Abstract
The authors review trend and cohort surveys and administrative data comparing prevalence of mental disorders during, versus, and before the COVID-19 pandemic and changes in mental health disparities. Best evidence suggests clinically significant anxiety-depression point prevalence increased by relative-risk (RR) = 1.3 to 1.5 during the pandemic compared with before. This level of increase is much less than the implausibly high RR = 5.0 to 8.0 estimates reported in trend studies early in the pandemic based on less-appropriate comparisons. Changes in prevalence also occurred during the pandemic, but relative prevalence appears not to have changed substantially over this time.
Keywords: Cohort study, COVID-19, Health disparities, Mental disorders, Trend study
Key points
-
•
Although thousands of articles have been published over the past 18 months on the mental health effects of COVID-19, only a few describing US samples were based on research designs that support valid inferences about changes in prevalence or disparities in common mental disorders either during the pandemic or before the pandemic or over the course of the pandemic.
-
•
Reports based on nonprobability general population surveys carried out early in the pandemic estimated that point prevalence of clinically significant anxiety-depression increased by relative risk (RR) = 5.0 to 8.0 during the pandemic compared with before the pandemic. A more focused analysis of available evidence suggests that the true change was probably in the range RR = 1.3 to 1.5, although the increase could have been greater in persistent anxiety-depression or in some segments of the population.
-
•
Disparities in prevalence of anxiety-depression during the pandemic compared with before the pandemic appear to have increased among people younger than 60 years of age, members of racial/ethnic minorities, and people with education levels less than a 4-year college degree.
-
•
Changes in prevalence over the course of the pandemic have occurred (both up and down at different times), but health disparities have not changed substantially overall based on sex, age, education, or race/ethnicity.
Video content accompanies this article at http://www.psych.theclinics.com.
As of August 2021, COVID-19 infection has caused more than 637,000 US deaths,1 and the pandemic has caused many more deaths owing to external causes (most notably drug overdose)2 beyond those projected from previous years. Mitigation measures have resulted in massive changes in day-to-day life and an unemployment rate early in the pandemic that was higher than any other time since the Great Depression.3 Unemployment remains high even now, 18 months after the pandemic began. Even more importantly, the long-term unemployment rate, an indicator of severe financial distress,4 , 5 is currently more than double the prepandemic rate.5 In addition, many more people are living on reduced incomes and are experiencing uncertainties about their financial futures.6 Adding to these stresses, the pandemic occurred during a time of civic polarization that highlighted inequalities exacerbated by the pandemic,7 leading to wide variation in responses to government mitigation efforts and consequent variations in pandemic spread.8
In the context of this enormous complexity, we were asked by the editors to review the literature on evolving changes in prevalence of mental disorders in the US adult general population during compared with those measured before the pandemic. Concerns about such changes have been raised since the beginning of the pandemic9 , 10 based partly on evidence from past infectious disease outbreaks11, 12, 13 and other natural disasters14 documenting adverse mental health effects of these events owing to exposure to component stressors, such as job loss,15 death of a loved one,16 social isolation,17 and multiple accumulated stressors that often occur during major disasters.18
Trends in mental disorder prevalence since before the COVID-19 pandemic
A search of American Psychological Association PsycINFO, OVID Medline, Embase, Scopus, and Web of Science for published English language articles on COVID-19 and mental health in July 2021 found 14,094 articles, including 49 reviews of research on the pandemic’s effects on general population mental health.19 Most of these reviews were not quantitative and concluded merely that the pandemic had the potential to increase psychopathology (eg, Ref.20) and that certain segments of the population are likely to be at especially high risk (eg, Refs.21 , 22). Most of the underlying studies in the reviews were based on nonprobability samples without established prepandemic baselines.
Accurate trend estimates require before and after comparisons based either on true trend studies (ie, sampling and field procedures that are the same before and after) or cohort studies (ie, the same individuals are assessed before and after). Trend studies are more common. Caution is needed in interpreting their results, though, as the pandemic might have changed response rates and field survey procedures. In the case of administrative trend data (eg, emergency department [ED] visits), there may have been new barriers to health care access during the pandemic. Cohort surveys are less subject to these biases but suffer from attrition bias. The remainder of this section reviews trend and cohort studies that attempted to make before and after comparisons of mental health in the COVID-19 pandemic.
