Abstract
Despite the actual availability of COVID-19 vaccines to combat the pandemic, many people are still vacillating in their decision to vaccinate. In this study, we considered the effect of two relevant contextual issues on vaccination intention: the number of people infected with COVID-19 is increasing, and the pace of vaccination is gaining speed. Specifically, we hypothesized that having already contracted SARS-CoV-2 (post-positive reluctance) could lead people to underestimate the importance of vaccination. Moreover, as the number of vaccinated people increases, more hesitant people could fall into the free-riding intention category, benefitting from the immunity provided by others' vaccinations. Vaccine hesitancy becomes more critical as the vaccination campaign proceeds: at one point, it will be inevitable to deal with hesitant people. This study is part of a WHO Regional Office for Europe project and involved a representative sample of 5006 Italians interviewed in January–February 2021. In case of post-positive reluctance, both young age and female gender increase vaccine hesitancy, while a high level of education reduces free-riding intention. Considering post-positive reluctance and free riding, a protective effect on hesitancy is associated with negative affective states, adherence to protective behaviors, trust in health information sources, and resilience. In contrast, increased vaccine hesitancy is associated with a high level of conspiracy-mindedness and trust in media information sources. Recognizing and studying the post-positive reluctance and the phenomenon of free-riding people can help us to become more efficient in combatting the virus.
Keywords: COVID-19, Vaccination intention, Vaccination hesitancy, Post-positive reluctance, Free-riding intention
Abbreviations: COVID-19, COronaVirus DIsease of 2019; SARS-CoV-2, Severe acute respiratory syndrome CoronaVirus-2; VH, Vaccine hesitancy; EFA, Explorative factorial analysis
1. Introduction
After more than a year, the SARS-CoV-2 pandemic remains ongoing, but the situation is evolving, mainly due to the growth of scientific knowledge and the development of vaccines. To date, studies have mostly focused on vaccine hesitancy per se (Lazarus et al., 2021; Caserotti et al., 2021), missing new salient aspects that need to be considered: many infected people have acquired some natural immunity, and vaccination proceeds at a rapid pace. If reaching out and vaccinating people who accept vaccination is certainly crucial, the real challenge is to convince reluctant persons. We know, for example, that people's beliefs and attitudes about vaccines are mainly shaped by the number of affected people and, in turn, by changes in individual risk perception (e.g., Caserotti et al., 2021; Schwarzinger et al., 2021). We also know that even politics may play a role in modifying people's beliefs and attitudes; for example, claims made during the US presidential campaign engendered worries that vaccines were rushed and thus not safe (Limaye et al., 2021; Thorp, 2020). Additionally, concerns are driven by the new technologies used for the development and manufacturing of some vaccines, such as worries related to the mRNA vaccines, sometimes fueled by the anti-vax community leveraging conspiracy beliefs (Ullah et al., 2021; Chirumbolo, 2021). Fortunately, over time, vaccine acceptance has increased globally (Daly et al., 2021; Imperial College London, 2021), but COVID-19 vaccine hesitancy could jeopardize high coverage, thus prolonging the need for lockdowns and other restrictive measures, with potentially negative socioeconomic consequences. According to a recent model developed by the Imperial College of London, the “mortality over a 2-year period could be up to 8 times higher in countries with high vaccine hesitancy compared to an ideal vaccination uptake,” resulting in an additional 236 deaths per million population (Johns and van Elsland, 2021).
It is noteworthy that the problem of vaccine hesitancy becomes more and more critical as the vaccination campaign proceeds. As time goes by, it is inevitable to deal with hesitant persons, which can mean not only the outright vaccine refusers but also those who for different reasons avoid vaccination. Here, we hypothesize that having already contracted SARS-CoV-2, especially if symptoms are mild, could lead people to underestimate the danger of the virus and also the importance of getting vaccinated despite recommendations by guidelines (CDC, 2021; ECDC, 2021). Additionally, as more people are getting vaccinated and the epidemiological situation improves, restrictions will decrease, and people still having lingering doubts about vaccination will be even less motivated to get vaccinated and may be tempted by free riding, benefitting from the immunity provided by others' vaccinations but hindering the protection of the whole community (Milman et al., 2021). From this perspective, it is essential to identify the predictors of vaccine acceptance and to establish who is likely to vacillate in their COVID-19 vaccination decision. In this study, conducted in the early stages of the vaccine roll-out in Italy, we first estimated the predictors of COVID-19 vaccination hesitancy and then modeled the additional effect of factors predicting a person's reluctance to vaccinate after testing positive for COVID-19 (i.e., post-positive reluctance) and factors predicting unwillingness to vaccinate while counting on others getting vaccinated (i.e., free riding). Investigating these factors will shed a unique light on vaccine acceptance and reluctance.
2. Methods
2.1. Participants
The online questionnaire was administered in two waves (January–February 2021) by a survey company (BDA-Doxa), which selected a national Italian representative sample (N = 5006), weighted by gender, age (18–70 years), area of residence, size of living center, education, and employment status (unemployed and employed). Employment status was further classified as unemployed, employed, and employed as a health worker. Details about the sampling strategy, response rates, and weights can be found in the supplementary materials (Method S1).
2.2. Materials and procedure
This cross-sectional study is part of a larger project promoted by the WHO Regional Office for Europe called “Monitoring knowledge, risk perceptions, preventive behavior and trust to inform pandemic outbreak response” and conducted in more than 30 countries (see WHO, 2021 for the full protocol). In Italy, the study has been approved by the Ethical Committee of the Italian coordinating institution (protocol 286/2020, registration ISRCTN 39724).
In the present study, we considered a subset of variables available in the entire dataset, including participants' Vaccine Hesitancy (VH) against SARS-CoV-2, post-positive reluctance, and free-riding intention, all rated on a 7-point response scale. In addition to the demographic variables used to collect the representative sample, participants were asked during the survey whether they suffered from chronic diseases and whether they had contracted COVID-19 (both “Yes,” “No,” “Do not know”), whether they knew people who had contracted the disease (“No,” “Yes and still alive,” “Yes, deceased”), and their employment status (“Unemployed,” “Employed,” “Employed as health worker”). Participants were asked about their concerns for the direct economic consequences of the pandemic (rated on a 7-point scale). The questionnaire also included the 5-item Conspiracy Mentality Questionnaire (Bruder et al., 2013) and three items taken from the Brief Resilience Scale (Smith et al., 2008). Finally, participants were asked whether they thought it would be appropriate for the entire population to follow national vaccination plans (vaccination propensity; “Yes,” “No,” “Do not know”). Questions related to other investigated domains are described in detail in the following section. The dataset has been uploaded on a public repository (https://doi.org/10.5281/zenodo.5040719).
