Abstract
As the athletic training profession continues to embrace evidence-based practice, athletic trainers should not only critically appraise the best available evidence but also effectively translate it into clinical practice to optimize patient outcomes. Whereas previous authors investigated the effectiveness of educational interventions on increasing knowledge of critical appraisal of evidence, little attention has been given to strategies for both researchers and clinicians to effectively translate evidence into clinical practice. The use of knowledge translation strategies has the potential to bridge the knowledge-to-practice gap, which could lead to reduced health costs, improved patient outcomes, and enhanced quality of care. The purpose of this article is to (1) highlight the current challenges preventing the successful translation of evidence into practice, (2) discuss knowledge translation and describe the conceptual frameworks behind the effective translation of evidence into practice, and (3) identify considerations for athletic trainers as they continue to provide high-quality patient care in an evidence-based manner.
Keywords: evidence-based practice, knowledge transfer, dissemination, implementation
Key Points
To minimize the current gap between research and clinical practice, knowledge translation strategies may offer a bridge between dissemination and utilization.
Knowledge translation models, such as the 4E framework and knowledge-to-action framework, may serve as valuable resources for guiding dissemination and utilization efforts in health care.
Knowledge producers (eg, researchers) and knowledge users (eg, clinicians) must work together so the available evidence can be effectively disseminated and efficiently adapted.
Evidence-based practice (EBP) was recommended by the Institute of Medicine almost 20 years ago with the aim of improving the quality of patient care and addressing global health care concerns, such as the use of unnecessary diagnostic tests and unsupported interventions and increasing costs.1 Defined as the integration of the best available evidence along with patient values and clinician expertise,2 EBP has become a keystone principle in health care. In athletic training, EBP has been highlighted for more than a decade as an imperative cultural shift for the progression of the profession.3 As a whole, the profession has made significant efforts to foster an EBP culture, including identifying EBP as a core competency throughout athletic training education4–6 as well as requiring EBP-specific continuing education units to demonstrate maintenance of competence.7 Despite concerted efforts to encourage EBP across all disciplines of health care, including athletic training, researchers8,9 suggested that the implementation of new and available evidence into routine care has remained limited.
The explanation for limited implementation of evidence is multifaceted, but one often overlooked aspect of the EBP process is the translation of knowledge gained from scientific findings to patient care. In general, athletic trainers (ATs) may think of EBP as identifying the available literature via online databases, incorporating strategies for an effective literature search, and critically appraising the evidence. Although these are indeed essential aspects of EBP, there is often little to no mention of what happens next. Truly embracing EBP will require ATs to constantly question practice as well as make changes to practices based on the current available evidence and evolving best-practice guidelines. Therefore, it is essential that ATs be able to not only critically appraise the available evidence but also effectively translate the evidence into their own practices.10
Translating evidence into practice poses multiple challenges to both individuals who create and disseminate new evidence (eg, researchers) and individuals who must interpret and implement new evidence in practice (eg, clinicians). Researchers are often limited by the formats in which findings can be disseminated. For promotion and tenure purposes, academic researchers are typically required to disseminate study findings through peer-reviewed journals, which are generally more concerned about the scientific merit of the evidence than the translation of the evidence into routine care. Thus, this approach often creates a linear gap whereby the researcher disseminates the scientific evidence and places the burden of translating the evidence into clinical practice on the clinician. Specifically, the passive nature of journal publications and noninteractive conference presentations often requires clinicians to actively seek out and appraise the new evidence, consider the local context or patient population or both, and then implement the new evidence with very little to no insight as to what the application of this evidence will actually look like in practice. Thus, whereas researchers might expend a great deal of time and effort to enhance awareness and knowledge of emerging evidence, traditional dissemination methods often stop short of providing actionable steps or clinical tools that can aid clinicians in readily implementing the new evidence in practice. Furthermore, in published reports, researchers11–13 suggested that although educational interventions are effective in increasing short-term knowledge gains, they often do not provide health care professionals with the necessary skills or tools to effectively translate this knowledge to promote clinical practice behaviors.
To directly address these challenges, knowledge translation (KT) models have been recognized as a mechanism for shifting away from the linear gap between the dissemination of evidence by researchers and the burden of evidence implementation by clinicians and instead facilitating a more collaborative exchange to enhance the level of evidence-based care provided to patients. Therefore, the objectives of this article are to (1) highlight the considerations and potential challenges of the dissemination and use of evidence in clinical practice, (2) discuss KT and describe the conceptual frameworks behind effectively translating evidence into practice, and (3) identify considerations for ATs as they continue to provide high-quality patient care in an evidence-based manner.
