Abstract
Objective: To analyze the effect of primary nursing on the improvement of potential risk and pain degree in elderly patients with cancer pain. Methods: Altogether 187 patients with cancer pain from June 2018 to November 2019 were selected as the research participants and grouped into two groups according to different nursing intervention methods, including 102 cases in the research group (RG) and 85 cases in the control group (CG). The pain relief and medication compliance were evaluated. General Self-efficacy Scale (GSES) and Exercise of Self-Care Agency (ESCA) were used to evaluate the self-efficacy and self-care ability. Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) were used to evaluate the anxiety and depression. Pittsburgh Sleep Quality Index (PSQI) was used to evaluate sleep quality. SF-36 Quality of Life Scale was used to evaluate the quality of life. Self-made nursing satisfaction questionnaire was used to evaluate the nursing satisfaction. Results: The improvement of pain relief in the RG was evidently higher than that in the CG. The scores of SAS and SDS in the RG after intervention were evidently lower than those in the CG. GSES and ESCA scores of patients in the RG after intervention were evidently higher than those in the CG. The compliance of patients in the RG after intervention was evidently higher than that in the CG. The PSQI scores of patients in the RG after intervention were evidently better than those in the CG. The scores of SF-36 and nursing satisfaction in the RG were evidently higher than those in the CG. Conclusion: The implementation of primary nursing intervention for elderly patients with cancer pain can effectively relieve their pain and improve their bad psychological state and medication compliance, thus improving patients’ quality of life.
Keywords: Primary nursing, cancer pain in the elderly, potential risk, pain degree
Introduction
Cancer is the main health problem of the elderly, and pain is one of the most common symptoms among elderly cancer patients [1]. In the whole disease process, it affects 70% of all cancer patients. In the planning treatment of cancer pain, most patients can effectively relieve pain during hospitalization, but due to the long course of some patients, they are treated at home for pain relief [2,3]. After discharge, most patients are unable to adhere to effective treatment due to the lack of professional advice and guidance, which will not only aggravate the clinical symptoms of patients, but also have a serious impact on their daily life [4,5]. Therefore, the treatment of cancer patients must be a continuous process, and various, convenient and timely methods should be adopted to improve the pain management of patients.
Studies have shown that [6] cancer pain will lead to anxiety, depression and other adverse emotions in patients, while the elderly, as a special group, have more serious adverse emotions. In addition, pain and bad psychological state will produce a vicious circle, which will have a very adverse impact on the treatment and prognosis [7]. Primary nursing is a new nursing service, which extends the inpatient nursing to the treatment and rehabilitation after discharge [8]. It takes the patient as the center, and the nursing team develops a purposeful and planned management mode for the patient [9]. Moreover, the nursing stuff regularly hold lectures after discharge, patiently communicate with patients, give patients psychological support and encouragement, eliminate patients’ fear, and timely understand patients’ recent pain control and adverse drug reactions through communication with patients [10-12]. For example, research shows that in order to enhance the self-management of cancer pain outpatients, nursing intervention measures were given to patients to effectively improve the treatment compliance of patients [13].
At present, there are few researches on the intervention of primary nursing in elderly patients with cancer pain. We observed the influence of this nursing mode on patients’ self-management, treatment compliance, psychological status and cancer pain by implementing this nursing mode in elderly patients with cancer pain after discharge, with a hope to provide a feasible nursing intervention for the patients.
Materials and methods
General data
Altogether 187 patients with cancer pain treated in Chongqing Hospital of Traditional Chinese Medicine from June 2018 to November 2019 were selected as the research participants, and assigned into two groups according to different nursing intervention methods, including 102 cases in the research group (RG) and 85 cases in the control group (CG). Inclusion criteria: all patients were diagnosed with malignant tumors by pathology, and all patients had pain symptoms [14]; the general clinical data of patients were complete; patients voluntarily accepted relevant nursing and treatment; patients were not dependent on alcohol and drugs; patients could correctly understand the relevant contents of the scale and answer. This study was approved by the ethics committee. The participants and their families have signed a fully informed consent form. Exclusion criteria: patients could not actively cooperate with the researcher; patients dropped out the experiment halfway; patients have recently received radiotherapy and chemotherapy; patients had pain caused by other diseases; patients had mental illness or family history of mental illness; patients had infectious diseases; patients lost to follow.
Nursing methods
The CG was given routine nursing: Pre-hospital guidance was given before the patients were discharged from the hospital, and the patients were given routine health education about cancer pain treatment, including medication method and dosage, the importance of taking medicine on time to effectively relieve cancer pain, inviting family members to know how to use pain assessment tools and how to express pain, giving records, and telling patients how to prevent and deal with adverse reactions of opioids and non-drug treatment measures for cancer pain.
