Abstract
Objective: To explore the effects of empathy nursing on the quality of life and treatment compliance of elderly patients with cerebral infarction (CI). Methods: Elderly patients (n=136) with CI hospitalized in our care were enrolled in this prospective study. The patients were randomly divided into an observation group and a control group by a random number table, with 68 patients in each group. Patients in the control group were given routine nursing, while patients in the observation group were given empathy nursing. The anxiety, depression, quality of life, treatment compliance, sleep quality and nursing satisfaction of the core family members of the two groups were compared. Results: The observation group had lower Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) scores, with significantly higher scores of physical function, general health, social function, emotional role, and mental health than the control group (all P<0.001). The treatment compliance rate (P<0.01) and nursing satisfaction of the core family members (P<0.05) of the observation group were significantly higher, and the Pittsburgh Sleep Quality Index scores were lower (P<0.001) than those of the control group. Conclusion: The application of empathy nursing in elderly patients with CI relieves depression and anxiety, improves quality of life, treatment compliance, sleep quality of patients, and improves nursing satisfaction of the core family members. As such, it is worth clinical promotion and application.
Keywords: Cerebral infarction, elderly patients, quality of life, treatment compliance, sleep quality
Introduction
Cerebral infarction (CI) results in necrosis of brain tissue caused by cerebral ischemia and hypoxia, and a high incidence of CI has been reported around the age of 50-60 [1-3]. In recent years, with the aging of the population, the number of elderly patients with CI has increased significantly [4]. More than 80% of patients after CI will have motor dysfunction and mood disorders due to impaired neurological function, which seriously affects patients’ quality of life [5]. Improving patients’ treatment compliance can reduce the recurrence rate of CI [6]. Therefore, improving the patient’s quality of life and treatment compliance has become the focus of nursing for patients with CI.
Empathy means going deeply into the subjective world of the patient, thinking from the perspective of the patient, and deeply understanding the inner world of the patient, so as to give targeted nursing to the patient [7]. At present, it has been shown that empathy nursing can improve the rehabilitation effect, mood and compliance of patients with CI, but there is no research on the impact of empathy nursing on the quality of life, sleep quality and nursing satisfaction of core care family members of patients with CI [8,9]. In order to provide theoretical guidance for clinical nursing, this study mainly explores the effect of empathy nursing in elderly patients with CI, and focuses on the analysis of the effect of empathy nursing on patients’ anxiety, depression, quality of life, treatment compliance, sleep quality, and nursing satisfaction of the core family members.
Materials and methods
General information
Elderly patients (n=136) with CI that were cared for in our hospital from June 12, 2019 to June 30, 2020 were enrolled in this prospective study. The patients were randomly divided into an observation group and a control group by a random number table, with 68 patients in each group. Patients in the control group were given routine nursing, and patients in the observation group were given empathy nursing. The general information of the patients in the two groups is shown in Table 1. This study was carried out in accordance with the recommendations of the Medical Ethics Committee of our hospital. Written informed consent was required for all patients.
Table 1.
Comparison of general baseline data (n, x̅±sd)
| Index | Observation group (n=68) | Control group (n=68) | χ2/t | P |
|---|---|---|---|---|
| Age (year) | 68.5±8.1 | 67.5±7.8 | 0.733 | 0.466 |
| BMI (kg/m2) | 22.80±2.15 | 22.78±2.32 | 0.052 | 0.958 |
| Gender (n) | 0.029 | 0.863 | ||
| Male | 37 | 36 | ||
| Female | 31 | 32 | ||
| Comorbid diseases (n) | ||||
| Hypertension (n) | 16 | 12 | 0.719 | 0.396 |
| Coronary heart disease (n) | 12 | 9 | 0.506 | 0.476 |
| Diabetes (n) | 7 | 6 | 0.085 | 0.770 |
| Smoking history (n) | 8 | 9 | 0.067 | 0.795 |
| Drinking history (n) | 4 | 6 | 0.431 | 0.511 |
| Major infarcts (n) | 0.180 | 0.996 | ||
| Basal ganglia | 24 | 26 | ||
| Frontal lobe | 11 | 10 | ||
| Parietal lobe | 10 | 9 | ||
| Temporal lobe | 9 | 9 | ||
| Occipital lobe | 14 | 14 | ||
| Sports involvement (n) | 0.282 | 0.595 | ||
| Yes | 27 | 24 | ||
| No | 41 | 44 |
Note: BMI: body mass index.
Inclusion criteria: (1) Patients were diagnosed with CI by MRI/CT [10]. (2) Patients had normal cognitive function. (3) Patients were older than 60 years old. (4) Patients had primary CI.
