Abstract
Introduction: The rapid use of an automated external defibrillator (AED) is crucial for increased survival after an out-of-hospital cardiac arrest (OHCA). Many factors could play a role in limiting the chance of an AED use. We aimed to verify the situation regarding AED legislation, the AED mapping system and first responders (FRs) equipped with an AED across European countries. Methods: We performed a survey across Europe entitled “European Study about AED Use by Lay Rescuers” (ENSURE), asking the national coordinators of the European Registry of Cardiac Arrest (EuReCa) program to complete it. Results: Nineteen European countries replied to the survey request for a population covering 128,297,955 inhabitants. The results revealed that every citizen can use an AED in 15 countries whereas a training certificate was required in three countries. In one country, only EMS personnel were allowed to use an AED. An AED mapping system and FRs equipped with an AED were available in only 11 countries. The AED use rate was 12–59% where AED mapping and FR systems were implemented, which was considerably higher than in other countries (0–7.9%), reflecting the difference in OHCA survival. Conclusions: Our survey highlighted a heterogeneity in AED legislation, AED mapping systems and AED use in Europe, which was reflected in different AED use and survival.
Keywords: out-of-hospital cardiac arrest (OHCA), automated external defibrillator (AED) system, legislation, first responders
1. Introduction
Early cardiopulmonary resuscitation (CPR) and a rapid use of an automated external defibrillator (AED) are essential steps to improve survival after an out-of-hospital cardiac arrest (OHCA), as highlighted in the “Chain of Survival” [1,2]. Early defibrillation increases not only the rate of return of spontaneous circulation (ROSC) and survival but also a favorable neurological outcome at the hospital discharge, irrespective of it being a witnessed event, bystander CPR or an initial rhythm [3,4,5]. AED use by a bystander or first responders (FRs; i.e., police officers, firefighters, off-duty medical personnel and trained lay persons alerted when a patient experiences an OHCA nearby) before the arrival of emergency medical service (EMS) personnel is of a primary importance particularly when considering that the earlier the defibrillation, the higher the chance of survival [6,7,8]. This concept was proven in the early 2000s, when the public-access defibrillation (PAD) trial was carried out in the USA involving security officers after cardiac arrests in casinos [9] and has been continuously reinforced by numerous scientific publications subsequently released [10,11]. A recent meta-analysis of six observational studies, without a critical risk of bias, confirmed that bystander AED use was associated with a higher survival to the hospital discharge (all rhythms OR: 1.73 (95% CI: 1.36, 2.18); shockable rhythms OR: 1.66 (95% CI: 1.54, 1.79)) and a favorable neurological outcome (all rhythms OR: 2.12 (95% CI: 1.36, 3.29); shockable rhythms OR: 2.37 (95% CI: 1.58, 3.57)) [12].
Considering that no particular skills are needed to correctly use an AED [13] and no risks for rescuers are present [14,15], the guidelines have highlighted from 2015 onwards [16,17] that the use of an AED even by untrained lay persons must be encouraged.
However, despite the well-established favorable role on survival and the resulting guideline recommendations, the rate of AED use is quite heterogenous among the different countries worldwide, including in Europe [18] where it is very low in many countries. Many factors could play a role in limiting the chance of AED use such as the availability of the AED, the presence of an FR alerting system and also local laws regulating the use of an AED by a bystander [19].
Therefore, we aimed to verify the situation regarding the legislation related to the use of an AED, an AED mapping system and the eventual dispatch of a first responder equipped with an AED across European countries. We also aimed to assess the eventual differences in the rates of AED use and the outcomes of patients among the countries according to the different organizational and legislation settings.
2. Materials and Methods
We performed a survey across Europe entitled “European Study About AED Use by Lay Rescuers” (ENSURE) asking primarily the 29 national coordinators of the European Registry of Cardiac Arrest (EuReCa) [20] program to fill in the questionnaire, referring to the EuReCa TWO period (October 2017–December 2017). The study was endorsed by the European Resuscitation Council (ERC) Research NET and by the Italian Resuscitation Council (IRC).
The questionnaire was divided into different parts (Supplementary File S1). The first part comprised general questions regarding the type of registry and the population covered; the second part focused on real-life data about OHCAs collected during the EuReCa TWO period and the third part queried the organizational and legislation setting both during the study period and at the time of survey completion (mid-2020). Considering the nature of the study, no further ethics approval was needed.
