Abstract
Nursing is considered to be an at-risk profession of burnout due to daily exposure to difficult situations such as death and pain care. In addition, some units such as the intensive care unit (ICU), can be stressful due to high levels of morbidity and mortality and ethical dilemmas. Burnout causes a deterioration in quality of care, increasing the risk of mortality in patients due to poor performance and errors in the healthcare environment. The aim of this study was to analyse the levels, prevalence and related factors of burnout in ICU nurses. A systematic review and meta-analysis were carried out in the Medline, Scopus and CINAHL databases. Fifteen articles were found for the systematic review and four for the meta-analysis. With a sample of n = 1986 nurses, the meta-analytic estimate prevalence for high emotional exhaustion was 31% (95% CI, 8–59%), for high depersonalization was 18% (95% CI, 8–30%), and for low personal accomplishment was 46% (95% CI, 20–74%). Within the dimensions of burnout, emotional exhaustion had a significant relationship with depression and personality factors. Both sociodemographic factors (being younger, single marital status, and having less professional experience in ICU) and working conditions (workload and working longer hours) influence the risk of burnout syndrome.
Keywords: burnout, nurses, occupational health, risk factors, stress, intensive care unit
1. Introduction
In 1974, the American psychiatrist Freudenberger referred to burnout as a state of fatigue or frustration that appears after dedication to a cause, lifestyle, or relationship in which the expected effort is not produced [1]. Burnout appears as a negative response caused after chronic work episodes of stress. Professionals with this syndrome perceive it as a constant imbalance between their needs, their values and the work they do [2].
This phenomenon has three main components: emotional exhaustion (EE) or gradual loss of energy, exhaustion, tiredness and fatigue, which is externalized in a physical or psychological way, or both; depersonalization (D) or negative behaviours along with indifferent responses towards those who receive care or treatment; and low personal accomplishment (PA) that consists of being limited and not feeling fulfilled with the work performed [2]. There are also other burnout measurement tools such as Copenhagen Burnout Inventory [3].
In 2001, Maslach et al. [4] developed a validated instrument, the Maslach Burnout Inventory (MBI), to measure burnout syndrome. It consists of a questionnaire that evaluates the three components described (EE, D, and PA) through 22 items using a 7-point Likert-type scale (where 0 is never and 6 is every day). A high score in EE and D, and a low level in PA indicate the presence of burnout, and it can be classified into different levels as it is an ordinal variable: low, medium and high [4].
Burnout is related to physical disorders such as respiratory, heart, and intestinal pathology, headaches, type 2 diabetes, hypercholesterolemia, prolonged fatigue, and muscle pain [5]. Burnout has also a negative effect on mental health causing depressive and anxiety symptoms, alcohol consumption, insomnia, and even suicidal ideas [6,7]. In addition, burnout syndrome can cause absenteeism and job dissatisfaction [8,9].
Nursing is considered to be a risk profession due to daily exposure to difficult situations such as death and pain care [10]. In particular, intensive care units (ICU) can be stressful due to high levels of mortality, critical medical condition, and ethical dilemmas [11]. This situation can increase when the staff does not require enough time to provide adequate care for each patient [12].
The chronicity of burnout syndrome can lead to provoke deep emotional reactions, that without intervention or guidance aimed at its prevention, can cause damage to the physical and psychological integrity of the health professional [10]. Burnout can also tend to cause a deterioration in the quality of care, increasing the risk of morbidity and mortality in patients, due to poor performance and increased errors in the healthcare environment [13]. In this sense, it is interesting to carry out a review about burnout in ICUs. This syndrome has been classified as an occupational phenomenon; thus, its prevention through the implementation of coping strategies is essential [12].
The objective of this study was to analyse the levels, prevalence, and related factors of burnout in intensive care nurses.
2. Materials and Methods
2.1. Design and Search Strategy
A systematic review with meta-analysis was performed following the PRISMA recommendations (Preferred Reporting Items for Systematic Reviews and Meta-analyses) [14]. The search was carried out through the databases Medline (PubMed), Scopus (Elsevier), and CINAHL (EBSCO). Using the MeSH terms the search strategy was “burnout AND nurses AND intensive care units”. The search was conducted in December 2020.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria were: (1) primary quantitative studies that measured burnout and its risk factors; (2) sample of nurses of intensive care unit nurses; (3) data of level; prevalence; or related factors; (4) published in English and Spanish language; (5) published in the last five years; (6) studies using the Maslach Burnout Inventory (MBI) were included in the meta-analysis. The exclusion criteria were: (1) systematic or bibliographic reviews; (2) studies carried out in paediatric or neonatal intensive care units; (3) studies that included different health professions without specific data for nurses.
2.3. Study Selection, Quality Appraisal, and Risk of Bias
For the selection of the studies, first, a screening was carried out based on the duplicate studies. In the article selection process, two of the authors (S.R.-E. and N.S.-M) independently reviewed the title and abstract of the articles found. Finally, the full text was read. A third author (J.L.R.-B) was consulted in case of disagreement.
