to a lack of confidence and courage, as well as depression, anxiety and other negative emotions [15,16]. Optimism and self-confidence are of great help to the treatment of diseases [17]. In this study, the patients in the high-quality group were given psychological support and professional solutions to eliminate their concerns and negative emotions. Therefore, the SAS and SDS scores in the high-quality group were lower than the corresponding scores in the regular group. Patients usually suffer from persistent pain after a radical mastectomy because it causes great physical damage to the body, which not only affects their normal activities, but also increases their psychological burden, reduces compliance with functional exercises, and delays recovery [18,19]. Thus, postoperative pain management is indispensable. In this study, we helped patients relieve pain through the scientific application of analgesia and the diversion of attention. As we speculated, the VAS scores of the patients in the high-quality group were lower than they were in the regular group, and the treatment compliance of the patients in the high-quality group was higher.
Radical mastectomy requires a wide range of resection of the breast, and this trauma leads to different degrees of upper limb dysfunction and seriously affects the QOL of patients [20]. Reasonable rehabilitation exercises can effectively enhance the upper limb function of patients undergoing radical mastectomies [21]. Therefore, according to the patient’s physical condition, we developed targeted training programs to promote functional recovery. Complications induced by radical mastectomy not only hinder the postoperative recovery, but they also seriously threaten patients’ health [22], making them a tricky problem to tackle. In this study, we carried out preventive care for the common complications in the high-quality group, so the incidence of postoperative complications was lower than the incidence in the regular group.
The QOL has been considered a key to evaluating the overall therapeutic effect and living condition of cancer patients [23]. Although radical mastectomy treats breast cancer effectively, it adversely affects the body image, femininity, sexual behavior, and self-worth of patients, resulting in poor QOL [24]. The patients in the high-quality group had higher general health, role-physical, physical functioning, social functioning, role-emotional, and mental health scores than the patients in the regular group. This may be related to the patient-centered characteristic of the high-quality care. The patients’ QOL and satisfaction in the high-quality group were found to be significantly higher than they were in the regular group, which indicates that the patients had a higher recognition of the high-quality care, providing solid evidence for the promotion of highquality care in the future. Studies by Li have shown that surgical intervention can improve the quality of life for patients with breast cancer [25]. The main purpose of nursing intervention is to improve the postoperative efficacy, reduce the complications and improve the survival rate for surgery patients. The postoperative 2-year survival rates of the two groups were compared in this study; however, the results showed that there was no significant difference between the two groups.
There are several limitations to this study. The differences in the nurses’ work experience may impact the quality of the nursing; The economic burden brought by the two nursing modes was also not analyzed. In addition, we evaluated the effectiveness of high-quality care in patients undergoing radical resection but failed to analyze its role in other breast cancer surgeries. Moreover, the patient follow-up times were too short in this study, so they should be extended.
To sum up, high-quality care following a radical mastectomy contributes to postoperative recovery, relief from negative emotions, the reduction of complications, as well as the enhancement of QOL and patient satisfaction, so it is worthy of clinical promotion.
Disclosure of conflict of interest
None.
References
- 1.Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biol Res. 2017;50:33. doi: 10.1186/s40659-017-0140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Stoyanov GS, Tsocheva D, Marinova K, Dobrev E, Nenkov R. Drainage after modified radical mastectomy-a methodological mini-review. Cureus. 2017;9:e1454. doi: 10.7759/cureus.1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cieslak K, Golusinski W. Coping with loss of ability vs. emotional control and self-esteem in women after mastectomy. Rep Pract Oncol Radiother. 2018;23:168–174. doi: 10.1016/j.rpor.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paganoni S, Karam C, Joyce N, Bedlack R, Carter GT. Comprehensive rehabilitative care across the spectrum of amyotrophic lateral sclerosis. NeuroRehabilitation. 2015;37:53–68. doi: 10.3233/NRE-151240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myrhaug HT, Mbalilaki JA, Lie NK, Hansen T, Nordvik JE. The effects of multidisciplinary psychosocial interventions on adult cancer patients: a systematic review and meta-analysis. Disabil Rehabil. 2020;42:1062–1070. doi: 10.1080/09638288.2018.1515265. [DOI] [PubMed] [Google Scholar]