UPTAKE OF EVIDENCE IN CLINICAL PRACTICE
In health care, a rigid dichotomy is presumed to exist between research and clinical practice. However, treating these areas as siloed entities leads to the assumption that a clinician cannot also produce research and that a researcher cannot also practice clinically. Several calls have been made in athletic training to break down such silos and bridge the gap between research and clinical practice.14–16 Furthermore, it is important to highlight roles in which an individual engages in both research and clinical practice (eg, clinician-scientists, scholarly clinicians). Thus, to avoid the use of dichotomous terms such as researcher and clinician, in this article, we will refer to individuals who regularly create and disseminate new knowledge or evidence as knowledge producers and those who routinely interpret and use new knowledge or evidence as knowledge users.
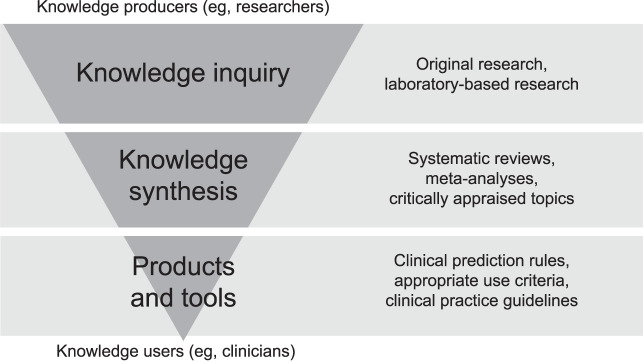
The uptake of evidence is often broken into 2 components: dissemination and utilization (Figure 1). In its most basic form, “dissemination is considered the process of communicating new findings and outcomes,”17(p48) whereas “utilization encompasses a more complex process of applying the evidence that has been disseminated.”17(p48) In terms of evidence dissemination, we most often think of journal publications, conference presentations, and webinars as means of disseminating the available evidence. Although commonplace in health care, these modes emphasize passive rather than active dissemination. The literature supports passive dissemination mechanisms for increasing awareness and familiarity, yet they often do not lead to clinical practice behavioral changes.18–21 Therefore, a lack of evidence uptake in athletic training may be due to the fact that evidence is often only passively disseminated, leaving knowledge users to not only navigate the complex process of evidence utilization on their own but also to actively seek out new knowledge. With hundreds of new research publications distributed monthly covering a diverse range of topics relevant to the unique patient populations ATs serve and often through platforms that require fees for access, it is unsurprising that a significant burden is placed on knowledge users to actively seek out, interpret, and then implement evidence that is only passively disseminated by knowledge producers.
Figure 1.
Examples of dissemination and utilization.
The use of the best available evidence not only requires effective dissemination from knowledge producers but also positive attitude changes from knowledge users considering implementation. To effectively apply evidence that has been disseminated, knowledge users must not only have a solid understanding of the evidence itself but also value its importance before they will adopt it into routine patient care. Similarly, knowledge producers also need to make more concerted efforts to disseminate evidence through methods that are easily accessible (eg, social media, open-access publications) and include active dissemination strategies (eg, podcasts, blog posts and tweets, virtual exchanges22) that promote actionable steps for clinical practice implementation. As a result, it is no surprise that educational interventions are not effective at promoting clinical practice behavioral changes because they typically focus on dissemination of evidence without making a connection as to how the evidence can be applied by knowledge users in a variety of practice settings in real time. This notion raises several questions about how information (ie, evidence) is both communicated to and received by health care professionals.
First, we must consider how evidence is being disseminated by knowledge producers to knowledge users and whether it is being presented in a manner that allows knowledge users to easily translate it into clinical practice. Although discussing the available literature on effective dissemination strategies to promote knowledge uptake is outside the scope of this article, it is important to highlight that an entire field of study, dissemination and implementation science, has emerged to conduct research to better understand these very topics. Second, we must consider whether knowledge users are equipped with the knowledge and skills to effectively translate available evidence into routine patient care.
To illustrate the gap between knowledge and its uptake and use in clinical practice, consider the use of the Ottawa Ankle Rules (OAR). Some literature suggested that clinicians were not implementing the OAR routinely in practice23,24 despite a strong evidence base supporting their use.25,26 For example, Graham et al23 examined emergency physicians' awareness and use of the OAR and Ottawa Knee Rules in 5 countries and found that even though 96% of US physicians were aware of the OAR, only 31% self-reported their use always or most of the time. A similar investigation in athletic training24 also highlighted a large knowledge-to-practice gap regarding OAR use. Hankemeier et al24 found the OAR to be the clinical prediction rule most familiar to ATs yet regularly implemented by only 22.6% of them. Through these studies, it is apparent that familiarity alone is not enough to change clinician behavior. That is, researchers proposed that the dissemination of the OAR has been effective at increasing knowledge but ineffective in supporting utilization. Although this dissemination and utilization gap is multifactorial, some reasons may include the use of passive methods to disseminate information or unsuccessful implementation strategies at the system, organizational, or individual provider levels. To address these primary limitations, there have been calls to adopt KT models.17,27,28
Knowledge Translation
Knowledge translation has gained attention due to revelations in the literature depicting the current state of health care, particularly the amount of care being provided that is ineffective or potentially harmful and the alarming costs associated with such care.29 Previous literature demonstrated a gap and major time lag between the best available evidence and its use in clinical practice,8 leading to the provision of suboptimal and potentially ineffective medical care, as well as inefficient use of health care resources. Therefore, KT aims to close this knowledge-to-practice gap, and numerous frameworks and models highlight the components of KT to help facilitate the process.