2.3. Statistical analysis
2.3.1. Descriptive analysis
The study variables were summarized in frequency tables and figures (frequency for categorical variables, median and InterQuartile Range (IQR) for continuous variables). Non-parametric tests were computed to compare the distribution of variables on ordinal Likert scale across the two waves. Categorical variables were compared using chi-squared or Fisher's exact test where expected frequencies in any combination were less than 10. Statistical significance was assumed at the 5% level.
2.3.2. Dimensionality reduction - exploratory factor analyses
A total of 11 different Explorative Factorial Analyses (EFAs) were performed on groups of variables related to specific domains: 1) COVID-19 perceived risk, 2) Negative affective states, 3) Control, 4) Protective behaviors, 5) Trust in media information sources (e.g., traditional and social media), 6) Trust in health information sources (e.g., Ministry of Health, WHO), 7) Frequency of use of media information sources, 8) Frequency of use of health information sources, 9) Trust in health institutions, 10) Conspiracy-mindedness, and 11) Resilience. The metric invariance between the two waves was confirmed for each domain by a likelihood ratio test, allowing us to consider the two waves together in each EFA (Method S2).
Since the scales of all variables reported 7-point discrete ordinal values, each factorial analysis was performed on the polychoric correlation matrix, hypothesizing normally distributed continuous latent variables. We extracted from each EFA only the first factor, which explained the highest percentage of variance: the amount of variance explained by the one-factor solution was satisfactory, ranging from 44% to 68%, with the exception of COVID-19 perceived risk and Control, which explained a limited amount of variability (30% and 28%, respectively). The estimated loadings were then used to calculate the regression factor scores for both waves. Regression scores were categorized in tertiles (1st tertile = low risk; 2nd tertile = medium risk; 3rd tertile = high risk) for inclusion in the following regression models. For each EFA, the number and the name of items included, their internal consistency (Cronbach's α), the estimated loadings, and the proportion of deviance explained are reported in Table S1.
2.3.3. Cumulative logistic models
To evaluate which factors influenced the respondent's motivation to avoid this measure against COVID-19, we employed Cumulative Logistic Models (CLM): one model was estimated on VH, and two other models were used to predict vacillation (Method S2).
3. Results
3.1. Descriptive analysis
The main characteristics of the sample are reported in Table 1 .
Table 1.
Main characteristics of the sample, overall and by wave. Statistical significance in bold.
| Characteristics | Overall, N = 50061 | Wave |
P-value2 | |
|---|---|---|---|---|
| 1 (Jan. 8-18, 2021) N = 25041 |
2 (Feb. 8-19, 2021) N = 25021 |
|||
| Gender | 0.98 | |||
| Female | 2520 (50%) | 1260 (50%) | 1260 (50%) | |
| Male | 2486 (50%) | 1244 (50%) | 1242 (50%) | |
| Age-class | >0.99 | |||
| 18-34 | 1302 (26%) | 651 (26%) | 651 (26%) | |
| 35-44 | 962 (19%) | 482 (19%) | 480 (19%) | |
| 45-54 | 1185 (24%) | 592 (24%) | 593 (24%) | |
| 55-70 | 1557 (31%) | 779 (31%) | 778 (31%) | |
| Educational level | 0.043 | |||
| Low (0-8 ys) | 2052 (41%) | 1027 (41%) | 1025 (41%) | |
| Medium (9-13 ys) | 1602 (32%) | 767 (31%) | 835 (33%) | |
| High (13+ ys) | 1352 (27%) | 710 (28%) | 642 (26%) | |
| Geographical area | 0.99 | |||
| North-west | 1340 (27%) | 669 (27%) | 671 (27%) | |
| North-east | 964 (19%) | 484 (19%) | 480 (19%) | |
| Center | 966 (19%) | 479 (19%) | 487 (19%) | |
| South and islands | 1736 (35%) | 872 (35%) | 864 (35%) | |
| Employment status | 0.41 | |||
| Unemployed | 2371 (47%) | 1196 (48%) | 1175 (47%) | |
| Employed | 2431 (49%) | 1215 (49%) | 1216 (49%) | |
| Health care worker | 204 (4.1%) | 93 (3.7%) | 111 (4.4%) | |
| Vaccination propensity | 0.37 | |||
| Low | 3642 (73%) | 1800 (72%) | 1842 (74%) | |
| Medium | 590 (12%) | 307 (12%) | 283 (11%) | |
| High | 774 (15%) | 397 (16%) | 377 (15%) | |
| Vaccine hesitancy | 2 (1, 4) | 3 (1, 4) | 2 (1, 4) | 0.13 |
| Post positive reluctance | 2 (1, 4) | 2 (1, 4) | 2 (1, 4) | 0.82 |
| Free riding intention | 3 (2, 4) | 3 (1, 4) | 3 (2, 4) | 0.061 |
| Supporting public health policies | 5 (4, 5) | 5 (4, 5) | 5 (4, 5) | 0.056 |
| Economic concern | 5 (4, 6) | 5 (4, 6) | 5 (4, 6) | 0.97 |
| Chronic diseases | 0.71 | |||
| No | 3771 (75%) | 1874 (75%) | 1897 (76%) | |
| Don't know | 177 (3.5%) | 89 (3.6%) | 88 (3.5%) | |
| Yes | 1058 (21%) | 541 (22%) | 517 (21%) | |
| Previous COVID-19 disease | 0.015 | |||
| No | 4205 (84%) | 2129 (85%) | 2076 (83%) | |
| Don't know | 466 (9.3%) | 233 (9.3%) | 233 (9.3%) | |
| Yes | 335 (6.7%) | 142 (5.7%) | 193 (7.7%) | |
| COVID-19 contact | 0.10 | |||
| No | 1388 (28%) | 709 (28%) | 679 (27%) | |
| Yes, but still alive | 1591 (32%) | 818 (33%) | 773 (31%) | |
| Yes, deceased | 2027 (40%) | 977 (39%) | 1050 (42%) | |
Median (IQR) or frequency (%).
