Abstract
Objective: The purpose of this study is to explore the effect of fine nursing interventions on the clinical efficacy of acute alcoholism patients (AA). Methods: A total of 100 patients with AA were included in the study. Among them, 51 patients who underwent fine nursing intervention were assigned to the research group (RG), and the remaining 49 patients were treated with routine nursing intervention and were assigned to the control group (CG). The nursing efficacy, the recovery times (consciousness and limb movement), the incidences of adverse events, the nursing compliance, the psychological states (the Symptom Checklist 90 and SCL-90 scores), and the nursing satisfaction levels were observed and compared between the two groups. Results: Compared with the CG, the nursing efficacy, the compliance, and the nursing satisfaction levels in the RG were markedly higher, while the consciousness and limb movement recovery times were significantly shorter; moreover, the RG presented a significantly lower incidence of adverse events and SCL-90 scores than the CG. Conclusion: While validly relieving the clinical symptoms and reducing the incidence of adverse events, fine nursing can effectively promote the recovery of patients with AA, and improve their treatment compliance and psychological states.
Keywords: Fine nursing, acute alcoholism, clinical symptoms, adverse events, prevention
Introduction
Alcoholism, also known as drunkenness, is commonly seen in the clinical emergency department, with an increasing incidence [1,2]. There are two types of alcoholism in clinical practice: acute alcoholism (AA) and chronic alcoholism. The damage caused by chronic alcoholism is cumulative and slow, while acute alcoholism develops rapidly and can be fatal in severe cases [3,4]. AA is an acute central nervous system inhibitory disease mainly derived from excessive drinking or high pressure, which can lead to poor compliance, as well as undesirable manifestations such as mania and fragility [5-7]. If left unattended without timely treatment and nursing intervention, it may aggravate the condition and endanger the cardiovascular and respiratory function of patients, posing a serious threat to their life safety [8,9]. The main clinical symptom of AA patients is restlessness, which may lead to a series of adverse events such as falling out of bed and tumbling; therefore, nursing intervention is particularly important and necessary for patients [10], and exploring new nursing interventions carries huge implications in ameliorating the adverse clinical outcomes of AA patients.
Fine nursing is a patient-centered innovative nursing model based on routine care, and it aims to improve patients’ satisfaction by strengthening nursing service awareness and providing fine and considerate targeted nursing services [11-13]. At present, this nursing model has been applied to the postpartum recovery of parturients with natural delivery, the growth of very low birth weight infants, and emergency post-care after percutaneous coronary intervention [14-16]. AA, a disease commonly seen in the emergency department, is characterized by rapid onset, multiple potential complications and poor patient compliance. The application of fine nursing may be beneficial to better deal with the clinical symptoms of patients, improve their compliance and mental state, and reduce the incidence of complications [17]. Meanwhile, fine nursing is a challenge for the nursing staff, requiring them to pay more attention to the patient’s psychological status, physical factors, and environmental conditions before, during, and after treatment [14].
Currently, the application of fine nursing in AA is difficult to track in the existing literature. The novelty of this study mainly lies in comparing it with conventional nursing, and verifying its effectiveness in the treatment of AA from various aspects such as nursing efficacy, recovery, safety, compliance, psychological state, and nursing satisfaction.
Materials and methods
General information
This is a retrospective study approved by the Ethics Committee of the General Hospital of the First Affiliated Hospital of Soochow University (approval No. Add-882-167). The subjects or their guardians signed the informed consent forms after being fully informed of the purpose and process of the study. A total of 100 acute alcoholism patients (AA) admitted to the General Hospital of the First Affiliated Hospital of Soochow University from January 1, 2019 to December 31, 2020 were recruited as the study cohort. Among them, 51 patients treated with fine nursing intervention were assigned to the research group (RG) and the remaining 49 patients treated with routine nursing intervention were included in the control group (CG). PASS software (Beijing HuanZhongRuiChi Technology Co., Ltd., China) was used to calculate the sample size based on the nursing efficacy (one of the primary outcome measures), in which the significance level was set as α (α=0.05) and the power of test as 1-β (β=80%). Diagnostic criteria for the AA [18]: patients who engaged in excessive drinking before alcoholism (a blood alcohol concentration >11 mmol/L), with a strong odor of alcohol in their breath and vomit, and who presented with an abnormally excited central nervous system as well as symptoms such as coma and ataxia. Exclusion criteria: patients in a coma caused by other causes such as underlying diseases, metabolic encephalopathy, cerebrovascular diseases; patients with malignant tumors or severe organic diseases; patients with brain organic diseases; patients with mental illnesses or cognitive and communication disorders; patients with other drug poisoning. The inclusion criteria were applicable to both groups.
