Abstract
Objective: This research aimed at observing the effect of applying high-quality nursing in the intensive care unit (ICU) to esophageal cancer (EC) patients after radical resection. Methods: From January 2015 to February 2020, 155 EC patients who underwent radical resection were divided into the control group (CG; n=77) and the observation group (OG; n=78). The CG was given conventional nursing intervention, and the OG was given high-quality nursing intervention. The scores of the visual analogue scale (VAS), clinical related indexes, complications, self-rating anxiety scale (SAS), self-rating depression scale (SDS), nursing satisfaction and SF-36 of patients were compared. Results: After nursing, compared with the CG, the duration of the indwelling drainage tube, time to getting out of bed, recovery of bowel sounds and hospitalization in the OG was shorter, and the incidence of postoperative complications was less. In addition, after nursing, the VAS, SAS and SDS scores of patients in both groups decreased, and these indexes in the OG decreased more than those in the CG. Patients were investigated upon discharge, and it was revealed that the nursing satisfaction of patients in the OG was obviously better than that in the CG. Three months after the operation, the scores of general health (GH), mental health (MH), role-physical (RP), role emotional (RE) and vitality (VT) of patients in the OG were higher than those in the CG. Conclusion: High-quality nursing exerts a better effect in the ICU for patients who underwent EC surgery; it can reduce pain and adverse events and promote rehabilitation.
Keywords: Esophageal cancer, operation, high-quality nursing, intensive care unit
Introduction
Esophageal cancer (EC) is a common malignancy in human beings, and most patients are diagnosed in the middle and late stages. Most of them have poor prognosis and EC is one of the fastest growing malignancies [1]. The overall survival rate is still very poor. The 5-year survival rate of all patients is about 10%-15%, while the rate of those undergoing a radical operation can be improved to 40% [2], which is an effective surgical method to cure the disease. However, patients who have undergone surgical treatment often need follow-up treatment in the ICU to ensure that the disease can be fully cured [3]. Radical resection of EC tissue causes great damage to patients, during the recovery period after operation patients have poor physical resistance and are prone to adverse events [4]. After the operation, because patients can’t eat and swallow normally, their psychology and physiology are also impaired [5]. Therefore, corresponding nursing intervention is needed, so as to reduce the incidence of postoperative complications and shorten the recovery time [6].
Although conventional nursing can reduce the incidence of postoperative complications, its effect is still unsatisfactory in regard to the improvement of people’s nursing requirements [7]. High-quality nursing focuses on being patient-centered, in which care is strengthened on the basis of conventional nursing intervention. It can deepen the connotation of nursing specialty and implement a nursing responsibility system, so as to improve the overall service consciousness [8]. In clinical practice, the high-quality nursing mode not only meets the basic living needs of patients, but also ensures their bodily comfort. By balancing the patients’ psychology, we can obtain the support of their families and society, so as to improve their overall satisfaction [9]. In various chronic diseases, it is considered important to provide high-quality nursing [10]. Cho et al. reported that cancer patients were happy to meet experienced nurses who could combine clinical and biological knowledge and nursing skills with human contact. High-quality nursing can alleviate patients’ physical pain and make them feel safe and secure [11]. Although it has been reported to be applied in clinical practice [12], the application effect in the ICU after EC operation is still vague.
In this research, 155 patients undergoing EC surgery were given high-quality nursing intervention, so as to discuss the application effect of this nursing mode.
Materials and methods
General data
A total of 155 EC patients who underwent radical resection in The First Affiliated Hospital, Hengyang Medical School, University of South China from January 2015 to February 2020 were included as the research subjects. This research was approved by the Ethics Committee of The First Affiliated Hospital, Hengyang Medical School, University of South China. The subjects and their families were informed in advance and informed consent forms were signed. Inclusion criteria were as follows: the disease met the diagnostic criteria of EC [13], which was diagnosed by barium meal before the operation and gastroscopy, and confirmed by pathological examination after operation; those patients who met the TNM classification standards of the eighth edition of EC in stages I, II and part of stage III [14]; those who met the indications of EC surgery [15]; those with American Society of Anesthesiologists (ASA) grades I-II; those with complete clinical data. Exclusion criteria were as follows: distant metastasis of tumor cells; patients complicated with severe liver, kidney, heart and lung diseases, chronic intestinal diseases, cognitive dysfunction and other malignancies.