The complexity of KT involves going beyond the simple dissemination of information and promotes the application of new knowledge by appropriate users (eg, health care professionals). Although researchers and organizations have developed and evolved definitions of KT over time, the Canadian Institutes of Health Research provided a comprehensive description that acknowledges the end goals and overall importance of the KT process. It defined KT as “a dynamic and iterative process that includes the synthesis, dissemination, exchange and ethically sound application of knowledge to improve health, provide more effective health services and products, and strengthen the health care system.”30 Despite multiple interpretations of the concept, a shared commonality is the active use of knowledge and evidence to inform decision making and improve outcomes for patients and the health care system as a whole.
Knowledge Translation Models
A significant number of KT models, theories, and frameworks were created to guide dissemination and implementation efforts, but most are lacking a strong evidence base to describe their use in clinical practice.31 We aim to fill this gap by discussing 2 frameworks that are most commonly referred to in the health professions literature and by providing a clinically relevant example. It is important that health care professionals maximize KT efforts to improve the quality of care and optimize patient outcomes. To use the KT frameworks and models effectively, a foundational understanding of their components is required. The 2 KT models that are most relevant in health care are the 4E framework17 and the knowledge-to-action framework.28
The 4E Framework
The 4E framework, developed by Farkas et al,17 promoted both dissemination and utilization of new knowledge by providing stakeholder-specific (user-specific) strategies for accomplishing each “step” of the evidence-to-practice pipeline32—exposure, experience, expertise, and embedding (Figure 2). Farkas et al17 identified a goal for each phase of the framework, which progressively closes the gap between new evidence and its use in clinical practice. The first step, exposure, aims to increase targeted users' knowledge of the evidence.17 This often takes the form of more passive modes of dissemination, including articles and conference presentations. The goal of the next step, experience, is to prepare knowledge users to implement the information and evidence by improving their knowledge and attitudes toward its use.17 This is where “buy-in” plays a role. Without a positive attitude and the perception that the implementation of evidence will add value to their clinical practice, knowledge users will be less likely to incorporate it on a routine basis. The third and fourth steps aim to address more complex processes whereby knowledge users become competent in the skill or task (expertise) and sustain the utilization of the new knowledge in their clinical practice over time (embedding).17
Figure 2.
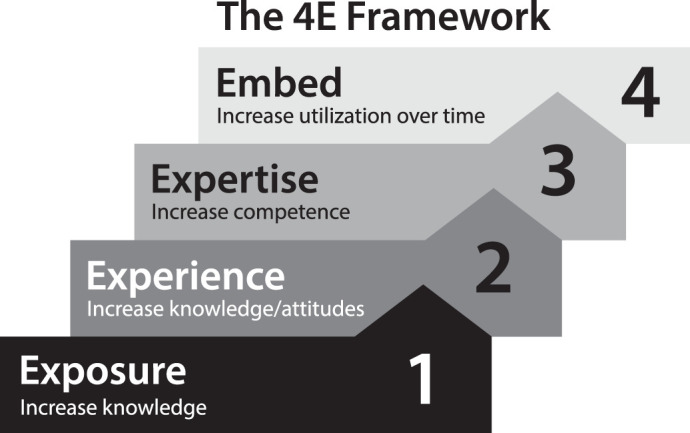
Components of the 4E framework.17
To further illustrate the functionality of the 4E framework, consider again the OAR example. As identified by Hankemeier et al,24 ATs were most familiar with the OAR compared with other clinical prediction rules, yet almost half reported using the OAR in 50% or fewer of applicable patient cases. This lack of OAR use suggests a halt in the process, prohibiting clinicians from translating their knowledge of the OAR into routine practice. Through professional or continuing education or both, clinicians are exposed to and made aware of the essential components of an injury evaluation, which should include any site-specific decision aids that can assist the evaluation process (eg, OAR). Clinicians progress to the experience phase of the framework and develop positive attitudes toward the use of the OAR when they perceive the decision aid as valuable to their practice (ie, effective tool for evaluation, good diagnostic accuracy, highly sensitive tool).
Having accomplished the first 2 phases, clinicians can now successfully move on to the next phase (expertise) and start incorporating the OAR into patient cases in their clinical practice. To effectively do so, Farkas et al17 proposed interactive training programs to directly teach and supervise clinicians who want to incorporate the new tool or technique (in this case, the OAR) to help increase their use and effectiveness. However, per the authors' suggestion, this phase of the 4E framework requires clinicians to seek out available training programs or individuals who are willing to supervise and provide feedback regarding OAR use in practice. Therefore, it is unsurprising that a clinician, particularly one with a limited community of practice, may be halted at this phase of the KT process.