Pearson's chi-squared test; Wilcoxon rank sum test.
Due to the sampling strategy, the distribution of gender (50% females), age, employment, and geographical area of residence were the same in both waves (Table 1). Educational level was low in 41% of the sample, with a slight reduction in the number of respondents who were placed in the highest category in the second wave (p = 0.043). The VH was summarily low (median 2, Fig. 1 ), as well as the post-positive reluctance or the free-riding intention (high intention with values 6 or 7 for only 10.1% and 8.2%, respectively, of the sample), with no statistically significant difference between the two waves (Table 1, Fig. 1). In general, concerns about the economic consequences and the support of the public health policies were medium to high (median 5), while a relevant proportion (21%) of respondents reported the presence of a chronic disease. The lifetime prevalence of COVID-19 disease was 6.7%, with an increase in the second wave (from 5.7% in wave 1 to 7.7% in wave 2, p = 0.015); at least 40% of respondents knew someone who had died from COVID-19.
Fig. 1.
Marginal distribution of the baseline VH, and due to post-positive reluctance and to free riding intention.
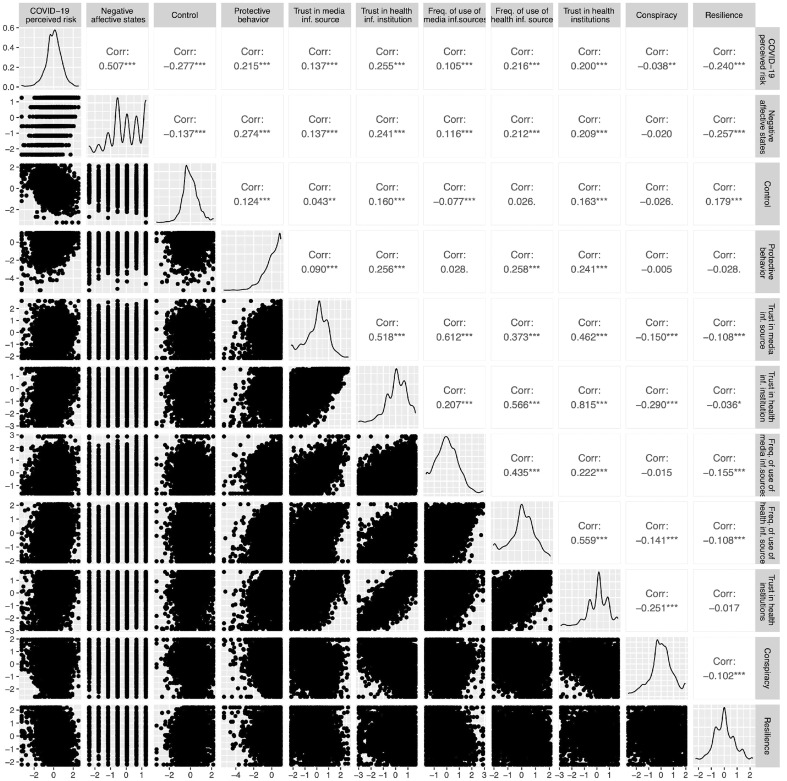
The pairwise marginal distribution and Spearman's correlations between 11 scores resulting from the EFAs performed on 11 dimensions are shown in Fig. 2 . We found good agreement between trust and frequency of use of information obtained from health institutions (Spearman's ρ = 0.57) and from media (ρ = 0.61). A strong correlation was seen between trust in health institutions and in the information they provide (ρ = 0.82). The COVID-19 perceived risk score was positively correlated with the negative affect score (ρ = 0.51) and negatively correlated with the score related to the feeling of control (ρ = −0.28).
Fig. 2.
Pairwise marginal distribution and Spearman's correlation§ between 11 regression scores resulted by the EFAs.
§Pairwise correlation test:*p < 0.05, **p < 0.01,***p < 0.001.
3.2. Cumulative logistic models
In Table 2 , the results of the first CLM regression showed no difference in the VH variable between waves. People over age 54 were less likely to report high VH compared to the reference group (age > years 54 vs. <34 years, OR: 0.73, 95%CI: 0.63–0.85), while females showed the opposite effects (OR: 1.22, 95%CI: 1.09–1.36). Respondents with higher education levels showed less VH (from medium OR: 0.87 to high OR: 0.66 with low educational level taken as reference) as did being a health care worker (OR: 0.64, 95%CI: 0.48–0.87). Having had a chronic disease decreased the probability of having high VH (OR: 0.82, 95%CI: 0.72–0.94), and a similar effect was attributable to the knowledge of someone who had died from COVID-19 (OR: 0.77; 95%CI: 0.67–0.88). Concerns about the economic consequences also moderately decreased the VH (OR: 0.71; 95%CI: 0.64–0.80). Having already had COVID-19 did not affect the VH. Agreeing with immunization practice strongly decreased the hesitancy to get a COVID-19 vaccine (medium vs. low OR: 0.39; 95%CI: 0.31–0.47; high vs. low OR: 0.05; 95%CI: 0.04–0.07). Belief in the appropriateness of the government measures against COVID-19 moderately decreased the probability of a higher VH (OR: 0.59; 95%CI: 0.51–0.69). Among the 11-dimensional scores, the following variables were statistically significant and were included in the model after a last check on their collinearity (Method S2): 1) COVID-19 perceived risk, 2) Negative affective states, 3) Protective behaviors, 4) Frequency of use of media information sources, 5) Frequency of use of health information sources, 6) Trust in health institutions, and 7) Conspiracy-mindedness. COVID-19 perceived risk, negative affective states, protective behaviors, trust in health information sources, frequency of use of health information sources, and trust in health institutions were reported to have a protective effect on VH, with ORs ranging from 0.88 (95%CI: 0.77–1.00) among those with medium (vs. low) COVID-19 perceived risk, to 0.49 (95%CI: 0.41–0.57) among respondents with a high (vs. low) trust in information from health institutions. High frequency of use of information provided by media information sources (OR: 1.22: 95%CI: 1.06–1.40) and a progressive adherence to conspiracy theories (OR: 1.40 and 1.89 in the medium vs. low and high vs. low category comparison, respectively) increased the hesitancy to get the COVID-19 vaccine.
