ABSTRACT
Background: Research is urgently needed to understand health care workers’ (HCWs’) experiences of moral-ethical dilemmas encountered throughout the COVID-19 pandemic, and their associations with organizational perceptions and personal well-being. This research is important to prevent long-term moral and psychological distress and to ensure that workers can optimally provide health services.
Objective: Evaluate associations between workplace experiences during COVID-19, moral distress, and the psychological well-being of Canadian HCWs.
Method: A total of 1362 French- and English-speaking Canadian HCWs employed during the COVID-19 pandemic were recruited to participate in an online survey. Participants completed measures reflecting moral distress, perceptions of organizational response to the pandemic, burnout, and symptoms of psychological disorders, including depression, anxiety, and posttraumatic stress disorder (PTSD).
Results: Structural equation modelling showed that when organizational predictors were considered together, resource adequacy, positive work life impact, and ethical work environment negatively predicted severity of moral distress, whereas COVID-19 risk perception positively predicted severity of moral distress. Moral distress also significantly and positively predicted symptoms of depression, anxiety, PTSD, and burnout.
Conclusions: Our findings highlight an urgent need for HCW organizations to implement strategies designed to prevent long-term moral and psychological distress within the workplace. Ensuring availability of adequate resources, reducing HCW risk of contracting COVID-19, providing organizational support regarding individual priorities, and upholding ethical considerations are crucial to reducing severity of moral distress in HCWs.
KEYWORDS: Moral distress, COVID-19, health care, depressive disorders, anxiety, posttraumatic stress disorder, organizational environment
HIGHLIGHTS
We sought to evaluate associations between workplace experiences during COVID-19, moral distress, and the well-being of Canadian health care workers.
Organizational variables predicted severity of moral distress.
Moral distress predicted symptoms of mental health conditions.
Short abstract
Antecedentes: Se necesita con urgencia investigaciones para comprender las experiencias de los dilemas éticos y morales que los trabajadores de la salud encontraron durante la pandemia de la COVID-19 y su asociación con las percepciones de la organización y el bienestar personal. Esta investigación es importante para prevenir la angustia moral y psicológica a largo plazo y para asegurar que los trabajadores de la salud puedan proveer de manera óptima los servicios de salud.
Objetivo: Evaluar la asociación entre las experiencias en el lugar de trabajo durante la COVID-19, la angustia moral y el bienestar psicológico de los trabajadores de salud canadienses.
Métodos: Se reclutó a un total de 1362 trabajadores de salud canadienses, que hablaban francés e inglés y que fueron contratados durante la pandemia de la COVID-19, para participar en un cuestionario en línea. Los participantes completaron mediciones que reflejaban la angustia moral, la percepción de la respuesta de la organización a la pandemia, el burnout y los síntomas de trastornos psicológicos, que incluían a la depresión, a la ansiedad y al trastorno de estrés postraumático (TEPT).
Resultados: El modelo de ecuaciones estructurales mostró que cuando los predictores de la organización se consideraban en conjunto – los recursos adecuados, el impacto positivo en la vida laboral y un ambiente de trabajo ético –, predijeron negativamente la gravedad de la angustia moral, mientras que la percepción del riesgo de contraer la COVID-19 predijo positivamente la gravedad de la angustia moral. La angustia moral también predijo de manera significativa y positiva los síntomas de la depresión, la ansiedad, el TEPT y el burnout.
Conclusiones: Nuestros hallazgos resaltan la urgente necesidad de que las organizaciones de trabajadores de salud implementen estrategias diseñadas para prevenir la angustia moral y psicológica a largo plazo en el lugar de trabajo. El asegurar la disponibilidad de los recursos adecuados, el reducir el riesgo de que los trabajadores de salud contraigan la COVID-19, el proveer un soporte organizacional adecuado según las prioridades individuales y el respetar las consideraciones éticas son fundamentales para reducir la gravedad de la angustia moral en los trabajadores de salud.
PALABRAS CLAVES: Angustia moral, COVID-19, atención de saludtrastornos depresivos, ansiedad, trastorno de estrés postraumático, ambiente de la organización
Short abstract
背景:亟需研究以了解卫生保健工作者 (HCW) 在整个 COVID-19 疫情期间遇到的道德伦理困境的经历, 及其与组织观念和个人幸福感的关联。本研究对于预防长期道德和心理困扰并确保工作人员能够最好地提供健康服务非常重要。
目的:评估加拿大医护人员的 COVID-19 期间工作场所经历, 道德困扰和心理健康之间的关联。
方法:共招募了 1362 名在 COVID-19 疫情期间受雇的讲法语和英语的加拿大 HCW 参与在线调查。参与者完成了反映道德困扰, 组织对疫情, 倦怠和心理障碍症状 (包括抑郁, 焦虑和创伤后应激障碍 (PTSD)) 的看法的测量。
结果:结构方程模型表明, 当同时考虑组织预测因素时, 资源充足性, 积极的工作生活影响和道德工作环境负向预测道德困扰的严重程度, 而 COVID-19 风险感知正向预测道德困扰的严重程度。道德困扰也显著且正向预测了抑郁, 焦虑, PTSD和倦怠的症状。
结论:我们的结果强调了 HCW 组织迫切需要实施旨在预防工作场所内长期道德和心理困扰的策略。确保可获取足够资源, 降低HCW接触 COVID-19 的风险, 提供个体优先性相关的组织支持以及坚持伦理考虑对于降低医护人员道德困境的严重程度至关重要
关键词: 道德困境, COVID-19, 医护, 抑郁, 焦虑, 创伤后应激障碍, 组织环境
1. Introduction
In early 2020, the World Health Organization declared a global pandemic due to the novel severe acute respiratory syndrome known as SARS-CoV-2 that causes COVID-19. As of July 2021, the COVID-19 pandemic has caused over 4 million deaths across 209 countries worldwide (World Health Organization, 2020). In addition to high levels of morbidity and mortality (Grech, 2020), this pandemic has since resulted in devastating impacts on individuals’ psychological well-being (Serafini et al., 2020).
Since the onset of the pandemic, health care workers (HCWs) have faced unprecedented situations involving potentially life-altering moral-ethical decisions, including rationing of limited medical resources (e.g. beds, ventilators) to patients who are equally in need (Greenberg, 2020), and the possibility of ending life for some patients to allocate resources to those with fewer comorbidities (Williamson et al., Williamson, et al., 2020). These complex moral-ethical decisions may have detrimental consequences for patients and HCWs alike, including reductions in quality of care (Kok, Hoedemaekers, van der Hoeven, Zegers, & van Gurp, 2020) and HCW moral distress (Khoo & Lantos, 2020). The overarching purpose of this study is to evaluate the associations between workplace experiences during COVID-19, moral distress, and the psychological well-being of HCWs.
