Abstract
The aim of this paper was to assess the state of resilience and well-being in the Polish population during the COVID-19 pandemic. We also assessed the relationship between resilience and mental health. Finally, we tested the mediating role of COVID-19 anxiety, persistent thinking, and the stress burden in the relationship between mental health and resilience. This research perspective can provide important insights into how individuals can become mentally stronger during the COVID-19 pandemic. Methods: This study included 1758 people (73% women) aged 18–80 years. The procedure consisted of completing a questionnaire measuring well-being, COVID-19 anxiety, obsession with COVID-19, stress over COVID-19, and resilience. Results: Bootstrap sampling analysis showed significant partial mediators for the relationship between resilience and well-being. Important mediators were coronavirus anxiety, persistent thinking, and perceived stress. Conclusions: The results of the present study clearly indicate that resilience as a protective factor is associated with reduced anxiety about COVID-19, perceived stress burden, obsessive thoughts about the pandemic, and increased well-being of individuals. Resilience plays an important role in minimizing negative and enhancing positive health indicators in the face of challenging life events.
Keywords: resilience, mental health, well-being, anxiety about COVID-19, obsession with COVID-19, stress over COVID-19
1. Introduction
Anxiety, a sense of being burdened, and stress are common responses to perceived or real threats, and also when faced with uncertainty or the unknown. So, it is understandable that people feel such tension in the context of the COVID-19 pandemic [1,2,3,4]. In addition to the fear of contracting the virus, there are significant changes in everyday life, as individuals are restricted in their functioning as part of efforts to contain and slow down the spread of the virus. In the face of this new reality, the World Health Organization (WHO) and researchers are paying attention to the need for a two-dimensional approach and recommend psychological interventions aimed at minimizing negative indicators of mental health (e.g., anxiety, depression, stress) and activating positive indicators (e.g., well-being, quality, and satisfaction with life) [5,6,7]. Therefore, the current definitions of health deviate from a one-sided understanding of disease and focus not only on reducing or eliminating disease manifestations, but also on taking into account pro-health aspects, considering physical, mental, and social areas. In this respect, a two-dimensional model of mental health is a solid basis for holistic and accurate diagnosis of individual health-related indicators [5,8]. In this paper, it was decided to use both types of mental health indicators. According to the assumptions of psychological resilience theories [9,10,11,12,13], in addition to both types of mental health indicators, personal resources and assets should be identified as means of helping individuals overcome difficulties and adapt to circumstances. For these reasons, this study looked at the role that resilience plays in mental health in the general population, considering both positive (well-being) and negative (anxiety, obsessive thinking, burden of stress) indicators.
The COVID-19 pandemic has created a critical global situation, with a particularly severe impact on the quality of life and mental health of many people. Publications on mental health during the pandemic and related determinants are still increasing. Many of them report worrying consequences for psycho-emotional and social functioning or increased susceptibility to mental health problems (e.g., high risk of depression, stress, and more frequent suicidal thoughts and behavior) [14]. According to recent meta-analyses, the incidence of stress, anxiety, and depression in the general population as a result of a pandemic is around 30% [15,16,17]. The current pandemic has been accompanied by numerous stressors that lead to anxiety and hopelessness [1,15,18].
COVID-19 research and media reports have revealed a rise in fear related to contracting the virus. Though fear is a common psychological outcome during a pandemic, the current pandemic is a continuously evolving disease outbreak and has unique risk factors. Therefore, fear related to COVID-19 could manifest in not only fear and anxiety related to contracting the disease and dying, but also associated socio-occupational stress [19,20]. The data also show that people who are isolated and quarantined have higher levels of anger, confusion, and post-traumatic stress [2]. The epidemic experience increases the long-term level of depression [21,22,23] and may also increase future suicide rates [24]. Experiencing more unpleasant events in life and having difficulty coping with them are also predictors of anxiety, stress, and depression [25]. Research indicates that the COVID-19 pandemic has caused significant declines in mental health, life satisfaction, and well-being in China, the USA, Japan, Germany, Ireland, and New Zealand, among countries. Therefore, we expect that the COVID-19 pandemic will also have a negative impact on mental health in Poland. In such a situation, it seems necessary to pay attention to resources on immunity, which are the basis for, inter alia, the theory of salutogenesis by Antonovsky [26] and the theory of resilience [9,11,27], which may protect against the negative impact of a pandemic and be helpful in finding answers to questions about maintaining and strengthening positive aspects of health [28,29].
Dealing with a pandemic requires an adequate ability to withstand failure, adapt positively, and react to adversity. It also requires the ability to cope with significant changes and take responsibility by recovering from adversity, uncertainty, and negativity, and even to make positive changes. This ability is referred to as resilience [30], which can be developed and strengthened and change over time. Strengthening mental health and developing specific facilities and skills can be an opportunity to develop the well-being of individuals.
It has been shown that some people are more mentally resistant to adversity than others, and that patterns of vulnerability and resilience differ [31]. The literature consistently shows a negative relationship between resilience and anxiety, persistent thinking, depression, and psychological distress, especially in the case of natural disasters such as the 2010 Haiti earthquake [32] and Hurricane Katrina in 2005 [33]. It is therefore crucial for researchers and clinicians to identify the factors that help build up the mental health of individuals and the well-being of society. It should be noted that, according to recent reports, resilience is a significant predictor of mental health behavior during the COVID-19 pandemic [34]. Researchers indicate that resilience may, inter alia, reduce the symptoms of post-traumatic stress, anxiety about the coronavirus, and the intensification of complicated grief in people who could not take care of their relatives’ final arrangements during the lockdown [35,36]. Researchers also found that the average immunity in the population during the outbreak was lower than published standards, but was higher among those who went outside more often, exercised more, had greater social support from family, friends, and other important people, slept better, and prayed more [37,38]. It should therefore be noted that resilience in the face of a pandemic is associated with modifiable factors. However, the impact of resilience on mental health (WHO) in the Polish population in the context of the COVID-19 pandemic has not been well documented.