Nursing methods
According to each patient’s condition, patients with mild alcoholism were given supportive treatments such as antiemetics, gastric mucosal protection, and cerebral edema alleviation, using vitamin C, vitamin B6, cimetidine and other drugs. Patients with moderate alcoholism were supplemented with awakening drugs, such as Xingnaojing, Shexiang injections and Dimeflini. Those with severe alcoholism were also given gastric lavage, catheterization, reduction of intracranial pressure and mannitol treatment.
The patients in the CG underwent routine nursing intervention. After admission, each patient’s condition was closely monitored and any abnormalities were handled effectively. In addition, the changes in the patients’ physical signs such as their vital signs and consciousness were observed. In the case of symptoms like abdominal pain and shock, the gastric lavage was stopped immediately for treatment.
Fine nursing was implemented in the RG in addition to the nursing administered to the CG [10,11,19]. (1) The patient’s vital signs were closely observed. The patients’ poisoning symptoms were observed, and their clinical symptoms, vital signs, consciousness and pupils were monitored. In addition, the alcohol concentration was determined to quickly judge the patient’s condition and formulate targeted rescue measures. (2) Fine nursing. The comatose patients with trauma complications had their vital signs stabilized as soon as possible, venous access established, and they were rescued in the resuscitation area with naloxone. The changes in their consciousness levels and pupils were observed. For those also suffering from trauma, bandages and hemostasis, as well as debridement and suturing were performed immediately. All the patients were treated with emesis, gastric lavage, and oxygen inhalation. Meanwhile, CT, debridement and X-rays were performed to rule out trauma in order to avoid an aggravation of the disease. For the patients without trauma during lethargy, their vital signs were stabilized to prevent the occurrence of complications such as respiratory failure, circulatory failure and inhalation pneumonia. Oxygen was given to the patients according to their symptoms to keep their respiratory tracts unobstructed. When necessary, indwelling catheters were placed and their oral and respiratory tracts were cleaned to prevent the occurrence of complications. For the ataxia patients with symptoms such as gait staggering, slurred speech, and nausea and vomiting, safety nursing management was applied to prevent falls and other adverse events. In addition, sundries on the ground were removed, and restraint belts were used selectively according to the circumstances. Furthermore, the nursing staff strengthened the monitoring of the patients. The intravenous indwelling needles were monitored to observe whether the patients had swelling in their local joints and restraints, and the indwelling needles were properly fixed to prevent needle removal. The patients during the excitement period were prone to self-injury and other injuries, so appropriate sedatives were given and the emotional changes in the patients were observed. In the case of self-injury or other injuries, emergency plans were carried out immediately. (3) Psychological nursing. After diagnosis, the nursing staff attended to the changes in the patient’s psychological states, explained the occurrence of the diseases to the patients, and actively communicated with the patient and his/her family members to eliminate their anxiety or depression.
Outcome measures
The nursing efficacy was evaluated and compared between the two groups. Markedly effective was considered if the patient recovered consciousness within 3 hours and was in a conscious state, with the complete disappearance of the main clinical symptoms. Effective indicated that the patient’s consciousness was basically recovered within 6 h, and the vital signs were stable and tended to be normal. Ineffective indicated that the patient’s consciousness had not been recovered at all within 6 hours, and the main clinical symptoms were not improved or were even aggravated. The nursing efficiency was the rescue success rate, and the calculation method was the percentage of the sum of the effective and effective patients in the total number of patients.