Table 2.
Odds Ratios (ORs) estimated by a CLM regressiona on VH.
| Variables | OR | 95% CI | P-value |
|---|---|---|---|
| Wave [2nd] | 0.95 | 0.85–1.05 | 0.309 |
| Age-class [35-44] | 1.11 | 0.94–1.31 | 0.210 |
| Age-class [45-54] | 0.98 | 0.84–1.15 | 0.842 |
| Age-class [55-70] | 0.73 | 0.63–0.85 | <0.001 |
| Gender [female] | 1.22 | 1.09–1.36 | <0.001 |
| Educational level [medium] | 0.87 | 0.77–0.99 | 0.035 |
| Educational level [high] | 0.66 | 0.57–0.76 | <0.001 |
| Employment status [employed] | 1.10 | 0.98–1.23 | 0.098 |
| Employment status [health care worker] | 0.64 | 0.48–0.87 | 0.004 |
| Chronic disease [Don't know] | 0.97 | 0.72–1.29 | 0.825 |
| Chronic disease [yes] | 0.82 | 0.72–0.94 | 0.005 |
| Previous COVID-19 disease [Don't know] | 1.15 | 0.96–1.38 | 0.136 |
| Previous COVID-19 disease [yes] | 1.14 | 0.92–1.42 | 0.216 |
| COVID-19 contact [yes, but still alive] | 0.87 | 0.76–1.00 | 0.044 |
| COVID-19 contact [yes, deceased] | 0.77 | 0.68–0.88 | <0.001 |
| Economic concern [>5] | 0.71 | 0.64–0.80 | <0.001 |
| Vaccination propensity [medium] | 0.39 | 0.31–0.47 | <0.001 |
| Vaccination propensity [high] | 0.05 | 0.04–0.07 | <0.001 |
| Supporting public health policies [>5] | 0.59 | 0.51–0.69 | <0.001 |
| COVID-19 perceived risk [medium] | 0.88 | 0.77–1.00 | 0.057 |
| COVID-19 perceived risk [high] | 0.73 | 0.63–0.85 | <0.001 |
| Negative affective states [medium] | 0.80 | 0.70–0.92 | 0.001 |
| Negative affective states [high] | 0.68 | 0.59–0.79 | <0.001 |
| Protective behavior [medium] | 0.76 | 0.67–0.87 | <0.001 |
| Protective behavior [high] | 0.65 | 0.56–0.75 | <0.001 |
| Frequency of use of media information sources [medium] | 0.90 | 0.79–1.02 | 0.100 |
| Frequency of use of media information sources [high] | 1.22 | 1.06–1.40 | 0.005 |
| Frequency of use of health information sources [medium] | 0.79 | 0.69–0.91 | 0.001 |
| Frequency of use of health information sources [high] | 0.67 | 0.57–0.79 | <0.001 |
| Trust in health institution [medium] | 0.71 | 0.62–0.81 | <0.001 |
| Trust in health institution [high] | 0.49 | 0.41–0.57 | <0.001 |
| Conspiracy [medium] | 1.40 | 1.23–1.59 | <0.001 |
| Conspiracy [high] | 1.89 | 1.65–2.16 | <0.001 |
Reference category: Wave [1st], age-class [18-34], gender [male], educational level [low], employment status [unemployed], chronic disease [no], previous COVID-19 disease [no], COVID-19 contact [no], economic concern [≤5], vaccination propensity [low], supporting public health policies [≤5], COVID-19 perceived risk [low], negative affective states [low], protective behavior [low], frequency of use of media information sources [low], frequency of use of health information sources [low], trust in health institution [low], conspiracy [low].
Table 3 reports the results of the two models estimated for COVID-19 hesitancy due to a post-positive reluctance or a free-riding intention. In the first model, there was a slightly increased hesitancy in the second wave (+20% with respect to the first wave, 95%CI: 1.08 − 1.33), and the intention not to get the COVID-19 vaccine due to a previous contagion increased with age (from [35 − 44] vs. <35 OR: 1.07 to [55 − 70] vs <35 OR: 1.47; the last comparison p < 0.001), while a different behavior was found among those who relied on free riding (45–54 vs <35 OR: 0.84, p = 0.041). The educational level was not significant in the first model, while in the second one a high education had a protective effect on free riding (OR: 0.85; 95%CI: 0.74 − 0.99). Females reported an increase in the intention not to get the COVID-19 vaccine because of a previous contagion (OR: 1.21, 95%CI: 1.09 − 1.35). People who were not sure about a previous COVID-19 infection slightly increased their hesitancy (OR: 1.25; 95%CI: 1.05 − 1.49) because of a COVID-19 contagion occurred. As observed in the VH model, inclination to vaccination strongly predicted adherence to vaccination despite a previous contagion or a free-riding intention (OR of 0.59 and 0.43 in the first model, 0.95 and 0.56 in the second model for the comparison of high and medium vs. low class, respectively). Among the 11-dimensional scores, we considered the following in the models: 1) COVID-19 perceived risk (only in the first model), 2) Negative affective states, 3) Protective behaviors, 4) Frequency of use of media information sources, 5) Frequency of use of health information sources (only in the second model), 6) Trust in health information sources, 7) Conspiracy-mindedness, and 8) Resilience. COVID-19 perceived risk, negative affective states, adherence to protective behaviors, trust in health information sources, and resilience exercised a protective effect on the COVID-19 VH due to both conditions. An opposite effect to vaccine uptake was associated with a high level of conspiracy-mindedness, frequency of use of media information sources, and frequency of use of health information sources (only in the second model). For both post-positive reluctance and free-riding intention, we kept into account of the baseline individual VH. A strong and progressive adverse effect of the baseline VH was observed in the conditional VH, in particular among the lowest categories of conditional COVID-19 hesitancy (Table S2).
Table 3.
