Abstract
Aim: This study aimed to report a case of a fully-covered metal stent for the treatment of post-Percutaneous Transhepatic Biliary Drainage (PTBD) obstruction caused by a blood clot in the common bile duct (CBD). Case presentation: The case involved a 75-year-old man who had a history of recurring upper abdominal pain and jaundice. The result of an abdominal computerized tomography showed a stricture in the CBD. After PTBD, bleeding in the tube of PTBD was noted. The bleeding sites were detected using superselective hepatic arteriography. After the bleeding was stopped, Endoscopic Retrograde Cholangiopancreatography (ERCP) was performed to insert a fully-covered metal stent to extract the blood clot. Five months later, He was performed whipple procedure successfully and the pathology shows adenocarcinoma (cholangicarcinoma). This was the first case reported in China. Conclusions: The complications related to post-PTBD obstruction, which was caused by a blood clot in the CBD, might lead to serious health issues or even death. The blood clot could be diagnosed according to laboratory and clinical data, particularly imaging. Digital subtraction angiography (DSA) and ERCP were necessary and effective for the patient in the present case. Successfully placement of a fully-covered stent could relieve jaundice. The residual thrombus was easily extracted through the stent. This was important for the preparation of the coming procedure.
Keywords: Percutaneous transhepatic biliary drainage (PTBD), blood clot, fully-covered metal stent (FCMS), digital subtraction angiography (DSA)
Introduction
Percutaneous transhepatic biliary drainage (PTBD) is a procedure to relieve benign and malignant obstructive jaundice for patients in whom the endoscopic cannulation of the common bile duct (CBD) has failed [1]. PTBD results in some complications, including infection, hemorrhage, pneumothorax, and biliary leakage into the peritoneum [2]. The reported rate of significant bleeding after PTBD is about 2%-2.5% [3,4].
Interventional therapy has been increasingly used to treat bleeding associated with severe hemobilia [5,6]. A blood clot in the bile duct caused by delayed bleeding following PTBD, with a time interval between 1 to 4 days, may cause cholangitis and jaundice. Fully-covered self-expandable metal stent (FCSEMS) placement has been used to achieve endoscopic hemostasis for bleeding after ERCP [7]. This study described a case of a blood clot in the CBD after PTBD, which was successfully treated by CSEMS placement.
Case presentation
A 75-year-old man was admitted because of abdominal pain and jaundice. He denied any consumption of alcohol. No biochemical or clinical sign of coagulopathy or primary liver disease was observed. The laboratory test results were as the following: total bilirubin, 248 μmol/L (2-18 μmol/L); direct bilirubin, 148 μmol/L (<7 μmol/L); alanine aminotransferase, 77 U/L (<64 U/L); aspartate aminotransferase, 99 U/L (<64 U/L); γ-glutamyl transpeptidase, 201 U/L (<47 U/L); alkaline phosphatase, 507 U/L (<47 U/L); and tumor marker carbohydrate antigen 19-9, 50.04 U/L. All other detected parameters, including hemoglobin and platelet counts, prothrombin time, renal function, and Alpha Fetoprotein (AFP) and Carcinoembryonic antigen (CEA) levels, appeared to be normal. Abdominal computed tomography showed a stricture in the CBD (Figure 1). The patient was highly suspected of malignant stenosis. After the patient was admitted, some medicines as hepatoprotective drugs and best care were provided to the patient routinely. PTBD was performed to relieve the jaundice for the next operation. Hemobilia occurred immediately after PTBD was performed for relieving jaundice.
Figure 1.
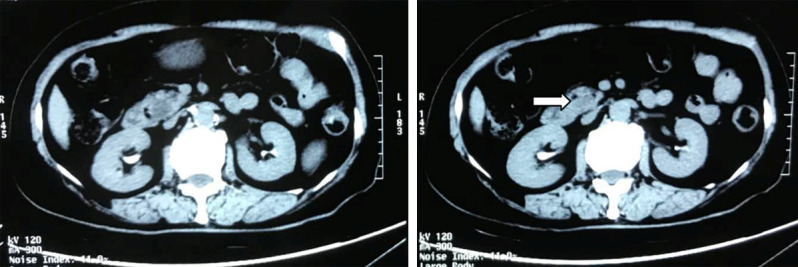
Abdominal computed tomography showed a stricture in the CBD (white arrow).