The RG was given primary nursing: (1) A primary nursing group was established, and individual nursing work plans and procedures were formulated for each patient, including the patient’s name, age, diagnosis, contact information, pain location, nature and score. The name, dosage and frequency of analgesic drugs prescribed in the doctor’s order at discharge, as well as patients’ cognition of cancer pain and medication compliance were recorded in detail. And the contact information of the patient care team leader and the doctor in charge was given to patients, and the patient was informed to contact the medical staff under all circumstances. (2) Follow-up: Nurses could shorten the distance with patients by chatting, understanding the current psychological status of patients, and alleviating the anxiety and depression of patients due to excessive worry about their illness through targeted intervention guidance, so that patients could relax physically and mentally and face the disease bravely. After being discharged from hospital, the team members who had been trained in professional knowledge of cancer pain and passed the examination with strong communication skills served as follow-up personnel. After being discharged from hospital, they made the telephone return visit once a week. For patients with pain score ≥ 3, they were followed up twice a week. (3) Follow-up contents: Whether the patients were taking analgesic drugs on time and in quantity according to the doctor’s advice, the current pain control effect, the impact of pain on their own emotions, sleep and daily life activities, and whether there were adverse drug reactions. (4) Strengthen communication: The nursing team held a health lecture every month, invited experts to explain the misunderstanding of cancer pain control and the prevention and treatment of adverse reactions caused by opioids. After the lecture, they communicated with patients and patiently answered questions raised by patients.
Observation index
1. Pain relief: The patient’s pain disappeared completely after care, which was rated as complete remission. After care, patients’ pain was obviously relieved and they could live normally, which was rated as partial remission. After care, the patient’s pain was relieved, but life was still disturbed, which was rated as mild remission. After care, the patient’s pain has not been alleviated, and there was a trend of aggravation, which was rated as invalid. Total remission rate = (complete remission + partial remission).
2. Self-rating Anxiety Scale (SAS) [15] was used, with a total score of 100 points. The score ranging from 50 to 70 points was regarded as mild anxiety, 71 to 90 points as moderate anxiety, and scores above 90 points as severe anxiety.
3. Self-rating Depression Scale (SDS) [16] was used, with a total score of 100 points. The score ranging from 50 to 70 was regarded as mild depression, 71 to 90 as moderate depression, and scores above 90 as severe depression.
4. General Self-Efficacy Scale (GSES) [17] was applied. There were 10 items in the scale, with a total score of 40 points, and the score of each question was 1-4 points. After evaluation and statistics, the higher score indicates the higher self-efficacy of patients.
5. Exercise of Self-Care Agency (ESCA) [18] was applied. There were 4 different fields and 43 items in the scale, and the total score after evaluation was 172 points. After self-evaluation, the score was counted, and the higher score indicates the higher self-care ability.
6. Medication compliance: The questionnaire mainly included taking painkillers on time, not adjusting dosage or changing medicine without authorization. If both items meet the requirements, it is regarded as completely compliant. If only one item meets the requirements, it is regarded as partially compliant, and if both items are inconsistent, it is regarded as non-compliant.
7. Pittsburgh Sleep Quality Index (PSQI) [19] was applied, with 7 dimensions and scores ranging from 0 to 21 points. The higher score after evaluation indicates the worse sleep quality of patients.
8. The Generic Quality of Life Inventory (GQLI) [20] was used. It included four items, namely psychological function, physical function, material life state and social function. Each item was scored 100 points, and the higher score indicates the better quality of life.
9. Nursing satisfaction: Patients were given a self-made satisfaction questionnaire, which consisted of five items, namely, service timeliness, management standardization, service attitude, hospitalization environment and comprehensive quality of nursing staff. The higher score indicates the higher satisfaction with service.
Statistical method
SPSS22.0 (Beijing Easybio Technology Co., Ltd., China) was used for statistical analysis. The counting data were represented as the number/percentage [n (%)] and compared by Chi-square test. When the theoretical frequency in Chi-square test was less than 5, continuous correction Chi-square test was used. The measurement data were represented by mean ± standard deviation (mean ± SD) and compared by independent sample t test. The comparison before and after the nursing adopted paired t test. When P < 0.05, the difference had statistical significance.
Result
General information
There were no significant differences in gender, average age, body mass index, educational level, residence, nationality, marital status, smoking history, drinking history, diet preference and pain duration between the two groups (P > 0.05) (Table 1).
Table 1.