Grouping and nursing methods
The 155 EC patients were divided into the control group (CG; n=77) and the observation group (OG; n=78). Thereunto, the CG received conventional nursing intervention: the wards were clean and well ventilated, and the indoor temperature was comfortable; patients’ body temperature, heart rate and other vital signs were closely monitored; breathing and thoracic drainage were performed after anesthesia; whether the patient had fever, chest and back pain, dyspnea and so on were observed. If so, nurses informed the attending physician in real time and advised the patients to take their medicine on time. On this basis, the OG was given high-quality nursing intervention.
Psychological nursing: Nurses actively communicated, listened to patients’ complaints and solved their problems according to their educational background and social environment; they also gave health education to patients, explained the related knowledge of diseases, precautions after operation and possible complications; furthermore, they communicated and cooperated with patients’ families in real time, and enhanced their awareness of treating diseases correctly to help the patient actively cooperate with treatment and nursing.
Pain care: Patients were instructed to keep a comfortable posture, breathe deeply and relax; their attention could be diverted by watching movies, listening to music, chatting with family members, etc., so as to avoid being too focused on the pain; within 48 h after operation, if the patient had severe pain, analgesic drugs were used in accordance with the doctor’s advice.
Nutritional nursing: Half-dose Peptisorb (25 mL/h) was injected by nutrition pump on the first day after operation, a half-dose Nutrison (50 mL/h) was injected on the next day, and full-dose Nutrison (100 mL/h) was injected on the third day. After the operation, a normal diet was forbidden for one week, and then food was changed from a liquid diet to a general diet. High-vitamin and high-protein foods were given. Water and food intake were monitered, with more meals per day but less food at each meal; all these standards conformed to the doctor’s advice.
Respiratory tract nursing: During bed stay, nurses cleaned the secretions in the nose and mouth in real time, and kept the respiratory tract wet by atomization twice a day, so as to promote expectoration; if the sputum was deep or sticky, a fiberoptic bronchoscope was employed for sputum aspiration and bronchial lavage; in case of dyspnea, cyanosis and other clinical symptoms, it was necessary to assist the patient in inhaling oxygen and inform the doctor in real time.
Nursing care of the incision: During postoperative bed rest, whether the incision was bleeding has seepage was closely monitored, the dressing was changed regularly, and incision drainage was performed as necessary; within 4 days after operation, the incision was soaked with Rivanol gauze every day (2-3 times a day) in light of the doctor’s advice; it was then cleaned with liquor hibitane (2-3 times/d).
Nursing of respiratory function training: After the vital signs of patients were stable, they were instructed to carry out respiratory function training; the abdominal breathing training method was as follows: patients kept a the supine position, they hung their hands on both sides of the body, inhaled slowly, held their breath for 1 s after the lung is raised, and then exhaled slowly, 10 times/d, 10 minutes/time; the training mode of lip-shrinking breathing was as follows: patients inhaled and held their breath for a moment, then exhaled, and placed the tip of their tongue at the bottom of the mandibular teeth when they exhaled, and whistled from ear to ear, twice a day, 10 minutes/time.
Main outcome measures
The complications were observed, including bleeding, incision infection, anastomotic fistula, pulmonary infection, adhesive intestinal obstruction and chylothorax. The pain of patients was evaluated by visual analogue score (VAS) [16], ranging from 0 to 10. The higher the score, the more severe the pain was.
Patients were evaluated by the self-rating anxiety scale (SAS) and self-rating depression scale (SDS) [17]. The total score was 100 points, and the higher the score, the more serious the degree of anxiety or depression was.
Secondary outcome measures
The clinical related indexes of patients were observed, including the duration of the indwelling drainage tube, time to getting out of bed, recovery of bowel sounds and hospitalization duration.
The nursing satisfaction of patients at discharge was analyzed via the nursing satisfaction questionnaire [18]. The total score is 100 points, which can be divided into three satisfaction levels: dissatisfied (> 70 points), relatively satisfied (70-89 points) and very satisfied (90-100 points) (very satisfied + relatively satisfied)/total cases × 100% = nursing satisfaction.
The quality of life of both groups before and 3 months after operation was assessed via the SF-36 Quality of Life Scale [19]. It includes 8 dimensions: general health (GH), mental health (MH), social function (SF), physiological function (PF), role physical (RP), role emotional (RE), bodily pain (BP) and vitality (VT). The full score of each dimension is 100 points, and the higher the score, the higher the quality of life is.
