Abstract
Characterizing the impacts of disruption attributable to the COVID-19 pandemic on clinical research is important, especially in pain research where psychological, social, and economic stressors attributable to the COVID-19 pandemic may greatly impact treatment effects. The National Institutes of Health – Department of Defense – Department of Veterans Affairs Pain Management Collaboratory (PMC) is a collective effort supporting 11 pragmatic clinical trials studying nonpharmacological approaches and innovative integrated care models for pain management in veteran and military health systems. The PMC rapidly developed a brief pandemic impacts measure for use across its pragmatic trials studying pain while remaining broadly applicable to other areas of clinical research. Through open discussion and consensus building by the PMC's Phenotypes and Outcomes Work Group, the PMC Coronavirus Pandemic (COVID-19) Measure was iteratively developed. The measure assesses the following domains (one item/domain): access to healthcare, social support, finances, ability to meet basic needs, and mental or emotional health. Two additional items assess infection status (personal and household) and hospitalization. The measure uses structured responses with a three-point scale for COVID-19 infection status and four-point ordinal rank response for all other domains. We recommend individualized adaptation as appropriate by clinical research teams using this measure to survey the effects of the COVID-19 pandemic on study participants. This can also help maintain utility of the measure beyond the COVID-19 pandemic to characterize impacts during future public health emergencies that may require mitigation strategies such as periods of quarantine and isolation.
Keywords: Pragmatic clinical trials, Phenotyping, Pain, COVID-19, Veterans, Military personnel
1. Introduction
Beginning in early 2020 in the United States, the COVID-19 pandemic rapidly disrupted many facets of everyday life. Healthcare systems were frequently taxed beyond their capacity to manage patients with COVID-19, and usual face-to-face care delivery was suspended with at least partial replacement through a rapid expansion of telehealth services. Clinical research grew in areas related to COVID-19 and the use of telehealth for healthcare delivery. However, there was also disruption of clinical research in many areas, including pain research.
Pain research is an area that is garnering increasing attention, particularly given the high prevalence and impact of chronic pain, as well as the recent focus on the opioid crisis [1,2]. There is an increasing shift in care delivery to emphasize integrated, multimodal models of pain care that incorporate evidence-based nonpharmacological approaches [1,2]. The COVID-19 pandemic has likely affected and will continue to affect chronic pain research in several important ways. First, during the COVID-19 era, pain care delivery and pain clinical trials shifted to telehealth and virtual delivery, presenting new challenges for patients and clinicians [3]. At present, there is limited evidence to help understand how this may impact pain outcomes [4,5]. Musculoskeletal pain may be a post-acute sequalae of COVID-19 infection [6]. In addition, an individual's pain experience may be adversely affected by psychological, social, and economic stressors attributable to the COVID-19 pandemic [7]. Recently published work suggests that the perceived severity and impact of chronic pain has increased during the pandemic [8]. This has implications for chronic pain research occurring during the COVID-19 pandemic as well as how these studies will be interpreted within the broader pain literature. The COVID-19 pandemic may also exacerbate existing disparities in pain and pain management, since members of racial and ethnic minority groups and members of lower socioeconomic groups are most likely to be affected by COVID-19 [[9], [10], [11]].
The National Institutes of Health (NIH) – Department of Defense (DOD) – Department of Veterans Affairs (VA) Pain Management Collaboratory (PMC) is a collective effort supporting 11 pragmatic clinical trials studying nonpharmacological approaches and innovative integrated care models for pain management in veteran and military health systems, supported by a centralized Pain Management Collaboratory Coordinating Center (PMC [3]) [12]. The PMC pragmatic trials responded and adapted to the disruption in clinical research attributable to the COVID-19 pandemic, leveraging their pragmatic designs to accommodate changes in the interventions being studied, recruitment approaches, approaches to collected data, and more [13].
As such, members of the Collaboratory recognized the importance of characterizing the impacts of the COVID-19 pandemic on the participants enrolled in their pragmatic trials. The purpose of this paper is to describe the rapid development of a brief measure to assess trial participants' perceptions of COVID-related impacts on their pain and life experiences. Our aim was to design a patient-centered measure for use across the Collaboratory trials that remained generalizable to broadly assess changing impacts in participant experience in clinical research during the COVID-19 pandemic.