Exclusion criteria: (1) Patients with severe heart, liver, and kidney dysfunction. (2) Patients who were in the subacute phase of CI. (3) Patients with a history of mental illness. (4) Patients with cognitive impairment were excluded. (5) Patients with transient cerebral ischemia.
Methods
Patients in the control group were given routine nursing [11]. Disease health education was carried out. ECG monitoring was performed to closely observe the changes of heart rate, blood pressure and other physical indicators. The ward was kept clean, quiet and with fresh air. Patients had a light diet and oral care twice a day. The airway was kept unobstructed and oxygen inhalation was given if necessary. Regular rollovers were given to patients who were unconscious and unable to roll over on their own. Skin care was given to prevent bedsores. Bleeding tendency was observed when patients were treated with anticoagulation and thrombolytic drugs. The functional position of the paralyzed limbs was maintained and rehabilitation training was strengthened.
Patients in the observation group were treated with empathy nursing. A 5-member empathy nursing team was established, consisting of 1 attending physician, 1 head nurse, 1 nursing team leader, and 2 nurses in charge. The empathy nursing team first formulated a scientific and reasonable empathy nursing plan, and conducted unified training for the members of the team according to the plan, and required the members to implement measures in accordance with the training plan. Medical staff closely observed and fully understood the patients’ emotional changes, actively listened to their true thoughts, and provided timely guidance to stabilize their psychological mood. Health education was carried out. Medical staff explained disease-related knowledge through manuals, videos, lectures, WeChat groups, etc. At the same time, they shared cases with good rehabilitation effects, and enabled patients to maintain a good and optimistic attitude to cooperate with treatment by causing resonance. When communicating with patients, medical staff used body language such as smiling, nodding, and touching to show their understanding to the patient. When communicating with patients, medical staff conveyed their feelings to patients. By letting patients feel the sincerity of medical staff, medical staff fully understood the emotional needs and psychological changes of patients. Medical staff guided the patient’s family to encourage and care for the patient, through understanding the patient’s desire to be cared for and respected.
Outcome measures
Primary outcome measures were as follows.
Self-Rating Anxiety Scale (SAS) was used for evaluation of anxiety before intervention and 1 month after intervention. SAS, using a four-level scoring method, includes 20 items, consisting of forward scoring questions and reverse scoring questions [12]. The sum of all item scores is the total score of the scale. The SAS score ≥50 indicates that the patient is accompanied by anxiety. The higher the score, the more serious the anxiety.
Self-Rating Depression Scale (SDS) was adopted to evaluate depression before intervention and 1 month after intervention. SDS has 20 items with a 4-level scoring system [13]. The SDS scores of 53-62, 63-72, and >72 indicate that patients are accompanied by mild depression, moderate depression, and moderate depression, respectively. The higher the score, the more severe the depression.
Quality of life was evaluated by Short Form-36 Health Survey (MOS SF-36) before intervention and 1 month after intervention. MOS SF-36 includes physical function, general health, social function, emotional role, and mental health. The full score of each dimension is 100 points. The higher the score, the higher the quality of life in the relevant dimensions [14].
Compliance was observed 1 month after intervention. A self-made questionnaire was used to evaluate the patient’s treatment compliance, and the options were divided into complete non-compliance, partial compliance, and complete compliance. Compliance rate = (partial compliance + complete compliance) cases/total cases *100%.
Secondary outcome measures are shown below.
Sleep quality was evaluated by Pittsburgh Sleep Quality Index (PSQI), which consists of 19 self-assessed and 5 other-rated items that were scored before intervention and 1 month after intervention. The cumulative score of each item is the total PSQI score and the total score ranges from 0 to 2l. The higher the PSQI score, the worse the quality of sleep [15].
A self-made questionnaire was used to evaluate the satisfaction of the core family members 1 month after intervention. The options were divided into satisfied (90-100), basically satisfied (60-89), dissatisfied (<60), satisfaction = (satisfied + basically satisfied) cases/total cases *100%.
Statistical analysis
SPSS 20.0 was used for data analysis. Counting data were expressed as (n, %), and tested by χ2. Measurement data conforming to a normal distribution was expressed as (x̅±sd), and independent t test was used for comparison between the two groups. Rank sum test was used to compare the composition of graded data between groups. P<0.05 indicates that the difference is statistically significant.
Results
Comparison of general baseline data
The general data, such as age, body mass index, gender, comorbid diseases, smoking history, drinking history, major infarcts, and sports involvement of the two groups were comparable (all P>0.05). See Table 1.
