Abstract
Background
The coronavirus disease 2019 pandemic necessitated the use of telemedicine for most medical specialties, including neurosurgery, although before the pandemic, neurosurgeons infrequently used telemedicine for outpatient visits. We conducted a patient-centric evaluation of telemedicine in our endovascular neurosurgery practice, covering a 4-month period early in the pandemic.
Methods
Survey e-mails after telemedicine visits were sent to all patients who underwent an outpatient telemedicine visit between March 11, 2020, and June 22, 2020, at an endovascular neurosurgery clinic affiliated with a tertiary care center.
Results
Of 140 patients, 65 (46%) completed the e-mail survey. Of the 65 respondents, 35 (54%) agreed or strongly agreed with the statement that even before their telemedicine experience, they thought telemedicine would be a convenient way to receive a neurological consultation. After their telemedicine visit, 47 (72%) agreed or strongly agreed with this statement, and 28 (43%) agreed or strongly agreed that they would prefer telemedicine for future visits. Of the 65 respondents, 61 (94%) rated their telemedicine visit as average or better: 34 (52%) rated it excellent, 12 (18%) rated it above average, and 15 (23%) rated it average. When patients compared their telemedicine visit with a prior in-person clinic visit, only 10 of 44 patients (23%) thought the telemedicine visit was more complicated than an in-person visit, and 21 of 44 (48%) said they would prefer telemedicine for future visits.
Conclusions
Our patients expressed satisfaction with their telemedicine visits, and telemedicine will likely play an important role in future outpatient endovascular neurosurgery consultations.
Key words: COVID-19, Endovascular, Neurosurgery, Pandemic, Telemedicine
Abbreviations and Acronyms: CARES, Coronavirus Aid, Relief, and Economic Security; COVID-19, Coronavirus disease 2019; HIPAA, Health Insurance Portability and Accountability Act
Introduction
The coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 virus, which started in late 2019 and escalated in 2020, has required a paradigm shift in how health care is delivered to patients. With traditional in-person medical visits limited by shutdowns and social distancing guidelines from public health agencies, health care providers began turning to telemedicine, which is the use of electronic communication for direct patient care. Telemedicine offers increased availability of health care services to patients, with decreased time required for patient visits, decreased financial costs, and decreased risk of potential exposure to the virus. When stricter social distancing measures were enacted across the United States in March 2020, the use of telemedicine became more prevalent. Although telemedicine in some form started nearly 50 years ago, it has not previously played an important role in health care delivery because of concerns regarding the need for patient confidentiality, the lack of technological infrastructure, poor third-party reimbursement, and difficulty in using telemedicine to conduct physical examinations.1, 2, 3
However, once the COVID-19 pandemic established the need for telemedicine and changes in regulations and the elimination of barriers facilitated the transition to telemedicine, many health care networks and subspecialties began strengthening the foundations of their telemedicine workflow. The field of neurosurgery has also adapted to this trend, with various institutions providing data about their own experiences and offering recommendations for best practices.4, 5, 6, 7 Within the specialty of endovascular neurosurgery, telemedicine has long been used to evaluate patients with stroke.8 The importance of telemedicine for patients requiring neuroendovascular intervention has grown even greater during the pandemic as new protocols and guidelines have been developed and implemented.9 , 10
The aim of this article was to present our findings on patient satisfaction with outpatient telemedicine visits to our institution’s endovascular neurosurgery practice during the early months of the COVID-19 pandemic in the United States. Our primary objective was to examine the experiences of patients and identify any concerns they had after their outpatient neuroendovascular consultations were conducted via telemedicine. To our knowledge, this study is the first to investigate patient satisfaction outcomes after telemedicine visits for neuroendovascular evaluation during the COVID-19 pandemic.