Adjusteda Odds Ratios (ORs) estimated by two separate CLM regressionsb on the vaccine hesitancy due to post-positive reluctance and free riding intention.
| COVID-19 vaccine hesitancy due to |
||||||
|---|---|---|---|---|---|---|
| Post-positive reluctance |
Free riding intention |
|||||
| Variables | OR | 95% CI | P-value | OR | 95% CI | P-value |
| Wave [2nd] | 1.20 | 1.08 – 1.33 | <0.001 | 1.10 | 0.99–1.22 | 0.091 |
| Age-class [35-44] | 1.07 | 0.91–1.26 | 0.407 | 0.89 | 0.75–1.06 | 0.187 |
| Age-class [45-54] | 1.17 | 1.00–1.37 | 0.046 | 0.84 | 0.72–0.99 | 0.041 |
| Age-class [55-70] | 1.47 | 1.28–1.70 | <0.001 | 0.91 | 0.78–1.06 | 0.218 |
| Gender [female] | 1.21 | 1.09 – 1.35 | <0.001 | 1.09 | 0.97–1.22 | 0.158 |
| Educational level [medium] | 1.00 | 0.89–1.13 | 0.965 | 0.91 | 0.80–1.04 | 0.161 |
| Educational level [high] | 1.12 | 0.97–1.28 | 0.119 | 0.85 | 0.74 – 0.99 | 0.036 |
| Previous COVID-19 disease [Don't know] | 1.25 | 1.05 – 1.49 | 0.013 | 0.88 | 0.73–1.06 | 0.176 |
| Previous COVID-19 disease [yes] | 1.07 | 0.87–1.32 | 0.497 | 1.22 | 0.98–1.51 | 0.077 |
| Employment status [employed] | 1.00 | 0.90–1.12 | 0.980 | 0.89 | 0.79–0.99 | 0.040 |
| Employment status [health care worker] | 0.90 | 0.68–1.18 | 0.440 | 0.73 | 0.54–1.00 | 0.049 |
| Vaccine propensity [medium] | 0.59 | 0.49–0.73 | <0.001 | 0.95 | 0.77–1.16 | 0.613 |
| Vaccine propensity [high] | 0.43 | 0.35–0.53 | <0.001 | 0.56 | 0.46–0.68 | <0.001 |
| COVID-19 perceived risk [medium] | 0.88 | 0.77–1.00 | 0.058 | |||
| COVID-19 perceived risk [high] | 0.78 | 0.68–0.91 | 0.001 | |||
| Negative affective states [medium] | 0.97 | 0.85–1.11 | 0.690 | 0.98 | 0.86–1.12 | 0.762 |
| Negative affective states [high] | 0.82 | 0.71–0.95 | 0.007 | 0.80 | 0.69–0.92 | 0.002 |
| Protective behavior [medium] | 0.99 | 0.87–1.12 | 0.851 | 0.88 | 0.77–1.01 | 0.061 |
| Protective behavior [high] | 0.85 | 0.75–0.98 | 0.022 | 0.79 | 0.68–0.91 | 0.001 |
| Freq. Of use of media information sources [medium] | 1.05 | 0.93–1.20 | 0.414 | 1.19 | 1.03–1.36 | 0.015 |
| Freq. Of use of media information sources [high] | 1.64 | 1.44–1.87 | <0.001 | 1.92 | 1.65–2.22 | <0.001 |
| Freq. of use of health information sources [medium] | – | – | – | 1.03 | 0.89–1.19 | 0.680 |
| Freq. of use of health information sources [high] | – | – | – | 1.34 | 1.13–1.58 | 0.001 |
| Trust in health institution [medium] | 0.92 | 0.81–1.05 | 0.214 | 0.92 | 0.81–1.06 | 0.266 |
| Trust in health institution [high] | 0.85 | 0.74–0.97 | 0.020 | 0.82 | 0.70–0.96 | 0.016 |
| Conspiracy [medium] | 1.15 | 1.01–1.30 | 0.029 | 1.30 | 1.13–1.49 | <0.001 |
| Conspiracy [high] | 1.34 | 1.18–1.53 | <0.001 | 1.49 | 1.29–1.71 | <0.001 |
| Resilience [medium] | 0.82 | 0.72–0.93 | 0.002 | 0.85 | 0.74–0.98 | 0.020 |
| Resilience [high] | 0.81 | 0.71–0.92 | 0.001 | 0.63 | 0.55–0.73 | <0.001 |
Adjusted for the vaccine hesitancy (VH) taken as continuous in a nominal form (see supplementary materials methods S2 and table S2).
Reference category: Wave [1st], age-class [18-34], gender [male], educational level [low], previous COVID-19 disease [no], employment status [unemployed], vaccine propensity [low], negative affective states [low], protective behavior [low], frequency of use of media information sources [low], frequency of use of health information sources [low], trust in health institution [low], conspiracy [low], resilience [low].
4. Discussion
4.1. Factors affecting VH
In line with the growing literature on the topic, our data confirmed several predictors of COVID-19 vaccination hesitancy. A decreased VH was associated with older age (Daly et al., 2021; Lazarus et al., 2020; Malik et al., 2020; KFF COVID-19 Vaccine Monitor - April, 2021; Murphy et al., 2021; Robertson et al., 2021; Schwarzinger et al., 2021; Seale et al., 2021; Soares et al., 2021), higher education level (Daly et al., 2021; Lazarus et al., 2020; Malik et al., 2020; Robertson et al., 2021; Schwarzinger et al., 2021), being a health worker (Gagneux-Brunon et al., 2021; Maltezou et al., 2021), having a chronic health condition (Schwarzinger et al., 2021; Seale et al., 2021; Soares et al., 2021), being in favor of vaccination in general (Attwell et al., 2021; Caserotti et al., 2021; Palamenghi et al., 2020; Schwarzinger et al., 2021), supporting public health policies (Soares et al., 2021), adopting recommended public health measures (Soares et al., 2021), higher risk perception (Attwell et al., 2021; Caserotti et al., 2021; Viswanath et al., 2021), trusting health sources of information (Murphy et al., 2021; Palamenghi et al., 2020), and trusting health institutions (Murphy et al., 2021; Viswanath et al., 2021).
Our data also confirmed that knowing someone who has been infected with COVID-19 decreased VH (e.g., Schwarzinger et al., 2021), as knowing someone who died of COVID-19. Furthermore, VH decreased for participants feeling strong negative affective states, similar to previous findings showing that COVID-19-related anxiety was positively associated with vaccine acceptance (Bendau et al., 2021). Our results also showed that worry about the future economic consequences of the pandemic decreased VH. While this is in line with the results of a Portuguese study showing that loss of income during the pandemic was a positive predictor of vaccine intention (Soaes et al., 2021), other studies conducted in Germany found an inverse relationship between economic fears and vaccine acceptance (Bendau et al., 2021) or no relationship with non-pharmaceutical intervention acceptance (Rosman et al., 2021).
