Abstract
Background
While literature on psychological consequences among frontline healthcare workers (HCWs) flourishes, understanding the psychological burden on this group is particularly crucial, as their exposure to COVID-19 makes them especially at high risk. We explored what is known about psychological effects of the COVID-19 pandemic on emergency HCWs.
Methods
We used a scoping review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews.
Results
The search identified 5432 articles, from which a total of 21 were included in the final review. Anxiety, burnout, depression, inadequate sleep, post-traumatic stress disorder (PTSD) symptoms, distress/stress and secondary trauma, were all reportedly experienced by emergency HCWs. Anxiety, burnout, depression and stress levels were higher among physicians and nurses compared to others. Post-traumatic stress disorder symptoms were higher among reserve medics, while Red Cross volunteers developed similar reactions of psychological stress and secondary trauma to other healthcare workers. Male HCWs reported more post-traumatic stress disorder symptoms than females, while stress was higher among females than male HCWs.
Conclusions
Emergency HCWs providing care during the COVID-19 pandemic are at risk from specific psychological impacts, including anxiety, burnout, depression, inadequate sleep, PTSD symptoms, psychological distress/stress and secondary trauma, and stress
Tweetable abstract
Emergency healthcare workers are at direct risk of psychological impacts from the COVID-19 pandemic.
Keywords: COVID-19, Emergency, Healthcare worker, Mental health, Psychological impact, Scoping review
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been an ongoing crisis since it was declared a public health emergency of international concern in January 2020 [1]. While vaccines against COVID-19 are currently available, the number of cases as of March 30, 2021 continues to increase, surpassing 127.9 million, with deaths reaching 2.7 million globally [2]. According to the World Health Organization [3], COVID-19 causes severe acute respiratory syndrome (SARS) related to SARS-associated coronavirus (SARS-CoV) disease in 2002–2003. Currently, management of the pandemic has caused confinement and movement restrictions, economic and educational shutdowns, overwhelmed healthcare systems, and provoked mixed negative emotions (e.g., fear, anxiety, worries, anger, and sadness), affecting the overall wellbeing of the public [4], [5], [6], as well as healthcare workers (HCWs).
HCWs are at high risk of contracting COVID-19 [7], [8]. Data obtained between 22 July and 15 August 2020 from 37 countries, WHO reported 570,000 HCWs were infected and 2500 had died due to the infection [5]. Additionally, a systematic review in 2020 revealed that Europe had the highest absolute numbers of morbidity (119,628 HCWs), while the Eastern Mediterranean region had the highest mortality, at 5.7 per 100 infections compared to other regions [9]. Considering the high burden resulting from the pandemic, there is an emergent need for efforts to protect and lower the risk of infection among HCWs across the globe by providing sufficient personal protective equipment (PPE), appropriate preparedness and response, training, food and rest, address fatigue, and counteract psychosocial impacts through family and psychological support [8], [10], [11], [12].
Literature on psychological consequences, including depression, anxiety and stress, and coping of frontline HCWs responding on the frontline and providing care to COVID-19 patients is emerging. The duration of the pandemic has already exceeded one year to the writing of this review and could affect the psychological status of emergency HCWs. Understanding the psychological burden on this group is particularly crucial, as their exposure to COVID-19 makes them especially at high risk to psychological distress [13]. Hence, this scoping review aimed to examine and summarise the reported effects of the COVID-19 pandemic on psychological status of emergency HCWs.
Objective of the study
This review was conducted to explore what is currently known about the psychological status of emergency HCWs arising from the COVID-19 pandemic. The primary research question guiding this review was: What are the reported effects of the COVID-19 pandemic on the psychological status of emergency healthcare workers? The aim of the review was to identify and summarise available research on the topic, and to determine areas of opportunity for future research focused on enhancing psychological support for emergency HCWs.
Methods
Research design
This study employed a scoping review design. Scoping reviews enable assessment of the potential size and scope of available research literature, to identify the nature and extent of research evidence on a topic [14]. As a means of synthesising broad ranging, available literature, scoping review methodology is continuing to evolve and reviews are becoming increasingly rigorous [15]. This methodology was chosen because it facilitated an efficient and focused review of the scope, nature, and extent of effects of the COVID-19 pandemic on the psychological status of emergency HCWs. This scoping review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA–ScR; [16]), (Supplementary File 1).
Inclusion criteria
Types of participants
In this review, studies were included that focused on emergency HCWs during the COVID-19 pandemic. HCWs included emergency department physicians, nurses, paramedics (including medical technicians, ambulance drivers, and reserve medics), advanced practice providers, and emergency volunteers (e.g., Red Cross).
Concept
The core concept underpinning the review was reported psychological conditions and manifestations, with the outcome being psychological impact.
Context
The context for the review was that of being an emergency HCW.
Types of sources
The review included qualitative or quantitative, and mixed-methods studies, along with review articles in English or Arabic language.
Information sources and search strategy
An initial search to identify key search terms was developed by all authors in consultation with an expert librarian. Databases searched were MEDLINE (Ovid), PsycINFO (Ovid), CINAHL (EBSCO), ProQuest Central, EMBASE (Ovid), Web of Science/Scopus, DOAJ, Saudi Digital Library (Arabic Language), and King Fahad National Library (Arabic Language) between February 2018 and March 2021. The search used the following Boolean keywords and medical subject headings (MeSH) search terms: “health worker” or “health professional”, “physician” or “doctor” or “medical personnel”, “nurse”, “ambulance” or “paramedic” or “medical technician”, “clinician”, “frontline”, “psychological” or “mental”, “stress”, “depress”, “burnout”, “anxiety”, “fear”, “helpless”, “PTSD”, “health”, “emergency” or “ED”, “COVID-19” or “COVID” or “coronavirus”. The search was restricted to full text papers published in English or Arabic. The search was limited to the years 2020–2021 being the duration of COVID-19. The search engine Google Scholar and reference lists from included studies were also searched for additional sources. Studies reporting effects on physical health, non-emergency health worker, commentaries, discussion papers, narratives, opinion pieces, editorials, and grey literature were excluded.
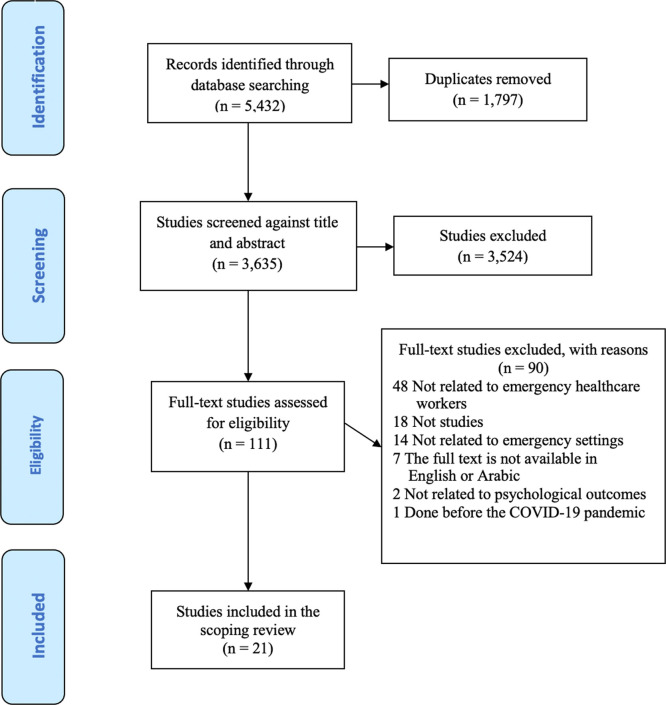
Selection and extraction
Two researchers independently assessed studies at each point, namely titles and abstracts and full-text screening, using Covidence Systematic Review Software [17], and conflicts were resolved by a third researcher. The PRISMA flow diagram shows the process of searching, screening, and selecting the studies (see Fig. 1). A total of 5432 titles and abstracts were screened with the following search results, MEDLINE (538), PsycINFO (33), CINAHL (1224), ProQuest Central (1125), EMBASE (1712), Web of Science/Scopus (724), DOAJ (52), Saudi Digital Library (9), and King Fahad National Library (15). After duplicates were removed, 3635 records remained. Titles and abstracts were reviewed for relevance with 111 studies subjected to further review. Out of the 111 studies, 90 were excluded with reasons including no ED specific data and/or ED setting was difficult to identify.
Fig. 1.
PRISMA flow chart of the scoping review.
In total, 21 studies were included in the final review. Data extraction tables were developed by the researchers and were divided into two parts. The first part ( Table 1) included general study characteristics, including author, year, country of origin, study aim, study design, participants, key findings, limitations and quality appraisal score using the Joanna Briggs Institute (JBI) guidelines [18]. The second part ( Table 2) comprised of specific characteristics, including measurement tool/s, reported conditions, manifestations, and impact.