3. Results
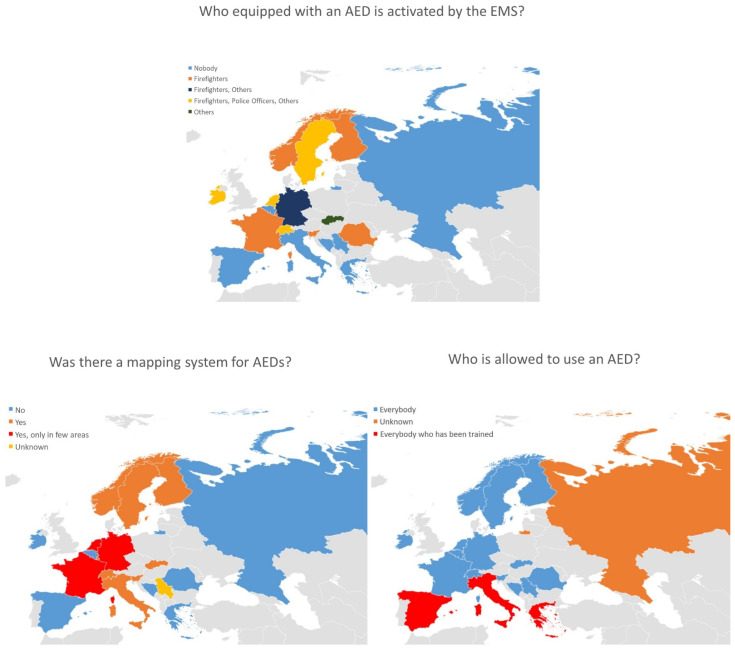
We received replies from 19 European countries out of the 29 invited. The answers referred to 10 national registries and 9 regional or provincial registries for a total population of about 128,297,955 inhabitants. Regarding AED legislation, in 15 out of 19 countries, every citizen was allowed to use an AED whereas a training certificate was required in three countries. In one country, only EMS personnel were allowed to use an AED (Table 1 and Figure 1). An AED mapping system covering the whole nation was available in only 8 out of 19 countries and it was available only in certain areas in 3 out of 19 countries. Concerning the dispatch of first responders equipped with an AED, this was available in 11 out of 19 countries (Figure 1).
Table 1.
AED legislation in different European countries updated in 2020 and the eventual differences compared with the EuReCa TWO period (late 2017).
| Country | Is There Any Special Legislation on the Use of AEDs? | Who Is Allowed to Use an AED? | Has the Legislation Changed after December 2017? | Are There Legislation Differences in the Different Regions of Your Country? | Was There An aed Mapping System in Your Region/Country in the Study Period? | Did the (EMS) Activate FRS Equipped with an Aed in Your Region/Country in the Study Period? |
|---|---|---|---|---|---|---|
| Belgium | Yes | Everybody | No | No | No | No |
| Bosnia and Herzegovina | No | Everybody | No | No | No | No |
| Finland | No | Everybody | No | No | Yes | Yes |
| France | Yes | Everybody | Yes ** | No | Yes, only in some areas | Yes |
| Germany | No | Everybody | No | No | Yes, only in a few areas | Yes, only in a few areas |
| Greece | Yes | Everybody trained * | No | No | No | No |
| Ireland | No | Everybody | No | No | No | Yes |
| Italy | Yes | Everybody trained | No *** | No | Yes | No |
| Luxembourg | Yes | Everybody | No | No | Yes | Yes |
| The Netherlands | No | Everybody | No | No | Yes, only in a few areas | Yes |
| Norway | No | Everybody | No | No | Yes | Yes, only in a few areas |
| Romania | Yes | Everybody | No | No | No | Yes |
| Russian Federation | No | EMS providers only | No | No | No | No |
| Serbia | No | Everybody | No | No | Unknown | No |
| Slovakia | No | Everybody | No | No | Yes | Yes |
| Slovenia | Yes | Everybody | No | No | Yes | Yes, only in a few areas |
| Spain | Yes | Everybody trained | No | No | No | No |
| Sweden | No | Everybody | No | No | Yes | Yes |
| Switzerland | No | Everybody | No | No | Yes | Yes |
* In Greece, the law allows only trained lay persons to use an AED but it also establishes that anyone who offers immediate help in goodwill to a cardiac arrest victim cannot be prosecuted. ** A “Good Samaritan” law allowing all citizens to use an AED was issued in July 2020 in France. *** In Italy, the Parliament approved a “Good Samaritan” law in late July 2021, which is currently being implemented.
Figure 1.
Graphical representation across the different European countries regarding who is, equipped with an AED, activated by the EMS, if there was an AED mapping system and who is allowed to use an AED.
The data regarding the number of OHCA occurred, the use of an AED before EMS arrival, the ROSC and survival across the different european countries during the EuReCa TWO period (October 2017–December 2017) are presented in Table 2.
Table 2.