2. Methods
2.1. Task and process
Based on the domain-oriented structure of the PMC, the Phenotypes and Outcomes (P&O) Work Group was tasked by the PMC [3] leadership [12] with developing a scalable, low-burden, patient-reported measure to complement existing trial data collection and assess the perceived impacts of COVID-19 and the COVID-19 pandemic. The P&O Work Group's role in the PMC is to identify reliable and clinically meaningful phenotypes of participants in the clinical trials for use in examining important treatment effect moderators and to promote harmonization of the measurement approaches when feasible. Work Group membership includes representatives from each pragmatic trial study team, two co-chairpersons, a project manager, and members of PMC [3] leadership, representing a diverse array of experience and expertise that contributes to the strategic planning and execution of Work Group contributions to the PMC. This Work Group complements other domain-oriented work groups across the PMC focusing on electronic health records, data sharing, biostatistics and study design, stakeholder engagement, implementation science, and ethics and regulatory issues.
While pandemic impacts on recruitment and follow up varied across the PMC pragmatic trials and some were temporarily suspended [13], we recognized that all would likely aim to resume or continue recruitment and follow up assessment as soon as it was deemed safe and appropriate to proceed, thus precipitating the need to rapidly develop a measure. Due to this time-sensitive nature of the task, the P&O Work Group adopted a consensus process approach to develop the measure, including formulating the construct, identifying domains of interest, developing items, and refining additional characteristics of the final measure. This capitalized on the subject matter expertise of the P&O Work Group members to efficiently and effectively complete the task.
Initial discussions began during the April 2020 Work Group meeting, with a follow up meeting occurring 3 weeks later. Item development was completed across Work Group meetings consistent with published best practice recommendations [14], with domain identification and item generation through open discussion and content validation through evaluation by experts across the group. Deductive and inductive methods defined domains of interest and identified questions to assess them, with an early emphasis on broad assessment that could be further refined as appropriate.
2.2. Purpose and construct
The purpose of the measure was to characterize and phenotype participants enrolled in clinical trials; examine baseline relationships between COVID-19 impacts measured by this and other phenotyping and outcomes measures; and to examine the role of COVID-19 impacts as a moderator or mediator of trial engagement, participation, outcome expectancies, and outcomes.
We define these impacts as any factors related to the COVID-19 pandemic that may be related to clinical trial outcomes, such as psychosocial factors (e.g., heightened stress, anxiety, depression, and isolation), economic and vocational status, and healthcare access and delivery. In the case of the PMC pragmatic trials, this primarily includes factors impacting pain severity and pain-related function and interference.
Validity is the extent to which an instrument measures what it purports to measure [15], and establishing a clear definition of the construct to be measured by an instrument is foundational prior to assessing validity. Through the consensus process, content validity (including face validity) was assessed by the expert group to identify the relevance and comprehensiveness of the domains of interest and items across those domains [16]. This included discussion on the relevance of domains and items in measuring the construct, relevance to the patient population, and relevance to the purpose. Discussions also focused on the comprehensiveness of the measure – whether the domains and items appropriately cover the construct.
2.3. Content domains
At the initial planning meeting, general themes and areas of interest related to assessing the impacts of COVID-19 emerged on 1) study outcomes, 2) the ability to access pain-related treatment interventions, and 3) quality of life domains related to pain experience. Also considered was self-report of COVID-19 infection status for individual participants and household contacts, as both were expected to potentially affect trial outcomes. Follow up communications via email solicited input from Work Group representatives for potentially relevant domains of interest that had not been discussed during the planning meeting.
Early discussions centered around assessing the directly attributable impacts of COVID-19 on pain-related outcomes, such as pain intensity, pain-related function, and quality of life. Other themes proposed included assessing pandemic-related and general mood, objective moderators like employment status, and effects on relevant social determinants of health.
The final domains of the measure aimed to reflect the respondents' perceptions of pandemic-related impacts on their own access to healthcare, social support, finances, ability to meet basic needs, mental or emotional health, and infection status. The iterative design process and the relationships between the identified general themes, intermediate considerations, and the final recommendations obtained through the Work Group discussions are summarized in Table 1 . Other domains considered, but ultimately excluded, included coping and self-care and technological literacy.
Table 1.