Comparison of anxiety
Before intervention, no difference was found in SAS scores between the two groups (P>0.05). After intervention, the SAS scores of the two groups were lower than before intervention, with statistical significance (P<0.001). After intervention, the observation group had lower SAS scores than the control group (P<0.001). See Figure 1.
Figure 1.

Comparison of SAS scores between the two groups. Compared with control group, ***P<0.001; compared with before intervention, ###P<0.001. SAS: self-rating anxiety scale.
Comparison of depression
Before intervention, no difference was found in SDS scores between the two groups (P>0.05). After intervention, the SDS scores of the two groups were lower than before intervention (P<0.001). After intervention, the observation group had lower SDS scores (P<0.001). See Figure 2.
Figure 2.
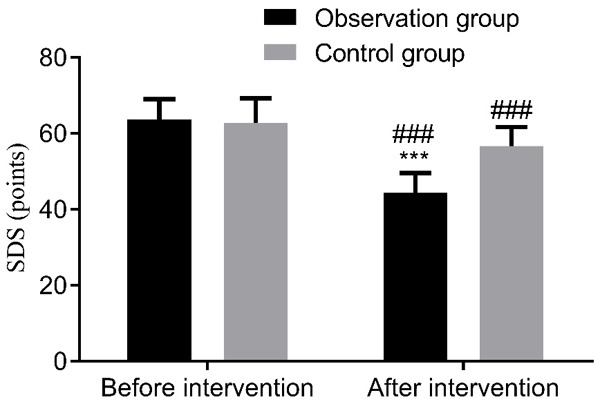
Comparison of SDS scores between the two groups. Compared with control group, ***P<0.001; compared with before intervention, ###P<0.001. SDS: Self-Rating depression Scale.
Comparison of quality of life
Before intervention, no difference was found in quality-of-life scores between the two groups (P>0.05). After intervention, the quality-of-life scores of the two groups were higher (P<0.001). After intervention, compared with the control group, the scores of physical function, general health, social function, emotional role and mental health in the observation group were all higher (all P<0.001). See Table 2.
Table 2.
Comparison of MOS SF-36 score of quality of life (x̅±sd)
| Quality of life scores | Physical function | General health | Social function | Emotional role | Mental health |
|---|---|---|---|---|---|
| Observation group (n=68) | |||||
| Before intervention | 60.50±8.21 | 72.09±12.30 | 58.28±9.09 | 49.97±6.09 | 50.00±6.08 |
| After intervention | 80.65±9.23### | 92.89±11.30### | 74.86±10.30### | 64.09±8.65### | 69.86±9.43### |
| Control group (n=68) | |||||
| Before intervention | 60.67±8.01 | 70.02±12.01 | 59.26±9.20 | 50.91±6.25 | 50.01±5.90 |
| After intervention | 65.54±8.31### | 83.09±12.32### | 63.29±9.23### | 54.98±6.21### | 55.09±6.34### |
| t | 10.032 | 4.834 | 6.898 | 7.055 | 10.719 |
| P | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Note: Compared with before intervention;
P<0.001.
SF-36: Short Form-36.
Comparison of treatment compliance
The treatment compliance rate of the observation group was significantly higher than that of the control group (P<0.01), as shown in Table 3.
Table 3.
Comparison of treatment compliance
| Group | Complete compliance | Partial compliance | Complete non-compliance | Compliance rate (%) |
|---|---|---|---|---|
| Observation group (n=68) | 20 (29.41) | 32 (47.06) | 16 (38.23) | 52 (76.47) |
| Control group (n=68) | 13 (19.11) | 22 (32.34) | 32 (47.05) | 35 (51.47) |
| χ2 | 8.663 | 9.219 | ||
| P | 0.013 | 0.002 | ||
Comparison of sleep quality
Before intervention, no difference was found in PSQI scores between the two groups (P>0.05). After intervention, the PSQI scores of the two groups were lower than those before intervention (P<0.001). After intervention, the observation group had lower PSQI scores than the control group (9.90±2.01 vs 15.53±2.44) (t=14.686, P<0.001). See Figure 3.
Figure 3.

PSQI scores were compared between the two groups. Compared with control group, ***P<0.001; compared with before intervention, ###P<0.001. PSQI: Pittsburgh Sleep Quality Index.
Comparison of nursing satisfaction of core family members
In the observation group, the nursing satisfaction of the core care family members during hospitalization was 89.71%, including 31 satisfied cases, 30 basically satisfied cases and 7 unsatisfied cases. While in the control group, the nursing satisfaction was 73.53%, including 25 satisfied cases, 25 basically satisfied cases and 18 unsatisfied cases. The nursing satisfaction of the core family members during hospitalization of the observation group was significantly higher (P<0.05). See Table 4.