Previous reports on the spread of infectious diseases found clear associations between perceived anxiety and stress over a pandemic and depressed well-being and symptoms of PTSD [39,40,41]. It therefore seems that perceived anxiety and stress may be effective markers for mental functioning during COVID-19. Accordingly, in recent reports, anxiety over coronavirus explained the impact of resilience to PTSD symptoms [42]. A similar mediator in the relationship between resilience and PTSD was reported to be persistent thinking about COVID-19 [43]. Persistent thinking is associated with passive attention to negative emotions [44]. According to Beck, distortions in information processing lead to a preoccupation with the threat and an underestimation of the ability to deal with the threat, which ultimately causes pathological anxiety or distress [45,46]. In the case of perceived stress, no similar analyses have been conducted so far. However, Gustafsson and colleagues [47] showed that perceived stress fully mediates the relationship between optimism and burnout symptoms, and according to Wang and colleagues [48], perceived stress partially mediates the relationship between hope and PTSD symptoms. Therefore, it seems that the direction of the relationship between resilience and well-being may be explained by anxiety over coronavirus, persistent thinking about COVID-19, and perceived stress.
The pandemic, while also being a global public health threat with multifaceted serious consequences for people’s lives and mental health, is raising the awareness not only of researchers, but also of practitioners and politicians around the world regarding the urgent need to focus on resilience resource-based programs, which are critical to managing with stress and trauma. Constructing them is necessary to maintain balance and the well-being, satisfaction, and quality of life of individuals and societies [49]. Chen and Bonanno [50] suggest that diagnosing the long-term patterns of COVID-19 effects on mental health is important to better understand risk factors and resilience. Such findings can provide valuable information that can be incorporated into prevention and intervention programs to help the general public cope with evolving multifaceted challenges at different stages of the pandemic [51]. Building resilience-based prevention programs can also activate other resources to overcome the acute effects of the pandemic, which will ultimately affect the mental health of individuals. The development of intervention programs can also help boost resilience and improve well-being among the affected populations. The results of the current study show important practical implications for improving mental health among people confronted with the COVID pandemic [52,53].
Previous literature on resilience theory and empirical findings indicate the importance of personality resources in promoting well-being and minimizing anxiety and stress in coping with the COVID-19 pandemic. Therefore, the analyzed problem is of key importance for researchers and clinicians, as identifying resilience resources and risk factors is important in order to better understand the functioning of individuals in the field of mental health. Such findings provide valuable information that can be incorporated into preventive and therapeutic interventions to help the general public cope with the evolving multifaceted challenges at different stages of the pandemic [49,50,51,52,53].
Purpose of the of Study
Studies that have assessed the effects of COVID-19 from a mental health perspective commonly highlight negative indicators and the mental disorders it can lead to [54,55,56]. However, it has been argued that focusing on positive indicators that make up a healthy psychological perspective, such as resilience and well-being, is more effective in developing adequate mental health [51,57,58]. Therefore, this paper aimed to assess the state of resilience and well-being in the Polish population during the COVID-19 pandemic. This research perspective can provide important insights into how individuals can become mentally stronger during the pandemic. We also assessed the relationship between resilience and mental health. Finally, we tested the mediating role of COVID-19 anxiety, persistent thinking, and the stress burden in the relationship between mental health and resilience. Based on the literature review described above [39,40,41,42,43,44,45,46,47,48], we suppose that the relationship between resilience and well-being will be mediated by (H1) anxiety over coronavirus, (H2) obsessive thinking about COVID-19, and (H3) the stress burden. Due to these formulated hypotheses, we assume that including a mediator in the analysis will decrease the strength of the relation between the independent variable (resilience) and the dependent variable (well-being).
2. Method
2.1. Participants and Procedure
The study was conducted from July to December 2020 with the approval of the university ethics committee (#15/IV/2020). A total of 1758 participants (73% of whom were female) aged 18–80 years (M = 29.08; SD = 11.33) participated in the study. The invitation to participate in the study was distributed through social media (e.g., Facebook) and websites (news portals). The Google Forms platform was used to collect data. Each participant gave informed consent to participate in the study anonymously. The procedure consisted of completing a questionnaire to measure resilience, coronavirus anxiety, obsessive thinking, stress, and well-being. The questionnaire took approximately 30 min to complete. At the end, each participant declared their age and sex.
2.2. Measures
The World Health Organization’s Five Well-Being Index (WHO-5) was used to assess participants’ well-being [59]. This short scale avoids symptom-related or negative phrasing and measures well-being instead of the absence of distress. Representative items include “I have felt cheerful and in good spirits” and “My daily life has been filled with things that interest me”. Respondents assess how often they had the respective feelings within the last 2 weeks, ranging from 0 (no times) to 5 (all the time). Here, we report the sum scores, ranging from 0 to 25. A score <13 would indicate reduced well-being or even a depressive state. The Polish version showed satisfactory accuracy and internal consistency (α = 0.87) [60]. Sample items include “I have felt cheerful and in good spirits” and “I have felt calm and relaxed”.
Perceived stress burden (PSB). Perceived effects on daily life due to disease-related symptoms, feelings of being restricted in daily life by the COVID-19 pandemic, and feelings of being under pressure (i.e., stress and fear) due to the pandemic were measured using 5 items, ranging from 0 (not at all) to 100 (very strong). This stress’ scale is strongly related to reduced well-being and life satisfaction, but only marginally with awe/gratitude. These 5 items can be combined into a factor termed “perceived stress’’ with good internal consistency (α = 0.80) [61]. Sample items include “I feel anxiety and uncertainty” and “I’m feeling stressed”.