Materials and Methods
All patients who had undergone a telemedicine visit conducted by one of our neuroendovascular clinicians between March 11, 2020, and June 22, 2020, were asked to complete a telemedicine experience survey sent through e-mail. Telemedicine visits were performed using the GoToMeeting platform (LogMeIn, Boston, Massachusetts, USA). Before the visit, the clinical office staff e-mailed patients the instructions on how to download the necessary software when booking an outpatient telemedicine appointment. The telemedicine visits were performed using a videoconference option. A small portion of the visits were converted to audio only if the patient’s internet connection did not allow for adequate videoconferencing. The patients were initially seen by the neurosurgery resident or endovascular fellow and then by the attending physician. History, imaging review, and a remote examination were performed.
After the neuroendovascular telemedicine visit, we e-mailed a 14-question survey to all eligible patients; patients who had previously undergone an in-person visit at our clinic were asked to respond to an additional 5 questions on the survey. Responses were made on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, and strongly agree). Patients also rated their overall telemedicine experience responses as poor, below average, average, above average, or excellent on a 5-point Likert scale. The St. Joseph’s Hospital and Medical Center Institutional Review Board for Human Research made a nonresearch determination for this quality-improvement project on the basis of internal experience. Written patient consent was not deemed necessary because returning the survey indicated tacit consent. Also, all survey responses were anonymized.
Statistical Analysis
Statistical analysis was performed using Prism 8 (GraphPad Software, San Diego, California, USA) and Excel (Microsoft Corporation, Redmond, Washington, USA). Patients were assessed as an overall group and as 6 subgroups classified by age (≤30, 31–40, 41–50, 51–60, 61–70, and >70 years old). Patients also were compared by first-time versus previous experience with telemedicine. Comparisons were made using unpaired t tests and 1-way analysis of variance. All results with a P value < 0.05 were considered significant.
Results
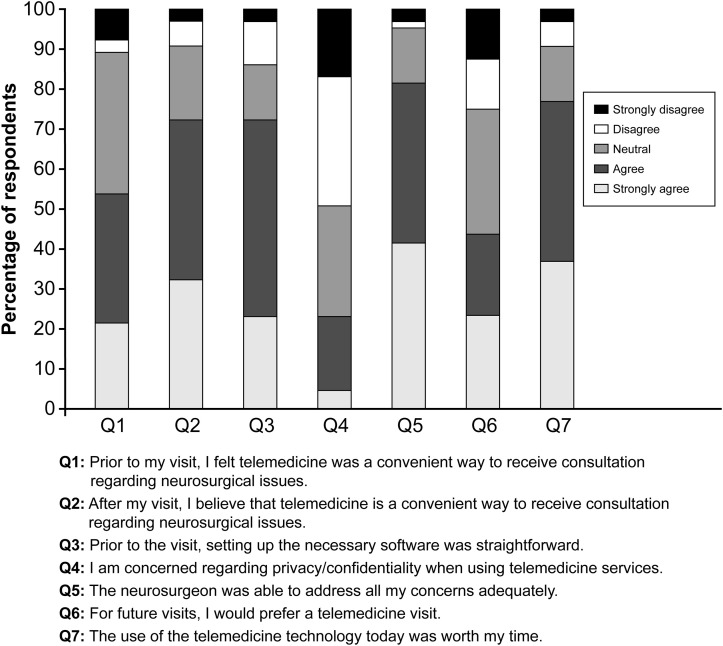
Of 140 patients who participated in telemedicine visits during the study period and were e-mailed the patient satisfaction survey, 65 patients (46%) completed the survey, although some patients did not answer all the questions. Of these 65 respondents, 54 (83%) were >50 years old. By age category, 2 patients (3%) were ≤30 years old, 3 patients (5%) were 31–40 years old, 6 patients (9%) were 41–50 years old, 9 patients (14%) were 51–60 years old, 22 patients (34%) were 61–70 years old, and 23 patients (35%) were >70 years old. Information on the sex of patients was not gathered in the survey. These neuroendovascular telemedicine visits were a first-time telemedicine experience for 40 patients (62%). Figure 1 summarizes the responses of patients to 7 of the 14 survey questions. Additional questions were asked to gather patient demographics and information about clinic visits.
Figure 1.
