Abstract
As contagious bovine pleuropneumonia (CBPP) is spreading fast in many African countries, there is an increasing demand for rapid and sensitive diagnostic methods that can be used to confirm the initial diagnosis based on clinical symptoms or pathological findings. Two PCR-based diagnostic systems for identification of the infectious agent, Mycoplasma mycoides subsp. mycoides SC (M. mycoides SC), in various samples are presented. Both systems involve group-specific amplification of the two 16S rRNA genes from mycoplasmas of the M. mycoides cluster. The laser-induced fluorescence assay is based on a unique sequence length difference between the two 16S rRNA genes in M. mycoides SC. This region was amplified by PCR, and the products were separated by polyacrylamide gel electrophoresis in a DNA sequencer. The resulting electropherogram showed two peaks for strains of M. mycoides SC and one peak for all other members of the M. mycoides cluster. The second system was based on restriction endonuclease analysis and agarose gel electrophoresis. Restriction of amplicons from a region containing a polymorphism, which is found in M. mycoides SC only, resulted in an extra band on the agarose gel because an AluI site is lacking in the rrnA operon. Specimens from cows with postmortem signs of CBPP were analyzed with the two PCR systems. M. mycoides SC was clearly identified in pleural fluid and lung tissue, and the methods were found to be robust and rapid. The results were in agreement with those obtained by conventional diagnostic techniques.
Contagious bovine pleuropneumonia (CBPP) is a severe respiratory disease affecting cattle. The symptoms range from hyperacute through acute to chronic and subclinical forms (10). Clinical signs of the acute form involve cessation of rumination, nasal discharge, a dry cough, and difficulty in breathing (27, 28). The rate of mortality in affected cattle is low in Europe, while in Africa CBPP causes more losses than any other cattle disease and the mortality rate varies from 10 to 70% (2, 10, 17). CBPP is present in 24 countries of tropical Africa, and the disease has been reported to spread very fast in the eastern and southeastern countries (14). In Europe, sporadic outbreaks of CBPP occur in the regions of endemicity in northwestern Portugal, and one or more outbreaks have been recorded yearly in Spain since 1991 (10, 23).
Mycoplasma mycoides subsp. mycoides SC (M. mycoides SC), the infectious agent of CBPP, was first isolated and described by Nocard and Roux in 1898 (18). Nearly 60 years later the organism was identified as a mycoplasma, and it was given its present name (9). Phylogenetic classification has grouped M. mycoides SC into the Mycoplasma mycoides cluster of the spiroplasma group, together with eight closely related mycoplasmas: Mycoplasma capricolum subsp. capricolum, Mycoplasma capricolum subsp. capripneumoniae, Mycoplasma mycoides subsp. mycoides type LC, Mycoplasma mycoides subsp. capri, Mycoplasma sp. bovine group 7, Mycoplasma cottewii, Mycoplasma yeatsii, and Mycoplasma putrefaciens (12, 21, 29). The latter three species are not included in the classical M. mycoides cluster. Mycoplasma sp. bovine group L (1) is believed to belong to the classical M. mycoides cluster.
The species within the classical M. mycoides cluster are difficult to distinguish by morphological and biochemical analyses. Many diagnostic methods for CBPP are based on serological reactions like those in enzyme-linked immunosorbent assays (ELISA), complement fixation tests, immunohistochemical tests, and protein immunoblotting, methods which can be time-consuming and some of which are not sufficiently specific or sensitive (7, 16). Furthermore, recent reports on variable surface proteins of mycoplasmas indicate that ambiguous results may occur when monospecific antibodies are used in diagnostics based on antigen detection (25, 26, 30).
PCR has the advantage of being a fast, specific, and very sensitive technique. Most of the diagnostic PCR systems which are used today (3, 8, 13, 15) are designed to target the CAP-21 gene, whose gene product has an unknown function. Alternative diagnostic PCR systems based on other parts of the genome can be useful. The 16S rRNA genes provide well-examined sequences with segments of different evolutionary variability, which are ideal target regions for primers in group-specific or species-specific amplification. Mycoplasmas belonging to the M. mycoides cluster have two rRNA operons (20). Species identification based on PCR of the 16S rRNA genes and restriction in positions where unique differences (polymorphisms) occur between the two operons has been demonstrated previously for M. capricolum subsp. capripneumoniae (24).
This study comprises the design and evaluation of two diagnostic systems based on PCR of the 16S rRNA genes. The aim of the first system was to achieve a highly sensitive PCR which would be suitable for large-scale diagnostic screening. The aim of the other system was to obtain a robust PCR assay which can be used in laboratories equipped with a thermocycler.
MATERIALS AND METHODS
Mycoplasma strains, cultivation, and sample preparation.
The mycoplasmas used in this study and their geographical origins are listed in Table 1. All strains were grown in F medium (4) except strains L2, Gladysdale, KH3J, 94111, Filfili, 9050-529/1, V5, and 6479, which were kindly provided by J. Frey (Institute for Veterinary Bacteriology, Berne, Switzerland) as DNA samples. Cells from 1 ml of culture were washed once in phosphate-buffered saline (PBS), resuspended in 1 ml of water, and lysed by heating the suspension to 100°C for 5 min. The suspension was chilled on ice and stored at −20°C until use.
TABLE 1.