Relationship between general themes of interest (identified during initial review of public COVID-19 surveys) related to COVID-19 impacts on clinical trial outcomes, intermediate considerations during the consensus process, and final recommendations that influenced the development of the PMC Coronavirus Pandemic (COVID-19) Measure.
| General themes | Intermediate considerations | Final recommendations |
|---|---|---|
| COVID-19 Status |
|
|
| Access to Healthcare |
|
|
| Quarantine & Social Isolation |
|
|
| Coping and Self-Care |
|
|
| Stress/Anxiety |
|
|
| Technology Literacy |
|
|
| Socioeconomic Status |
|
|
| General/Other |
|
|
| Qualitative |
|
|
2.4. Item development
In April 2020, we conducted a broad search for COVID-19 surveys available in the public domain, the NIH Public Health Emergency and Disaster Research Response (DR2) Resources Portal [17] (https://tools.niehs.nih.gov/dr2), and the PhenX Toolkit [18] (https://www.phenxtoolkit.org/covid19). An open call for other measures adopted by PMC investigators was also solicited via email. The search and subsequent review were completed by two members of the study team (BCC and MG) to synthesize any available, ongoing efforts to assess the impact of COVID-19 through questionnaires. Our search was unsuccessful in identifying a brief measure of patient-reported perceived pandemic impact across a handful of important domains; thus, we used our findings to inform development our own original measure. In reviewing available instruments, we aimed to consider how other researchers and policymakers were ascertaining the impacts of COVID-19 on daily life (in general and related to healthcare) and to consider how these questions may be relevant for pain and other health related outcomes. General themes of surveys in the public domain and from the DR2 and PhenX Toolkit resources were used to facilitate early Work Group discussions on domains of interest. Questions identified as potentially relevant were reviewed to inform the language used in the initial draft version of the measure to be presented and reviewed at the subsequent Work Group meeting, though none were ultimately included in the final measure.
Through discussion, the team navigated tension between the need for a brief, concise measure and interest in including all potentially relevant items in detail to cover the domains. Email communication iteratively solicited other potentially relevant items to the domains of interest, with subsequent discussion across the consensus meetings. Ongoing discussions during the Work Group meetings and in ad-hoc communication led to a rapid redesign of the proposed measure.
Questions were structured in a generalizable way that could increase their application across many individuals and clinical disciplines, including, but not limited, to the veteran and military populations and people with pain. Discussion to promote generalizability and use of the measure across diverse clinical trial settings led to prioritization of items whose wording would not be specific to pain (e.g., impact on social support) but whose content would likely influence the experience of pain. It was also recognized that pain outcomes were being assessed in other patient reported outcome measures by each trial, thus pain-specific questions were excluded to avoid redundant effort by participants.
To parallel five of the six domains identified and prioritized, five concise items were used to assess the effects of the COVID-19 pandemic on the ability to access healthcare, social support, finances, ability to meet basic needs, and mental or emotional health. This represented the endpoint of a collaborative process of winnowing questions down to the handful of pandemic impacts that were considered by the group as being most essential to address. Other domains of impact (e.g., sleep, anxiety, employment) were viewed as important, but were left off to preserve brevity and usability (e.g., physical activity) or were subsumed under more general queries (e.g., anxiety as a part of “mental health”, employment as a part of “finances”). To address the sixth and final domain of infection status, an additional two items were added to self-report personal and household experiences with COVID-19, including asking about hospitalization status in a nested item. Work Group discussions centered around the framing of items describing self-report of infection status and of hospitalization. Infection status was particularly troublesome as a balance was needed to appropriately represent self-identified infection, healthcare professional identified infection without confirmatory diagnostic testing, and infection confirmed with diagnostic testing. Work Group members prioritized carefully wording the infection status item to reflect the goal of the item and the overall measure to establish what patients believe happened to them (i.e., perceptions of infection status). Work Group members recognized that wording asking about “symptoms consistent with COVID-19” or “diagnosed with COVID-19 via confirmed laboratory test” may be confusing to patients. The Work Group's decision not to include confirmatory diagnostic testing (or include this as an additional item) was further rooted in potential influence of external factors such as variability in accessibility to confirmatory diagnostic testing during the period of measure development due to recognized resource, logistics, and supply chain challenges. While COVID-19 diagnosis was expected to be available in the individual participant's electronic health record data, self-report was thought to account for personal or household experience with COVID-19 in the context of potential limitations in testing (particularly early in the pandemic period) and in receiving healthcare from systems outside of the Veterans Health Administration and the Military Health System. Hospitalization due to COVID-19 was included to characterize severity of infection.