1.1. COVID-19 and moral distress in health care workers
HCWs may become increasingly vulnerable to experiencing high severity of moral distress as a result of the moral-ethical challenges encountered throughout the COVID-19 pandemic (Khoo & Lantos, 2020; Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD, 2020). Moral distress occurs when an individual is constrained to behave in a way that they perceive as morally or ethically inappropriate, and as such, they are unable to act in accordance with their core values (Hamric, 2014; Jameton, 1993). For example, moral distress may occur if HCWs must attend to patients without typical recommended personal protective equipment (PPE), risking infection to self, to patients, or to family and community members, and are thus forced to compromise their typical standard of care (Binkley & Kemp, 2020; Hossain, 2020; Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD, 2020; Ranney, Griffeth, & Jha, 2020). It should be noted that distress can be distinguished from moral injury, defined as outcomes associated with perpetration, failure to prevent, or witnessing morally-transgressive acts (Litz & Kerig, 2019). When considered on a continuum of severity and frequency, morally injurious events occur less frequently and result in more severe impairment and harm than moral stressors (Litz & Kerig, 2019). For example, morally injurious events are more likely to involve life-threatening situations or major risks to personal integrity (Litz & Kerig, 2019).
Moral distress has been related to poor psychiatric outcomes in HCWs, including symptoms of depression and anxiety, even prior to the pandemic (Christodoulou-Fella, Middleton, Papathanassoglou, & Karanikola, 2017; Colville, Dawson, Rabinthiran, Chaudry-Daley, & Perkins-Porras, 2019; Lamiani, Borghi, & Argentero, 2017). Furthermore, throughout the pandemic, inconsistent and delayed guidance from government and workplace leaders may be associated with feelings of distrust and betrayal that could lead to doubts about the integrity of trusted figures and values (Hossain, 2020). It is possible that this distrust could call into question the moral soundness of organizational policies and associated job requirements under the pandemic, further increasing the likelihood of moral distress.
1.2. Moral distress and associations with organizational variables
HCWs’ experiences with moral-ethical dilemmas may be associated with adverse professional outcomes and perceptions of organizational environments, collectively referred to here as organizational variables or factors. Past empirical research has demonstrated that for nurses and physicians, high severity of moral distress was associated with negative professional outcomes, including increases in burnout, secondary traumatic stress, and intent to leave one’s professional position, as well as decreases in job satisfaction and perceptions of an ethical work environment (Austin et al., 2017; Christodoulou-Fella et al., 2017; Corley, Minick, Elswick, & Jacobs, 2005; De Veer, Francke, Struijs, & Willems, 2013; Fumis, Amarante, de Fátima Nascimento, & Junior, 2017; Lamiani et al., 2017; Pauly, Varcoe, Storch, & Newton, 2009). In addition to these organizational factors, nurses and physicians have also reported concerns regarding quality and safety of care delivered to patients (Lerkiatbundit & Borry, 2009; Mrayyan & Hamaideh, 2009; Wilkinson, 1987; Wolf et al., 2016), which results in increased severity of moral distress (Wolf et al., 2016). Although associations between workplace experiences and moral distress have not been empirically tested in HCWs during the COVID-19 pandemic, it is plausible to hypothesize that these findings would generalize across physicians, nurses, and other HCWs worldwide.
To best prevent long-term moral and psychological distress and to ensure that workers can optimally provide health services, research is urgently needed to understand experiences of workplace moral-ethical dilemmas throughout the COVID-19 pandemic, and their associations with HCWs’ organizational perceptions and personal well-being.
1.3. Aims of the study
The first objective of this study is to evaluate the effect of organizational variables on frequency/severity of moral distress during the COVID-19 pandemic within a Canadian HCW sample. Based on past findings (Austin et al., 2017; De Veer et al., 2013; Fumis et al., 2017), we hypothesize that perceptions of COVID-19 risk in an organizational setting will positively predict severity of moral distress during the COVID-19 pandemic. Conversely, we predict that perceptions of an ethical work environment, adequacy of resources, leadership, and positive work life impact will negatively predict severity of moral distress.
Next, we aim to assess the effect of frequency/severity of moral distress during the COVID-19 pandemic on symptoms of psychiatric disorders. Based on past findings (Christodoulou-Fella et al., 2017; Colville et al., 2019; Lamiani et al., 2017), we predict that severity of moral distress will positively predict symptoms of depression, anxiety, posttraumatic stress disorder (PTSD), and burnout. This study is the first to empirically examine the relations between moral distress, organizational factors, and symptoms of psychiatric disorders in a Canadian sample reflecting diverse health care backgrounds in the context of the COVID-19 pandemic.
2. Method
2.1. Participants
Participants included 1362 English- or French-speaking HCWs employed across Canada. We defined HCWs as those ‘who provide health treatment and advice based on formal training and experience, or who work to directly support those providers in a clinical setting.’ HCWs were eligible to participate if they were at least 18 years of age and currently or previously employed as a HCW in Canada between the start of the pandemic and the baseline end date.
2.2. Measures
2.2.1. Moral distress
Moral distress was evaluated using the Measure of Moral Distress for Healthcare Professionals (MMD-HP; Epstein, Whitehead, Prompahakul, Thacker, & Hamric, 2019). The MMD-HP is a revision of the Moral Distress Scale – Revised (MDS-R; Hamric, Borchers, & Epstein, 2012), specifically revised to adequately capture team and system-level sources of moral distress. In addition, the MMD-HP was designed using items that are applicable across health care disciplines, whereas the original MDS-R had six versions applicable to different types of HCWs. The MMD-HP comprises 27 items measured on 4-point scales designed to assess the frequency (0 = never, 4 = very frequently) and distress severity (0 = none, 4 = very distressing) associated with dilemmas that may cause moral distress in the workplace. Composite scores were calculated by multiplying participants’ frequency scores by their distress scores (Epstein et al., 2019). Higher scores represent higher severity of moral distress. Past research has supported the reliability and validity of the MMD-HP (e.g. α = .93; Epstein et al., 2019).
2.2.2. Burnout
The Expanded Well-Being Index (WBI; Dyrbye, Satele, & Shanafelt, 2016) was used to assess severity of HCW burnout throughout the past month. The WBI consists of seven dichotomous (yes/no) items, and two additional items that evaluate how meaningful the individual’s work is to them (7-point scale from very strongly disagree to very strongly agree) and work-life balance (5-point scale from strongly agree to strongly disagree). Scores were calculated in accordance with scoring guidelines, ranging from −2 to 9, with higher scores indicating more burnout (Dyrbye et al., 2016). Past empirical research has supported the validity of the WBI (Dyrbye, Satele, Sloan, & Shanafelt, 2014; Dyrbye et al., 2011).