Mycoplasma strains and their origins
| Species | Strain | Origin | IS1296 patterna |
|---|---|---|---|
| Mycoplasma capricolum subsp. capricolum | California kidT | United States | |
| B304 | Portugal | ||
| Mycoplasma capricolum subsp. capripneumoniae | F38T | Kenya | |
| 7/1a | Oman | ||
| Mycoplasma mycoides subsp. capri | PG3T | Turkey | |
| Mycoplasma mycoides subsp. mycoides LC | Y-goatT | Australia | |
| 1456-11 | Israel | ||
| G10 | Sweden | ||
| D2482 | Switzerland | ||
| Mycoplasma mycoides subsp. mycoides SC | PG1T | Unknown | P |
| Gladysdale | Australia | A1 | |
| V5 | Australia | A7 | |
| Afadé | Chad | A1 | |
| I 57/13 | Italy | E1b | |
| L2 | Italy | E1 | |
| 6479 | Italy | E2 | |
| 130/20p | Italy | NDc | |
| 438/20p | Italy | ND | |
| Bf138d | Italy | ND | |
| 9050-529/1 | Ivory Coast | A5 | |
| B 421 | Portugal | E1b | |
| C 425e | Portugal | ND | |
| O 326f | Portugal | E1 | |
| B345/94 | Portugal | ND | |
| B674/93 | Portugal | ND | |
| 94111 | Rwanda | A6 | |
| Filfili | Senegal | A3 | |
| Madrid | Spain | ND | |
| Segovia | Spain | ND | |
| Cantabria | Spain | ND | |
| Asturias | Spain | ND | |
| KH3J | Sudan | A2 | |
| M223/90 | Tanzania | A1b | |
| T1Sr49 | Tanzania | ND | |
| Mycoplasma sp. bovine group 7 | PG50T | Australia | |
| D318b | Germany | ||
| Calf1 | Nigeria | ||
| 4055 | Portugal | ||
| Mycoplasma sp. bovine group L | B144P | United States | |
| Mycoplasma cottewii | VIST | Australia | |
| Mycoplasma putrefaciens | KS-1T | United States | |
| Mycoplasma yeatsii | GIHT | Australia | |
| Mycoplasma bovigenitalium | PG11T | United Kingdom | |
| Mycoplasma bovirhinis | M213/84 | Sweden | |
| Mycoplasma bovis | DonettaT | United States | |
| Mycoplasma bovoculi | M165/69T | Canada | |
| Mycoplasma canis | PG14T | United Kingdom |
IS1296 pattern of M. mycoides SC according to Cheng et al. (6).
Determined by X. Cheng and J. Frey for this work.
ND, not determined.
Isolated from a buffalo.
Isolated from a goat.
Isolated from a sheep.
Clinical material such as pleural fluid, lung effusion, or minced lung tissue was applied to Whatman 3MM chromatography paper, allowed to dry, and sent to us by mail. The exposed spots of 2 cm in diameter were excised, placed in 50 μl of PBS, incubated at room temperature for 30 min, and then heated to 100°C for 5 min. The samples were chilled and stored as described above.
A piece of frozen lung tissue from a Tanzanian cow was obtained for analysis. DNA from the tissue was prepared by homogenizing the lung piece thoroughly in PBS, treating the mixture with proteinase K, and performing two phenol extractions. After ethanol precipitation of the aqueous phase, the DNA was dissolved in sterile water and stored at −20°C.
PCR of the 16S rRNA genes from the rrnA and rrnB operons.
Double-stranded DNA to be used for solid-phase sequencing was generated in two seminested amplification reactions as described by Pettersson et al. (20, 22). In the first reaction, the rrnA and rrnB operons were amplified simultaneously with primers which are complementary to the universal regions U1 and U8 at the termini of the 16S rRNA genes (11). Subsequent seminested amplifications were used to produce biotinylated amplicons from the U1 to the U5 region (about 900 bp) and from the U2 to the U8 region (about 1,250 bp) which were suitable for immobilization on superparamagnetic beads.
The DNA template for cycle sequencing reactions was produced by direct U1-to-U8 amplification with the Advantage cDNA PCR Kit (Clontech Laboratories, Inc., Palo Alto, Calif.) according to the manufacturer's recommendations. The temperature profile was as described (20).
rrnB-specific amplification.
For members of the M. mycoides cluster it is possible to amplify the rrnB operon separately with primers that are complementary to the flanking regions of the 16S rRNA gene. This amplicon can be used to determine the operon-specific sequence in polymorphic sites as described previously (22). The nested reactions which generated amplicons from U1 to U5 and from U2 to U8 for the solid-phase DNA sequencing were performed as above.
Solid-phase DNA sequencing.
Biotinylated PCR products were immobilized on streptavidin-coated superparamagnetic beads, and the strands were separated as described by the manufacturer (Dynal AS, Oslo, Norway). Sequencing reactions were prepared from both strands with the Cy5 AutoRead Sequencing Kit (Amersham Pharmacia Biotech, Uppsala, Sweden), and the sequences were determined with the ALFexpress DNA Sequencer (Amersham Pharmacia Biotech). Sequence data were exported in PC/Gene format and assembled by using ASSEMGEL software, which is included in the PC/Gene package (Intelligenetics Inc., Mountain View, Calif.).
Cycle sequencing.
To reduce the manual work in the sequencing procedure, some strains were analyzed by cycle sequencing instead of solid-phase sequencing. The PCR product covering the region U1 to U8 was diluted sixfold in sterile water, and the sequencing reactions were prepared according to the manufacturer's recommendations for dye primer sequencing (Thermo Sequenase fluorescent labelled primer cycle sequencing kit with 7-deaza-dGTP; Amersham Pharmacia Biotech). The reactions were run for 25 cycles with 30 s of annealing and extension at 60°C and 30 s of denaturation at 95°C. Electrophoresis and analyses were performed as for solid-phase sequencing.