In addition, items were proposed that would aim to explicate the acute, short-term impacts of COVID-19 versus the chronic, residual effects – although these were ultimately determined to be beyond the scope of the measure. Following an iterative process of consensus building, the final measure focused on respondent attribution of impacts to COVID-19, including pandemic-related disruptions and social and economic changes. To affirm this attribution to COVID-19, the stem for all questions was: “Over the last 3 months, how has the coronavirus pandemic affected your…” The rationale for using this time frame for this measure was based on recommendations for pain outcomes across other measures adopted by the PMC trials and paralleling the analytic approach adopted by most trials for their outcome measures. It was further recommended that individual study teams review the recommended recall window and adapt, as appropriate, to fit within their serial assessment protocols.
2.5. Nature of measure and mode of administration
Some Work Group members initially objected to the apparently subjective nature of the items and were concerned that they might not provide reliable information about changes in the domains covered by the measure. Ultimately, the group was unable to identify any alternative, pragmatic strategy to reliably obtain more objective measures of COVID-related impacts, particularly in a short survey format, and through discussion, consensus was achieved about the appropriateness of this approach.
Several Work Group members proposed implementing a mixed-methods approach involving both quantitative ratings and free-text responses to open-ended items. Other early discussions that shaped the final design focused on the burden of interpretation and analyses of the final measure, which would be the responsibility of the individual trial study teams. Thus, the Work Group recognized that adding length and complexity to the finalized measure could also become time and resource intensive to both participants and study teams. Therefore, to minimize administration burden, a concise measure was designed with structured response items only.
2.6. Item response format
For structured response questions, discussions centered on the scale to be used, including a Likert-type 5 response scale, a 0–10 numerical rating scale, or a visual analog scale with appropriate anchors for response levels. Sensitivity to the type of response was important to facilitate administration of the measure across different forms of outcome assessment delivery (written/digital-based vs. verbal/telephone-based).
After considering using a binary response scale to represent impact versus no impact, an ordinal rating scale was determined to be the most appropriate response scale to support inferences or exploratory analyses in trial results for questions assessing the effects of COVID-19. This ordinal rating scale was structured to capture the direction and magnitude of the effects measured by each question, with two magnitudes of negative effect, a neutral effect, and a positive effect identifiable. Initially, Work Group members were primarily interested in measuring the degree of negative impact in anticipation that negative impacts would likely be more common, more severe, and more relevant to pain outcomes. Although the group ultimately agreed on the importance of identifying perceived positive impacts as well, there was a determination that there may be less need to assess degree of these positive impacts (e.g. “a little better” or “a lot better”) with respect to pain outcomes. Thus, to prioritize conciseness and simplicity, the four-item ordinal scale was adopted in place of a more traditional five-item scale. For questions about individual and household experience with COVID-19, a three-item scale (yes, no, unsure) was used to collect self-report of experience, with a binary scale (yes, no) for hospitalization status.
Investigators were invited to conduct supplemental open-ended assessment as they viewed appropriate. A proposed multi-part, comprehensive open-ended item that replicated items being used by an individual pragmatic clinical trial in their outcome assessments was considered (Table 2 ), although ultimately excluded from the final survey to maintain conciseness and limit participant reporting burden.
Table 2.
Proposed, multipart open-ended response question for inclusion in PMC Coronavirus Pandemic (COVID-19) Measure.
| Question Stem | Some people have been affected by the coronavirus including by spread of the virus in the community, by the community's response, or by contracting the virus itself. |
| Follow Up Questions |
|
| |
| |
| |
|
While an open-ended question was ultimately excluded from the final measure, one or more variations considered by the PMC may be useful in end-user adaptations. Discussion centered on including a common question stem, followed by adapted individual responses to ascertain generalized and pain-related impacts.
2.7. Additional considerations
An overarching recommendation from the Work Group was to ensure that the measure reflected difficulties and potentially even benefits from disrupted life during the COVID-19 pandemic, not limited to difficulties/benefits caused by direct experience with the disease itself (impacts of lockdowns, changes in work and school schedules and formats, etc.). The introduction used to define the scope and explain the measure makes this explicit: “When we say the coronavirus pandemic, we are referring to the spread of the COVID-19 virus through many communities, whether or not you or people you know actually had the virus.”
