Abstract
Context
Concussion underreporting leads to delays in diagnosis and treatment, prolonging recovery time. Athletes' self-reporting of concussion symptoms, therefore, reduces risk.
Objective
To evaluate the effectiveness of 3 concussion-education programs in improving concussion-reporting intention.
Design
Randomized controlled clinical trial.
Setting
Three high schools in California.
Patients or Other Participants
A total of 118 male football players (age = 14.88 ± 1.19 years).
Intervention(s)
Participants were randomly assigned to receive concussion education via CrashCourse (CC), Centers for Disease Control and Prevention (CDC) video education materials (CDC-Vi), or CDC written education materials (CDC-Wr).
Main Outcome Measure(s)
The primary outcome was concussion-reporting intention, which was assessed at baseline, immediately after education, and at 1-month follow-up. Secondary outcomes were concussion knowledge, concussion-reporting attitudes, perceived concussion-reporting norms, and perceived behavioral control.
Results
Across all education formats, a total sample of athletes improved in concussion-reporting intention at immediate and 1-month follow-ups (mean improvements = 6.8% and 11.4%, respectively; F4,224 = 11.1, P < .001). Similar findings were observed across all education formats in secondary analyses examining knowledge, attitudes, and perceived behavioral control. However, we noted differences in concussion-reporting intention by education format and time (F4,224 = 2.8, P = .03). Post hoc analysis showed that athletes who received CC had increased concussion-reporting intentions at immediate and 1-month follow-ups (baseline = 4.7, immediate follow-up = 6.1, 1-month follow-up = 6.0; F16,61.1 = 6.1, P = .007) compared with increases only at 1-month follow-up for CDC-Vi (baseline = 4.3, immediate follow-up = 5.2, 1-month follow-up = 5.8; F1.6,61.6 = 8.4, P = .001) and no improvement for CDC-Wr (P = .10). Secondary analyses indicated differences between CC and both CDC interventions in concussion knowledge and attitudes at immediate and 1-month follow-ups. We identified no differences in perceived behavioral control among interventions (F4,216 = 0.2, P = .93) or perceived concussion-reporting norms across (F4,224 = 0.3, P = .73) or among (F4,224 = 1.7, P = .15) interventions.
Conclusions
All athletes exhibited an improved intent to report concussions, increased concussion knowledge, better concussion attitudes, and more perceived behavioral control at both immediate and 1-month follow-ups. However, athletes randomized to receive CC reported a greater intent to report concussion, more knowledge, and improved concussion-reporting attitudes when compared with those who received CDC-Vi and CDC-Wr.
Keywords: mild traumatic brain injury, CrashCourse, reporting
Key Points
The total sample of athletes exhibited improved intentions to report concussions immediately after education and at 1-month follow-up.
Only athletes who received CrashCourse or Centers for Disease Control and Prevention video educational materials showed improvement in concussion-reporting intention, whereas those who received Centers for Disease Control and Prevention written educational materials did not.
An education program such as CrashCourse may be more effective in improving concussion-reporting intentions immediately after education.
In the United States, an estimated 1.1 to 1.9 million concussions occur annually in people aged ≤18 years, with most sustained during athletics and recreational activities.1 Although the vast majority of concussions are thought to lead only to acute symptoms that resolve in days or weeks, serious acute and chronic neurologic consequences are possible.2,3 Despite the high incidence of concussion and possible consequences associated with these injuries, athletes underreport concussions, which may lead to delays in treatment and recovery, an increased risk of future concussions, and worse outcomes.4–10 Increasing youth awareness, knowledge, and reporting norms can promote prevention, enhance recovery, and benefit public health.9,11,12
Researchers13–20 have evaluated the efficacy of available concussion-education materials using the theory of planned behavior (TPB). This theory posits that true behavioral change is presaged by behavioral intent (motivation), which is most closely linked to an individual's attitudes toward positive behavioral outcomes and thus to behavior (reporting), subjective and social normative behavior (peer and social approval of reporting), and perceived behavioral control (ease of reporting). The TBP model has limitations, one assumption being that individuals have equal access to the resources and knowledge necessary to engage in a specific behavior. As such, directly examining the immediate and delayed efficacy of concussion-education programs bridges the gap between TBP theoretical limitations and its application to concussion reporting. Investigators9,14,15,20 have shown that TPB is a useful predictive model for adolescent concussion-reporting behavior: all 3 constructs (behavioral beliefs, perceived reporting norms, and control beliefs) were associated with concussion-reporting intention (motivation) and concussion reporting (behavioral change).
Although substantial focus has been placed on concussion-education paradigms, little empirical evidence of their efficacy is available. Comparative evaluation of concussion-education programs is also limited. In addition, few authors have examined the extent to which changes persist over time; most have addressed changes in concussion-reporting intent and TPB constructs immediately after the education, with no follow-up to evaluate the retention of observed changes.
For the most widely used concussion-education interventions, the long-term effects on concussion-reporting intention and concussion-reporting behavior have not been studied.21 However, those that have been assessed may not have shown long-term changes in athlete concussion-reporting intent and behavior for several reasons.22 First, educational programs may inadequately target the perceived and tangible interpersonal, team-based, and societal pressures that result in an athlete's decision not to report concussions.12 Second, educational programs may not effectively address the knowledge gaps necessary to understand the consequences of not reporting a concussion due to lack of engagement, lack of perceived validity of the education messenger, or health inequities.12,23 Third, educational interventions administered at a single time point may be ill suited to the sustained conversations necessary for long-term behavioral change.12
Over the past decade, the most commonly used concussion-education materials in the United States have been free resources provided by the Centers for Disease Control and Prevention (CDC). Evaluations of previous versions of these materials have provided unclear evidence of efficacy.18,19 In November 2018, the free video-based concussion-education program CrashCourse (CC) was released by TeachAids, a 501(c)3 nonprofit organization. This program has been adopted by most youth football organizations (eg, USA Football, American Youth Football, and Pop Warner Football), various US Olympic Committee partnerships (eg, US Speedskating, USA Field Hockey, USA Wrestling), medical organizations (eg, Brain Injury Association of America, Lucile Packard Children's Hospital Stanford), and high school partnerships (eg, state high school athletic associations of North Carolina and Arkansas). The efficacy of this program has not been formally assessed.
The purpose of our study was to evaluate the efficacy of 3 concussion-education programs, CC, CDC video materials (CDC-Vi), and CDC written materials (CDC-Wr), in improving athletes' concussion-reporting intentions. Concussion-reporting intention was used as the primary outcome given its proximal relationship to true concussion reporting.14,15,20 We hypothesized that athletes would improve in concussion-reporting intention after all educational interventions, with greater gains after CC than after CDC-Vi or CDC-Wr. Secondary analyses were performed to evaluate the effect of the programs on metrics related to concussion knowledge and TPB constructs.