Analysis by PCR and LIF.
Oligonucleotide primers (Table 2) to be used for PCR–laser-induced fluorescence (LIF) were synthesized and purified by fast protein liquid chromatography by Amersham Pharmacia Biotech. The forward primer F-SCAP, which has a Cy5 label in the 5′ end, targets the 3′ end of the universal region U6 and the 5′ end of the variable region V9 in the two 16S rRNA genes. The reverse primer R-SCAP is complementary to a sequence in the universal region U7. Amplification was carried out in a mixture of 10 mM Tris-HCl buffer (pH 8.3), 2 mM MgCl2, 50 mM KCl, 0.1% Tween, 0.8 mM deoxynucleoside triphosphate (dNTP), 5 pmol of the forward primer, 5 pmol of the reverse primer, and 0.6 U of AmpliTaq DNA polymerase (Roche Molecular Systems, Inc., Branchburg, N.J.) in a total volume of 50 μl. Target DNA was either 5 ng of pure genomic DNA, 1 μl of a heat-lysed cell suspension, 1 μl of a pleural-fluid suspension, or 500 ng of a lung tissue preparation. The reactions were performed in a Techne (Cambridge, United Kingdom) Thermocycler. Denaturation for 3 min at 96°C was followed by 28 cycles consisting of 30 s of denaturation at 96°C, 30 s of annealing at 60°C, and 2 min of extension at 72°C, and finally extension was prolonged for 5 min at 72°C in the last cycle. Electrophoresis and analysis of the amplicons were carried out with the ALFexpress DNA Sequencer and Fragment Manager software (FM v. 1.2; Amersham Pharmacia Biotech). A denaturing acrylamide gel (8% acrylamide and 7 M urea) was prepared by adding 1.6 ml of a stock solution of 40% acrylamide to 25 ml of ALF-grade Ready Mix Gel (Amersham Pharmacia Biotech), and the gel was cast in a short gel cassette with a vertical length of 15 cm and a thickness of 0.3 mm. The PCR product was diluted in sterile water when required, and 4 μl was mixed with 5 fmol of Cy5-labeled size markers of 100 and 200 bp in a formamide-containing loading dye. The samples were loaded onto the gel, and an external size marker with 50-bp spacing was loaded in two lanes. Electrophoresis was run in 0.6× TBE buffer (10× TBE buffer contained 1 M Tris base, 1 M boric acid, and 20 mM EDTA) at 1,500 V, 60 mA, 25 W, and 55°C with a sampling interval of 2 s. To overcome situations where light from a sample in one lane is transferred into the detector of the adjacent lane, samples were first loaded in every second well, electrophoresis was run for 4 min, and then the rest of the samples were loaded in the remaining wells. This time shift minimized the risk of false-positive data.
TABLE 2.
Oligonucleotide primers used for the PCR-LIF and PCR-REA systems
| Name | Position in the 16S rRNA genesa | Sequence |
|---|---|---|
| F-SCAP | 1225–1249 | 5′-Cy5-GTACAAAGAGTTGCAATCCTGTGAA-3′ |
| R-SCAP | 1353–1330 | 5′-ACCGCGACATAGCTGATTCGCGA-3′ |
| F-REAP | 143–168 | 5′-GAAACGAAAGATAATACCGCATGTAG-3′ |
| R-REAP | 927–907 | 5′-CCACTTGTGCGGGTCCCCGTC-3′ |
Numbering conforms to the consensus sequence of the 16S rRNA genes of the M. mycoides cluster (22).
Diagnosis by PCR-REA.
The PCR for subsequent restriction endonuclease analysis (REA) amplifies a segment in the 16S rRNA genes of the rrnA and the rrnB operons for species belonging to the classical M. mycoides cluster. The forward primer F-REAP targets the variable region V2, and the reverse primer R-REAP is complementary to the universal region U5 in the 16S rRNA genes. Oligonucleotide sequences and positions are listed in Table 2. All amplifications were performed in a reaction mixture consisting of 50 mM KCl, 4 mM MgCl2, 10 mM Tris-HCl buffer (pH 8.3), 0.8 mM dNTP, 5 pmol of each primer, and 0.6 U of AmpliTaq DNA polymerase in a total volume of 50 μl. Target DNA was either 5 ng of pure genomic DNA, 1 μl of a heat-lysed cell suspension, 1 μl of a pleural-fluid suspension, or 500 ng of a lung tissue preparation. PCR was performed in a Techne Thermocycler for 33 cycles of denaturation at 96°C for 30 s, annealing at 60°C for 30 s, and extension at 72°C for 1 min. The reaction mixtures were preheated to 96°C for 3 min in order to complete denaturation before the first primer annealing step, and the final extension step was kept at 72°C for 5 min. To differentiate M. mycoides SC from the other members of the classical M. mycoides cluster, the PCR product was digested with AluI (Promega Corporation, Madison, Wis.). Restriction was performed in 0.7× B buffer (1× B buffer contains 6 mM Tris-HCl [pH 7.5], 6 mM MgCl2, 50 mM NaCl, and 1 mM dithiothreitol) and bovine serum albumin (0.1 mg/ml) with 5 U of the enzyme for a 20-μl reaction volume, and the mixtures were incubated at 37°C for at least 1 h. The samples were analyzed by agarose gel electrophoresis in 3.2% MetaPhor Agarose (FMC BioProducts, Rockland, Maine).
RESULTS
Sequence analysis of the 16S rRNA genes.