The quality of the articles selected for this review was evaluated using the levels of evidence and grades of recommendation stipulated by the Oxford Centre for Evidence- Based Medicine (OCEBM) [15]. Table 1.
Table 1.
Characteristics of the included studies (n = 15).
| Author, Year, (Country) | Study Design | Sample | Burnout Prevalence | Main Results | OCEBM * LE/GR |
|
|---|---|---|---|---|---|---|
| Arrogante & Aparicio, 2017 (Spain) [16] | Cross-sectional study | n = 30 ICU nurses | Levels of emotional exhaustion and depersonalization were medium and personal accomplishment level was high | Emotional exhaustion and depersonalization were negatively related to mental health, resiliency, and physical health Personal accomplishment was positively related to mental health and resiliency |
2c/B | |
| Cañadas-De la Fuente et al., 2016 (Spain) [17] | Cross-sectional study | n = 1225 ICU nurses | 44.1% were in the highest levels of the syndrome | Nurses with extra shifts were more prone to high levels of emotional exhaustion, depersonalization, and low personal accomplishment | 2c/B | |
| Cañadas-de la Fuente et al., 2018 (Spain) [18] | Cross-sectional study | n = 337 ICU nurses | High Emotional Exhaustion 11% High Depersonalization 17% Low personal accomplishment 63.3% |
Personality factors and depression were related with high levels of burnout Emotional exhaustion was statistically related to neuroticism, amiability, responsibility, extraversion and with anxiety and depression Depersonalization and personal accomplishment were related to the five personality factors and with anxiety and depression High Burnout level was associated with neuroticism and amiability |
2c/B | |
| Da Silva et al., 2017 (Brazil) [19] | Cross-sectional study | n = 130 ICU nurses | Burnout prevalence 55.3% | - | 2c/B | |
| Denat et al., 2016 (Turkey) [20] | Cross-sectional study | n = 51 ICU nurses | Nurses showed low levels of emotional exhaustion, low depersonalization, and medium personal accomplishment | There was no relationship between burnout and ventricular extrasystoles or atrial extrasystoles | 2c/B | |
| Filho et al., 2019 (Brazil) [21] | Cross-sectional study | n = 209 ICU nurses | High emotional exhaustion 29.4% High depersonalization 22% Low personal accomplishment 52.9% |
Each patient added to nurses workload was associated with a 67% and 37% increase in the probability of emotional exhaustion and low personal accomplishment Each year working at the ICU was associated with a 7% higher probability of low personal accomplishment |
2c/B | |
| Galleta et al., 2016 (Italy) [22] | Cross-sectional study | n = 101 ICU nurses | 53% emotional exhaustion and 61.5% medium or high levels of depersonalization | Burnout was related with psychosocial aspects and with hospital rate infection | 2c/B | |
| Hu et al., 2021 (China) [23] | Cross-sectional study | n = 1315 ICU nurses | High Emotional Exhaustion 56.6% High Depersonalization 30% Low Personal accomplishment 20% |
Professionals working in ICU were more prone to burnout. The associated factors were low frequency of physical exercise, having comorbidities, working in a high-quality hospital, having more years of professional experience, night shifts, and having fewer holidays | 2c/B | |
| Kim & Yeom, 2018 (South Korea) [24] | Cross-sectional study | n = 318 ICU nurses | Burnout levels was 3.15 in a scale to 5 | Higher burnout levels were significantly associated with being younger, unmarried, having a lower education level, lower professional experience, and having no religion Higher levels of spiritual well-being were related with lower burnout |
2c/B | |
| Miranda Alvares et al., 2020 (Brazil) [25] | Cross-sectional study | n = 125 ICU nurses | High Emotional Exhaustion 30% High Depersonalization 6% Low personal accomplishment 53% Burnout prevalence was 0.41% following Maslach criteria |
Being 35 years old or more showed a lower probability of emotional exhaustion and depersonalization More working hours were related to lower personal accomplishment Men had lower personal accomplishment Less physical activity was related to higher emotional exhaustion and depersonalization |
2c/B | |
| Ntantana et al., 2017 (Greece) [26] | Cross-sectional study | n = 493 ICU nurses | Burnout was present in 2.6% Exhaustion was higher in nurses than physicians |
Neuroticism was positively related to exhaustion and extraversion was negatively related to exhaustion. Personality factors, labour satisfaction, and end-of-life care are related to burnout |
2c/B | |
| Padilla Fortunatti & Palmeiro Silva 2017 (Chile) [27] | Cross-sectional study | n = 36 ICU nurses. | - | Emotional exhaustion was negatively related to age and positively related to an imbalance between effort-reward; depersonalization was negatively related to age | 2c/B | |
| Saravanabavan et al., 2019 (India) [28] | Cross-sectional study | n= 164 ICU nurses | 69% nurses had burnout | Laboral satisfaction was significantly correlated with Burnout; stress levels were correlated with emotional exhaustion and depersonalization | 2c/B | |
| Sok et al., 2020 (South Korea) [29] | Cross-sectional study | n =115 ICU nurses | The mean score of burnout was 64.03 in the Copenhagen Burnout Inventory, indicating a high level | Burnout had a significant and positive relationship with depression and job stress and a negative significant relation with age | 2c/B | |
| Vasconcelos et al., 2018 (Brazil) [30] | Cross-sectional study | n = 91 ICU nurses | 14.3% showed burnout | Higher levels of depression were correlated with higher levels of emotional exhaustion and depersonalization and with lower levels of personal accomplishment | 2c/B |
*—levels of evidence of the Oxford Centre for Evidence-Based Medicine; LE, level of evidence; GR, grade of recommendation.