Table 4.
Comparison of nursing satisfaction of core family members (n, %)
| Group | Satisfied | Basically satisfied | Unsatisfied | Satisfaction % |
|---|---|---|---|---|
| Observation group (n=68) | 31 (45.59) | 30 (44.12) | 7 (10.29) | 61 (89.71) |
| Control group (n=68) | 25 (36.76) | 25 (36.76) | 18 (26.48) | 50 (73.53) |
| U/χ2 | 5.937 | 5.930 | ||
| P | 0.051 | 0.014 | ||
Discussion
Empathy means going deeply into the subjective world of the patient, thinking from the perspective of the patient, and deeply understanding the inner world of the patient, so as to take targeted nursing for the patient [9]. Most patients with CI have different degrees of paralysis, language barriers, or even complete loss of self-care ability, which seriously affects patients’ quality of life [16,17]. At the same time, exercise dysfunction often leads to great mental trauma and negative emotions, and such negative emotions and psychological state will affect patients’ treatment compliance and disease prognosis [18].
In this study, the observation group was treated with empathy nursing and compared with the routine nursing in the control group. The outcomes showed that SAS and SDS scores in the observation group were lower than those in the control group, indicating that empathy nursing reduced anxiety and depression, which was consistent with the findings of Hu et al. [8]. The treatment compliance rate of the observation group was significantly higher, which was consistent with the idea of Wang et al., suggesting that empathy nursing improved the treatment compliance of patients [7]. The reason may be that patients were cared for from a compassionate perspective and given targeted care through empathy nursing. They felt real care, thus their negative emotions were eliminated and they could cooperate with the treatment with a positive attitude.
Sequelae of CI generally lead to a low quality of life [11]. It is reported that empathy nursing promotes the rapid recovery of elderly patients with CI by improving their neurological function and limb movement function [9]. In this study, empathy nursing was adopted in the observation group, and the scores of all dimensions of quality of life in the observation group were higher, indicating that empathy nursing improved patients’ quality of life. The reason may be that empathy nursing can improve patients’ negative emotions, and patients were more active in cooperating with treatment, thus greatly improving patients’ neurological function and limb function, and finally achieving the purpose of improving patients’ quality of life.
Chen et al. found that the PSQI scores of patients with CI were significantly lower than those of patients without CI, revealing that patients with CI were often accompanied by sleep disorders [19]. Fu et al. and Wang et al. found that depression and aphasia are independent risk factors for insomnia in patients with CI [20,21]. The results of this study demonstrated that the sleep quality of the observation group was significantly better than that of the control group, indicating that empathy nursing improved the sleep quality, which may be because empathy nursing can alleviate the depression of patients. In this study, nursing satisfaction of core family members was also compared between the two groups. It was found that the nursing satisfaction of the core family members of the observation group was higher than that of the control group. That was, core family members were very satisfied with empathy nursing, which may be due to the empathy nursing relieving patients’ anxiety and depression, improving the living quality and clinical prognosis, so that the patients cooperated with treatment to reduce the psychological burden of core family members.
However, there are some shortcomings in this study, such as small sample size, being a single center study, with a short follow-up time, and no study on anxiety and depression of core family members. In the later stages, a long-term nursing effect study of a larger sample should be conducted to confirm the feasibility and importance of empathy nursing in elderly patients with CI.
In conclusion, the application of empathy nursing in elderly patients with CI can relieve depression and anxiety, improve quality of life, treatment compliance, sleep quality of patients, and improve nursing satisfaction of the core family members. It is worth clinical promotion and application.
Disclosure of conflict of interest
None.