METHODS
Participants
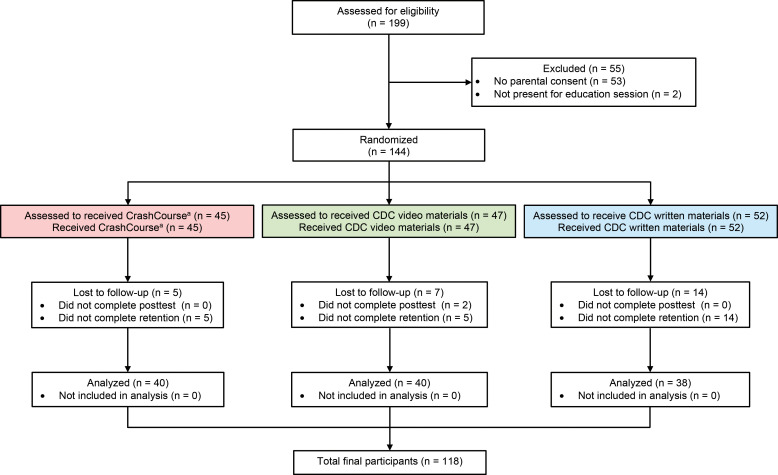
Participants were recruited from the rosters of 3 high school football teams in California. Volunteers were included if they attended practice on both study dates and provided written informed assent and parental or guardian consent. Individuals were excluded if they did not complete >50% of the questionnaire. Figure 1 outlines study enrollment. All research activities were reviewed and approved by the Stanford University Institutional Review Board. The ClinicalTrials.gov trial ID number was NCT04492696.
Figure 1.
Study enrollment. a TeachAids. Abbreviation: CDC, Centers for Disease Control and Prevention.
Procedures
In this randomized controlled trial, all participants (n = 118) completed study questionnaires and education using individual computers with personal headsets between August 2018 and October 2018. A randomizing program assigned students to 1 of 3 classrooms to ensure that no athletes viewed any of the other concussion-education programs. After conducting roll call, confirming athlete assent and parental or guardian consent, and reading a scripted instruction, the research assistants presented athletes with a Qualtrics link that administered the initial questionnaire and the specific intervention for that group (CC, CDC-Vi, or a PDF of CDC-Wr). After the education was provided, the software automatically loaded the immediate follow-up questionnaire. One month after the education, athletes completed another follow-up. The study staff were not affiliated with any of the concussion-education programs. Interventions and questionnaires were administered simultaneously for all athletes across the interventions.
Independent Variables
Intervention 1: The CrashCourse Video
The CrashCourse approach to concussion education was informed by user-centered formative-design research studies. The 12-minute video-based curriculum synthesized first- and third-person experiential perspectives to inform and motivate learning about concussion signs and symptoms, correct myths and misconceptions, recognize the seriousness of reporting, and communicate the importance of working with a physician to determine the best strategy for improvement. CrashCourse integrated these topics into a narrative, story-driven format with the learner at the center of the educational experience. Specifically, it began by placing learners in a simulated real-life, high-stakes sport scenario (Friday night football game). During the scenario, the learner received a concussion. Through a choose your own adventure approach, the learner decided between 2 options: Take a Knee or Stay in the Game. Each decision led the learner down a different path to reflecting the consequences (both positive and negative). However, the educational content presented in the 2 pathways was identical, as the learner was also shown what would have happened if the alternate decision had been made. Throughout the educational intervention, the learner was guided by near-peer National Collegiate Athletic Association Division I collegiate football athletes.24
Intervention 2: The CDC “Concussion in Sports” Video
The CDC-Vi was an online learning module developed by the CDC and the National Federation of State High School Associations Learning Center. The course aimed to educate high school coaches, officials, parents, and students on the importance of proper concussion recognition and management. The material highlighted the effect of sport-related concussion on athletes, taught how to recognize a suspected concussion, and provided protocols for managing a suspected concussion with steps to help players return to play safely postconcussion. The curriculum had 4 units: “Concussion Overview,” “The Problem,” “Your Responsibilities,” and “Review.” The content was delivered via videos (total time = 25 minutes), 6 slides, and a final 9-question quiz. The video content included a “teachable-moment” scenario between a coach and athlete discussing their school's return-to-school and return-to-play policies. Learners progressed through the curriculum sequentially and must have completed each unit before proceeding to the next. Each state's concussion-management requirements were included in the course. A Spanish track was also available. The primary narrator of CDC-Vi was Michael Koester, MD, Chair of the National Federation of State High School Associations Sports Medicine Advisory Committee.25
Intervention 3: The CDC Concussion Fact Sheets
The CDC-Wr consisted of educational PDFs available for download from the CDC website as part of the CDC's “HEADS UP” brain injury awareness initiative. The PDFs used for the CDC-Wr condition were specific to high school athlete concussion education: “Concussion Fact Sheet for High School Athletes” (590 words), “Concussion Information Sheet” (1244 words), “A Fact Sheet for Athletes” (540 words), “Facts About Concussion and Brain Injury” (493 words), “Signs and Symptoms Poster” (122 words), and “Sports Safety Posters: Football Brain Safety” (61 words).25
Dependent Variables: Education Efficiency Measures
All primary and secondary outcomes, besides those related to concussion knowledge, were assessed based on the athletes' responses on a 10-point Likert-type scale ranging from 1 (strongly disagree) to 10 (strongly agree) to specific questions related to that domain. A composite measure for each outcome was created by summing athletes' responses and dividing by the number of questions asked, resulting in outcomes scaled from 1 to 10. Specific survey items were individually evaluated to ensure construct validity while maximizing brevity of the overall assessment.
Concussion-Reporting Intention
A composite measure (Cronbach α = 0.92) was created based on the inverse of athletes' responses to 5 questions about their concussion-reporting intentions (ie, whether they would continue playing with a concussion during the beginning of the season, a practice, the middle of the season, or a championship game and at the end of the season).
Concussion Knowledge
Athletes answered 23 true/false questions modified from previous concussion-education assessments to assess their concussion knowledge.26 A composite measure of athlete concussion knowledge was created by summing athletes' correct responses and dividing by the number of questions asked (Cronbach α = 0.77).
Concussion-Reporting Attitudes
A composite measure (Cronbach α = 0.87) was created based on athletes' responses to 6 questions about their attitudes toward concussion reporting (ie, the extent to which an athlete who reports a concussion would be better off in the long run, back on the field much faster, proud even if teammates call me weak, better off avoiding participation with signs and symptoms of a concussion, not better off hiding symptoms from a doctor to not stay out as long, and not better off toughing it out because concussions are just another injury).
Perceived Concussion-Reporting Norms
A composite measure (Cronbach α = 0.80) was created based on athletes' responses to 2 questions assessing perceived concussion-reporting norms (normative beliefs; ie, the extent to which the athlete worried my teammates would think less of me if he reported a concussion or needed to hide my symptoms from my coach).
Perceived Behavioral Control
A composite measure (Cronbach α = 0.97) was created based on the athletes' responses to 6 questions about their perceived ability and confidence in concussion reporting (ie, confidence in my ability to report a concussion, to help my teammate report a concussion, to report symptoms of a concussion, to help my teammate report symptoms of a concussion, to report symptoms of a concussion even if I don't think they're that bad, and to help my teammate report symptoms of a concussion even if I don't think they're that bad).