Table 1.
General study characteristics.
| Author, year, country of origin | Study aim | Study design | Participants (n) |
Key findings | Limitations | Quality appraisal (JBI score) |
|---|---|---|---|---|---|---|
| Altinbilek et al. (2021) Turkey [31] |
To investigate the stress and anxiety of healthcare workers due to COVID-19 | Prospective multi-centre survey in two hospitals | 205 ED healthcare workers | Physicians and nurses had higher anxiety and stress scores than other staff, and scores of nurses were significantly higher than physicians (p < 0.05). | Survey was conducted online for only one week with no evidence of reminder. | 10/12 |
| An et al. (2020) China [23] |
To examine the prevalence of depressive symptoms (depression hereafter) and their correlates and association between depression and quality of life | National, cross-sectional online survey | 1103 frontline ED nurses | Overall prevalence of depression in nurses was 43.61% (95% CI = 40.68–46.54%). Multiple logistic regression analysis revealed that working in tertiary hospitals (OR = 1.647, p = 0.009), direct patient care of COVID-19 patients (OR = 1.421, p = 0.018), and current smokers (OR = 3.843, p < 0.001) were significantly associated with depression. | Some variables associated with depression, such as social support, collegial relationship, health status and pre-existing psychiatric disorders, were not examined. Because of the cross-sectional study design, causality between depression and other variables could not be examined. | 8/8 |
| More than 90% of participants were female nurses, which may have biased the findings. | ||||||
| Araç and Dönmezdil (2020) Turkey [28] | To examine psychiatric disorders such as anxiety, depression and sleep disorders among healthcare professionals working in an emergency department and a COVID-19 clinic | Cross-sectional survey | 198 healthcare professionals: 100 in ED and 98 in a COVID-19 clinic | Perceived stress levels and PSQI sub-scores were found to be significantly higher among volunteers working in the emergency department than among those in other departments. The risk of development of anxiety among women was 16.6 times higher than among men. | The study was conducted at a single academic medical centre at one point in time and was limited to a relatively small sample size and low response rate. The authors also identified there were limitations of the tests used in the study. | 8/8 |
| Gender (OR = 16.631, p 0.001), profession (physicians, OR = 8.750, p = 0.022; nurses, OR = 4.845, p = 0.045), HADS-depression (OR = 9.194, p = 0.002), the use of sleeping medication subscale score of the PSQI (OR = 6.357, p = 0.012), and the perceived stress level (OR = 8.639, p = 0.003) were found to be effective risk factors of mental health. | ||||||
| Baumann et al. (2021) USA [21] | To provide a longitudinal assessment of anxiety levels and work and home concerns of U.S. emergency physicians during the COVID-19 pandemic | Longitudinal, cross-sectional email survey | 262 physicians | In examining the relationship between demographics, living situations, and institution location on having a PC-PTSD-5 score ≥ 3, only female sex was associated with a PC-PTSD-5 score ≥ 3 (adjusted OR = 2.48, 95% CI = 1.28–4.79). | The researchers reported a low response rate (61.5%) and no sample size calculation was evident. | 8/8 |
| There were different phases of the pandemic at various sites during the study period so responses at the time of reporting may vary. | ||||||
| A lack of baseline stress, burnout and PTSD measures from before the pandemic is problematic. | ||||||
| The authors noted a discrepancy between median burnout stress scores and PC-PTSD-5 screener ≥ 3 scores. | ||||||
| Caliskan and Dost (2020) Turkey [29] | To evaluate emergency physicians’ levels of depression and anxiety in dealing with the COVID-19 pandemic | Descriptive, cross-sectional study using an online questionnaire | 290 emergency physicians | According to the physicians’ HADS scores, depression was detected in 180 participants (62%) while anxiety was detected in 103 (35.5%), with median depression and anxiety scores found to be 8 (0–21) and 7 (0–21), respectively. | The data and relevant analyses presented were derived from a cross-sectional study design. Thus, it was difficult to make causal inferences. Secondly, the authors used a web-based survey method to avoid bias, necessitating inclusion of volunteer participants; therefore, the possibility of selection bias should be considered. | 7/8 |
| Cui et al. (2020) China [24] | To identify the impact of COVID-19 on the psychology of Chinese nurses in emergency departments and fever clinics and to identify associated factors | Online cross-sectional study | 453 nurses in ED and fever clinics | Fear of infecting family members was the most influential and predictive of anxiety (β = 0.263, p = 0.000), stress (β = 0.239, p = 0.000), and inverse stress coping tendency (β = − 0.188, p = 0.000) of nurses. | The method of snowball sampling may reduce generalisability of the results. Secondly, the data’s cross-sectional nature constrained making causal links among anxiety, stress, and coping tendency. Finally, the survey relied only on self-reported questionnaires, which may reduce data collection objectivity. | 7/8 |
| de Wit et al. (2020) Canada [39] | To report burnout time trends and describe psychological effects of working as a Canadian emergency physician during the first weeks of the coronavirus disease 2019 (COVID-19) pandemic | Mixed-methods study (both quantitative and qualitative) | 468 physicians | Being tested for COVID-19 (OR = 11.5, 95% CI = 3.1–42.5) and the number of shifts worked (OR = 1.3, 95% CI = 1.1–1.5 per additional shift) were associated with high emotional exhaustion. Having been tested for COVID-19 (OR = 4.3, 95% CI = 1.1–17.8) was also associated with high depersonalisation. | The authors identified possible reasons why the study did not establish association between burnout and progression of time during the first weeks of the pandemic including: | 7/10 & 8/8 |
| (1) psychological distress was associated with high levels of exposure to traumatic events, which may explain the lack of worsening burnout levels over time during the pandemic where the cohort possibly did not experience rigorous numbers of sick patients seen in other parts of the world. | ||||||
| (2) mental health effects of the pandemic, particularly burnout, may have been measured too soon after the start of the pandemic. | ||||||
| Elhadi et al. (2021) Libya [34] | To examine prevalence of anxiety, depression, and burnout among frontline emergency physicians of the COVID-19 pandemic | Cross-sectional survey | 154 physicians | Comparison between groups of physicians experiencing anxiety (HADS anxiety ≥ 11) and depression (HADS depression ≥ 11) demonstrated the following elements to be statistically significant: for anxiety, only age range, working hours per week, and transport issues were associated with a higher prevalence of anxiety (p < 0.05). | Firstly, the study focused only on one country, where several additional and unique factors may have contributed to high levels of mental distress. These aspects may, in turn, have aggravated COVID-19 effects. Furthermore, interviewer bias may be present, as some respondents may have opted to hide or alter their responses out of a fear of stigmatisation, despite the anonymous nature of the survey. Additionally, due to the cross-sectional study design, lower causation and linkage ability may be apparent. | 7/8 |
| Fitzpatrick et al. (2020) USA [19] | To determine the effect that the COVID-19 pandemic had on the wellness of emergency physicians | Prospective survey | 55 physicians | During the pandemic, emergency physicians felt less in control (p = 0.001); felt decreased happiness while at work (p = 0.001); had more trouble falling asleep (p = 0.001); had increased sense of dread when thinking of work needing to be done (p = 0.04); felt more stress on days not at work (p < 0.0001) and were more concerned about their own health (p < 0.0001). | The sample size (n = 55) was relatively small. The population originated from a single hospital network, was a convenience sample, and was limited by non-response bias. Survey questions were derived from a previously validated study, but the specific question that subjects answered might not have covered the broad range of physician wellness. The survey used physician self-report of feelings up to six months earlier, which introduced the potential for recall bias, as well as social-desirability bias. Even though statistical significance was found in several questions, there may not be clinical significance given how similar the medians and/or general distribution of scores were in some cases. | 7/8 |
| Havlioğlu and Demir (2020) Turkey [30] | To determine anxiety levels of emergency service employees working during the COVID-19 pandemic | Descriptive, cross-sectional study | 95 emergency service employees | It was observed that women in comparison to men and doctors and nurses in comparison to other emergency employees experienced more anxiety (p < 0.05). | One limitation is that there was no sample size calculation made for the study. Also, the study was conducted in a single institution with small sample size which could impact the generalisability of the results. Some degree of response bias may have been present. | 6/8 |