Comparison of general data between the two groups [n (%)] (mean ± SD)
| Classification | RG (n=102) | CG (n=85) | t/χ2 value | P value |
|---|---|---|---|---|
| Gender | 0.018 | 0.893 | ||
| Male | 53 (51.96) | 45 (52.94) | ||
| Female | 49 (48.04) | 40 (47.06) | ||
| Average age (years) | 62.16±6.36 | 62.04±6.21 | 0.129 | 0.896 |
| Body mass index (kg/m2) | 23.24±3.71 | 22.61±3.45 | 1.193 | 0.234 |
| Educational level | 0.087 | 0.769 | ||
| ≥ high school | 47 (46.08) | 41 (48.24) | ||
| < high school | 55 (53.92) | 44 (51.76) | ||
| Residence | 0.560 | 0.454 | ||
| Urban | 46 (45.10) | 43 (50.59) | ||
| Rural | 56 (54.90) | 42 (49.41) | ||
| Nationality | 0.261 | 0.609 | ||
| Han | 55 (53.92) | 49 (57.65) | ||
| Minorities | 47 (46.08) | 36 (42.35) | ||
| Marital status | 0.908 | 0.635 | ||
| Unmarried | 21 (20.95) | 14 (16.47) | ||
| Married | 36 (35.29) | 28 (32.94) | ||
| Divorced/widowed | 45 (44.12) | 43 (50.59) | ||
| Smoking history | 0.779 | 0.377 | ||
| Yes | 57 (55.88) | 42 (49.41) | ||
| No | 45 (44.12) | 43 (50.59) | ||
| Drinking history | 0.257 | 0.612 | ||
| Yes | 53 (51.96) | 41 (48.24) | ||
| no | 49 (48.04) | 44 (51.76) | ||
| Dietary preference | 0.046 | 0.829 | ||
| Light | 58 (56.86) | 47 (55.29) | ||
| Spicy | 44 (43.14) | 38 (44.71) | ||
| Duration of pain (months) | 0.227 | 0.973 | ||
| ≤ 1 | 23 (22.55) | 19 (22.35) | ||
| 1-6 | 36 (35.29) | 30 (35.29) | ||
| 7-12 | 24 (25.53) | 22 (25.88) | ||
| > 12 | 19 (18.63) | 14 (16.47) |
Comparison of pain remission after care between the two groups
The total pain remission rate after care was 92.16% in the RG and 68.24% in the CG. The total pain remission rate in the RG was evidently higher than that in the CG (P < 0.05) (Table 2).
Table 2.
Comparison of pain remission after care between the two groups (mean ± SD)
| Group | n | Complete remission | Partial remission | Mild remission | Invalid | Total remission rate |
|---|---|---|---|---|---|---|
| RG | 102 | 63 (61.76) | 39 (38.24) | 6 (5.88) | 2 (1.96) | 94 (92.16) |
| CG | 85 | 23 (27.06) | 35 (41.18) | 15 (17.65) | 12 (14.12) | 58 (68.24) |
| χ2 | - | 22.481 | 0. 682 | 6.437 | 9.893 | 17.441 |
| P | - | < 0.001 | 0.168 | 0.011 | 0.002 | < 0.001 |
Comparison of SAS and SDS scores between the two groups before and after care
There was no significant difference in SAS and SDS scores between the two groups before care (P > 0.05), but after care, SAS and SDS scores of patients in the RG were evidently lower than those in the CG (P < 0.05) (Table 3).
Table 3.
Comparison of SAS and SDS scores between the two groups before and after care (mean ± SD)
| Group | n | SAS score | SDS score | ||
|---|---|---|---|---|---|
|
|
|
||||
| Before nursing | After nursing | Before nursing | After nursing | ||
| RG | 102 | 39.29±3.56 | 26.45±2.42 | 36.04±3.15 | 25.94±2.21 |
| CG | 85 | 39.72±3.46 | 31.76±2.95 | 35.88±3.18 | 32.62±2.72 |
| t | - | 0.833 | 13.520 | 0.344 | 18.530 |
| P | - | 0.406 | < 0.001 | 0.731 | < 0.001 |
Comparison of GSES scores between the two groups before and after care
There was no significant difference in GSES scores between the two groups before care (P > 0.05), but the GSES scores of the two groups improved after care, and the GSES scores of the RG after care were evidently higher than those of the CG (P < 0.05) (Figure 1).
Figure 1.