DNA sequencing of 25 M. mycoides SC strains and one of the pleural-fluid samples from Tanzania showed that all strains have identical 16S rRNA genes with two exceptions: the type strain PG1, which had a G/T polymorphism in position 887, where the other strains had guanosines in the two genes, and the Tanzanian field sample, which had a G/T polymorphism in position 829, which normally contains guanosines in both operons. All nucleotide positions are numbered according to the consensus sequence of the 16S rRNA genes of the members of the M. mycoides cluster (22). As reported earlier, the 16S rRNA genes of the PG1T strain has a total of eight polymorphisms and a 2-bp sequence length difference between the genes (22).
Importantly, all sequenced strains contained the poly(A) region where the rrnA has 5 adenosines and the rrnB has 7 adenosines, which is the basis for discrimination of M. mycoides SC with the PCR-LIF system. Also the T/G polymorphism in position 426, which is discriminatory in the PCR-REA system, was found in all analyzed strains. There were no variations in the primer target sequences for the analyzed M. mycoides SC strains.
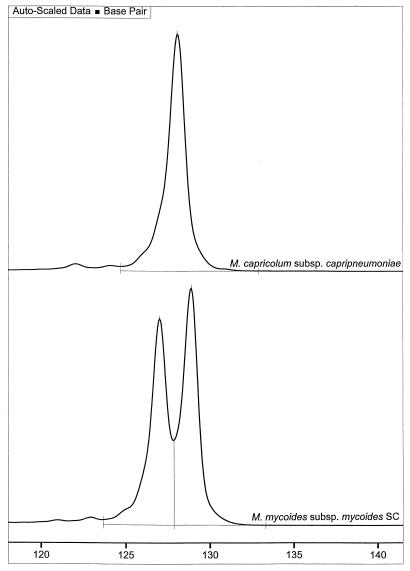
Diagnostic system based on PCR-LIF.
Amplification by the PCR-LIF system resulted in two different amplicons of 127 and 129 bp for all M. mycoides SC strains that were included in the study. These DNA fragments were clearly detected as two peaks in the electropherogram of the sequencer (Fig. 1). The sizes of the fragments were accurately determined when appropriate size standards were co-run with the PCR product and when the FM 1.2 software was used for analyses. Strains of M. capricolum subsp. capricolum, M. capricolum subsp. capripneumoniae, M. mycoides subsp. mycoides type LC, M. mycoides subsp. capri, Mycoplasma sp. bovine group 7, and Mycoplasma sp. bovine group L were amplified by the PCR. However, none of these species contain the insertion and deletion in the poly(A) region between positions 1264 and 1270, and accordingly, equal-sized fragments of 128 bp were produced from the two genes (Fig. 1). The control strains of Mycoplasma bovigenitalium, Mycoplasma bovirhinis, Mycoplasma bovis, Mycoplasma bovoculi, and Mycoplasma canis were not amplified with the SCAP primers. M. cottewii, M. putrefaciens, and M. yeatsii, which all belong to the phylogenetic M. mycoides cluster, were amplified when concentrated template preparations were added to the reaction mixture. The amounts of the PCR products from these species were considerably lower than that of any species of the classical M. mycoides cluster, and they all generated single peaks corresponding to 128 bp in the electropherogram. A mixture of M. mycoides SC and another mycoplasma of the M. mycoides cluster resulted in a misshaped peak upon electrophoresis, but the resolution was too poor to allow separation of the fragments into three distinct entities (data not shown).
FIG. 1.
Electropherogram of samples analyzed by PCR-LIF. The amplicon from M. capricolum subsp. capripneumoniae appeared as a single peak in the electropherogram, and the size was calculated in relation to internal size standards (not shown) as 128.0 bp. Amplicons from M. mycoides SC were clearly detected as two peaks, and the sizes were calculated as 127.0 and 128.9 bp.
The sensitivity of the assay was determined on two different dilution series of culture from strain PG1T. Amplification of a 1-μl suspension from each fraction in either of the dilution series resulted in a detection level corresponding to 0.3 or 0.4 CFU, respectively.
Diagnostic system based on PCR-REA.
Each strain of the classical M. mycoides cluster that was amplified with the REAP primers generated a 785-bp fragment by PCR (Fig. 2A). Further processing of the amplicon by restriction with AluI distinguished M. mycoides SC from the other species. M. mycoides SC has a unique polymorphism located at position 426 of the 16S rRNA gene. The rrnA operon, which has thymidine instead of guanosine in this position, lacks one of the AluI restriction sites. Consequently, AluI restriction of amplicons from M. mycoides SC gives a 370-bp fragment in addition to the 236-, 186-, 184-, 98-, and 81-bp fragments that are shared by all members of the classical M. mycoides cluster (Fig. 2B).
FIG. 2.
Agarose gel electrophoresis of amplicons from mycoplasmas of the M. mycoides cluster that were analyzed by PCR-REA. (A) PCR products of M. capricolum subsp. capricolum (lane 1), M. capricolum subsp. capripneumoniae (lane 2), M. mycoides subsp. capri (lane 3), M. mycoides subsp. mycoides LC (lane 4), M. mycoides SC (lane 5), Mycoplasma sp. bovine group 7 (lane 6), M. putrefaciens (lane 7), and a negative control (lane 8). (B) AluI restriction fragments of the amplicons from the experiment shown in panel A. Note the additional band of 370 bp for M. mycoides SC. Lane M, molecular size standard with 100-bp spacing.