Statistical methods
The counting data were represented by number of cases and percentage [n (%)]. The differences between groups were compared by Chi-square test, and when the theoretical frequency was less than 5, the likelihood ratio Chi-square value or Fisher exact test method was used. The measurement data conforming to a normal distribution in data analysis were expressed by mean ± standard deviation (Mean ± SD), the comparison of mean was made by t-test or analysis of variance, and that between groups before and after was tested through paired t-test. P < 0.05 was taken as the basis of statistical conclusion, indicating that there were remarkable differences. Data were processed by SPSS 25.0 purchased from IBM Corporation of America.
Results
Clinical data
We collected the clinical data of both groups of patients. There was no marked difference between the CG and the OG in clinical information such as educational level, age, gender, esophageal diameter and TNM stage (P > 0.05) (Table 1).
Table 1.
Clinical data of two groups [n (%)]/(Means ± SD)
| Clinical data | Control group (n=77) | Observation group (n=78) | χ2/t | P |
|---|---|---|---|---|
| Education level | 0.352 | 0.839 | ||
| Primary school | 7 (9.09) | 6 (7.69) | ||
| Junior high school | 15 (19.48) | 18 (23.08) | ||
| High school and above | 55 (71.43) | 54 (69.23) | ||
| Age (years) | 66.58±3.49 | 67.15±3.85 | 0.956 | 0.336 |
| Gender | 0.158 | 0.691 | ||
| Male | 40 (51.95) | 43 (55.13) | ||
| Female | 37 (48.05) | 35 (44.87) | ||
| Diameter of diseased esophagus (cm) | 3.39±0.35 | 3.42±0.37 | ||
| Tumor site | 0.589 | 0.745 | ||
| Upper esophagus | 24 (31.17) | 20 (25.64) | ||
| Middle esophagus | 27 (35.06) | 30 (38.46) | ||
| Lower esophagus | 26 (33.77) | 28 (35.90) | ||
| TNM staging | 0.372 | 0.830 | ||
| Stage I | 6 (7.79) | 5 (6.41) | ||
| Stage II | 32 (41.56) | 36 (46.15) | ||
| Stage III | 39 (50.65) | 37 (47.44) | ||
| Marital status | 0.236 | 0.627 | ||
| Unmarried | 7 (9.09) | 10 (12.82) | ||
| Married | 70 (90.91) | 68 (87.18) |
Pain intensity in both groups before and after nursing
The pain intensity of patients before and after nursing was assessed via VAS scoring. Before nursing, there was no obvious difference in VAS scores between the two groups (P > 0.05). After nursing, the VAS scores decreased (P < 0.05), and scores in the OG decreased more than those in the CG (P < 0.05) (Figure 1).
Figure 1.
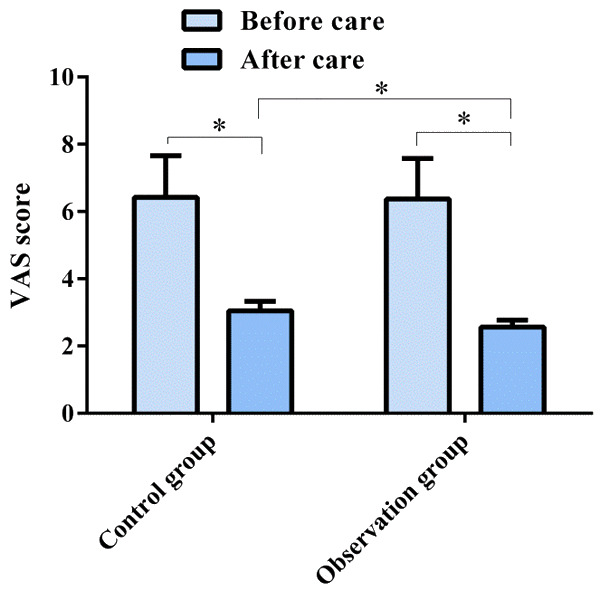
VAS score changes of two groups before and after nursing. After nursing, the VAS scores of patients in the two groups decrease, and the scores in the OG decrease more than those in the CG. *P < 0.05.
Clinical related indicators in both groups of patients
We observed the clinical related indexes after nursing, such as time of the indwelling drainage tube, getting out of bed, recovery of bowel sounds and hospitalization. After nursing, the time of the above factors in patients in the OG were shorter than those in the CG (P < 0.05) (Figure 2).
Figure 2.