The patient recovery, the incidences of adverse events, the compliance, the psychological states, and the nursing satisfaction levels after the nursing were observed and compared between the two groups. The patients’ recovery was mainly evaluated from the time of consciousness and limb movement recovery, while the main adverse events included falling out of bed, tumbling, and asphyxia. With regard to compliance, it was mainly scored by the nurses in the emergency department after the nursing for patients’ cooperation and anxiety during the nursing. The scale has a score ranging from 0 to 10 points, with less than 2 being poor, 3-4 being fair, 5-7 being good, and 8 or more being excellent [the compliance rate = (excellent + good + fair) cases/total cases]. After the nursing, the mental states of the patients were evaluated using Symptom Checklist 90 (SCL-90) [20] from 9 dimensions of anxiety, depression, paranoid, hostility, terror, interpersonal sensitivity, obsessive-compulsive symptoms, psychotic and somatization. Each item scores 0-5 points, with 1 being asymptomatic, 2 being mild, 3 being moderate, 4 being severe, and 5 being extremely severe. At the time of discharge, the nursing satisfaction questionnaire was distributed to the patients to evaluate their satisfaction (dissatisfied, satisfied or very satisfied) with the nursing service.
Statistical analysis
Both the data analysis and picture rendering were performed using GraphPad Prism 6 (GraphPad Software, San Diego, USA). The count data were expressed as the number of cases/percentages (n/%), and the measurement data were described as the mean ± SME. Chi-square tests were used to compare the count data among the groups, and continuous correction chi-square tests were used when the theoretical frequency in the chi-square test was less than 5. For the measurement data, the inter-group comparisons were performed using independent sample t-tests, and the intra-group comparisons were conducted using paired t-test. When P<0.05, a difference was considered statistically significant.
Results
Baseline data
There were no significant differences in terms of gender, age, average age, alcohol consumption, admission time, educational level, drinking history, residence, or marital status between the control group (CG) and the research group (RG) (P>0.05; Table 1).
Table 1.
Baseline data of the CG and the RG [n (%), mean ± SD]
| Variable | n | CG (n=49) | RG (n=51) | χ2/t | P |
|---|---|---|---|---|---|
| Gender | 0.017 | 0.896 | |||
| Male | 70 | 34 (69.39) | 36 (70.59) | ||
| Female | 30 | 15 (30.61) | 15 (29.41) | ||
| Age (years) | 2.529 | 0.112 | |||
| <40 | 41 | 24 (48.98) | 17 (33.33) | ||
| ≥3 | 59 | 25 (51.02) | 34 (66.67) | ||
| Average age (years) | 100 | 45.57±10.02 | 47.19±11.25 | 0.759 | 0.450 |
| Alcohol consumption (L) | 3.628 | 0.163 | |||
| <0.5 | 17 | 10 (20.41) | 7 (13.73) | ||
| 0.5-1 | 68 | 29 (59.18) | 39 (76.47) | ||
| >1 | 15 | 10 (20.41) | 5 (9.80) | ||
| Admission time (h) | 5.684 | 0.058 | |||
| <1 | 24 | 12 (24.49) | 12 (23.53) | ||
| 1-3 | 55 | 26 (53.06) | 29 (56.86) | ||
| >3 | 21 | 11 (22.45) | 10 (19.61) | ||
| Educational level | 1.966 | 0.579 | |||
| Primary school | 18 | 8 (16.33) | 10 (19.61) | ||
| High school | 36 | 15 (30.61) | 21 (41.18) | ||
| College or university | 30 | 17 (34.69) | 13 (25.49) | ||
| Bachelor’s degree or above | 16 | 9 (18.37) | 7 (13.72) | ||
| Drinking history | 0.519 | 0.471 | |||
| No | 32 | 14 (28.57) | 18 (35.29) | ||
| Yes | 68 | 35 (71.43) | 33 (64.71) | ||
| Residence | 0.323 | 0.570 | |||
| Urban | 62 | 29 (59.18) | 33 (64.71) | ||
| Rural | 38 | 20 (40.82) | 18 (35.29) | ||
| marital status | 2.301 | 0.129 | |||
| Unmarried | 36 | 14 (28.57) | 22 (43.14) | ||
| Married | 64 | 35 (71.43) | 29 (56.86) |
The nursing efficacy in the two groups
The nursing efficacy in RG was markedly higher than it was in CG (P<0.05; Table 2).