The type strains of the species M. cottewii, M. putrefaciens, and M. yeatsii were also amplified under low-stringency conditions or with high template concentrations as with the PCR-LIF system. Only weak bands were observed on the gel after electrophoresis, and restriction of the amplicons would not result in clearly visible band patterns. As judged from the sequences of the type strains (accession no. U67945, U67946, and U26055), these three strains were expected to give a band pattern similar to that of the majority of the species in the classical M. mycoides cluster. The other control strains of M. bovigenitalium, M. bovirhinis, M. bovis, M. bovoculi, and M. canis were not amplified with the REAP primer pair.
Amplification of 1-μl suspensions from the two dilution series of the cultured PG1T strain resulted in detection levels of the PCR that correspond to 3 and 4 CFU per reaction, respectively. The PCR products were detected by agarose gel electrophoresis and ethidium bromide staining. However, these PCR products could not be seen on the agarose gel after restriction with AluI. Detection of M. mycoides SC after restriction of the amplicons was achieved in fractions containing 30 and 40 CFU/reaction, and the sensitivity was therefore estimated to be at least 30 copies of DNA per amplification reaction.
Analysis of specimens from cattle.
Specimens from two Tanzanian cows with postmortem diagnoses of CBPP were analyzed by the two PCR assays (Table 3). The samples consisted of pleural fluid applied to chromatography paper. DNA from the samples was eluted by heating the pieces of paper in a buffer as described in Materials and Methods. Amplification of the material by the PCR-LIF and PCR-REA systems showed that both samples were clearly positive for M. mycoides SC with either of the two systems. The method of preserving and sending noninfectious clinical samples on chromatography paper was shown to be cheap, convenient, and functional.
TABLE 3.
Results for specimens which were applied to chromatography paper and analyzed by PCR-LIF and PCR-REA
| Specimen no. (herd) | Specimen type | Country | Result of:
|
Postmortem observations | Commentsa | Mycoplasma growth in culture | GI testb result | |
|---|---|---|---|---|---|---|---|---|
| PCR-LIF | PCR-REA | |||||||
| 1 (a) | Pleural fluid | Tanzania | + | + | Typical CBPP lesions | |||
| 2 (a) | Pleural fluid | Tanzania | + | + | Typical CBPP lesions | |||
| 3 (b) | Lung | Kenya | − | − | No CBPP lesions | |||
| 4 (c) | Lung | Kenya | + | + | Typical CBPP lesions | Treated with antibiotics | + | + |
| 5 (c) | Lung effusion | Kenya | + | +c | Typical CBPP lesions | From the same animal as specimen 4 | + | + |
| 6 (c) | Lung | Kenya | − | − | No CBPP lesions | Positive by CFT and cELISA | − | |
| 7 (c) | Lung | Kenya | − | − | Normal appearance | Positive by CFT and cELISA | − | |
| 8 (c) | Lung | Kenya | + | +c | Typical CBPP lesions | Positive by CFT and cELISA | − | |
| 9 (d) | Lung | Kenya | − | − | Positive by CFT and cELISA | − | ||
| 10 (c) | Lung | Kenya | + | + | Typical CBPP lesions | + | + | |
| 11 (e) | Lung | Uganda | − | − | Pneumonia | + | − | |
| 12 (e) | Lung | Uganda | − | − | Pneumonia | − | ||
| 13 (e) | Lung | Uganda | − | − | Pneumonia | − | ||
| 14 (e) | Lung | Uganda | − | − | Pneumonia | − | ||
| 15 (c) | Culture of specimen 10 | + | + | + | + | |||
| 16 (a) | Lung tissued | Tanzania | + | + | Typical CBPP lesions | − | ||
CFT, complement fixation test; cELISA, competitive ELISA.
GI test, growth inhibition test for M. mycoides subsp. mycoides.
Nested PCR was required to produce an amount of amplicon that was sufficient for identification of M. mycoides SC after AluI restriction.
The sample was not applied to chromatography paper; DNA was extracted from frozen lung tissue.
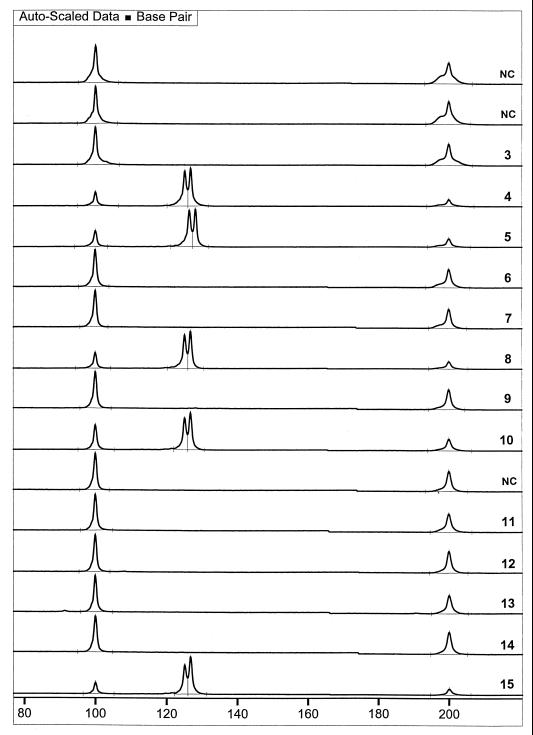
In another investigation we received and analyzed 13 pieces of chromatography paper which had been exposed to samples of various material from 11 different cows (Table 3). Analysis by the PCR-LIF system gave a clear-cut result: five of the samples were positive for M. mycoides SC, and eight were negative (Fig. 3). When analyzed by the PCR-REA system, the same five samples were positive by PCR, but only three of them proved to be M. mycoides SC after restriction. The other two samples contained too little DNA of each fragment size after the restriction procedure to be visible by ethidium bromide staining of the agarose gel. Therefore, the samples were reanalyzed by nested PCR in which a U1–U8 amplification preceded the amplification with REAP primers. Again, by nested PCR, the same five samples were positive for the M. mycoides cluster, and they were confirmed to be M. mycoides SC by REA, while the other eight samples were still negative for the M. mycoides cluster.