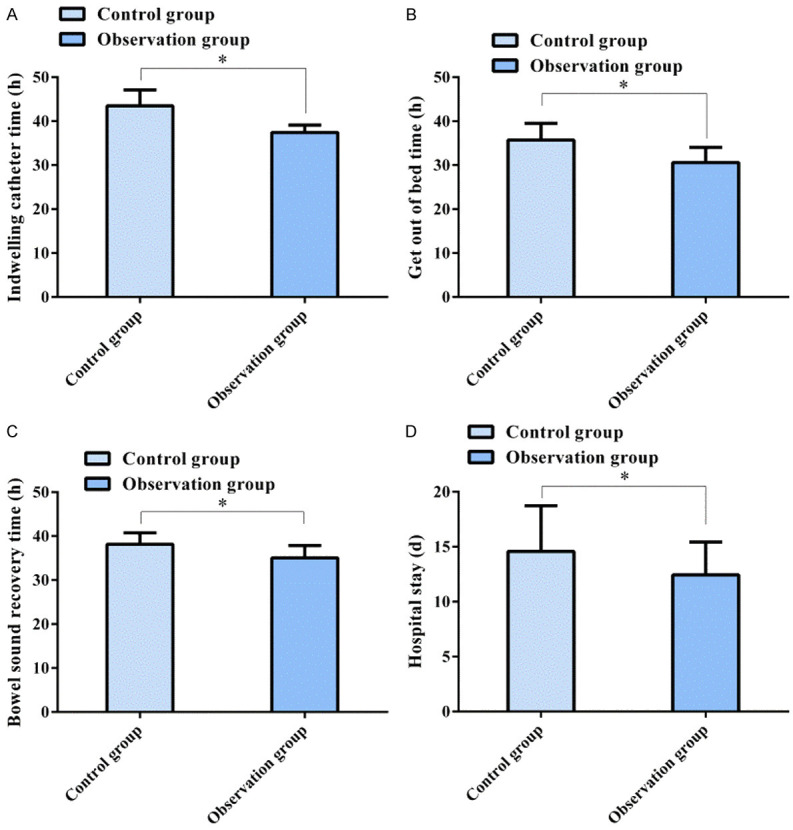
Clinical related indexes of two groups of patients. After nursing, the time of the indwelling drainage tube (A), time to getting out of bed (B), time to recovery of bowel sounds (C) and hospitalization time (D) in the OG are shorter than those in the CG. *P < 0.05.
Incidence of complications in both groups of patients
The complications in the two groups of patients during nursing were observed. In the OG, there was bleeding, anastomotic leak, pulmonary infection, adhesive intestinal obstruction and chylothorax in 1 case, and incision infection in 2 cases, with a complication rate of 8.97%. In the CG, there were 5 cases of bleeding, 3 of incision infection, 2 cases with anastomotic leak, 3 of pulmonary infection, 1 of adhesive intestinal obstruction and 2 of chylothorax, with an incidence rate of 20.78%. The incidence of postoperative complications in the OG was less than that in the CG (P < 0.05) (Table 2).
Table 2.
Incidence of complications in both groups [n (%)]
| Nursing satisfaction | Control group (n=77) | Observation group (n=78) | χ2 | P |
|---|---|---|---|---|
| Hemorrhage | 5 (6.49) | 1 (1.28) | 1.601 | 0.206 |
| Incision infection | 3 (3.90) | 2 (2.56) | 0.220 | 0.639 |
| Anastomotic leak | 2 (2.60) | 1 (1.28) | 0.353 | 0.552 |
| Pulmonary infection | 3 (3.90) | 1 (1.28) | 1.053 | 0.304 |
| Adhesive intestinal obstruction | 1 (1.30) | 1 (1.28) | 0.494 | 0.482 |
| Chylothorax | 2 (2.60) | 1 (1.28) | 0.353 | 0.552 |
| Total incidence rate (%) | 20.78 | 8.97 | 4.273 | 0.039 |
SAS and SDS scale scores before and after nursing in both groups
The anxiety and depression of patients in the two groups were evaluated via SAS and SDS scales. The results revealed that there was no marked difference in SAS and SDS scores between the OG and the CG before operation (P > 0.05). After nursing, the scores were reduced (P < 0.05), especially in the OG (P < 0.05) (Figure 3).
Figure 3.
