Abstract
Aims
Patients with brief psychotic episodes (BPE) have variable and fluctuating clinical outcomes which challenge psychiatric care. Our meta-analysis aims at providing a comprehensive summary of several clinical outcomes in this patient group.
Methods
A multistep systematic PRISMA/MOOSE-compliant literature search was performed for articles published from inception until 1st March 2021. Web of Science database was searched, complemented by manual search of original articles reporting relevant outcomes (psychotic recurrence, prospective diagnostic change or stability, remission, quality of life, functional status, mortality and their predictors) for patients diagnosed with acute and transient psychotic disorders (ATPD), brief psychotic disorders (BPD), brief intermittent psychotic symptoms (BIPS) and brief limited intermittent psychotic symptoms (BLIPS). Random-effects methods and Q-statistics were employed, quality assessment with Newcastle-Ottawa Scale, assessment of heterogeneity with I2 index, sensitivity analyses (acute polymorphic psychotic disorders, APPD) and multiple meta-regressions, assessment of publication bias with funnel plot, Egger's test and meta-regression (psychotic recurrence and sample size).
Results
A total of 91 independent articles (n = 94 samples) encompassed 37 ATPD, 24 BPD, 19 BLIPS and 14 BIPS samples, totalling 15 729 individuals (mean age: 30.89 ± 7.33 years, mean female ratio: 60%, 59% conducted in Europe). Meta-analytical risk of psychotic recurrence for all BPE increased from 15% (95% confidence interval (CI) 12–18) at 6 months, 25% (95% CI 22–30) at 12 months, 30% (95% CI 27–33) at 24 months and 33% (95% CI 30–37) at ⩾36 months follow-up, with no differences between ATPD, BPD, BLIPS and BIPS after 2 years of follow-up. Across all BPE, meta-analytical proportion of prospective diagnostic stability (average follow-up 47 months) was 49% (95% CI 42–56); meta-analytical proportion of diagnostic change (average follow-up 47 months) to schizophrenia spectrum psychoses was 19% (95% CI 16–23), affective spectrum psychoses 5% (95% CI 3–7), other psychotic disorders 7% (95% CI 5–9) and other (non-psychotic) mental disorders 14% (95% CI 11–17). Prospective diagnostic change within APPD without symptoms of schizophrenia was 34% (95% CI 24–46) at a mean follow-up of 51 months: 18% (95% CI 11–30) for schizophrenia spectrum psychoses and 17% (95% CI 10–26) for other (non-psychotic) mental disorders. Meta-analytical proportion of baseline employment was 48% (95% CI 38–58), whereas there were not enough data to explore the other outcomes. Heterogeneity was high; female ratio and study quality were negatively and positively associated with risk of psychotic recurrence, respectively. There were no consistent factor predicting clinical outcomes.
Conclusions
Short-lived psychotic episodes are associated with a high risk of psychotic recurrences, in particular schizophrenia spectrum disorders. Other clinical outcomes remain relatively underinvestigated. There are no consistent prognostic/predictive factors.
Keywords: ATPD, BPD, brief psychotic episode, psychosis
Introduction
Since the 19th century, brief psychotic episodes (BPE) have been characterised as a divergent and shifting nosographic concept, providing a major challenge both for clinical practice and classification. Historically, their fleeting and dynamical nature constituted an early anomaly within the Kraepelinian dichotomous concept of psychoses (dementia praecox v. manic-depressive illness; Kraepelin, 1899). The historical development of operationalisations for BPE has been previously appraised (Fusar-Poli et al., 2016a) by our group. Briefly, World Health Organization includes the concept of acute and transient psychotic disorders (ATPD) in ICD-10 within the group of ‘schizophrenia, schizotypal and delusional disorders’ (World Health Organization, 1992), with six subtypes, including disorders defined by acute onset of frank psychotic symptoms (acute within 2 weeks; abrupt within 48 h) and complete recovery within 1–3 months even with antipsychotic treatment. However, the 11th edition of the ICD has narrowed the ATPD category to the subtype of acute polymorphic psychotic disorders (APPD) without the symptoms of schizophrenia (Castagnini and Foldager, 2014). DSM-5 includes brief psychotic disorder (BPD) within the ‘schizophrenia spectrum and other psychotic disorders’, defined by the presence of at least one across four of five core symptoms of schizophrenia (negative symptoms are not included): delusions, hallucinations, disorganised speech and grossly disorganised or catatonic behaviour (American Psychiatric Association, 2013). Duration of the episode must be less than 1 month and sudden onset and polymorphic and fluctuating nature of symptoms are not mandatory criteria (Gaebel, 2012). The paradigm of clinical high-risk states of psychosis (CHR-P) operationalised BPE not as frank psychotic disorder, but as a state of increased clinical risk for developing subsequent persistent psychotic disorders. Brief limited intermittent psychotic symptoms (BLIPS) (Yung et al., 1996) last less than 7 days and accommodate potential ‘transdiagnostic’ (Fusar-Poli, 2019; Fusar-Poli et al., 2019c) comorbidities. Brief intermittent psychotic symptoms (BIPS) exclude individuals with seriously disorganising and dangerous features (Miller et al., 2003) and extend the duration of brief psychotic symptoms up to 3 months.
Given these differences, in previous studies we employed meta-analyses to test the prognostic significance of these competing operationalisations. We found no difference in their risk of psychotic recurrence at any follow-up timepoint, but a lower risk of recurrence compared to first-episode remitting schizophrenia (Fusar-Poli et al., 2016a). We also demonstrated meta-analytically that, at 4.5 years follow-up, about 56% of patients with BPE retained their index diagnosis (prospective diagnostic stability) whereas 44% shifted to other diagnoses (prospective diagnostic change), schizophrenia being the most frequent one (21%, 95% confidence interval (CI) 16–25) (Fusar-Poli et al., 2016c). Other clinical outcomes such as remission, quality of life, vocational status and mortality have traditionally seen as more favourable than in schizophrenia (Pillmann and Marneros, 2005) but findings have been conflicting. Similarly, predictors of these outcomes appear patchy and inconsistent and require a systematic appraisal. These meta-analytic summaries had been completed more than 5 years ago, and several recent publications have emerged, which require periodical updates of the evidence. Our aim was to provide an updated systematic review and meta-analysis which comprehensively addresses for the first time multiple clinical outcomes in BPE encompassing psychotic recurrence, prospective diagnostic stability and change, remission, quality of life, functional/vocational status and mortality and systematically appraise the consistency of predictors of these outcomes.
Methods
This study (protocol registered on https://osf.io/5dw98) was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (Moher et al., 2009) and the Meta-analysis Of Observational Studies in Epidemiology (Stroup et al., 2000) (online Supplementary eTables 1 and 2).
Search strategy and selection criteria
A multistep systematic PRISMA-compliant literature search was performed for articles published from inception until 1st March 2021 (see the details in online Supplementary eMethods 1). The references of systematic reviews or meta-analyses that were retrieved during the systematic literature search were manually searched. Articles identified were screened as abstracts. The remaining articles were assessed for inclusion eligibility against the inclusion and exclusion criteria and decisions were made regarding their final inclusion in the meta-analysis.