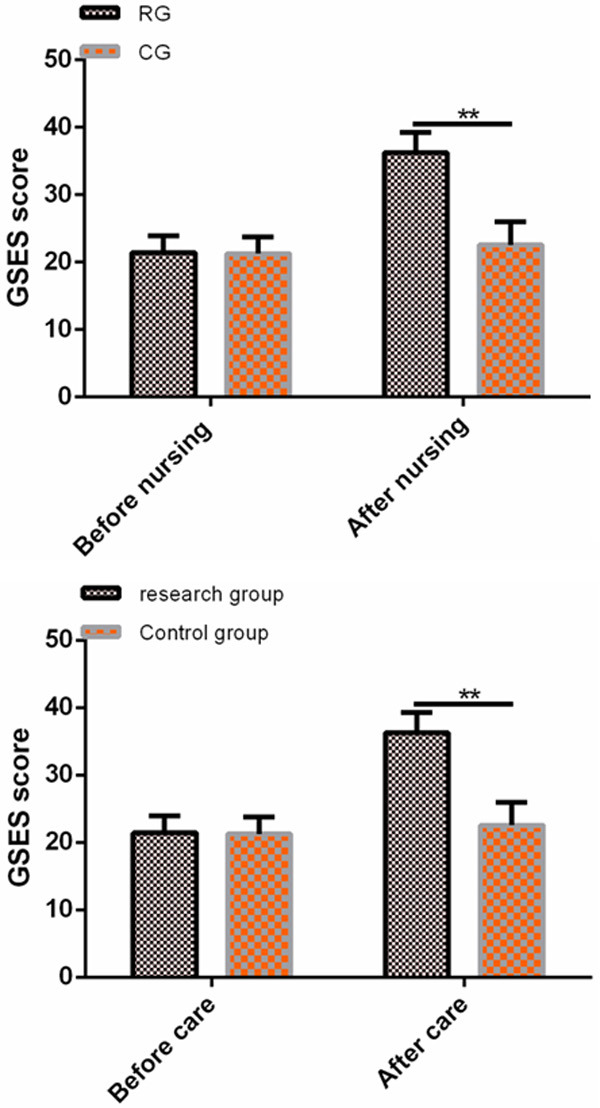
Comparison of GSES scores between the two groups before and after care. There was no significant difference in GSES scores between the two groups before care (P > 0.05), but the GSES scores of the RG after care were evidently higher than those of the CG. Note: *indicates compared with before nursing, P < 0.05; **indicates compared with the control group, P < 0.01.
Comparison of ESCA scores between the two groups before and after care
There was no significant difference in ESCA scores between the two groups before care (P > 0.05), but the ESCA scores of the two groups improved after care, and the ESCA scores of the RG after care were evidently higher than those of the CG (P < 0.05) (Figure 2).
Figure 2.
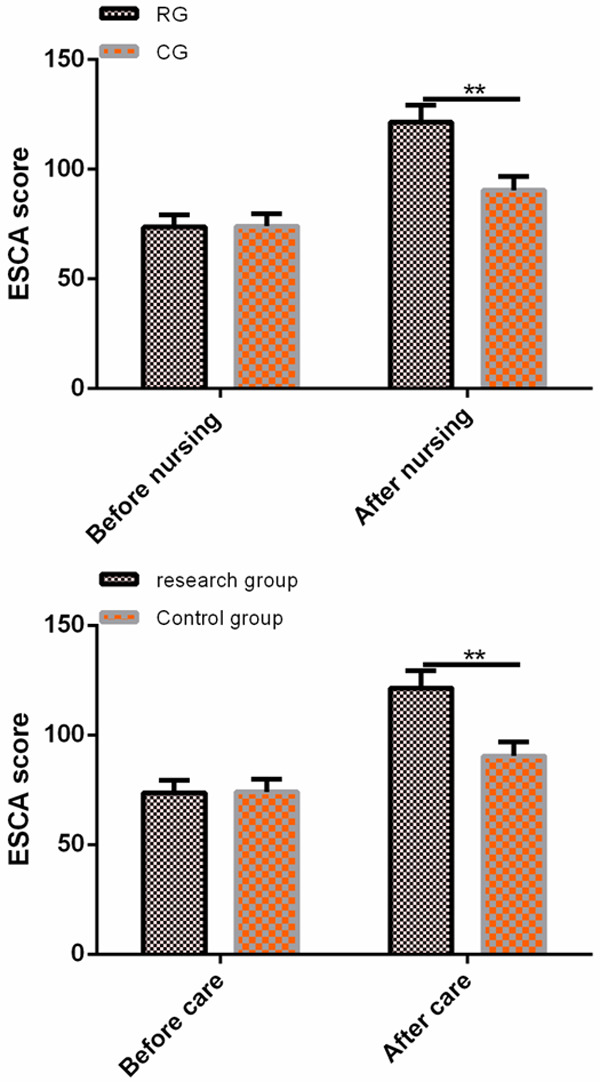
Comparison of ESCA scores between the two groups before and after care. There was no significant difference in ESCA scores between the two groups before care (P > 0.05), but the ESCA scores of the RG after care were evidently higher than those of the CG. Note: *indicates compared with before nursing, P < 0.05; **indicates compared with the control group, P < 0.01.