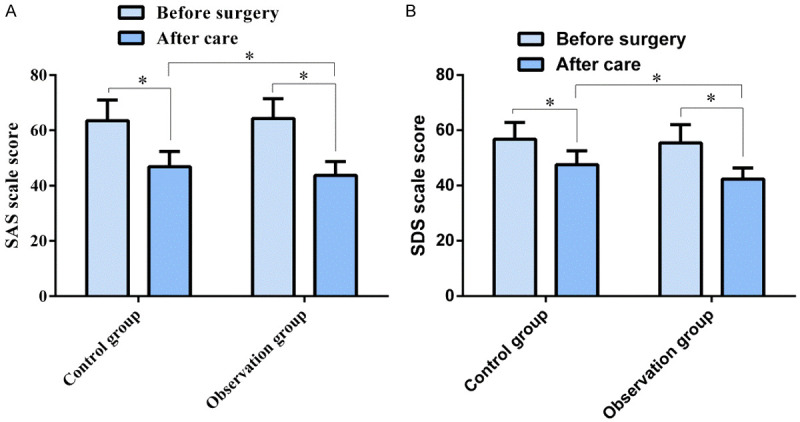
Scores of SAS and SDS before and after nursing in both groups. After nursing, the SAS (A) and SDS (B) scale scores of patients in the two groups reduce, especially in the OG. *P < 0.05.
Nursing satisfaction in both groups of patients
Before and after nursing, we investigated the nursing satisfaction in the two groups of patients. The results revealed that 44 patients in the OG were very satisfied after nursing, 32 were quite satisfied, and 2 were dissatisfied. In the CG, 31 patients were very satisfied, 36 were relatively satisfied and 10 were dissatisfied. The nursing satisfaction of patients in the OG was obviously better than that in the CG (P < 0.05) (Table 3).
Table 3.
Nursing satisfaction of patients in both groups [n (%)]
| Nursing satisfaction | Control group (n=77) | Observation group (n=78) | χ2 | P |
|---|---|---|---|---|
| Very satisfied | 31 (40.26) | 44 (56.41) | 5.894 | 0.015 |
| Satisfied | 36 (46.75) | 32 (41.03) | ||
| Dissatisfied | 10 (12.99) | 2 (2.56) | ||
| Satisfaction (%) | 87.01 | 97.44 |
SF-36 scale scores in both groups
The quality of life of patients in both groups was assessed via the SF-36 scale. There was no remarkable difference in GH, MH, SF, PF, RP, RE, BP and VT scores between the two groups before operation (P > 0.05). After 3 months of operation, the scores of GH, MH, RP, RE, BP and VT increased significantly (P < 0.05), and those of SF and PF in the OG also increased significantly (P < 0.05) (Figure 4).
Figure 4.
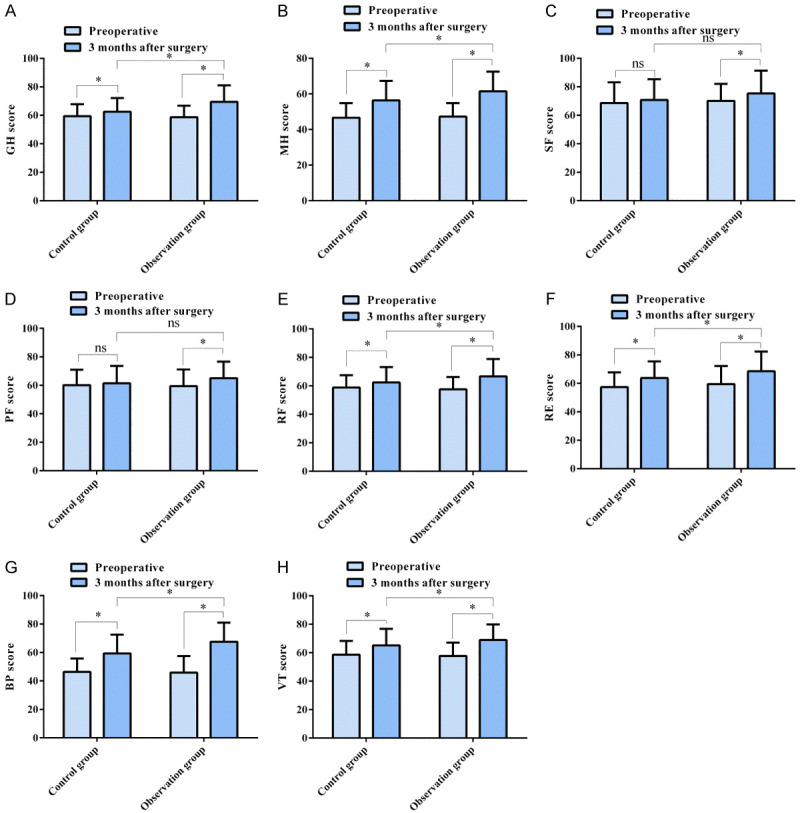
Comparison of scores of SF-36 between both groups. There is no marked difference in the scores of GH (A), MH (B), SF (C), PF (D), RP (E), RE (F), BP (G) and VT (H) between the two groups before operation. After 3 months of operation, the scores of GH, MH, RP, RE, BP and VT were improved, and those of SF and PF in the OG were also improved. In addition, the scores of GH, MH, RP, RE, BP and VT in the OG were higher than those in the CG. Note: nsP > 0.05, *P < 0.05.