2.4. Data Abstraction
Two authors (S.R.-E. and N.S.-M.) collected data from each selected study. A third author verified the data in case of disagreement (L.-A.-G.). The following collected as data were obtained for each included article: year of publication, country of study, type of study, sample size, and main results.
For the systematic review, a descriptive analysis of the data included in the studies was performed. StatsDirect software for Windows was used for the meta-analysis. A random effects meta-analysis of the prevalence of high EE, high D, and low PA was performed with the data from the total study sample and the prevalence of burnout syndrome. Heterogeneity was analysed with the I2 test, publication bias with the Egger test, and a sensitivity analysis was performed.
3. Results
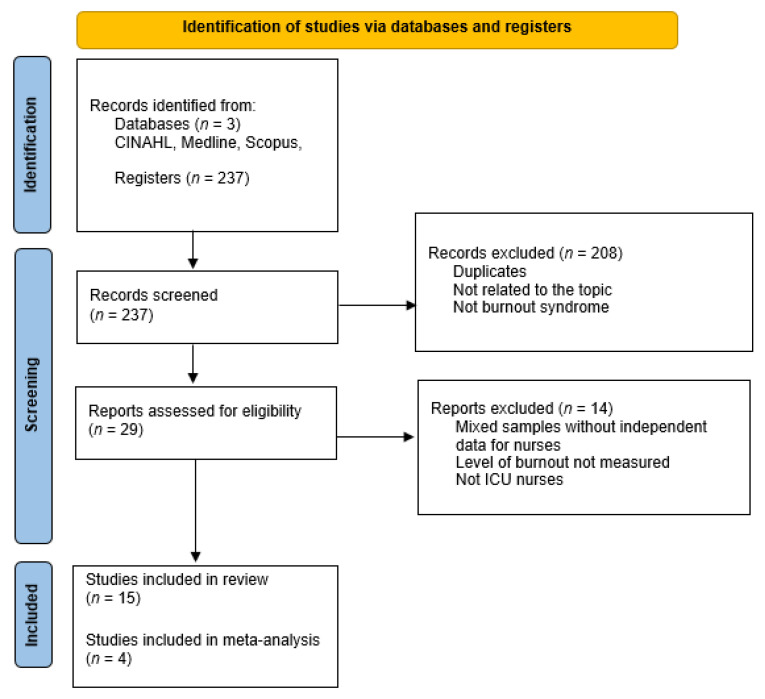
In total, 237 articles were found. After screening by title and abstract and reading the full text, a total of 15 studies were included for the systematic review.
The selection process of included studies is shown in Figure 1. Most of the studies selected for this review were conducted in Brazil (n = 4), Spain (n = 3), and South Korea (n = 2), with the remainder conducted in Turkey, China, Greece, Chili, Italy, and India. The detailed information of each study is shown in Table 1.
Figure 1.
Flow diagram of the publication search process.
3.1. Prevalence of Burnout Syndrome
In the articles selected, there were several instruments to measure burnout syndrome. Among them, there was high use of MBI in 87.5% of studies. The prevalence of burnout varies depending on the country where the research was carried out. Two studies carried out in Brazil showed disparate results, in one low level of burnout, in all its dimensions [25], and in the other, a high prevalence of burnout [19]. In another study carried out in India, most of the participants obtained a high level in the three dimensions established by the Maslach questionnaire [28]. Burnout levels of each article are shown in Table 1.
3.2. Socio-Demographic Factors
Sociodemographic factors such as being younger, single marital status, and having less professional experience in the intensive care unit (ICU were associated with burnout levels [24,25,27,29]. Age was negatively correlated with EE, and the effort–reward imbalance was positively correlated with EE [27]. For nursing professionals, for each year of work that they spent in the ICU, there was an increase in the levels of low PA [21]. Other related factors of burnout were a lack of time for physical exercise, work in a high-quality hospital, the presence of comorbidities, and years of experience [18].
3.3. Personality Related Factors
A high EE score was significantly related to depression and personality factors [18,29,30]. Some authors showed that EE was significantly related to four personality factors, neuroticism, agreeableness, responsibility, and extraversion. Likewise, the D and PA were related to these same factors by adding openness [18].