The Coronavirus Anxiety Scale (CAS) is a single-factor instrument designed to assess the severity of anxiety related to the psychological crisis caused by the new human coronavirus pandemic [62]. Participants respond to 5 statements (physical symptoms of anxiety) on a 5-point Likert scale, ranging from 0 (not at all) to 4 (almost every day). The CAS is a diagnostically accurate and reliable tool for assessing the severity of coronavirus anxiety. CAS scores correlated statistically significantly with general anxiety, depression, suicidal thinking, and drug and alcohol use. The Polish version showed satisfactory accuracy and internal consistency (α = 0.86) [42]. Sample items include “I lost interest in eating when I thought about or was exposed to information about the coronavirus” and “I felt nauseous or had stomach problems when I thought about or was exposed to information about the coronavirus”.
The Obsession with COVID-19 Scale (OCS) is a self-reported mental health screen for persistent and disturbed thinking about COVID-19 [63]. Participants express their attitude toward 4 statements on a 5-point Likert scale, ranging from 0 (not at all) to 4 (almost every day). The OCS is a reliable instrument with solid factorial (single-factor) and construct (correlated with coronavirus anxiety, spiritual crisis, alcohol/drug coping, extreme hopelessness, and suicidal ideation) validity. The diagnostic properties of the OCS (81 to 93% sensitivity and 73 to 76% specificity) are comparable to related screening instruments such as the General Health Questionnaire (GHQ). The Polish version of the OCS was characterized by satisfactory psychometric properties (α = 0.82) [43]. Sample items include “I had disturbing thoughts that I may have caught the coronavirus” and “I had disturbing thoughts that certain people I saw may have the coronavirus”.
The Brief Resilience Scale (BRS) is a reliable means of assessing resilience as the ability to bounce back or recover from stress [64]. The BRS has 6 items with a 5-point Likert response scale, ranging from 1 (strongly disagree) to 5 (strongly agree); 3 items are positively phrased and 3 are negatively phrased. The BRS is scored by reverse coding items 2, 4, and 6, and then calculating the mean of the 6 items. The BRS is reliable and was measured as a unitary construct. It was predictably related to personal characteristics, social relations, coping, and health in all samples. It was negatively related to anxiety, depression, negative affect, and physical symptoms when other resilience measures and optimism, social support, and type D personality were controlled. The Polish version of the BRS was characterized by good internal compatibility assessment based on Cronbach’s alpha (α = 0.88) and McDonald’s omega (ω = 0.88) [65]. Sample items include “I tend to bounce back quickly after hard times” and “I have a hard time making it through stressful events”.
2.3. Statistical Analysis
Data analysis was conducted in IBM SPSS Statistics 26 and the PROCESS macro in version 3.2 [66]. Pearson’s correlation analysis was used to determine the relations between variables. The significance level was determined at p < 0.050. The effect size was assessed based on R2. In order to verify the mediating role of COVID-19 anxiety, stress burden, and obsession with COVID-19 on the relationship between resilience and well-being, a bootstrapping analysis (for 2000 samplings) was carried out to establish 95% percentile confidence intervals for the estimated effects. When the value of the confidence interval exceeds 0, it means that the given effect is insignificant.
3. Results
The mean values obtained in the study, together with the standard deviation regarding the controlled variables of resilience (BRS), coronavirus anxiety (CAS), persistent thinking (OCS), perceived stress (PBS), and well-being (WHO-5), as well as correlation coefficient values, are depicted in Table 1. Statistically significant relations were observed between resilience and coronavirus anxiety, persistent thinking, perceived stress, and well-being; between coronavirus anxiety and persistent thinking, perceived stress, and well-being; between persistent thinking and perceived stress and well-being; and between perceived stress and well-being. In addition, a significant association was observed between age and resilience (r = 0.14; p < 0.010), perceived stress (r = −0.15; p < 0.010), and well-being (r = 0.13; p < 0.010). In this study, sex did not have a statistically significant impact on the controlled variables.
Table 1.
Descriptive statistics and correlations (n = 1758).
| M (SD) | Min | Max | 1. | 2. | 3. | 4. | |
|---|---|---|---|---|---|---|---|
| 1. Resilience | 18.64 (5.28) | 6 | 30 | 1 | |||
| 2. Coronavirus anxiety | 1.59 (2.95) | 0 | 20 | −0.18 *** | 1 | ||
| 3. Persistent thinking | 3.03 (3.18) | 0 | 16 | −0.17 *** | 0.54 *** | 1 | |
| 4. Perceived stress | 173.03 (123.69) | 0 | 500 | −0.29 *** | 0.36 *** | 0.44 *** | 1 |
| 5. Well-being | 13.72 (5.72) | 0 | 25 | 0.38 *** | −0.23 *** | −0.31 *** | −0.48 *** |
*** p < 0.001.
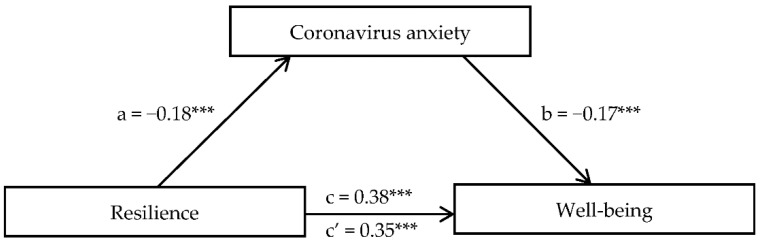
Bootstrap sampling analysis (5000) with a 95% confidence interval displayed significant partial mediators for the relationship between resilience and well-being. An important mediator was coronavirus anxiety, persistent thinking, and perceived stress. The total effect (c path) amounted to β = 0.38 (t = 15.89, p < 0.001; R2 = 0.15). In the case of coronavirus anxiety, the regression coefficient of the independent variable on the mediator (a path) amounted to β = −0.18 (t = −7.85, p < 0.001; R2 = 0.03). The mediator regression coefficient on the dependent variable with simultaneous control of the independent variable (b path) amounted to β = −0.17 (t = −7.54, p < 0.001; R2 for the entire model = 0.17). Mediation decreased the strength of the relationship between resilience and mental well-being in a direct effect (c′ path), amounting to β = 0.35 (t = 15.89, p < 0.001). The a path for persistent thinking totaled β = −0.17 (t = −7.28, p < 0.001; R2 = 0.03), the b path totaled β = −0.25 (t = −11.79, p < 0.001; R2 for the entire model = 0.21), and the c′ path totaling β = 0.34 (t = 15.69, p < 0.001). The a path for perceived stress totaled β = −0.29 (t = −12.82, p < 0.001; R2 = 0.09), the b path totaled β = −0.41 (t = −19.45, p < 0.001; R2 for the entire model = 0.30), and the c′ path totaled β = 0.26 (t = 12.55, p < 0.001). The significance level for the effects is presented in Table 2. To illustrate the mediation pattern, Figure 1 shows the relationship of resilience and well-being with coronavirus anxiety as a mediator.