Number of OHCAs, AED use, ROSCs and survival across the different European countries during the EuReCa TWO period (October 2017–December 2017).
| Country | Regional or National Registry | Population Covered (n) | Name of the Registry | OHCAs with EMS Attempted Resuscitation Occurring in the Period Oct 2017–Dec 2017 (EuReCa TWO Period) (n) | OHCAs in the Utstein Comparator Group (UCG) * (n, %) | OHCAs in Which an AED Was Attached before EMS Arrival (n, %) | OHCAs in Which the AED Was Attached by Firefighters, Police Officers or Other FRs (n, %) | OHCAs in Which the AED Was Attached by Bystanders (n, %) | OHCAs in Which an AED Was Attached before EMS Arrival and a Shock Was Delivered (n) | OHCAs in Which the Shock Was Delivered by Firefighters, Police Officers or Other FRs (%) | OHCAs in Which the Shock Was Delivered by Bystanders (%) | ROSC in the UCG (n, %) | Survival at Discharge in the UCG (n, %) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Belgium | National | 2,834,000 | Belgian Cardiac Registry (B-CAR) | 377 | 57 (15.1) | 26 (6.9) | 22 (84.6) | 4 (15.4) | 16 (4.2) | 12 (75) | 4 (25) | 31 (54.4) | 16 (28.1) |
| Bosnia and Herzegovina | Regional | 110,979 | Utstein Resuscitation Registry | 22 | 1 (4.5) | 0 (0) | N/A | N/A | 0 (0) | N/A | N/A | 0 (0) | 0 (0) |
| Finland | Regional | 655,395 | Helsinki out-of-hospital cardiac arrest registry | 76 | 19 (25) | 6 (7.9) | N/A | N/A | 3 (3.9) | N/A | N/A | 13 (68) | 7 (37) |
| France | National | 17,833,002 | Electronic Registry of Cardiac Arrests (RéAC) | 2604 | 177 (6.8) | 2066 (79.3) ** | 1874 (90.7) | 192 (9.3) | 418 (16) | 368 (88) | 50 (12) | 95 (53.7) | 40 (22.6) |
| Germany | National | 26,600,000 | Deutsches Reanimations Register (German Resuscitation Registry) | 6969 | 524 (7.5) | 0 (0) | N/A | N/A | 0 (0) | N/A | N/A | 372 (71) | 30 (17) |
| Greece | Regional | 1,500,000 | National Center For Emergency Care (Northern Greece, Thessaloniki) | 71 | 22 (31) | 5 (7) | N/A | N/A | 1 (1.4) | N/A | N/A | 8 (36) | 1 (4.6) |
| Ireland | National | 4,757,976 | Out-of-Hospital Cardiac Arrest Register (OHCAR) | 594 | 72 (12.1) | 21 (3.5) | 17 (81) | 4 (19) | 21 (3.5) | 15 (71.4) | 6 (28.6) | 28 (39) | 18 (25) |
| Italy | Regional | 545,810 | Lombardia Cardiac Arrest Registry (LombardiaCARe) | 152 | 17 (11.2) | 4 (2.6) | 0 (0) | 4 (100) | 2 (1.3) | 0 (0) | 2 (100) | 9 (52.9) | 3 (17.6) |
| Luxembourg | National | 602,005 | Cardlux | 140 | 24 (17.1) | 12 (8.6) | N/A | N/A | 5 (3.6) | N/A | N/A | 10 (41.6) | 4 (16.6) |
| The Netherlands | Regional | 2,578,552 | Amsterdam Resuscitation Studies (ARREST) | 314 | 81 (25.8) | 183 (58.2) | 146 (79.8) | 37 (20.2) | 74 (23.6) | 52 (70) | 22 (30) | 5 (69) | 33 (40.7) |
| Norway | National | 5,336,494 | Norwegian Cardiac Arrest Registry | 848 | 95 (11.2) | 103 (12.1) | 57 (55.3) | 46 (44.7) | 30 (3.5) | N/A | N/A | 56 (59) | 42 (44.2) |
| Romania | National | 4,086,753 | Registrul Roman al Stopului Cardiac (Romanian Registry of Cardiac Arrest) | 512 | 30 (5.8) | 27 (5.3) | 27 (100) | 0 (0) | 12 (2.3) | 12 (100) | 0 (0) | N/A | N/A |
| Russian Federation | Regional | 1,913,731 | Crimean Out-of-Hospital Cardiac Arrest and Resuscitation Registry (COHCARR) *** | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Serbia | National | 1,227,069 | EuReCa Srbija | 409 | 42 (10.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 8 (19.1) | 16 (38) |
| Slovakia | Other | 3,300,000 | Ad hoc for EuReCa TWO | 693 | 93 (13.4) | 6 (0.9) | N/A | N/A | 2 (0.3) | N/A | N/A | 45 (48.4) | 24 (25.8) |
| Slovenia | Other | 1,191,479 | Ad hoc for EuReCa TWO | 178 | 35 (19.7) | 13 (7.3) | 10 (76.9) | 3 (23.1) | 11 (6.2) | 8 (73) | 2 (18) | 22 (63) | 11 (31.4) |
| Spain | National | 42,750,768 | Out-of-Hospital Spanish Registry of Cardiac Arrest (OHSCAR) | 2148 | 342 (15.9) | 75 (3.5) | 44 (58.7) | 31 (41.3) | 38 (1.8) | 13 (34.2) | 25 (65.8) | 209 (61.1) | 100 (29.2) |
| Sweden | National | 10,120,242 | The Swedish Registry of Cardiopulmonary Resuscitation (SRCR) | 1466 | 171 (11.7) | 336 (25) | 269 (80) | 44 (13.1) | 84 (5.7) | 46 (55) | 27 (32) | 96 (56.1) | 101 (59.1) |
| Switzerland | Regional | 353,700 | Ticino Registry Cardiac Arrest (TiReCA) | 53 | 9 (17) | 19 (35.8) | 12 (63.1) | 7 (36.8) | 2 (3.8) | 1 (50) | 1 (50) | 4 (44.4) | 2 (22.2) |
AED: automated external defibrillator; OHCA: out-of-hospital cardiac arrest. * Utstein comparator group: bystander-witnessed for the first shockable rhythm. ** In France, the emergency medical system is by definition medicalized. Firefighters are trained in BLS and routinely alerted in case of an OHCA but they are considered not to be part of the EMS response and, therefore, are classified as first responders. *** The Crimean Out-of-Hospital Cardiac Arrest and Resuscitation Registry (COHCARR) started to collect data from 1 January 2018 onwards.