Statistical Analysis
Independent-samples t tests for continuous measures or χ2 tests for categorical measures were used to assess demographic differences among groups. We calculated the Shapiro-Wilk test to evaluate the data for normality and nonparametric testing for non-normal data. When expected cell values were <5, the Fisher exact test was conducted in place of a χ2 test. Group differences in outcomes across time points were investigated using repeated-measures analysis of variance (ANOVA) with 1 between-subjects factor (group) and 1 within-subject factor (pretest, immediate follow-up, and 1-month follow-up) and an α level of .05. Although repeated-measures ANOVA assumes normality, an advantage of this analysis was its robustness to violations of normality, particularly with sample sizes >20. When sphericity could not be assumed, we applied Greenhouse-Geisser corrections. We calculated 95% CIs for repeated-measures and post hoc ANOVAs. Bonferroni corrections were performed for all post hoc tests to account for multiple comparisons, with an α level of .0125. To examine the effect of attrition on outcomes, ANOVA was used to determine if the dependent variables differed at baseline or if the data could be assumed to be missing at random (demographic information was not examined in this way because it was collected at the 1-month follow-up). Next, for all participants who completed the baseline assessment, multiple imputation using predictive mean matching generated 5 imputed data sets to plausibly approximate values missing because of attrition; these imputed datasets were combined and analyzed for group differences in outcomes across time points using repeated-measures ANOVA as described. Analyses were performed using SPSS (version 20.0; IBM Corp) or R (version 3.6; The R Project for Statistical Computing).
RESULTS
Sample Characteristics
A total of 118 male football players (age = 14.88 ± 1.19 years, age range = 13–18 years), participated in the study (Table 1). Age was not normally distributed (W112 = 0.92, P < .001). Of the 79 athletes reporting ethnicity, 32.9% (n = 26) identified as Hispanic/Latino, with no differences between groups ( = 0.2, P = .92). Of the 79 athletes reporting race, 12.7% (n = 10) identified as African American/Black; 5.1% (n = 4) as Asian; 17.7% (n = 14) as Native Hawaiian/Pacific Islander; 1.3% (n = 1) as Native American/Alaskan Native; 48.1% (n = 38) as White; and 10.1% (n = 8) as other/multiple. Among athletes, 35.7% (n = 25 of 70) reported qualifying for free or reduced-cost lunch, with no differences between groups (
= 0.2, P = .92). Of the 79 athletes reporting race, 12.7% (n = 10) identified as African American/Black; 5.1% (n = 4) as Asian; 17.7% (n = 14) as Native Hawaiian/Pacific Islander; 1.3% (n = 1) as Native American/Alaskan Native; 48.1% (n = 38) as White; and 10.1% (n = 8) as other/multiple. Among athletes, 35.7% (n = 25 of 70) reported qualifying for free or reduced-cost lunch, with no differences between groups ( = 0.2, P = .43); 61.5% (n = 48 of 69) reported competing at the varsity level, with no differences between groups (
= 0.2, P = .43); 61.5% (n = 48 of 69) reported competing at the varsity level, with no differences between groups ( = 2.9, P = .24); 26.1% (n = 18) reported that they had a previously diagnosed concussion, with no differences between groups (
= 2.9, P = .24); 26.1% (n = 18) reported that they had a previously diagnosed concussion, with no differences between groups ( = 0.89, P = .96); and 85.0% (n = 51 of 60) reported having a close friend or family member with a previously diagnosed concussion. We observed no differences among groups across demographic variables.
= 0.89, P = .96); and 85.0% (n = 51 of 60) reported having a close friend or family member with a previously diagnosed concussion. We observed no differences among groups across demographic variables.
Table 1.
Participant Characteristics
| Characteristic |
Education Formata |
Total |
P Valuec |
||
| CrashCourseb |
Centers for Disease Control and Prevention Video Materials |
Centers for Disease Control and Prevention Written Materials |
|||
|
|
Mean ± SD |
||||
| Age, y | 14.4 ± 1.0 | 15.1 ± 1.3 | 15.1 ± 1.1 | 14.9 ± 1.2 | .10 |
| No. (%) |
|
||||
| n = 39 | n = 40 | n = 36 | n = 115 | ||
| 13 | 8 (20.5) | 6 (15.0) | 3 (8.3) | 17 (14.8) | |
| 14 | 14 (35.9) | 6 (15.0) | 7 (19.4) | 27 (23.5) | |
| 15 | 10 (25.6) | 10 (25.0) | 13 (36.1) | 33 (28.7) | |
| 16 | 7 (17.9) | 13 (32.5) | 10 (27.8) | 30 (26.1) | |
| 17 | 0 (0.0) | 5 (12.5) | 2 (5.6) | 7 (6.1) | |
| 18 | 0 (0.0) | 0 (0.0) | 1 (2.8) | 1 (0.9) | |
| Race | .29 | ||||
| African American or Black | 3 (12.0) | 6 (20.4) | 1 (4.0) | 10 (12.7) | |
| Asian | 1 (4.0) | 0 (0.0) | 3 (12.0) | 4 (5.1) | |
| Native Hawaiian or Pacific Islander | 3 (12.0) | 4 (13.6) | 7 (28.0) | 14 (17.7) | |
| Native American or Alaskan Native | 1 (4.0) | 0 (0.0) | 0 (0.0) | 1 (1.3) | |
| White | 11 (44.4) | 15 (15.7) | 12 (48.0) | 38 (48.1) | |
| Other/multiple | 4 (16.0) | 2 (6.9) | 2 (8.0) | 8 (10.1) | |
| Ethnicity | n = 25 | n = 79 | .92 | ||
| Hispanic/Latino | 9 (36.0) | 9 (30.9) | 8 (32.0) | 26 (32.9) | |
| Not Hispanic/Latino | 16 (64.0) | 20 (69.1) | 17 (68.0) | 53 (67.1) | |
| Parent's highest education | n = 22 | n = 28 | n = 25 | n = 75 | .33 |
| Less than high school | 2 (9.1) | 2 (7.1) | 1 (4.0) | 5 (6.7) | |
| Some high school | 4 (18.2) | 4 (14.3) | 2 (8.0) | 10 (13.3) | |
| High school diploma/GED | 0 (0) | 1 (3.6) | 5 (20.0) | 6 (8.0) | |
| Some college | 0 (0.0) | 0 (0.0) | 7 (28.0) | 7 (9.3) | |
| Technical school | 9 (40.9) | 5 (17.9) | 1 (4.0) | 15 (20.0) | |
| Bachelor's degree | 2 (9.1) | 6 (21.4) | 2 (8.0) | 10 (13.3) | |
| Graduate/professional degree | 5 (22.7) | 10 (35.7) | 7 (28.0) | 22 (29.3) | |
| Free or reduced-cost lunch? | n = 21 | n = 25 | n = 24 | n = 70 | .43 |
| Yes | 6 (28.6) | 8 (32.0) | 11 (45.8) | 25 (35.7) | |
| No | 15 (71.4) | 17 (68.0) | 13 (54.2) | 45 (64.3) | |
| Annual household income, $ | n = 8 | n = 11 | n = 4 | n = 23 | .63 |
| <20 000 | 1 (12.5) | 0 (0.0) | 0 (0.0) | 1 (4.3) | |
| 20 000–30 000 | 1 (12.5) | 2 (18.2) | 0 (0.0) | 3 (13.0) | |
| 30 000–49 000 | 1 (12.5) | 0 (0.0) | 1 (25.0) | 2 (8.7) | |
| 50 000–74 000 | 0 (0.0) | 1 (9.1) | 0 (0.0) | 1 (4.3) | |
| >75 000 | 5 (62.5) | 8 (72.7) | 3 (75.0) | 16 (69.6) | |
| Position | .39 | ||||
| Lineman | 9 (36.0) | 8 (29.6) | 13 (54.2) | 30 (39.5) | |
| Linebacker | 5 (20.0) | 7 (25.9) | 5 (20.8) | 17 (22.4) | |
| Defensive back | 5 (20.0) | 4 (14.8) | 3 (12.5) | 12 (15.8) | |
| Receiver | 2 (8.0) | 6 (22.2) | 5 (20.8) | 13 (17.1) | |
| Special teams | 2 (8.0) | 1 (3.7) | 2 (8.3) | 5 (6.6) | |
| Quarterback | 1 (4.0) | 0 (0.0) | 2 (8.3) | 3 (3.9) | |
| Other | 1 (4.0) | 1 (3.7) | 3 (12.5) | 5 (6.6) | |
| Level | n = 25 | n = 27 | n = 26 | n = 78 | .24 |
| Varsity | 12 (48.0) | 18 (66.7) | 18 (69.2) | 48 (61.5) | |
| Junior varsity | 13 (52.0) | 9 (33.3) | 8 (30.8) | 30 (38.5) | |
| Past concussion diagnosis | |||||
| Self | 6 (27.3) | 6 (27.3) | 6 (24.0) | 18 (26.1) | .96 |
| Close friend/family | 19 (95.0) | 18 (90.0) | 14 (70.0) | 51 (85.0) | .06 |
Abbreviation: GED, general equivalency diploma.