The inclusion criteria were: (a) original studies, published in English; (b) conducted in individuals meeting BIPS or BLIPS criteria according to Structured Interview for Psychosis-Risk Syndromes (SIPS any version) (McGlashan TH, 2010) or Comprehensive Assessment of At-Risk Mental States (CAARMS any version) (Yung et al., 2006); ATPD according to ICD (any version) criteria (World Health Organization, 1992); or BPD according to DSM (any version) criteria (American Psychiatric Association, 2013) and (c) reporting on at least one of meta-analytic outcomes (see below).
The exclusion criteria were: (a) reviews, conference proceedings or pilot data sets; (b) unpublished data; (c) studies evaluating BPE but using criteria different from those established above; (d) studies that did not report specific information on the ATPD/BPD/BIPS/BLIPS group alone, but reported composite results including other subgroups (e.g. attenuated psychosis syndrome, APS and genetic risk and deterioration syndrome, GRD) and (e) studies with samples of individuals with other persisting psychotic disorders (e.g. schizophrenia). For the meta-analyses we additionally excluded studies with overlapping datasets, selecting the largest and most recent data set. Disagreements in selection criteria were resolved through discussion and consensus with a senior researcher.
Outcome measures and data extraction
Two independent researchers extracted data. The primary outcome was risk of psychotic recurrence after at least 3 months since the index BPE. Secondary outcomes were the prospective diagnostic stability (defined as the proportion of baseline patients retaining the same ICD/DSM psychotic diagnosis over time) (Fusar-Poli et al., 2016c) or diagnostic change to any other mental disorder (defined as the proportion of baseline patients shifting to other ICD/DSM diagnoses at follow-up) (Fusar-Poli et al., 2016c), remission (defined as indicated in each study), quality of life (defined as indicated in each study, at baseline and/or follow-up), functional/vocational status (defined as indicated in each study at baseline and/or follow-up), mortality (number of patients deceased during the follow-up) or predictors of these outcomes (any regression models testing the association between factors and clinical outcomes, within longitudinal designs). When the predictors were not directly presented in the text, they were extracted from associated information (e.g. graphs); corresponding authors were also contacted to retrieve missing data. From each study, a predetermined set of variables characterising the study, outcomes or predictors was included (online Supplementary eMethods 2). Data were extracted closest to the follow-up time of interest. Disagreements in selection/extraction criteria were resolved through discussion and consensus with a senior researcher.
Quality assessment
The quality of the included studies was evaluated using a modified version of the Newcastle-Ottawa Scale (NOS) for cohort studies, which has been repeatedly used (Catalan et al., 2020). Studies were awarded a maximum of eight points on items related to the representativeness, exposure, outcomes, follow-up period and loss to follow-up.
Strategy for data synthesis
Meta-analyses were attempted when there were enough data for each outcome, otherwise outcomes were systematically described.
The primary meta-analytical outcome was risk of psychotic recurrence across BPE. This was estimated by extracting the raw counts of psychotic recurrence in individuals with an initial short BPE (defined according to the inclusion criteria (b)) at 6 months (including a 3–9 months range); 12 months (including a 10–18 months range); 24 months (including a 19–29 months range); 36 months (including ⩾30 months) follow-up. The primary effect size was the meta-analytical proportion of psychotic recurrence. Because the studies were expected to be heterogenous, random-effects models were used. Heterogeneity among study point estimates was assessed with the Q-statistics, with the proportion of the total variability in the effect size estimates being evaluated with the I2 index (Lipsey and Wilson, 2001) which does not depend upon the number of studies included. The meta-analysis was stratified by operationalisations of BPE: BIPS, BLIPS, ATPD or BPD. The four main operationalisations (BIPS, BLIPS, ATPD and BPD) were compared testing for between-group heterogeneity (Q). Sensitivity analyses, removing one study at a time, were conducted to test the robustness of results. Publication bias was assessed with funnel plot inspection, Egger's test and meta-regression between the main outcome (psychotic recurrence) as dependent variable and sample size as independent variable.
Planned meta-analyses on secondary outcomes included: (i) prospective diagnostic stability (effect size: proportion), (ii) prospective diagnostic change to any other mental disorder (effect size: proportion), (iii) remission (effect size: standardised mean difference), (iv) quality of life (effect size: standardised mean difference) at baseline and/or follow-up, (v) functional/vocational status (effect size: proportion) at baseline and/or follow-up and (vi) mortality (effect size: proportion). The analyses (i–ii) were not conducted for BLIPS/BIPS because these do not correspond to standard ICD/DSM diagnoses at baseline and were conducted pooling all available studies and estimating the average follow-up time. Within analyses (i–ii), we additionally clustered the individual ICD/DSM diagnoses across NICE-compliant diagnostic spectra (National Institute for Health and Care Excellence, 2014): schizophrenia spectrum psychoses (schizophrenia, schizophreniform disorder and schizoaffective disorder), affective spectrum psychoses (mania with psychosis and/or bipolar disorder with psychosis and/or depression with psychosis), other psychotic disorders and other (non-psychotic) mental disorders. For all outcomes (primary and secondary), we also sought to perform additional analyses restricted to the ATPD subtype which will be retained in the ICD-11 version (APPD without symptoms of schizophrenia). Sensitivity analyses were planned on the primary outcome, by excluding one study per time and rerunning the analyses. We performed multiple meta-regression analyses (i.e. employing two meta-regressor factors at the same time) of factors that were known to moderate transition risk when at least ten studies were available. The fixed meta-regressor factor was follow-up time, which was combined with: mean age, female ratio, publication year and study quality (NOS score). Comprehensive Meta-Analysis Software v3.0 was used for the analyses (Borenstein et al., 2013).
Results
Database
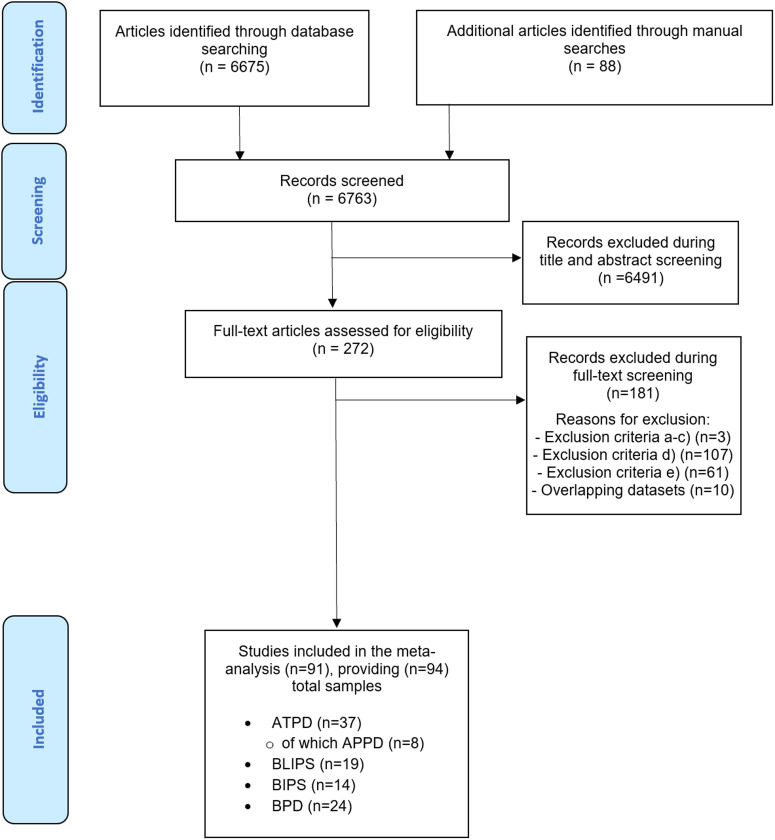
The systematic literature search (PRISMA flow-chart, Fig. 1) identified 91 independent articles, some of which contributed with more than one sample. The total number of samples (n = 94) included 37 ATPD, 24 BPD, 19 BLIPS and 14 BIPS samples. Eight samples (1262 patients) comprising ATPD subjects also provided data for APPD without symptoms of schizophrenia subtype. The total database included 15 729 individuals, with a mean age of 30.89 ± 7.33 years and an average female ratio of 60.0% (range from 8.3 to 86.2%). In total, 59% of the studies were conducted in Europe, 28% in Asia, 7% in North America, 3% in Australia, 2% in Africa and 1% in South America. The characteristics of the studies included in the meta-analyses are illustrated in online Supplementary eTable 3.