2.2.3. Organizational response to the pandemic
We assessed HCWs’ perceptions of their organizations’ responses to the COVID-19 pandemic using an adapted version of the Pandemic Experiences and Perceptions Survey (PEPS; Leiter, 2020). The PEPS measures organizational response to the pandemic across five domains: Disruption (i.e. to workflow; 1 = no effect at all to 5 = completely dominated the work), Resource Adequacy (e.g. PPE; 1 = completely inadequate to 5 = completely adequate), COVID-19 Risk Perception (1 = no risk at all to 7 = life threatening risk), Positive Work Life Impact (e.g. work hours, social support; 1 = strongly disagree to 5 = strongly agree), and Leadership (i.e. supervisor/management; 1 = not at all to 5 = frequently, if not always). We included all domains except for Disruption. Mean scores on each subscale were calculated to create four separate scores, with higher scores indicating higher levels of resource adequacy, risk perception, more positive work life impact, and stronger leadership. The validity of the PEPS has been supported in recent research (AlMulla, 2020).
2.2.4. Ethical work environment
We used the 20-item Ethics Environment Questionnaire (EEQ; McDaniel, 1997) to measure health care workers’ perceptions about ethics in their organizations on a 5-point scale (1 = strongly disagree to 5 = strongly agree). We calculated participant mean scores on the EEQ, such that higher scores indicated a more ethical work environment. For descriptive purposes, we interpreted a mean value of ≥ 3.50 as indicative of a positive ethics environment (McDaniel, 1997). Past research has supported the reliability, validity, and unidimensional factor structure of the EEQ (e.g. α = .93; Corley et al., 2005; McDaniel, 1997).
2.2.5. Depression
HCWs’ depression symptom severity was assessed using the Patient Health Questionnaire-9 (PHQ-9; Spitzer et al., 1995) Participants responded to items on a scale ranging from 0 = not at all to 3 = nearly every day about their depressive symptoms throughout the past 14 days. Item responses were summed, such that higher scores reflect greater depression symptom severity. For descriptive purposes, we used a cut-off score of ≥ 10 for probable depression diagnosis (Kroenke, Spitzer, & Williams, 2001). The PHQ-9 has demonstrated strong reliability and validity in past research (e.g. α = .89; Kroenke et al., 2001).
2.2.6. Anxiety
To assess anxiety symptoms among HCWs, we used the 7-item General Anxiety Disorder-7 (GAD-7;Spitzer, Kroenke, Williams, & Löwe, 2006). Participants responded to items on a scale ranging from 0 = not at all to 3 = nearly every day about their anxiety symptoms throughout the past 14 days. Item responses were summed for a total anxiety score, with higher scores representing more severe anxiety. For descriptive purposes, we used a cut-off score of ≥ 10 for probable generalized anxiety diagnosis (Spitzer et al., 2006). Past research has supported the reliability and validity of the GAD-7 (e.g. α = .89; Löwe et al., 2008).
2.2.7. Posttraumatic stress disorder
The 20-item PTSD Checklist for the DSM-5 (PCL-5; Blevins, Weathers, Davis, Witte, & Domino, 2015) was used to measure PTSD symptom severity over the past month. Participants endorsed items on a 5-point scale ranging from 0 = not at all to 4 = extremely. Item responses were summed to create a total score, with higher scores reflecting greater PTSD symptom severity. For descriptive purposes, we used a cut-off score of ≥ 33 for probable PTSD diagnosis (Weathers et al., 2013). Empirical research supports the reliability and validity of the PCL-5 (e.g. α = .94; Blevins et al., 2015).
2.3. Procedure
Data presented here were drawn from a bilingual (i.e. English and French) survey exploring longitudinal changes in psychological functioning of HCWs during the COVID-19 pandemic. This research was approved by the ethical review board at Western University (approval number 115894). HCWs were recruited to participate via word of mouth, social media and online advertisements, participant recruitment websites, and media releases through Lawson Health Research Institute. Interested participants were directed to the survey-hosting platform, Research Electronic Data Capture (REDCap), where they read a letter of information and provided informed consent to volunteer in the study. Participants were provided with a choice to complete a long-form (approximately 25-minute duration) or short-form (approximately 10-minute duration) of the study. They then completed a series of demographic items and surveys related to their organizational experiences, burnout, and psychiatric symptoms. Participants complete follow-up surveys every three months to assess longitudinal changes in their well-being. However, the results presented here are based on cross-sectional baseline data collected between 26 June 2020, and 29 December 2020.
2.4. Data analytic strategy
Participant total scores were created for those who had completed at least 80% of the measures’ items except for the PEPS subscales. For the PEPS, participant scores were calculated for those who completed at least 50% due to the small number of items. Preliminary analyses, including descriptive statistics and bivariate correlations were calculated for all study variables using SPSS Version 26.0 (IBM Corp, 2019). Correlation magnitudes were evaluated based on Cohen’s (1988) guidelines, with correlations of .10 representing a small effect size, .30 representing a medium effect size, and .50 representing a large effect size.
Next, we tested predictive models to assess the associations between moral distress and organizational variables and psychiatric sequelae using structural equation modelling (SEM) in MPlus Version 8 (Muthén & Muthén, 1998–2017). We used the maximum likelihood robust estimator to correct standard errors for data non-normality, and the default full-information maximum likelihood to estimate missing data. To ensure that our sample size was adequate with consideration for model parameters (Bentler & Chou, 1987; Kline, 2015; Schreiber, Nora, Stage, Barlow, & King, 2006), we conducted two separate SEMs.
In the first model, we regressed the indicator variable, moral distress, onto latent variables associated with each subscale of the PEPS, as well as latent EEQ. We used four parcels as indicators for the unidimensional EEQ factor, as this measure comprises 20 unidimensional items. Item parcelling is recommended to stabilize parameter estimates for measures with a large number of items (Matsunaga, 2008). Specifically, if instead all 20 EEQ items were specified to load onto one factor, this item-level data may exhibit a large amount of measurement error. This would result in an unstable solution with a lack of potential for replicability across samples (Little, Cunningham, Shahar, & Widaman, 2002; Matsunaga, 2008). We used an indicator variable to represent moral distress because the MMD-HP aligns more with a formative (cf. reflective) model of measurement, and as such, it is not appropriate to specify that the exposure indicators occur as a result of latent moral distress (Bollen & Bauldry, 2011).
In the second model, we regressed outcome variables, including symptoms of anxiety, depression, PTSD, and burnout on moral distress. We used PCL-5 symptom cluster subscores as indicator variables for PTSD symptoms. Burnout was classified as an indicator variable, as its final two items were measured on Likert scales in contrast to the remaining dichotomous items. Model fit was established using cut-off values recommended by Hu and Bentler (1999).
3. Results
3.1. Sample characteristics
The top five occupations in the current study included nursing (42.8%), community health/personal support worker (10.7%), physician (4.9%), paramedic (4.0%), and social worker (3.1%). Of those enrolled in the study, n = 373 indicated they were working part-time or casual, and n = 989 were working full-time. A total of 792 HCWs were directly involved in clinical activities including diagnosis, treatment, or provision of direct care to patients with elevated temperature or confirmed COVID-19 in the month preceding participation. Additional demographic information and more detailed occupational information is presented in Table 1.
Table 1.