Table 2.
The nursing efficacy in the CG and the RG [n (%)]
| Group | n | Cured | Effective | Ineffective | Effective rate (%) |
|---|---|---|---|---|---|
| CG | 49 | 16 (32.65) | 21 (42.86) | 12 (24.49) | 75.51 |
| RG | 51 | 28 (54.90) | 21 (41.18) | 2 (3.92) | 96.08 |
| χ2 value | - | 10.432 | 8.781 | ||
| P value | - | 0.005 | 0.003 | ||
Recovery of the patients in the two groups
We assessed the patients’ recovery using the recovery times of consciousness and the body movements. The results showed that the recovery times of consciousness and the limb movements in RG were markedly shorter than they were in CG (P<0.05; Figure 1).
Figure 1.
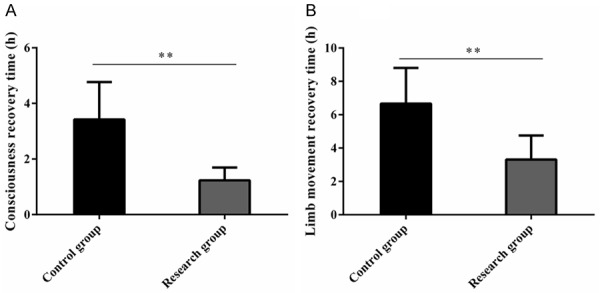
Recovery of the CG and the RG. A. The consciousness recovery times in the RG were markedly shorter than they were in the CG. B. The limb movement recovery times in the RG were markedly shorter than they were in CG. Note: **indicates P<0.01.
Incidence of adverse events in the two groups
We compared the incidences of adverse events such as falling out of bed, tumbling, and asphyxia between the CG and the RG. The data showed that the incidence of asphyxia and the total incidence of adverse events in RG were markedly lower than they were in the CG (P<0.05; Table 3).
Table 3.
The incidence of adverse events in the two groups [n (%)]
| Category | CG (n=49) | RG (n=51) | χ2 value | P value |
|---|---|---|---|---|
| Falling out of bed | 8 (16.33) | 4 (7.84) | 1.703 | 0.192 |
| Tumbling | 6 (12.24) | 2 (3.92) | 2.352 | 0.125 |
| Asphyxia | 8 (16.33) | 0 (0.00) | 9.051 | 0.003 |
| Total | 22 (44.90) | 6 (11.76) | 13.608 | <0.001 |
The patient compliance in the two groups
The clinical compliance rate of the patients in the RG was markedly higher than it was in the CG (P<0.05; Table 4).
Table 4.
The compliance of the two groups before and after the treatment [n (%)]
| Group | Excellent | Good | Fair | Poor | Compliance rate |
|---|---|---|---|---|---|
| CG (n=49) | 20 (40.82) | 10 (20.41) | 11 (22.45) | 8 (16.33) | 41 (83.67) |
| RG (n=51) | 27 (52.94) | 12 (23.53) | 10 (19.61) | 2 (3.92) | 49 (96.08) |
| χ2 value | 4.834 | 4.273 | |||
| P value | 0.184 | 0.039 | |||
The psychological states of the patients in the two groups
We also evaluated the psychological states of the patients in the two groups using the SCL-90 from 9 dimensions of anxiety, depression, paranoid, hostility, terror, interpersonal sensitivity, obsessive-compulsive symptoms, psychosis, and somatization. The data showed that the psychological state scores of the patients in RG were markedly lower than those in CG, and the differences were statistically significant (P<0.05; Figure 2).
Figure 2.