Noncomparable Trend Surveys
Twenge and Joiner23 carried out a national survey of n = 19,330 adults in April 2020 from an online consumer panel sample that was designed to be representative of the US population on broad geographic and sociodemographic characteristics.24 The same short self-report screening scale of serious mental illness (SMI)25 used in the US government’s 2018 National Health Interview Survey (NHIS)26 was administered in that online survey. The investigators estimated that SMI prevalence increased 8-fold in the United States since the 2018 NHIS. However, the NHIS was a face-to-face household survey carried out by the Census Bureau with a response rate of 61%, whereas the online survey was based on a nonprobability sample with an unknown response rate. That sample, although balanced to the population on basic geographic-demographic characteristics, might have been quite different from the population on psychological characteristics.27 Other widely cited studies that used similar noncomparable trend designs (ie, comparing the prevalence of mental illness in prepandemic benchmark government surveys to estimates in online nonprobability surveys carried out during the pandemic) came to a similar conclusion: that there were massive increases in the prevalence of common mental disorders (CMD) during the pandemic, with relative risk (RR) ranging from 3.0 to 5.0.23 , 28, 29, 30, 31 These comparisons all had the same fundamental design flaw as the Twenge and Joiner study. Although methods exist to improve estimates of population prevalence in such nonprobability surveys,32 particularly when other surveys with the same instruments and more systematic sampling are available, these methods were not used in any of these noncomparable trend studies.
Several other studies compared prevalence estimates in baseline prepandemic benchmark government surveys with estimates in the Centers for Disease Control and Prevention (CDC) Household Pulse Survey (HPS), a major ongoing US government trend survey initiated in April 2020 to track mental health, health insurance coverage, and problems accessing care during the pandemic.33 The HPS has so far collected self-report survey data from more than 2.7 million respondents. The HPS includes the 4-item Patient Health Questionnaire (PHQ-4) screening scale of current anxiety-depression,34 which was the same scale used in the benchmark NHIS and in subsamples of another important national benchmark government survey, the CDC Behavioral Risk Factor Surveillance Survey (BRFSS).35 The studies that used the HPS as the follow-up survey during the pandemic and made comparisons with prepandemic estimates based on the 2018 or 2019 NHIS or BRFSS drew similar conclusions to those of the studies that used commercial noncomparable trend surveys: that the prevalence of clinically significant PHQ-4 scores increased during the pandemic with RR of 3.0 to 5.0.23 , 28 , 36
However, none of these HPS trend study reports noted that the HPS, unlike the NHIS or BRFSS, is one of the Census Bureau’s “Experimental Data Products,”37 which the Bureau uses to provide rapid response to time-sensitive questions before more definitive results can be generated from benchmark surveys. The HPS achieves this rapid response by using an online self-report questionnaire administered to large samples of people residing in households across the country recruited via e-mail and text invitations either weekly (in the first 12 HPS waves) or biweekly (in subsequent HPS waves). As in online consumer surveys, the HPS uses weights to match sample distributions to Census population distributions on the cross-classification of age, sex, race/ethnicity, education, and geography (the 50 states, the District of Columbia, and the 15 largest metropolitan statistical areas). However, unlike benchmark government surveys like the NHIS, the weekly phase 1 HPS (April 14 to July 23, 2020) had a response rate of only 1.3% to 2.9%. The response rate increased in subsequent HPS phases to 6.3% to 10.3% based on important design changes, including shifting to a 2-week rather than 1-week field period.38 The Census Bureau documentation is clear that these low response rates make it hazardous to compare prevalence estimates in the HPS with those in earlier benchmark government surveys,39 but this caution did not deter researchers from making such comparisons and declaring that COVID-19 had a dramatic effect on US mental health.
Cohort surveys
A living systematic review of high-quality cohort studies is being carried out by a Canadian research group to assess pandemic effects on population mental health.40 Study inclusion requires the same participants to be assessed both before and during the pandemic with either a high follow-up response rate or usage of a statistical adjustment for follow-up survey nonresponse bias. A first report by this research group posted in May 2021 based on 33 cohorts41 concluded, in striking contrast to the results of the noncomparable trend studies described above, that “mental health in the general population has not worsened compared to pre-COVID-19 levels.”