Fig. 1.
PRISMA 2009 flow diagram.
Risk of psychotic recurrence of BPE
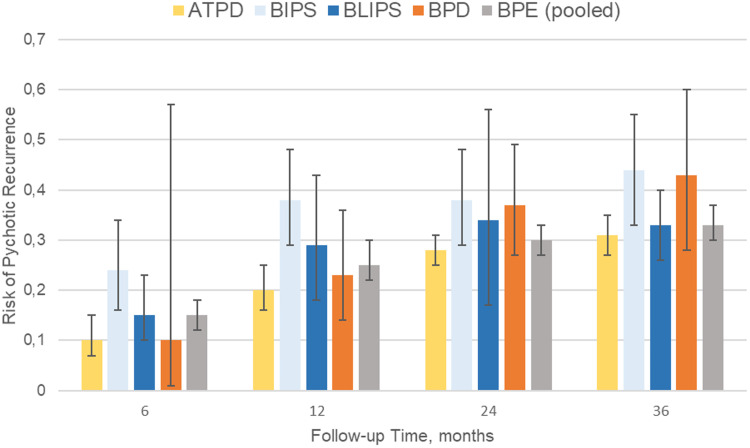
Ninety-one independent samples reported primary outcome data at different follow-up time points (Table 1 and Fig. 2). The meta-analytical risk of psychotic recurrence for all BPE was 15% (95% CI 12–18) at 6 months, 25% (95% CI 22–30) at 12 months, 30% (95% CI 27–33) at 24 months and 33% (95% CI 30–37) at ⩾36 months follow-up. The meta-analytical risk of psychotic recurrence for ATPD was 10% (95% CI 7–15) at 6 months, 20% (95% CI 16–25) at 12 months, 28% (95% CI 25–31) at 24 months and 31% (95% CI 27–35) at ⩾36 months follow-up; for BIPS, 24% (95% CI 16–34) at 6 months, 38% (95% CI 29–48) at 12 months, 38% (95% CI 29–48) at 24 months and 44% (95% CI 33–55) at ⩾36 months follow-up; for BLIPS, 15% (95% CI 10–23) at 6 months, 29% (95% CI 18–43) at 12 months, 34% (95% CI 17–56) at 24 months and 33% (95% CI 26–40) at ⩾36 months follow-up; for BPD, 10% (95% CI 1–57) at 6 months, 23% (95% CI 14–36) at 12 months, 37% (95% CI 27–49) at 24 months and 43% (95% CI 30–37) at ⩾36 months follow-up. There were significant between-group differences at 6 months (p = 0.020) and 12 months (p = 0.003), mostly driven by the BIPS group, but not at 24 (p = 0.110) and at ⩾36 (p = 0.100) months (Table 1). The risk of psychotic recurrence in APPD without symptoms of schizophrenia was 21% (95% CI 14–31) at mean follow-up of 51 months (online Supplementary eFig. 1).
Table 1.
Meta-analysis of risk of psychotic recurrences in BPE
| Follow-up, months | ||||
|---|---|---|---|---|
| Characteristic | 6 | 12 | 24 | ⩾36 |
| No. of samples | 22 | 35 | 31 | 40 |
| No. of patients analysed | 3874 | 4559 | 4189 | 13 624 |
| Risk of psychotic recurrence, mean (95% CI) | ||||
| ATPD | 0.10 (0.07–0.15) | 0.20 (0.16–0.25) | 0.28 (0.25–0.31) | 0.31 (0.27–0.35) |
| BIPS | 0.24 (0.16–0.34) | 0.38 (0.29–0.48) | 0.38 (0.29–0.48) | 0.44 (0.33–0.55) |
| BLIPS | 0.15 (0.10–0.23) | 0.29 (0.18–0.43) | 0.34 (0.17–0.56) | 0.33 (0.26–0.40) |
| BPD | 0.10 (0.01–0.57) | 0.23 (0.14–0.36) | 0.37 (0.27–0.49) | 0.43 (0.28–0.60) |
| BPE (pooled) | 0.15 (0.12–0.18) | 0.25 (0.22–0.30) | 0.30 (0.27–0.33) | 0.33 (0.30–0.37) |
| ATPD v. BIPS v. BLIPS v. BPD test for between-group heterogeneity (Q) | 9.80 | 13.70 | 6.10 | 6.17 |
| p value | 0.02 | <0.01 | 0.11 | 0.10 |
| I2 (%) | 67.78 | 66.67 | 43.81 | 84.55 |
ATPD, acute and transient psychotic disorder; BIPS, brief intermittent psychotic symptoms; BLIPS, brief limited intermittent psychotic symptoms; BPD, brief psychotic disorder; BPE, brief psychotic episodes.
Fig. 2.
Meta-analysis of risk of psychotic recurrences in BPE. ATPD, acute and transient psychotic disorder; BIPS, brief intermittent psychotic symptoms; BLIPS, brief limited intermittent psychotic symptoms; BPD, brief psychotic disorder.