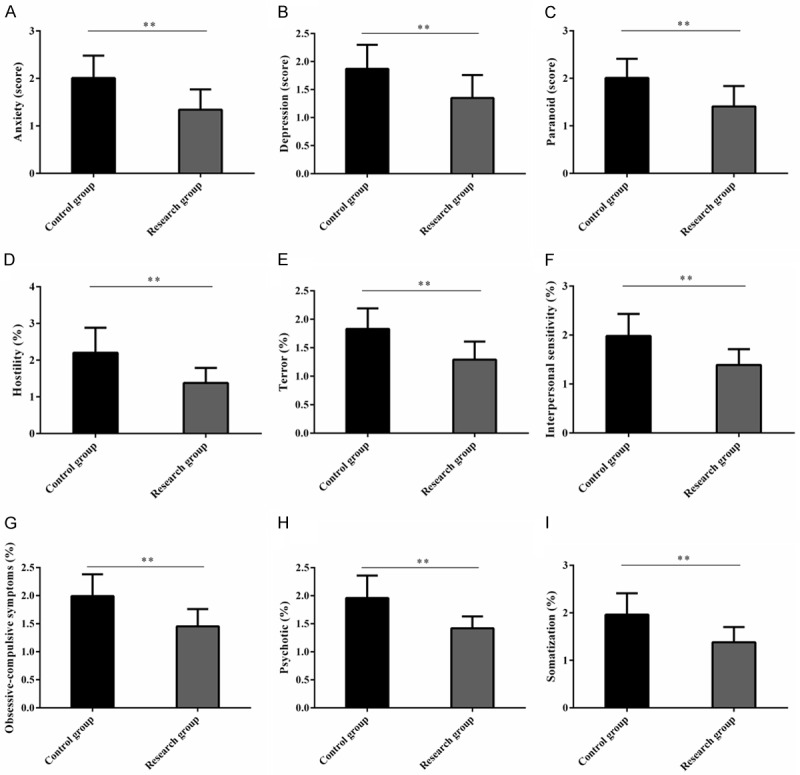
The psychological states of the patients in the two groups. A. The anxiety scores of the RG were markedly lower than they were in the CG. B. The depression scores in the RG were markedly lower than they were in the CG. C. The paranoid scores in the RG were markedly lower than they were in CG. D. The hostility scores in the RG were markedly lower than they were in the CG. E. The terror scores in the RG were markedly lower than they were in the CG. F. The interpersonal sensitivity scores in the RG were markedly lower than they were in the CG. G. The obsessive-compulsive symptom scores in the RG were markedly lower than they were in the CG. H. The psychotic scores in the RG were markedly lower than they were in the CG. I. The somatization scores in the RG were markedly lower than they were in the CG. Note: **indicates P<0.01.
The nursing satisfaction levels of patients in the two groups
The nursing satisfaction levels between CG and RG were compared. The data showed that the total nursing satisfaction in the RG was significantly higher than it was in the CG (P<0.05; Table 5).
Table 5.
The nursing satisfaction levels of the patients in the two groups [n (%)]
| Category | CG (n=49) | RG (n=51) | χ2 value | P value |
|---|---|---|---|---|
| Dissatisfied | 11 (22.45) | 3 (5.88) | 10.522 | 0.005 |
| Satisfied | 20 (40.82) | 14 (27.45) | ||
| Very satisfied | 18 (36.73) | 34 (66.67) | ||
| Total satisfaction | 38 (77.55) | 48 (94.12) | 5.697 | 0.017 |
Discussion
Acute alcoholism (AA) usually occurs in people who drink excessively in a short period of time. Excessive alcohol entering the body will overload the metabolic capacity of the liver, and enhance the activity of the endorphins for their penetration into the cerebral cortex, thus inhibiting the normal operation of the nervous system [21]. As one of the main causes of cirrhosis and liver failure worldwide, AA is characterized by excitement, dizziness, irritability, impaired cognitive and motor functions, as well as coma [22]. It may also cause trauma and damage to the function of multiple organs, especially renal dysfunction [23]. In order to reduce the potential harm of AA to the human body, studying its nursing model carries huge implications for improving the medical experience of patients during treatment.