Comparison of medication compliance between the two groups of patients after care
The total compliance rate of patients in the RG after care was 96.08%, while that in the CG was 85.88%. The total compliance rate of patients in the RG was evidently higher than that in the CG (P < 0.05) (Table 4).
Table 4.
Comparison of medication compliance between the two groups after care [n (%)]
| Group | n | Complete compliance | Partial compliance | Non-compliance | Total compliance rate |
|---|---|---|---|---|---|
| RG | 102 | 73 (71.57) | 25 (24.51) | 4 (3.92) | 98 (96.08) |
| CG | 85 | 31 (36.47) | 42 (49.41) | 12 (14.12) | 73 (85.88) |
| χ2 | - | - | - | - | 6.160 |
| P | - | - | - | - | 0.013 |
Comparison of PSQI scores between the two groups before and after care
There was no significant difference in PSQI scores between the two groups before care (P > 0.05). After care, the PSQI scores of the two groups were improved, and the PSQI scores of the RG after care were evidently lower than those of the CG (P < 0.05) (Table 5).
Table 5.
Comparison of PSQI scores between the two groups before and after care (mean ± SD)
| Group | n | PSQI score | |
|---|---|---|---|
|
| |||
| Before nursing | After nursing | ||
| RG | 102 | 13.54±1.45 | 5.64±0.24 |
| CG | 85 | 13.32±1.48 | 9.35±0. 51 |
| t | - | 1.023 | 65.320 |
| P | - | 0.307 | < 0.001 |
Comparison of GQLI scores between the two groups before and after care
There was no significant difference in psychological function, physical functioning, material life and social functioning between the two groups before care (P > 0.05). After care, the GQLI scores of the two groups were improved, and the scores in the RG after care were evidently higher than those in the CG (P < 0.05) (Table 6).
Table 6.
Comparison of GQLI scores between the two groups before and after care (mean ± SD)
| Group | n | Psychological function | Physical functioning | Material life | Social functioning | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||
| Before nursing | After nursing | Before nursing | After nursing | Before nursing | After nursing | Before nursing | After nursing | ||
| RG | 102 | 56.58±5.23 | 72.36±7.03 | 56.43±5.21 | 72.73±7.04 | 58.94±5.73 | 74.37±7.19 | 50.38±4.79 | 71.93±7.84 |
| CG | 85 | 56.83±5.37 | 63.79±6.38 | 56.27±5.16 | 63.38±6.71 | 58.47±5.61 | 65.28±6.53 | 50.36±4.77 | 60.64±6.27 |
| t | - | 0.322 | 0.654 | 0.210 | 9.237 | 0.563 | 8.973 | 0.028 | 10.720 |
| P | - | 0.748 | < 0.001 | 0.834 | < 0.001 | 0.574 | < 0.001 | 0.977 | < 0.001 |
Comparison of nursing satisfaction between the two groups
After care, the scores of timeliness of service, standardization of management, service attitude, hospitalization environment and comprehensive quality of nursing staff in the RG were evidently higher than those in the CG (P < 0.05) (Table 7).
Table 7.
Comparison of nursing satisfaction between the two groups [mean ± SD]
| Group | n | Timeliness of service | Management standardization | Service attitude | Hospitalization environment | Comprehensive quality of nursing staff |
|---|---|---|---|---|---|---|
| RG | 102 | 25.95±2.24 | 24.23±2.46 | 13.96±2.15 | 14.65±2.23 | 10.53±0.86 |
| CG | 85 | 20.21±2.16 | 19.16±2.33 | 10.64±2.11 | 11.86±2.19 | 7.45±0.68 |
| t | - | 17.730 | 14.370 | 10.600 | 8.589 | 26.770 |
| P | - | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Discussion
Cancer pain is a kind of complex and chronic pain, which is mainly caused by severe pain in patients’ bodies when cancer develops to advanced stage, thus greatly weakening the survival will of cancer patients [21,22]. As the compression and direct invasion of tumor will directly cause visceral pain, the pain caused by the treatment of tumor will physiologically affect the normal activities and sleep of patients, and also reduce the appetite of patients [23,24]. Moreover, studies have shown that cancer patients are psychologically troubled in the treatment process, which leads to a series of psychological obstacles in patients, resulting in a decrease in the therapeutic effect [25]. Therefore, it is of great significance to strengthen nursing intervention for patients with cancer pain to improve their psychological status and reduce pain degree.