Discussion
Clinically, EC is treated in the ICU after radical operation. In order to ensure the recovery of patients, it is vital to give targeted nursing measures in this process [20]. In this research, we provided high-quality nursing service for patients undergoing EC surgery, and the results revealed that this nursing model promoted postoperative recovery.
EC patients experience a variety of psychological problems (including depression, anxiety and stress), and timely intervention of psychological problems can improve their quality of life [21]. Secondly, radical resection of EC can bring great trauma to patients, which may affect physical activities such as cough and breathing after the operation [22]. Mitchell et al. reported that while patients were in the ICU, providing basic care for patients included cooperation with their families, which can improve respect, collaboration, support and overall success in a 48-hour family-centered nursing survey [23]. Based on this, we provided psychological and pain nursing intervention for patients and the results revealed that high-quality nursing could reduce negative emotions and pain after EC surgery. Similarly, Liu et al. explained that high-quality nursing can relieve depression, anxiety and stress in EC patients during the perioperative period [24]. It may be that high-quality nursing success is enhanced through a series of optimized nursing measures, and through psychological and incision nursing. So, it can reduce the postoperative stress reaction of patients and reduce their negative emotions. Although resection is the main means of radical treatment, this highly invasive operation can cause a series of postoperative complications, such as pulmonary infection and decreased blood oxygen content [25]. After the operation, we gave the patients nursing for respiratory tract care, incision care, and nutrition and respiratory function care. Cleaning their respiratory tract and incision in real time can guide them to effectively cough, and avoid pain and bleeding of the wound caused by thoracic expansion and traction during coughing [26]. A reasonable energy intake plan was formulated and high-quality nutritious meals were made for patients based on their condition. In our research, after the implementation of high-quality nursing, the time of the indwelling drainage tube, getting out of bed, recovery of bowel sounds, and hospitalization were shortened. Thus, it can be seen that high-quality nursing can promote the recovery of physical function of patients after radical resection of esophageal cancer. Yin et al. explained that with a frequent incidence of infection after esophageal cancer surgery, and through effective early warning monitoring, the risk of postoperative complications can be reduced [27]. Our research shows that the incidence of complications, such as bleeding and incision infection, is reduced, which may be due to the strengthening of the monitoring of patients postoperatively. Therefore, high-quality nursing can promote the recovery of physical function of patients after radical resection of EC, and shorten the hospitalization time, which can reduce their economic burden. Cheng et al. claimed that EC patients experienced a decline of quality of life (QOL) after esophagectomy due to malnutrition, lack of physical exercise and psychological symptoms, and that a comprehensive intervention model of mobile health support could improve the quality of life of patients and promote their postoperative recovery [28]. Similarly, the quality of life of patients with high-quality nursing intervention has been improved. Through a series of optimized nursing measures, in the early stages, through psychological nursing, patients can have positive effects when facing diseases. In this process, by giving corresponding nursing measures to patients, the stress response in patients after surgery can be alleviated, thus maintaining a better physical and mental state, improving the quality of life and promoting their rehabilitation. We also investigated patients’ satisfaction before discharge. The results revealed that patients’ overall nursing satisfaction was better after high-quality nursing intervention. Besides, shortening the length of stay in the hospital can reduce the economic burden of patients, and patients recognize the quality of nursing service.
Our research confirmed the feasibility of implementing high-quality nursing in the ICU for patients undergoing EC surgery. However, there are still some limitations. First of all, we don’t know patients’ quality of life after one year. Secondly, it is unclear whether an individualized nursing mode has an impact on the survival of EC patients after operation, which needs further exploration in the future.
In this research, high-quality nursing exerted a better effect for patients in the ICU undergoing EC surgery; it can reduce their pain and adverse events and promote their rehabilitation.
Disclosure of conflict of interest
None.