| Ilczak et al. (2021) Poland [35] | To assess predictors of stress that paramedics, nurses and doctors experience in the face of the COVID-19 pandemic | Online survey | 955 personnel (doctors, nurses, and paramedics) | The predictors of stress in the professional environment included fear of contracting COVID-19, decrease in the level of safety while conducting emergency medical procedures, and marginalisation of treatment for patients not suffering from COVID-19. Additional socio-demographic factors that increased stress among emergency medical personnel were being female and working in the nursing profession. | Use of an online survey may have impacted on response rate and generalisability of findings. There could be other factors predictive of stress aside from what were explored in the study such as the speed and availability of COVID-19 testing and other socio-demographic variables. | 6/8 |
| Jose et al. (2020) India [37] | To assess the burnout and resilience among frontline nurses in the emergency department of a tertiary care center in North India during COVID-19 pandemic | Cross-sectional descriptive design | 120 nurses | The two metrics of burnout, emotional exhaustion and personal inefficacy had a significantly negative correlation with resilience among the frontline nurses in the emergency (r = 0.25, p < 0.05 and r = 0.31, p < 0.01, respectively). A significant negative correlation has been identified between burnout and resilience that informs the role of resilience in alleviating burnout during this pandemic. | The study included nurses working only in the emergency department, while nurses working in other non-COVID areas also may face burnout in varying degrees. Other healthcare providers working in an emergency who are also potential for burnout were not included in our study. Hence, the generalisability of the present study may be limited to only nurses working in the emergency departments. | 7/8 |
| Kelker et al. (2020) USA [20] | To assess the well-being, resilience, burnout, and wellness factors and needs of EM physicians and advanced practice providers (APPs) during the initial phase of the COVID-19 pandemic | Longitudinal, descriptive, prospective cohort survey study | 213 EM physicians and APPs | Concern for personal safety decreased from 85% to 61% (p < 0.001). | The study used an online survey which may subject to susceptible to response biases (i.e., self-selection bias, nonresponse bias, fatigue bias). The response rates ranged from 31% to 53% over four weeks and may impact generalisability of results. Other limitations include: (1) the authors could not assess individual-level change over time due to anonymous data collection; (2) there was lack of race/ethnicity demographic data; and (3) the WBI was used on a weekly basis though the instrument asks questions regarding symptoms “over the last month,” which may lack sensitivity to such degree of change. | 12/12 |
| Impact on basic self-care declined from 66% to 32% (p = 0.009). | ||||||
| Reported strain on relationships and feelings of isolation affected > 50% of respondents initially without significant change (p = 0.05 and p = 0.30 respectively). | ||||||
| Women were nearly twice as likely to report feelings of isolation as men (OR=1.95; 95% CI=1.82–5.88). | ||||||
| Working part-time carried twice the risk of burnout (OR=2.45; 95% CI=1.10–5.47). Baseline resilience was normal to high. Provider well-being improved over the four-weeks (30–14%; p = 0.01), but burnout did not significantly change (30–22%; p = 0.39). | ||||||
| Li et al. (2020) China [25] | To examine the incidence of mental health symptoms and predictors of Post-Traumatic Stress Disorders (PTSD) symptoms among reserve medics working in Wuhan, the capital city of Hubei Province | Empirical, cross-sectional study | 225 reserve medics dispatched to Wuhan | PTSD symptoms and its subscales were significantly associated with age, collegial relationship and mental health status during medics’ service in Wuhan. | Firstly, recall bias may have influenced participants' reported mental health condition while in Wuhan. It is also unclear how long PTSD symptoms may persist or develop in the future. Secondly, study participants were not randomly selected, and findings were not generalisable to the larger population of reserve medics during the pandemic. Thirdly, although the authors surveyed the types of facilities where the healthcare workers were stationed, they did not measure level of exposure, a factor for developing PTSD symptoms. | 8/8 |
| Mental health counselling was significantly associated with PTSD symptoms (OR = 6.30, 95% CI = 2.95–13.46, p 0.01) and having anxiety symptoms (OR = 4.32, 95% CI1.66–11.23, p 0.01) and stress symptoms (OR = 5.95, 95% CI = 1.95–18.15, p 0.01) were associated with PTSD symptoms. | ||||||
| Mental health counselling was a significant factor of avoidance (OR = 4.88, 95% CI = 1.88–12.71, p 0.01) and having anxiety symptoms (OR = 12.67, 95% CI = 4.72–33.98, p 0.01) was significantly associated with avoidance. | ||||||
| Mental health counselling was a significantly factor of intrusion (OR = 5.4, 95% CI = 2.44–11.93, p 0.01) and those with anxiety symptoms (OR = 4.09, 95% CI = 1.69–9.89, p 0.001) were significantly associated with reporting intrusion. | ||||||
| Both depression (OR = 3.4, 95% CI = 1.43–8.1, p = 0.01) and stress symptoms (OR = 3.48, 95% CI = 1.45–8.35, p = 0.01) were significantly associated with hyperarousal. | ||||||
| Munawar and Choudhry (2021) Pakistan [38] | To examine the psychological impact of COVID-19 on emergency HCWs and understand how they dealt with COVID-19 pandemic, their stress coping strategies or protective factors, and challenges while dealing with COVID-19 patients | Qualitative study | 15 frontline emergency HCWs | Findings highlighted a major theme of stress coping, including, limiting media exposure, limited sharing of COVID-19 duty details, religious coping, just another emergency approach, and altruism. A second major theme of challenges included, psychological response and noncompliance of public/denial by religious scholar. | The study was carried out when the pandemic was ongoing and the researchers describe being conscious of not distracting participants from their essential work. Hence, interviews were often paused or interrupted because participants had to attend other emergency calls and duties. Furthermore, the researchers report being conscious of social/physical distancing guidelines, hence, focus group discussions could not be conducted. This study did not report findings of HCWs from private facilities who may have had different experiences of the pandemic and different coping mechanisms. | 10/10 |
| Nie et al. (2020) China [26] | To explore the prevalence and associated factors of psychological distress among nurses working in the frontline during COVID-19 outbreak | Cross-sectional study | 196 ED nurses | Multiple logistic analyses showed that perceptions of having more social support (OR = 0.960, 95% CI = 0.936–0.984) and effective precautionary measures (OR = 0.469, 95% CI = 0.235–0.933) were negatively related to psychological distress. However, working in ED (OR = 3.378, 95% CI = 1.404–8.130), being treated differently (OR = 2.045, 95% CI = 1.072–3.891), concern for family (OR = 2.171, 95% CI = 1.294–3.643), COVID-19-related impact of event (OR = 1.084, 95% CI = 1.052–1.117), and negative coping style (OR = 1.587, 95% CI = 0.712–3.538) were positively correlated to psychological distress. | There were relatively small sample size and low response rates (30–40%). Secondly, the study was based on a self-administered questionnaire so potential for response bias. | 8/8 |
| Data were collected in the early stage of the outbreak so may underestimate prevalence of psychological distress as the impact of the outbreak might be long term, changeable and continuous, on psychological status among nurses at the frontline. Finally, the cross-sectional design limits interpretation of causal relationships between psychological distress and risk factors. | ||||||
| Rodriguez et al. (2020) USA [22] | To assess anxiety and burnout levels, home life changes, and measures to relieve stress of U.S. academic emergency medicine (EM) physicians during the COVID-19 pandemic acceleration phase | Cross-sectional e-mail survey | 426 EM physicians | On a scale of 1–7 (1 = not at all, 4 = somewhat, and 7 = extremely), the median (interquartile range) reported effect of the pandemic on both work and home stress levels was 5 (4–6). Reported levels of emotional exhaustion/burnout increased from a pre-pandemic median (IQR) of 3 (2–4) since the pandemic started a to median of 4 (3–6), with a difference in medians of 1.8 (95% confidence interval = 1.7–1.9). Most physicians (90.8%) reported changing their behaviour toward family and friends, especially by decreasing signs of affection (76.8%). | The primary limitation is the moderate response rate of 57%, which was attributed to using a general e-mail and clinical work overload during the busy early stage of the pandemic and inability to provide gift cards or other incentives. | 7/8 |
| In terms of spectrum effects, the survey was limited to providers at academic institutions and therefore may not reflect experiences of non-academic EM physicians. | ||||||
| Most of the participant sites were in cities in California that had not seen large patient surges as had been seen in other areas of the country at the time of the study. | ||||||
| Song et al. (2020) China [27] | To assess the mental health of emergency department medical staff during the epidemic in China | Cross-sectional design | 14,825 doctors and nurses | Men were more likely to have depressive symptoms and PTSD than women (OR = 1.12, 95% CI = 1.01–1.24). Those who were middle aged, worked for fewer years, had longer daily work time, and had lower levels of social support were at a higher risk of developing depressive symptoms and PTSD. Working in the Hubei province (OR = 1.70, 95% CI = 1.26–2.29) was associated with a higher risk of depressive symptoms, while those working in the Hubei province but residing in another province had a lower risk of depressive symptoms and PTSD. Being a nurse was associated with a higher risk of PTSD. | This study had a cross-sectional design and as the epidemic changed, the mental health of the medical staff may also change. Further research is needed to track the dynamic changes of medical staff’s mental health status. In addition, all participants in the current study are from the emergency department. Due to the diverse working environments and experience of medical staff in other departments, the generalisability of these results to other populations remains to be verified. | 8/8 |