Stacked bar chart summarizing responses to 7 questions answered by 65 survey respondents (n = 64 for question 6) regarding their neuroendovascular telemedicine experience. Responses were on a 1-to-5 scale: 1 for strongly disagree to 5 for strongly agree.
Used with permission from Barrow Neurological Institute, Phoenix, Arizona, USA.
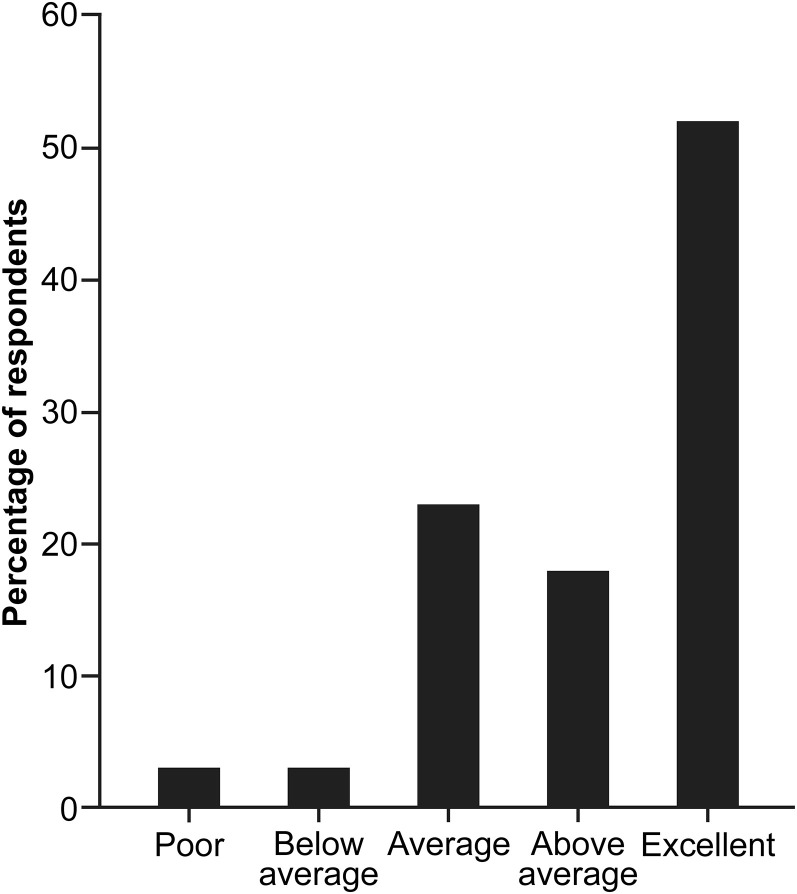
Of the 65 respondents, 35 (54%) agreed or strongly agreed with a statement indicating that even before their neuroendovascular telemedicine experience, they thought telemedicine was a convenient way to receive a consultation about neurosurgical issues. After their telemedicine visit, an increased number of respondents (n = 47, 72%) agreed or strongly agreed that telemedicine was a convenient way to receive such a consultation. When questioned about technical difficulties with their telemedicine visit, only 9 patients (14%) indicated that setting up the necessary software had not been straightforward. Only 15 patients (23%) expressed concern about privacy and confidentiality. Of respondents, 53 (82%) agreed or strongly agreed that the endovascular neurosurgeon had been able to address all their questions adequately. When asked about their preference of telemedicine for future visits, 28 of 64 patients (44%) agreed or strongly agreed that they would prefer telemedicine, and 50 patients (77%) believed that the telemedicine visit was worth their time. Of patients, 61 (94%) rated their telemedicine visit as average or better: 34 patients (52%) rated it as excellent, 12 patients (18%) rated it as above average, and 15 patients (23%) rated it as average (percentages for subgroups total <100% owing to rounding) (Figure 2 ). Of 28 patients for whom a procedure was recommended, 25 agreed to the recommendation and scheduled the procedure, and 3 patients declined to do so.
Figure 2.
Bar chart summarizing how 65 survey respondents rated their overall patient experience with a telemedicine visit for a neuroendovascular consultation, with more than one half (52%) rating it as excellent. Percentages total <100% owing to rounding.