4. Discussion
Our study has presented data regarding the legislations regulating AED use, the AED mapping systems and AED use across Europe, highlighting a great heterogeneity across European countries. This is reflected in important variations in AED use and OHCA patient survival in different countries.
4.1. The Importance of the Legislation Rule
It is reasonable to assume that the rate of AED use is influenced by the type of legislation regulating the use of an AED by lay persons [19] although evidence in the literature on this topic is limited. Notably, in those countries where a certificate is needed for lay persons to be allowed to use an AED, the use of an AED is low (between 2.4% and 5%) [21,22] compared with those countries where a “Good Samaritan” law is in force and all citizens can freely use an AED if necessary (about 15–20% of an AED use before EMS arrival) [10,23,24,25]. Concerning Europe, the last survey about legislation rules on AED use dates back 11 years [26]. It highlighted that the use of an AED was allowed for all the citizens in one third of interviewed countries, for citizens with a certificate in another third and only for physicians or EMS personnel in the last third. Our study outlined that the situation has considerably improved in ten years: in about 80% of the countries, every citizen was allowed to use an AED. However, a training certificate was still required in three countries (Greece, Italy and Spain) and in one (Russia Federation) only EMS personnel were allowed to use an AED. Considering that six years have passed since the ERC 2015 guidelines were issued, we believe that the situation is quite alarming and suggests that several countries need to rapidly adhere to the recommendations allowing untrained bystanders to use an AED, thus increasing the rate of lay defibrillation and, therefore, the chance of survival of OHCA patients.
4.2. AED Mapping and First Responder Systems
The chance of receiving an early defibrillation depends on the availability of PADs [27]. Considering that the survival to discharge decreases for every minute of delay to defibrillation [17], it is crucial to retrieve an AED as soon as possible [28]. For this reason, the guidelines since 2015 have recommended that publicly accessible AEDs are registered and mapped so that dispatchers can direct CPR providers to the closest AED, optimizing the system response [29]. Our survey highlighted that an AED mapping system was available in just over half of the countries and this percentage dropped to only 40% if we considered only the countries with an AED mapping system available for the whole nation. No system mapping AEDs was available in 8 out of 19 countries. This aspect should be improved to increase the chance that an AED is brought to the scene in case of an OHCA. From a scientific point of view, the possibility of merging the location of the OHCA and the position of the AED by using both cardiac arrest registries and AED mapping systems could allow the development of new algorithms to relocate the AEDs with the intent to improve optimal coverage [30] to use more properly the AEDs already available without necessarily increasing their numbers as well as to exploit new innovative methods to get an AED to the scene such as the use of drones [31]. Furthermore, a crucial role in enhancing the possibility of providing early defibrillation is played by FRs [6,25,32,33,34]. FRs are commonly divided into “professional FRs” such as police officers, firefighters or off-duty medical personnel and “citizen FRs” meaning trained lay persons [7]. For this latter category, the only chance of using an AED depends on the availability of an AED on site and the possibility of receiving instructions from the dispatch center (or by the alerting APP) about the closest AED, stressing once again the importance of AED mapping. For the professional FRs, the situation is different because they are often equipped with an AED and can bring the defibrillator to the OHCA scene when alerted, resulting in a reduction of the time to the first defibrillation, which is associated with an increased chance of survival [35]. The effectiveness and the capability of the FR system to increase survival is already well-documented [8]. In our survey, we found that only in 11 out of 19 countries were the professional FRs alerted by the EMS equipped with an AED, stressing the need to improve this aspect throughout Europe.