FIG. 3.
Fluorogram curves of 13 samples from 11 African cattle which were supplied on chromatography paper and subsequently analyzed by PCR-LIF. Specimen numbers correspond to those in Table 3. NC, negative controls. All peaks at 100 and 200 bp are internal size standards. Samples 4, 5, 8, 10, and 15 were positive for M. mycoides SC, as shown by the characteristic double peak. The absence of peaks in the fluorogram curves of samples 3, 6, 7, 9, 11, 12, 13, and 14 showed that these were negative for the M. mycoides cluster.
Analysis of lung tissue (Table 3, specimen 16) by PCR-LIF resulted in the characteristic double peak, thus confirming the presence of M. mycoides SC in the lung. The disease of the animal was also diagnosed as CBPP upon postmortem examination.
DISCUSSION
Differentiation between M. mycoides SC, a highly important species in veterinary medicine, and its close relatives is a great need but also a challenging task. An outbreak of CBPP may require large-scale screening of samples in a short time. This emphasizes the need for well-designed diagnostic systems which combine different molecular biology techniques to attain high throughput as well as specificity and sensitivity of the tests. PCR is already known as a quick, sensitive, and specific method, but it involves a high risk of cross-contamination and carryover contamination, especially if nested PCR is used. We believe that the use of LIF for detection of the amplicons eliminates the need for nested PCR, thus saving time, diminishing the manual work, and most important, reducing the risk of contamination. Furthermore, it gives an accurate identification of the PCR product compared to that of an agarose gel. Gels can be reloaded for an increased capacity of analysis.
As revealed in this study, the specificity of the two diagnostic PCR systems may include not only members of the classical M. mycoides cluster but also species within the phylogenetic M. mycoides cluster. Amplification of M. cottewii, M. yeatsii, and M. putrefaciens was observed when the annealing temperature was lowered but also when the amount of template was substantial, as is the case for PCR on concentrated and heat-lysed mycoplasma culture. The resulting amount of PCR product was always less than the amount of PCR product produced from any species of the classical M. mycoides cluster. This can be explained by several mismatches between the reverse primers in both PCR systems and their corresponding target sequences in M. cottewii, M. yeatsii, and M. putrefaciens. Nevertheless, all strains of M. mycoides SC could clearly be discriminated by both systems, indicating their usefulness in the detection of this important organism.
Clinical samples may contain various PCR inhibitors that affect the yield of an amplification. For example, if the ratio of host DNA to mycoplasma DNA is high, there is a risk that the total amount of DNA in the sample that is needed for detection of the mycoplasma exceeds the amount that is functional with regard to the concentration of free magnesium ions in the PCR buffer. The problem with PCR inhibitors, despite a high sensitivity of the PCR, might be overcome by performing a nested PCR in order to increase the number of target molecules and dilute the inhibitors in the diagnostic PCR. Both diagnostic systems can easily be used in a nested fashion with the primers complementary to 16S rRNA regions U1 and U8 in the first amplification. As determined from the dilution series of a mycoplasma culture in logarithmic growth, the sensitivity of the PCR-LIF system corresponds to 0.3 to 0.4 CFU per PCR, which is approximately 100 times more sensitive than the PCR-REA system. Theoretically, it is excessive to perform nested PCR when the PCR-LIF system is used, while the analyses in this study showed that performing nested PCR improved the results obtained by PCR-REA in several cases.
Specimens of pleural fluid can be considered to contain only trace amounts of PCR-inhibitory substances, as judged from the strongly positive results obtained from some pleural-fluid samples. Furthermore, M. mycoides SC seems to be present in the pleural fluid of most infected cattle, which makes it a suitable specimen for PCR analysis. However, it is difficult to collect samples from suspected carrier animals in general, and sometimes also at the postmortem. M. mycoides SC may be completely sequestered and therefore absent in, e.g., nasal fluid and some parts of the lungs. Three of the lung samples that were found negative by PCR-LIF and PCR-REA came from animals that were seropositive for M. mycoides as shown by a complement fixation test and competitive ELISA (Table 3, specimens 6, 7, and 9). This might be an example of cases where the sampling procedure rather than the diagnostic method causes misleading results. It is also possible that these animals had acquired immunity before they were acutely infected or that the infections were cured before the samples were taken.
It can always be questioned whether diagnostic systems involving group-specific amplification and differentiation based on single nucleotide substitutions are robust. In the PCR-LIF system, the differentiation is based on a 2-nucleotide sequence length difference between the two operons. An insertion or deletion in the amplified gene region would be detected in the electropherogram from the sequencer due to accurate size determination, and the species would still differ from the other members of the M. mycoides cluster. The detection of an aberrant amplicon would prompt further analysis by DNA sequencing of at least a part of the 16S rRNA genes in order to identify the species. In the restriction system, however, identification is based on a single nucleotide in one of the two 16S rRNA genes, which is found in a semiconserved region. DNA sequencing of 25 strains of M. mycoides SC which represent different IS1296 patterns and come from distant regions (Table 1) showed that new mutations in the 16S rRNA genes are extremely rare in this species. It is therefore reasonable to assume that relying on a single polymorphism for identification of M. mycoides SC is safe. A similar diagnostic system for identification of M. capricolum subsp. capripneumoniae (5, 24) has proved to be very robust despite a greater intraspecific variation in the 16S rRNA genes of this species (19).