In this study, we used primary nursing to intervene the pain degree, medication compliance, psychological status and quality of life of elderly cancer patients, and found that the patients’ condition improved obviously after care. In the research of Cope et al. [26], giving personalized care to elderly cancer pain patients can effectively improve the pain control of patients, and improve the patients’ awareness of diseases and medication compliance. This is similar to the result of this study, which showed that the total pain relief rate of the patients in the RG was evidently higher than that in the CG after nursing, indicating that primary nursing intervention could find out the patients’ wrong medication ideas and methods in time and correct them, thus improving the pain relief rate of the patients. It also showed that effective nursing intervention can effectively reduce patients’ pain, relieve disease symptoms and promote rehabilitation. Some studies have shown that [27] many cancer pain patients have psychological distress symptoms such as anxiety and depression, and these adverse psychological symptoms may lead to a decline in the patient’s ability to bear the burden of disease, and also prolong the patient’s hospitalization time, resulting in a decline in the quality of life of patients and a significant increase in suicide risk. However, after effective nursing intervention in this study, the scores of SAS and SDS in the research group were significantly lower than those in the control group, which indicated that the primary nursing could effectively eliminate the psychological burden caused by treatment, keep the patients optimistic in the treatment process, and improve the curative effect, thus improving the patients’ ability to tolerate diseases and their rehabilitation. Previous studies have shown that most elderly patients have higher self-management and medication compliance during hospitalization due to the timely delivery of medicines and the guidance and supervision of patients’ medication. However, due to the lack of medication supervision by medical staff after discharge, as time goes by, most patients will gradually forget the medical staff’s instructions, resulting in lower medication compliance and behaviors such as not taking medicines on time or privately changing medicines, resulting in lower pain treatment effect [28,29]. The results of this study showed that GSES, ESCA scores and medication compliance of patients in the RG were evidently higher than those in the CG after nursing, indicating that regular follow-up after discharge can supervise and urge patients to take painkillers regularly, thus improving their self-efficacy, self-care ability and medication compliance.
Sleep of patients with advanced cancer is often disturbed, especially those receiving opioid therapy, which often leads to the poor improvement of pain and overall score of sleep quality [30]. Other studies showed that [31] after giving psychological education intervention to cancer patients, the symptoms of sleep disorder, anxiety and depression were obviously reduced. This is similar to the result of this study, which showed that the PSQI scores of patients in the RG were evidently lower than those in the CG after nursing, indicating that the psychological state, medication compliance and cancer pain of patients were evidently improved after giving the primary nursing, thus improving patients’ confidence in treatment and improving their sleep quality. Previous studies have shown that [32,33] the cancer pain of patients is aggravated with the metastasis and enlargement of their tumors, thus affecting the normal quality of life of patients. The results of this study showed that the scores of psychological function, physical function, material life and social function in GQLI score of patients in the RG after nursing were evidently higher than those in the CG, indicating that the primary nursing can improve the cancer pain, psychological state and curative effect of patients and improve their quality of life. We further compared the satisfaction of the two groups of patients after nursing and found that the satisfaction of the RG was higher than that of the CG, indicating that the patients had high recognition of the primary nursing, which provided a powerful reference for the follow-up clinical application.
To sum up, the implementation of primary nursing for elderly patients with cancer pain can not only effectively relieve their cancer pain, but also improve their bad psychological state and medication compliance, thus contributing to the improvement of patients’ quality of life. However, there is still room for improvement in this study. For example, we can analyze the risk factors affecting the poor prognosis of elderly cancer patients, which will help nurses to know which risk factors need to pay more attention. In the future, supplementary research will be carried out gradually from the above perspectives.
Acknowledgements
Construction of Anning and Nursing Program Based on the Symptom Group of Patients with Advanced Lung Cancer (ZY201703008).
Disclosure of conflict of interest
None.