The patient after PTBD had drainage of about 60 mL of bleeding bile. The blood test showed a decrease in red blood count and hemoglobin content. The bleeding sites were detected by superselective hepatic arteriography (Figure 2). The results showed that the bleeding was caused by a hepatic arterio-biliary fistula. A steel ring and medical tissue adhesive were used for embolization.
Figure 2.
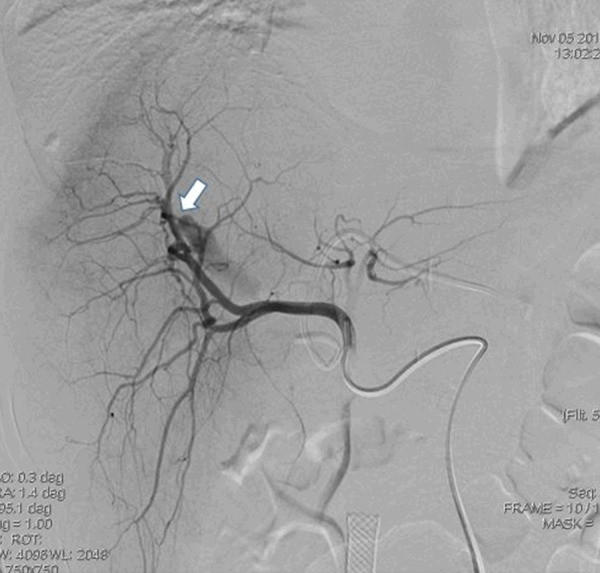
Right hepatic angiogram reveals a fistula between the right hepatic artery and the right intrahepatic duct (white arrow).
ERCP was performed after an increase in the total bilirubin level. The result showed the obstruction of the end of the CBD, the dilatation of the intrahepatic bile duct, and a large number of irregular filling defects in the bile duct (Figure 3). The papilla was incised, and a fully-covered SEMS (10 mm diameter, 6 cm long; COOK MEDICAL LLC, Bloomington, U.S.A.) was inserted into the CBD. The distant end of the stent was outside the papilla (Figure 4). After the CSEMS was placed, a balloon and a basket were used to clear a large amount of brown floc. The bile flowed out smoothly. One week later, the patient had recovered after the treatment using repeated ERCP. All the blood clot remains were fully extracted. Five months later, he was performed whipple procedure successfully and the pathology shows adenocarcinoma (cholangicarcinoma).
Figure 3.
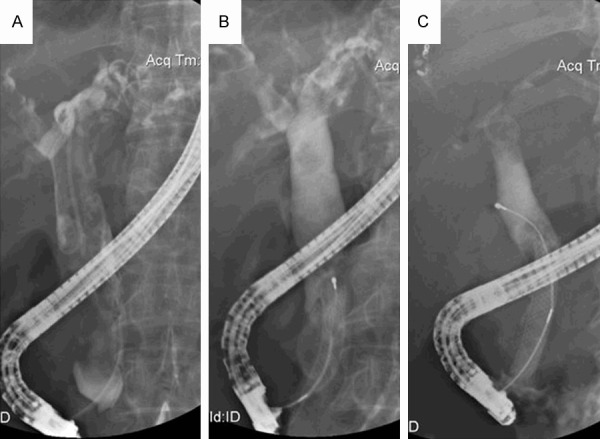
Patient with obstructive jaundice by blood clot underwent FCSMES treatment. A. Cholangiogram showing a large number of irregular filling defects in the dilation of bile duct. B. Fully-covered SEMS (10 mm diameter, 6 cm long; COOK MEDICAL LLC, Bloomington, USA) was inserted in the common bile duct. The distant end of stent was outside the papilla. C. Blood clots remains were fully extracted with a repeated ERCP one week later.