4.3. Differences in AED Use, ROSC and Survival across Europe
Important differences among the countries regarding the rate of AED use before the arrival of the EMS have been already evidenced [18]. Our survey confirmed that in those countries where the law permits only trained bystanders to use an AED such as Greece, Italy and Spain, the chance of being defibrillated before the arrival of the EMS is particularly low (from 2.6 to 7%). However, the percentage of AED use before the arrival of the EMS appeared to be deeply varied across the European countries and it was low also in several countries where everybody is allowed to use an AED (e.g., Belgium, Ireland, Romania, Slovakia and Slovenia), suggesting that probably it is not only a matter of law. Our survey hinted that in countries where AED mapping and an FRs system are implemented alongside a permissive law, the rate of AED use was higher. This was particularly clear in several countries such as The Netherlands, Norway, Sweden and Switzerland, where systems to save a life were implemented many years ago [6,10,34]. In these countries, the rate of AED use was between 12 and 59%, considerably higher than in other countries (from 0 to 7.9%). All the above is perfectly in line with the latest ERC guidelines, which, for the very first time, have dedicated an entire chapter to the importance of the “Systems saving lives” [28], embracing the philosophy of the European Resuscitation Academy (ERA) and the Global Resuscitation Alliance (GRA) [36,37].
4.4. Limitations
Our study has limitations. The first is that we received data from 19 European countries; this does not represent all the countries present in Europe. However, considering that the registries included covered more than 125 million people, we believe that our study could be considered to be representative of the European situation. The second limitation is that we decided to refer, regarding OHCA data, to the EuReCa TWO period. This was chosen to consider the same time period in all the countries facilitating data retrieving and because a few registries collected data only during the EuReCa surveys, allowing an increase in the data collected for the present study. We decided to overcome this limitation by allowing the presentation of past data and to ask in the survey for the organizational and legislation setting both during the EuReCa TWO period and at the time of the survey completion (mid-2020). This allowed us to present data representing as much as possible the actual European situation. Considering this type of situation is constantly evolving, we marked the eventual subsequent changes that intervened after the survey completion, as seen in Table 1.
5. Conclusions
Our survey highlighted a great heterogeneity in terms of the legislations regulating the use of an AED, AED mapping systems and AED use across Europe, therefore limiting the OHCA survival in many European regions and countries. Considering the undoubted importance of all these three actions to maximize the chance of survival after an OHCA, we strongly suggest the following to all the European countries and their governments:
To issue a law that allow all citizens, including untrained ones, to use an AED in the case of a suspected OHCA and protecting them against any legal consequences.
To make an AED map compulsory that includes all public AEDs and that is linked to the emergency medical system dispatch center.
To implement FR systems, including both citizens trained in CPR and professional FRs (i.e., police officers, firefighters, off-duty medical personnel) possibly equipped with an AED, to increase the rate of defibrillation before the arrival of the EMS.
To unify cardiac arrest registries among European countries to harmonize data collection and better comprehend the European strategies to implement an improved OHCA survival.
Acknowledgments
The present survey was promoted by the Italian Resuscitation Council and has been endorsed by the ERC Research NET.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10215018/s1, Supplementary File S1: ENSURE study questionnaire.
Author Contributions
Conceptualization, E.B., N.B.G., G.R. and S.S.; methodology, E.B. and S.S.; formal analysis, E.B. and S.S.; investigation, H.A., V.C., A.B., R.C., D.C., C.C., J.G., A.M., P.M., O.N., M.Q., V.R., F.R.O., A.S. (Ari Salo), R.S., A.S. (Anneli Strömsöe), I.T., S.T. and J.W.; data curation, E.B.; writing—original draft preparation, E.B.; writing—review and editing, J.-T.G., B.W.B. and S.S.; supervision, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. The publication fee was covered by Italian Resuscitation Council with funds for dissemination within the “iProcureSecurity” H2020 project (Grant Agreement No 833291).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Each cardiac arrest registry that provided the data for the present study has been approved by the relevant ethics committee in accordance with its national law. No further ethics approval was required.
Informed Consent Statement
Considering the type of the study, no specific written consent was needed.