References
- 1.Alizadeh-Khoei M, Sharifi F, Akbari ME, Fadayevatan R, Haghi M. Iranian brief pain inventory: validation and application in elderly people with cancer pain. J Pain Symptom Manage. 2017;54:563–569. doi: 10.1016/j.jpainsymman.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Ahmedzai SH, Bautista MJ, Bouzid K, Gibson R, Gumara Y, Hassan AAI, Hattori S, Keefe D, Kraychete DC, Lee DH, Tamura K, Wang JJ CAncer Pain management in Resource-limited settings (CAPER) Working Group. Optimizing cancer pain management in resource-limited settings. Support Care Cancer. 2019;27:2113–2124. doi: 10.1007/s00520-018-4471-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu Y, Lin B. Application of quality control circle in the treatment of moderate cancer pain in inpatients. Jpn J Clin Oncol. 2020;50:581–585. doi: 10.1093/jjco/hyz214. [DOI] [PubMed] [Google Scholar]
- 4.Paice JA. Cancer pain management and the opioid crisis in America: how to preserve hard-earned gains in improving the quality of cancer pain management. Cancer. 2018;124:2491–2497. doi: 10.1002/cncr.31303. [DOI] [PubMed] [Google Scholar]
- 5.Zheng RJ, Fu Y, Zhu J, Xu JP, Xiang QF, Chen L, Zhong H, Li JY, Yu CH. Long-term low-dose morphine for patients with moderate cancer pain is predominant factor effecting clinically meaningful pain reduction. Support Care Cancer. 2018;26:4115–4120. doi: 10.1007/s00520-018-4282-2. [DOI] [PubMed] [Google Scholar]
- 6.Lantheaume S, Montagne M, Shankland R. Intervention focused on resources to reduce anxiety and depression disorders in cancer patients: a pilot study. Encephale. 2020;46:13–22. doi: 10.1016/j.encep.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Pilania M, Yadav V, Bairwa M, Behera P, Gupta SD, Khurana H, Mohan V, Baniya G, Poongothai S. Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: a systematic review and meta-analysis. BMC Public Health. 2019;19:832. doi: 10.1186/s12889-019-7136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabrielsson S, Savenstedt S, Olsson M. Taking personal responsibility: nurses’ and assistant nurses’ experiences of good nursing practice in psychiatric inpatient care. Int J Ment Health Nurs. 2016;25:434–443. doi: 10.1111/inm.12230. [DOI] [PubMed] [Google Scholar]
- 9.Manuel J, Crowe M. Clinical responsibility, accountability, and risk aversion in mental health nursing: a descriptive, qualitative study. Int J Ment Health Nurs. 2014;23:336–343. doi: 10.1111/inm.12063. [DOI] [PubMed] [Google Scholar]
- 10.Bauerle K, Feicke J, Scherer W, Sporhase U, Bitzer EM. Evaluation of a standardized patient education program for inpatient asthma rehabilitation: impact on patient-reported health outcomes up to one year. Patient Educ Couns. 2017;100:957–965. doi: 10.1016/j.pec.2016.11.023. [DOI] [PubMed] [Google Scholar]
- 11.Nail LM, Greene D, Jones LS, Flannery M. Nursing care by telephone: describing practice in an ambulatory oncology center. Oncol Nurs Forum. 1989;16:387–395. [PubMed] [Google Scholar]
- 12.Allen CA, Ivester JR Jr. Ketamine for pain management-side effects & potential adverse events. Pain Manag Nurs. 2017;18:372–377. doi: 10.1016/j.pmn.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 13.Hochstenbach LM, Zwakhalen SM, Courtens AM, van Kleef M, de Witte LP. Feasibility of a mobile and web-based intervention to support self-management in outpatients with cancer pain. Eur J Oncol Nurs. 2016;23:97–105. doi: 10.1016/j.ejon.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Kuznetsova SM, Kudritskaia OV, Kasumov C. Bioelectrical activity of the brain and aging (a review) Zh Nevropatol Psikhiatr Im S S Korsakova. 1988;88:128–133. [PubMed] [Google Scholar]
- 15.Wang Y, Tang H, Guo Q, Liu J, Liu X, Luo J, Yang W. Effects of intravenous patient-controlled sufentanil analgesia and music therapy on pain and hemodynamics after surgery for lung cancer: a randomized parallel study. J Altern Complement Med. 2015;21:667–672. doi: 10.1089/acm.2014.0310. [DOI] [PubMed] [Google Scholar]
- 16.Wang X, Lai Q, Tian Y, Zou L. Effect of evidence-based nursing intervention on upper limb function in postoperative radiotherapy patients with breast cancer. Medicine (Baltimore) 2020;99:e19183. doi: 10.1097/MD.0000000000019183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fueyo-Diaz R, Magallon-Botaya R, Gascon-Santos S, Asensio-Martinez A, Palacios-Navarro G, Sebastian-Domingo JJ. The effect of self-efficacy expectations in the adherence to a gluten free diet in celiac disease. Psychol Health. 2020;35:734–749. doi: 10.1080/08870446.2019.1675658. [DOI] [PubMed] [Google Scholar]