The responsibility of the expertise phase should not be placed solely on the knowledge user. Knowledge producers and organizations can support this phase by developing training resources and tools that are translatable for knowledge users. Moreover, it is crucial that these resources and tools are also easily accessible and publicized for knowledge users seeking information and for those who are unaware. Currently, a majority of continuing education falls short of providing knowledge users with actionable steps to easily translate information. Although knowledge producers do a good job of introducing and discussing the details of emerging evidence, minimal time is spent on guiding the knowledge user in what to actually do with that information. This is true of the OAR example presented but also for other topics such as patient-reported outcome (PRO) measures. Most of the educational offerings regarding PRO measures detail the importance of PRO measures and how they are developed, validated, and scored, yet little attention has been given to what knowledge users should do with these scores and how that information should inform clinical decision making.
Alongside knowledge producers, professional organizations that offer continuing education efforts, such as the National Athletic Trainers' Association and the Board of Certification, can support the expertise phase of the 4E framework by creating opportunities within their infrastructure to facilitate KT. To do so, it is important that these organizations evaluate their current mechanisms for knowledge producers to disseminate information to knowledge users in order to determine whether restructuring is warranted and feasible. For example, a professional organization may do a good job of providing tools for knowledge users to assess areas of weakness and create professional development plans with goal setting, but without additional guidance, it is left to the knowledge user to seek out, complete, and translate evidence gained from continuing education opportunities to address those weaknesses and goals. This approach not only places a burden on knowledge users to filter through thousands of continuing education opportunities, but it does not aid the knowledge user in efficiently navigating the KT process.
The last phase of the framework, embedding, is more easily accomplished with programmatic or system-level support.17 Incorporating techniques at the system level, such as strategies that include organizational rules and policy changes to promote new norms and expectations, is typically effective because they include maintenance of change, which helps to drive knowledge use over time. For ATs looking to increase OAR use, this might entail the incorporation of a clinical-decision support feature within an electronic medical record to remind clinicians of the OAR or employer expectations to demonstrate the cost-effectiveness of athletic training services provided to patients with lower extremity injuries. However, it is possible that the embedding phase may also be facilitated without employer expectations, especially when clinicians directly see the value brought to their own practice from using the skill, technique, or procedure. Through OAR application, clinicians can see the significance of their use in providing more effective and efficient medical care (eg, limiting unnecessary referrals for imaging, reducing health care costs) to their patients, which promotes the sustained use of this clinical prediction rule over time.
Although the 4E framework provides a global approach to KT, the framework does not identify the specific steps needed to help overcome the knowledge-to-practice gap. For example, a knowledge user with limited support at the systems level to promote changes based on available evidence may struggle to complete both the expertise and embedding phases of the KT process. Therefore, to truly aid knowledge users in translating knowledge or evidence into practice, it is necessary to consider a more comprehensive KT model.
Knowledge-to-Action Framework
Graham et al28 provided a framework for understanding how research can be applied in clinical practice and how the best available evidence can be used as a component of decision making. The knowledge-to-action framework is composed of 2 interactive and dynamic processes—(1) knowledge creation and (2) knowledge application, also known as the action cycle28—and emphasizes the importance of both the knowledge producers and knowledge users in the KT process. Knowledge producers drive the “knowledge creation” component of the knowledge-to-action framework, in which the production of knowledge through primary research is combined and synthesized into more digestible and accessible formats. Graham et al28 illustrated that knowledge creation should ultimately lead to user-friendly products and tools (eg, practice guidelines, patient decision aids, algorithms) that knowledge users can directly implement in their practice to assist with the decision-making process (Figure 3). However, new knowledge, without an audience that uses it, remains just that—knowledge. Given that KT moves beyond the simple dissemination of information, it is important to consider the knowledge user's role in improving KT in the health care professions.
Figure 3.
Examples of each progression stage of the knowledge creation process.
As knowledge producers create and disseminate information, knowledge users are responsible for driving the information application (action cycle) component of the knowledge-to-action framework. Graham et al28 identified the action cycle as a fluid, multistep process that could be affected by the knowledge creation process, causing knowledge users to respond and adapt to the presence of new knowledge or outdated practices that may no longer be beneficial according to the best available evidence. The action cycle requires knowledge users to go through several steps, which, depending on contextual factors, may not be accomplished in this particular order: (1) identify the problem; (2) identify, review, and select knowledge to implement; (3) adapt knowledge to the local context; (4) select, tailor, and implement KT interventions; (5) monitor the interventions; (6) evaluate outcomes of knowledge use; and (7) determine strategies to sustain knowledge use (Figure 4).28 It has been widely reported that only about 14% of evidence is implemented into clinical practice,8 indicating a break or barrier in the action cycle that is preventing the complete application of new knowledge. It is plausible that the limited implementation of available evidence is due to the lack of evidence that is truly meaningful for clinical practice or to the lack of user-friendly products and tools that can aid in clinical implementation. Identifying exactly where that break occurs is a bigger challenge, but given the professional and continued preparation of knowledge users and skills mastered during those times, it may provide insight into this matter.