Numbers in parentheses reflect percentages of total respondents for that question; not all athletes responded to every question.
TeachAids.
Independent-samples t test for continuous data or χ2 test of categorical data was used to assess differences among groups. Fisher exact test was used in place of χ2 test when expected cell values were <5.
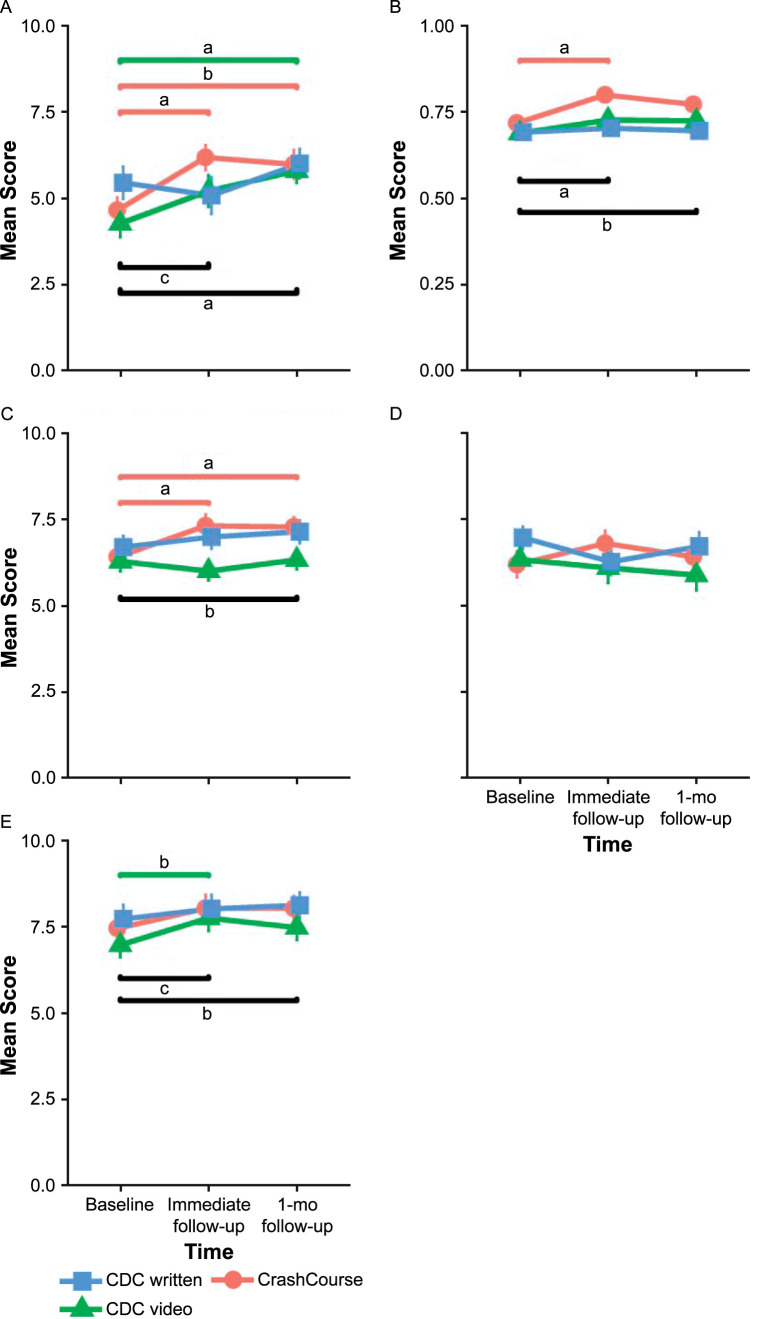
Intention to Report Concussions
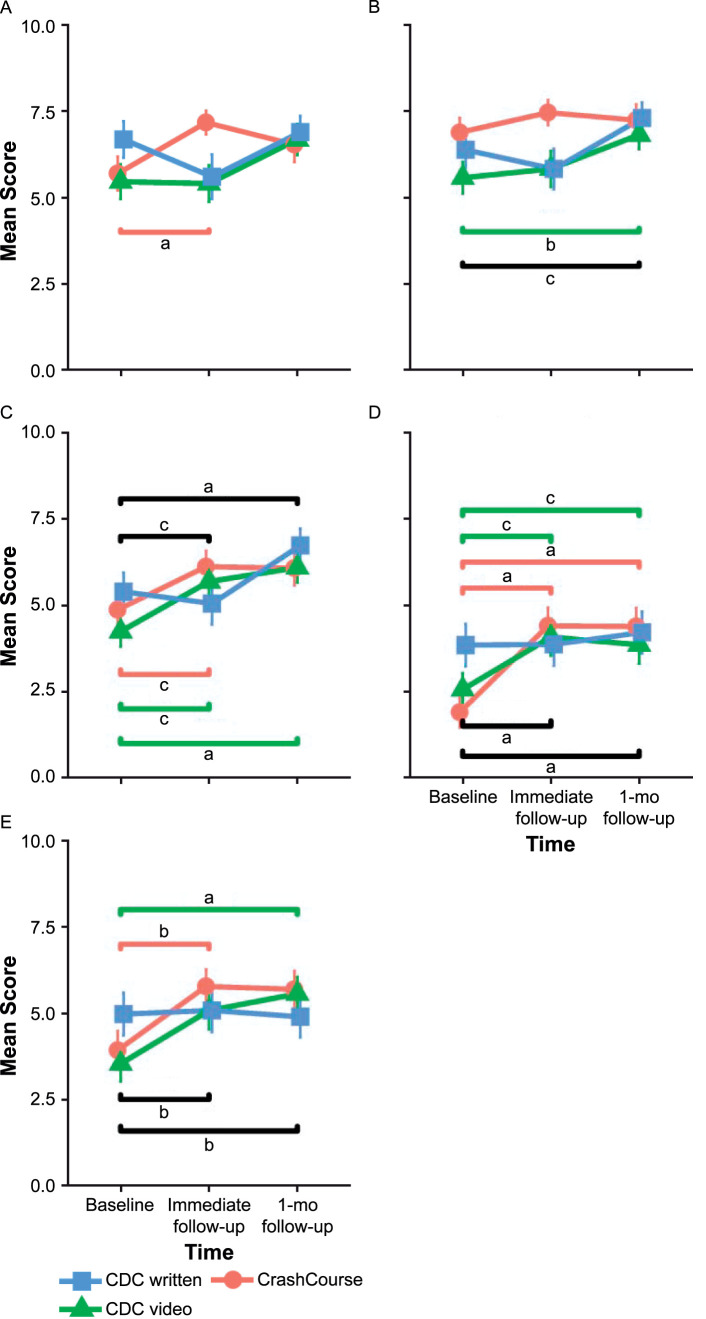
All results for the primary and secondary outcomes, including 95% CIs and differences, are provided in Table 2. We observed an improvement in the intention to report concussions across the total sample of athletes (baseline = 4.8, immediate follow-up = 5.5, and 1-month follow-up = 5.9; F4,224 = 11.1, P < .001; Figure 2A). However, a repeated-measures ANOVA indicated differences by education format and time (F4,224 = 2.8, P = .03). Post hoc testing revealed that the improved scores for intention to report concussions were driven entirely by CC and CDC-Vi; we noted improved concussion-reporting intention scores for CC (baseline = 4.7, immediate follow-up = 6.1, 1-month follow-up = 6.0; F1.6,61.1 = 6.1, P = .007) and CDC-Vi (baseline = 4.3, immediate follow-up = 5.2, 1-month follow-up = 5.8; F1.6,61.6 = 8.4, P = .001) but not for CDC-Wr (baseline = 5.5, immediate follow-up = 5.1, 1-month follow-up = 6.0; F1.6,60 = 2.6, P = .10). Secondary analyses to evaluate reporting at different hypothetical time points within the season showed differences among the interventions at immediate follow-up in the intention to report concussions at the beginning of the season (CC baseline = 5.7, immediate follow-up = 7.1; CDC-Vi baseline = 5.4, immediate follow-up = 5.4; CDC-Wr baseline = 6.7, immediate follow-up = 5.6; F4,218 = 0.5, P = .009) and during a championship game (CC baseline = 1.9, immediate follow-up = 4.3; CDC-Vi baseline = 2.6, immediate follow-up = 4.1; CDC-Wr baseline = 3.8, immediate follow-up = 3.9; F2,218 = 0.5, P = .02; Figure 3). Behavioral intention was not normally distributed in the primary (W112 = 0.96, P = .002) or secondary (W112 = 0.96, P = .004) analysis.
Table 2.
Differences in Outcome Measures Among Education Interventionsa Continued on Next Page
| Outcome |
All Athletes (n = 118) |
Group |
Group × Time P Valuec |
||
| CrashCourseb (n = 40) |
Centers for Disease Control and Prevention Video Materials (n = 40) |
Centers for Disease Control and Prevention Written Materials (n = 38) |
|||
| Primary outcome | |||||
| Concussion-reporting intention | .03e | ||||
| Participants, No. | 115 | 38 | 39 | 38 | |
| Time | |||||
| Baseline (95% CI) | 4.8 (4.3, 5.3) | 4.7 (3.8, 5.5) | 4.3 (3.4, 5.1) | 5.5 (4.6, 6.3) | |
| Immediate follow-up (95% CI) | 5.5 (5.0, 6.0) | 6.1 (5.2, 7.0) | 5.2 (4.3, 6.1) | 5.1 (4.2, 6.0) | |
| 1-mo follow-up (95% CI) | 5.9 (5.5, 6.4) | 6.0 (5.2, 6.8) | 5.8 (5.0, 6.6) | 6.0 (5.2, 6.8) | |
| P value across all time pointsd | <.001e | .007e | .001e | .10 | |
| Difference from baseline to immediately after education (P value) | 0.7 (.002)e | 1.5 (<.001)e | 0.9 (.05) | −0.4 (.29) | |
| Difference from baseline to 1-mo follow-up (P value) | 1.1 (<.001)e | 1.3 (.02)e | 1.5 (<.001)e | 0.6 (.15) | |
| Secondary outcomes | |||||
| Concussion knowledge | .03e | ||||