Neuroticism was a positive predictor of EE [18,26] and extraversion was a negative predictor [26]. Conversely, EE was interrelated with depression, job stress, and job satisfaction within intensive care nursing staff [29]. Depressive symptoms are more likely to appear in nurses who work in the ICU and who have a high level of burnout [26,30].
3.4. Occupational Related Factors
Regarding working hours among nurses who perform complementary physical days, 15.3% presented high levels of EE, 17.9% high D, and 65.9% low PA. The percentages of those who did not perform complementary physical work were 10.8%, 11.8%, and 61%, respectively. These data reflect that high work overload was related to high levels of EE and D [17]. In the same way, high EE and low PA were associated with an increase in the workload, reflected in a greater number of patients [21].
3.5. Other Outcomes of Interest
Some authors analysed resilience as a way of adapting to adverse situations. Resilience was negatively related to D and positively to PA. A higher level of resilience was related to an improvement in nurse mental health, as well as the willingness to work effectively [16].
Other studies also studied the relation of burnout with the infection rate in ICU [22], or the prevalence between ventricular and atrial extra systoles in ICU nurses [20], although the results showed no relationship.
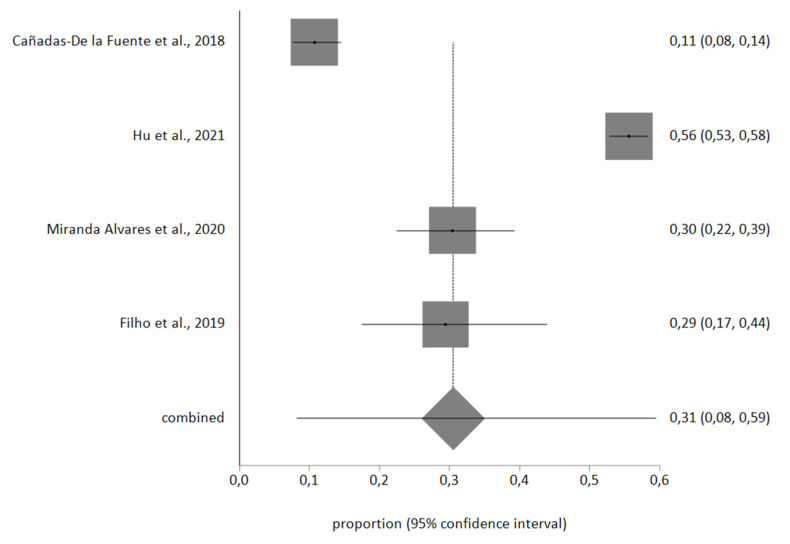
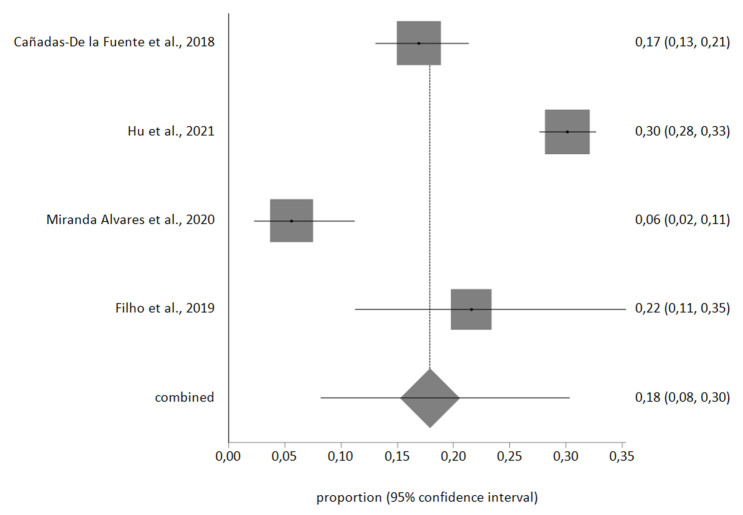
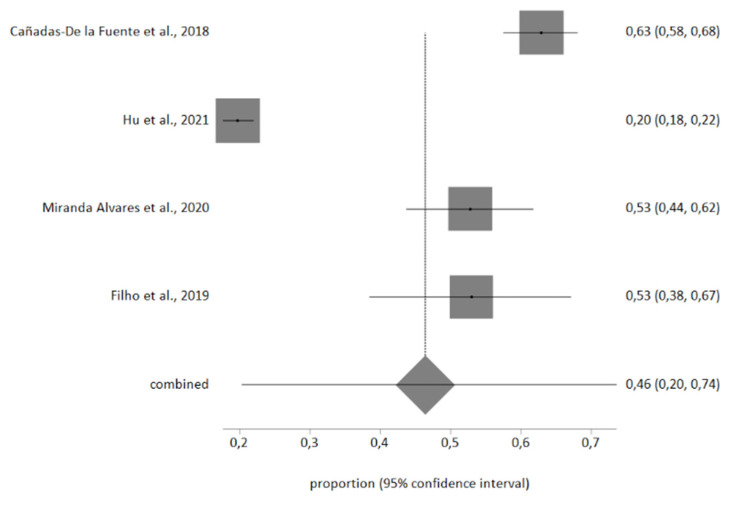
3.6. Meta-Analysis of the Prevalence of High EE, High D and Low PA
Four studies included the information necessary for the meta-analysis, with a total sample of n = 1986 nurses. Egger’s test showed no publication bias, and no studies were excluded after sensitivity analysis. Heterogeneity in the three meta-analyses performed was high, therefore a random-effects meta-analysis was used.