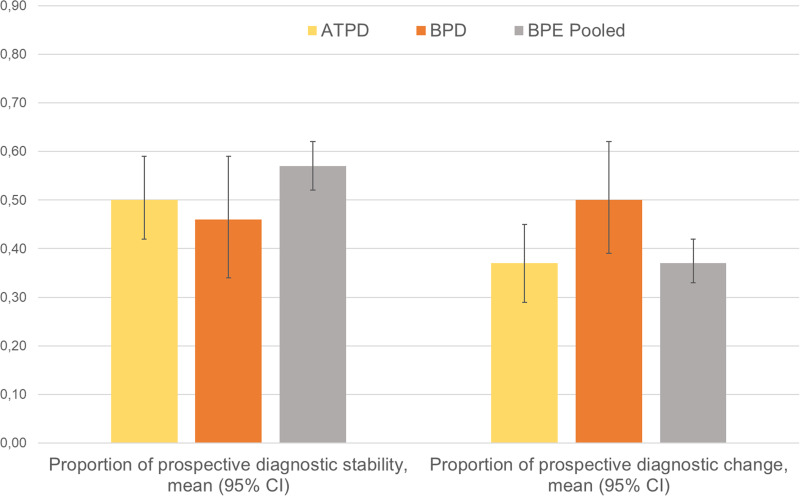
Proportion of prospective diagnostic stability and diagnostic change
Sixty-one independent samples (15 034 patients) reported prospective diagnostic stability or diagnostic change data at different follow-up time points (Table 2). The meta-analytical proportion of prospective diagnostic stability (average follow-up 47 months) was 49% (95% CI 42–56) for all BPE. It was 50% (95% CI 42–59) for ATPD and 46% (95% CI 34–59) for BPD (Table 2 and Fig. 3), with no significant between-group differences (p = 0.59).
Table 2.
Prospective diagnostic stability and change of BPE
| Proportion of prospective diagnostic stability, mean (95% CI) | Proportion of prospective diagnostic change, mean (95% CI) | |
|---|---|---|
| ATPD | 0.50 (0.42–0.59) | 0.37 (0.29–0.45) |
| BPD | 0.46 (0.34–0.59) | 0.50 (0.39–0.62) |
| BPE (pooled) | 0.49 (0.42–0.56) | 0.41 (0.35–0.48) |
| ATPD v. BPD test for between-group heterogeneity (Q) | 0.30 | 3.47 |
| p value | 0.59 | 0.06 |
| I2 | 97.33 | 97.17 |
ATPD, acute and transient psychotic disorder; BPD, brief psychotic disorder; BPE, brief psychotic episodes.
Fig. 3.
Meta-analysis of prospective diagnostic stability and change of BPE. ATPD, acute and transient psychotic disorder; BPD, brief psychotic disorder
Note: Diagnostic stability and diagnostic change values are not reciprocal, because they were calculated analysing different datasets.
The meta-analytical proportion of prospective diagnostic change (average follow-up 47 months) was 41% (95% CI 35–48) for all BPE: 37% (95% CI 29–45) for ATPD and 50% (95% CI 39–62) for BPD. There were no significant between-group differences (p = 0.063). Specifically, the meta-analytical proportion of diagnostic change to schizophrenia spectrum psychoses was 19% (95% CI 16–23) for all BPE: 19% (95% CI 15–24) for ATPD, 20% (95% CI 14–28) for BPD (between-group difference p = 0.770); to affective spectrum psychoses: 5% (95% CI 3–7) for all BPE, 1% (95% CI 0.6–2) for ATPD, 10% (95% CI 6–15) for BPD (between-group difference p < 0.01); to other psychotic disorders: 7% (95% CI 5–9) for all BPE, 3% (95% CI 2–5) for ATPD, 12% (95% CI 8–16) for BPD (between-group difference p < 0.010); to other (non-psychotic) mental disorders: 14% (95% CI 11–17) for all BPE, 14% (95% CI 12–18) for ATPD, 14% (95% CI 8–23) for BPD (between-group difference p = 0.950).
The meta-analytical prospective diagnostic stability for APPD without symptoms of schizophrenia (average follow-up 51 months) was 56% (95% CI 46–66), prospective diagnostic change was 34% (95% CI 24–46), proportion of diagnostic change to schizophrenia spectrum psychoses was 18% (95% CI 11–30) and of other (non-psychotic) mental disorders was 17% (10–26%) (online Supplementary eFig. 1). There were not enough data to meta-analyse change from APPD to affective spectrum psychoses or to other psychotic disorders.
Remission
There were not enough data to meta-analyse this outcome. Four studies (two BPD and two ATPD samples) (Rahm and Cullberg, 2007; Castagnini et al., 2008; Castro-Fornieles et al., 2011; Bjorkenstam et al., 2013) reported proportion of remitted patients, defined as not having any mental disorder at follow-up, ranging from 14 (Castagnini et al., 2008) to 67% (Rahm and Cullberg, 2007).
Quality of life
There were not enough data to meta-analyse this outcome. Two studies reported outcomes related to quality of life. One study (Aadamsoo et al., 2011) found that the World Health Organization Quality of Life scale (WHO-QoL) scores were not significantly different between ATPD and schizophrenia at baseline, but it became better in ATPD at follow-up. Another study (Satghare et al., 2020) reported that BPD, but not schizophrenia, is positively correlated with WHO-QoL scores at baseline.
Functional/vocational status
Twelve samples (907 patients) (nine ATPD, two BLIPS, one BPD) reported the functional/vocational status. The meta-analytical proportion of patients with BPE who were employed at baseline was 48% (95% CI 38–58). There were not enough data to meta-analyse this outcome at follow-up.
Mortality
There were not enough data to meta-analyse this outcome. Three studies (Castagnini et al., 2008, 2013a; Korner et al., 2009), all including ATPD samples, independently reported a proportion of deaths of 17.0% at 60 months follow-up (Castagnini et al., 2008), 5.6% at 84 months (Castagnini et al., 2013a) and 33.5% at 96 months (Korner et al., 2009).
Predictors of clinical outcomes
Ten studies reported predictors for psychotic recurrence in BPE (Table 3). No factor was consistently associated with psychotic recurrence. Predictors of diagnostic stability partially overlap (but not consistently) with predictors of recurrence, with studies suggesting that older age at onset (Aadamsoo et al., 2011; Queirazza et al., 2014; Poon and Leung, 2017; Wang et al., 2018), female gender (Singh et al., 2004; Castagnini et al., 2013b; Castagnini and Foldager, 2014; Queirazza et al., 2014; Wang et al., 2018), abrupt onset (Sajith et al., 2002; Rusaka and Rancans, 2014a), seriously disorganising or dangerous symptoms (Fusar-Poli et al., 2017a), polymorphic symptomatology and absence of schizophrenic features at onset (Sajith et al., 2002; Aadamsoo et al., 2011; Salvatore et al., 2011; Castagnini et al., 2013b; Rusaka and Rancans, 2014a, 2014b) predict higher diagnostic stability (Lopez-Diaz et al., 2020). One study suggested that female gender was associated with early remission (Esan and Fawole, 2014). There were no predictors of quality of life, functional/vocational status or mortality.
Table 3.