Demographic and organization information
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Age (years) | ||
| ≤25 | 39 | 2.9 |
| 26–40 | 443 | 32.5 |
| 41–60 | 537 | 39.4 |
| >60 | 65 | 4.8 |
| Prefer not to answer | 4 | 0.3 |
| Missing | 274 | 20.1 |
| Gender | ||
| Women | 974 | 71.5 |
| Men | 92 | 6.8 |
| Other | 7 | 0.5 |
| Prefer not to answer | 14 | 1.0 |
| Missing | 275 | 20.2 |
| Marital status | ||
| Single | 224 | 16.4 |
| Married/common law | 709 | 52.1 |
| Separated | 44 | 3.2 |
| Divorced | 76 | 5.6 |
| Widowed | 10 | 0.7 |
| Prefer not to answer | 27 | 2.0 |
| Missing | 272 | 20.0 |
| Province/territory | ||
| Prince Edward Island | 4 | 0.3 |
| Northwest Territories | 5 | 0.4 |
| Newfoundland | 6 | 0.4 |
| New Brunswick | 14 | 1.0 |
| Nova Scotia | 21 | 1.5 |
| Quebec | 34 | 2.5 |
| Saskatchewan | 34 | 2.5 |
| Manitoba | 48 | 3.5 |
| British Columbia | 93 | 6.8 |
| Alberta | 126 | 9.3 |
| Ontario | 435 | 31.9 |
| Missing | 542 | 39.8 |
| Highest level of education | ||
| Secondary or lower | 29 | 2.1 |
| Post-secondary or higher | 1061 | 77.9 |
| Missing | 272 | 20.0 |
| Primary job function | ||
| Administration | 86 | 6.3 |
| Outreach | 13 | 1.0 |
| Research | 15 | 1.1 |
| Direct client/patient care | 1169 | 85.8 |
| Other | 64 | 4.7 |
| Missing | 15 | 1.1 |
| Number of years as a health care worker | ||
| <6 months | 9 | 0.7 |
| 6 months to 1 year | 19 | 1.4 |
| 1 to 5 years | 253 | 18.6 |
| 6 to 10 years | 279 | 20.5 |
| 11+ years | 797 | 58.5 |
| Missing | 5 | 0.4 |
| Percentage direct patient care | ||
| No direct patient care | 75 | 5.5 |
| 1–24% | 71 | 5.2 |
| 25–50% | 78 | 5.7 |
| 51–74% | 148 | 10.9 |
| 75–100% | 985 | 72.3 |
| Missing | 5 | 0.4 |
| Workplace setting | ||
| Private practice | 116 | 8.5 |
| Hospital/community health centre | 923 | 67.8 |
| Other | 321 | 23.6 |
| Missing | 2 | 0.1 |
3.2. Preliminary analyses
Descriptive statistics, Cronbach’s alpha values, and bivariate correlations are reported in Table 2. The mean moral distress score in the current sample was 117.57 (Table 2), which is unsurprisingly higher than mean values reported among HCWs prior to the COVID-19 pandemic (e.g. M = 108.9, SD = 70.70; Epstein et al., 2019), and comparable to moral distress research conducted among non-Canadian HCWs during the COVID-19 pandemic (e.g. M = 113.4, SD = 60.30; Clark, Crawford, Hulse, & Polivka, 2021). The most frequently encountered morally distressing events, according to our sample, included witnessing low quality patient care due to poor team communication (82.9%), watching patient care suffer because of a lack of provider continuity (80.2%), and experiencing lack of administrative action or support for a problem that was compromising patient care (78.6%). Of those who had experienced a morally distressing event, the most distressing events (endorsed by participants as ‘very distressing’, or 4 on the 4-point scale) included a requirement to care for more patients than they could safely care for (48.5%), participating in care that caused unnecessary suffering or did not adequately relieve pain or symptoms (47.0%), and working with team members who did not treat vulnerable or stigmatized patients with dignity and respect (45.6%).
Table 2.
Descriptive statistics and bivariate correlations
| Measures | α | Skewness | Kurtosis | M (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Moral distress composite | .95 | .73 | .05 | 117.57(87.46) | |||||||||
| 2. Resource adequacy | .79 | −.21 | −.58 | 3.25(0.92) | −.46 | ||||||||
| 3. COVID-19 risk perception | .87 | −.14 | −.07 | 4.01(1.32) | .35 | −.19 | |||||||
| 4. Positive work life impact | .83 | −.07 | −.24 | 3.18(0.85) | −.45 | .52 | −.14 | ||||||
| 5. Leadership | .95 | −.08 | −.76 | 3.04(1.05) | −.41 | .52 | −.12 | .64 | |||||
| 6. Depression | .90 | .44 | −.55 | 10.75(6.59) | .37 | −.29 | .19 | −.37 | −.23 | ||||
| 7. Anxiety | .93 | .36 | −.89 | 9.21(6.00) | .34 | −.28 | .22 | −.34 | −.20 | .81 | |||
| 8. PTSD | .96 | .30 | −.79 | 31.96(19.37) | .49 | −.32 | .30 | −.40 | −.28 | .77 | .73 | ||
| 9. Burnout | .67 | −.41 | −.27 | 3.72(2.27) | .42 | −.34 | .21 | −.47 | −.33 | .61 | .56 | .56 | |
| 10. Ethical work environment | .93 | .10 | −.01 | 2.98(0.71) | −.54 | .54 | −.21 | .57 | .62 | −.29 | −.26 | −.33 | −.36 |
Note: All correlations significant at p < .001. n ranges from 885 to 1362. PTSD = posttraumatic stress disorder. Burnout α does not include items 8 and 9, which are used to add or subtract one item from participants’ initial scores (see WBI scoring information).
Of those who responded, a total of 46.6% of HCWs in our sample met the diagnostic cut-off score for probable PTSD, 52.2% met the cut-off score for depression, and 44.3% met the cut-off score for generalized anxiety (Spitzer et al., 2006). Means and standard deviations of the PEPS subscales were comparable to research conducted in Kuwait during the pandemic (AlMulla, 2020), with our Canadian sample scoring higher on resource adequacy and COVID-19 risk perceptions. However, we could not test whether these differences were statistically significant. The mean EEQ score in our sample (M = 2.98) did not reach the recommended value of 3.50, indicating that on average, our HCW sample did not perceive their work environment as ethical.
Bivariate correlations between study variables were all statistically significant (p < .001) with effect sizes ranging in magnitude from small to large based on Cohen’s (1988) guidelines (see Table 2).