References
- 1.Watanabe M, Otake R, Kozuki R, Toihata T, Takahashi K, Okamura A, Imamura Y. Recent progress in multidisciplinary treatment for patients with esophageal cancer. Surg Today. 2020;50:12–20. doi: 10.1007/s00595-019-01878-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mariette C, Markar SR, Dabakuyo-Yonli TS, Meunier B, Pezet D, Collet D, D’Journo XB, Brigand C, Perniceni T, Carrère N, Mabrut JY, Msika S, Peschaud F, Prudhomme M, Bonnetain F, Piessen G Fédération de Recherche en Chirurgie (FRENCH) and French Eso-Gastric Tumors (FREGAT) Working Group. Hybrid minimally invasive esophagectomy for esophageal cancer. N Engl J Med. 2019;380:152–162. doi: 10.1056/NEJMoa1805101. [DOI] [PubMed] [Google Scholar]
- 3.Wang X, Li X, Cheng H, Zhang B, Zhong H, Wang R, Zhong B, Cao Q. Single-port inflatable mediastinoscopy combined with laparoscopic-assisted small incision surgery for radical esophagectomy is an effective and safe treatment for esophageal cancer. J Gastrointest Surg. 2019;23:1533–1540. doi: 10.1007/s11605-018-04069-w. [DOI] [PubMed] [Google Scholar]
- 4.Xu QL, Li H, Zhu YJ, Xu G. The treatments and postoperative complications of esophageal cancer: a review. J Cardiothorac Surg. 2020;15:163. doi: 10.1186/s13019-020-01202-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steenhagen E. Preoperative nutritional optimization of esophageal cancer patients. J Thorac Dis. 2019;11(Suppl 5):S645–S653. doi: 10.21037/jtd.2018.11.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang YL, Tsai YF, Hsu CL, Chao YK, Hsu CC, Lin KC. The effectiveness of a nurse-led exercise and health education informatics program on exercise capacity and quality of life among cancer survivors after esophagectomy: a randomized controlled trial. Int J Nurs Stud. 2020;101:103418. doi: 10.1016/j.ijnurstu.2019.103418. [DOI] [PubMed] [Google Scholar]
- 7.Li W, Gao J, Wei S, Wang D. Application values of clinical nursing pathway in patients with acute cerebral hemorrhage. Exp Ther Med. 2016;11:490–494. doi: 10.3892/etm.2015.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao SH, Akkadechanunt T, Xue XL. Quality nursing care as perceived by nurses and patients in a Chinese hospital. J Clin Nurs. 2009;18:1722–1728. doi: 10.1111/j.1365-2702.2008.02315.x. [DOI] [PubMed] [Google Scholar]
- 9.Ryu JI, Kim K. The influence of nursing care integration services on nurses’ work satisfaction and quality of nursing care. J Nurs Manag. 2018;26:1024–1032. doi: 10.1111/jonm.12629. [DOI] [PubMed] [Google Scholar]
- 10.Thorsteinsson LS. The quality of nursing care as perceived by individuals with chronic illnesses: the magical touch of nursing. J Clin Nurs. 2002;11:32–40. doi: 10.1046/j.1365-2702.2002.00575.x. [DOI] [PubMed] [Google Scholar]
- 11.Cho SH, June KJ, Kim YM, Cho YA, Yoo CS, Yun SC, Sung YH. Nurse staffing, quality of nursing care and nurse job outcomes in intensive care units. J Clin Nurs. 2009;18:1729–1737. doi: 10.1111/j.1365-2702.2008.02721.x. [DOI] [PubMed] [Google Scholar]
- 12.Kousoulou M, Suhonen R, Charalambous A. Associations of individualized nursing care and quality oncology nursing care in patients diagnosed with cancer. Eur J Oncol Nurs. 2019;41:33–40. doi: 10.1016/j.ejon.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 13.Barret M, Prat F. Diagnosis and treatment of superficial esophageal cancer. Ann Gastroenterol. 2018;31:256–265. doi: 10.20524/aog.2018.0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.D’Journo XB. Clinical implication of the innovations of the 8(th) edition of the TNM classification for esophageal and esophago-gastric cancer. J Thorac Dis. 2018;10(Suppl 22):S2671–S2681. doi: 10.21037/jtd.2018.03.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Rijswijk AS, Hagens ERC, van der Peet DL, van Berge Henegouwen MI, Gisbertz SS. Differences in esophageal cancer surgery in terms of surgical approach and extent of lymphadenectomy: findings of an international survey. Ann Surg Oncol. 