3. Results
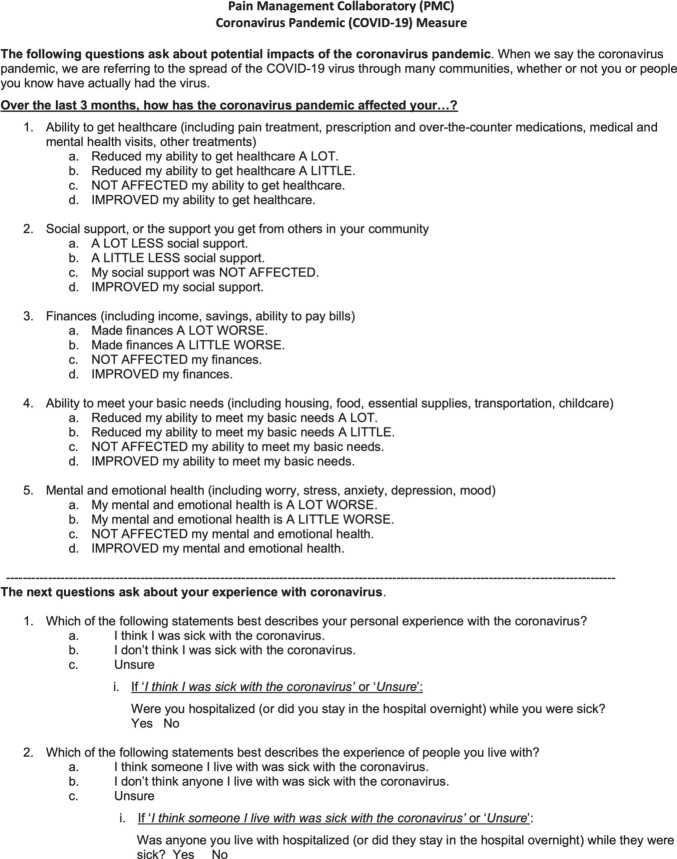
Design considerations were rapidly proposed and iteratively reviewed leading to the final design for the PMC Coronavirus Pandemic (COVID-19) Measure (Fig. 1 , and available for download as Supplemental Material).
Fig. 1.
Final Pain Management Collaboratory Coronavirus Pandemic (COVID-19) Measure. A printable version of the measure is included as supplemental material.
There was strong engagement across the PMC from the P&O Work Group chairs, project manager, members, the PMC [3] directors, and the PMC Steering Committee. One of the major strengths to the collaborative nature of the PMC was also a potential challenge when it came to development of this measure. While detailed and thoughtful consensus building for phenotyping and outcomes measures can often take months of iterative deliberation, doing so within a time-sensitive, compressed schedule to address the suspected impacts of COVID-19 created a new challenge. All collaborators reviewed preliminary draft versions of the measure, proposed feedback, and revised, and recirculated the draft. This intensive, iterative review process occurred four times across the period of 1 month, with individual contributions and proposals addressed in detail each time – including thoughtful discussion as to why changes were or were not incorporated into the final measure. Consensus was obtained about which core items would be harmonized for data collection across all PMC trials adopting this measure. Throughout the consensus process, the P&O Work Group identified a series of recommendations to inform the final design and recommended, but did not require, use by the PMC trials. A final version of the measure was presented to the PMC Steering Committee for their approval for use across the PMC trials.
4. Discussion
The PMC Coronavirus Pandemic (COVID-19) Measure was proposed, rapidly developed, and finalized for harmonized use across the Collaboratory over a 1-month period shortly after the beginning of the COVID-19 pandemic in the United States. The rapid development of the measure stems from the strong interdisciplinary and collaborative nature of the PMC, fostered over the first 3 years of its operation. With its multidisciplinary array of leading experts in pain research, psychosocial assessment, implementation science, biostatistics, study design, and computational phenotyping, the PMC was well positioned to respond swiftly to this challenge and to conduct content validation.