To begin reconciling the striking inconsistency between this conclusion and the conclusion of the noncomparable trend surveys, it is important to note that the cohort studies in the review were international, covered diverse population segments, and varied enormously in size. Focusing only on the large national probability-based samples in the review shows clearly that pandemic impact differed significantly both within and across countries and over time. A national UK cohort study in the review, which was made up of more than 40,000 households studied since 2009,42 found that the prevalence (95% confidence interval [CI]) of current clinically significant CMD43 was significantly higher in April 2020 than the average across the 19 prepandemic waves (29.5% [28.0–31.0] vs 20.8% [19.4–22.2]),44 but that current prevalence decreased to the prepandemic level (20.8% [19.5–22.1]) in a follow-up survey 5 months later.45 In comparison, a large Norwegian cohort study based on a panel of more than 230,000 people studied since 198442 initiated a new wave of data collection shortly before the start of the pandemic to assess 30-day prevalence of CMD using the World Health Organization Composite International Diagnostic Interview.46 That survey was carried out in random replicates to test the new instrument. The prevalence (95% CI) was significantly higher in the first random replicate (15.3% [12.4–18.8]) implemented just before the pandemic started (January 28 to March 11, 2020), than in the replicate carried out during the first 3 months of the pandemic (March 12 to May 31; 8.7% [6.8–11.0]). The prevalence then increased back to the prepandemic level in the next 2 random replicates (June 1 to July 21; 14.2% [11.4–17.5] and August 1 to September 18; 11.9% [9.0–15.6]).47 These large studies demonstrate clearly that pandemic effects on mental health varied both by country and by time of assessment during the pandemic.
With those results in mind, it is noteworthy that only 3 of the 33 studies in the cohort study review40 came from the United States. These all involved small population segments: a convenience sample of n = 2288 sex- and gender-minority adults and 2 even smaller (n = 178–205) samples of students from single universities. Significant increases in screening scales of current anxiety-depression were found in all 3 studies. Although each study reported results in terms of means rather than proportions with clinically significant disorders, standardized mean differences can be converted into estimates of RR if we make assumptions about prepandemic prevalence and distributions.48 When we did this using the assumption that prepandemic anxiety-depression prevalence was in the plausible range of 5% to 10%, the RR equivalents were 1.3 to 2.8, which are below the lower end of the 3.0 to 8.0 range estimated in the noncomparable trend surveys.
All 3 US cohort studies in the review were carried out in small population segments, whereas the trend surveys were based on samples of the general population. We are aware of only one US cohort study that was carried out in a national general population sample shortly before and then again during the pandemic. This study was not included in the systematic review because it did not meet the requirement for a high follow-up response rate or nonresponse adjustment. Based on the RAND American Life Panel (ALP),49 this cohort study included an online survey of n = 2555 adults ages 20+ in February 2019, n = 2020 of whom also completed a follow-up survey in May 2020. SMI was assessed using the same screening scale as in the 2018 NHIS.25 However, the 2019 survey used the “worst month” version of that scale, which asks respondents to think of the 1 month in the past 12 when they had the most persistent and severe psychological distress when answering the questions, whereas the 2020 survey used the past-month version of the scale, which asks respondents to think of the month before the survey in answering the questions. The recommended approach is to administer both versions in a single survey,50 with the past-month version administered first to obtain information that approximates point prevalence and then only administering the worst month questions to the subset of respondents who report having a worse month than the current one. The latter estimate is needed in some jurisdictions for policy planning purposes.
SMI prevalence (95% CI) in these ALP cohort surveys was 10.9% (7.6–14.0) 12-month prevalence in 2019 and 10.1% (6.9–13.3) 1-month prevalence in 2020.51 Based on previous surveys that administered both versions of the scale to the same samples of respondents,50 the ratio of 1-month to 12-month prevalence in high-income countries is estimated to have a median (interquartile range) of 73.8% (50.4–80.2; Appendix Table 1). This would put the prepandemic 1-month SMI prevalence estimate in the ALP sample at 8.0% and RR during the pandemic versus before at approximately RR = 1.3. The latter is at the lower end of the RR = 1.3 to 2.8 range across the 3 true US cohort studies in the systematic review and well below the RR = 3.0 to 8.0 range in the US noncomparable trend surveys.