Figure 4.
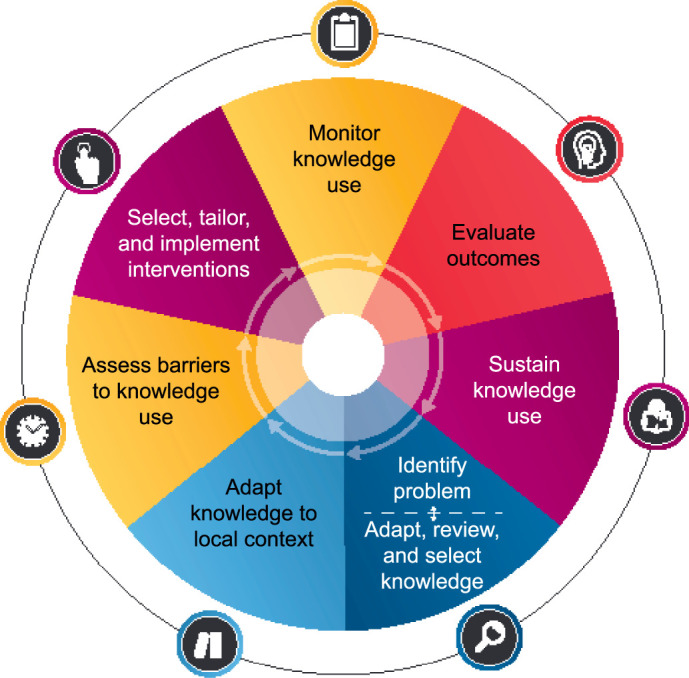
The knowledge application process of the knowledge-to-action framework. Adapted from Graham et al.28
Educational efforts are structured in a way that prepares knowledge users to appropriately appraise evidence (steps 2 and 3 of the action cycle in the knowledge-to-action framework) yet may not go as far as teaching them how to take what was found during the appraisal process and implement (or not implement) it into routine clinical practice using tailored interventions. Knowledge users appear to be skilled in identifying a problem when it occurs and searching and appraising the literature to find the most appropriate answer based on the available evidence. However, the actual implementation of evidence seems to be lacking.
Referring back to the OAR example, the identified lack of OAR use suggests a halt in the action cycle of the knowledge-to-action framework as early as the second phase, which requires knowledge users to adapt knowledge to the local context. Typically, a halt in adapting knowledge to the local context is tied to the burden of facing and overcoming barriers. From the available evidence, we can surmise that clinicians who are familiar with the OAR but do not implement them routinely in practice may likely encounter one or both of the following barriers:
Clinicians may be familiar with the overarching intent of the OAR, yet they may not recognize the utility of these clinical prediction rules to promote evidence-based clinical decision making or cost-effectiveness of care for patients or both.
Clinicians may understand the clinical utility of the OAR to support evidence-based decision making, but they may encounter barriers such as perceived time constraints, limited resources, and uncertainty about changing practice (eg, adopting the OAR into routine practice).
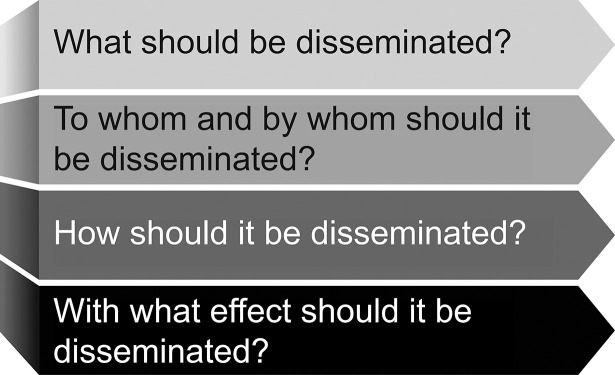
In both instances, it becomes the clinicians' responsibility to customize knowledge of the OAR to their particular situation. Identifying solutions to the first barrier is relatively straightforward. In this instance, clinicians need additional education to help promote positive attitudes and motivation to adapt OAR use to their local context. Although the clinicians may have felt they acquired enough knowledge about the OAR to progress to the next phase of the action cycle, recognizing the clinical utility of this decision aid is a necessary step before successful implementation can occur. Concurrently, knowledge producers and organizations can also aid in the development of solutions to overcome barriers by being mindful of what and how evidence is disseminated. Thus, as part of the dissemination process, knowledge producers should consider a series of questions to guide the development and distribution of evidence resources (Figure 5).
Figure 5.
The second barrier to OAR use identified herein is more challenging to overcome and represents real circumstances that ATs have reported facing when trying to make behavioral changes in their clinical practice.33,34 Still, by considering the phases of the action cycle as outlined by Graham et al,28 it is possible for clinicians to overcome these obstacles. Consider the perceived barrier of time and how the action cycle of the knowledge-to-action framework can be applied to help an AT implement the OAR into routine practice (Figure 4). The perception of time as a barrier is thought to be a complicated process. Whereas physical time constraints may certainly exist because of the culture and resources available at the clinical practice setting, it is also possible that mental time (ie, the time needed for cognitive processes to appraise and apply knowledge into practice) may account for the perception of insufficient time.33,35 Regardless, identifying interventions to overcome both physical and mental time constraints can help to achieve the end goal.