- 7.Bachnick S, Ausserhofer D, Baernholdt M, Simon M, Match RN. Patient-centered care, nurse work environment and implicit rationing of nursing care in Swiss acute care hospitals: a cross-sectional multi-center study. Int J Nurs Stud. 2018;81:98–106. doi: 10.1016/j.ijnurstu.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Pang L, Wang Y, Xing Y, Zhao C. Application effects of whole course high-quality nursing on patients with liver cancer during radiotherapy. Iran J Public Health. 2019;48:1777–1785. [PMC free article] [PubMed] [Google Scholar]
- 9.Samus QM, Davis K, Willink A, Black BS, Reuland M, Leoutsakos J, Roth DL, Wolff J, Gitlin LN, Lyketsos CG, Johnston D. Comprehensive home-based care coordination for vulnerable elders with dementia: maximizing independence at home-plus-study protocol. Int J Care Coord. 2017;20:123–134. doi: 10.1177/2053434517744071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, Harris JD. Validation of digital visual analog scale pain scoring with a traditional paper-based visual analog scale in adults. J Am Acad Orthop Surg Glob Res Rev. 2018;2:e088. doi: 10.5435/JAAOSGlobal-D-17-00088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahabier KC, Den Hartog D, Theyskens N, Verhofstad MHJ, Van Lieshout EMM HUMMER Trial Investigators. Reliability, validity, responsiveness, and minimal important change of the disabilities of the arm, shoulder and hand and constant-murley scores in patients with a humeral shaft fracture. J Shoulder Elbow Surg. 2017;26:e1–e12. doi: 10.1016/j.jse.2016.07.072. [DOI] [PubMed] [Google Scholar]
- 12.Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, Zhang Z, Wang W, Cheng Y, Wang H. Comparison of hospital anxiety and depression scale (HADS) and zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236:170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 13.Arcopinto M, Salzano A, Giallauria F, Bossone E, Isgaard J, Marra AM, Bobbio E, Vriz O, Aberg DN, Masarone D, De Paulis A, Saldamarco L, Vigorito C, Formisano P, Niola M, Perticone F, Bonaduce D, Sacca L, Colao A, Cittadini A T.O.S.CA. (Trattamento Ormonale Scompenso CArdiaco) Investigators. Growth hormone deficiency is associated with worse cardiac function, physical performance, and outcome in chronic heart failure: insights from the T.O.S.CA. GHD study. PLoS One. 2017;12:e0170058. doi: 10.1371/journal.pone.0170058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liang HF, Zhang XZ, Liu BG, Jia GT, Li WL. Circular RNA circ-ABCB10 promotes breast cancer proliferation and progression through sponging miR-1271. Am J Cancer Res. 2017;7:1566–1576. [PMC free article] [PubMed] [Google Scholar]
- 15.Hubbeling HG, Rosenberg SM, Gonzalez-Robledo MC, Cohn JG, Villarreal-Garza C, Partridge AH, Knaul FM. Psychosocial needs of young breast cancer survivors in Mexico City, Mexico. PLoS One. 2018;13:e0197931. doi: 10.1371/journal.pone.0197931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kocan S, Gursoy A. Body image of women with breast cancer after mastectomy: a qualitative research. J Breast Health. 2016;12:145–150. doi: 10.5152/tjbh.2016.2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan DK, Zhang X, Fung HH, Hagger MS. Does emotion and its daily fluctuation correlate with depression? A cross-cultural analysis among six developing countries. J Epidemiol Glob Health. 2015;5:65–74. doi: 10.1016/j.jegh.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang X, Lai Q, Tian Y, Zou L. Effect of evidence-based nursing intervention on upper limb function in postoperative radiotherapy patients with breast cancer. Medicine (Baltimore) 2020;99:e19183. doi: 10.1097/MD.0000000000019183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsumoto M, Flores EM, Kimachi PP, Gouveia FV, Kuroki MA, Barros ACSD, Sampaio MMC, Andrade FEM, Valverde J, Abrantes EF, Simões CM, Pagano RL, Martinez RCR. Benefits in radical mastectomy protocol: a randomized trial evaluating the use of regional anesthesia. Sci Rep. 2018;8:7815. doi: 10.1038/s41598-018-26273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galantino ML, Stout NL. Exercise interventions for upper limb dysfunction due to breast cancer treatment. Phys Ther. 2013;93:1291–1297. doi: 10.2522/ptj.20120049. [DOI] [PubMed] [Google Scholar]
- 21.Brookham RL, Cudlip AC, Dickerson CR. Examining upper limb kinematics and dysfunction of breast cancer survivors in functional dynamic tasks. Clin Biomech (Bristol, Avon) 2018;55:86–93. doi: 10.1016/j.clinbiomech.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Josephine DSP. Evaluation of lymphedema prevention protocol on quality of life among breast cancer patients with mastectomy. Asian Pac J Cancer Prev. 2019;20:3077–3084. doi: 10.31557/APJCP.2019.20.10.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Nieuwenhuizen AJ, Buffart LM, Brug J, Leemans CR, Verdonck-de Leeuw IM. The association between health related quality of life and survival in patients with head and neck cancer: a systematic review. Oral Oncol. 2015;51:1–11. doi: 10.1016/j.oraloncology.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Turk KE, Yilmaz M. The effect on quality of life and body image of mastectomy among breast cancer survivors. Eur J Breast Health. 2018;14:205–210. doi: 10.5152/ejbh.2018.3875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li ZJ, Zhang P, Zhang W, Zhang Z, Wang XM, Xiao CH. Oncological safety and prognosis factors analysis of immediate breast reconstruction after nipple-areola-complex sparing mastectomy. Zhonghua Zhong Liu Za Zhi. 2018;40:690–695. doi: 10.3760/cma.j.issn.0253-3766.2018.09.011. [DOI] [PubMed] [Google Scholar]