Fine nursing has been proved to be effective in various medical scenarios. For example, Park and his colleagues revealed that the application of this nursing model improved the physical state of middle-aged and elderly people in nursing homes to varying degrees [24]. Another paper reported that the continuous nursing model developed based on the concept of fine nursing exerted positive effects on improving treatment compliance, mitigating negative emotions and reducing the complication rate in patients undergoing coronary artery bypass grafting [25]. In this study, the patients in the research group (RG) were given fine nursing, while those in the control group (CG) they were treated with routine nursing. The data showed that the nursing efficacy of RG was significantly higher than it was in the CG, which suggests that fine nursing is beneficial for improving the nursing efficacy of AA patients. Starting from patients, fine nursing takes into account the adverse situations that patients may encounter in all aspects, and makes emergency plans in advance, so that emergency situations can be dealt with promptly and effectively, and it is also a favorable factor for achieving high efficacy [26]. The patient recovery in the two groups was evaluated from the recovery of consciousness and limb movement. It was found that the recovery of the patients in the RG was markedly better than the patient recovery in the CG, indicating that fine nursing is beneficial for facilitating patient recovery. The advantage of fine nursing lies in the initiative of nursing service, which is different from conventional nursing and a major reason for faster patient recovery [27,28]. In terms of safety, we found that the total incidence of adverse events (falling out of bed, tumbling, and asphyxia) in RG was significantly lower than it was in CG, indicating that the adverse events were better prevented under the intervention of fine nursing. Patients with AA are often unconscious during treatment, which may lead to accidents [29]. Fine nursing intervention can better deal with emergencies during treatment, and it can not only effectively prevent adverse events, it can also improve the nursing efficacy.
The emergency department where AA patients underwent treatment is the place with the most medical disputes and doctor-patient conflicts. The nursing team under fine nursing has excellent predictive thinking and keen observation skills, which can not only enhance doctor-patient cooperation through good communication with patients and their families, but it also enables the capacity to solve problems [30]. In order to better quantify the impact of fine nursing on AA patients, we evaluated the compliance and psychological states of the patients in the two groups. The data show that the clinical compliance of the patients in the RG was significantly higher than it was in the CG, suggesting that the patients had a higher degree of treatment cooperation under fine nursing intervention. In terms of psychological state, the Symptom Checklist 90 (SCL-90) scores of the RG were markedly lower than those of the CG, indicating that fine nursing was effective in calming the patients’ emotions. Under fine nursing, the nursing staff will pay extra attention to the patients’ emotional states, give tailored psychological counseling to those with bad emotions, and communicate with the patients’ families to understand the situation of the patients, which also explains the lower SCL-90 scores of the patients in the RG. Finally, the nursing satisfaction was investigated. Unsurprisingly, the nursing satisfaction levels in the RG were markedly higher than the nursing satisfaction levels in the CG, indicating that fine nursing is more popular and the nursing quality was highly recognized by the patients.
This study confirms that fine nursing can alleviate the clinical symptoms of patients with AA, improve their compliance and psychological states, and reduce the incidence of adverse events. However, there is still room for improvement. First of all, we can analyze the risk factors affecting the incidence of adverse events in patients with AA and further clarify the weight hierarchy of the various concerns in the care model. Second, we can supplement the impact of fine nursing on the quality of life and sleep quality of the patients with AA, which is conducive to further expanding the potential application advantages of fine nursing in AA patients. We will address these limitations in the future.
To sum up, with a high safety profile, fine nursing can improve nursing efficacy, compliance, psychological states, and the nursing satisfaction levels of patients while relieving the clinical symptoms of AA patients, so it is of high clinical application value and worthy of promotion.
Disclosure of conflict of interest
None.