The final domains of the PMC Coronavirus Pandemic (COVID-19) Measure aimed to ascertain the impacts of the COVID-19 pandemic on trial participants' access to healthcare, social support, finances, ability to meet basic needs, mental or emotional health, and infection status. These domains and items were generated through a consensus building process and prioritized to appropriately measure impacts of COVID-19 relevant to clinical research and maintain a concise final measure. PMC investigative teams were given the option of including assessment items for additional domains, including those described but excluded, as appropriate on a case-by-case basis outside of the harmonized measure. For example, with respect to coping and self-care, discussions focused on an individual's ability to cope and maintain self-care in general during pandemic period/periods of social isolation and related to coping and self-management of health conditions. While likely relevant to pain management given widespread recommendations emphasizing self-care for musculoskeletal pain conditions [19], data regarding self-care for musculoskeletal pain were captured in other outcome measures used by individual trials. Technological literacy was thought to be a relevant domain given the use of technology-based interventions to varying degrees across many PMC pragmatic trial protocols and the rapid expansion of telehealth and other remote healthcare delivery methods in response to the COVID-19 pandemic. This shift towards digital health approaches was suspected to be potentially important with respect to participation in trials adopting technology-based interventions or other telehealth services in their protocols and with access to healthcare outside of trial participation for pain or other health conditions. While deemed important, technological literacy was ultimately excluded to maintain conciseness and a focused scope. Work Group discussions recognized that the scope for technological literacy may be too broad in that it can be related to the COVID-19 pandemic or remain an important issue independent of the COVID-19 pandemic for any study incorporating technology in its study protocols.
The P&O Work Group advised on the frequency of assessments for the measure in the PMC pragmatic clinical trials, which may be applicable to other clinical trials. The broad recommendation was to consider serial assessment (rather than single assessment) that aligns with the frequency of administration of other outcome assessments in the respective pragmatic trials while remaining sensitive to participant burden. In the context of longitudinal assessment of study outcomes across clinical research (i.e., at baseline, post-treatment, at follow-up), responses to the measure can be used as a potential moderator (if collected only at baseline), a mediator (if collected across multiple phases of trial participation), a confounder, or a covariate in clinical outcome analyses [20]. This may also be important as potential impacts of and experiences with COVID-19 may change over the course of time, including across participation in a clinical trial. Early feedback from study teams who have begun using this measure has indicated its ease of use and highlighted the usefulness of specific questions related to their study objectives.
In an effort to support dissemination of the developed measure for use in other clinical trial settings, the finalized version was deposited in the NIH Disaster Research Response (DR2) Resource Portal [17] and the PhenX Toolkit [18]. The NIH DR2 program supports timely research in response to disaster and public health emergency, such as the COVID-19 pandemic. The measure was also shared with other interested collaborative research groups, such as the NIH Health Care Systems Research Collaboratory [21] aiming to strengthen collaborative clinical research between healthcare systems and research partners.
Not only can the results of this measure be used to describe the impacts of COVID-19 on patients with chronic pain or other physical and mental health conditions, but responses can also be used to adjust for or explain trial results that occur during the pandemic period. Future plans include conducting a formal psychometric evaluation of the measure, including investigation of criterion validity of this measure in comparison to other measures being used to assess study outcomes across the PMC trials. The PMC trials are using harmonized measures related to constructs assessed in our COVID-19 measure, including psychological distress and use of pain services. We intend to analyze the extent to which participants with self-reported COVID impacts on mental health and on treatment services used show disproportionate changes in the other harmonized measures of these constructs collected serially. Other future plans will capitalize on the data collected from the use of this measure across the PMC trials and include examining validation of self-report data and correspondence with data available in the electronic health record; describing response patterns, scoring, and effective use in statistical analyses of trial outcomes; investigating association with COVID-19 vaccination uptake; and examining disparities in the impact of the COVID-19 pandemic for vulnerable and disadvantaged groups such as racial and ethnic minorities, women, low socioeconomic status individuals, and individuals with medical and mental health comorbidities.
The final measure may apply across clinical trials and other studies examining mental and physical health outcomes during the COVID-19 pandemic, including pain and other chronic medical conditions. For example, the only time “pain” is mentioned is in giving an example of types of healthcare that might have been impacted by the pandemic. The measure's purpose to assess the impacts of the COVID-19 pandemic facilitates statistical analyses as moderators, mediators, confounders, and covariates of intervention effects across clinical research more broadly. It may also be useful in studies aiming to differentiate the indirect effects of COVID-19-related impacts from direct effects of COVID-19 infection on musculoskeletal pain and other post-acute sequelae [6]. One example of use of the scale for non-pain conditions is a trial on dementia care, which highlights the application of this measure outside of clinical trials studying pain. However, for studies examining the impact of COVID-19 as a principal aim, this measure may not be an appropriate outcome measure until it is formally validated for this purpose. We also recognized that there may be lasting psychosocial influences and stressors attributable to the COVID-19 pandemic that may persist beyond its potential endpoint, during which time this measure may remain useful. Indeed, while we hope that future pandemics may be averted, recent reviews by experts in the field suggest that the COVID-19 pandemic will likely not be the last time that governments have to issue public health recommendations and implement lockdown and quarantine orders in response to infectious disease emergencies [22].