References
- 1.Zhu H, Zhao T, Liu J. Role of Paraoxonase 1 activity and oxidative/antioxidative stress markers in patients with acute cerebral infarction. Clin Lab. 2018;64:1049–1053. doi: 10.7754/Clin.Lab.2018.180201. [DOI] [PubMed] [Google Scholar]
- 2.Aizawa Y, Nakai T, Saito Y, Monno K, Morikawa T, Kogawa R, Hatta T, Tamaki T, Kato M, Arimoto M, Osaka S, Sunagawa K, Tang XY, Tanaka M, Hao H, Hirayama A. Calcified amorphous tumor-induced acute cerebral infarction. Int Heart J. 2018;59:240–242. doi: 10.1536/ihj.17-020. [DOI] [PubMed] [Google Scholar]
- 3.Nai Y, Liu H, Bi X, Gao H, Ren C. Protective effect of astaxanthin on acute cerebral infarction in rats. Hum Exp Toxicol. 2018;37:929–936. doi: 10.1177/0960327117745693. [DOI] [PubMed] [Google Scholar]
- 4.Gu BJ, Wang CH, Hao XX, Chen CS, Wang ZH. Risk factors of renal function injury in patients with first-episode acute cerebral infarction. J Clin Neurol. 2020;33:135–138. [Google Scholar]
- 5.Sun F, Liu H, Fu HX, Zhang S, Qian XD, Li JJ, Zhu YB, Zhang XX, Zhang J, Qiu HP, Kang LL, Hu YJ, Zhao L, Mi YJ, Gao YJ, Dou ZJ, Ma Z. Comparative study of intravenous thrombolysis with rt-PA and urokinase for patients with acute cerebral infarction. J Int Med Res. 2020;48:300060519895352. doi: 10.1177/0300060519895352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng LS, Chi SH, Mo L, Yi LH, Wang J, Liu Y, Zhao CS. Relationship between standardized treatment compliance and recurrence of cerebral infarction. Chin J Med Univ. 2018;47:1008–1010. [Google Scholar]
- 7.Wang XL, Hu L, Wan X, Zhong YJ, Chen YY. Effect of empathic nursing on emotion, treatment compliance and rehabilitation effect of elderly patients with cerebral infarction. Int J Psychiatry. 2018;45:375–377. [Google Scholar]
- 8.Hu ZP, Guo M, LV DZ, Chen LW. Effect of empathic nursing on negative emotion and treatment compliance of elderly patients with cerebral infarction. Chongqing Med J. 2020;49:183–186. [Google Scholar]
- 9.Zhao HM, Gao CX, Xue N, Mu PY, Bai YX. The effect of empathic nursing on anxiety and depression in elderly patients with cerebral infarction. Int J Psychiatry. 2015;42:131–134. [Google Scholar]
- 10.Zhang AW, Han XS, Xu XT, Fang YN, Chen HB, Jiang T. Acute phase serum cathepsin S level and cathepsin S/cystatin C ratio are the associated factors with cerebral infarction and their diagnostic value for cerebral infarction. Kaohsiung J Med Sci. 2019;35:95–101. doi: 10.1002/kjm2.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang LJ. Nursing progress of acute cerebral infarction. Heilongjiang Sci Technol Inf. 2012:33. [Google Scholar]
- 12.Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the zung scales. BMC Psychiatry. 2017;17:329. doi: 10.1186/s12888-017-1489-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sepehry AA. Zung self-rating depression scale. In: Sepehry AA, editor. New York: Springer; 2011. [Google Scholar]
- 14.Vitorino DFDM, Martins FLM, Souza ADC, Galdino D, Prado GFD. Utilizao do SF-36 em ensaios clínicos envolvendo pacientes fibromiálgicos: determinao de critérios mínimos de melhora clínica. Revista Neurociências. 2019;12:147–151. [Google Scholar]
- 15.Buysse DJ, Hall ML, Strollo PJ, Kamarck TW, Owens J, Lee L, Reis SE, Matthews KA. Relationships between the Pittsburgh sleep quality index (PSQI), epworth sleepiness scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4:563–571. [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang XY, Wang SG. Effect of emotional nursing with traditional Chinese medicine characteristics on quality of life and treatment compliance in convalescent cerebral infarction. Chin J Med Clin. 2019;19:327–328. [Google Scholar]
- 17.Zeng LL, Ren FF. Study on the effect of optimized nursing mode on improving the quality of life and promoting the therapeutic effect of patients with cerebral infarction. Lab Med Clin. 2019;16:3496–3498. [Google Scholar]
- 18.Liu Y, Zhang L, Feng XH, Shi YF, Zhu KY, Xie ST. Clinical analysis of flupentixol melitracen tablets in the treatment of mild depression and anxiety after acute cerebral infarction. Int J Psychiatry. 2019;46:151–153. 157. [Google Scholar]
- 19.Chen X, Bi H, Zhang M, Liu H, Wang X, Zu R. Research of sleep disorders in patients with acute cerebral infarction. J Stroke Cerebrovasc Dis. 2015;24:2508–2513. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.033. [DOI] [PubMed] [Google Scholar]
- 20.Fu XY, Li YY, Chen Y, Wang M, Wang H, Yu GL. Correlation between insomnia and human factors, vascular risk factors and characteristics of cerebral infarction in patients with cerebral infarction. Chin J Physicians. 2020;22:1493–1496. [Google Scholar]
- 21.Wang LR, Fu XY, Wang H, Ma RX, Tan QH, Dong MY, Zhou HD. Correlation between post-stroke depression and human factors, vascular risk factors and stroke characteristics. Chin J Gen Pract. 2017;15:286–288. [Google Scholar]