Used with permission from Barrow Neurological Institute, Phoenix, Arizona, USA.
When the overall experience of patients with their telemedicine visit was evaluated by age group using 1-way analysis of variance, no statistically significant difference was found (P = 0.40). In addition, no statistically significant difference was found using an unpaired t test to compare the overall experience of patients who were first-time telemedicine users with the overall experience of patients who were repeat users (P = 0.30).
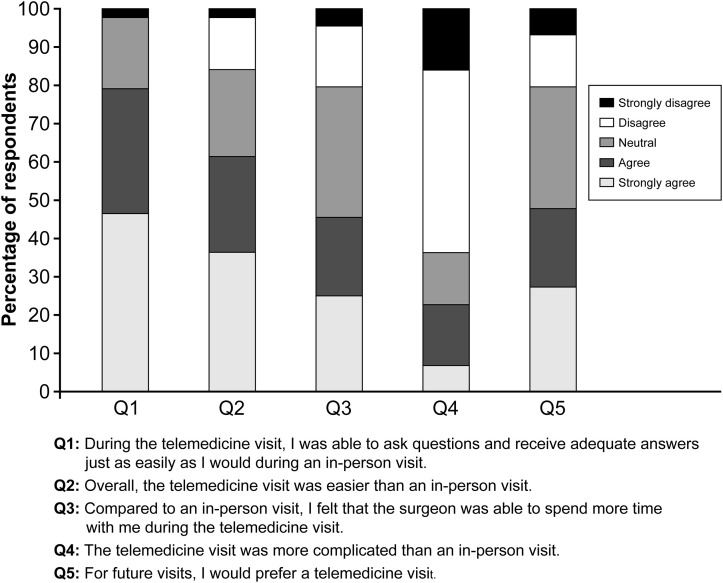
There were 44 patients who had completed an in-person clinic visit before their telemedicine visit and were asked to answer 5 additional survey questions comparing their telemedicine visit with their in-person visit (Figure 3 ). Most patients (34 of 43, 79%) agreed or strongly agreed that they were able to ask questions and receive adequate answers in their telemedicine visit just as easily as they could during an in-person visit. Overall, most of the 44 patients (n = 27, 61%) agreed or strongly agreed that they had found their telemedicine visit easier than an in-person visit. Concerning the amount of time the physician spent with the patient, 20 of 44 patients (45%) agreed or strongly agreed that the physician was able to spend more time with them during their telemedicine visit than during their in-person visit. Only 10 of 44 patients (23%) considered the telemedicine visit more complicated than an in-person visit. Finally, 21 patients (48%) indicated that they would prefer a telemedicine visit to an in-person visit in the future.
Figure 3.
Stacked bar chart summarizing responses to 5 questions answered by 44 survey respondents (n = 43 for question 1) who were comparing their previous in-person visit at our clinic with their neuroendovascular telemedicine experience. Responses were on a 1-to-5 scale: 1 for strongly disagree to 5 for strongly agree.
Used with permission from Barrow Neurological Institute, Phoenix, Arizona, USA.
Discussion
Although telemedicine has been reported to offer both economic and clinical benefits, its use for neurosurgery outpatient consultations was limited before the COVID-19 pandemic.1 , 4 The use of telemedicine had not been widespread because of a lack of clear reimbursement policies, interstate licensure and liability issues, lack of access to technology, potential patient confidentiality issues, and the absence of a clear need for these remote services.1 , 4 Previous telemedicine legislation also limited the use of telemedicine to patients living in rural areas who required access to geographically distant services.1
The U.S. Congress passed the Coronavirus Aid, Relief, and Economic Security (CARES) Act, which was signed into law on March 27, 2020. The CARES Act supported the increased use of telemedicine, as did a waiver allowed by Section 1135 of the Social Security Act, which temporarily set aside many of the regulatory barriers previously impeding the regular use of telemedicine, specifically, reimbursement rates and geographical limitations for persons with Medicare and Medicaid insurance.11 The CARES Act allowed health care providers to bill for telemedicine visits at the same rate as in-person, face-to-face visits. In addition, out-of-state providers no longer had to be licensed within the state where the patient resides, thereby allowing out-of-state patients to be seen via telemedicine providers.