Taken together, these results suggest that the noncomparable trend surveys substantially overestimated the effect of the pandemic on population mental health. A central reason for this is likely to be selection bias owing to very high nonresponse in the nonprobability online surveys used to assess mental disorders during the pandemic. As mentioned earlier, although these nonprobability surveys were balanced to the population on basic geographic-demographic characteristics, it is likely that they were different in psychological characteristics from the population in ways that were not corrected by adjustments for geographic-demographic variables. To that point, it is noteworthy that the 8.0% best estimate of SMI prevalence in the prepandemic ALP survey, which had a similar sample design as the other online surveys used in the noncomparable trend comparisons, was more than 2 times the 3.4% estimate in the 2018 NHIS.23 Although the ALP is described as a “nationally representative, probability-based panel,”49 it is “representative” only in the sense that weights were used to make the joint distribution of the weighted sample on basic sociodemographic and geographic variables comparable to the distribution of the Census population. There is no reason to assume that the mental health of people in the ALP sample represents the mental health of the US population. The ALP response rate is likely less than 5%52 compared with the 61% response rate of the 2018 NHIS.
True trend surveys
True trend studies can provide equally, if not more, accurate information about change in disorder prevalence than cohort studies but with lower statistical power. Three relevant large-scale US government benchmark trend surveys exist to do this. Two of them, the NHIS and the BRFSS, were already mentioned. The third is the National Health and Nutrition Examination Survey (NHANES), a face-to-face household survey that combines physical examinations with self-reports in a sample of about 5000 respondents per year.53 The 2020 to 2021 NHIS and NHANES are both face-to-face surveys that were disrupted by the pandemic. The BRFSS, in comparison, is a telephone survey that continued without interruption during the pandemic in monthly replicates interviewing more than 400,000 respondents each year.35 At the time of writing this article, the 2020 BRFSS were only recently posted. We are not aware of any reports that have analyzed BRFSS trends into 2020.
We are aware of only one other true US national trend survey that has reported relevant data as of now: the annual November Gallup Poll Health and Healthcare survey. This is a national telephone survey carried out since 2001 in a random digit dial telephone sample with demographic weighting targets comparable to those in online surveys carried out during the pandemic.54 However, unlike the latter, the same design and field procedures used for many years in the annual Gallup survey were repeated in its November 2020 survey. One of the survey questions is “How would you describe your own mental health or emotional well-being at this time? Would you say it is excellent, good, only fair, or poor?” The proportion of respondents who answered “fair” or “poor” was higher in the 2020 survey than in any year since the survey began 2 decades ago: 23% compared with a median (interquartile range) in previous years of 13% (13–15). RR in 2020 versus 2019 was 1.5.55 Responses to this type of general excellent-to-poor mental health question are known to be strongly correlated with prevalence of CMDs (Appendix Table 2). Thus, although the Gallup survey does not provide direct estimates of depression anxiety, it does indirectly support the finding in cohort studies of more modest elevations in prevalence.
Administrative Trend Data
Emergency department visits
As noted above, changes in factors other than true prevalence can influence trends in administrative data, making it important to be cautious in interpreting such data. These extraneous influences are perhaps not clearer than in trend data on ED visits, which dropped by 42% nationwide in the first 2 months of the COVID-19 pandemic compared with the same months in 2019,56 increased subsequently up until August 2020 to become about 15% lower than in the prior year, and then decreased again to become about 25% lower than the prior year in the first months of 2021.57 The disorder-specific patterns in these ED visit trends are inconsistent with changes in true prevalence.58 , 59 The trends more likely occurred because people who would otherwise have come to the ED failed to do so because of fear of COVID-19 exposure, minimizing nonurgent care, or reduced access to care because of loss of insurance in conjunction with job loss.
