Abstract
The posterior tibial muscle (PTM) is a key muscle in diagnosing the level of the neurologic lesion that causes steppage gate that is a paralysis of nervous origin of the muscles ensuring the foot dorsiflexion.
The aim of this manuscript is to illustrate the anatomical peculiarities of the PTM, the ultrasound (US) anatomy of the infero-posterior part of the leg, and the technique of US-guided electro-neuro-myography (ENMG) of the PTM, which is considered a key muscle in the diagnosis of the neurological lesion causing steppage gate.
The US-guided ENMG of the PTM is technically easy and safe for young practitioners provided there is a good knowledge of US anatomy of the infero-posterior part of the leg.
Keywords: foot drop, posterior tibial muscle, ultrasound, electromyography, steppage gate
Introduction
Nowadays, the needle electro-neuro-myography (ENMG) plays a major role in the site diagnosis of neurological lesions of the limbs, for example in steppage gate. The latter is also known as drop foot that is a paralysis of nervous origin of the muscles ensuring the dorsiflexion of the foot.
But this type of exploration requires a lot of expertise when it comes to deep nerve or muscle that has crucial contribution to diagnosis because of its anatomical peculiarities.
The use of ultrasound (US) facilitates the implementation of the ENMG of these anatomical elements and makes it accessible to less-experienced clinicians [1].
The aim of this manuscript is to illustrate the anatomical peculiarities of the posterior tibial muscle (PTM), the US anatomy of the infero-posterior part of the leg, and the technique of US-guided ENMG of the PTM, which is considered a key muscle in the diagnosis of the neurological lesion causing steppage gate.
Technical report
A good knowledge of the US anatomy of the leg makes it easy to locate the PTM so as to prick it with ENMG needle.
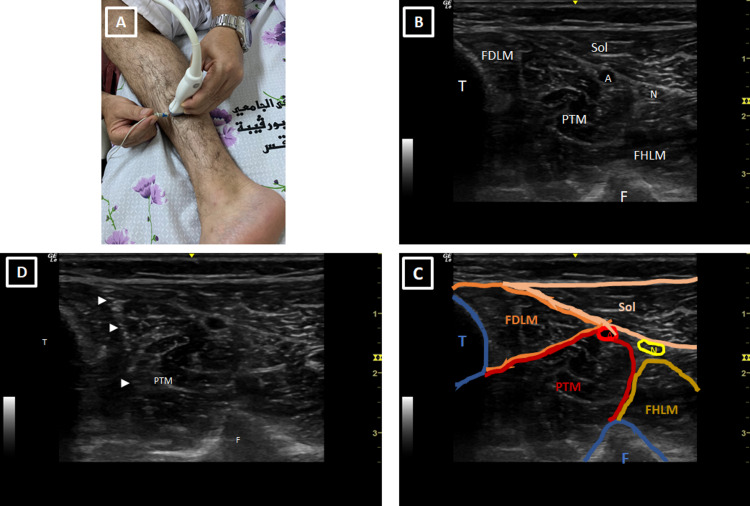
Indeed, a physician must first place the US probe in the middle third of the posteromedial side of the leg as shown in Figure 1A. The obtained US image should show the two bones of the leg centered by the PTM and part of the muscles of the anterior compartment of the leg (Figures 1B, 1C). It is then easy to prick the PTM by the ENMG needle under US guidance as shown in Figures 1A, 1D.
Figure 1. Technique of ultrasound-guided ENMG of the posterior tibial muscle.
(A) Placement of the ENMG needle under ultrasound control in the PTM. The ultrasound probe is placed in the middle of the posteromedial side of the leg. (B, C) Ultrasound sections in the middle part of the leg illustrating the different anatomical elements and locating the PTM. (D) Ultrasound view showing the ENMG needle (arrow heads) in the PTM.
ENMG: electro-neuro-myography; T: tibia; F: fibula; PTM: posterior tibial muscle; Sol: soleus muscle; FDLM: flexor digitorum longus muscle; FHLM: flexor hallucis longus muscle; A: posterior tibial artery; N: posterior tibial nerve.
Discussion
Anatomy reminder
The PTM is a deep muscle in the posterior compartment of the leg. It originates from the interosseous membrane and from the two bones of the leg: the proximal 2/3 of the medial face of the body of the fibula and of the dorsal face of the body of the tibia. Then it follows a slightly oblique path downwards and inwards up to the ankle where it is continued by a tendon which goes behind the medial malleolus in the gutter of the flexor muscles then passes above the sustentaculum tali, along the internal surface of the navicular bone to end at the plantar surface of the latter giving expansions toward all the bones of the foot except the talus, the first and the fifth metatarsals [2].
This muscle has several roles, namely plantar flexion, supination, and adduction of the foot. The combination of the last two movements results in the inversion of the foot. In addition, this muscle also helps maintain the arch or the hollow of the foot.
The PTM is innervated by the posterior tibialis nerve, which is a branch of the sciatic nerve. However, the PTM has the anatomical peculiarity of being the only muscle of the posterior compartment of the leg to be innervated by the L5 root like the foot levator muscles of the anterolateral compartment of the leg.