Reduced vaccination intentions were associated with female gender (Daly, 2021; Lazarus et al., 2020; Murphy et al., 2021; Robertson et al., 2021; Schwarzinger et al., 2021; Soares et al., 2021; Ishimaru et al., 2021; but see also Caserotti et al., 2021; Seale et al., 2021), high trust in media information sources (Murphy et al., 2021), and high conspiracy-mindedness (Murphy et al., 2021).
4.2. Vacillation: Post-positive reluctance and free-riding intention
We also aimed at investigating which factors hinder vaccination hesitancy among people who tested positive for COVID-19 and among those who counted on others getting vaccinated. Those who were more likely to vacillate in their COVID-19 intention, both for post positive reluctance and free riding intention, had medium or high frequency of use of media information and medium or high levels of conspiracy-mindedness. A high frequency of use of health information sources only increased the free riding intention. This might be moderated by the protective role played by trust in health information sources, which is highly correlated with their use. Additionally, not knowing exactly if you have had COVID-19, older age (over 55 vs. younger than 35) and female gender increased specifically post-positive reluctance, as did answering the questionnaire later on (wave: February vs. January). It is important to note that during the first months of the vaccination campaign in Italy, it was mainly health professionals, people with high-risk medical conditions, and those over 80 who were vaccinated, and that those infected with COVID-19 were to wait at least 90 days after the documented infection before being vaccinated.
In both instances, people vacillated less in their COVID-19 vaccination intention in cases of high propensity for vaccination in general, adoption of recommended public health measures, high negative affective states, high trust in health information sources, and medium to high (vs. low) levels of resilience. High (vs. low) perception of risk related to COVID-19 only reduces post-positive reluctance. In contrast, high (vs. low) education level is a protective factor that reduces the free-riding intention, such as being employed or employed as a health care worker (vs. being unemployed) and being between the ages of 45 and 54 as opposed to younger (under 35). The latter result needs to be carefully considered, as younger people are less likely to develop serious health consequences but can still spread the disease to older persons. To promote adequate adherence to vaccine campaigns, several governments have resorted to behavioral strategies specifically addressed to young people. For example, some US states have offered college scholarships or travel incentives; others have held a lottery for the vaccinated with prizes up to million dollars, in addition to walk-ins (during which people can be vaccinated without booking) to encourage those on the fence to get vaccinated. The enthusiastic adherence to these initiatives may depend not only on the attractiveness of the conditions but also on the overt positive consequences of COVID-19 vaccination, such as getting the vaccine passport or green pass and restarting one's social life. Despite the goal of maximizing vaccination, we should carefully reflect on the ethical issues related to some incentives used to encourage vaccinations: free marijuana (Washington State, 2021), alcohol (New Jersey, 2021), and hunting shotguns (West Virginia, 2021).
Additionally, it should be pointed out that the COVID-19 pandemic has fueled conspiracy beliefs with some people questioning the safety of vaccines and viewing the incentives as “bribes.” Moreover, incentives are aimed not only at the “maybes” (Attwell et al., 2021) but also at those who would have been vaccinated anyway, resulting in a large waste of resources that might be used to promote more targeted interventions to increase, for example, confidence in vaccines among vulnerable and underserved groups (Curtis et al., 2021). Further, given that convenience (e.g., free administration, ease of access, time, and place) affects uptake of the vaccine (Betsch et al., 2018; MacDonald, 2015), these resources could be used, for example, to ensure compensation for lost wages among those who take time off work to be vaccinated, or to ensure convenient vaccination times and spaces, by securing widespread access to vaccines.
While incentives are mainly directed at individuals, evidence is growing about the benefits of vaccines for the community too, although the issue is complex and dynamic (Milman et al., 2021). Protecting vulnerable people in the community is a common benefit of most vaccines, and there is some evidence that efforts to improve understanding of community immunity (e.g., Hakim et al., 2020) may increase vaccination intention (Arnesen et al., 2018; Betsch et al., 2017; Logan et al., 2018). Some studies suggest that stressing the pro-social benefits of vaccination might not be as decisive as focusing on aspects related to one's own emotions (Chou and Budenz, 2020; Gavaruzzi et al., 2021; Tomljenovic et al., 2020). In the COVID-19 context, prosocial messages seem to be effective in promoting protective behavior (e.g., Jordan et al., 2020), but this may be driven by the protection of closer circles rather than by the community at large (Banker and Park, 2020). It remains to be determined whether the pandemic has changed the way people understand community immunity and whether it can foster vaccine acceptance.
Finally, we have all testified that the pandemic has been accompanied by an infodemic (Zarocostas, 2020), with social media often considered as one of the factors contributing to vaccine hesitancy and anti-vaccine sentiment (e.g., Basch et al., 2021), even if they can also be leveraged to promote critical thinking using pre-inoculation against fake news (Banas and Rains, 2010; van der Linden and Roozenbeek, 2021). Pre-inoculation could be effective also for a segment of hesitant people who adhere to conspiracy beliefs, as it leverages people's fear of manipulation, to alert them against misinformation (Basol et al., 2021; Lewandowsky et al., 2021; van der Linden et al., 2020).
We view these results as useful pieces of a puzzle in which psychological aspects must be considered to better understand vaccination intention.
4.3. Limitations
This study's main limitation is that we assessed intention, and, while intention is considered the best predictor of behavior, there might be mediating factors between the two (Brewer et al., 2017). Another limitation is that we asked participants whether they had SARS-CoV-2 without inquiring about the timing of infection. Indeed, having already had COVID-19 reduced the baseline VH (Table 2), but it did not affect conditional hesitancy (Table 3). This might be because people who got infected were included without being asked how long ago they had had it. As clear information about the duration of antibodies following infection is still lacking, it is possible that those who had it more recently are more reluctant to get vaccinated than those who had it earlier on in the pandemic. Finally, the two conditional hesitations are not mutually exclusive events and further analysis could clarify how the estimates would change taking into account their competitive effect.