The amplicon of the PCR-REA system contains the PstI restriction site that was used to identify M. capricolum subsp. capripneumoniae in the diagnostic system described by Ros Bascuñana et al. (24). It is therefore possible to use the PCR-REA system for diagnosis of contagious caprine pleuropneumonia as well as for CBPP, by replacing the AluI enzyme with PstI. Digestion of the REAP amplicon with PstI resulted in two bands of 82 and 703 bp for all members of the M. mycoides cluster except M. capricolum subsp. capripneumoniae, where three bands of 82, 703, and 785 bp were formed (data not shown).
In conclusion, we have presented two alternative methods for diagnosis of CBPP based on PCR of the 16S rRNA genes. Both systems were shown to identify M. mycoides SC in various types of samples.
ACKNOWLEDGMENTS
We thank Joachim Frey for providing DNA from several mycoplasma strains, Xiaoxing Cheng for analyses of IS1296 patterns, and Hezron Wesonga for sending us the specimens on chromatography paper. We are also grateful to John Bashiruddin, José Regalla, and Fulgencio Garrido for providing the Italian, Portugese, and Spanish strains, respectively. Finally, we thank Johan Wahlberg for helpful discussions and Marianne Persson for skillful technical assistance.
This work has been financially supported by grants from the Agriculture and Fisheries RTD programme of the Commission of the European Communities for “Development of new and improved diagnostic tests for CBPP in Europe” (FAIR1-CT95-0711), the Swedish Council for Forestry and Agricultural Research, and the Swedish International Development Cooperation Agency. The study also forms a part of the EU research collaboration COST 826 on ruminants' mycoplasmoses.
REFERENCES
- 1.Al-Aubaidi J M, Fabricant J. Characterization and classification of bovine mycoplasma. Cornell Vet. 1971;61:490–518. [PubMed] [Google Scholar]
- 2.Anonymous. Report on the meeting of the OIE foot and mouth disease and other epizootics commission. 15 to 19 May. Paris, France: Office International des Epizooties; 1995. [Google Scholar]
- 3.Bashiruddin J B, Taylor T K, Gould A R. A PCR-based test for the specific identification of Mycoplasma mycoides subspecies mycoides SC. J Vet Diagn Investig. 1994;6:428–434. doi: 10.1177/104063879400600405. [DOI] [PubMed] [Google Scholar]
- 4.Bölske G. Survey of mycoplasma infections in cell cultures and a comparison of detection methods. Zentbl Bakteriol Parasitenkd Infektkrankh Hyg Abt 1 Orig A. 1988;269:331–340. doi: 10.1016/s0176-6724(88)80176-7. [DOI] [PubMed] [Google Scholar]
- 5.Bölske G, Mattsson J G, Ros Bascuñana C, Bergström K, Wesonga H, Johansson K-E. Diagnosis of contagious caprine pleuropneumonia by detection and identification of Mycoplasma capricolum subsp. capripneumoniae by PCR and restriction enzyme analysis. J Clin Microbiol. 1996;34:785–791. doi: 10.1128/jcm.34.4.785-791.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng X, Nicolet J, Poumarat F, Regalla J, Thiaucourt F, Frey J. Insertion element IS1296 in Mycoplasma mycoides subsp. mycoides small colony identifies a European clonal line distinct from African and Australian strains. Microbiology. 1995;141:3221–3228. doi: 10.1099/13500872-141-12-3221. [DOI] [PubMed] [Google Scholar]
- 7.Dedieu L, Bréard A, Le Goff C, Lefèvre P-C. Diagnostic de la péripneumonie contagieuse bovine: problèmes et nouveaux développements. Rev Sci Tech O I E. 1996;15:1331–1353. [PubMed] [Google Scholar]
- 8.Dedieu L, Mady V, Lefèvre P C. Development of a selective polymerase chain reaction assay for the detection of Mycoplasma mycoides subsp. mycoides SC (contagious bovine pleuropneumonia agent) Vet Microbiol. 1994;42:327–339. doi: 10.1016/0378-1135(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 9.Edward D G, Freundt E A. The classification and nomenclature of organisms of the pleuropneumonia group. J Gen Microbiol. 1956;14:197–207. doi: 10.1099/00221287-14-1-197. [DOI] [PubMed] [Google Scholar]
- 10.Egwu G O, Nicholas R A J, Ameh J A, Bashiruddin J B. Contagious bovine pleuropneumonia: an update. Vet Bull. 1996;66:875–888. [Google Scholar]
- 11.Gray M W, Sankoff D, Cedergren R J. On the evolutionary descent of organisms and organelles: a global phylogeny based on a highly conserved structural core in small subunit ribosomal RNA. Nucleic Acids Res. 1984;12:5837–5852. doi: 10.1093/nar/12.14.5837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heldtander M, Pettersson B, Tully J G, Johansson K-E. Sequences of the 16S rRNA genes and phylogeny of the goat mycoplasmas Mycoplasma adleri, Mycoplasma auris, Mycoplasma cottewii, and Mycoplasma yeatsii. Int J Syst Bacteriol. 1998;48:263–268. doi: 10.1099/00207713-48-1-263. [DOI] [PubMed] [Google Scholar]