Table 2.
Mediating role of coronavirus anxiety, persistent thinking, and perceived stress in relationship between resilience and well-being (n = 1758).
| a Path | b Path | c Path | c′ Path | Indirect Effect and B (SE) | 95% CI Lower Upper | |
|---|---|---|---|---|---|---|
| Resilience → Coronavirus anxiety → Well-being | −0.18 *** | −0.17 *** | 0.38 *** | 0.35 *** | 0.031 (0.006) | 0.020; 0.043 |
| Resilience → Persistent thinking → Well-being | −0.17 *** | −0.25 *** | 0.38 *** | 0.34 *** | 0.044 (0.007) | 0.030; 0.058 |
| Resilience → Perceived stress → Well-being | −0.29 *** | −0.41 *** | 0.38 *** | 0.26 *** | 0.119 (0.010) | 0.099; 0.141 |
*** p < 0.001; a path effect of independent variable on mediator; b path effect of mediator on dependent variable; c path effect of independent variable on dependent variable; c′ path direct effect of independent variable on dependent variable while controlling for mediator.
Figure 1.
Coronavirus anxiety as mediator in relationship between resilience and well-being. (*** p ≤ 0.001).
4. Discussion
The main goal of this paper was to investigate potential mental health mediators in the relationship between resilience and well-being. Although early studies looked at this relationship [67,68,69], there is a lack of studies assessing the mediating role of anxiety, aggravating stress, and persistent thinking in connection with the pandemic. The first finding shows that anxiety over COVID-19 partially mediates the relationship between resilience and well-being, which supports our first hypothesis (H1). The second hypothesis (H2) was also confirmed. Obsessive thinking about COVID-19 partially mediates the relationship between resilience and well-being. The third hypothesis (H3), that perceived stress in a pandemic might mediate the relationship between resilience and well-being, is also confirmed. For this reason, by preventing the development of COVID-19 anxiety, obsessive thoughts, and burdensome stress, resilience helps protect well-being. Therefore, it should be said that building resilience helps in coping with stress, persistent thoughts, and anxiety caused by COVID-19. In other words, resilience minimizes the anxiety, obsessive thinking, and burdensome stress of a pandemic that disrupt daily functioning. The obtained data seem to confirm the previous findings, which indicated that resilience is a helpful resource in protecting mental health. The positive psychological approach assumes that resilience is a human strength and that instead of treating mental disorders, developing psychological strength is an alternative way to protect mental health [51,57,58,70]. So far, it has been shown that intervention programs focused on positive psychology reduce, inter alia, stress and anxiety and increase aspects of health [71,72,73]. Taking the above into account, our research findings are consistent with previous theoretical knowledge in the field of positive psychology, as well as with the results of experimental and other cross-sectional studies [47,48,74,75].
We found resilience to be a wellness-enhancing construct that may have temporal or long-term psychological consequences, and tested the mediating effects of anxiety, stress, and obsessive thinking on the relationship between resilience and well-being. Although mediation studies do not directly test causality, they are very fruitful in terms of providing data that help change the therapeutic or interventional approach [76]. Our report is an important contribution to the scope of research to date on health-related psychological factors, taking into account positive and negative indicators in the general population. Through general population research, this study complements previous research in which the effects of COVID-19 have generally been studied among healthcare professionals [77].
This study also looked at the relationship between resilience and mental health. Resilience was moderately positively associated with well-being and negatively and weakly associated with anxiety, obsessive thinking, and perceived stress. Our research results confirm earlier research findings [35,49,54,78,79,80], which indicate a positive role of resilience in terms of well-being and buffering in terms of negative health aspects, such as perceived stress, anxiety, or persistent thinking. Moreover, a significant positive relationship was observed between age and resilience as well as age and well-being. Age was also negatively related to perceived stress, which corresponds to previous findings.
It is worth noting that the average results in terms of resilience were comparable to the Polish adaptation studies conducted by Konaszewski and colleagues [65]. Although research so far has shown a lower level of resilience during the COVID-19 pandemic, our data were collected during the period of relaxed government restrictions. It was also influenced by a decrease in infections, hospitalizations, and deaths. Moving within the country has become permissible, as well as physical exercise outside, praying in small groups, and meeting with loved ones. These factors, according to PeConga and colleagues [37,38], can moderate the level of resilience during a pandemic. In the studied population, the resilience result can be described as average. On the other hand, the result in terms of well-being shows a relatively low level. Scores below 13 indicate depressed mood or even a depressive state [61]. Poor mental well-being can make it difficult for individuals to use psychological resources to deal with their burdens [81]. The intensity of perceived stress indicates a feeling of low burden in the studied population [61]. The average level of anxiety about the coronavirus and persistent thinking about COVID-19 was within the fourth sten score, which proves the low intensity of these phenomena among the study participants. The obtained data correspond to previous research in this area, as high intensity of these variables is mainly observed in clinical groups [42,43].