Predictors of psychotic recurrence in BPE (ATPD/BPD/BLIPS/BIPS)
| Predictor | Association with psychotic recurrence |
|---|---|
| Acute onset | ↓(Rusaka and Rancans, 2014b) ↔ (Rusaka and Rancans, 2014b; Fusar-Poli et al., 2019a, 2019b, 2019c) |
| Acute stress | ↔(Fusar-Poli et al., 2019a, 2019b, 2019c) |
| Affective disturbances | ↔(Rusaka and Rancans, 2014a, 2014b) |
| Antipsychotic dosage | ↑(Wang et al., 2018) |
| Anxiety | ↑ (Rusaka and Rancans, 2014a); ↔(Suda et al., 2005; Rusaka and Rancans, 2014b) |
| Delusional ideation | ↔(Suda et al., 2005; Rusaka and Rancans, 2014a, 2014b) |
| Depressed mood | ↔(Suda et al., 2005; Rusaka and Rancans, 2014a, 2014b) |
| Duration of psychotic symptoms | ↔(Fusar-Poli et al., 2017a, 2019a, 2019b, 2019c; Wang et al., 2018) |
| Duration/number of hospitalisations over follow-up | ↑(Aadamsoo et al., 2011; Queirazza et al., 2014; Poon and Leung, 2017; Wang et al., 2018); ↔(Suda et al., 2005; Rusaka and Rancans, 2014b) |
| Employment | ↔(Aadamsoo et al., 2011; Fusar-Poli et al., 2017a) |
| Ethnicity | ↔(Fusar-Poli et al., 2017a) |
| Family history of mental disorders | ↑(Wang et al., 2018); ↔(Suda et al., 2005; Abe et al., 2006; Rusaka and Rancans, 2014b; Poon and Leung, 2017) |
| Frequency of episodes over follow-up | ↑(Fusar-Poli et al., 2017a); ↔ (Suda et al., 2005) |
| Hallucinations | ↑(Rusaka and Rancans, 2014a); ↔ (Suda et al., 2005; Rusaka and Rancans, 2014b) |
| Hazardousness | ↔(Aadamsoo et al., 2011) |
| Illicit substances | ↔(Fusar-Poli et al., 2019a, 2019b, 2019c) |
| Irritability or mood elation | ↔(Suda et al., 2005) |
| Level of functioning | ↔(Aadamsoo et al., 2011; Fusar-Poli et al., 2017a) |
| Life events | ↔(Suda et al., 2005; Abe et al., 2006) |
| Male gender | ↑(Queirazza et al., 2014; Wang et al., 2018); ↔(Suda et al., 2005; Abe et al., 2006; Aadamsoo et al., 2011; Fusar-Poli et al., 2017a; Poon and Leung, 2017) |
| Marital status | ↔(Aadamsoo et al., 2011; Fusar-Poli et al., 2017a) |
| Polymorphic symptomatology | ↓(Rusaka and Rancans, 2014a); ↔(Suda et al., 2005; Rusaka and Rancans, 2014b) |
| Poor premorbid social functioning | ↑(Suda et al., 2005); ↔(Suda et al., 2005; Rusaka and Rancans, 2014b) |
| Quality of life | ↔(Aadamsoo et al., 2011) |
| Seriously disorganising or dangerous symptoms | ↑(Fusar-Poli et al., 2017a, 2019a, 2019b, 2019c) |
| Severity of psychotic symptoms | ↔(Aadamsoo et al., 2011; Fusar-Poli et al., 2017a) |
| Sleep disturbances | ↑ (Suda et al., 2005); ↔(Suda et al., 2005; Rusaka and Rancans, 2014a, 2014b) |
| Thought disorder | ↑(Suda et al., 2005); ↔(Suda et al., 2005; Rusaka and Rancans, 2014a, 2014b) |
| Years of education | ↔(Aadamsoo et al., 2011) |
| Younger age | ↑(Abe et al., 2006; Aadamsoo et al., 2011; Queirazza et al., 2014; Poon and Leung, 2017; Wang et al., 2018); ↔(Suda et al., 2005; Rusaka and Rancans, 2014b; Fusar-Poli et al., 2017a) |
BPE, brief psychotic episodes.
↑: predictor is associated with higher risk of psychotic recurrence.
↔: predictor is not associated with a change in psychotic recurrence.
↓: predictor is associated with lower risk of psychotic recurrence.
Sensitivity analyses
Excluding one study at a time at each follow-up point for primary outcome confirmed the robustness of the findings (sensitivity plots are presented in the online Supplementary eFigs 2a–d).
Heterogeneity and multiple meta-regression
Heterogeneity (I2) ranged from 43.8% at 24 months to 84.6% at ⩾36 months for risk of psychotic recurrences (online Supplementary eResults 1). Significant multiple meta-regression analyses (online Supplementary eTable 4) associated the female ratio (β = 0.0040; f = 4.03, p = 0.022) with a lower proportion of recurrence; study quality (β = 0.0018; f = 3.47, p = 0.036) and with higher proportion of recurrence (scatterplots are depicted in online Supplementary eFigs 3 and 4).
Publication bias
Visual inspection of the funnel plot did not reveal publication bias. Egger's test for funnel plot asymmetry was not significant (p = 0.27). There was no meta-regression association between sample size and psychotic recurrence (online Supplementary eFigs 5a–c).
Discussion
To our best knowledge, this is the first systematic review and meta-analysis to have appraised multiple clinical outcomes across several operationalisations of BPE. We showed that these patients have a high risk of developing psychotic recurrences, in particular schizophrenia spectrum psychoses, and high proportion of baseline unemployment, while there were not enough data to explore remission, quality of life and mortality and no consistent factors predicting outcomes. As one in two patients presenting with short-lived psychotic episodes is at risk of recurrences, close monitoring and secondary preventive strategies should be systematically implemented for this vulnerable patient group.
This is the largest meta-analysis of BPE, which encompasses four operationalisations (ATPD, BPD, BLIPS and BIPS) over 91 independent articles and 15 729 individuals. Their mean age of about 31 years falls in the upper range of the 15–35-year window for highest risk of psychosis in the general population (Radua et al., 2018). A recent meta-analysis of epidemiological studies completed by our group confirmed that the peak age at onset is 18.5 years, and the median age of onset for ATPD is past 30 years (at 35 years), compared to 25 years for schizophrenia spectrum disorder (Solmi et al., 2021). Despite a variable pattern of course and outcome reported by the individual studies, reflected by the high levels of heterogeneity in our analyses, we found that about one-third of patients with BPE will develop a psychotic recurrence after 3 years. In the short term, the BIPS group showed a higher risk of psychotic recurrence. This finding is in line with previous evidence highlighting the substantial higher level of risk in BLIPS/BIPS subgroups compared to other CHR-P subgroups (APS and GRD) (Fusar-Poli et al., 2016b). The higher risk of recurrence in BIPS might be related to its 3-month duration criteria, compared to 7-days in BLIPS and 1 month in BPD and most ATPD subtypes. A longer duration of baseline psychotic symptoms is expected to increase the risk of recurrence (Aadamsoo et al., 2011; Queirazza et al., 2014; Poon and Leung, 2017; Wang et al., 2018). We also demonstrated that the presence of seriously disorganising or dangerous features within BLIPS/BIPS is associated with an extreme risk of psychotic recurrence over time (90% at 5-years) (Fusar-Poli et al., 2017a). However, these differences of risk for psychotic recurrences across operationalisations were not maintained in the long term. Importantly, we observed that the risk of psychotic recurrence continues increasing up to 3 years, suggesting that these patients should be offered clinical monitoring and relapse prevention strategies for at least 3 years after their index episode (Fusar-Poli et al., 2017b, 2020; Rutigliano et al., 2018). Unfortunately, first-episode services tend to discharge patients who have spontaneously remitted from an initial episode of psychosis, whereas CHR-P services typically cap their care at 2 years only (the average duration of care in these teams is of 24 months; Salazar de Pablo et al., 2021). Consequently, patients with BPE have several unmet needs that are not addressed by current mental health services. For example, only 3% of BLIPS engage with the minimum effective dose of cognitive behavioural therapy, which is also of questionable efficacy for this patient population (Fusar-Poli et al., 2019a, 2019b, 2021a).