- 18.Raffaele B, Biagioli V, Cirillo L, De Marinis MG, Matarese M. Cross-validation of the Self-care Ability Scale for Elderly (SASE) in a sample of Italian older adults. Scand J Caring Sci. 2018;32:1398–1408. doi: 10.1111/scs.12585. [DOI] [PubMed] [Google Scholar]
- 19.Pilz LK, Keller LK, Lenssen D, Roenneberg T. Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep. 2018;41 doi: 10.1093/sleep/zsy029. [DOI] [PubMed] [Google Scholar]
- 20.Ding Z, Chen Y, Jiang CQ, Wu YH, Zheng KY, Qin QB, Qian Q. Total colonic exclusion plus side to side ileorectal antiperistaltic anastomosis in the treatment for elderly patients with slow transit constipation. Zhonghua Wei Chang Wai Ke Za Zhi. 2013;16:637–640. [PubMed] [Google Scholar]
- 21.Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, Citron M, Constine LS, Cooper A, Glare P, Keefe F, Koyyalagunta L, Levy M, Miaskowski C, Otis-Green S, Sloan P, Bruera E. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J. Clin. Oncol. 2016;34:3325–3345. doi: 10.1200/JCO.2016.68.5206. [DOI] [PubMed] [Google Scholar]
- 22.Higashibata T, Tagami K, Miura T, Okizaki A, Watanabe YS, Matsumoto Y, Morita T, Kinoshita H. Usefulness of painDETECT and S-LANSS in identifying the neuropathic component of mixed pain among patients with tumor-related cancer pain. Support Care Cancer. 2020;28:279–285. doi: 10.1007/s00520-019-04819-9. [DOI] [PubMed] [Google Scholar]
- 23.Vissers KC, Besse K, Wagemans M, Zuurmond W, Giezeman MJ, Lataster A, Mekhail N, Burton AW, van Kleef M, Huygen F. Pain in patients with cancer. Pain Pract. 2011;11:453–475. doi: 10.1111/j.1533-2500.2011.00473.x. [DOI] [PubMed] [Google Scholar]
- 24.Nie J, Liu S, Di L. Cancer pain and its influence on cancer patients’ quality of life. Zhonghua Zhong Liu Za Zhi. 2000;22:432–434. [PubMed] [Google Scholar]
- 25.Moussas GI, Papadopoulou AG. Substance abuse and cancer. Psychiatriki. 2017;28:234–241. doi: 10.22365/jpsych.2017.283.234. [DOI] [PubMed] [Google Scholar]
- 26.Cope DG. Cancer pain management considerations in older adults. Semin Oncol Nurs. 2019;35:274–278. doi: 10.1016/j.soncn.2019.04.008. [DOI] [PubMed] [Google Scholar]
- 27.Arora A, Saini SK, Nautiyal V, Verma SK, Gupta M, Kalra BP, Ahmad M. Cancer pain, anxiety, and depression in admitted patients at a tertiary care hospital: a prospective observational study. Indian J Palliat Care. 2019;25:562–566. doi: 10.4103/IJPC.IJPC_4_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green CF, Burgul K, Armstrong DJ. A study of the use of medicine lists in medicines reconciliation: please remember this, a list is just a list. Int J Pharm Pract. 2010;18:116–121. [PubMed] [Google Scholar]
- 29.Jung SH, Lee OS, Kim HS, Park CS, Lee HJ, Kwon KH, Lee HY. Medication adherence improvement by using administration timing simplification protocol (ATSP) in cardiovascular disease patients. J Atheroscler Thromb. 2017;24:841–852. doi: 10.5551/jat.36335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jakobsen G, Engstrom M, Fayers P, Hjermstad MJ, Kaasa S, Kloke M, Sabatowski R, Klepstad P. Sleep quality with WHO Step III opioid use for cancer pain. BMJ Support Palliat Care. 2019;9:307–315. doi: 10.1136/bmjspcare-2017-001399. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen LT, Alexander K, Yates P. Psychoeducational intervention for symptom management of fatigue, pain, and sleep disturbance cluster among cancer patients: a pilot quasi-experimental study. J Pain Symptom Manage. 2018;55:1459–1472. doi: 10.1016/j.jpainsymman.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 32.Wu XP, Yang YP, She RX, Xing ZM, Chen HW, Zhang YW. microRNA-329 reduces bone cancer pain through the LPAR1-dependent LPAR1/ERK signal transduction pathway in mice. Ther Adv Med Oncol. 2019;11:1758835919875319. doi: 10.1177/1758835919875319. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 33.Hajj A, Halepian L, Osta NE, Chahine G, Kattan J, Rabbaa Khabbaz L. OPRM1 c. 118A>G polymorphism and duration of morphine treatment associated with morphine doses and quality-of-life in palliative cancer pain settings. Int J Mol Sci. 2017;18:669. doi: 10.3390/ijms18040669. [DOI] [PMC free article] [PubMed] [Google Scholar]