5. Implications
In terms of practical implications, our findings offer important guidance for the development of resilience-based interventions to protect the mental health of individuals, improve their quality of life, and provide policy recommendations. The results of this study essentially indicate that developing strong psychological resources can help protect people’s mental health against the anxiety, persistent thinking, and stress caused by the spread of an infectious disease. Resources such as resilience can be enhanced through psychological intervention and therapeutic programs [82,83,84,85]. Protecting mental health with regard to the risk of infection is key to the successful fight against the pandemic. The purpose of such interventions may include the following: (a) They may help in maintaining mental health so that individuals can function with the provision of primary health care and health services in times of crisis without psychological problems. (b) They may help in identifying individuals who may be vulnerable to stressors due to their inability to cope with adversity during the pandemic. In addition to resilience-enhancing interventions, medical clinics can be effectively used to provide services to individuals who develop symptoms of mental health problems such as anxiety, obsessive thinking, and stress disorder disorders during a pandemic [50,51,52,53,54,55,56,57,58,59,60,61,62,63]. (c) Targeted psychological interventions for communities affected by the spread of an infectious disease and special support for people at high risk of mental illness are recommended, by improving the diagnosis of mental disorders and access to such interventions (especially those provided online, which reduces the risk of infection), which may ultimately help to improve people’s wellbeing.
6. Limitations
This study has some limitations. First, while questionnaire assessment is an important method of measuring mental health problems and related factors, relying solely on self-reports may run the risk of encountering a common method error. It is suggested that future research use alternative methods to complement the current findings. Second, given the cross-sectional nature of the study design, it was difficult to draw conclusions about the cause-and-effect relationship between the variables studied. Therefore, longitudinal studies are necessary to confirm the cause-and-effect sequence of relationships between the studied variables. Such data are particularly relevant to the design of mental health programs in the wake of a pandemic. In addition, the study did not assess what percentage of respondents contracted coronavirus or had a sick/deceased relative. The severity of the variables in these groups may differ from the data collected from participants in the general population. Finally, the current findings should be replicated in other clinical and non-clinical trials. Despite these limitations, these results may shed light on a possible underlying mechanism between resilience and well-being by considering the mediating role of stress, obsessive thinking, and anxiety. The results may also point to the direction of future research to investigate the relationship between resilience and mental health in terms of both negative and positive indicators, and provide opportunities for implementing resilience-based programs.
7. Conclusions
Protecting people’s mental health from the consequences of COVID-19 is currently one of the most psychologically and socially challenging issues. The results of the present study clearly indicate that resilience as a protective factor is associated with reduced anxiety over COVID-19, perceived stress burden, obsessive thoughts about the pandemic, and increased well-being of individuals. In other words, resilience plays an important role in minimizing negative and enhancing positive health indicators in the face of challenging life events. Thus, it is worthwhile to develop individuals’ psychological resources by strengthening emotional, cognitive, mental, physical, and spiritual resilience, among other aspects. Training in these areas can improve resilience and well-being and reduce stress and anxiety by teaching individuals to view life’s inevitable challenges as opportunities.
Author Contributions
Conceptualization, J.S., K.K. and S.S.; methodology, K.K., S.S. and J.S.; formal analysis, K.K., S.S., J.S., P.P.D. and J.M.; writing—original draft preparation, K.K., S.S., J.S., P.P.D. and J.M.; writing—review and editing, K.K., S.S., J.S., P.P.D. and J.M.; statistical analysis, K.K. and S.S.; supervision, J.S., K.K. and S.S.; project administration, J.S., S.S. and K.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
All subjects gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Witten/Herdecke University (#15/IV/2020).
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
All authors declare they have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang C., Zhao H. The Impact of COVID-19 on Anxiety in Chinese University Students. Front. Psychol. 2020;11:1168. doi: 10.3389/fpsyg.2020.01168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bendau A. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:283–291. doi: 10.1007/s00406-020-01171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dymecka J., Gerymski R., Machnik-Czerwik A. How does stress affect life satisfaction during the COVID-19 pandemic? Moderated mediation analysis of sense of coherence and fear of coronavirus. Psychol. Health Med. 2021;31:1–9. doi: 10.1080/13548506.2021.1906436. [DOI] [PubMed] [Google Scholar]