| Participants, No. | 113 | 38 | 37 | 38 | |
| Time | |||||
| Baseline (95% CI) | 0.70 (0.68, 0.72) | 0.72 (0.68, 0.75) | 0.69 (0.65, 0.72) | 0.69 (0.66, 0.73) | |
| Immediately after education (95% CI) | 0.74 (0.72, 0.77) | 0.80 (0.76, 0.84) | 0.73 (0.69, 0.77) | 0.70 (0.66, 0.74) | |
| 1-mo follow-up (95% CI) | 0.73 (0.71, 0.75) | 0.77 (0.74, 0.81) | 0.73 (0.69, 0.76) | 0.70 (0.66, 0.73) | |
| P value across all time pointsd | <.001e | .001e | .11 | .74 | |
| Difference from baseline to immediately after education (P value) | 0.04 (<.001)e | 0.08 (<.001)e | 0.04 (.08) | 0.01 (.45) | |
| Difference from baseline to 1-mo follow-up (P value) | 0.03 (.01)e | 0.05 (.04) | 0.04 (.06) | 0.00 (.84) | |
| Concussion-reporting attitudes | .03e | ||||
| Participants, No. | 114 | 38 | 38 | 38 | |
| Time | |||||
| Baseline (95% CI) | 6.5 (6.2, 6.9) | 6.5 (5.9, 7.1) | 6.3 (5.7, 6.9) | 6.7 (6.1, 7.3) | |
| Immediately after education (95% CI) | 6.8 (6.4, 7.2) | 7.3 (6.7, 8.0) | 6.0 (5.3, 6.6) | 7.0 (6.4, 7.7) | |
| 1-mo follow-up (95% CI) | 7.0 (6.6, 7.3) | 7.3 (6.7, 7.9) | 6.4 (5.8, 7.0) | 7.2 (6.6, 7.8) | |
| P value across all time pointsd | .009e | <.001e | .24 | .26 | |
| Difference from baseline to immediately after education (P value)d | 0.3 (.03) | 0.9 (<.001)e | −0.3 (.14) | 0.3 (.22) | |
| Difference from baseline to 1-mo follow-up (P value)d | 0.5 (.004)e | 0.8 (.001)e | 0.1 (.77) | 0.5 (.13) | |
| Perceived concussion-reporting norms | .15 | ||||
| Participants, No. | 115 | 38 | 39 | 38 | |
| Time | |||||
| Baseline (95% CI) | 6.5 (6.1, 6.9) | 6.2 (5.5, 6.9) | 6.3 (5.6, 7.0) | 7.0 (6.3, 7.7) | |
| Immediately after education (95% CI) | 6.4 (5.9, 6.9) | 6.8 (6.0, 7.6) | 6.1 (5.3, 6.9) | 6.3 (5.5, 7.1) | |
| 1-mo follow-up (95% CI) | 6.3 (5.9, 6.8) | 6.4 (5.6, 7.2) | 5.9 (5.1, 6.7) | 6.7 (5.9, 7.6) | |
| P value across all time pointsd | .73 | .25 | .53 | .11 | |
| Difference from baseline to immediately after education (P value)d | −0.1 (.56) | 0.5 (.05) | −0.2 (.64) | −0.7 (.04) | |
| Difference from baseline to 1-mo follow-up (P value)d | −0.2 (.42) | 0.2 (.61) | −0.4 (.24) | −0.3 (.36) | |
| Perceived behavioral control | .93 | ||||
| Participants, No. | 115 | 38 | 39 | 38 | |
| Time | |||||
| Baseline (95% CI) | 7.4 (7.0, 7.9) | 7.4 (6.6, 8.2) | 7.1 (6.3, 7.9) | 7.7 (6.9, 8.5) | |
| Immediately after education (95% CI) | 8.0 (7.5, 8.4) | 8.1 (7.3, 8.9) | 7.7 (6.9, 8.5) | 8.0 (7.2, 8.8) | |
| 1-mo follow-up (95% CI) | 8.0 (7.5, 8.4) | 8.0 (7.3, 8.8) | 7.7 (6.9, 8.4) | 8.1 (7.4, 8.9) | |
| P value across all time pointsd | .003e | .11 | .05 | .41 | |
| Difference from baseline to immediately after education (P value)d | 0.5 (.002)e | 0.7 (.05) | 0.6 (.01)e | 0.3 (.29) | |
| Difference from baseline to 1-mo follow-up (P value)d | 0.5 (.005)e | 0.6 (.03) | 0.6 (.08) | 0.40 (.27) | |
All primary and secondary outcomes, besides those related to concussion knowledge, were assessed based on athletes' responses on a 10-point Likert-type scale ranging from 1 (strongly disagree) to 10 (strongly agree) to specific questions related to that domain. A composite measure for each outcome was created by summing athletes' responses and dividing by the number of questions asked, resulting in outcomes scaled from 1 to 10.