3.3. Structural equation models
In the first SEM model, we regressed the indicator variable, moral distress, onto latent variables associated with resource adequacy, COVID-19 risk perception, positive work life impact, leadership, and ethical work environment. The first SEM regressing moral distress on PEPS variables and ethical work environment demonstrated poor fit (see Model 1 in Table 3). Upon closer inspection, modification indices demonstrated that correlating errors on the PEPS Leadership subscale would improve model fit, as item pairs reflected identical content and were endorsed separately for organizational management and immediate supervisor. To account for these identical item pairs, we conducted two additional structural models: Model 2) two separate latent variables representing Organizational Management Leadership and Immediate Supervisor Leadership, and Model 3) correlated errors between seven Leadership item pairs based on modification indices. Although model fit improved slightly (Table 3), modification indices showed that errors should again be correlated across the two latent Leadership variables due to content overlap. In addition, correlating errors without a priori theoretical rationale can inflate model fit and reduce potential for replication (Hermida, 2015; Landis, et al., 2009). We believe that the psychometric properties of the Leadership subscale should be revisited prior to its use in research, and therefore, we did not include Leadership in the final model.
Table 3.
Structural equation model fit indices
| Model | χ2 (df) | CFI | TLI | RMSEA | RMSEA 90% CI |
|---|---|---|---|---|---|
| Moral distress as outcome | |||||
| Model 1: All outcomes | 3954.901*(420) | .840 | .822 | .079* | .076, .081 |
| Model 2: Two leadership latent variables | 2791.768*(414) | .892 | .879 | .065* | .063, .067 |
| Model 3: Leadership correlated errors | 2497.325*(413) | .905 | .894 | .061* | .059, .063 |
| Model 4: Final model without leadership | 971.823*(180) | .926 | .914 | .057* | .053, .060 |
| Moral distress as predictor | 1248.522*(201) | .920 | .908 | .067* | .064, .071 |
Note: CFI = comparative fit index. TLI = Tucker-Lewis index. RMSEA = root mean square error of approximation.
CI = confidence interval. *p < .001.
The SEM without including the Leadership subscale included showed strong fit (see Model 4 in Table 3). As shown in Figure 1, resource adequacy, positive work life impact, and ethical work environment negatively predicted severity of moral distress, whereas COVID-19 risk perception positively predicted severity of moral distress.
Figure 1.
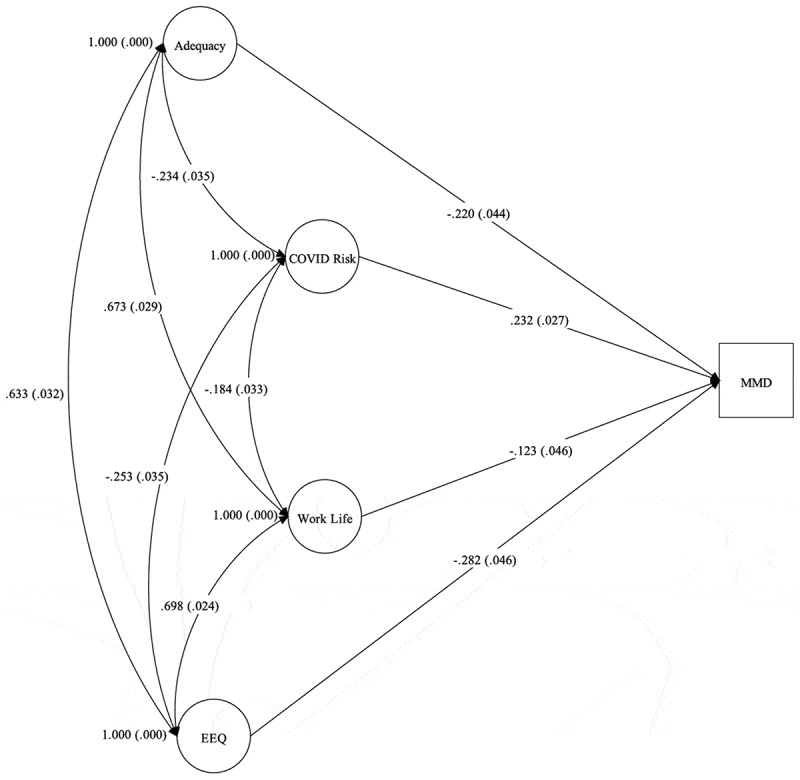
Moral distress regressed on organizational variables and ethical work environment without leadership: standardized path coefficients and latent variable correlations
n = 1362. Circles represent latent variables; square represents indicator variable. Curved lines represent latent variable correlations. Straight lines represent path coefficients. MMD = Moral distress composite. EEQ = Ethics Environment Questionnaire. Adequacy = Resource Adequacy. Coefficients are standardized. Standard error in brackets. All path coefficients and latent variable correlations significant at p < .01.
In the second model, we regressed latent outcome variables, including symptoms of anxiety, depression, PTSD, and burnout on the indicator variable, moral distress. This SEM fit the data well (see Table 3). As shown in Figure 2, moral distress significantly and positively predicted symptoms of depression, anxiety, PTSD, and burnout.
Figure 2.
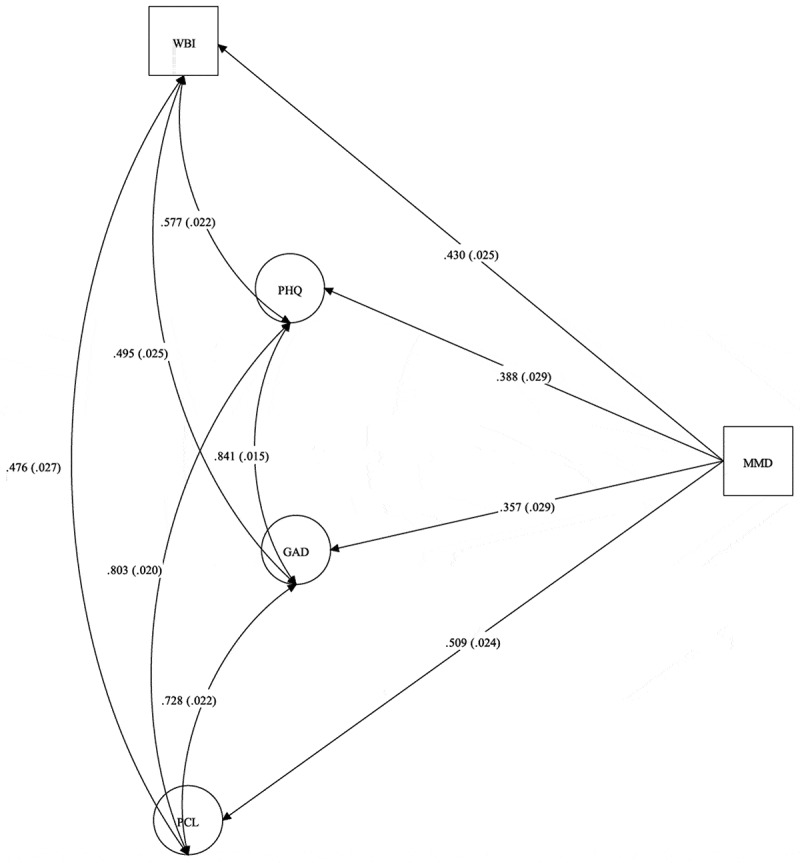
Burnout, depression, anxiety, and PTSD symptoms regressed on moral distress: standardized path coefficients and latent variable correlations
n = 1158. Circles represent latent variables; square represents indicator variable. Curved lines represent latent variable correlations. Straight lines represent path coefficients. MMD = Moral distress composite. WBI = Well-Being Index. PHQ = Patient Health Questionnaire (depression symptoms). GAD = Generalized Anxiety Disorder-7 (anxiety symptoms). PCL = PTSD Checklist for the DSM-5. Coefficients are standardized. Standard error in brackets. All path coefficients and latent variable correlations significant at p < .001.