- 4.Dobrakowski P.P., Skalski S., Surzykiewicz J., Muszyńska J., Konaszewski K. Religious Coping and Life Satisfaction during the COVID-19 Pandemic among Polish Catholics. The Mediating Effect of Coronavirus Anxiety. J. Clin. Med. 2021;10:4865. doi: 10.3390/jcm10214865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winzer R., Lindblad F., Sorjonen K., Lindberg L. Positive versus negative mental health in emerging adulthood: A national cross-sectional survey. BMC Public Health. 2014;14:1238. doi: 10.1186/1471-2458-14-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Westerhof G.J., Keyes C.L.M. Mental Illness and Mental Health: The Two Continua Model across the Lifespan. J. Adult Dev. 2009;17:110–119. doi: 10.1007/s10804-009-9082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Langford R., Bonnell C.P., Jones H.E., Pouliou T., Murphy S.M., Waters E., Komro K.A., Gibbs L.F., Magnus D., Campbell R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement. Cochrane Database Syst. Rev. 2014;4:CD008958. doi: 10.1002/14651858.CD008958.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Headey B., Kelley J., Wearing A. Dimensions of mental health: Life satisfaction, positive affect, anxiety and depression. Soc. Indic. Res. 1993;29:63–82. doi: 10.1007/BF01136197. [DOI] [Google Scholar]
- 9.Richardson G.E. The metatheory of resilience and resiliency. J. Clin. Psychol. 2002;58:307–321. doi: 10.1002/jclp.10020. [DOI] [PubMed] [Google Scholar]
- 10.Bonanno G.A., Mancini A.D. The Human Capacity to Thrive in the Face of Potential Trauma. Pediatrics. 2008;121:369–375. doi: 10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- 11.Fletcher D., Sarkar M. Psychological resilience: A review and critique of definitions, concepts, and theory. Eur. Psychol. 2013;18:12–23. doi: 10.1027/1016-9040/a000124. [DOI] [Google Scholar]
- 12.Ong A.D., Bergeman C.S., Bisconti T.L., Wallace K.A. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J. Pers. Soc. Psychol. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- 13.Collins P.Y. Grand challenges in global mental health. Nature. 2011;475:27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M., Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health. 2020;16:57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salari N., Khazaie H., Hosseinian-Far A., Khaledi-Paveh B., Kazeminia M., Mohammadi M., Shohaimi S., Daneshkhah A., Eskandari S. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Hum. Resour. Health. 2020;18:1–14. doi: 10.1186/s12960-020-00544-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. 2020;291:113190. doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry. 2020;51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arora A., Jha A.K., Alat P., Das S.S. Understanding coronaphobia. Asian J. Psychiatry. 2020;54:102384. doi: 10.1016/j.ajp.2020.102384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor S. COVID stress syndrome: Concept, structure, and correlates. Depress. Anxiety. 2020;37:706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee S.A., Jobe M.C., Mathis A.A., Gibbons J.A. Incremental validity of coronaphobia: Coronavirus anxiety explains depression, generalized anxiety, and death anxiety. J. Anxiety Disord. 2020;74:102268. doi: 10.1016/j.janxdis.2020.102268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morganstein J.C., Ursano R.J. Ecological Disasters and Mental Health: Causes, Consequences, and Interventions. Front. Psychiatry. 2020;11:1. doi: 10.3389/fpsyt.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheung Y.T., Chau P.H., Yip P.S.F. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- 25.Zou P., Sun L., Yang W., Zeng Y., Chen Q., Yang H., Zhou N., Zhang G., Liu J., Li Y., et al. Associations between negative life events and anxiety, depressive, and stress symptoms: A cross-sectional study among Chinese male senior college students. Psychiatry Res. 2018;270:26–33. doi: 10.1016/j.psychres.2018.09.019. [DOI] [PubMed] [Google Scholar]
- 26.Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promot. Int. 1996;11:11–18. doi: 10.1093/heapro/11.1.11. [DOI] [Google Scholar]
- 27.Zimmerman M.A. Resiliency Theory: A Strengths-Based Approach to Research and Practice for Adolescent Health. Sage Publications; Los Angeles, CA, USA: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Länsimies H., Pietilä A.-M., Hietasola-Husu S., Kangasniemi M. A systematic review of adolescents’ sense of coherence and health. Scand. J. Caring Sci. 2017;31:651–661. doi: 10.1111/scs.12402. [DOI] [PubMed] [Google Scholar]
- 29.Edward K.-L. Resilience: A Protector from Depression. J. Am. Psychiatr. Nurses Assoc. 2005;11:241–243. doi: 10.1177/1078390305281177. [DOI] [Google Scholar]
- 30.Luthar S.S., Cicchetti D., Becker B. Research on Resilience: Response to Commentaries. Child. Dev. 2000;71:573–575. doi: 10.1111/1467-8624.00168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sominsky L., Walker D.W., Spencer S.J. One size does not fit all–Patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity of disease matters. Brain. Behav. Immun. 2020;87:1. doi: 10.1016/j.bbi.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Blanc J., Rahill G.J., Laconi S., Mouchenik Y. Religious Beliefs, PTSD, Depression and Resilience in Survivors of the 2010 Haiti Earthquake. J. Affect. Disord. 2016;190:697–703. doi: 10.1016/j.jad.2015.10.046. [DOI] [PubMed] [Google Scholar]
- 33.Hansel T.C., Osofsky J.D., Osofsky H.J., Friedrich P. The Effect of Long-Term Relocation on Child and Adolescent Survivors of Hurricane Katrina. J. Trauma. Stress. 2013;26:613–620. doi: 10.1002/jts.21837. [DOI] [PubMed] [Google Scholar]