TeachAids.
Represents the interaction term from the repeated-measures analysis of variance with 1 between-subjects factor (group) and 1 within-subject factor (time point).
Represents the results of the post hoc analysis of variance, with Bonferroni correction to account for multiple comparisons.
Indicates difference.
Figure 2.
Relationship between education type and A, intention to report concussions; B, concussion knowledge; and constructs of the theory of planned behavior including C, concussion-reporting attitudes; D, perceived concussion-reporting norms; and E, perceived behavioral control. Comparisons shown with a black line represent the post hoc analysis of variance that was different across all athletes, with Bonferroni correction to account for multiple comparisons. Comparisons shown with a red or green line represent post hoc analysis of variance that was different by education program type (Crash Course [TeachAids] or Centers for Disease Control and Prevention [CDC] video materials, respectively), with Bonferroni correction to account for multiple comparisons. a P < .001. b P < .05. c P < .01.
Figure 3.
Relationship between education type and intention to report concussions at key hypothetical time points during the season. Athletes were asked how likely they would be to report a concussion at hypothetical time points during a season including A, beginning of the season; B, practice; C, middle of the season; D, championship game; and E, end of the season. Comparisons shown with a black line represent the post hoc analysis of variance that was different across all athletes, with Bonferroni correction to account for multiple comparisons. Comparisons shown with a red or green line represent the post hoc analysis of variance that was different by education program type (Crash Course [TeachAids] or Centers for Disease Control and Prevention [CDC] video materials, respectively), with Bonferroni correction to account for multiple comparisons. a P < .001. b P < .01. c P < .05.
Concussion Knowledge
We observed improvements in concussion knowledge scores across all athletes at immediate and 1-month follow-ups (baseline = 70% correct, immediate follow-up = 74% correct, 1-month follow-up = 73% correct; F4,224 = 8.6, P < .001; Figure 2B). However, a repeated-measures ANOVA indicated differences among groups by time (F4,224 = 2.0, P = .03). Post hoc testing showed that only athletes who received CC displayed improved knowledge scores at immediate and 1-month follow-ups (CC baseline = 72% correct, immediate follow-up = 80% correct, 1-month follow-up = 77% correct; F65.6,1.7 = 8.1, P = .001; CDC-Vi baseline = 69% correct, immediate follow-up = 73% correct, 1-month follow-up = 73% correct; F2,72 = 2.3, P = .11; and CDC-Wr baseline = 69% correct, immediate follow-up = 70% correct, 1-month follow-up = 70% correct; F2,74 = 0.3, P = .74). Knowledge was not normally distributed (W112 = 0.94, P < .001).
Concussion-Reporting Attitudes
Attitudes about concussion reporting improved across all athletes (mean improvement at immediate follow-up = 2.8% and at 1-month follow-up = 4.5%; F1.9,209.5 = 4.8, P = .01; Figure 2C). However, we again noted differences in concussion-reporting attitudes among groups by time (F3.7,209.5 = 2.8, P = .03), with only the CC group demonstrating changes in concussion-reporting attitudes on post hoc analysis (CC baseline = 6.5, immediate follow-up = 7.3, 1-month follow-up = 7.3; F2,76 = 9.6, P < .001; CDC-Vi baseline = 6.3, immediate follow-up = 6.0, 1-month follow-up = 6.4; F2,74 = 1.5, P = .24; and CDC-Wr baseline = 6.7, immediate follow-up = 7.0, 1-month follow-up = 7.2; F2,74 = 1.4, P = .26). Attitudes were not normally distributed (W112 = 0.98, P = .05).
Concussion-Reporting Normative Beliefs
We observed no differences in perceived concussion-reporting norms across the total sample (F2,224 = 0.3, P = .73) or among education groups by time (F1,224 = 1.7, P = .15; Figure 2D). Although their scores were not different, athletes who received CDC-Vi reported worse perceived concussion-reporting norms both immediately after the education and at 1-month follow-up (baseline = 6.3, immediate follow-up = 6.1, 1-month follow-up = 5.9; P = .53). A similar negative relationship that was not different was evident for athletes who received CDC-Wr (baseline = 7.0, immediate follow-up = 6.3, 1-month follow-up = 6.7; P = .11). Athletes who received CC displayed improvements that were not different in perceived concussion-reporting norms (baseline = 6.2, immediate follow-up = 6.8, 1-month follow-up = 6.4; P = .25). Normative beliefs were not normally distributed (W112 = 0.91, P < .001).
Perceived Behavioral Control
All educational interventions resulted in improved perceived behavioral control related to concussion reporting (baseline = 7.4, immediate follow-up = 8.0, 1-month follow-up = 8.0; F2,216 = 5.8, P = .003; Figure 2E). No differences were present among groups (F4,216 = 0.2, P = .93). Perceived behavioral control was not normally distributed (W112, = 0.9, P < .001).
Multiple Imputation
We found no differences between participants who completed the study and those who did not based on group (P = .33), baseline intention to report concussion (P = .63), concussion knowledge (P = .58), concussion-reporting attitudes (P = .91), perceived concussion-reporting norms (P = .24), or perceived behavioral control (P = .70). Repeated-measures ANOVA from the combined imputed dataset, which incorporated data from all 144 athletes who completed the baseline assessment, demonstrated group-by-time interactions for concussion-reporting intention (P < .001), knowledge (P < .001), attitudes (P < .001), and normative beliefs (P < .001) but not for perceived behavioral control (P = .08).