US contribution for performing ENMG
Several studies have proven the indisputable utility of US guidance for performing ENMG.
Precise ENMG needle placement is possible with US guidance for testing of nerves (particularly deep ones) and it is obviously superior to surface recordings of sensitive nerves [3-5].
Standard ENMG may show the absence of any motor unit potential (MUP) in patients with muscle plegia due to nerve trauma. But the US is very helpful for detection of isles of muscle contractility that should have MUP in ENMG and this has a clear prognostic impact [6].
US guidance has also proven to be useful in challenging ENMG of certain deep muscles as diaphragm muscle, teres minor muscle, and external anal sphincter [7-9].
Diagnostic value of the PTM
Steppage (also known as drop foot) is a paralysis of nervous origin of the muscles ensuring the dorsiflexion of the foot (also known as the elevator muscles of the foot and toes). These muscles are the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and third fibularis. Any damage or compression of the nerve axis anywhere along its path has the potential to cause the foot to fall and steppage gate [10,11].
Involvement of the foot elevator motor nerve can be localized either at the level of the L5 root or at the level of the peroneal nerve (also known as the external popliteal sciatic nerve [EPS]). Consequently, in case of steppage gate it is mandatory to eliminate L5 root damage, which can perfectly simulate EPS damage without any radicular pain [12].
Taking into account that PTM is innervated by the L5 root but does not depend on the peroneal nerve, its clinical, US, and electromyographic evaluation is of great help in the diagnosis of the level of neurological lesion causing the steppage gate [12].
Conclusions
Thanks to its anatomical peculiarities, the PTM is a key muscle in determining the level of the neurologic lesion that causes steppage gate. Its exploration by standard ENMG requires a lot of expertise but has been revolutionized by US, which has greatly facilitated and made it accessible to young practitioners provided they have a good knowledge of US anatomy of the infero-posterior part of the leg.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Accuracy of electromyography needle placement in cadavers: non-guided vs. ultrasound guided. Boon AJ, Oney-Marlow TM, Murthy NS, Harper CM, McNamara TR, Smith J. Muscle Nerve. 2011;44:45–49. doi: 10.1002/mus.22008. [DOI] [PubMed] [Google Scholar]
- 2.Dufour M. Paris, France: Elsevier Masson; 2015. Anatomie de l'appareil locomoteur-Tome 1 Membre inférieur 3rd Edition . [Google Scholar]
- 3.Ultrasound-guided electrodes for conduction studies of the saphenous nerve. Evangelopoulos ME, Humpert S, Rösler KM. J Clin Neurophysiol. 2017;34:243–247. doi: 10.1097/WNP.0000000000000361. [DOI] [PubMed] [Google Scholar]
- 4.Utility of ultrasound-guided near-nerve needle recording for lateral femoral cutaneous sensory nerve conduction study: does it increase reliability compared with surface recording? Deimel GW, Hurst RW, Sorenson EJ, Boon AJ. Muscle Nerve. 2013;47:274–276. doi: 10.1002/mus.23694. [DOI] [PubMed] [Google Scholar]
- 5.Ultrasound-guided needle positioning near the sciatic nerve to elicit compound muscle action potentials from the gastrocnemius muscle of the rat. Nijhuis TH, Smits ES, van Neck JW, Visser GH, Walbeehm ET, Blok JH, Hovius SE. J Neurosci Methods. 2011;194:283–286. doi: 10.1016/j.jneumeth.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 6.Ultrasound guidance increases diagnostic yield of needle EMG in plegic muscle. Gentile L, Coraci D, Pazzaglia C, Del Tedesco F, Erra C, Le Pera D, Padua L. Clin Neurophysiol. 2020;131:446–450. doi: 10.1016/j.clinph.2019.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Ultrasound-guided needle EMG of the diaphragm: technique description and case report. Boon AJ, Alsharif KI, Harper CM, Smith J. Muscle Nerve. 2008;38:1623–1626. doi: 10.1002/mus.21187. [DOI] [PubMed] [Google Scholar]
- 8.Verification of a standardized method for inserting intramuscular electromyography electrodes into teres minor using ultrasound. Rathi S, Zacharias A, Green RA. Clin Anat. 2015;28:780–785. doi: 10.1002/ca.22561. [DOI] [PubMed] [Google Scholar]
- 9.Ultrasound-guided needle electromyography of the external anal sphincter. Park DY, Park JH. PM R. 2019;11:731–736. doi: 10.1002/pmrj.12012. [DOI] [PubMed] [Google Scholar]
- 10.Foot drop. Stevens F, Weerkamp NJ, Cals JW. BMJ. 2015;350:0. doi: 10.1136/bmj.h1736. [DOI] [PubMed] [Google Scholar]
- 11.Peroneal neuropathy misdiagnosed as L5 radiculopathy: a case report. Reife MD, Coulis CM. Chiropr Man Therap. 2013;21:12. doi: 10.1186/2045-709X-21-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varus of the hindfoot in foot drop: a key for the etiologic diagnosis. Elleuch MH, Jelassi O, Trabelsi E, Kerkeni H, Elleuch M, Ghroubi S. Med Chir Pied. 2020;36:44–51. [Google Scholar]