5. Conclusion
Despite the constant monitoring of the efficacy of vaccines against new variants of the virus, adequate vaccination coverage undoubtedly remains one of the best weapons we have to prevent SARS-CoV-2 infection. It is therefore evident how crucial it is to know people's response to vaccination campaigns, as the context changes. The unprecedented analyses considered in this paper confirmed the importance of investigating how the predictors of post-positive reluctance and free-riding intention affect COVID-19 VH.
Funding
This work was supported by Fondazione Cariplo (grant n° 2020-5195), the Italian Ministry of Health (Ricerca Corrente), and IRCCS Centro San Giovanni di Dio Fatebenefratelli institutional resources.
Declaration of Competing Interest
All authors declare that they have no competing interests to be disclosed.
Acknowledgments
Acknowledgments are due to Katrine Bach Habersaat and Martha Scherzer (Insights Unit, World Health Organization Regional Office for Europe, Copenhagen, Denmark); they tirelessly developed the European project and ensured valuable support for the conduct of the survey in Italy. Thanks are due to Roberta Ghidoni (Scientific Director, IRCCS Fatebenefratelli, Brescia) for the enthusiasm she put into this initiative: her strong commitment was a key factor in allowing the survey to take off. Carlo Mango, Diana Pozzoli, and Beatrice Fassati (Fondazione CARIPLO, Milan) provided an invaluable support, which made the survey possible. Twenty years after our initial close collaboration in the framework of the World Mental Health Survey Initiative, Vilma Scarpino and Valeria Reda (BVA-Doxa, Milan) guaranteed perfect planning and organization of the fieldwork and took care of many requests from the participating researchers. Finally, Gustavo Calcagno Baldini made possible the initial contacts with some of the institutions involved in the project.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2021.106885.
Appendix A. Supplementary data
Supplementary material
References
- Arnesen S., Bærøe K., Cappelen C., Carlsen B. Could information about herd immunity help us achieve herd immunity? Evidence from a population representative survey experiment. Scand. J. Public Health. 2018;46(8):854–858. doi: 10.1177/1403494818770298. [DOI] [PubMed] [Google Scholar]
- Attwell K., Lake J., Sneddon J., Gerrans P., Blyth C., Lee J. Converting the maybes: crucial for a successful COVID-19 vaccination strategy. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0245907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banas J.A., Rains S.A. A meta-analysis of research on inoculation theory. Commun. Monogr. 2010;77(3):281–311. doi: 10.1080/03637751003758193. [DOI] [Google Scholar]
- Banker S., Park J. Evaluating prosocial COVID-19 messaging frames: evidence from a field study on Facebook. Judgm. Decis. Mak. 2020;15(6):1037–1043. doi: 10.2139/ssrn.3684901. [DOI] [Google Scholar]
- Basch C.E., Basch C.H., Hillyer G.C., Meleo-Erwin Z.C., Zagnit E.A. YouTube videos and informed decision-making about COVID-19 vaccination: successive sampling study. JMIR Public Health Surveill. 2021;7(5) doi: 10.2196/28352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basol M., Roozenbeek J., Berriche M., Uenal F., McClanahan W.P., Linden S.V.D. Towards psychological herd immunity: cross-cultural evidence for two prebunking interventions against COVID-19 misinformation. Big Data Soc. 2021;8(1) doi: 10.1177/20539517211013868. [DOI] [Google Scholar]
- Bendau A., Plag J., Petzold M.B., Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021;97:107724. doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betsch C., Böhm R., Korn L., Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat. Hum. Behav. 2017;1(3):0056. doi: 10.1038/s41562-017-0056. [DOI] [Google Scholar]
- Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer N.T., Chapman G.B., Rothman A.J., Leask J., Kempe A. Increasing vaccination: putting psychological science into action. Psychol. Sci. Public Interest. 2017;18(3):149–207. doi: 10.1177/1529100618760521. [DOI] [PubMed] [Google Scholar]
- Bruder M., Haffke P., Neave N., Nouripanah N., Imhoff R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: conspiracy mentality questionnaire. Front. Psychol. 2013;4:225. doi: 10.3389/fpsyg.2013.00225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caserotti M., Girardi P., Rubaltelli E., Tasso A., Lotto L., Gavaruzzi T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021;113688 doi: 10.1016/j.socscimed.2021.113688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirumbolo S. Vaccination hesitancy and the “myth” on mRNA-based vaccines in Italy in the COVID-19 era: does urgency meet major safety criteria? J. Med. Virol. 2021 doi: 10.1002/jmv.26922. 10-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou W.Y.S., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- Curtis H.J., Inglesby P., Morton C.E., MacKenna B., Walker A.J., Morley J.…Goldacre B. Trends and clinical characteristics of COVID-19 vaccine recipients: a federated analysis of 57.9 million patients' primary care records in situ using OpenSAFELY. medRxiv. 2021 doi: 10.1101/2021.01.25.21250356v3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Jones A., Robinson E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to march 29, 2021. JAMA. 2021;325(23):2397–2399. doi: 10.1001/jama.2021.8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., Botelho-Nevers E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J. Hosp. Infect. 2021;108:168–173. doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavaruzzi T., Caserotti M., Leo I., Tasso A., Speri L., Ferro A.…Lotto L. The role of emotional competences in Parents' vaccine hesitancy. Vaccines. 2021;9(3):298. doi: 10.3390/vaccines9030298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakim H., Bettinger J.A., Chambers C.T., Driedger S.M., Dubé E., Gavaruzzi T.…Witteman H.O. A web application about herd immunity using personalized avatars: development study. J. Med. Internet Res. 2020;22(10) doi: 10.2196/20113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishimaru T., Okawara M., Ando H., Hino A., Nagata T., Tateishi S.…Fujino Y. Gender differences in the determinants of willingness to get the COVID-19 vaccine among the working-age population in Japan. medRxiv. 2021 doi: 10.1101/2021.04.13.21255442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan J., Yoeli E., Rand D. Don't get it or don't spread it? Comparing self-interested versus prosocially framed COVID-19 prevention messaging. PsyArXiv. 2020 doi: 10.31234/osf.io/yuq7x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J.V., Wyka K., Rauh L., Rabin K., Ratzan S., Gostin L.O.…El-Mohandes A. Hesitant or not? The association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J. Health Commun. 2020;25(10):799–807. doi: 10.1080/10810730.2020.1868630. [DOI] [PubMed] [Google Scholar]
- Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowsky S., Cook J., Schmid P., Holford D.L., Finn A., Leask J.…Vraga E.K. The COVID-19 Vaccine Communication Handbook. 2021. https://sks.to/c19vax A practical guide for improving vaccine communication and fighting misinformation.