The meta-analytic estimate prevalence for high EE was 31% (95% CI, 8–59%), for high D was 18% (95% CI, 8–30%), and finally for low PA was 46% (95% CI, 20–74%). The forest plots are shown in Figure 2, Figure 3 and Figure 4.
Figure 2.
High EE forest plot.
Figure 3.
High D forest plot.
Figure 4.
Low PA forest plot.
4. Discussion
The prevalence of burnout in the included studies differs between countries and health systems where the studies were performed. Similarly, in other reviews carried out in other nursing areas, there were similar differences [31,32,33], although, these data are inferior to nurses from other services, such as mental health, paediatrics, oncology or primary care [34,35,36,37]. Given that the health system of each country has different characteristics, competencies in the nursing area, training programs, workload, and costs of care, the levels of burnout can be diverse [38,39].
As demographic factors, we found work overload, seniority, and age as main factors related to burnout syndrome in ICU nurses. As corroborated by other studies, the excessive number of daily working hours and a high workload, in addition to a lack of time for patient care, produced emotional disorders and low job satisfaction [40,41]. In critical care service, the emotional and physical domains are overloaded due to the complex labour interventions carried out by nursing staff [42,43]. Other authors highlight that high levels of EE were related to personal factors such as being single and caring for children, as well as work factors such as long working days, poor quality work life, and a lack of time to dedicate to self-care [44]. In relation to the experience, some studies indicated that older professionals with a permanent job showed a high EE related to the daily routine within the workplace, stress, and high workload [45]. An adequate work environment, with good working relationships [46] and support by the institution [47], were found as protective factors. Other authors also found that an improvement in salary [48] leads to improved motivation [49]; as a consequence, job satisfaction increases, and professionals are less prone to suffer burnout syndrome [50].
In relation to the psychological factors, ICU nurses with high levels of anxiety and depression have shown high levels of burnout. Work practice is faced with an exhausting and unfavourable work environment that deteriorates the professional’s quality of life, adding a lack of interest and frustration that provokes leaving the job [51]. Thus, it is essential to provide interventions to improve mental health and promote coping strategies [52,53].
The study had some limitations. The number of articles included in the meta-analysis was low. The heterogeneity (I2 index) was high because population samples of included studies were analysed in different countries with diverse healthcare systems. The results also reflected the working conditions of each geographical area, an important aspect for its subsequent interpretation. Another limitation was that not all studies used the same measurement questionnaire; therefore, it was not possible to combine all the results, the meta-analytic estimate of the prevalence measured only with MBI was analysed.
5. Conclusions
ICU nurses tend to have high emotional exhaustion and low personal accomplishment. The main sociodemographic factors related to burnout syndrome were being younger, single marital status, and having less professional experience in the ICU, and the work-related factors were workload and working longer hours. Emotional exhaustion had a significant relationship with depression and personality factors. The work environment had a great influence on reducing the prevalence of burnout; therefore, support and job satisfaction, as well as an improvement in the worker’s self-esteem, can be protective factors. Health policy should develop interventions and training to improve working conditions, the environment, and coping skills in order to improve the quality of patients and professionals care.