4. Discussion
The aim of this study was to evaluate the associations between workplace experiences during COVID-19, moral distress, and the psychological well-being of HCWs. Unsurprisingly, moral distress scores were comparable to those found in studies conducted in a USA sample during the COVID-19 pandemic (Clark et al., 2021), and were higher than studies conducted prior to the COVID-19 pandemic (Epstein et al., 2019). Interestingly, events endorsed in the current study as the most morally distressing included, for example, compromised quality of patient care as evidenced by lack of team support, provider continuity, and overburdened patient loads, as well as experiencing lack of support from administration. These moral stressors are consistent with commonly reported issues experienced during COVID-19, including scarcity of resources and workplace support (e.g. Borges, Barnes, Farnsworth, Bahraini, & Brenner, 2020; Dryden-Palmer et al., 2020). In accordance with this, the mean EEQ score in our sample did not reach the recommended value that is reflective of a positive ethical work environment.
Approximately half of our sample who responded to the PHQ-9, GAD-7, and PCL-5 surveys met the cut-off scores for probable depression, anxiety, and PTSD. These rates are alarmingly high and exceed those published in recent COVID-19 research conducted in the UK (Choudhury et al., 2020), Norway (Johnson, Ebrahimi, & Hoffart, 2020), and Poland (Szepietowski et al., 2020), although rates of anxiety were similar in Polish HCWs. This may reflect the large toll that the COVID-19 pandemic has taken on the mental health of HCWs (Greenberg, 2020).
As expected, bivariate correlations showed that COVID-19-related organizational variables, including workplace resource adequacy, positive work life impact, managerial and organizational leadership, and perceptions of an ethical work environment were negatively associated with moral distress composite scores. On the other hand, moral distress was positively related to scores on COVID-19 risk perception. These findings are consistent with literature indicating that an organization’s response to the COVID-19 pandemic plays a strong role in HCW exposure and distress associated with moral-ethical dilemmas (Dryden-Palmer et al., 2020; Hlubocky et al., 2021). Specifically, issues encountered throughout (and even prior to) the pandemic, such as rationing of limited PPE and additional resources required to treat patients (Borges et al., 2020; Khoo & Lantos, 2020; Shanafelt, Ripp, & Trockel, 2020), lack of organizational leadership (Dryden-Palmer et al., 2020; Lamiani et al., 2017), and potential contact with the virus (Hlubocky et al., 2021) are all factors that contribute to the development and maintenance of moral distress in HCWs. Furthermore, when HCW organizations integrate core ethical values in their processes and strategies, this has been associated with reduced severity of moral distress, even prior to the COVID-19 pandemic (Corley et al., 2005).
These results were corroborated using SEM. Specifically, when all organizational variables were considered together, workplace resource adequacy, positive work life impact, and perceptions of an ethical work environment negatively predicted severity of moral distress, whereas COVID-19 risk perceptions positively predicted severity of moral distress. Interestingly, managerial and supervisor leadership was not a significant predictor of moral distress when all variables were included in the model. Upon inspection of the modification indices, it was evident that there was a surplus of shared error variance between item pairs reflecting managerial and supervisor leadership due to their identical wording. We opted to interpret a model without Leadership included, as this measure should be refined prior to future use. Similar to the model with Leadership included, each of the organizational variables significantly predicted severity of moral distress. Overall, these findings suggest that organizational responses to COVID-19 play a role in HCWs’ experiences of moral-ethical dilemmas and distress associated with such dilemmas.
As hypothesized, bivariate correlations between moral distress and psychiatric outcomes, including burnout, depression, anxiety, and PTSD symptoms were significant and medium in magnitude based on Cohen’s (1988) guidelines, ranging from .34 to .49. When the variables were entered into an SEM, similar results emerged, such that moral distress predicted levels of latent burnout, depression, anxiety, and PTSD symptoms with medium-to-large effect sizes. These findings support the notion that when HCWs engage in activities that they perceive to be morally or ethically conflicting, such as rationing scant PPE and risking infection to self and others, individuals may perceive themselves as failing to uphold their core personal and professional values and roles as caregivers to patients (Austin et al., 2017; Binkley & Kemp, 2020; Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD, 2020). This, in turn, leads to feelings and symptoms of guilt, shame, anger, anxiety, traumatic stress, burnout, and depression (Austin et al., 2017; Christodoulou-Fella et al., 2017; Colville et al., 2019; Lamiani et al., 2017; Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD, 2020).
Overall, our findings highlight an urgent need for HCW organizations to implement strategies designed to prevent moral and psychological distress within the workplace. Specifically, our results indicated that ensuring the perceived availability of adequate resources (e.g. PPE, ventilators, medications, staffing numbers), reducing HCW risk of contracting COVID-19, providing organizational support regarding decisions and individual priorities, and upholding ethical considerations are crucial to reducing severity of moral distress in HCWs.
4.1. Limitations and future directions
This study is not without limitations. Although we sampled a large number of HCWs from each Canadian province/territory, our sample is not representative of the greater Canadian HCW population (e.g. geographical, occupational, gender). In addition, our sample comprised mostly women. However, this is not surprising, as the most common HCW occupation in our sample comprises mainly women (nursing). Future research should ensure accurate representation of the Canadian HCW population using stratified sampling strategies, accounting for non-response bias, and exploring gender-specific effects.
The data presented here were cross-sectional in nature, which limits the conclusions that can be drawn from our findings. Longitudinal data reflecting moral distress and well-being to test mediation hypotheses, including whether moral distress mediates the associations between organizational variables and psychiatric outcomes measured, may elucidate the causal relationships among these domains. In addition, more research exploring the nuances of moral distress in HCWs (e.g. potential gender and occupational group differences, longitudinal trajectories) will inform the optimal development of resilience interventions aimed at the individual, group, institutional, and government levels.
Finally, it would be useful in future research to distinguish between moral stressors and morally injurious events encountered by HCWs. Although the MMD-HP addresses morally distressing situations, it is plausible that HCWs may experience a range of more severe (albeit less frequent) morally injurious events in the workplace (e.g. lack of resources resulting in patient death). Future research should consider whether more severe morally injurious events result in greater functional impairment and longer lasting consequences for HCWs, and potential protective factors and interventions for moral injury.