We also showed that about half of patients with BPE will retain the initial diagnoses, compared to 90% in schizophrenia (90%) (Fusar-Poli et al., 2016c). About 19% of BPE is being rediagnosed as schizophrenia spectrum psychoses, 5% as affective spectrum psychoses (higher in BPD than ATPD), 7% as other psychotic disorders (higher in BPD than ATPD) and 14% other (non-psychotic) mental disorders. These findings corroborate the conceptual foundations of BPE, which are not static nosological entities (Ey, 1954; Pillmann and Marneros, 2003), but have an intrinsically dynamic nature. Diagnostic changes are therefore to be expected, reflecting the natural trajectory of the disorders. This presents an unprecedented empirical prognostic and preventive opportunity for clinical practice, overcoming the sterile discussion about prospective instability of static diagnostic snapshots (Fusar-Poli et al., 2018).
Notably, our sensitivity analyses provided useful data in view of the forthcoming ICD-11 revisions. The APPD without symptoms of schizophrenia showed a 21% meta-analytic risk of psychotic recurrence (at 51 months), a prospective diagnostic stability comparable to the whole ATPD group (56 v. 49%), as well as a comparable proportion of diagnostic change to schizophrenia spectrum psychoses (18 v. 19%) and of other (non-psychotic) mental disorders (17 v. 14%). These findings do not align with the arguments made by the ICD-11 Panel that APPD is ‘not indicative of schizophrenia’ (Reed et al., 2019). The ICD-11 field study also showed that the ICD-11 ATPD diagnostic reliability (moderate: kappa = 0.45) is lower than for the ICD-10 ATPD (Reed et al., 2018). Some authors have argued that ICD-11 ATPD category is too narrow and may counter-productively reduce its clinical utility (Castagnini and Berrios, 2019).
We also uncovered gaps of knowledge because evidence relating to remission, functional status, quality of life and mortality in brief psychoses is still to sparse and insufficient. For example, most studies addressing quality of life focused on first-episode psychosis without distinguishing across short lived and persistent disorders (Sevilla-Llewellyn-Jones et al., 2019; Tan et al., 2019; Satghare et al., 2020). We were only able to meta-analyse the proportion of patients with brief psychoses who were employed at baseline (48%) and we uncovered no robust and replicated predictors of any outcomes in short-lived psychotic episodes. Our meta-regressions confirm previous findings underlining reduced risk for transition to schizophrenia in females (Queirazza et al., 2014; Radua et al., 2018; Wang et al., 2018). Overall, it is unlikely that single prognostic factors can be robustly associated with this complex and evolving condition. Some multivariable prognostic models that can forecast clinical outcomes in patients with BPE have been developed (Lopez-Diaz et al., 2020; Fusar-Poli, 2021). We have recently developed and internally validated (3018 individuals with short-lived psychotic episodes, up to 8 years of follow-up) an individualised clinical prediction model based on Electronic Health Records which adequately predicts the long-term risk of psychotic recurrence in this patient group (prognostic accuracy = 0.7, Damiani et al., 2021). This clinical prediction models retained adequate prognostic performance when tested in the context of the ICD-11 changes to this groups and could further be improved by incorporating a dynamic component (Lopez-Diaz et al., 2020; Studerus et al., 2020) which better captures the evolving nature of this condition.
Overall, based on the findings of this study best practice affords for patients with short-lived psychotic episodes would require repeated clinical monitoring bolstered by complementary relapse prevention strategies (Alvarez-Jimenez et al., 2016) for at least 3 years follow-up, to align with the current early intervention recommendations (Chandra et al., 2018). At a research level, larger prospective studies with a harmonised set of assessment and outcome measures are needed to further advance precision psychiatry efforts that are essential in this field. Future clinical and research perspective have been fully elaborated in an independent study (Fusar-Poli et al., 2021b). The limitations are appended in the online Supplementary eLimitations.
Conclusions
Short-lived psychotic episodes are associated with a high risk of psychotic recurrences, in particular schizophrenia spectrum disorders. Other clinical outcomes remain relatively underinvestigated. There are no consistent prognostic/predictive factors.
Financial support
None.
Availability of data and materials
The authors give no permission to share raw data.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796021000548.
click here to view supplementary material
Conflict of interest
PFP received honoraria or grant fees from Lundbeck, Angelini and Menarini in the past 36 months outside the current work.
References
- Aadamsoo K, Saluveer E, Kueuenarpuu H, Vasar V and Maron E (2011) Diagnostic stability over 2 years in patients with acute and transient psychotic disorders. Nordic Journal of Psychiatry 65, 381–388. [DOI] [PubMed] [Google Scholar]
- Abe T, Otsuka K and Kato S (2006) Long-term clinical course of patients with acute polymorphic psychotic disorder without symptoms of schizophrenia. Psychiatry and Clinical Neurosciences 60, 452–457. [DOI] [PubMed] [Google Scholar]
- Alvarez-Jimenez M, O'Donoghue B, Thompson A, Gleeson JF, Bendall S, Gonzalez-Blanch C, Killackey E, Wunderink L and McGorry PD (2016) Beyond clinical remission in first episode psychosis: thoughts on antipsychotic maintenance vs. guided discontinuation in the functional recovery era. CNS Drugs 30, 357–368. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association. [Google Scholar]
- Bjorkenstam E, Bjorkenstam C, Hjern A, Reutfors J and Boden R (2013) A five year diagnostic follow-up of 1840 patients after a first episode non-schizophrenia and non-affective psychosis. Schizophrenia Research 150, 205–210. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J and Rothstein H (2013) Comprehensive Meta-Analysis Version 3. Englewood, NJ: Biostat. [Google Scholar]
- Castagnini A and Berrios GE (2019) Approach to refine ICD-11 acute and transient psychotic disorder (polymorphic psychotic disorder). Schizophrenia Research 212, 239–240. [DOI] [PubMed] [Google Scholar]
- Castagnini A and Foldager L (2014) Epidemiology, course and outcome of acute polymorphic psychotic disorder: implications for ICD-11. Psychopathology 47, 202–206. [DOI] [PubMed] [Google Scholar]
- Castagnini A, Bertelsen A and Berrios GE (2008) Incidence and diagnostic stability of ICD-10 acute and transient psychotic disorders. Comprehensive Psychiatry 49, 255–261. [DOI] [PubMed] [Google Scholar]
- Castagnini A, Foldager L and Bertelsen A (2013a) Excess mortality of acute and transient psychotic disorders: comparison with bipolar affective disorder and schizophrenia. Acta Psychiatrica Scandinavica 128, 370–375. [DOI] [PubMed] [Google Scholar]