DISCUSSION
In this study, we compared 3 concussion-education programs using predictors of concussion-reporting behavior informed by the TPB. The only measured TPB construct that did not change after the educational interventions was athletes' perceived concussion-reporting norms. When examining athletes across all educational interventions, we observed improvements in their intention to report concussions, knowledge about concussion, concussion-reporting attitudes, and perceived behavioral control over the decision to report concussions. All improvements were sustained at 1 month after receiving concussion education.
However, post hoc testing showed that these changes across all study participants were largely driven by the CC and CDC-Vi education programs; when examined independently, differences among education programs were notable. Students who participated in CC had improvement in the intention to report concussion at immediate and 1-month follow-ups, concussion knowledge at immediate follow-up, and concussion-reporting attitudes at immediate and 1-month follow-ups. Students who participated in CDC-Vi had improvement in the intention to report concussion at 1-month follow-up. Students who participated in CDC-Wr had no change in any of the 4 measures either at immediate or 1-month follow-ups, which is in line with reports of previous researchers18,19 who evaluated these materials.
The findings related to concussion-reporting intention are particularly valuable given its relationship to true concussion reporting.14 Although concussion-reporting intention is most closely related to reporting behavior, intentions are thought to explain only 20% of the variance in reporting behavior.14 Nonetheless, even a small improvement in concussion reporting would yield important benefits considering the millions of annual concussions sustained in sports.1 The statistically significant findings may also reflect clinically meaningful differences in outcomes, given the high incidence of concussions, the sequelae of these injuries, and the estimated 50% of concussions that remain unreported and thus undiagnosed.1,2,5,6
Other comparative differences, such as athletes' greater improvement in concussion knowledge and concussion-reporting attitudes after CC compared with other interventions, persisted at 1-month follow-up. These factors are clinically relevant because of their previously demonstrated link to concussion reporting.14–16
Several explanations are possible for the differences in outcomes among interventions. One explanation may reside in the development process of CC. Specifically, CC was developed iteratively with regular feedback and evaluation by hundreds of stakeholders, including athletes, coaches, athletic trainers, educators, scientists, and physicians. It was created to target the interpersonal, team-based, and societal pressures that result in concussion underreporting,15,21 and the messaging was modified based on athlete feedback to ensure it “spoke the same language” as the target audience to potentially improve perceived validity. The use of a near-peer educator or guide may also result in greater perceived messenger validity.9 However, collegiate athletes may not represent true peers for high school athletes. In addition, the interactive scenario and game-based decision-tree algorithm may increase athletes' information retention due to increased engagement with the material.27
This increased engagement potential may be key to further influencing perceived normative behavior.18,19,27 An education program that encourages organic conversations and sharing via multiple communicative platforms will be well suited to facilitating recurring conversations among athletes, ultimately leading to changing athletes' perceptions of their peers' views and, thus, increasing the likelihood of behavioral change.12
These relative differences among education programs in concussion-reporting intention and related outcomes should not detract from the overall message of the value of concussion-education programs, which are based on multiple studies15,28 indicating that athletes with concussion education were more likely to report suspected concussions. Given the risks and potential long-term sequelae of undiagnosed concussions, athletes must receive concussion education. It is troubling that, despite the passage of legislation to address concussions across all 50 states, nearly 25% of collegiate athletes reported not having received concussion education.29 These deficiencies in the dissemination of concussion education must be addressed to ensure athlete safety.
Athletes across all educational groups improved in their perceived behavioral control over concussion reporting, with no differences observed among education types. Although the education programs provided athletes with resources to consult during the concussion-reporting decision process to varying degrees, none of the programs explicitly target these concussion-reporting skills. Concussion-reporting skill, therefore, represents a potential avenue for further improving perceived behavioral control and would likely result in additional gains in concussion reporting given the data linking it to concussion-reporting intention.30
We found no changes in athletes' perceived concussion-reporting norms after any study intervention. Although perceived norms are an important factor in athletes' concussion reporting, it is perhaps unsurprising that no improvements occurred across the 3 interventions. Perceived norms are based on athletes' comparative experiences with the attitudes and behaviors of those around them, including coaches and teammates.12 Although the interventions were informative, they did not directly engage teammates and coaches in discussion. A single time-point education program may not be sufficient to change perceived norms. However, concussion education can potentially be modified to encourage using direct discussions between athletes and coaches as part of a broader learning environment on concussion.
Post hoc testing did not show any improvement in concussion-reporting intention or secondary measures for athletes who received CDC-Wr. Despite randomization, the athletes who participated in CDC-Wr had higher baseline scores that were not different on concussion-reporting intention, attitudes, perceived norms, or perceived behavioral control. It is possible that ceiling effects minimized the observed gains for these athletes; yet athletes who participated in CDC-Wr had lower scores for all of these measures immediately after education than did the athletes who participated in CC. It is also possible that written education is less effective than video education or that passive education is less effective than active education.
Our study had several limitations. First, the primary outcome measure was concussion-reporting intention, an appropriate but indirect measure of concussion reporting. We investigated male high school football players, and the results cannot be generalized beyond that context. Participants were randomized within teams, so there may have been contamination effects at follow-up; however, this limitation would have biased differences among education types toward the null. Educational materials were provided at only 1 time point. Effective, long-term behavioral change may be best targeted using sustained, repeated messaging that engenders ongoing discussions. The sample was small; this again would have biased the results toward the null. Demographic information was collected from participants at the 1-month follow-up; therefore, the characteristics of individuals who did not complete the study cannot be compared with the characteristics of those who did. These analyses would have been of specific value given the greater loss to follow-up in the CDC-Wr cohort. Nonetheless, the analyses of those who completed the study and those who did not, as well as the analysis of data from multiple imputation, were consistent with the reported findings. Finally, the clinical importance of the effects reported was unclear.
CONCLUSIONS
Undiagnosed concussions result in an increased risk of future concussion and prolonged recovery. Prompt concussion reporting is important for the proper management of these injuries. Understanding the effect of concussion-education interventions is critical for enhancing concussion decision making. This study represents one of the first randomized evaluations of concussion-education programs. All athletes exhibited improved concussion-reporting intentions, increased concussion knowledge, better concussion attitudes, and increased perceived behavioral control at both immediate and 1-month follow-ups. When examined independently, athletes who received CDC-Wr materials did not improve on any measure. Furthermore, athletes who participated in CC had higher scores on intention to report concussion at the immediate and 1-month follow-ups, more knowledge at the immediate and 1-month follow-ups, and improved concussion-reporting attitudes at the immediate and 1-month follow-ups. Athletes participating in CDC-Vi had higher scores only for intent to report concussion and only at the 1-month follow-up.
ACKNOWLEDGMENTS
This study was funded by the Taube Stanford Concussion Collaborative with Lucile Packard Children's Hospital Stanford. The funding agency was not involved in study oversight, data acquisition, data analysis, or reporting. We thank Coach Dick Gould for his fearless leadership and determination to bring concussion education to the global sports community. We also thank the research team who made this study possible: Noura Bou Zeid, Ryan Burns, Hannah D'Apice, Krishna Teja Gorrepati, Cara Hanelin, Anafia Thomas, and Jennifer Wiener.