Based on this complex set of possibilities, some researchers have focused on proportional changes in presenting problems in ED visits rather than absolute changes.57 , 60 These studies show that even though absolute volume of ED visits for mental health problems decreased since the beginning of the pandemic, the proportional decrease has been lower than that for many other presenting problems. This finding has sometimes been interpreted to mean that a higher proportion of mental disorders that would otherwise be seen at an ED exceed the severity threshold that led people to seek ED treatment even during the pandemic.60 However, this interpretation is difficult to accept given that substantial reductions in ED visits occurred for many life-threatening illnesses during the pandemic, resulting in the proportion of deaths from natural causes occurring at home increasing substantially since the beginning of the pandemic.61
Another possibility is that alternatives to ED treatment decreased more for mental disorders than physical disorders during the pandemic.62 A related possibility is that changes in relative severity of ED presentations within conditions changed during than before the pandemic in ways that led to differences in overall visits across conditions because of delays in typical help-seeking patterns. For example, the number of patients presenting at EDs with complicated appendicitis increased significantly during the pandemic, whereas the number with uncomplicated appendicitis decreased, indicating that people with appendicitis were waiting longer before going to the ED during the pandemic than before.63 We are aware of no attempts to compare changes in severity of ED mental disorder presentations during versus before the pandemic.
Although these complexities make it impossible to draw firm conclusions from ED trend data about changes in true prevalence of mental disorders during the pandemic, there are 2 exceptions: ED visits for suicide attempts among adolescents and Emergency Medical Services (EMS) activations for drug overdoses both increased in absolute numbers during the pandemic. The most plausible interpretation of these increases is that they were caused by true increases in prevalence, as the ED would normally be the first-line treatment for both these presentations. The number of adolescent (ages 12–17) ED visits for suspected suicide attempts was 22.3% higher in the summer of 2020 than the summer of 2019 and 39.1% higher in the winter of 2021 than the winter of 2019.64 No comparable absolute increase occurred among adults. In the case of drug overdoses, although an absolute increase in number of ED visits reported by the CDC60 appears to have been an artifact of the ED sample in that study increasing in size over time,62 data from the National Emergency Medical Services Information System documents a 42.1% increase in EMS activations for overdose-related cardiac arrests in 2020 compared with 2019.65 This appears to be another example of delays in help-seeking resulting in a higher proportion of comparatively severe cases presenting for care during than before the pandemic. The fact that this dramatic increase in EMS activations was not reflected in ED visits suggests that many of the overdoses resulted in death before reaching the ED. As we see in the next subsection, mortality trend data are consistent with this interpretation.
Mortality
Total number of deaths in the United States increased by 503,976 in 2020 compared with 2019.66 An estimated 345,323 of these excess deaths were classified by CDC as directly owing to COVID-19,67 making COVID-19 the third leading cause of death in 2020 behind only heart disease and cancer. However, there were also substantial increases in death from several other leading causes, including cardiometabolic disorders: heart disease (20% of the total excess not owing directly to COVID-19), diabetes (8%), and stroke (6%).68 These increases presumably occurred because of disrupted treatments and incorrect classification of some such deaths as due to chronic conditions when they were in fact due to COVID-19.69
Suicide deaths did not increase in 2020. Indeed, the US suicide rate was slightly lower in 2020 than 2019,68 consistent with evidence from other countries in the early months of the pandemic.70 However, initial declines in suicides during other infectious disease outbreaks have sometimes been followed by increases,71 so it might be that increased suicides will occur as a late consequence of the COVID-19 pandemic. Preliminary evidence for such a scenario has already been reported in Japan.72
Deaths owing to 3 other external causes increased significantly during the pandemic: homicides, drug overdoses, and unintentional injury deaths.73 The most recent CDC quarterly provisional mortality data found that there were 30% more homicides in both the second and the third quarters of 2020 compared with the same quarters in 2019.74 An important factor in this trend is that close to 80% of all US homicides are committed with firearms,75 and firearm sales skyrocketed during the early part of the pandemic in conjunction with the social and political unrest and violent protests that surrounded the last year of the Trump presidency.76 A recent report found that between-state variation in increased firearm purchases during the COVID-19 pandemic was correlated with between-state increases in both fatal and nonfatal firearm-related interpersonal violence during the early months of the pandemic.77 Importantly, this significant pattern was only for domestic violence (RR = 1.8–2.6), not for nondomestic violence (RR = 0.8–1.0).