- Castagnini A, Foldager L and Bertelsen A (2013b) Long-term stability of acute and transient psychotic disorders. Australian and New Zealand Journal of Psychiatry 47, 59–64. [DOI] [PubMed] [Google Scholar]
- Castro-Fornieles J, Baeza I, de la Serna E, Gonzalez-Pinto A, Parellada M, Graell M, Moreno D, Otero S and Arango C (2011) Two-year diagnostic stability in early-onset first-episode psychosis. Journal of Child Psychology and Psychiatry 52, 1089–1098. [DOI] [PubMed] [Google Scholar]
- Catalan A, Salazar de Pablo G, Vaquerizo Serrano J, Mosillo P, Baldwin H, Fernández-Rivas A, Moreno C, Arango C, Correll CU, Bonoldi I and Fusar-Poli P (2020) Annual research review: prevention of psychosis in adolescents – systematic review and meta-analysis of advances in detection, prognosis and intervention. Journal of Child Psychology and Psychiatry 62, 657–673. [DOI] [PubMed] [Google Scholar]
- Chandra A, Patterson E and Hodge S (2018) Standards for Early Intervention in Psychosis Services, 1st Edn., London: EPIN CCQI. [Google Scholar]
- Damiani A, Rutigliano G, Fazia T, Berzuini C, Bernardinelli LP and Fusar-Poli P (2021) Developing and validating an individualised clinical prediction model to forecast psychotic recurrence in acute and transient psychotic disorders: electronic health record cohort study. Schizophrenia Bulletin 47, 1695–1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esan O and Fawole OI (2014) Acute and transient psychotic disorder in a developing country. International Journal of Social Psychiatry 60, 442–448. [DOI] [PubMed] [Google Scholar]
- Ey H (1954) Bouffées délirantes et psychoses hallucinatoires aiguës. Études Psychiatriques T III, étude 23, 201. [Google Scholar]
- Fusar-Poli P (2019) TRANSD recommendations: improving transdiagnostic research in psychiatry. World Psychiatry 18, 361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P (2021) New electronic health records screening tools to improve detection of emerging psychosis. Frontiers in Psychiatry 12, 698406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Bonoldi I, Hui LM, Rutigliano G, Stahl DR, Borgwardt S, Politi P, Mishara AL, Lawrie SM, Carpenter WT Jr and McGuire PK (2016a) Prognosis of brief psychotic episodes: a meta-analysis. JAMA Psychiatry 73, 211–220. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Borgwardt S, Woods SW, Addington J, Nelson B, Nieman DH, Stahl DR, Rutigliano G, Riecher-Rossler A, Simon AE, Mizuno M, Lee TY, Kwon JS, Lam ML, Perez J, Keri S, Amminger P, Metzler S, Kawohl W, Rossler W, Lee J, Labad J, Ziermans T, An SK, Liu CC, Woodberry KA, Braham A, Corcoran C, McGorry P, Yung AR and McGuire PK (2016b) Heterogeneity of psychosis risk within individuals at clinical high risk a meta-analytical stratification. JAMA Psychiatry 73, 113–120. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Rutigliano G, Heslin M, Stahl D, Brittenden Z, Caverzasi E, McGuire P and Carpenter WT (2016c) Diagnostic stability of ICD/DSM first episode psychosis diagnoses: meta-analysis. Schizophrenia Bulletin 42, 1395–1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, De Micheli A, Rutigliano G, Bonoldi I, Tognin S, Ramella-Cravaro V, Castagnini A and McGuire PK (2017a) Diagnostic and prognostic significance of brief limited intermittent psychotic symptoms (BLIPS) in individuals at ultra high risk. Schizophrenia Bulletin 43, 48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Rutigliano G, Stahl D, Davies C, De Micheli A, Ramella-Cravaro V, Bonoldi I and McGuire P (2017b) Long-term validity of the at risk mental state (ARMS) for predicting psychotic and non-psychotic mental disorders. European Psychiatry 42, 49–54. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Hijazi Z, Stahl D and Steyerberg EW (2018) The science of prognosis in psychiatry: a review. JAMA Psychiatry 75, 1289–1297. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Davies C, Solmi M, Brondino N, De Micheli A, Kotlicka-Antczak M, Shin JI and Radua J (2019a) Preventive treatments for psychosis: umbrella review (just the evidence). Frontiers in Psychiatry 11, 764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, De Micheli A, Chalambrides M, Singh A, Augusto C and McGuire P (2019b) Unmet needs for treatment in 102 individuals with brief and limited intermittent psychotic symptoms (BLIPS): implications for current clinical recommendations. Epidemiology and Psychiatric Sciences 29, e67–e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Solmi M, Brondino N, Davies C, Chae C, Politi P, Borgwardt S, Lawrie SM, Parnas J and McGuire P (2019c) Transdiagnostic psychiatry: a systematic review. World Psychiatry 18, 192–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, De Micheli A, Signorini L, Baldwin H, Salazar de Pablo G and McGuire P (2020) Real-world long-term outcomes in individuals at clinical risk for psychosis: the case for extending duration of care. EClinicalMedicine 28, 100578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Davies C and Jauhar S (2021a) Lack of robust meta-analytic evidence to favour cognitive behavioural therapy for prevention of psychosis. World Psychiatry 20, 443–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Salazar de Pablo G, Rajkumar RP, Lopez-Diaz A, Malhotra S, Heckers S, Lawrie S and Pillmann F (2021b) Diagnosis, prognosis and treatment of brief psychotic episodes: a review and research agenda. The Lancet. Psychiatry, in press. [DOI] [PubMed] [Google Scholar]
- Gaebel W (2012) Status of psychotic disorders in ICD-11. Schizophrenia Bulletin 38, 895–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korner A, Lopez AG, Lauritzen L, Andersen PK and Kessing LV (2009) Acute and transient psychosis in old age and the subsequent risk of dementia: a nationwide register-based study. Geriatrics & Gerontology International 9, 62–68. [DOI] [PubMed] [Google Scholar]
- Kraepelin E (1899) Psychiatrie - ein Lehrbuch für Studierende und Ärzte. Leipzig: Barth. [Google Scholar]
- Lipsey MW and Wilson DB (2001) Practical Meta-Analysis. Thousand Oaks: Sage Publications, Inc. [Google Scholar]
- Lopez-Diaz A, Fernandez-Gonzalez JL, Lara I and Ruiz-Veguilla M (2020) Predictors of diagnostic stability in acute and transient psychotic disorders: validation of previous findings and implications for ICD-11. European Archives of Psychiatry and Clinical Neuroscience 270, 291–299. [DOI] [PubMed] [Google Scholar]
- McGlashan TH and Wood SJ (2010) The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-up. New York, NY: Oxford University Press. [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD and Woods SW (2003) Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin 29, 703–715. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J and Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6, e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2014) Psychosis and schizophrenia in adults: prevention and management. NICE guidelines [CG178]. [PubMed]
- Pillmann F and Marneros A (2003) Brief and acute psychoses: the development of concepts. History of Psychiatry 14, 161–177. [DOI] [PubMed] [Google Scholar]