4.2. Concluding remarks
Overall, our findings provide insight into the moral-ethical dilemmas and the major detrimental effects these dilemmas have on HCWs’ psychological well-being. To best prevent long-term moral and psychological distress and to provide high quality care to patients, HCWs and their organizations, communities, and governments must work together and communicate standardized decision-making processes effectively to ensure that core ethical principles are upheld and that the mental and physical well-being of HCWs are maintained.
Funding Statement
This project was funded through the support of the MacDonald Franklin OSI Research Centre by the St. Joseph’s Health Care Foundation (London, Ontario, Canada) and through a partnership with the Centre of Excellence for PTSD (Ottawa, Ontario, Canada);Centre of Excellence for Post-Traumatic Stress Disorder;St. Joseph’s Health Care Foundation.
Data Availability
Study data are not available on a repository to protect participant privacy. However, data are available from the corresponding author, RP, upon reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- AlMulla, M. (2020). A measurement of radiographers pandemic experiences & perceptions survey (PEPS) during the coronavirus pandemic in Kuwait. ResearchSquare. doi: 10.21203/rs.3.rs-43360/v1. [DOI] [Google Scholar]
- Austin, C. L., Saylor, R., & Finley, P. J. (2017). Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 399–12. doi: 10.1037/tra0000201. [DOI] [PubMed] [Google Scholar]
- Bentler, P. M., & Chou, C. P. (1987). Practical issues in structural modeling. Sociological Methods & Research, 16(1), 78–117. doi: 10.1177/0049124187016001004. [DOI] [Google Scholar]
- Binkley, C. E., & Kemp, D. S. (2020). Ethical rationing of personal protective equipment to minimize moral residue during the COVID-19 pandemic. Journal of the American College of Surgeons, 230(6), 1111–1113. doi: 10.1016/j.jamcollsurg.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., & Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- Bollen, K. A., & Bauldry, S. (2011). Three Cs in measurement models: Causal indicators, composite indicators, and covariates. Psychological Methods, 16(3), 265–284. doi: 10.1037/a0024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges, L. M., Barnes, S. M., Farnsworth, J. K., Bahraini, N. H., & Brenner, L. A. (2020). A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychological Trauma, 12(S1), S138–S140. doi: 10.1037/tra0000698. [DOI] [PubMed] [Google Scholar]
- Choudhury, T., Debski, M., Wiper, A., Abdelrahman, A., Wild, S., Chalil, S., … Abdelaziz, H. K. (2020). Covid-19 pandemic: Looking after the mental health of our healthcare workers. Journal of Occupational and Environmental Medicine, 62(7), e373–e376. doi: 10.1097/JOM.0000000000001907. [DOI] [PubMed] [Google Scholar]
- Christodoulou-Fella, M., Middleton, N., Papathanassoglou, E. D., & Karanikola, M. N. (2017). Exploration of the association between nurses’ moral distress and secondary traumatic stress syndrome: Implications for patient safety in mental health services. BioMed Research International, 1908712. doi: 10.1155/2017/1908712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, P., Crawford, T. N., Hulse, B., & Polivka, B. J. (2021). Resilience, moral distress, and workplace engagement in emergency department nurses. Western Journal of Nursing Research, 43(5), 442–451. doi: 10.1177/0193945920956970. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Colville, G., Dawson, D., Rabinthiran, S., Chaudry-Daley, Z., & Perkins-Porras, L. (2019). A survey of moral distress in staff working in intensive care in the UK. Journal of the Intensive Care Society, 20(3), 196–203. doi: 10.1177/1751143718787753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corley, M. C., Minick, P., Elswick, R., & Jacobs, M. (2005). Nurse moral distress and ethical work environment. Nursing Ethics, 12(4), 381–390. doi: 10.1191/0969733005ne809oa. [DOI] [PubMed] [Google Scholar]
- De Veer, A. J., Francke, A. L., Struijs, A., & Willems, D. L. (2013). Determinants of moral distress in daily nursing practice: A cross sectional correlational questionnaire survey. International Journal of Nursing Studies, 50(1), 100–108. doi: 10.1016/j.ijnurstu.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Dryden-Palmer, K., Moore, G., McNeil, C., Larson, C. P., Tomlinson, G., Roumeliotis, N., … Parshuram, C. S. (2020). Moral distress of clinicians in Canadian pediatric and Neonatal ICUs. Pediatric Critical Care Medicine, 21(4), 314–323. doi: 10.1097/PCC.0000000000002189. [DOI] [PubMed] [Google Scholar]
- Dyrbye, L. N., Satele, D., & Shanafelt, T. (2016). Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. Journal of Occupational and Environmental Medicine, 58(8), 810–817. doi: 10.1097/JOM.0000000000000798. [DOI] [PubMed] [Google Scholar]
- Dyrbye, L. N., Satele, D., Sloan, J., & Shanafelt, T. D. (2014). Ability of the physician well-being index to identify residents in distress. Journal of Graduate Medical Education, 6(1), 78–84. doi: 10.4300/JGME-D-13-00117.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyrbye, L. N., Schwartz, A., Downing, S. M., Szydlo, D. W., Sloan, J. A., & Shanafelt, T. D. (2011). Efficacy of a brief screening tool to identify medical students in distress. Academic Medicine, 86(7), 907–914. doi: 10.1097/ACM.0b013e31821da615. [DOI] [PubMed] [Google Scholar]
- Epstein, E. G., Whitehead, P. B., Prompahakul, C., Thacker, L. R., & Hamric, A. B. (2019). Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empirical Bioethics, 10(2), 113–124. doi: 10.1080/23294515.2019.1586008. [DOI] [PubMed] [Google Scholar]
- Fumis, R. R. L., Amarante, G. A. J., de Fátima Nascimento, A., & Junior, J. M. V. (2017). Moral distress and its contribution to the development of burnout syndrome among critical care providers. Annals of Intensive Care, 7(1), 1–8. doi: 10.1186/s13613-017-0293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, V. (2020). Unknown unknowns–COVID-19 and potential global mortality. Early Human Development, 144, 105026. Article. doi: 10.1016/j.earlhumdev.2020.105026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Greenberg, N. (2020). Mental health of health-care workers in the COVID-19 era. Nature Reviews Nephrology, 16(8), 1–2. doi: 10.1038/s41581-020-0314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamric, A. B., Borchers, C. T., & Epstein, E. G. (2012). Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Primary Research, 3(2), 1–9. doi: 10.1080/21507716.2011.652337.26137345 [DOI] [Google Scholar]
- Hamric, A. B. (2014). A case study of moral distress. Journal of Hospice & Palliative Nursing, 16(8), 457–463. doi: 10.1097/NJH.0000000000000104. [DOI] [Google Scholar]
- Hermida, R. (2015). The problem of allowing correlated errors in structural equation modeling: Concerns and considerations. Computational Methods in Social Sciences, 3(1), 5–17. [Google Scholar]
- Hlubocky, F. J., Symington, B. E., McFarland, D. C., Gallagher, C. M., Dragnev, K. H., Burke, J. M., … Shanafelt, T. D. (2021). Impact of the COVID-19 pandemic on oncologist burnout, emotional well-being, and moral distress: Considerations for the cancer organization’s response for readiness, mitigation, and resilience. JCO Oncology Practice, 17(7), 365–374. doi: 10.1200/OP.20.00937. [DOI] [PubMed] [Google Scholar]
- Hossain, F. (2020). Moral distress among healthcare providers and mistrust among patients during COVID‐19 in Bangladesh. Developing World Bioethics. doi: 10.1111/dewb.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- IBM Corp . (2019). IBM SPSS statistics for windows. (Version 26.0).