Figure 4.
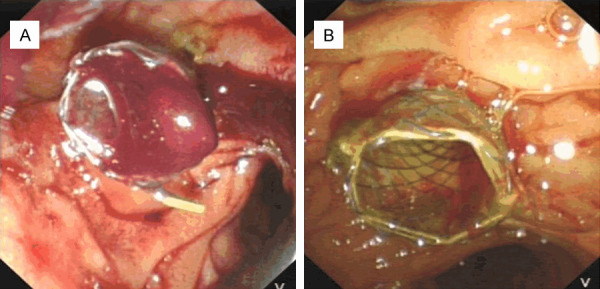
Endoscopic image shows FCSEMS treated the obstructive jaundice by blood clot successfully. A. Massive hemobilia developed after PTBD. B. Blood clots remains were fully extracted with a repeated ERCP one week later.
Discussion
Severe hemobilia sometimes occurs following PTBD, leading to life-threatening hemorrhagic shock. This has been shown to be associated with a mortality rate up to 50% [8]. The symptoms of biliary hemorrhage after PTBD include abdominal pain, gastrointestinal bleeding, and blood pressure decline. The incidence of hemobilia is about 4.6% [9]. Its major reasons are repeated puncture injury or abnormal coagulation function or vessel invasion by tumor and biliary tract infection. The operators need to improve their technical level and also to improve blood coagulation function before surgery to reduce postoperative biliary bleeding in the bile duct to a certain extent.
Most bleeding can be alleviated after general treatment including the application of hemostasis, thrombin, and growth inhibition. The source and location of biliary bleeding should be identified first for severe hemophilia. Cholangiography and angiography are the key to diagnosis and treatment. Superselective hepatic artery embolization [10,11] has been increasingly used as an interventional therapy to treat serious hemobilia after PTBD. Most physicians and medical scientists have agreed that embolizing the bleeding artery simultaneously is the standard procedure. This treatment has been proven effective in preventing recurrent hemorrhage caused by the countercurrent flow of blood through a branch to the bleeding artery, controlling the initial hemorrhage. In this case, an arterio-biliary fistula was found by DSA, and the bleeding was controlled successfully with a steel ring and medical tissue adhesive.
A blood clot in the bile duct after PTBD may lead to its obstruction or cholangitis. The obstructions could be related to the long oval shape and elastic, dense, and soft features [12]. Instead of removing the blood clot completely, Maroy et al. [13] placed a plastic bile duct stent over the clot. The delayed recovery of the patient might be caused by inadequate drainage. In the present case, a fully covered metal stent was inserted into the CBD due to several reasons. Since the patient had biliary obstruction, the placement of a covered metal stent compressed the extrahepatic bile duct thrombus to promote bile drainage. When PTBD could not relieve jaundice, the residual thrombus was also easily extracted using the stent. After the jaundice was reduced to a certain extent, the thrombus was cleaned completely and prepared for the next surgery. The pancreatic duct stent was failed to be replaced because of failure of intubation, but no pancreatitis occurred because the papilla was incised before placing the metal stent.
It can be concluded that for patients with distant biliary obstruction, it is an effective method to treat post-PTBD obstruction caused by a blood clot in the CBD by FCMS and can be the preparation for the next surgical treatment.
Disclosure of conflict of interest
None.