- Pillmann F and Marneros A (2005) Longitudinal follow-up in acute and transient psychotic disorders and schizophrenia. British Journal of Psychiatry 187, 286–287. [DOI] [PubMed] [Google Scholar]
- Poon JYK and Leung CM (2017) Outcome of first-episode acute and transient psychotic disorder in Hong Kong Chinese: a 20-year retrospective follow-up study. Nordic Journal of Psychiatry 71, 139–144. [DOI] [PubMed] [Google Scholar]
- Queirazza F, Semple DM and Lawrie SM (2014) Transition to schizophrenia in acute and transient psychotic disorders. British Journal of Psychiatry 204, 299–305. [DOI] [PubMed] [Google Scholar]
- Radua J, Ramella-Cravaro V, Ioannidis JPA, Reichenberg A, Phiphopthatsanee N, Amir T, Yenn Thoo H, Oliver D, Davies C, Morgan C, McGuire P, Murray RM and Fusar-Poli P (2018) What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 17, 49–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahm C and Cullberg J (2007) Diagnostic stability over 3 years in a total group of first-episode psychosis patients. Nordic Journal of Psychiatry 61, 189–193. [DOI] [PubMed] [Google Scholar]
- Reed GM, Sharan P, Rebello TJ, Keeley JW, Elena Medina-Mora M, Gureje O, Luis Ayuso-Mateos J, Kanba S, Khoury B, Kogan CS, Krasnov VN, Maj M, de Jesus Mari J, Stein DJ, Zhao M, Akiyama T, Andrews HF, Asevedo E, Cheour M, Domínguez-Martínez T, El-Khoury J, Fiorillo A, Grenier J, Gupta N, Kola L, Kulygina M, Leal-Leturia I, Luciano M, Lusu B, Nicolas J, Martínez-López I, Matsumoto C, Umukoro Onofa L, Paterniti S, Purnima S, Robles R, Sahu MK, Sibeko G, Zhong N, First MB, Gaebel W, Lovell AM, Maruta T, Roberts MC and Pike KM (2018) The ICD-11 developmental field study of reliability of diagnoses of high-burden mental disorders: results among adult patients in mental health settings of 13 countries. World Psychiatry 17, 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, Maj M, Stein DJ, Maercker A, Tyrer P, Claudino A, Garralda E, Salvador-Carulla L, Ray R, Saunders JB, Dua T, Poznyak V, Medina-Mora ME, Pike KM, Ayuso-Mateos JL, Kanba S, Keeley JW, Khoury B, Krasnov VN, Kulygina M, Lovell AM, de Jesus Mari J, Maruta T, Matsumoto C, Rebello TJ, Roberts MC, Robles R, Sharan P, Zhao M, Jablensky A, Udomratn P, Rahimi-Movaghar A, Rydelius PA, Bährer-Kohler S, Watts AD and Saxena S (2019) Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry 18, 3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusaka M and Rancans E (2014a) First-episode acute and transient psychotic disorder in Latvia: a 6-year follow-up study. Nordic Journal of Psychiatry 68, 24–29. [DOI] [PubMed] [Google Scholar]
- Rusaka M and Rancans E (2014b) A prospective follow-up study of first-episode acute transient psychotic disorder in Latvia. Annals of General Psychiatry 13, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutigliano G, Merlino S, Minichino A, Patel R, Davies C, Oliver D, De Micheli A, McGuire P and Fusar-Poli P (2018) Long term outcomes of acute and transient psychotic disorders: the missed opportunity of preventive interventions. European Psychiatry 52, 126–133. [DOI] [PubMed] [Google Scholar]
- Sajith SG, Chandrasekaran R, Unni KES and Sahai A (2002) Acute polymorphic psychotic disorder: diagnostic stability over 3 years. Acta Psychiatrica Scandinavica 105, 104–109. [DOI] [PubMed] [Google Scholar]
- Salazar de Pablo G, Estradé A, Cutroni M, Andlauer O and Fusar-Poli P (2021) Establishing a clinical service to prevent psychosis: what, how and when? Systematic review. Translational Psychiatry 11, 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvatore P, Baldessarini RJ, Tohen M, Khalsa HM, Sanchez-Toledo JP, Zarate CA Jr, Vieta E and Maggini C (2011) McLean–Harvard international first-episode project: two-year stability of ICD-10 diagnoses in 500 first-episode psychotic disorder patients. Journal of Clinical Psychiatry 72, 183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satghare P, Abdin E, Shahwan S, Chua BY, Poon LY, Chong SA and Subramaniam M (2020) Subjective quality of life and its associations among first episode psychosis patients in Singapore. International Journal of Environmental Research and Public Health 17, 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevilla-Llewellyn-Jones J, Cano-Domínguez P, de-Luis-Matilla A, Espina-Eizaguirre A, Moreno-Kustner B and Ochoa S (2019) Subjective quality of life in recent onset of psychosis patients and its association with sociodemographic variables, psychotic symptoms and clinical personality traits. Early Intervention in Psychiatry 13, 525–531. [DOI] [PubMed] [Google Scholar]
- Singh SP, Burns T, Amin S, Jones PB and Harrison G (2004) Acute and transient psychotic disorders: precursors, epidemiology, course and outcome. British Journal of Psychiatry 185, 452–459. [DOI] [PubMed] [Google Scholar]
- Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, Shin J, Kirkbride PJ, Kim JH, Kim JY, Carvalho AF, Seeman MV, Correll CU and Fusar-Poli P (2021). Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Molecular Psychiatry. 10.1038/s41380-021-01161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- Studerus E, Beck K, Fusar-Poli P and Riecher-Rössler A (2020) Development and validation of a dynamic risk prediction model to forecast psychosis onset in patients at clinical high risk. Schizophrenia Bulletin 46, 252–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suda K, Hayashi N and Hiraga M (2005) Predicting features of later development of schizophrenia among patients with acute and transient psychotic disorder. Psychiatry and Clinical Neurosciences 59, 146–150. [DOI] [PubMed] [Google Scholar]
- Tan XW, Shahwan S, Satghare P, Chua BY, Verma S, Tang C, Chong SA and Subramaniam M (2019) Trends in subjective quality of life among patients with first episode psychosis – a 1 year longitudinal study. Frontiers in Psychiatry 10, 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H-Y, Guo W-J, Li X-J, Tao Y-J, Meng Y-J, Wang Q, Deng W and Li T (2018) Higher required dosage of antipsychotics to relieve the symptoms of first-onset Acute and Transient Psychotic Disorder (ATPD) predicted the subsequent diagnostic transition to schizophrenia: a longitudinal study. Schizophrenia Research 193, 461–462. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1992) The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneve, Switzerland: World Health Organization. [Google Scholar]
- Yung AR, McGorry PD, McFarlane CA, Jackson HJ, Patton GC and Rakkar A (1996) Monitoring and care of young people at incipient risk of psychosis. Schizophrenia Bulletin 22, 283–303. [DOI] [PubMed] [Google Scholar]
- Yung AR PL, Yuen HP and McGorry PD (2006) Comprehensive Assessment of At-Risk Mental State. Parkville, Australia: PACE Clinic, ORYGEN Research Centre, Dept of Psychiatry, University of Melbourne. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796021000548.
click here to view supplementary material
Data Availability Statement
The authors give no permission to share raw data.