| Vagni et al. (2020) Italy [33] | To identify the direct and mediating effects of hardiness and coping strategies activated by emergency workers on stress and secondary trauma during the COVID-19 pandemic | Online survey questionnaire | 513 Red Cross volunteers | Hardiness and coping strategies, in particular, which stop unpleasant emotions and thoughts and problem-focused, emerged as mediators in reducing the predicted effect of stress on secondary trauma. The mediating effects of hardiness and coping strategies were found to reduce the effect of stress on arousal by 15% and the effect on avoidance by 25%. | This study has several limitations. The first concern is the sampling method, and the second is that the study involved participants from only one region of Northern Italy, Veneto. This region was among the most affected by COVID-19, and this could be a geographical limit, because in other regions of Italy, the pandemic situation was not as serious. The third limitation was the involvement of only a single emergency organisation, the Red Cross. | 7/8 |
| Vagni et al. (2020) Italy [32] | To analyse the relationship of emergency stress and hardiness with burnout among emergency workers | Online survey questionnaire | 494 emergency volunteers | Hardiness showed an effect in reducing emergency stress levels except for inefficacy-decisional stress, emotional exhaustion (β = − 0.277, p < 0.001), and depersonalisation (β = − 0.215, p < 0.001), and simultaneously increased personal accomplishment (β = 0.332, p < 0.001). | One limitation is that the research was conducted through an online survey. Another limitation is that this was the cross-sectional design used in the study, whereas a longitudinal study would allow for a better analysis of phenomena such as the development of symptoms of burnout. The other limitation is the use of a self-reported questionnaire and participants’ lack of knowledge about the presence of previous psychological problems. Finally, the study lacks comparison with other emergency workers involved throughout the national territory and belonging to other organisations, limiting the generalisation of the results. | 7/8 |
| Zakaria et al. (2021) Malaysia [36] | To identify the prevalence of burnout among emergency healthcare worker in this hospital and to identify the factors contributed to the burnout | Cross-sectional study | 216 HCWs | There was weak correlation (r = 0.148) with the years of experience working in emergency department and the level of burnout (p = 0.03). Among the burnout features were fatigue with 52.2% and frequent physical illness and feel unappreciated with 48.6% and 45.9%, respectively. The job-related issues which predisposed to burnout were demand coping with an angry public (70.2%), job overload (63.9%), lack clear guideline or rapid programme changes (54%), and pay too little (53.1%). | There is potential that non-responders might have been suffering from burnout, thus not being willing to participate. Hence, findings might not be an accurate representation. | 7/8 |
HADS = Hospital Anxiety and Depression Scale; PSQI = Pittsburgh Sleep Quality Index.
Table 2.
Specific characteristics.
| Author, year | Reported conditions | Measurement tool | Reported manifestations | Reported impact |
|---|---|---|---|---|
| Altinbilek et al. (2021) [31] |
Anxiety |
Beck Anxiety Inventory |
Concerned about being unable to find enough adequate PPE in the future |
Higher anxiety and stress scores among physicians and nurses compared to other ED personnel, including security, staff working in patient transport, cleaning staff and patient data entry staff |
| Stress | Perceived Stress Scale | Anxious about getting support from management and salary payments | ||
| An et al. (2020) [23] |
Depression | Patient Health Questionnaire | Of the 481 ED nurses with reported depression, 305 (27.7%) reported mild, 95 (8.6%) reported moderate, 58 (5.3%) experienced moderate-to-severe, and 23 (2.1%) reported severe depression. | Nurses with depression had lower quality of life compared to their colleagues who were not depressed. |
| Quality of life | World Health Organization | |||
| Quality of Life Questionnaire-Brief Version | ||||
| Araç and Dönmezdil (2020) [28] | Anxiety and depression | Hospital Anxiety Depression Scale (HADS) | Presence of severe anxiety and depression, and perceived stress levels and PSQI subscale scores were significantly higher among ED staff than those working in other departments. | Anxiety and depression scores were higher in the first encounters with COVID-19 patients than succeeding encounters. Anxiety was due to fear of infecting family members that could be prevented through precautions such as isolation. However, it should be remembered that loneliness and feelings of missing family members, consequent to isolation could increase the risk of depression. |
| Sleep quality | Pittsburgh Sleep Quality Index (PSQI) | |||
| Baumann et al. (2021) [21] | COVID-19 patient exposure, availability of COVID-19 testing, levels of home and workplace anxiety/stress, changes in behaviours, and performance on a primary care posttraumatic stress disorder screen (PC-PTSD-5) | Researcher–developed instrument with 5 items validated from the PC-PTSD-5 scale | Median (IQR) work and home stress levels decreased over time from the initial survey 5 (4–6) versus 4 (4–5) at follow-up. Most concerns that were reassessed were less highly rated at this follow-up study. | While exposure to suspected COVID-19 patients was nearly universal, stress levels in emergency physicians decreased with time. |
| Caliskan and Dost (2020) [29] | Depression and anxiety | Hospital Anxiety Depression Scale (HADS) | Depression was detected in 180 participants (62%) while anxiety was detected in 103 participants (35.5%), with the median depression and anxiety scores found to be 8 (0–21) and 7 (0–21), respectively | Psychological trauma manifested by reported depression and anxiety of emergency physicians was caused by providing care during the COVID-19 pandemic |
| Cui et al. (2020) [24] | AnxietyStress | Self-Rating Anxiety Scale (SAS) | Among the participants, 281 (62.03%) reported no anxiety symptoms, 154 (34.00%) reported mild, 16 (3.53%) reported moderate, and two (0.44%) reported severe anxiety. There were 146 (32.23%) participants with scores greater than 25 in the PSS, suggesting excessive stress; 229 (50.55%) participants were more likely to respond positively to stress, while 224 (49.45%) were more likely to respond negatively.Participants who had the following characteristics had more mental health problems: female gender, fear of infection among family members, regretting being a nurse, less rest time, more night shifts, having children, lack of confidence in fighting transmission, not having emergency protection training, and negative professional attitude. | Participants reported presence of anxiety, stress, and stress coping tendency primarily due to fear of infecting their family members. |
| Coping tendency | Perceived Stress Scale (PSS) | |||
| Simplified Coping Style Questionnaire (SCSQ) | ||||
| de Wit et al. (2020) [39] | Burnout | Emotional exhaustion and depersonalisation items, from the Maslach Burnout Inventory | The study did not find a time trend in burnout levels (P = 0.632 for emotional exhaustion and P = 0.155 for depersonalisation). | The impact of COVID-19 on the work environment and personal perceptions and fears about the impact on lifestyle affected physician well-being. Personal safety, academic and educational work, personal protective equipment, the workforce, patient volumes, work patterns, and work environment had an impact on physician well-being. A new financial reality and contrasting negative and positive experiences affected participants’ psychological health. |
| Emergency physician burnout levels remained stable during the initial 10 weeks of this pandemic | ||||
| Elhadi et al. (2021) [34] | Depression and anxiety | Hospital Anxiety and Depression Scale (HADS) | With respect to the prevalence of anxiety and depression, the data based on the HADS indicated that ∼ 65.6% of subjects (n = 101) were experiencing anxiety (those who received a score ≥ 11), and about 73.4% of subjects (n = 113) were experiencing depressive symptoms (those who received a score ≥ 11). Findings demonstrated that 67.5% (n = 104) of subjects suffered from emotional exhaustion, while 48.1% (n = 74) experienced depersonalisation (both derived from scores of ≥ 10 out of 18 on the aMBI). However, for low personal accomplishment (PA), only 21.4% (n = 33) scored < 10 (indicating burnout for this category). About 46.1% (n = 71) of respondents had encountered at least one episode of verbal abuse, while 12.3% (n = 19) had experienced physical abuse. | The study demonstrated higher than expected levels of anxiety, depression, and burnout among 154 emergency doctors from Libya who worked during the COVID-19 pandemic. |
| Burnout | Abbreviated Maslach Burnout Inventory (aMBI) scale | |||