References
- 1.Studer J, Gmel G, Bertholet N, Marmet S, Daeppen JB. Alcohol-induced blackouts at age 20 predict the incidence, maintenance and severity of alcohol dependence at age 25: a prospective study in a sample of young Swiss men. Addiction. 2019;114:1556–1566. doi: 10.1111/add.14647. [DOI] [PubMed] [Google Scholar]
- 2.Zhu Y, Lu H, Han J, Jiang H, Li S, Chen X, Lin P. Using of pre-hospital emergency resources by acute alcoholism patients in a hospital in Guangzhou: a data survey from 2009 to 2018. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31:1411–1415. doi: 10.3760/cma.j.issn.2095-4352.2019.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Du A, Dai X, Dong J, Liu J, Zhang Y, Fu P, Qin H, Li R, Zhang R. Effects of aminooxyacetic acid on hippocampal mitochondria in rats with chronic alcoholism: the analysis of learning and memory-related genes. J Integr Neurosci. 2019;18:451–462. doi: 10.31083/j.jin.2019.04.1119. [DOI] [PubMed] [Google Scholar]
- 4.Erokhin IuA, Paukov VS, Kirillov IuA. Causes of the people death from drunkenness and alcoholism. Arkh Patol. 2012;74:33–36. [PubMed] [Google Scholar]
- 5.Xu JF, Lu JJ, Cao Y, Wang W, Li HH, Chen JG, Wang F, Wu PF. Sulforaphane alleviates ethanol-mediated central inhibition and reverses chronic stress-induced aggravation of acute alcoholism via targeting Nrf2-regulated catalase expression. Neuropharmacology. 2020;176:108235. doi: 10.1016/j.neuropharm.2020.108235. [DOI] [PubMed] [Google Scholar]
- 6.Wang G, Li Z, Li M, Liu S, Shan T, Liu J, Zhang Y. Clinical therapeutic effect of naloxone combined with hemodialysis on acute severe alcoholism. Med Sci Monit. 2018;24:5363–5367. doi: 10.12659/MSM.908382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao W, Hu Y, Li C, Li N, Zhu S, Tan X, Li M, Zhang Y, Xu Z, Ding Z, Hu L, Liu Z, Sun J. Transplantation of fecal microbiota from patients with alcoholism induces anxiety/depression behaviors and decreases brain mGluR1/PKC epsilon levels in mouse. Biofactors. 2020;46:38–54. doi: 10.1002/biof.1567. [DOI] [PubMed] [Google Scholar]
- 8.Krishnamoorthy P, Kalla A, Figueredo VM. Cardiovascular events in alcoholic syndrome with alcohol withdrawal history: results from the national inpatient sample. Am J Med Sci. 2018;355:425–427. doi: 10.1016/j.amjms.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Jones AW, Holmgren P. Comparison of blood-ethanol concentration in deaths attributed to acute alcohol poisoning and chronic alcoholism. J Forensic Sci. 2003;48:874–879. [PubMed] [Google Scholar]
- 10.Littlejohn C, Holloway A. Nursing interventions for preventing alcohol-related harm. Br J Nurs. 2008;17:53–59. doi: 10.12968/bjon.2008.17.1.28062. [DOI] [PubMed] [Google Scholar]
- 11.Bove HM, Lisby M, Norlyk A. Do the carers care? A phenomenological study of providing care for patients suffering from alcohol use disorders. Nurs Inq. 2020;27:e12322. doi: 10.1111/nin.12322. [DOI] [PubMed] [Google Scholar]
- 12.Ng SM, Mariguddi S, Coward S, Middleton H. Paediatric community home nursing: a model of acute care. Br J Nurs. 2014;23:209–212. doi: 10.12968/bjon.2014.23.4.209. [DOI] [PubMed] [Google Scholar]
- 13.Jaiteh C, Steinauer R, Frei IA. Individuals with opioid dependence using polysubstances: how do they experience acute hospital care and what are their needs? A qualitative study. J Addict Nurs. 2019;30:177–184. doi: 10.1097/JAN.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 14.Ou Y, Zhou Y, Xiang P. Effect of obstetric fine nursing on pain during natural childbirth and postpartum recovery. Iran J Public Health. 2018;47:1703–1708. [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma D, Farahbakhsh N, Sharma S, Sharma P, Sharma A. Role of kangaroo mother care in growth and breast feeding rates in very low birth weight (VLBW) neonates: a systematic review. J Matern Fetal Neonatal Med. 2019;32:129–142. doi: 10.1080/14767058.2017.1304535. [DOI] [PubMed] [Google Scholar]