We continue to support the recommendation for adaptation as appropriate for individualized use by study teams using this measure to survey the effects of the pandemic on their study participants. Adaptation for individual needs will help maintain utility of the measure beyond an endpoint of the COVID-19 pandemic to characterize impacts during future public health emergencies that may require mitigation strategies such as periods of quarantine and isolation.
Funding sources
Research reported in this publication from the Pain Management Collaboratory Coordinating Center was made possible by Grant Number U24-AT009769 from the National Center for Complementary and Integrative Health (NCCIH) and the Office of Behavioral and Social Sciences Research (OBSSR). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCCIH, OBSSR, and the National Institutes of Health.
This work was supported, in part, through cooperative agreement award numbers UG3/UH3-AT009761 from the National Center for Complementary and Integrative Health (NCCIH) and the Office of Research on Women's Health; UG3/UH3-AT009765 from the National Center for Complementary and Integrative Health (NCCIH) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD); and UG3/UH3-AT009758 from the from the National Center for Complementary and Integrative Health (NCCIH) and National Institute on Drug Abuse (NIDA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This work was supported, in part, by the U.S. Army Medical Research Acquisition Activity and the Assistant Secretary of Defense for Health Affairs endorsed by the Department of Defense, through the Pain Management Collaboratory - Pragmatic Clinical Trials Demonstration Projects under Award No. W81XWH-18-2-0003. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702–5014 is the awarding and administering acquisition office. Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense.
This work was supported, in part, by HSR&D Award # SDR-17-306 from the United States (U.S.) Department of Veterans Affairs Health Services Research and Development Service. The contents of this manuscript represent the view of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the United States Government.
Competing interests
The authors have no competing interests to declare.
Acknowledgements
This manuscript is a product of the NIH-DoD-VA Pain Management Collaboratory. For more information about the Collaboratory, visit https://painmanagementcollaboratory.org/. The contents of this publication are the sole responsibility of the author(s) and do not necessarily reflect the views, opinions or policies of the National Institutes of Health, the United States (U.S.) Department of Veteran Affairs Health Services Research and Development Service, Uniformed Services, University of the Health Sciences (USUHS), The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., the Department of Defense (DoD), the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
The authors would also like to acknowledge all members of the Pain Management Collaboratory Phenotypes and Outcomes Work Group for their thoughtful contributions to the discussions supporting this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cct.2021.106619.
Appendix A. Supplementary data
Supplementary material: Pain Management Collaboratory (PMC) Coronavirus Pandemic (COVID-19) Measure
References
- 1.Interagency Pain Research Coordinating Committee . US Department of Health and Human Services; 2016. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain.https://www.iprcc.nih.gov/sites/default/files/documents/NationalPainStrategy_508C.pdf Accessed June 23, 2021. [Google Scholar]
- 2.Institute of Medicine . National Academies Press; Washington (DC): 2011. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. [PubMed] [Google Scholar]
- 3.Fernandes L.G., Devan H., Fioratti I., Kamper S.J., Williams C.M., Saragiotto B.T. At my own pace, space and place: a systematic review of qualitative studies of enablers and barriers to telehealth interventions for people with chronic pain. Pain. 2021 doi: 10.1097/j.pain.0000000000002364. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Fritz J.M., Davis A.F., Burgess D.J., Coleman B., Cook C., Farrokhi S., Goertz C., Heapy A., Lisi A.J., McGeary D.D., Rhon D.I., Taylor S.L., Zeliadt S., Kerns R.D. Pivoting to virtual delivery for managing chronic pain with nonpharmacological treatments: implications for pragmatic research. Pain. 2021;162(6):1591–1596. doi: 10.1097/j.pain.0000000000002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eccleston C., Blyth F.M., Dear B.F., Fisher E.A., Keefe F.J., Lynch M.E., Palermo T.M., Reid M.C., Williams A.C.C. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020;161:889–893. doi: 10.1097/j.pain.0000000000001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Aly Z., Xie Y., Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature. 2021;594:259–264. doi: 10.1038/s41586-021-03553-9. [DOI] [PubMed] [Google Scholar]