- 13.Hotzel H, Sachse K, Pfützner H. A PCR scheme for differentiation of organisms belonging to the Mycoplasma mycoides cluster. Vet Microbiol. 1996;49:31–43. doi: 10.1016/0378-1135(95)00176-x. [DOI] [PubMed] [Google Scholar]
- 14.Masiga W N, Domenech J, Windsor R S. Manifestation and epidemiology of contagious bovine pleuropneumonia in Africa. Rev Sci Tech O I E. 1996;15:1283–1308. doi: 10.20506/rst.15.4.980. [DOI] [PubMed] [Google Scholar]
- 15.Miserez R, Pilloud T, Cheng X, Nicolet J, Griot C, Frey J. Development of a sensitive nested PCR method for specific detection of Mycoplasma mycoides subsp. mycoides SC. Mol Cell Probes. 1997;11:103–111. doi: 10.1006/mcpr.1996.0088. [DOI] [PubMed] [Google Scholar]
- 16.Nicholas R A J, Bashiruddin J B. Mycoplasma mycoides subspecies mycoides (small colony variant): the agent of contagious bovine pleuropneumonia and member of the “Mycoplasma mycoides cluster.”. J Comp Pathol. 1995;113:1–27. doi: 10.1016/s0021-9975(05)80065-9. [DOI] [PubMed] [Google Scholar]
- 17.Nicholas R A J, Santini F G, Clark K M, Palmer N M A, De Santis P, Bashiruddin J B. A comparison of serological tests and gross lung pathology for detecting contagious bovine pleuropneumonia in two groups of Italian cattle. Vet Rec. 1996;139:89–93. doi: 10.1136/vr.139.4.89. [DOI] [PubMed] [Google Scholar]
- 18.Nocard E, Roux E. Le microbe de la péripneumonie. Ann Inst Pasteur (Paris) 1898;12:240–262. [Google Scholar]
- 19.Pettersson B, Bölske G, Thiaucourt F, Uhlén M, Johansson K-E. Molecular evolution of Mycoplasma capricolum subsp. capripneumoniae strains, based on polymorphisms in the 16S rRNA genes. J Bacteriol. 1998;180:2350–2358. doi: 10.1128/jb.180.9.2350-2358.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pettersson B, Johansson K-E, Uhlén M. Sequence analysis of 16S rRNA from mycoplasmas by direct solid-phase DNA sequencing. Appl Environ Microbiol. 1994;60:2456–2461. doi: 10.1128/aem.60.7.2456-2461.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pettersson B, Uhlén M, Johansson K-E. Phylogeny of some mycoplasmas from ruminants based on 16S rRNA sequences and definition of a new cluster within the hominis group. Int J Syst Bacteriol. 1996;46:1093–1098. doi: 10.1099/00207713-46-4-1093. [DOI] [PubMed] [Google Scholar]
- 22.Pettersson B, Leitner T, Ronaghi M, Bölske G, Uhlén M, Johansson K-E. Phylogeny of the Mycoplasma mycoides cluster as determined by sequence analysis of the 16S rRNA genes from the two rRNA operons. J Bacteriol. 1996;178:4131–4142. doi: 10.1128/jb.178.14.4131-4142.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Regalla J, Caporale V, Giovannini A, Santini F, Martel J L, Penha Gonçalves A. Manifestation and epidemiology of contagious bovine pleuropneumonia in Europe. Rev Sci Tech O I E. 1996;15:1309–1329. doi: 10.20506/rst.15.4.979. [DOI] [PubMed] [Google Scholar]
- 24.Ros Bascuñana C, Mattsson J G, Bölske G, Johansson K-E. Characterization of the 16S rRNA genes from Mycoplasma sp. strain F38 and development of an identification system based on PCR. J Bacteriol. 1994;176:2577–2586. doi: 10.1128/jb.176.9.2577-2586.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosengarten R, Behrens A, Stetefeld A, Heller M, Ahrens M, Sachse K, Yogev D, Kirchhoff H. Antigen heterogeneity among isolates of Mycoplasma bovis is generated by high-frequency variation of diverse membrane surface proteins. Infect Immun. 1994;62:5066–5074. doi: 10.1128/iai.62.11.5066-5074.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosengarten R, Yogev D. Variant colony surface antigenic phenotypes within mycoplasma strain populations: implications for species identification and strain standardization. J Clin Microbiol. 1996;34:149–158. doi: 10.1128/jcm.34.1.149-158.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ross R F. Mycoplasma—animal pathogens. In: Kahane I, Adoni A, editors. Rapid diagnosis of mycoplasmas. New York, N.Y: Plenum Press; 1993. pp. 69–109. [Google Scholar]
- 28.Scudamore J M. Contagious bovine pleuropneumonia. State Vet J. 1995;5:13–16. [Google Scholar]
- 29.Weisburg W G, Tully J G, Rose D L, Petzel J P, Oyaizu H, Yang D, Mandelco L, Sechrest J, Lawrence T G, Van Etten J, Maniloff J, Woese C R. A phylogenetic analysis of the mycoplasmas: basis for their classification. J Bacteriol. 1989;171:6455–6467. doi: 10.1128/jb.171.12.6455-6467.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wise K S, Yogev D, Rosengarten R. Antigenic variation. In: Maniloff J, McElhaney R N, Finch L R, Baseman J B, editors. Mycoplasmas: molecular biology and pathogenesis. Washington, D.C: American Society for Microbiology; 1992. pp. 473–489. [Google Scholar]