Before the COVID-19 pandemic, the use of telemedicine at our institution was quite limited. Although we routinely used telephone and e-mail consultations to evaluate patient imaging before in-person clinic visits for new patients, perform follow-up imaging reviews for established patients, and provide second opinions, we conducted very few formal telemedicine encounters. As was the case with medical practices worldwide, the pandemic forced our outpatient practice to incorporate telemedicine visits into our daily schedule.
Along with the experiences reported by other neurosurgery practices, our patient satisfaction survey results substantiate the use of telemedicine for neurosurgery outpatient care during the COVID-19 pandemic and show it to be a promising opportunity for eventual routine use.4 , 5 , 12 , 13 In a recent survey that evaluated the use of telemedicine by neurosurgeons during the COVID-19 pandemic, 87.1% of the 271 respondents reported that they were using telemedicine for consultation.7 Interestingly, although these providers indicated that telemedicine increased their ability to see patients with urgent needs, most respondents (55.7%) believed that telemedicine would compromise the quality of the doctor-patient relationship.7 This concern, which is an important consideration for both physicians and patients, would likely affect patient satisfaction and comfort when a patient decides to undergo a neurosurgical procedure or intervention. However, our survey results indicate that 25 of 28 patients (89%) for whom a procedure was recommended opted to schedule that procedure, which leads us to conclude that our patients feel comfortable about undergoing neurosurgical procedures discussed and scheduled during a telemedicine visit.
Although concerns about possible compromise of the doctor-patient relationship may be valid, the level of satisfaction expressed by our patients did not seem to be negatively affected by telemedicine, with 61 of 65 patients (94%) reporting an average-to-excellent experience, and 53 of 65 patients (82%) agreeing or strongly agreeing that all their questions had been adequately addressed. This was also true among patients who had previously undergone an in-person clinic visit, with 34 of 43 patients (79%) agreeing or strongly agreeing that they had been able to ask questions and receive adequate answers just as easily during the telemedicine encounter as during an in-person visit, and with 27 of 44 patients (61%) indicating that their telemedicine visit had been easier than an in-person visit. The use of videoconferencing software allowing the patient and physician to be face to face may alleviate some of the concerns patients may have about seeing their physician remotely.
Other neurosurgery groups have also published their early experiences with the use of telemedicine for neurosurgery outpatient care, but these reports are limited to physicians sharing their experiences. LoPresti et al.12 compiled a list of problems they had encountered early in their launch of telemedicine, along with the solutions they used to resolve them. For example, they suggested using telephone encounters to determine clinical urgency and to evaluate whether an in-person assessment was required to address the problem of “patient access and barriers for elderly or nontechnologically accessible or knowledgeable patient populations.” In the report by Eichberg et al.4 of lessons learned from a systematic review of telemedicine in neurosurgery, technological failure (81.5%) was the primary cause of an unsuccessful telemedicine visit. Lack of universal access to technology has long been thought to be a limitation in the effectiveness of telemedicine.1 Furthermore, the lack of Health Insurance Portability and Accountability Act (HIPAA)–compliant software has been a significant barrier. With the advent of HIPAA-compliant software and increasing accessibility to high-speed internet connections, technological failure poses less of a challenge.
In response to our patient survey, only 9 of 65 patients (14%) indicated that setting up the necessary software was not straightforward, whereas 47 patients (72%) said it was straightforward. Nine patients (14%) were neutral on this point. In addition, we found no statistically significant difference in the overall experience of patients in different age groups. Before patients met with their physicians, the office staff initiated the telemedicine visit to ensure that the patients had an adequate audiovisual setup and a good internet connection. When technical issues were encountered in setting up the software or maintaining a connection because of poor internet access, the visit was converted to a telephone call to bypass these issues. Converting to a telephone call precludes the performance of a telemedicine-tailored neurological examination, but it does allow for the completion of the visit and the conveyance of any important information regarding the consultation. We found neuroendovascular surgery patients to be well suited to telemedicine because imaging review is paramount. Most patients showed no signs of illness on physical examination. In our experience, the success of this program required adequate support personnel to facilitate ready access to imaging.