- Jameton, A. (1993). Dilemmas of moral distress: Moral responsibility and nursing practice. AWHONN’s Clinical Issues in Perinatal and Women’s Health Nursing, 4(4), 542–551. [PubMed] [Google Scholar]
- Johnson, S. U., Ebrahimi, O. V., & Hoffart, A. (2020). PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PloS One, 15(10), e0241032. doi: 10.1371/journal.pone.0241032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo, E. J., & Lantos, J. D. (2020). Lessons learned from the COVID‐19 pandemic. Acta Paediatrica, 109(7), 1323–1325. doi: 10.1111/apa.15307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, R. B. (2015). Principles and practice of structural equation modeling. New York: Guilford Publications. [Google Scholar]
- Kok, N., Hoedemaekers, A., van der Hoeven, H., Zegers, M., & van Gurp, J. (2020). Recognizing and supporting morally injured ICU professionals during the COVID-19 pandemic. Intensive Care Medicine, 46(8), 1653–1654. doi: 10.1007/s00134-020-06121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamiani, G., Borghi, L., & Argentero, P. (2017). When healthcare professionals cannot do the right thing: A systematic review of moral distress and its correlates. Journal of Health Psychology, 22(1), 51–67. doi: 10.1177/1359105315595120. [DOI] [PubMed] [Google Scholar]
- Landis, R., Edwards, B. D., and Cortina, J (2009). Correlated residuals among items in the estimation of measurement models Lance, C. E., and Vandenberg, R. J. (Eds), 195-214. Statistical and methodological myths and urban legends: Doctrine, verity, and fable in the organizational and social sciences. New York: Routledge. [Google Scholar]
- Leiter, M. (2020). The Pandemic Experiences and Perceptions Survey (PEPS) (Group report).
- Lerkiatbundit, S., & Borry, P. (2009). Moral distress part I: Critical literature review on definition, magnitude, antecedents and consequences. Thai J Pharm Pract, 1(1), 1–10. [Google Scholar]
- Little, T. D., Cunningham, W. A., Shahar, G., & Widaman, K. F. (2002). To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 151–173. doi: 10.1207/S15328007SEM0902_1. [DOI] [Google Scholar]
- Litz, B. T., & Kerig, P. K. (2019). Introduction to the special issue on moral injury: Conceptual challenges, methodological issues, and clinical applications. Journal of Traumatic Stress, 32(3), 341–349. doi: 10.1002/jts.22405. [DOI] [PubMed] [Google Scholar]
- Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Matsunaga, M. (2008). Item parceling in structural equation modeling: A primer. Communication Methods and Measures, 2(4), 260–293. doi: 10.1080/19312450802458935. [DOI] [Google Scholar]
- McDaniel, C. (1997). Development and psychometric properties of the ethics environment questionnaire. Medical Care, 35(9), 901–914. doi: 10.1097/00005650-199709000-00003. [DOI] [PubMed] [Google Scholar]
- Mrayyan, M. T., & Hamaideh, S. H. (2009). Clinical errors, nursing shortage and moral distress: The situation in Jordan. Journal of Research in Nursing, 14(4), 319–330. doi: 10.1177/1744987108089431. [DOI] [Google Scholar]
- Muthén, L. K., & Muthén, B. O. (1998-2017). Mplus User’s Guide (Eighth ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pauly, B., Varcoe, C., Storch, J., & Newton, L. (2009). Registered nurses’ perceptions of moral distress and ethical climate. Nursing Ethics, 16(5), 561–573. doi: 10.1177/0969733009106649. [DOI] [PubMed] [Google Scholar]
- Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD . (2020) Moral Stress Amongst Healthcare Workers During COVID-19: A Guide to Moral Injury. Phoenix Australia – Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence – PTSD, ISBN online: 978-0-646-82024-8.
- Ranney, M. L., Griffeth, V., & Jha, A. K. (2020). Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. New England Journal of Medicine, 382(18), e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., & King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: A review. The Journal of Educational Research, 99(6), 323–338. doi: 10.3200/JOER.99.6.323-338. [DOI] [Google Scholar]
- Serafini, G., Parmigiani, B., Amerio, A., Aguglia, A., Sher, L., & Amore, M. (2020). The psychological impact of COVID-19 on the mental health in the general population. QJM: An International Journal of Medicine, 113(8), 531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanafelt, T., Ripp, J., & Trockel, M. (2020). Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA, 323(21), 2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Linzer, M., Hahn, S. R., Williams, J. B., Degruy, F. V., … Davies, M. (1995). Health-related quality of life in primary care patients with mental disorders: Results from the PRIME-MD 1000 study. JAMA, 274(19), 1511–1517. doi: 10.1001/jama.1995.03530190025030. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Szepietowski, J. C., Krajewski, P., Biłynicki‐Birula, R., Poznański, P., Krajewska, M., Rymaszewska, J., & Matusiak, Ł. (2020). Mental health status of health care workers during the COVID‐19 outbreak in Poland: One region, two different settings. Dermatologic Therapy, e13855. doi: 10.1111/dth.13855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD Accessed 1 March 2021. www.ptsd.va.gov.
- Wilkinson, J. M. (1987). Moral distress in nursing practice: Experience and effect. Nursing Forum, 23(1), 16–29. doi: 10.1111/j.1744-6198.1987.tb00794.x. [DOI] [PubMed] [Google Scholar]
- Williamson, V, Murphy, D, and Greenberg, N (2020). COVID-19 and experiences of moral injury in front-line key workers. Occupational Medicine, 70(5), 317–319. 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, L. A., Perhats, C., Delao, A. M., Moon, M. D., Clark, P. R., & Zavotsky, K. E. (2016). “It’s a burden you carry”: Describing moral distress in emergency nursing. Journal of Emergency Nursing, 42(1), 37–46. doi: 10.1016/j.jen.2015.08.008. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). WHO Coronavirus (COVID-19) Dashboard. Retrieved March 08, 2021 from https://covid19.who.int/?gclid=Cj0KCQiAs5eCBhCBARIsAEhk4r4dsuP522kuirJJazxnGZ9DEMcaEN4PjJr796Yo0GkENqQ_DcUuAn0aAjwrEALw_wcB.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Study data are not available on a repository to protect participant privacy. However, data are available from the corresponding author, RP, upon reasonable request.