- Limaye R.J., Sauer M., Truelove S.A. Politicizing public health: the powder keg of rushing COVID-19 vaccines. Hum. Vaccines Immunother. 2021;17(6):1662–1663. doi: 10.1080/21645515.2020.1846400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Linden S., Roozenbeek J. The Psychology of Fake News: Accepting, Sharing, and Correcting Misinformation. Taylor & Francis Group; 2021. Psychological inoculation against fake news. [Google Scholar]
- van der Linden S., Roozenbeek J., Compton J. Inoculating against fake news about COVID-19. Front. Psychol. 2020;11:2928. doi: 10.3389/fpsyg.2020.566790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan J., Nederhoff D., Koch B., Griffith B., Wolfson J., Awan F.A., Basta N.E. ‘What have you HEARD about the HERD?’Does education about local influenza vaccination coverage and herd immunity affect willingness to vaccinate? Vaccine. 2018;36(28):4118–4125. doi: 10.1016/j.vaccine.2018.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maltezou H.C., Pavli A., Dedoukou X., Georgakopoulou T., Raftopoulos V., Drositis I.…Sipsas N.V. Determinants of intention to get vaccinated against COVID-19 among healthcare personnel in hospitals in Greece. Infection, Dis. Health. 2021 doi: 10.1016/j.idh.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman O., Yelin I., Aharony N., Katz R., Herzel E., Ben-Tov A.…Kishony R. Community-level evidence for SARS-CoV-2 vaccine protection of unvaccinated individuals. Nat. Med. 2021:1–3. doi: 10.1038/s41591-021-01407-5. [DOI] [PubMed] [Google Scholar]
- Murphy J., Vallières F., Bentall R.P., Shevlin M., McBride O., Hartman T.K.…Hyland P. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021;12(1):1–15. doi: 10.1038/s41467-020-20226-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur. J. Epidemiol. 2020;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M.…Benzeval M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosman T., Kerwer M., Steinmetz H., Chasiotis A., Wedderhoff O., Betsch C., Bosnjak M. Will COVID-19-related economic worries superimpose health worries, reducing nonpharmaceutical intervention acceptance in Germany? A prospective pre-registered study. Int. J. Psychol. 2021 doi: 10.1002/ijop.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale H., Heywood A.E., Leask J., Sheel M., Durrheim D.N., Bolsewicz K., Kaur R. Examining Australian public perceptions and behaviors towards a future COVID-19 vaccine. BMC Infect. Dis. 2021;21(120):1–9. doi: 10.1186/s12879-021-05833-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int. J. Behavl Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R.…Nunes C. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorp H.H. A dangerous rush for vaccines. Science. 2020;369(6506):885. doi: 10.1126/science.abe3147. [DOI] [PubMed] [Google Scholar]
- Tomljenovic H., Bubic A., Erceg N. It just doesn't feel right–the relevance of emotions and intuition for parental vaccine conspiracy beliefs and vaccination uptake. Psychol. Health. 2020;35(5):538–554. doi: 10.1080/08870446.2019.1673894. [DOI] [PubMed] [Google Scholar]
- Ullah I., Khan K.S., Tahir M.J., Ahmed A., Harapan H. Myths and conspiracy theories on vaccines and COVID-19: Potential effect on global vaccine refusals. Vacunas. 2021;22(2):93–97. doi: 10.1016/j.vacun.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanath K., Bekalu M., Dhawan D., Pinnamaneni R., Lang J., McLoud R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. 2021;21(818) doi: 10.1186/s12889-021-10862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Web references
- CDC Vaccines for COVID-19. 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.htm Retrieved at. last accessed on June 28th, 2021.
- ECDC Questions and Answers on COVID-19. 2021. https://www.ecdc.europa.eu/en/covid-19/questions-answers Retrieved at. last accessed on June 28th, 2021.
- Imperial College London Global Attitudes Towards a COVID-19 Vaccine as of February 2021. 2021. https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/EMBARGOED-0502.-Feb-21-GlobalVaccineInsights_ICL-YouGov-Covid-19-beavior-Tracker_20210301.pdf Retrieved at. last accessed on June 28th, 2021.
- Johns S., van Elsland S.L. COVID-19 Vaccine Hesitancy Could Lead to Thousands of Extra Deaths. 2021. www.imperial.ac.uk/news/218313/covid-19-vaccine-hesitancy-could-lead-thousands/ Retrieved at. last accessed on June 28th, 2021.
- KFF COVID-19 Vaccine Monitor. 2021. https://www.kff.org/report-section/kff-covid-19-vaccine-monitor-april-2021-findings Retrieved at. last accessed on June 28th, 2021.
- New Jersey State Governor Murphy Announces New Incentives to Encourage COVID-19 Vaccinations, Including Free Entrance to State Parks and Free Wine at Participating Wineries. 2021. https://nj.gov/governor/news/news/562021/approved/20210519a.shtml Retrieved at. last accessed on June 28th, 2021.
- Washington State LCB Allows “Joints for Jabs” Promotions to Support Vaccinations. 2021. https://content.govdelivery.com/accounts/WALCB/bulletins/2e303d6 Retrieved at. last accessed on June 28th, 2021.
- West Virginia State COVID-19 UPDATE: Gov. Justice Provides Additional Details on Vaccine Lottery Giveaway. 2021. https://governor.wv.gov/News/press-releases/2021/Pages/COVID19-UPDATE-Gov.-Justice-provides-additional-details-on-vaccine-lottery-giveaway.aspx last accessed on June 28th, 2021.
- WHO Survey Tool and Guidance: Behavioural Insights on COVID-19, 29 July 2020 (produced by the WHO-European Region) 2021. https://www.euro.who.int/en/health-topics/health-emergencies/publications/2020/survey-tool-and-guidance-behavioural-insights-on-covid-19-produced-by-the-who-european-region last accessed on June 28th, 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material