REFERENCES
- 1.Daneshvar DH, Nowinski CJ, McKee AC, Cantu RC. The epidemiology of sport-related concussion. Clin Sports Med . 2011;30(1):1–17. doi: 10.1016/j.csm.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daneshvar DH, Riley DO, Nowinski CJ, McKee AC, Stern RA, Cantu RC. Long-term consequences: effects on normal development profile after concussion. Phys Med Rehabil Clin N Am . 2011;22(4):683–700. doi: 10.1016/j.pmr.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howell DR, Kriz P, Mannix RC, Kirchberg T, Master CL, Meehan WP. Concussion symptom profiles among child, adolescent, and young adult athletes. Clin J Sport Med . 2019;29(5):391–397. doi: 10.1097/JSM.0000000000000629. [DOI] [PubMed] [Google Scholar]
- 4.Giza CC, Difiori JP. Pathophysiology of sports-related concussion: an update on basic science and translational research. Sports Health . 2011;3(1):46–51. doi: 10.1177/1941738110391732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med . 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Baugh CM, Kiernan PT, Kroshus E, et al. Frequency of head-impact–related outcomes by position in NCAA Division I collegiate football players. J Neurotrauma . 2015;32(5):314–326. doi: 10.1089/neu.2014.3582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esterov D, Lennon RJ, Bergquist T, Brown A. Predictors of neurobehavioral symptom reporting in a community based sample with mild traumatic brain injury. NeuroRehabilitation . 2020;47(1):65–77. doi: 10.3233/NRE-203082. [DOI] [PubMed] [Google Scholar]
- 8.Bookbinder HA, Houston MN, Peck KY, et al. Factors associated with delayed concussion reporting by United States service academy cadets. J Athl Train . 2020;55(8):843–849. doi: 10.4085/1062-6050-362-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Register-Mihalik JK, Marshall SW, Kay MC, et al. Perceived social norms and concussion-disclosure behaviours among first-year NCAA student-athletes: implications for concussion prevention and education. Res Sports Med . 2021;29(1):1–11. doi: 10.1080/15438627.2020.1719493. [DOI] [PubMed] [Google Scholar]
- 10.Houston MN, Bay RC, Valovich McLeod TC. The relationship between post-injury measures of cognition, balance, symptom reports and health-related quality-of-life in adolescent athletes with concussion. Brain Inj . 2016;30(7):891–898. doi: 10.3109/02699052.2016.1146960. [DOI] [PubMed] [Google Scholar]
- 11.Kroshus E, Baugh CM. Concussion education in US collegiate sport: what is happening and what do athletes want? Health Educ Behav . 2016;43(2):182–190. doi: 10.1177/1090198115599380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kroshus E, Chrisman SPD. A new game plan for concussion education. Health Educ Behav . 2019;46(6):916–921. doi: 10.1177/1090198119859414. [DOI] [PubMed] [Google Scholar]
- 13.Hickling A, Mallory KD, Wilson KE, et al. The youth concussion awareness network (You-CAN) – a school-based peer-led intervention to improve concussion reporting and social support: the protocol for a cluster randomized trial. BMC Public Health . 2020;20(1):186. doi: 10.1186/s12889-020-8244-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroshus E, Baugh CM, Daneshvar DH, Nowinski CJ, Cantu RC. Concussion reporting intention: a valuable metric for predicting reporting behavior and evaluating concussion education. Clin J Sport Med . 2015;25(3):243–247. doi: 10.1097/JSM.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 15.Register-Mihalik JK, Linnan LA, Marshall SW, Valovich McLeod TC, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes' intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj . 2013;27(7–8):878–886. doi: 10.3109/02699052.2013.775508. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan L, Pursell L, Molcho M. Evaluation of a theory-based concussion education program for secondary school student-athletes in Ireland. Health Educ Res . 2018;33(6):492–504. doi: 10.1093/her/cyy034. [DOI] [PubMed] [Google Scholar]
- 17.Kroshus E, Baugh CM, Daneshvar DH, Viswanath K. Understanding concussion reporting using a model based on the theory of planned behavior. J Adolesc Health . 2014;54(3):269–274.e2. doi: 10.1016/j.jadohealth.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Kroshus E, Baugh CM, Hawrilenko M, Daneshvar DH. Pilot randomized evaluation of publically available concussion education materials: evidence of a possible negative effect. Health Educ Behav . 2015;42(2):153–162. doi: 10.1177/1090198114543011. [DOI] [PubMed] [Google Scholar]
- 19.Kroshus E, Daneshvar DH, Baugh CM, Nowinski CJ, Cantu RC. NCAA concussion education in ice hockey: an ineffective mandate. Br J Sports Med . 2014;48(2):135–140. doi: 10.1136/bjsports-2013-092498. [DOI] [PubMed] [Google Scholar]
- 20.Register-Mihalik JK, Cameron KL, Kay MC, et al. Determinants of intention to disclose concussion symptoms in a population of US military cadets. J Sci Med Sport . 2019;22(5):509–515. doi: 10.1016/j.jsams.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Caron JG, Bloom GA, Falcão WR, Sweet SN. An examination of concussion education programmes: a scoping review methodology. Inj Prev . 2015;21(5):301–308. doi: 10.1136/injuryprev-2014-041479. [DOI] [PubMed] [Google Scholar]
- 22.Piana LE, Garvey KD, Kroshus E, Brook EM, Matzkin EG. Implementation and effect of concussion education in collegiate women's ice hockey. Phys Sportsmed . 2020;48(1):46–52. doi: 10.1080/00913847.2019.1624657. [DOI] [PubMed] [Google Scholar]
- 23.Taylor ME, Sanner JE. The relationship between concussion knowledge and the high school athlete's intention to report traumatic brain injury symptoms: a systematic review of the literature. J Sch Nurs . 2017;33(1):73–81. doi: 10.1177/1059840515619683. [DOI] [PubMed] [Google Scholar]
- 24.CrashCourse free products. TeachAids Web site. 2020. Accessed June 27. https://teachaids.org/for-concussions/products .
- 25.HEADS UP to school sports. Centers for Disease Control and Prevention Web site. 2019. Published March 5. Accessed December 1, 2020. https://www.cdc.gov/headsup/highschoolsports/index.html .
- 26.Rosenbaum AM, Arnett PA. The development of a survey to examine knowledge about and attitudes toward concussion in high-school students. J Clin Exp Neuropsychol . 2010;32(1):44–55. doi: 10.1080/13803390902806535. [DOI] [PubMed] [Google Scholar]
- 27.Kolberg K, Larson J, Almeida A, et al. The feasibility of using comic-based concussion discharge instructions: gauging likeability and knowledge improvement among adolescents and parents. Pediatr Emerg Care . 2020. Published online June 11. [DOI] [PubMed]
- 28.Bramley H, Patrick K, Lehman E, Silvis M. High school soccer players with concussion education are more likely to notify their coach of a suspected concussion. Clin Pediatr (Phila) . 2012;51(4):332–336. doi: 10.1177/0009922811425233. [DOI] [PubMed] [Google Scholar]
- 29.Carroll-Alfano M. Mandated high school concussion education and collegiate athletes' understanding of concussion. J Athl Train . 2017;52(7):689–697. doi: 10.4085/1062-6050-52.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warmath D, Winterstein AP. Reporting skill: the missing ingredient in concussion reporting intention assessment. Sports Health . 2019;11(5):416–424. doi: 10.1177/1941738119856609. [DOI] [PMC free article] [PubMed] [Google Scholar]