Conflicts of Interest
J.W. is member of the German Resuscitation Registry steering committee and EuReCa study management team and has no financial COIs to declare. J.-T.G. is member of the German Resuscitation Registry steering committee, EuReCa project leader and obtained funding for the Institute for Emergency Medicine, University Hospital Schleswig-Holstein from Corpuls (GS Stemple) and personal speaker fees and travel costs from ZOLL, Corpuls, Philips and Weinmann-emergency. B.W.B. is treasurer of the European Resuscitation Council (ERC), Chairman of the German Resuscitation Council (GRC), Member of the Advanced Life Support (ALS) Task Force of the International Liaison Committee on Resuscitation (ILCOR), Member of the Executive Committee of the German Interdisciplinary Association for Intensive Care and Emergency Medicine (DIVI), Founder of the “Deutsche Stiftung Wiederbelebung”, Co-Editor of “Resuscitation”, Editor of the Journal “Notfall + Rettungsmedizin” and Co-Editor of the Brazilian Journal of Anesthesiology. He received fees for lectures from the following companies: Forum für medizinische Fortbildung (FomF), Baxalta Deutschland GmbH, ZOLL Medical Deutschland GmbH, C.R. Bard GmbH, GS Elektromedizinische Geräte G. Stemple GmbH, Novartis Pharma GmbH, Philips GmbH Market DACH and Bioscience Valuation BSV GmbH. The other authors reported no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cummins R.O., Ornato J.P., Thies W.H., Pepe P.E. Improving Survival From Sudden Cardiac Arrest: The “Chain of Survival” Concept. Circ. AHA Statement. 1991;83:1831–1843. doi: 10.1161/01.cir.83.5.1832. [DOI] [PubMed] [Google Scholar]
- 2.Deakin C.D. The chain of survival: Not all links are equal. Resuscitation. 2018;126:80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Weisfeldt M.L., Sitlani C.M., Ornato J.P., Rea T., Aufderheide T.P., Davis D., Dreyer J., Hess E.P., Jui J., Maloney J., et al. Survival After Application of Automatic External Defibrillators Before Arrival of the Emergency Medical System. Evaluation in the Resuscitation Outcomes Consortium Population of 21 Million. J. Am. Coll. Cardiol. 2010;55:1713–1720. doi: 10.1016/j.jacc.2009.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kishimori T., Kiguchi T., Kiyohara K., Matsuyama T., Shida H., Nishiyama C., Kobayashi D., Okabayashi S., Shimamoto T., Hayashida S., et al. Public-access automated external defibrillator pad application and favorable neurological outcome after out-of-hospital cardiac arrest in public locations: A prospective population-based propensity score-matched study. Int. J. Cardiol. 2020;299:140–146. doi: 10.1016/j.ijcard.2019.07.061. [DOI] [PubMed] [Google Scholar]
- 5.Savastano S., Baldi E., Compagnoni S., Fracchia R., Ristagno G., Grieco N. The automated external defibrillator, an underused simple life-saving device: A review of the literature. A joint document from the Italian Resuscitation Council (IRC) and Associazione Italiana di Aritmologia e Cardiostimolazione (AIAC) J. Cardiovasc. Med. 2020;21:733–739. doi: 10.2459/JCM.0000000000001047. [DOI] [PubMed] [Google Scholar]
- 6.Caputo M.L., Muschietti S., Burkart R., Benvenuti C., Conte G., Regoli F., Mauri R., Klersy C., Moccetti T., Auricchio A. Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: A comparison with SMS-based system notification. Resuscitation. 2017;114:73–78. doi: 10.1016/j.resuscitation.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Baldi E., Caputo M.L., Auricchio A., Vanetta C., Cresta R., Benvenuti C. A quantitative assessment of the contribution of “citizen First Responder” in the adult out-of-hospital chain of survival during COVID-19 pandemic. Resuscitation. 2021;166:41–42. doi: 10.1016/j.resuscitation.2021.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oving I., de Graaf C., Masterson S., Koster R.W., Zwinderman A.H., Stieglis R., AliHodzic H., Baldi E., Betz S., Cimpoesu D., et al. European first responder systems and differences in return of spontaneous circulation and survival after out-of-hospital cardiac arrest: A study of registry cohorts. Lancet Reg. Health-Eur. 2021;1:100004. doi: 10.1016/j.lanepe.2020.100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hallstrom A.P., Ornato J.P., Weisfeldt M., Travers A.H., Christenson J., McBurnie M., Zalenski R., Becker L.B., Schron E., Proschan M. Public-Access Defibrillation and Survival after Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 10.Ringh M., Jonsson M., Nordberg P., Fredman D., Hasselqvist-Ax I., Håkansson F., Claesson A., Riva G., Hollenberg J. Survival after Public Access Defibrillation in Stockholm, Sweden—A striking success. Resuscitation. 2015;91:1–7. doi: 10.1016/j.resuscitation.2015.02.032. [DOI] [PubMed] [Google Scholar]