- 16.Kulkarni H, Thangam M, Amin AP. Artificial neural network-based prediction of prolonged length of stay and need for post-acute care in acute coronary syndrome patients undergoing percutaneous coronary intervention. Eur J Clin Invest. 2021;51:e13406. doi: 10.1111/eci.13406. [DOI] [PubMed] [Google Scholar]
- 17.Strobbe S, Hagerty B, Boyd C. Applying the nursing theory of human relatedness to alcoholism and recovery in alcoholics anonymous. J Addict Nurs. 2012;23:241–247. doi: 10.1097/JAN.0b013e31826f67e8. [DOI] [PubMed] [Google Scholar]
- 18.Gacouin A, Roussel M, Le Priol J, Azzaoui I, Uhel F, Fest T, Le Tulzo Y, Tadie JM. Acute alcohol exposure has an independent impact on C-reactive protein levels, neutrophil CD64 expression, and subsets of circulating white blood cells differentiated by flow cytometry in nontrauma patients. Shock. 2014;42:192–198. doi: 10.1097/SHK.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 19.Abidi L, Oenema A, Verhaak P, Tan FES, van de Mheen D. The introduction of the practice nurse mental health in general practices in the Netherlands: effects on number of diagnoses of chronic and acute alcohol abuse. BMC Fam Pract. 2019;20:48. doi: 10.1186/s12875-019-0938-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wetterling T, Junghanns K. Psychopathology of alcoholics during withdrawal and early abstinence. Eur Psychiatry. 2000;15:483–488. doi: 10.1016/s0924-9338(00)00519-8. [DOI] [PubMed] [Google Scholar]
- 21.Yu X, Wang R, Lai B, Tan M. Effect of Auricularia auricula fermentation broth on the liver and stomach of mice with acute alcoholism. Food Funct. 2021;12:191–202. doi: 10.1039/d0fo02688c. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Z, Guo Y, Qiu C, Deng G, Guo M. Protective action of se-supplement against acute alcoholism is regulated by Selenoprotein P (SelP) in the liver. Biol Trace Elem Res. 2017;175:375–387. doi: 10.1007/s12011-016-0780-6. [DOI] [PubMed] [Google Scholar]
- 23.Tsai JP, Lee CJ, Subeq YM, Lee RP, Hsu BG. Acute alcohol intoxication exacerbates rhabdomyolysis-induced acute renal failure in rats. Int J Med Sci. 2017;14:680–689. doi: 10.7150/ijms.19479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park MS, Lim SY, Kim EY, Lee SJ, Chang SO. Examining practical nursing experiences to discover ways in which to retain and invigorate the remaining functions of the elderly with a demented and complex disability in nursing homes. Jpn J Nurs Sci. 2018;15:77–90. doi: 10.1111/jjns.12174. [DOI] [PubMed] [Google Scholar]
- 25.Zhou SH, Huang ST, Xu N, Chen Q, Chen LW, Kuo YR. The application and value of continuous nursing in patients after coronary artery bypass grafting. J Cardiothorac Surg. 2020;15:168. doi: 10.1186/s13019-020-01210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Slemon A, Jenkins E, Bungay V. Safety in psychiatric inpatient care: the impact of risk management culture on mental health nursing practice. Nurs Inq. 2017;24:e12199. doi: 10.1111/nin.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanafin S, Dwan O’Reilly E. Multiple stakeholder views on changes in delivery of public health nursing services in Ireland. Br J Community Nurs. 2015;20:389–393. doi: 10.12968/bjcn.2015.20.8.389. [DOI] [PubMed] [Google Scholar]
- 28.Beyer J, Seidel EJ. Acute care rehabilitation is the first link in a chain of rehabilitation interventions. Rehabilitation (Stuttg) 2017;56:272–285. doi: 10.1055/s-0043-112071. [DOI] [PubMed] [Google Scholar]
- 29.Harrison NL, Skelly MJ, Grosserode EK, Lowes DC, Zeric T, Phister S, Salling MC. Effects of acute alcohol on excitability in the CNS. Neuropharmacology. 2017;122:36–45. doi: 10.1016/j.neuropharm.2017.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dubovsky SL, Antonius D, Ellis DG, Ceusters W, Sugarman RC, Roberts R, Kandifer S, Phillips J, Daurignac EC, Leonard KE, Butler LD, Castner JP, Richard Braen G. A preliminary study of a novel emergency department nursing triage simulation for research applications. BMC Res Notes. 2017;10:15. doi: 10.1186/s13104-016-2337-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