Although our survey did not assess patients’ perceptions of wait times, it is plausible that reduced travel times to and from the clinic, along with the ability to complete a visit from home, positively impacted their perception of this metric. A recent report by Lun et al.14 shared survey results of 118 patients and 6 physicians who participated in a virtual interventional neuroradiology clinic. Notably, 64.4% of the patients (76 of 118) reported no wait time before their virtual appointment. Five of the 6 physicians participating in the survey also perceived the virtual visits to be shorter. Overall, Lun et al.14 found that 94.9% of the patients (112 of 118) and 67% of the providers (4 of 6) were generally satisfied with the virtual visits, both of which are remarkably encouraging results for telemedicine. The perceptions of patients regarding reduced wait times for telemedicine appointments may also positively impact their overall satisfaction with a virtual appointment.
The protection of patient confidentiality has also long been thought to be one of the concerns limiting the widespread use of telemedicine.1 LoPresti et al.12 listed privacy and confidentiality concerns as one of the early problems encountered in launching telemedicine because patients are unfamiliar with the consent process for this technology. LoPresti et al.12 resolved this issue by involving the compliance team of their organization and providing videos to patients regarding the telehealth process. In our survey of 65 patients, about one fourth (n = 15, 23%) had concerns about privacy and confidentiality when using telemedicine services, whereas nearly one half (n = 32, 49%) did not have these concerns. Theoretically, telemedicine may pose privacy or security threats to patients when used incorrectly; therefore, it is imperative to use a HIPAA-compliant software program. In our practice, our office staff conveyed the details regarding the telemedicine visit to patients when scheduling their appointments. Before discussing the patient’s medical history, the provider obtained verbal consent, which should be obtained before the formal consultation and documented in the patient’s medical record. Although we did not record telemedicine visits with our patients, we did notify them regarding the possibility of sessions being video recorded.
As to the future use of telemedicine after the COVID-19 pandemic wanes, our survey points to an important result. When asked about patients’ preferences for telemedicine for future visits, almost half of the patients (28 of 64, 44%) said they would prefer telemedicine for future visits. Although telemedicine provides convenience and safety during a pandemic, patients may still prefer in-person visits when discussing their health care with a neurosurgeon. This key finding suggests that telemedicine cannot replace the in-person clinic. Therefore, the future model may be a hybrid clinic, with the physician meeting with patients who wish to meet in person and alternatively conducting virtual visits with patients who prefer telemedicine.
Limitations
This study was a patient satisfaction study conducted at a single treatment center. Although our results are promising for the routine use of telemedicine in a neuroendovascular surgery clinic, they may be affected by restrictions implemented during the COVID-19 pandemic. Furthermore, patients in our clinic were predominantly seen for neuroendovascular consultations, and the majority of respondents (83%) were >50 years old. Other neurosurgery specialties, especially spine, may require in-person visits because of the emphasis on physical examination findings, including surgical-site evaluations, which are key to diagnosis and management. Our study was also conducted over a brief period of time, thereby limiting our response rate to 46%. A learning curve regarding telehealth visits at our institution was unable to be assessed because this study was conducted over a short period of time early during the pandemic.
Conclusions
This patient-centric study investigated and reported patient satisfaction rates for telemedicine in endovascular neurosurgery during the COVID-19 pandemic. Along with the experiences published by other neurosurgery practices, our results support the use of telemedicine for neurosurgery outpatient care during the pandemic and show its promise for eventual routine use. Although these positive outcomes demonstrate that the regulatory expansion of telemedicine implemented during the COVID-19 pandemic should be made permanent, we do not recommend that telemedicine replace all in-person visits once these can be safely conducted again. Instead, our findings demonstrate that telemedicine can be a valuable adjunct to in-person visits for patients and neurosurgery providers.