- 11.Kiyohara K., Kitamura T., Sakai T., Nishiyama C., Nishiuchi T., Hayashi Y., Sakamoto T., Marukawa S., Iwami T. Public-access AED pad application and outcomes for out-of-hospital cardiac arrests in Osaka, Japan. Resuscitation. 2016;106:70–75. doi: 10.1016/j.resuscitation.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 12.Holmberg M.J., Vognsen M., Andersen M.S., Donnino M.W., Andersen L.W. Bystander automated external defibrillator use and clinical outcomes after out-of-hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2017;120:77–87. doi: 10.1016/j.resuscitation.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Yeung J., Okamoto D., Soar J., Perkins G.D. AED training and its impact on skill acquisition, retention and performance—A systematic review of alternative training methods. Resuscitation. 2011;82:657–664. doi: 10.1016/j.resuscitation.2011.02.035. [DOI] [PubMed] [Google Scholar]
- 14.Hoke R.S., Heinroth K., Trappe H.J., Werdan K. Is external defibrillation an electric threat for bystanders? Resuscitation. 2009;80:395–401. doi: 10.1016/j.resuscitation.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 15.Baldi E., Contri E. Using an AED in particular environments: Is it safe or not? Suggestions for lay people and their instructors. Resuscitation. 2016;106:e25. doi: 10.1016/j.resuscitation.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 16.Perkins G.D., Graesner J.T., Semeraro F., Olasveengen T., Soar J., Lott C., Van de Voorde P., Madar J., Zideman D., Mentzelopoulos S., et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation. 2021;161:1–60. doi: 10.1016/j.resuscitation.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 17.Perkins G.D., Handley A.J., Koster R.W., Castrén M., Smyth M.A., Olasveengen T., Monsieurs K.G., Raffay V., Gräsner J.T., Wenzel V., et al. European Resuscitation Council Guidelines for Resuscitation 2015. Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015;95:81–99. doi: 10.1016/j.resuscitation.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 18.Kiguchi T., Okubo M., Nishiyama C., Maconochie I., Ong M.E.H., Kern K.B., Wyckoff M.H., McNally B., Christensen E., Tjelmeland I., et al. Out-of-hospital cardiac arrest across the World: First report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 19.Baldi E., Savastano S. AED use before EMS arrival: When survival becomes a matter of law and system in Italy, which can be improved. Eur. Heart J. 2018;39:1664. doi: 10.1093/eurheartj/ehy196. [DOI] [PubMed] [Google Scholar]
- 20.Gräsner J.T., Wnent J., Herlitz J., Perkins G.D., Lefering R., Tjelmeland I., Koster R.W., Masterson S., Rossell-Ortiz F., Maurer H., et al. Survival after out-of-hospital cardiac arrest in Europe—Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 21.Masterson S., Wright P., O’Donnell C., Vellinga A., Murphy A.W., Hennelly D., Sinnott B., Egan J., O’Reilly M., Keaney J., et al. Urban and rural differences in out-of-hospital cardiac arrest in Ireland. Resuscitation. 2015;91:42–47. doi: 10.1016/j.resuscitation.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 22.Irfan F.B., Bhutta Z.A., Castren M., Straney L., Djarv T., Tariq T., Thomas S.H., Alinier G., Al Shaikh L., Owen R.C., et al. Epidemiology and outcomes of out-of-hospital cardiac arrest in Qatar: A nationwide observational study. Int. J. Cardiol. 2016;223:1007–1013. doi: 10.1016/j.ijcard.2016.08.299. [DOI] [PubMed] [Google Scholar]
- 23.Mauri R., Burkart R., Benvenuti C., Caputo M.L., Moccetti T., Del Bufalo A., Gallino A., Casso C., Anselmi L., Cassina T., et al. Better management of out-of-hospital cardiac arrest increases survival rate and improves neurological outcome in the Swiss Canton Ticino. Europace. 2016;18:398–404. doi: 10.1093/europace/euv218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kragholm K., Wissenberg M., Mortensen R.N., Hansen S.M., Malta Hansen C., Thorsteinsson K., Rajan S., Lippert F., Folke F., Gislason G., et al. Bystander Efforts and 1-Year Outcomes in Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2017;376:1737–1747. doi: 10.1056/NEJMoa1601891. [DOI] [PubMed] [Google Scholar]