| Fitzpatrick et al. (2020) [19] | Wellness | Wellness survey with 10 primary questions and 2 supplemental questions | Physicians felt less in control, felt decreased happiness while at work, had more trouble falling asleep, had an increased sense of dread when thinking of work needing to be done, felt more stress on days not at work, and were more concerned about their own health. | This study showed a statistically significant decrease in EP wellness during the COVID-19 pandemic when compared to the pre-pandemic period. |
| Havlioğlu and Demir (2020) [30] | Anxiety | Beck Anxiety Inventory | Among the participants, 53.7% had mild, 28.4% had moderate and 17.9% had severe anxiety levels. | Anxiety levels of emergency healthcare employees who are were at in the front lines, were increasing. Among the participants, 82.1% stated that they encountered COVID-19-positive patients, 44.2% said they experienced suspected COVID-19%, and 96.8% stated they were afraid of carrying the COVID-19 virus home. |
| Ilczak et al. (2021) [35] | Stress | Researcher-developed questionnaire with 18 questions | One aspect of professional life that, according to research, was felt particularly severely was occupational stress, as illustrated by Polish emergency medical personnel. | During the COVID-19 pandemic, stress among emergency medical personnel had increased considerably due to new factors that did not previously exist. |
| Jose et al. (2020) [37] | Burnout | Maslach Burnout Inventory | The nurses in the emergency during pandemic experienced moderate-to-severe levels of burnout in emotional exhaustion (29.13 ± 10.30) and depersonalisation (12.90 ± 4.67) but mild-to-moderate level of burnout in reduced personal accomplishment (37.68 ± 5.17) and showed moderate to high levels of resilience (77.77 ± 12.41). | The fear of infection to self and family resulted in the frontline staff being more susceptible to anxiety and stress during the pandemic. Increased patient physical workloads led to severe burnout in the form of emotional exhaustion, depersonalisation, and reduced personal accomplishment. In general, the outbreak of an emerging disease contributed to a general atmosphere of fear that needed to be psychologically studied through comprehensive research activity to understand its possible negative impacts on individuals’ mental health and productivity, to mitigate such impacts on the HCWs, in particular, who are in the frontline of counteracting the disease. |
| Resilience | Connor-Davidson Resilience Scale | |||
| Kelker et al. (2020) [20] | Wellness | Well Being Index | Frontline EM physicians and APPs advanced practice providers during the initial surge of the COVID-19 pandemic in Indiana found significant levels of stress, anxiety, fear, concerns about safety, and relationship strain, all of which improved but endured. Additionally, while providers were a resilient group, feelings of isolation and burnout persisted, but did not significantly worsen. | Despite being considered a resilient group, the majority experienced stress, anxiety, fear, and concerns about personal safety due to COVID19, with many at risk for burnout. |
| Burnout | Physician Work Life Study item | |||
| Resilience | Brief Resilience Scale | |||
| Li et al. (2020) [25] | PTSD symptoms | Impact of Event Scale Revised (IES-R) | During their stay in Wuhan, the medics experienced high levels of depression (46.7%), anxiety (35.6%) and stress symptoms (16.0%). Upon returning home, the overall prevalence of clinically concerned PTSD symptoms was as high as 31.6%. | The reserve medics reported a high prevalence of depression, anxiety and stress as well as clinically concerned PTSD symptoms. |
| Anxiety and stress (Mental health status) | Depression Anxiety Stress Scales-21 (DASS-21) | |||
| Munawar and Choudhry (2021) [38] | Psychological impact of COVID-19 on emergency HCWs | Semi-structured interviews | It was found that during the pandemic, media was mentioned to be a major source of exacerbating anxiety and stress levels of masses as authenticity of updates or news shared could not be ascertained. | The findings of thematic analysis revealed that participants practised and recommended various coping strategies to deal with stress and anxiety emerging from the COVID-19 pandemic. |
| Nie et al. (2020) [26] | Psychological distress | General Health Questionnaire (GHQ-12) | A majority of nurses experienced psychological distress because of the COVID-19 outbreak. Most reported variable degrees of concern about their families or themselves being infected with COVID-19. | Nurses who were working in the ED were concerned for their families being infected with COVID-19, being treated differently, having been affected by COVID-19 and having negative coping style made them at high risk of being psychologically distressed. |
| Coping style | Simplified Coping Style Questionnaire (SCSQ) | |||
| Intrusive thoughts related to COVID-19 and consequent avoidance behaviour | Revised version of the Impact of Event Scale (IES-R) | |||
| Social support | Perceived Social Support Scale (PSSS) | |||
| Rodriguez et al. (2020) [22] | Stress, perceptions and key elements in the following domains: numbers of suspected COVID-19 patients, availability of diagnostic testing, levels of home and workplace anxiety, severity of work burnout, identification of stressors, changes in home behaviours, and measures to decrease provider anxiety. | Researcher-developed tool | On the 1–7 scale, the median reported effect of the COVID-19 pandemic on work stress levels was 5 (IQR = 4–6) and on home stress levels was 5 (IQR = 4–6). | COVID-19 exposure during work had a major impact on home lives of physicians.The most commonly reported changes by friends and family were expressions of concern about the EM physician participants’ health, expressions of concern about their exposure to COVID-19 because of contact with the EM physician, and a reluctance of family members to be in close contact with the EM physician. |
| Reported levels of emotional exhaustion/burnout increased from a pre-pandemic median of 3 to since the pandemic started a median of 4 after the pandemic had started, with a difference in medians of 1.8. | ||||
| Most physicians (90.8%) reported changing their behaviour toward family and friends, especially by decreasing signs of affection (76.8%). | ||||
| Worries included: adequacy of personal protective equipment (PPE), ability to accurately diagnose COVID-19 cases quickly, well-being of co-workers who had been diagnosed with COVID-19, and that patients with unclear diagnoses were exposing others in the community | ||||
| Song et al. (2020) [27] | PTSD | PTSD Checklist for DSM-5 (PCL-5) | The prevalence rates of depressive symptoms and post-traumatic stress disorder (PTSD) were 25.2% and 9.1%, respectively. | A considerable number of medical staff in the emergency department suffered from depressive symptoms and PTSD. |
| Depressive symptoms | Centre for Epidemiologic Studies Depression Scale (CES-D) | |||
| Social support | Perceived Social Support Scale (PSSS) | |||
| Vagni et al. (2020) [33] | Psychological stress | Emergency Stress Questionnaire | Volunteers who had worked even a few hours a week to carry out emergency interventions seemed to have developed similar reactions of stress and secondary trauma, probably because they were exposed to a sense of helplessness and gravity, given the high number of patients and deaths from this pandemic in Italy. | High stress reactions, associated with manifestations of arousal, avoidance, and intrusion of secondary trauma, therefore, appear to be linked to the characteristics of the pandemic and not to possible factors of inexperience. |
| Secondary trauma | Secondary Traumatic Stress Scale—Italian Version | |||
| Hardiness | Dispositional Resilience Scale-15—Italian Version | |||
| Coping style | Coping Self-Efficacy Scale—Short Form | |||
| Vagni et al. (2020) [32] | Psychological stress | Emergency Stress Questionnaire | The results of this study highlighted how emergency workers who worked with COVID-19 patients experienced high stress levels and burnout. | Lack of suitable and needed instructions to be able to intervene in a timely manner had a significant impact on stress levels. Correspondingly, stress levels had high positive associations with depersonalisation and emotional exhaustion components of burnout. Nonetheless, the study revealed that hardiness played a protective role in relation to experiencing high stress levels and the risk of developing burnout. |
| Burnout | Maslach Burnout Inventory–Human Services Survey, Italian version | |||
| Hardiness | Dispositional Resilience Scale-15—Italian Version | |||
| Stress factors | Original questionnaire or checklist on stressful factors | |||
| Zakaria et al. (2021) [36] | Burnout | Burnout Questionnaire with 28 questions on behaviour, attitude, and job-related questions that evaluated burnout levels | 51.3% of respondents had burnout, consisting of 61.2% of nurses, 35.1% of doctors, and 29.6% of assistant medical officers. | Factors leading to burnout were frequent exposure to angry members of the public, job overload, lack of clear guidelines, and perceptions of being underpaid. |
| Emergency HCWs had a high rate of burnout, especially nurses and senior staff in comparison to juniors. They reported commonly exhibited fatigue, feeling tired, and suffered from frequent illness as part of their burnout symptoms. |
Data appraisal
In this review, a total of 21 studies were ultimately included after adhering to the JBI guidelines in assessing the quality of each full-text study [18]. All included studies were independently critically appraised by two researchers. However, no studies were removed from the review based on quality appraisal.
Data synthesis
The findings of this review were synthesised narratively with consideration of the odds ratio (OR), relative risk (RR), β–values, or p–values, except for the qualitative study and clinical review.