CRediT authorship contribution statement
Neil Majmundar: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Andrew F. Ducruet: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. D. Andrew Wilkinson: Formal analysis, Writing – review & editing. Joshua S. Catapano: Formal analysis. Jimmy Patel: Formal analysis. Jacob F. Baranoski: Formal analysis. Tyler S. Cole: Formal analysis. Felipe C. Albuquerque: Conceptualization, Formal analysis, Investigation, Project administration, Supervision, Writing – original draft, Writing – review & editing.
Acknowledgments
We thank the staff of Neuroscience Publications at Barrow Neurological Institute for assistance with manuscript preparation.
Footnotes
Conflict of interest statement: A. F. Ducruet is a consultant for Medtronic, Cerenovus (Johnson & Johnson), Stryker, Penumbra, Inc., and Koswire, Inc. The remaining authors have no conflicts to report.
References
- 1.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 2.Glazer E., Marshall C., Cunningham N. Remote pediatric consultation in the inner city: television or telephone? Am J Public Health. 1978;68:1133–1135. doi: 10.2105/ajph.68.11.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 4.Eichberg D.G., Basil G.W., Di L., et al. Telemedicine in neurosurgery: lessons learned from a systematic review of the literature for the COVID-19 era and beyond. Neurosurgery. 2020;88:E1–E12. doi: 10.1093/neuros/nyaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daggubati L.C., Eichberg D.G., Ivan M.E., et al. Telemedicine for outpatient neurosurgical oncology care: lessons learned for the future during the COVID-19 pandemic. World Neurosurg. 2020;139:e859–e863. doi: 10.1016/j.wneu.2020.05.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blue R., Yang A.I., Zhou C., et al. Telemedicine in the era of coronavirus disease 2019 (COVID-19): a neurosurgical perspective. World Neurosurg. 2020;139:549–557. doi: 10.1016/j.wneu.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gadjradj P.S., Matawlie R.H., Harhangi B.S. Letter to the Editor: the use of telemedicine by neurosurgeons during the Covid era: preliminary results of a cross-sectional research. World Neurosurg. 2020;139:746–748. doi: 10.1016/j.wneu.2020.05.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaMonte M.P., Bahouth M.N., Hu P., et al. Telemedicine for acute stroke: triumphs and pitfalls. Stroke. 2003;34:725–728. doi: 10.1161/01.STR.0000056945.36583.37. [DOI] [PubMed] [Google Scholar]
- 9.Fraser J.F., Arthur A.S., Chen M., et al. Society of NeuroInterventional Surgery recommendations for the care of emergent neurointerventional patients in the setting of COVID-19. J Neurointerv Surg. 2020;12:539–541. doi: 10.1136/neurintsurg-2020-016098. [DOI] [PubMed] [Google Scholar]
- 10.Yang B., Wang T., Chen J., et al. Impact of the COVID-19 pandemic on the process and outcome of thrombectomy for acute ischemic stroke. J Neurointerv Surg. 2020;12:664–668. doi: 10.1136/neurintsurg-2020-016177. [DOI] [PubMed] [Google Scholar]
- 11.Center for Medicare and Medicaid Services COVID-19 emergency declaration blanket waivers for health care providers. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf Available at:
- 12.LoPresti M.A., McDeavitt J.T., Wade K., et al. Letter: telemedicine in neurosurgery—a timely review. Neurosurgery. 2020;87:E208–E210. doi: 10.1093/neuros/nyaa175. [DOI] [PubMed] [Google Scholar]
- 13.Mouchtouris N., Lavergne P., Montenegro T.S., et al. Telemedicine in neurosurgery: lessons learned and transformation of care during the COVID-19 pandemic. World Neurosurg. 2020;140:e387–e394. doi: 10.1016/j.wneu.2020.05.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lun R., Walker G., Daham Z., et al. Transition to virtual appointments for interventional neuroradiology due to the COVID-19 pandemic: a survey of satisfaction. J Neurointerv Surg. 2020;12:1153–1156. doi: 10.1136/neurintsurg-2020-016805. [DOI] [PubMed] [Google Scholar]