Athletic trainers familiar with the OAR may not recognize that they already incorporate the components of these clinical prediction rules as part of their routine patient evaluation (eg, palpation of bony landmarks, weight-bearing status). Therefore, a solution to overcome the perceived time barrier may be as simple as posting a visual depiction of the OAR near locations where patient evaluations routinely occur (eg, athletic training facility, athletic training kit for off-site evaluations). Similarly, the OAR can be incorporated into the electronic medical records system used for patient care documentation or embedded in evaluation sheets. Doing so will remind clinicians of the 4 OAR components each time a patient with a suspected ankle injury is evaluated. Over time, the clinician should become familiar with the OAR considerations and no longer rely on the visual aid.
The next phase of the action cycle (ie, monitor knowledge use) is a critical step for ensuring knowledge is being effectively translated.28 Simply posting a visual aid to remind oneself of the components of the OAR during patient evaluations is not sufficient. Instead, it is important that the clinician routinely monitor the effectiveness of the visual aid solution until the desired clinical practice change has been achieved. Doing so will allow the clinician to assess whether the targeted intervention (ie, posting a visual aid) has been effective in promoting behavioral change. If it is effective, the clinician can continue with the intent that, over time, the visual aid will no longer be necessary and the OAR will become a routine part of the evaluation process for patients with suspected ankle injuries. Conversely, if it is ineffective, the clinician should reflect on why the visual aid was not sufficient in promoting change and return to the “select, tailor, and implement KT interventions” phase28 to assess other possible solutions.
In addition to monitoring the application of the OAR in routine practice, it is also important for the clinician to take the time to evaluate whether OAR use has improved patient and systems outcomes.28 Although the OAR are promoted as a tool to help clinicians make more efficient clinical decisions grounded in evidence, it is critical for the clinician to consider how patient outcomes (eg, time loss due to injury) and systems outcomes (eg, cost-effectiveness of athletic training services) have been altered since routine implementation of the OAR. Doing so will help to further establish the sustainability of knowledge use (ie, incorporation of the OAR into routine patient care) and will also foster a feedback loop to ensure continuous quality improvement of the athletic training services provided. In summary, whereas the OAR example was used to illustrate the functionality of 2 KT models (4E framework,17 knowledge-to-action framework28), it is important to recognize that both models can be used globally across the profession to incorporate evidence into clinical practice.
A Call to Action for the Athletic Training Profession
The athletic training profession has made great progress in supporting evidence-based practice over the last decade; however, challenges persist, including the gap between the dissemination of evidence by knowledge producers (eg, researchers) and the utilization of evidence by knowledge users (eg, clinicians). In short, knowledge producers, knowledge users, and professional organizations that offer continuing education platforms (eg, National Athletic Trainers' Association, Board of Certification) must work together so that the knowledge users can effectively and efficiently adapt what the knowledge producers create and implement it in routine clinical practice. This not only requires that these 3 groups work together to ensure that clinically meaningful evidence is created and disseminated14 but also that each group identifies strategies to assist in the KT process.
Knowledge producers must consider dissemination and KT as part of their research design process and bear in mind the many different methods of dissemination, such as infographics, step-by-step guides, and interactive training tutorials. To facilitate the dissemination phase of a research study, knowledge producers should consider the basic questions proposed by others28,36 (Figure 5). Throughout this process, input from important stakeholders, including clinicians and patients, should be sought and considered. Professional organizations must reevaluate the platforms and mechanisms they offer for knowledge producers to disseminate evidence and consider whether changes to their infrastructure are warranted to serve as a bridge between knowledge dissemination and knowledge utilization. To facilitate KT, it is imperative that such organizations shift away from passive methods of dissemination and provide platform opportunities for knowledge producers that enable active learning while simultaneously requiring they provide actionable steps or accessible products and tools (or both) that knowledge users can readily translate into practice. Knowledge users must recognize both the benefits and barriers to incorporating evidence in their local context and seek support from knowledge producers and organizations to identify solutions for overcoming perceived barriers. Together, knowledge producers and knowledge users should work side-by-side to establish effective mechanisms to collect data at the point of care with the long-term goal of producing evidence that is clinically meaningful and translatable in routine clinical practice.15,16
Over the last decade, general calls have been made for researchers and clinicians to collaborate to narrow the research-to-practice gap on a global scale.14–16 Recently, Driban and Laursen14 further highlighted this gap and proposed several activities for both clinicians and researchers to aid in bridging the gap between athletic training research and clinical practice. Although these activities provide a strong foundational steppingstone to align athletic training research and clinical practice, most focus on collaboration throughout the research process with some attention to collaborative dissemination strategies. Despite these efforts, however, clinicians may continue to struggle to translate new evidence and overcome obstacles in their own local context, particularly if they do not have a strong community of practice. Therefore, in addition to the activities for evidence creation and dissemination suggested by Driban and Laursen,14 athletic training researchers and clinicians should consider KT models to help translate knowledge disseminated into knowledge used. This is a critical phase in the EBP process and, if implemented effectively, it may help to reduce health care costs, improve patient outcomes, and enhance the overall quality of care provided by ATs.