Results
Characteristics of included studies
We included a total of 21 studies in this review (see Table 1). Of the 21 included studies, four were conducted in the US, including two prospective cohort studies which involved 55 physicians [19] and 213 physicians and advanced practice providers [20], and two cross-sectional studies which involved 262 [21] and 426 [22] physicians, respectively. An additional five cross-sectional studies were conducted in China and were participated by different HCWs including 1103 nurses [23], 453 nurses [25], 225 reserve medics from a Shanghai-based large hospital who were dispatched to Wuhan [25], 196 nurses [26] and 14,825 physicians and nurses [27]. Four studies were conducted in Turkey consisting of three cross-sectional which involved 198 HCWs (physicians, nurses and others) [28], 290 physicians [29], and 95 HCWs (physicians, nurses and others) [30]; and one prospective-multi-centred survey-based study participated by 205 HCWs (physicians, nurses and others) [31]. Two cross-sectional studies using online survey questionnaires were implemented in Italy which involved 494 emergency volunteers [32] and 513 Red Cross volunteers [33]. The remaining four cross-sectional studies were conducted in different countries namely, Libya involving 154 physicians [34], Poland with 955 HCWs (physicians, nurses and paramedics) [35], Malaysia which included 216 HCWs (physicians, nurses and assistant medical officers) [36], and India which involved 120 nurses [37]. In Pakistan, a qualitative study involving 15 HCWs (medical technicians and ambulance drivers) was conducted by Munawar and Choudhry [38], while a mixed methods study with 468 physicians was conducted in Canada [39].
Study findings were categorised according to the reported psychological conditions and manifestations, with the outcome being psychological impact (see Table 2). These categories guided the structure of the succeeding sections this scoping review.
Anxiety
Of the 21 included studies, nine revealed that anxiety affected the psychological status of emergency HCWs. In Turkey, two studies [30], [31] indicated that among the HCWs in the ED, physicians and nurses had higher anxiety scores compared to other ED personnel. Additionally, HCWs were concerned about being unable to find enough adequate PPE and anxious about getting support from management and salary payments [31]. In another Turkish study, as well as in a Libyan study, HCWs were reported to have experienced severe anxiety due to fear of infecting family members [28], [34]. Likewise in China, Cui et al. [24] reported that fear of infecting family members was the most influential and predictive factor of anxiety (β = 0.263, p = 0.000). It was also reported that the risk of developing anxiety among females was higher than among male HCWs [28], [30].
In another study in China, Li et al. [25] revealed that having anxiety symptoms was reported to have significant impact on the psychological status of HCWs, particularly on having PTSD symptoms (OR = 4.32, 95% CI = 1.66–11.23, p < 0.01), experiencing avoidance (OR = 12.67, 95% CI = 4.72–33.98, p < 0.01), and reporting intrusive thoughts (OR = 4.09, 95% CI = 1.69–9.89, p < 0.001). In the US, Kelker et al. [20] reported that mid-career HCWs had four times greater odds to report anxiety or fear than their early-career counterparts (OR = 4.38; 95% CI = 1.27–15.05). Kelker et al. [20] added that HCWs who were at greatest risk of experiencing anxiety or fear due to COVID-19 were those who screened “at-risk” on their well-being index (OR = 14.97; 95% CI = 3.58–62.53). On the other hand, the qualitative study of Munawar and Choudhry [38] found that during the pandemic, media was mentioned to be a major source of exacerbating anxiety levels as authenticity of updates or news shared could not be ascertained.
Burnout
Six studies reported that burnout affected the psychological status of HCWs. In the US, the reported levels of emotional exhaustion/burnout increased from a pre-pandemic median of 3 to a median of 4 (using an adapted emotional exhaustion and burnout tool rated on a 1–7 scale) after the pandemic had started, with a difference in medians of 1.8 [22]. In another US study, HCWs who were working part-time (OR;= 2.45; 95% CI = 1.10–5.47) carried twice the risk of burnout [20]. In Canada, a mixed methods study reported that being tested for COVID-19 (OR = 11.5, 95% CI = 3.1– 42.5), and the number of shifts worked (OR = 1.3, 95% CI = 1.1–1.5 per additional shift), were associated with high emotional exhaustion/burnout [39]. In Libya, a study demonstrated higher than expected levels of burnout among emergency doctors who reported low personal accomplishment when working during the COVID-19 pandemic [34]. Similarly, Jose et al. [37] reported that Indian nurses in the emergency during pandemic experienced moderate-to-severe levels of burnout in emotional exhaustion (29.13 ± 10.30) and depersonalisation (12.90 ± 4.67) but mild-to-moderate levels of burnout in reduced personal accomplishment (37.68 ± 5.17) and showed moderate to high levels of resilience (77.77 ± 12.41). In Malaysia, emergency HCWs reported a high rate of burnout, especially among nurses and senior staff in comparison to juniors, exhibiting fatigue, feeling tired, and suffering from frequent illness as part of their burnout symptoms [36]. Moreover, in Italy, Vagni et al. [33] indicated that the hardiness of HCWs did not show an effect in reducing emotional exhaustion/burnout (β = − 0.277, p < 0.001).
Depression
As depression was also reported to have affected the psychological status of HCWs, there were four studies that accounted these reports. One conducted in China revealed that the overall prevalence of depression in nurses was 43.61% (95% CI = 40.68–46.54%) and that working in tertiary hospitals (OR = 1.647, p = 0.009), providing direct patient care of COVID-19 patients (OR = 1.421, p = 0.018), and being a current smoker (OR = 3.843, p < 0.001) were significantly associated with depression [23]. In Turkey, a study reported that HCWs working in the ED reported severe depression (OR = 9.194, p = 0.002), and was found to be one of the effective risk factors of HCWs’ mental health [28]. In another Turkish study, according to physicians’ HADS scores, depression was detected in 180 participants (62%) with the median depression scores found to be 8 (0–21) [29]. In Libya, a cross-sectional study examined prevalence of depression among emergency physicians on the COVID-19 pandemic frontline and found that around 73.4% of participants (n = 113) were experiencing depressive symptoms, being those who received a score of ≥ 11 [34].
Inadequate sleep
Two studies reported effects on psychological status of HCWs. A study in the US revealed that during the pandemic, emergency physicians had more trouble falling asleep (p = 0.001) [19]. While the other study in Turkey revealed that the use of sleeping medication subscale score (OR = 6.357, p = 0.012) was also found to be an effective risk factor of the mental health of HCWs [28].
Post-traumatic stress disorder (PTSD) symptoms
According to Li et al. [25], overall prevalence of clinical PTSD symptoms was as high as 31.6% among reserve medics dispatched to Wuhan, China. The study also indicated that mental health counselling was significantly associated with PTSD symptoms (OR = 6.30, 95% CI = 2.95–13.46, p < 0.01) and having anxiety (OR = 4.32, 95% CI = 1.66–11.23, p < 0.01) and stress symptoms (OR = 5.95, 95% CI = 1.95–18.15, p < 0.01) were associated with PTSD symptoms [25]. In another Chinese study, that assessed the mental health of ED medical staff during the epidemic, those who were middle-aged, worked for fewer years, had longer daily work time, and had lower levels of social support were at higher risk of developing PTSD symptoms [27]. With regard to gender profile of the ED staff, males were reported to be more likely to have PTSD symptoms than females (OR = 1.12, 95% CI = 1.01, 1.24).
Psychological distress/stress and secondary trauma
In China, nurses working in the frontline during the COVID-19 outbreak in Guangdong Province were reportedly suffering high level of psychological distress [26]. The study findings of the multiple logistic analyses revealed that the high level of psychological distress of frontline nurses were positively correlated to the concern for their family of being infected with COVID-19 (OR = 2.171, 95% CI = 1.294–3.643), being treated differently (OR = 2.045, 95% CI = 1.072–3.891), COVID-19-related impact of event (OR = 1.084, 95% CI = 1.052–1.117), having negative coping style (OR = 1.587, 95% CI = 0.712–3.538) and being working in the ED (OR = 3.378, 95% CI = 1.404–8.130) [26].
On the other hand, Red Cross volunteers who had worked even a few hours a week carrying out emergency interventions were found to have developed similar reactions of psychological stress and secondary trauma (e.g. stress of helping others who have been traumatised, or suffering such as having anxiety and depressive symptoms), as they were exposed to a sense of helplessness and gravity, given the high number of patients and deaths from the pandemic in Italy [32]. Vagni et al. [32] also reported that all stress subscales, including organisational-related (p < 0.001), physical (p < 0.001), inefficacy decisional (i.e. stress related to self-efficacy and decision-making aspects) (p < 0.05), emotional (p < 0.001), cognitive (p < 0.001), and COVID stress (p < 0.01) were positively correlated with secondary trauma.