2019;26:2063–2072. doi: 10.1245/s10434-019-07316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gong DH, Liu JF, Zhao X, Zhang L. The effect of nursing intervention on preoperative cataract. Medicine (Baltimore) 2018;97:e12749. doi: 10.1097/MD.0000000000012749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao T, Zhu H, Zhang C, Chai Y, Guo C, Zhu X, Bao B, Li X, Lin J, Zheng X. Efficacy of acetaminophen with and without oxycodone for analgesia in non-operative treatment of extremity fractures in adults: protocol for a double-blind randomized clinical trial. Trials. 2019;20:510. doi: 10.1186/s13063-019-3579-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang YY, Zhang C, Han XR, Li W, Wang YL. Determinants of compassion satisfaction, compassion fatigue and burn out in nursing: a correlative meta-analysis. Medicine (Baltimore) 2018;97:e11086. doi: 10.1097/MD.0000000000011086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu L, Sun Y, Wang L, Gao Q, Li A, Wang J, Gao Y. Total hip arthroplasty for intertrochanteric fracture fixation failure. Eur J Med Res. 2019;24:39. doi: 10.1186/s40001-019-0398-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanekiyo S, Takeda S, Iida M, Nishiyama M, Kitahara M, Shindo Y, Tokumitsu Y, Tomochika S, Tsunedomi R, Suzuki N, Abe T, Yoshino S, Hazama S, Ueno T, Nagano H. Efficacy of perioperative immunonutrition in esophageal cancer patients undergoing esophagectomy. Nutrition. 2019;59:96–102. doi: 10.1016/j.nut.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Heo J, Noh OK. Psychiatric comorbidities among patients with esophageal cancer in South Korea: a nationwide population-based, longitudinal study. J Thorac Dis. 2020;12:1312–1319. doi: 10.21037/jtd.2020.02.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inoue T, Ito S, Ando M, Nagaya M, Aso H, Mizuno Y, Hattori K, Nakajima H, Nishida Y, Niwa Y, Kodera Y, Koike M, Hasegawa Y. Changes in exercise capacity, muscle strength, and health-related quality of life in esophageal cancer patients undergoing esophagectomy. BMC Sports Sci Med Rehabil. 2016;8:34. doi: 10.1186/s13102-016-0060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell M, Chaboyer W, Burmeister E, Foster M. Positive effects of a nursing intervention on family-centered care in adult critical care. Am J Crit Care. 2009;18:543–552. doi: 10.4037/ajcc2009226. [DOI] [PubMed] [Google Scholar]
- 24.Liu XY, Jiao CH, Zhao D, Chen Y, Zhang HM. Psychological impact of high-quality nursing care on patients with esophageal cancer during perioperative period: a protocol of systematic review. Medicine (Baltimore) 2020;99:e22270. doi: 10.1097/MD.0000000000022270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guerrero I, Cuenca JA, Cardenas YR, Nates JL. Hemorrhagic shock secondary to aortoesophageal fistula as a complication of esophageal cancer. Cureus. 2020;12:e7146. doi: 10.7759/cureus.7146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song YN, Qi Y, Zhang CY, Sheng YL, Wu K, Zhu SL, Han L, Shan TT, Ye GC, Zhang QY, Chen YL, Chen JW, Liu YF, Gao LB, Yang Y, He ZF, Zhu DY, Liu DL, Wen FB, Zheng TL, Li JL, Zhao S. A new technology for reducing anastomotic fistula in the neck after esophageal cancer surgery. J Thorac Dis. 2019;11:3084–3092. doi: 10.21037/jtd.2019.07.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yin LX, Chen BM, Zhao GF, Yuan QF, Xue Q, Xu K. Scoring system to predict the risk of surgical site infection in patients with esophageal cancer after esophagectomy with cervical anastomosis. Surg Infect (Larchmt) 2018;19:696–703. doi: 10.1089/sur.2018.051. [DOI] [PubMed] [Google Scholar]
- 28.Cheng C, Ho RTH, Guo Y, Zhu M, Yang W, Li Y, Liu Z, Zhuo S, Liang Q, Chen Z, Zeng Y, Yang J, Zhang Z, Zhang X, Monroe-Wise A, Yeung SC. Development and feasibility of a mobile health-supported comprehensive intervention model (CIMmH) for improving the quality of life of patients with esophageal cancer after esophagectomy: prospective, single-arm, nonrandomized pilot study. J Med Internet Res. 2020;22:e18946. doi: 10.2196/18946. [DOI] [PMC free article] [PubMed] [Google Scholar]