CONCLUSIONS
The athletic training profession has made significant progress toward developing an EBP culture over the last 2 decades. In general, knowledge producers have generated and disseminated more sophisticated research, whereas knowledge users have become more savvy consumers of the available literature. Yet a gap remains between the dissemination and use of evidence. Knowledge translation models have been demonstrated to be valuable tools to help bridge this gap within the health care community and should be encouraged within the athletic training profession. With the successful implementation of KT models by all stakeholders (eg, researchers, clinicians, professional organizations), the athletic training profession may be able to realize a more complete EBP culture and enhance the overall quality of care provided to patients.
Supplementary Material
ACKNOWLEDGMENTS
We thank Jamie Carroll for his contributions to the graphic design of the figures included in this report.
REFERENCES
- 1.Institute of Medicine (US) Committee on the Health Professions Education Summit; Greiner AC, Knebel E. Health Professions Education: A Bridge to Quality. National Academies Press; 2003. [PubMed]
- 2.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ . 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sauers EL. Establishing an evidence-based practice culture: our patients deserve it. Athl Train Sports Health Care . 2009;1(6):244–247. doi: 10.3928/19425864-20091019-01. [DOI] [Google Scholar]
- 4.Standards for the Accreditation of Professional Athletic Training Programs. Commission on Accreditation of Athletic Training Education. 2020. Published. Accessed August 12, 2020. https://caate.net/pp-standards/
- 5.Standards for the Accreditation of Post-Professional Athletic Training Degree Programs. Commission on Accreditation of Athletic Training Education. 2020. Accessed August 12. https://caate.net/wp-content/uploads/2017/01/2014-Standards-for-Accreditation-of-Post-Professional-Degree-Programs.pdf .
- 6.Standards for the Accreditation of Post-Professional Athletic Training Residency Programs. Commission on Accreditation of Athletic Training Education. 2020. Accessed August 12. http://caate.net/wp-content/uploads/2014/06/CAATE-Post-Professional-Residency-Standards-2012-2.pdf .
- 7.Board of Certification. Certification maintenance requirements. Published 2015. Accessed August 12, 2020. https://bocatc.org/athletic-trainers#ebp-category .
- 8.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform . 2000;(1):65–70. [PubMed] [Google Scholar]
- 9.Grol R, Grimshaw J. Evidence-based implementation of evidence-based medicine. Jt Comm J Qual Improv . 1999;25(10):503–513. doi: 10.1016/s1070-3241(16)30464-3. [DOI] [PubMed] [Google Scholar]
- 10.Welch CE, Hankemeier DA, Wyant AL, Hays DG, Pitney WA, Van Lunen BL. Future directions of evidence-based practice in athletic training: perceived strategies to enhance the use of evidence-based practice. J Athl Train . 2014;49(2):234–244. doi: 10.4085/1062-6050-49.2.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron C, Naylor CD. No impact from active dissemination of the Ottawa Ankle Rules: further evidence of the need for local implementation of practice guidelines. CMAJ . 1999;160(8):1165–1168. [PMC free article] [PubMed] [Google Scholar]
- 12.Fritsche L, Greenhalgh T, Falck-Ytter Y, Neumayer H, Kunz R. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin Questionnaire and before and after study of courses in evidence based medicine. BMJ . 2002;325(7376):1338–1341. doi: 10.1136/bmj.325.7376.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy T, Regehr G, Rosenfield J, Roberts SW, Lingard L. Exploring the gap between knowledge and behavior: a qualitative study of clinician action following an educational intervention. Acad Med . 2004;79(5):386–393. doi: 10.1097/00001888-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Driban JB, Laursen RM. Starting a dialogue: athletic training researchers and clinicians. Int J Athl Ther Train . 2019;24(2):41–43. doi: 10.1123/ijatt.2019-0018. [DOI] [Google Scholar]
- 15.Sauers EL, Valovich McLeod TC, Bay RC. Practice-based research networks, part I: clinical laboratories to generate and translate research findings into effective patient care. J Athl Train . 2012;47(5):549–556. doi: 10.4085/1062-6050-47.5.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lam KC, Welch Bacon CE, Sauers EL, Bay RC. Point-of-care clinical trials in sports medicine research: identifying effective treatment interventions through comparative effectiveness research. J Athl Train . 2020;55(3):217–228. doi: 10.4085/1062-6050-307-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farkas M, Jette AM, Tennstedt S, Haley SM, Quinn V. Knowledge dissemination and utilization in gerontology: an organizing framework. Gerontologist . 2003;43(suppl 1):47–56. doi: 10.1093/geront/43.suppl_1.47. [DOI] [PubMed] [Google Scholar]