Stress
In Turkey, higher stress scores among physicians and nurses were reported compared to other ED personnel, including security, staff working in patient transport, cleaning staff and patient data entry staff. However, stress scores of nurses were significantly higher than physicians (p < 0.05) [31] where perceived stress level (OR = 8.639, p = 0.003) was also found to be an effective risk factor of mental health [28]. In USA, a cross-sectional study among physicians revealed that on a scale of 1–7 (1 = not at all, 4 = somewhat, and 7 = extremely), the median (interquartile range) reported effect of the pandemic on both work and home stress levels was 5 (4–6) [22]. In addition, a longitudinal US study indicated that the median (IQR) work and home stress levels decreased over time from the initial survey 5 (4–6) versus 4 (4–5) at follow-up [21]. In another US study, Fitzpatrick et al. [19] reported that the effect of the pandemic among physicians was they felt more stress on days not at work (p < 0.0001). In China, a study indicated that fear of infecting family members was the most influential and predictive of stress (β = 0.239, p = 0.000) for nurses in the ED and fever clinics [24]. In another Chinese study, Li et al. [25] reported that stress symptoms (OR = 5.95, 95% CI = 1.95–18.15, p < 0.01) were associated with PTSD symptoms. Additionally, one aspect of professional life that is reportedly felt particularly severely is occupational stress, as illustrated by Polish emergency medical personnel [35]. Ilczak et al. [35] added that the predictors of stress in the professional environment included the fear of contracting COVID-19, a decrease in the level of safety while conducting emergency medical procedures, and the marginalisation of treatment for patients not suffering from COVID-19. In the qualitative study [38], it was found that during the pandemic, media was identified as a major source of exacerbating stress levels of masses as authenticity of updates or news shared could not be ascertained. Lastly, an Italian study reported that hardiness showed an effect in reducing emergency stress levels among emergency volunteers [33]. Vagni et al. [33] added that hardiness as well as coping strategies appeared as mediators in decreasing the predicted consequence of stress on secondary trauma in emergency workers by avoiding unpleasant emotions and thoughts related to the pandemic.
Discussion
The COVID-19 pandemic continues to spread across the globe and the two worst regions impacted are Europe and the Americas [40]. Upon finalising this review, it was noted that there was no available literature review on currently hard-hit countries such as Saudi Arabia and India. Currently, the second wave of infection in India has reportedly spread much faster and caused devastating health crisis, with highest daily reported cases surpassing 400,000 by May 14, 2021 [41]. Similarly, Brazil has been heavily impacted by the infection with 15.3 million reported cases from the beginning of January 2021 to middle of May 2021 [42]. Saudi Arabia too, has experienced sustained community transmission of the infection [43]. By contrast, Australia, New Zealand, Thailand, Taiwan, South Korea and Japan have been reported as the most successful countries at preventing large-scale outbreaks and containing the pandemic through closure of borders and nationwide lockdowns [44]. Under these conditions, if countries across the globe continue to enable community spread and cannot control the pandemic, COVID-19 infections and deaths among HCWs will also continue to follow that of the general population [9]. Moreover, HCWs will have to continue putting their greatest effort and services on the frontline and suffer more psychological and mental health burden.
The findings of this review suggest that emergency HCWs experienced a myriad of psychological impacts including significant levels of anxiety, burnout, depression, lack of sleep, PTSD symptoms, psychological stress and secondary trauma, and stress. We also found that most studies examined doctors and only a limited number were focused on others such as paramedics and nurses. In particular, only three studies focused on evaluating the impact of the pandemic on psychological status of ED nurses in China [23], [24], and in India [37]. The findings imply that there is a gap in current evidence, specifically on the psychological impact of the pandemic among ED nurses who are always at the frontline of care. The review findings indicate a need for more research on this topic and the necessity for psychological support among HCWs who continue to work in the ED during the current pandemic. Furthermore, the second wave is spreading faster in Brazil [42], and India [41] where the healthcare systems of such countries are reportedly on the brink of collapse [44].
As adverse mental health and psychological impacts caused by the pandemic are prevalent among emergency HCWs, adequate interventions and measures are necessary to minimise the adverse impacts among countries with sustained community transmission of the COVID-19 infection. Comprehensive screening of the mental health or psychological issues is vital including other factors such as job overload, perception of being underpaid, lack of clear precautionary guidelines, frequent exposure to angry public [25], [36]. Psychological interventions and measures must be targeted and prioritised to HCWs experiencing high levels of anxiety and stress due to fear of contracting the infection and infecting family members, and low levels of perceived safety and security [28], [35]. To improve the psychological status of emergency HCWs related to the pandemic, measures addressing the negative mental health impacts must be implemented, both at organisational and national levels [20], [27], [31]. HCWs need regular psychological support and counselling [28], [30]. Additionally, hardiness and resilience of emergency HCWs as well as their coping strategies including religious coping and passion to serve humanity and country must be upheld in dealing with the COVID-19 pandemic [25], [32], [33], [38].
This review has identified that emergency physicians have decreased wellness (i.e., fears about impact on lifestyle, impact of the pandemic at workplace, personal perceptions), and their psychological burden can be addressed by enhancing availability of PPE at the workplace, rapid turnaround of COVID-19 testing, clear communications about precautionary guideline changes [19], [22], [39]. Reports revealed that awareness and implementation of evidence-based strategies and recommendations in mitigating the risks and preventing psychological distress and burnout are needed [22]. Caliskan and Dost [29] emphasised that recognition of psychological trauma, due to providing care during the pandemic and provision of psychological support, is important to protect the mental health of doctors on the frontline. With the current conditions of the pandemic worldwide, additional investigations may shed light on why and how doctors are more impacted than other emergency HCWs [21] or whether this is only because many studies are reporting on the topic among doctors.
Among emergency nurses, resilience has also been indicated to reduce burnout and workplace stressors during the pandemic [37]. Jose et al. [37] added that the development and administration of effective interventions to improve resilience should ensure healthy workplaces and adoption of positive attitudes and harmonious relationships with other HCWs which could lead to better quality care of patients in the ED. Cui et al. [24] reported that effective measures were necessary to protect the mental health of emergency nurses during the pandemic including ensuring enough rest time, decreasing night shifts, strengthening protective training, and provision of up-to-date information of the pandemic situation. Nie et al. [26] recommended for a need of early detection and supportive strategy to prevent varying degrees of psychological distress among ED nurses. Furthermore, An et al. [23] indicated that the negative impact of depression, including quality of life and quality of patient care, must be considered in addressing and treating depression among emergency nurses. With all these findings, the psychological burden in emergency HCWs including physicians, nurses, and medics suggests the need to study the long-term impacts of the pandemic on psychological status.
Strengths and limitations of the study
It is recognised that this scoping review has strengths and limitations that need to be considered. The review utilised a systematic and robust search strategy based on our study objective, and the findings present a summary of current reported effects of the COVID-19 pandemic on psychological status of emergency HCWs to a particular time point. As the pandemic continues, newer research may have been conducted since our search. Furthermore, our review included only studies published in English or Arabic language and may have missed reports published in other languages. Additionally, we also excluded studies involving critical care and ward HCWs who could also be at risk from psychological impact of COVID-19 given their roles in providing care to infected patients and their families. Finally, most included studies only examined physicians, and there is an obvious deficiency of effects on other disciplines, such as emergency department nurses and paramedics. Overall, the findings of this review could inform strategies for psychological support for emergency HCWs during the current and future pandemics.
Conclusions
This review explored the psychological status of emergency HCWs arising from the COVID-19 pandemic. We found that providing care in the ED, or working as an emergency HCW on the frontline, could predispose the individual to various psychological impacts including anxiety, burnout, depression, inadequate sleep, post-traumatic stress disorder (PTSD) symptoms, psychological distress/stress and secondary trauma, and stress. To combat these psychological impacts, several interventions are recommended including early and comprehensive screening, psychological support and counselling, utilisation of hardiness and resilience as well as the individual’s own coping strategies, enhancing availability of PPE at the workplace, rapid turnaround of COVID-19 testing, clear communications about precautionary guideline changes, ensuring enough rest time, decreasing night shifts, strengthening protective training, and up-to-date information on the pandemic situation.
Emergency HCWs are clearly impacted from psychological burden due to the COVID-19 pandemic, while the crisis is still ongoing. Psychological harm is a significant concern, both for the individual and the organisation, and should be addressed through implementation and evaluation of interventions and measures to protect the mental health of emergency HCWs. Future research is needed to explore measures for effectively alleviating the psychological burden of HCWs during the COVID-19 and other future pandemics.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest relevant to this article.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.auec.2021.10.002.
Appendix A. Supplementary material
Supplementary material
References
- 1.Word Health Organization. Coronavirus disease (COVID-19) outbreak; 2020. 〈https://www.who.int/westernpacific/emergencies/covid-19〉.