- 34.Li F., Luo S., Mu W., Li Y., Ye L., Zheng X., Xu B., Ding Y., Ling P., Zhou M., et al. Effects of sources of social support and resilience on the mental health of different age groups during the COVID-19 pandemic. BMC Psychiatry. 2021;21:1–14. doi: 10.1186/s12888-020-03012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hou W.K., Tong H., Liang L., Li T.W., Liu H., Ben-Ezra M., Goodwin R., Lee T.M.-C. Probable anxiety and components of psychological resilience amid COVID-19: A population-based study. J. Affect. Disord. 2021;282:594–601. doi: 10.1016/j.jad.2020.12.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skalski S., Konaszewski K., Dobrakowski P., Surzykiewicz J., Lee S.A. Pandemic grief in Poland: Adaptation of a measure and its relationship with social support and resilience. Curr. Psychol. 2021:1–9. doi: 10.1007/s12144-021-01731-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.PeConga E.K., Gauthier G.M., Holloway A., Walker R.S.W., Rosencrans P.L., Zoellner L.A., Bedard-Gilligan M. Resilience is spreading: Mental health within the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy. 2020;12:S47–S48. doi: 10.1037/tra0000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.PeConga E.K., Thøgersen M.H. Post-traumatic stress disorder, depression, and anxiety in adult Syrian refugees: What do we know? Scand. J. Public Health. 2020;48:677–687. doi: 10.1177/1403494819882137. [DOI] [PubMed] [Google Scholar]
- 39.Chong M.-Y., Wang W.-C., Hsieh W.-C., Lee C.-Y., Chiu N.-M., Yeh W.-C., Huang O.-L., Wen J.-K., Chen C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- 40.Wheaton M., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological Predictors of Anxiety in Response to the H1N1 (Swine Flu) Pandemic. Cogn. Ther. Res. 2011;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- 41.Yip P.S., Cheung Y.T.D., Chau P.H., Law Y. The Impact of Epidemic Outbreak. Crisis. 2010;31:86–92. doi: 10.1027/0227-5910/a000015. [DOI] [PubMed] [Google Scholar]
- 42.Skalski S., Uram P., Dobrakowski P., Kwiatkowska A. The link between ego-resiliency, social support, SARS-CoV-2 anxiety and trauma effects. Polish adaptation of the Coronavirus Anxiety Scale. Pers. Individ. Differ. 2021;171:110540. doi: 10.1016/j.paid.2020.110540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skalski S., Uram P., Dobrakowski P., Kwiatkowska A. Thinking too much about the novel coronavirus. The link between persistent thinking about COVID-19, SARS-CoV-2 anxiety and trauma effects. Curr. Issues Pers. Psychol. 2020;8:169–174. [Google Scholar]
- 44.Langlois F., Freeston M.H., Ladouceur R. Differences and similarities between obsessive intrusive thoughts and worry in a non-clinical population: Study 1. Behav. Res. Ther. 2000;38:157–173. doi: 10.1016/S0005-7967(99)00027-3. [DOI] [PubMed] [Google Scholar]
- 45.Beck A.T. Cognitive approaches to panic disorder: Theory and therapy. In: Rachman S., Maser J.D., editors. Panic: Psychological Perspectives. Lawrence Erlbaum Associates, Inc.; Mahwah, NJ, USA: 1988. pp. 91–109. [Google Scholar]
- 46.Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988;56:893. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- 47.Gustafsson H., Skoog T. The mediational role of perceived stress in the relation between optimism and burnout in competitive athletes. Anxiety Stress Coping. 2012;25:183–199. doi: 10.1080/10615806.2011.594045. [DOI] [PubMed] [Google Scholar]
- 48.Wang Q., Xu W., Ren L., Wang W., Wang Y. The relationship between hope and post-traumatic stress disorder in Chinese shidu parents: The mediating role of perceived stress. J. Affect. Disord. 2019;251:23–30. doi: 10.1016/j.jad.2019.03.049. [DOI] [PubMed] [Google Scholar]
- 49.Vinkers C.H., van Amelsvoort T., Bisson J.I., Branchi I., Cryan J.F., Domschke K., Howes O.D., Manchia M., Pinto L., de Quervain D., et al. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020;35:12–16. doi: 10.1016/j.euroneuro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen S., Bonanno G.A. Psychological adjustment during the global outbreak of COVID-19: A resilience perspective. Psychol. Trauma Theory Res. Pract. Policy. 2020;12:S51–S54. doi: 10.1037/tra0000685. [DOI] [PubMed] [Google Scholar]
- 51.Burke J., Arslan G. Positive Education and School Psychology during COVID-19 Pandemic. J. Posit. Sch. Psychol. 2020;4:137–139. doi: 10.47602/jpsp.v4i2.243. [DOI] [Google Scholar]
- 52.Mahamid F.A., Bdier D. The Association between Positive Religious Coping, Perceived Stress, and Depressive Symptoms During the Spread of Coronavirus (COVID-19) Among a Sample of Adults in Palestine: Across Sectional Study. J. Relig. Health. 2021;60:34–49. doi: 10.1007/s10943-020-01121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fuhrman S., Kalyanpur A., Friedman S., Tran N.T. Gendered implications of the COVID-19 pandemic for policies and programmes in humanitarian settings. BMJ Glob. Health. 2020;5:e002624. doi: 10.1136/bmjgh-2020-002624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Conversano C., Miniati M. Psychological distress among healthcare professionals involved in the COVID-19 emergency: Vulnerability and resilience factors. Neuropsychiatry. 2020;17:94–96. doi: 10.36131/CN20200212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jahanshahi A.A., Dinani M.M., Madavani A.N., Li J., Zhang S.X. The distress of Iranian adults during the COVID-19 pandemic—More distressed than the Chinese and with different predictors. Brain Behav. Immun. 2020;87:124–125. doi: 10.1016/j.bbi.2020.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Asmundson G.J.G., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020;71:102211. doi: 10.1016/j.janxdis.2020.102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seligman M.E. Positive psychology, positive prevention, and positive therapy. Handb. Posit. Psychol. 2002;2:3–12. [Google Scholar]
- 58.Peterson C., Seligman M.E. Character Strengths and Virtues: A Handbook and Classification. Oxford University Press; Oxford, UK: 2004. [Google Scholar]
- 59.Topp C.W., Østergaard S.D., Søndergaard S., Bech P. The WHO-5 Well-Being Index: A Systematic Review of the Literature. Psychother. Psychosom. 2015;84:167–176. doi: 10.1159/000376585. [DOI] [PubMed] [Google Scholar]