- 18.Shuval K, Berkovits E, Netzer D, et al. Evaluating the impact of an evidence-based medicine educational intervention on primary care doctors' attitudes, knowledge and clinical behaviour: a controlled trial and before and after study. J Eval Clin Pract . 2007;13(4):581–598. doi: 10.1111/j.1365-2753.2007.00859.x. [DOI] [PubMed] [Google Scholar]
- 19.Welch CE, Van Lunen BL, Hankemeier DA, et al. Perceived outcomes of web-based modules designed to enhance athletic trainers' knowledge of evidence-based practice. J Athl Train . 2014;49(2):220–233. doi: 10.4085/1062-6050-49.2.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tu K, Davis D. Can we alter physician behavior by educational methods? Lessons learned from studies of the management and follow-up of hypertension. J Contin Educ Health Prof . 2002;22(1):11–22. doi: 10.1002/chp.1340220103. [DOI] [PubMed] [Google Scholar]
- 21.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ . 1998;317(7156):465–468. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bernhardt JM, Mays D, Kreuter MW. Dissemination 2.0: closing the gap between knowledge and practice with new media and marketing. J Health Commun . 2011;16(suppl 1):32–44. doi: 10.1080/10810730.2011.593608. [DOI] [PubMed] [Google Scholar]
- 23.Graham ID, Stiell IG, Laupacis A, et al. Awareness and use of the Ottawa Ankle and Knee rules in 5 countries: can publication alone be enough to change practice? Ann Emerg Med . 2001;37(3):259–266. doi: 10.1067/mem. 2001.113506. [DOI] [PubMed] [Google Scholar]
- 24.Hankemeier DA, Popp JK, Walker SE. Familiarity with and use of clinical prediction rules and patient-rated outcome measures. Athl Train Sports Health Care . 2017;9(3):108–123. doi: 10.3928/19425864-20170112-02. [DOI] [Google Scholar]
- 25.Barelds I, Krijnen WP, van de Leur JP, van der Schans CP, Goddard RJ. Diagnostic accuracy of clinical decision rules to exclude fractures in acute ankle injuries: systematic review and meta-analysis. J Emerg Med . 2017;53(3):353–368. doi: 10.1016/j.jemermed. 2017.04.035. [DOI] [PubMed] [Google Scholar]
- 26.Jenkin M, Sitler MR, Kelly JD. Clinical usefulness of the Ottawa Ankle Rules for detecting fractures of the ankle and midfoot. J Athl Train . 2010;45(5):480–482. doi: 10.4085/1062-6050-45.5.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciliska D. Evidence-based nursing: how far have we come? What's next? Evid Based Nurs. 2006;9(2):38–40. doi: 10.1136/ebn.9.2.38. [DOI] [PubMed] [Google Scholar]
- 28.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof . 2006;26(1):13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- 29.Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential for savings. JAMA . 2019;322(15):1501–1509. doi: 10.1001/jama.2019.13978. [DOI] [PubMed] [Google Scholar]
- 30.About us. Canadian Institutes of Health Research. Published July 28, 2016. Accessed August 12, 2020. http://www.cihr-irsc.gc.ca/e/29418.html .
- 31.Strifler L, Cardoso R, McGowan J, et al. Scoping review identifies significant number of knowledge translation theories, models, and frameworks with limited use. J Clin Epidemiol . 2018;100:92–102. doi: 10.1016/j.jclinepi.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 32.Lang ES, Wyer PC, Haynes RB. Knowledge translation: closing the evidence-to-practice gap. Ann Emerg Med . 2007;49(3):355–363. doi: 10.1016/j.annemergmed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 33.McCarty CW, Hankemeier DA, Walter JM, Newton EJ, Van Lunen BL. Use of evidence-based practice among athletic training educators, clinicians, and students, part 2: attitudes, beliefs, accessibility, and barriers. J Athl Train . 2013;48(3):405–415. doi: 10.4085/1062-6050-48.2.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Welch Bacon CE, Eppelheimer BL, Kasamatsu TM, Lam KC, Nottingham SL. Athletic trainers' perceptions of and barriers to patient care documentation: a report from the Athletic Training Practice-Based Research Network. J Athl Train . 2017;52(7):667–675. doi: 10.4085/1062-6050-52.3.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thompson DS, O'Leary K, Jensen E, Scott-Findlay S, O'Brien-Pallas L, Estabrooks CA. The relationship between busyness and research utilization: it is about time. J Clin Nurs . 2008;17(4):539–548. doi: 10.1111/j.1365-2702.2007.01981.x. [DOI] [PubMed] [Google Scholar]
- 36.Lavis JN, Robertson D, Woodside JM, McLeod CB, Abelson J. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q . 2003;81(2):221–248. doi: 10.1111/1468-0009.t01-1-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.