Author Contributions
Conceptualization, N.S.-M. and G.A.C.-D.l.F.; methodology, J.L.G.-U. and G.A.C.-D.l.F.; software, J.L.G.-U. and J.L.R.-B.; validation, N.S.-M., C.M.-R. and J.L.G.-U.; formal analysis, J.L.R.-B., J.L.G.-U. and L.A.-G.; investigation, S.R.-E., N.S.-M. and J.L.R.-B.; resources, S.R.-E. and C.M.-R.; data curation, S.R.-E., N.S.-M. and J.L.R.-B.; writing—original draft preparation, S.R.-E. and N.S.-M.; writing—review and editing, S.R.-E., J.L.R.-B. and N.S.-M.; visualization, J.L.G.-U. and G.A.C.-D.l.F.; supervision, G.A.C.-D.l.F. and L.A.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Freudenberger H.J. Staff burn-out. J. Soc. Issues. 1974;30:159–165. doi: 10.1111/j.1540-4560.1974.tb00706.x. [DOI] [Google Scholar]
- 2.Maslach C., Jackson S., Leiter M. The Maslach Burnout Inventory: Manual. Consulting Psychologist Press; Palo Alto, CA, USA: 1996. [Google Scholar]
- 3.Borritz M., Kristensen T. Copenhagen Burnout Inventory. National Institute of Occupational Health; Copenhagen, Denmark: 1999. [Google Scholar]
- 4.Maslach C., Schaufeli W., Leiter M. Job burnout. Annu. Rev. Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 5.Salvagioni D.A.J., Melanda F.N., Mesas A., González A., Gabani F.L., De Andrade S.M. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLoS ONE. 2017;12:e0185781. doi: 10.1371/journal.pone.0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schulz M., Damkröger A., Voltmer E., Löwe B., Driessen M., Ward M., Wingenfeld K. Work-related behaviour and expe-rience pattern in nurses: Impact on physical and mental health. J. Psychiatr. Ment. Health Nurs. 2011;18:411–417. doi: 10.1111/j.1365-2850.2011.01691.x. [DOI] [PubMed] [Google Scholar]
- 7.Bakhamis L., Paul D.P., Smith H., Coustasse A. Still an Epidemic: The Burnout Syndrome in Hospital Registered Nurses. Health Care Manag. 2019;38:3–10. doi: 10.1097/HCM.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 8.Geuens N., Leemans A., Bogaerts A., Van Bogaert P., Franck E. Interpersonal behaviour in relation to burnout. Nurs. Manag. 2015;22:26–32. doi: 10.7748/nm.22.8.26.s27. [DOI] [PubMed] [Google Scholar]
- 9.Meeusen V., Van Dam K., Brown-Mahoney C., Van Zundert A., Knape H. Burnout, psychosomatic symptoms and job satisfaction among Dutch nurse anaesthetists: A survey. Acta Anaesthesiol. Scand. 2010;54:616–621. doi: 10.1111/j.1399-6576.2010.02213.x. [DOI] [PubMed] [Google Scholar]
- 10.Tobajas D., Celia M., Ortiz J., Martínez G., Gavilán S. Enfermería Global Study on anxiety in intensive care nursing pro-fessionals facing the process of death. Enfermería Glob. 2017;45:265. [Google Scholar]
- 11.Oliveira E.G., Garcia P.C., Filho C.M.C., Nogueira L.D.S. The influence of delayed admission to intensive care unit on mortality and nursing workload: A cohort study. Nurs. Crit. Care. 2018;24:381–386. doi: 10.1111/nicc.12402. [DOI] [PubMed] [Google Scholar]
- 12.Moss M., Good V., Gozal D., Kleinpell R., Sessler C. An Official Critical Care Societies Collaborative Statement: Burnout Syndrome in Critical Care Healthcare Professionals: A Call for Action. Crit. Care Med. 2016;44:1414–1421. doi: 10.1097/CCM.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 13.Hall L.H., Johnson J., Watt I., Tsipa A., O’Connor D.B. Healthcare staff wellbeing, burnout, and patient safety: A systematic review. PLoS ONE. 2016;11:e0159015. doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howick J., Chalmers I., Glasziou P., Greenhalg T., Heneghan C., Liberati A., Moschetti I., Phillips B., Thornton H. The Oxford 2011 Levels of Evidence. [(accessed on 10 May 2020)]. Available online: https://www.cebm.net/2016/05/ocebm-levels-of-evidence.
- 16.Arrogante O., Aparicio-Zaldivar E. Burnout and health among critical care professionals: The mediational role of resilience. Intensive Crit. Care Nurs. 2017;42:110–115. doi: 10.1016/j.iccn.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Cañadas-De la Fuente G.A., Albendín-García L., de la Fuente E., San Luis C., Gómez-Urquiza J.L., Cañadas G. Burnout in Nursing Professionals Performing Overtime Workdays in Emergency and Critical Care Departments. Rev. Esp. Salud. Publica. 2016;90:e1-9. [PubMed] [Google Scholar]
- 18.Cañadas-de la Fuente G.A., Albendín-García L., Cañadas G., San Luis-Costas C., Ortega-Campos E., de la Fuente-Solana E. Nurse burnout in critical care units and emergency departments: Intensity and associated factors. Emergencias. 2018;30:328–331. [PubMed] [Google Scholar]
- 19.Da Silva J., Reis Texeira L., dos Santos Costa F., Dos Santos Aranha J., Rangel Texeira E. Job strain and psychosocial as-pects of intensive care nurses. Enfermería Glob. 2017;48:108–120. [Google Scholar]