- 2.Johns Hopkins University and Medicine. Coronavirus COVID-19 Global Cases; 2021. 〈https://coronavirus.jhu.edu/map.html〉.
- 3.World Health Organization. Coronavirus disease (COVID-19): how is it transmitted?; 2020. 〈https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-how-is-it-transmitted〉.
- 4.Al Omari O., Al Sabei S., Al Rawajfah O., Abu Sharour L., Aljohani K., Alomari K., et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an online cross-sectional multicountry study. Depress Res Treat. 2020;2020:8887727. doi: 10.1155/2020/8887727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Erdem H., Lucey D.R. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239–241. doi: 10.1016/j.ijid.2020.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang H. The influence of the ongoing COVID-19 pandemic on family violence in China. J Fam Violence. 2020:1–11. doi: 10.1007/s10896-020-00196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koh D. Occupational risks for COVID-19 infection. Occup Med. 2020;70(1):3–5. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang J., Zhou M., Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105(1):100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bandyopadhyay S., Baticulon R.E., Kadhum M., Alser M., Ojuka D.K., Badereddin Y., et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health. 2020;5(12) doi: 10.1136/bmjgh-2020-003097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavallo J.J., Donoho D.A., Forman H.P. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—planning for the nth patient. JAMA Health Forum. 2020;1(3) doi: 10.1001/jamahealthforum.2020.0345. [DOI] [PubMed] [Google Scholar]
- 11.Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Legido-Quigley H., Mateos-García J.T., Campos V.R., Gea-Sánchez M., Muntaner C., McKee M. The resilience of the Spanish health system against the COVID19 pandemic. Lancet Public Health. 2020;2667(20):19–20. doi: 10.1016/S2468-2667(20)30060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan B., Chew N., Lee G., Jing M., Goh Y., Teoh H., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arksey H., O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. 2005;8:19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 15.Cooper S., Cant R., Kelly M., Levett-Jones T., McKenna L., Seaton P., et al. An evidence-based checklist for improving scoping review quality. Clin Nurs Res. 2021;30(3):230–240. doi: 10.1177/1054773819846024. [DOI] [PubMed] [Google Scholar]
- 16.Tricco A.C., Lillie E., Zarin W., O’Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 17.Covidence Systematic Review Software . Veritas Health Innovation; Melbourne, AU: 2021. 〈www.covidence.org〉 (Better systematic review management). [Google Scholar]
- 18.Joanna Briggs Institute . Critical appraisal tools. 2021. 〈https://joannabriggs.org/critical-appraisal-tools〉 [Google Scholar]
- 19.Fitzpatrick K., Patterson R., Morley K., Stoltzfus J., Stankewicz H. Physician wellness during a pandemic. West J Emerg Med. 2020;21(6):83–87. doi: 10.5811/westjem.2020.7.48472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelker H., Yoder K., Musey P., Jr., Harris M., Johnson O., Sarmiento E., et al. Prospective study of emergency medicine provider wellness across ten academic and community hospitals during the initial surge of the COVID-19 pandemic. BMC Emerg Med. 2021;21(1):36. doi: 10.1186/s12873-021-00425-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baumann B.M., Cooper R.J., Medak A.J., Lim S., Chinnock B., Frazier R., et al. Emergency physician stressors, concerns, and behavioral changes during COVID-19: a longitudinal study. Acad Emerg Med. 2021;28(3):314–324. doi: 10.1111/acem.14219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodriguez R.M., Medak A.J., Baumann B.M., Lim S., Chinnock B., Frazier R., et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27(8):700–707. doi: 10.1111/acem.14065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.An Y., Yang Y., Wang A., Li Y., Zhang Q., Cheung T., et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. 2020;276:312–315. doi: 10.1016/j.jad.2020.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cui S., Jiang Y., Shi Q., Zhang L., Kong D., Qian M., et al. Impact of COVID-19 on anxiety, stress, and coping styles in nurses in emergency departments and fever clinics: a cross-sectional survey. Risk Manag Health Policy. 2021;14:585–594. doi: 10.2147/RMHP.S289782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li X., Li S., Xiang M., Fang Y., Qian K., Xu J., et al. The prevalence and risk factors of PTSD symptoms among medical assistance workers during the COVID-19 pandemic. J Psychosom Res. 2020;139 doi: 10.1016/j.jpsychores.2020.110270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nie A., Su X., Zhang S., Guan W., Li J. Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J Clin Nurs. 2020;29:4217–4226. doi: 10.1111/jocn.15454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song X., Fu W., Liu X., Luo Z., Wang R., Zhou N., et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60–65. doi: 10.1016/j.bbi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Araç S., Dönmezdil S. Investigation of mental health among hospital workers in the COVID-19 pandemic: a cross-sectional study. Sao Paulo Med J. 2020;138(5):433–440. doi: 10.1590/1516-3180.2020.0272.R3.21072020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Çalişkan F., Dost B. The evaluation of knowledge, attitudes, depression and anxiety levels among emergency physicians during the COVID-19 pandemic. Signa Vitae. 2021;1(16):163–171. doi: 10.22514/sv.2020.16.0022. [DOI] [Google Scholar]
- 30.Havlioglu S., Demir H.A. Determining the anxiety levels of emergency service employees working during the Covid-19 pandemic. J Harran Univ Med Fac. 2020;17(2):251–255. doi: 10.35440/hutfd.752467. [DOI] [Google Scholar]
- 31.Altinbilek E., Ozturk D., Erdem S.C. Covid-19 adversely affects the psychological status of healthcare workers in the emergency room. Ann Clin Anal Med. 2021;12(1):9–14. [Google Scholar]
- 32.Vagni M., Giostra V., Maiorano T., Santaniello G., Pajardi D. Personal accomplishment and hardiness in reducing emergency stress and burnout among COVID-19 emergency workers. Sustainability. 2020;12(21):9071. doi: 10.3390/su12219071. [DOI] [Google Scholar]
- 33.Vagni M., Maiorano T., Giostra V., Pajardi D. Coping with COVID-19: emergency stress, secondary trauma and self-efficacy in healthcare and emergency workers in Italy. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.566912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elhadi M., Msherghi A., Elgzairi M., Alhashimi A., Bouhuwaish A., Biala M., et al. The mental well-being of frontline physicians working in civil wars under coronavirus disease 2019 pandemic conditions. Front Psychiatry. 2021;11 doi: 10.3389/fpsyt.2020.598720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ilczak T., Rak M., Ćwiertnia M., Mikulska M., Waksmańska W., Krakowiak A., et al. Predictors of stress among emergency medical personnel during the COVID-19 pandemic. Int J Occup Med Environ Health. 2021;34(2):139–149. doi: 10.13075/ijomeh.1896.01688. [128640] [DOI] [PubMed] [Google Scholar]
- 36.Zakaria M.I., Remeli R., Shahamir M.F., Yusuf M.H., Ariffin M.A., Azhar A.M. Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong J Emerg Med. 2021:1–6. doi: 10.1177/1024907921989499. [DOI] [Google Scholar]
- 37.Jose S., Dhandapani M., Cyriacn M.C. Burnout and resilience among frontline nurses during COVID-19 pandemic: a cross-sectional study in the emergency department of a tertiary care center, North India. Indian J Crit Care Med. 2020;24(11):1081–1088. doi: 10.5005/jp-journals-10071-23667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Munawar K., Choudhry F.R. Exploring stress coping strategies of frontline emergency health workers dealing Covid-19 in Pakistan: a qualitative inquiry. Am J Infect Control. 2021;49(3):286–292. doi: 10.1016/j.ajic.2020.06.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Wit K., Mercuri M., Wallner C., Clayton N., Archambault P., Ritchie K., et al. Network of Canadian Emergency Researchers. Canadian emergency physician psychological distress and burnout during the first 10 weeks of COVID-19: a mixed-methods study. JACEP Open. 2020;1(5):1030–1038. doi: 10.1002/emp2.12225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lowy Institute. COVID-19 Performance Index; 2021. 〈https://interactives.lowyinstitute.org/features/covid-performance/〉.
- 41.Ministry of Health and Family Welfare. COVID-19 Statewide Status; 2021. 〈https://www.mohfw.gov.in〉.
- 42.World Health Organization. COVID-19 Dashboard: Brazil Situation; 2021. 〈https://covid19.who.int/region/amro/country/br〉.
- 43.Ministry of Health, Saudi Arabia. COVID-19 Dashboard; 2021. 〈https://covid19.moh.gov.sa〉.
- 44.Hollingsworth J. New Zealand and Australia were COVID success stories. Why are they behind on vaccine rollouts?; 2021. 〈https://edition.cnn.com/2021/04/15/asia/new-zealand-australia-covid-vaccine-intl-dst-hnk/index.html〉.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material