- 7.Karos K., McParland J.L., Bunzli S., Devan H., Hirsh A., Kapos F.P., Keogh E., Moore D., Tracy L.M., Ashton-James C.E. The social threats of COVID-19 for people with chronic pain. Pain. 2020;161:2229–2235. doi: 10.1097/j.pain.0000000000002004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hruschak V., Flowers K.M., Azizoddin D.R., Jamison R.N., Edwards R.R., Schreiber K.L. Cross-sectional study of psychosocial and pain-related variables among chronic pain patients during a time of social distancing imposed by the coronavirus disease 2019 (COVID-19) pandemic. Pain. 2021;162(2):619–629. doi: 10.1097/j.pain.0000000000002128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holmes L., Jr., Enwere M., Williams J., Ogundele B., Chavan P., Piccoli T., Chinacherem C., Comeaux C., Pelaez L., Okundaye O., Stalnaker L., Kalle F., Deepika K., Philipcien G., Poleon M., Ogungbade G., Elmi H., John V., Dabney K.W. Black-white risk differentials in COVID-19 (SARS-COV2) transmission, mortality and case fatality in the United States: translational epidemiologic perspective and challenges. Int. J. Environ. Res. Public Health. 2020;17 doi: 10.3390/ijerph17124322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson K.O., Green C.R., Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J. Pain. 2009;10:1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Tait R.C., Chibnall J.T. Racial/ethnic disparities in the assessment and treatment of pain: psychosocial perspectives. Am. Psychol. 2014;69:131–141. doi: 10.1037/a0035204. [DOI] [PubMed] [Google Scholar]
- 12.Kerns R.D., Brandt C.A., Peduzzi P. NIH-DoD-VA pain management collaboratory. Pain Med. 2019;20:2336–2345. doi: 10.1093/pm/pnz186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coleman B.C., Kean J., Brandt C.A., Peduzzi P., Kerns R.D. Adapting to disruption of research during the COVID-19 pandemic while testing nonpharmacological approaches to pain management. Transl. Behav. Med. 2020;10:827–834. doi: 10.1093/tbm/ibaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boateng G.O., Neilands T.B., Frongillo E.A., Melgar-Quinonez H.R., Young S.L. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front. Public Health. 2018;6:149. doi: 10.3389/fpubh.2018.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cronbach L.J., Meehl P.E. Construct validity in psychological tests. Psychol. Bull. 1955;52:281–302. doi: 10.1037/h0040957. [DOI] [PubMed] [Google Scholar]
- 16.Mokkink L.B., Terwee C.B., Knol D.L., Stratford P.W., Alonso J., Patrick D.L., Bouter L.M., de Vet H.C. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med. Res. Methodol. 2010;10:22. doi: 10.1186/1471-2288-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute of Environmental Health Sciences Disaster Research Response (DR2) Program. https://www.niehs.nih.gov/research/programs/disaster/ Accessed June 23, 2021.
- 18.Hamilton C.M., Strader L.C., Pratt J.G., Maiese D., Hendershot T., Kwok R.K., Hammond J.A., Huggins W., Jackman D., Pan H., Nettles D.S., Beaty T.H., Farrer L.A., Kraft P., Marazita M.L., Ordovas J.M., Pato C.N., Spitz M.R., Wagener D., Williams M., Junkins H.A., Harlan W.R., Ramos E.M., Haines J. The PhenX toolkit: get the most from your measures. Am. J. Epidemiol. 2011;174:253–260. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin I., Wiles L., Waller R., Goucke R., Nagree Y., Gibberd M., Straker L., Maher C.G., O’Sullivan P.P.B. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br. J. Sports Med. 2019;54:79–86. doi: 10.1136/bjsports-2018-099878. [DOI] [PubMed] [Google Scholar]
- 20.MacKinnon D.P., Krull J.L., Lockwood C.M. Equivalence of the mediation, confounding and suppression effect. Prev. Sci. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NIH Health Care Systems Research Collaboratory Rethinking Clinical Trials: A Living Textbook of Pragmatic Clinical Trials. https://rethinkingclinicaltrials.org Accessed June 23, 2021.
- 22.Relman D.A. Opinion: to stop the next pandemic, we need to unravel the origins of COVID-19. Proc. Natl. Acad. Sci. U. S. A. 2020;117:29246–29248. doi: 10.1073/pnas.2021133117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material: Pain Management Collaboratory (PMC) Coronavirus Pandemic (COVID-19) Measure