- 20.Denat Y., Gökçe S., Gungor H., Zencir C., Akgüllü C. Relationship of Anxiety and Burnout with Extrasystoles in Critical Care Nurses in Turkey. Pak. J. Med. Sci. 1969;32:196–200. doi: 10.12669/pjms.321.8407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Filho F., Rodrigues M., Cimiotti J. Burnout in Brazilian Intensive Care Units: A Comparison of Nurses and Nurse Techni-cians. AACN Adv. Crit. Care. 2019;30:16–21. doi: 10.4037/aacnacc2019222. [DOI] [PubMed] [Google Scholar]
- 22.Galletta M., Portoghese I., D’Aloja E., Mereu A., Contu P., Coppola R.C., Finco G., Campagna M. Relationship between job burnout, psychosocial factors and health care-associated infections in critical care units. Intensive Crit. Care Nurs. 2016;34:59–66. doi: 10.1016/j.iccn.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Hu Z., Wang H., Xie J., Zhang J., Li H., Liu S., Li Q., Yang Y., Huang Y. Burnout in ICU doctors and nurses in main-land China-A national cross-sectional study. J. Crit. Care. 2021;62:265–270. doi: 10.1016/j.jcrc.2020.12.029. [DOI] [PubMed] [Google Scholar]
- 24.Kim H.S., Yeom H.-A. The association between spiritual well-being and burnout in intensive care unit nurses: A descriptive study. Intensive Crit. Care Nurs. 2018;46:92–97. doi: 10.1016/j.iccn.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Alvares M.E.M., Thomaz E.B.A.F., Lamy Z.C., de Abreu Haickel Nina R.V., Pereira M.U.L., Garcia J.B.S. Burnout syndrome among healthcare professionals in intensive care units: A cross-sectional population-based study. Rev. Bras. Ter. Intensiva. 2020;32:251–260. doi: 10.5935/0103-507X.20200036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ntantana A., Matamis D., Savvidou S., Giannakou M., Gouva M., Nakos G., Koulouras V. Burnout and job satisfaction of intensive care personnel and the relationship with personality and religious traits: An observational, multicenter, cross-sectional study. Intensive Crit. Care Nurs. 2017;41:11–17. doi: 10.1016/j.iccn.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Padilla Fortunatti C., Palmeiro-Silva Y. Effort-Reward Imbalance and Burnout among ICU Nursing Staff: A Cross-Sectional Study. Nurs. Res. 2017;66:410–416. doi: 10.1097/NNR.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 28.Sivakumar M., Hisham M., Saravanabavan L. Stress and Burnout among Intensive Care Unit Healthcare Professionals in an Indian Tertiary Care Hospital. Indian J. Crit. Care Med. 2019;23:462–466. doi: 10.5005/jp-journals-10071-23265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sok S., Sim H., Han B., Park S.J. Burnout and Related Factors of Nurses Caring for DNR Patients in Intensive Care Units, South Korea. Int. J. Environ. Res. Public Health. 2020;17:8899. doi: 10.3390/ijerph17238899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vasconcelos E., Martino M., França S. Burnout and depressive symptoms in intensive care nurses: Relationship analysis. Rev. Bras. Enferm. 2018;71:135–141. doi: 10.1590/0034-7167-2016-0019. [DOI] [PubMed] [Google Scholar]
- 31.Adriaenssens J., De Gucht V., Maes S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int. J. Nurs. Stud. 2015;52:649–661. doi: 10.1016/j.ijnurstu.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 32.De La Fuente-Solana E.E.I., Suleiman-Martos N., Pradas-Hernández L., Gomez-Urquiza J.L., Cañadas-De La Fuente G.G.A., Albendín-García L., Gómez-Urquiza J., Cañadas-De La Fuente G.G.A., Albendín-García L. Prevalence, Related Factors, and Levels of Burnout Syndrome among Nurses Working in Gynecology and Obstetrics Services: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health. 2019;16:2585. doi: 10.3390/ijerph16142585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kavurmacı M., Cantekin I., Tan M., Cantekin I. Burnout levels of hemodialysis nurses. Ren. Fail. 2014;36:1038–1042. doi: 10.3109/0886022X.2014.917559. [DOI] [PubMed] [Google Scholar]
- 34.López-López I.M., Gómez-Urquiza J.L., Cañadas G.R., De la Fuente E.I., Albendín-García L., Cañadas-De la Fuente G.A. Prevalence of burnout in mental health nurses and related factors: A systematic review and meta-analysis. Int. J. Ment. Health. Nurs. 2019;28:1032–1041. doi: 10.1111/inm.12606. [DOI] [PubMed] [Google Scholar]
- 35.Pradas-Hernández L., Ariza T., Gómez-Urquiza J.L., Albendín-García L., De la Fuente E.I., Cañadas-De la Fuente G.A. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS ONE. 2018;13:e0195039. doi: 10.1371/journal.pone.0195039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cañadas-De la Fuente G.A., Gómez-Urquiza J.L., Ortega-Campos E.M., Cañadas G.R., Albendín-García L., De la Fuente-Solana E.I. Prevalence of burnout syndrome in oncology nursing: A meta-analytic study. Psychooncology. 2018;27:1426–1433. doi: 10.1002/pon.4632. [DOI] [PubMed] [Google Scholar]