References
- 1.Pedicini V, Poretti D, Mauri G, Trimboli M, Brambilla G, Sconfienza LM, Cornalba G, Sardanelli F. Management of post-surgical biliary leakage with percutaneous transhepatic biliary drainage (PTBD) and occlusion balloon (OB) in patients without dilatation of the biliary tree: preliminary results. Eur Radiol. 2010;20:1061–1068. doi: 10.1007/s00330-009-1637-6. [DOI] [PubMed] [Google Scholar]
- 2.Al Mahjoub A, Menahem B, Fohlen A, Dupont B, Alves A, Launoy G, Lubrano J. Preoperative biliary drainage in patients with resectable perihilar cholangiocarcinoma: is percutaneous transhepatic biliary drainage safer and more effective than endoscopic biliary drainage? A meta-analysis. J Vasc Interv Radiol. 2017;28:576–582. doi: 10.1016/j.jvir.2016.12.1218. [DOI] [PubMed] [Google Scholar]
- 3.Fidelman N, Bloom AI, Kerlan RK Jr, Laberge JM, Wilson MW, Ring EJ, Gordon RL. Hepatic arterial injuries after percutaneous biliary interventions in the era of laparoscopic surgery and liver transplantation: experience with 930 patients. Radiology. 2008;247:880–886. doi: 10.1148/radiol.2473070529. [DOI] [PubMed] [Google Scholar]
- 4.Aung TH, Too CW, Kumar N, Damodharan K, Urlings TA, Patel A, Chan S, Toh L, Gogna A, Irani F, Lo R, Tan BS, Tay KH, Sum L. Severe bleeding after percutaneous transhepatic drainage of the biliary system. Radiology. 2016;278:957–958. doi: 10.1148/radiol.2016151954. [DOI] [PubMed] [Google Scholar]
- 5.Rerknimitr R, Kongkam P, Kullavanijaya P. Treatment of tumor associated hemobilia with a partially covered metallic stent. Endoscopy. 2007;39(Suppl 1):E225. doi: 10.1055/s-2007-966555. [DOI] [PubMed] [Google Scholar]
- 6.Marynissen T, Maleux G, Heye S, Vaninbroukx J, Laleman W, Cassiman D, Verslype C, Van der Merwe S, Van Steenbergen W, Nevens F. Transcatheter arterial embolization for iatrogenic hemobilia is a safe and effective procedure: case series and review of the literature. Eur J Gastroenterol Hepatol. 2012;24:905–909. doi: 10.1097/MEG.0b013e328354ae1b. [DOI] [PubMed] [Google Scholar]
- 7.Itoi T, Yasuda I, Doi S, Mukai T, Kurihara T, Sofuni A. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011;43:369–372. doi: 10.1055/s-0030-1256126. [DOI] [PubMed] [Google Scholar]
- 8.Cao H, Liu J, Li T, Cao G, Xu G, Zhai S, Xue J, Wang Z, Shi S, Bai W. Interventional therapy for the treatment of severe hemobilia after percutaneous transhepatic cholangial drainage: a case series. Int Surg. 2013;98:223–228. doi: 10.9738/INTSURG-D-13-CC194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takahara O, Ichikawa M, Hisanaga Y, Shimizu M, Onizuka T, Ichikawa K. Treatment of hemobilia after percutaneous transhepatic cholangiography and drainage (PTCD) Nihon Shokakibyo Gakkai Zasshi. 1992;89:2030–2036. [PubMed] [Google Scholar]
- 10.Zhang AB, Xu ZB, Zhang M, Zheng SS. Successful superselective embolization of posttraumatic pseudoaneurysm of replaced hepatic artery in a child with situs inversus totalis. Chin Med J (Engl) 2007;120:1465–1467. [PubMed] [Google Scholar]
- 11.Tisnado J, Beachley MC, Cho SR. Control of intrahepatic bleeding by superselective embolization of the middle hepatic artery. South Med J. 1982;75:70–71. doi: 10.1097/00007611-198201000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Sandblom P, Mirkovitch V, Saegesser F. Formation and fate of fibrin clots in the biliary tract: a clinical and experimental study. Ann Surg. 1977;185:356–366. doi: 10.1097/00000658-197703000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maroy B. Life-threatening angiocholitis following clot formation after balloon dilation for extraction of a large stone in the lower bile duct. Endoscopy. 2013;45(Suppl 2 UCTN):E97–98. doi: 10.1055/s-0032-1326248. [DOI] [PubMed] [Google Scholar]