- 60.Cichoń E., Kiejna A., Kokoszka A., Gondek T., Rajba B., Lloyd C.E., Sartorius N. Validation of the Polish version of WHO-5 as a screening instrument for depression in adults with diabetes. Diabetes Res. Clin. Pract. 2020;159:107970. doi: 10.1016/j.diabres.2019.107970. [DOI] [PubMed] [Google Scholar]
- 61.Büssing A., Recchia D.R., Hein R., Dienberg T. Perceived changes of specific attitudes, perceptions and behaviors during the Corona pandemic and their relation to wellbeing. Health Qual. Life Outcomes. 2020;18:1–17. doi: 10.1186/s12955-020-01623-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee S.A., Mathis A.A., Jobe M.C., Pappalardo E.A. Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale. Psychiatry Res. 2020;290:113112. doi: 10.1016/j.psychres.2020.113112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee S.A. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain. Behav. Immun. 2020;87:97. doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 65.Konaszewski K., Niesiobędzka M., Surzykiewicz J. Validation of the Polish version of the Brief Resilience Scale (BRS) PLoS ONE. 2020;15:e0237038. doi: 10.1371/journal.pone.0237038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hayes A.F. Methodology in the Social Sciences: Introduction to Mediation, Moderation, and Conditional Process. Analysis: A Regression-Based Approach. Guilford Press; New York, NY, USA: 2013. [Google Scholar]
- 67.Cosco T.D., Howse K., Brayne C. Healthy ageing, resilience and wellbeing. Epidemiol. Psychiatr. Sci. 2017;26:579–583. doi: 10.1017/S2045796017000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith J., Hollinger-Smith L. Savoring, resilience, and psychological well-being in older adults. Aging Ment. Health. 2014;19:192–200. doi: 10.1080/13607863.2014.986647. [DOI] [PubMed] [Google Scholar]
- 69.Burack J., Blidner A., Flores H., Fitch T. Constructions and Deconstructions of Risk, Resilience and Wellbeing: A Model for Understanding the Development of Aboriginal Adolescents. Australas. Psychiatry. 2007;15:S18–S23. doi: 10.1080/10398560701701148. [DOI] [PubMed] [Google Scholar]
- 70.Benson P.L., Scales P.C., Hamilton S.F., Sesma A., Jr. Positive Youth Development: Theory, Research, and Applications. In: Damon W., RM L., editors. Handbook of Child Psychology. 6th ed. John Wiley & Sons; Hoboken, NJ, USA: 2007. [Google Scholar]
- 71.Turner K., McCarthy V.L. Stress and anxiety among nursing students: A review of intervention strategies in literature between 2009 and 2015. Nurse Educ. Pract. 2017;22:21–29. doi: 10.1016/j.nepr.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 72.Haggerty R.J., Sherrod L.R., Garmezy N., Rutter M. Stress, Risk, and Resilience in Children and Adolescents: Processes, Mechanisms, and Interventions. Cambridge University Press; Cambridge, UK: 1996. [Google Scholar]
- 73.Melnyk B.M., Small L., Morrison-Beedy D., Strasser A., Spath L., Kreipe R., Crean H., Jacobson D., Kelly S., O’Haver J. The COPE Healthy Lifestyles TEEN Program: Feasibility, Preliminary Efficacy, & Lessons Learned from an After School Group Intervention with Overweight Adolescents. J. Pediatr. Health Care. 2007;21:315–322. doi: 10.1016/j.pedhc.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 74.Satici S.A. Psychological vulnerability, resilience, and subjective well-being: The mediating role of hope. Pers. Individ. Differ. 2016;102:68–73. doi: 10.1016/j.paid.2016.06.057. [DOI] [Google Scholar]
- 75.Karreman A., Vingerhoets A.J. Attachment and well-being: The mediating role of emotion regulation and resilience. Pers. Individ. Differ. 2012;53:821–826. doi: 10.1016/j.paid.2012.06.014. [DOI] [Google Scholar]
- 76.Windgassen S., Goldsmith K., Moss-Morris R., Chalder T. Establishing how psychological therapies work: The importance of mediation analysis. J. Ment. Health. 2016;25:93–99. doi: 10.3109/09638237.2015.1124400. [DOI] [PubMed] [Google Scholar]
- 77.Chmielewski J.P., Raczek M., Puścion M., Chmielowiec B., Pawlas N., Luszczki J.J. COVID-19, wywołany przez wirus SARS-CoV-2, jako choroba zawodowa osób wykonujących zawody medyczne. Med. Ogólna Nauk. O Zdrowiu. 2021;27:235–243. doi: 10.26444/monz/139319. [DOI] [Google Scholar]
- 78.Sagone E., De Caroli M.E. Relationships between Psychological Well-being and Resilience in Middle and Late Adolescents. Procedia-Soc. Behav. Sci. 2014;141:881–887. doi: 10.1016/j.sbspro.2014.05.154. [DOI] [Google Scholar]
- 79.Bajaj B., Pande N. Mediating role of resilience in the impact of mindfulness on life satisfaction and affect as indices of subjective well-being. Pers. Individ. Differ. 2016;93:63–67. doi: 10.1016/j.paid.2015.09.005. [DOI] [Google Scholar]
- 80.Souri H., Hasanirad T. Relationship between Resilience, Optimism and Psychological Well-Being in Students of Medicine. Procedia-Soc. Behav. Sci. 2011;30:1541–1544. doi: 10.1016/j.sbspro.2011.10.299. [DOI] [Google Scholar]
- 81.Takebayashi Y., Tanaka K., Sugiura Y., Sugiura T. Well-Being and Generalized Anxiety in Japanese Undergraduates: A Prospective Cohort Study. J. Happiness Stud. 2018;19:917–937. doi: 10.1007/s10902-017-9852-3. [DOI] [Google Scholar]
- 82.Ritchie S., Wabano M.J., Russell K., Enosse L., Young N. Promoting resilience and wellbeing through an outdoor intervention designed for Aboriginal adolescents. Rural Remote Health. 2014;14:2523. [PubMed] [Google Scholar]
- 83.Davydov D.M., Stewart R., Ritchie K., Chaudieu I. Resilience and mental health. Clin. Psychol. Rev. 2010;30:479–495. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 84.Dunn L.B., Iglewicz A., Moutier C. A Conceptual Model of Medical Student Well-Being: Promoting Resilience and Preventing Burnout. Acad. Psychiatry. 2008;32:44–53. doi: 10.1176/appi.ap.32.1.44. [DOI] [PubMed] [Google Scholar]
- 85.Haase J.E. The Adolescent Resilience Model as a Guide to Interventions. J. Pediatr. Oncol. Nurs. 2004;21:289–299. doi: 10.1177/1043454204267922. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.