- 37.Monsalve-Reyes C.S., San Luis-Costas C., Gómez-Urquiza J.L., Albendín-García L., Aguayo R., Cañadas-De la Fuente G.A. Burnout syndrome and its prevalence in primary care nursing: A systematic review and meta-analysis. BMC Fam. Pract. 2018;19:59. doi: 10.1186/s12875-018-0748-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hämmig O. Explaining burnout and the intention to leave the profession among health professionals—A cross-sectional study in a hospital setting in Switzerland. BMC Health Serv. Res. 2018;18:785. doi: 10.1186/s12913-018-3556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moloney W., Boxall P., Parsons M., Cheung G. Factors predicting Registered Nurses’ intentions to leave their organization and profession: A job demands-resources framework. J. Adv. Nurs. 2017;74:864–875. doi: 10.1111/jan.13497. [DOI] [PubMed] [Google Scholar]
- 40.Hellyar M., Madani C., Yeaman S., O’Connor K., Kerr K.M., Davidson J.E. Case Study Investigation Decreases Burnout While Improving Interprofessional Teamwork, Nurse Satisfaction, and Patient Safety. Crit. Care Nurs. Q. 2019;42:96–105. doi: 10.1097/CNQ.0000000000000243. [DOI] [PubMed] [Google Scholar]
- 41.Rudman A., Gustavsson P., Hultell D. A prospective study of nurses’ intentions to leave the profession during their first five years of practice in Sweden. Int. J. Nurs. Stud. 2014;51:612–624. doi: 10.1016/j.ijnurstu.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 42.Li P., Kuang H., Tan H. The occurrence of post-traumatic stress disorder (PTSD), job burnout and its influencing factors among ICU nurses. Am. J. Transl. Res. 2021;13:8302–8308. [PMC free article] [PubMed] [Google Scholar]
- 43.Levi P., Patrician P.A., Vance D.E., Montgomery A.P., Moss J. Post-Traumatic Stress Disorder in Intensive Care Unit Nurses: A Concept Analysis. Work. Health Saf. 2020;69:224–234. doi: 10.1177/2165079920971999. [DOI] [PubMed] [Google Scholar]
- 44.Rizo-Baeza M., Mendiola-Infante S., Palazón-Bru A., Gil-Guillén V., Cortés-Castell E. Burnout syndrome in nurses work-ing in palliative care units: An analysis of associated factors. J. Nurs. Manag. 2018;26:19–25. doi: 10.1111/jonm.12506. [DOI] [PubMed] [Google Scholar]
- 45.Azizkhani R., Basravi M., Ahmadi O. Correlation between workplace and occupational burnout syndrome in nurses. Adv. Biomed. Res. 2014;3:44. doi: 10.4103/2277-9175.125751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Galdikienė N., Asikainen P., Balčiūnas S., Suominen T. Do nurses feel stressed? A perspective from primary health care. Nurs. Health Sci. 2013;16:327–334. doi: 10.1111/nhs.12108. [DOI] [PubMed] [Google Scholar]
- 47.Koinis A., Giannou V., Drantaki V., Angelaina S., Stratou E., Saridi M. The Impact of Healthcare Workers Job Environ-ment on Their Mental-emotional Health. Coping Strategies: The Case of a Local General Hospital. Health Psychol. Res. 2015;3:1984. doi: 10.4081/hpr.2015.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chang H., Shyu Y., Wong M., Friesner D., Chu T., Teng C. Which Aspects of Professional Commitment Can Effectively Retain Nurses in the Nursing Profession? J. Nurs. Scholarsh. 2015;47:468–476. doi: 10.1111/jnu.12152. [DOI] [PubMed] [Google Scholar]
- 49.Teles M.A.B., Barbosa M.R., Vargas A.M.D., Gomes V.E., e Ferreira E.F., de Barros Lima A.M.E., Ferreira R.C. Psychosocial work conditions and quality of life among primary health care employees: A cross sectional study. Health Qual. Life Outcomes. 2014;12:1–12. doi: 10.1186/1477-7525-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang L.-F., You L.-M., Liu K., Zheng J., Fang J.-B., Lu M.-M., Lv A.-L., Ma W.-G., Wang J., Wang S.-H., et al. The association of Chinese hospital work environment with nurse burnout, job satisfaction, and intention to leave. Nurs. Outlook. 2013;62:128–137. doi: 10.1016/j.outlook.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gascon S., Leiter M.P., Andrés E., Santed M.A., Pereira J.P., Cunha M., Albesa A., Montero-Marín J., García-Campayo J., Martínez-Jarreta B. The role of aggressions suffered by healthcare workers as predictors of burnout. J. Clin. Nurs. 2013;22:3120–3129. doi: 10.1111/j.1365-2702.2012.04255.x. [DOI] [PubMed] [Google Scholar]
- 52.Ruotsalainen J., Verbeek J., Mariné A., Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst. Rev. 2014;12:CD002892. doi: 10.1002/14651858.CD002892.pub3. [DOI] [PubMed] [Google Scholar]
- 53.Suleiman-Martos N., Gómez-Urquiza J.L., Aguayo-Estremera R., Cañadas-De La Fuente G.A., De La Fuente-Solana E.I., Albendín-García L. The effect of mindfulness training on burnout syndrome in nursing: A systematic review and meta-analysis. J. Adv. Nurs. 2020;76:1124–1140. doi: 10.1111/jan.14318. [DOI] [PubMed] [Google Scholar]