- 25.Pijls R.W.M., Nelemans P.J., Rahel B.M., Gorgels A.P.M. A text message alert system for trained volunteers improves out-of-hospital cardiac arrest survival. Resuscitation. 2016;105:182–187. doi: 10.1016/j.resuscitation.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 26.Bahr J., Bossaert L., Handley A., Koster R., Vissers B., Monsieurs K. AED in Europe. Report on a survey. Resuscitation. 2010;81:168–174. doi: 10.1016/j.resuscitation.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 27.Hansen C.M., Lippert F.K., Wissenberg M., Weeke P., Zinckernagel L., Ruwald M.H., Karlsson L., Gislason G.H., Nielsen S.L., Køber L., et al. Temporal trends in coverage of historical cardiac arrests using a volunteer-based network of automated external defibrillators accessible to laypersons and emergency dispatch centers. Circulation. 2014;130:1859–1867. doi: 10.1161/CIRCULATIONAHA.114.008850. [DOI] [PubMed] [Google Scholar]
- 28.Semeraro F., Greif R., Böttiger B.W., Burkart R., Cimpoesu D., Georgiou M., Yeung J., Lippert F., Lockey A.S., Olasveengen T.M., et al. European Resuscitation Council Guidelines 2021: Systems saving lives. Resuscitation. 2021;161:80–97. doi: 10.1016/j.resuscitation.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 29.Monsieurs K.R.G., Nolan J.P., Bossaert L.L., Greif R., Maconochie I.K., Nikolaou N.I., Perkins G.D., Soar J., Truhlář A., Wyllie J., et al. European Resuscitation Council Guidelines for Resuscitation 2015. Section 1. Executive summary. Resuscitation. 2015;95:1–80. doi: 10.1016/j.resuscitation.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 30.Tierney N.J., Reinhold H.J., Mira A., Weiser M., Burkart R., Benvenuti C., Auricchio A. Novel relocation methods for automatic external defibrillator improve out-of-hospital cardiac arrest coverage under limited resources. Resuscitation. 2018;125:83–89. doi: 10.1016/j.resuscitation.2018.01.055. [DOI] [PubMed] [Google Scholar]
- 31.Derkenne C., Jost D., Miron De L’Espinay A., Corpet P., Frattini B., Hong V., Lemoine F., Jouffroy R., Roquet F., Marijon E., et al. Automatic external defibrillator provided by unmanned aerial vehicle (drone) in Greater Paris: A real world-based simulation. Resuscitation. 2021;162:259–265. doi: 10.1016/j.resuscitation.2021.03.012. [DOI] [PubMed] [Google Scholar]
- 32.Ringh M., Rosenqvist M., Hollenberg J., Jonsson M., Fredman D., Nordberg P., Järnbert-Pettersson H., Hasselqvist-Ax I., Riva G., Svensson L. Mobile-Phone Dispatch of Laypersons for CPR in Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2015;372:2316–2325. doi: 10.1056/NEJMoa1406038. [DOI] [PubMed] [Google Scholar]
- 33.Stein P., Spahn G.H., Müller S., Zollinger A., Baulig W., Brüesch M., Seifert B., Spahn D.R. Impact of city police layperson education and equipment with automatic external defibrillators on patient outcome after out of hospital cardiac arrest. Resuscitation. 2017;118:27–34. doi: 10.1016/j.resuscitation.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 34.Zijlstra J.A., Stieglis R., Riedijk F., Smeekes M., van der Worp W.E., Koster R.W. Local lay rescuers with AEDs, alerted by text messages, contribute to early defibrillation in a Dutch out-of-hospital cardiac arrest dispatch system. Resuscitation. 2014;85:1444–1449. doi: 10.1016/j.resuscitation.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 35.Krammel M., Lobmeyr E., Sulzgruber P., Winnisch M., Weidenauer D., Poppe M., Datler P., Zeiner S., Keferboeck M., Eichelter J., et al. The impact of a high-quality basic life support police-based first responder system on outcome after out-of-hospital cardiac arrest. PLoS ONE. 2020;15:e0233966. doi: 10.1371/journal.pone.0233966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baldi E., Contri E., Burkart R., Bywater D., Duschl M. The three dimension model of the out-of-hospital cardiac arrest. Resuscitation. 2019;138:44–45. doi: 10.1016/j.resuscitation.2019.02.042. [DOI] [PubMed] [Google Scholar]
- 37.Nadarajan G.D., Tiah L., Ho A.F.W., Azazh A., Castren M.K., Chong S.L., El Sayed M.J., Hara T., Leong B.S., Lippert F.K., et al. Global resuscitation alliance utstein recommendations for developing emergency care systems to improve cardiac arrest survival. Resuscitation. 2018;132:85–89. doi: 10.1016/j.resuscitation.2018.08.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.