Although the increased RR in firearm-related domestic violence was higher than that for increased drug overdose deaths (RR = 1.5 in Q2 2020), overdoses accounted for a much larger absolute number of excess deaths.74 Indeed, the CDC estimated that drug overdose deaths increased by 22,473 in 2020 compared with 2019 (14% of the total excess deaths not owing directly to COVID-19),78 which was a worsening of a trend that began in 2019.79 As a result, the United States saw the highest number of overdose deaths, 95,230 total in 2020, ever recorded in a single year.78 The pandemic also saw an increased proportion of overdose deaths owing to synthetic opioids other than methadone, with the greatest increases observed in the West and among racial/ethnic minorities and people living in socioeconomically disadvantaged communities.80
Although drug overdoses accounted for most increased unintentional injury deaths so far during the pandemic, an increase in unintentional firearm deaths also occurred. We noted above that firearm sales spiked early in the pandemic. It is noteworthy that a similar spike in firearm purchasing in the aftermath of the Sandy Hook school shooting was found to be associated with a time-lagged spike in unintentional firearm deaths that covaried with between-state variation in increased firearm purchasing.81 A similar increase during the COVID-19 pandemic can be inferred from the observation that the absolute increase in firearm deaths in the second and third quarters (Q2–Q3) of 2020 increased more than firearm-related homicides.74 Although we are aware of no direct study of such deaths among adults, unintentional firearm-related injuries increased among children by RR = 1.9 during 2020 Q2–Q3 and were especially pronounced in states with high increases during the pandemic in firearms purchases.82
Surprisingly, road traffic fatalities were another significant contributor to the increase in unintentional injury deaths during the first year of the pandemic. The National Safety Council (NSC) estimated that 42,060 people died in motor vehicle crashes in 2020, which represented an 8% increase compared with 2019. This happened despite the number of miles driven in 2020 dropping 13% compared with 2019.83 The 2020 increase in rate of traffic deaths was the largest single-year jump documented by the NSC in the last 96 years. Similar findings were described by the National Highway Traffic Safety Administration.84
Crisis Line Calls
Numerous mass media stories early in the pandemic reported that suicide and mental health crisis lines were being overwhelmed with increased calls85 and that increased crisis line calls from teenagers continued as school closings went into the next fall.86 We are aware of only one large-scale study on this trend. That study examined trends in calls to the National Suicide Prevention Lifeline (NSCL)87 and found that call volume increased in 2020 Q2 compared with 2019 Q2 in 28 states by RR = 1.01 to 1.3 but decreased in the remaining 22 states.88 No association was found between state-level COVID-19 infection and change in NSCL call volume. We subsequently examined associations of the state-level call volume data in this report with (i) state-level prevalence of anxiety-depression in the 2 years before the beginning of the pandemic (as assessed in the BRFSS), (ii) increase in state-level anxiety-depression over 2020 Q2 compared with 2018 to 2019 (as assessed in the HPS compared with predicted values based on the BRFSS), and (iii) increases in the state-level unemployment rate in 2020 Q2 compared with 2019 Q2. None of these associations was significant either statistically or substantively (R 2 = −0.020–0.011).
A more focused study of 911 calls for mental health issues in Detroit during the early months of the pandemic found that call volume declined relative to the same months in the prior 3 years.89 This finding is broadly consistent with 2 surveys carried out in April 2020 and April 2021 by the National Association of Emergency Medical Technicians with leaders of EMS agencies throughout the country.90 Of agencies, 61% reported decreases in call volume in the 2020 and 43% in 2021. In comparison, several reports showed that 911 calls for domestic violence increased RR = 1.1 to 1.3 during the early months of the pandemic (reviewed by Refs.91, 92, 93). However, more recent evidence suggests that call volume might have subsequently returned to prepandemic levels.94
Summary of the evidence on trends in mental disorder prevalence since before the pandemic
Taken together, the above evidence suggests that COVID-19 has so far had a significant impact on point prevalence of anxiety-depression spectrum disorders and serious drug use disorders in the US adult population, albeit substantially less than that posited by early reviews. The point prevalence of anxiety-depression likely increased by about 30% to 50%, although the impact on more persistent anxiety-depression was not assessed in any of these studies. It is also noteworthy that data collected in within-pandemic cohort and trend surveys reviewed later in the article show that the numerator for these ratios (ie, prevalence within the pandemic) changed rather substantially over the course of the pandemic. In particular, the during-pandemic waves in the ALP national cohort survey and the Gallup national trend survey both occurred at times during the pandemic estimated to have comparatively high prevalence. Effects in this range RR = 1.3 to 1.5 are important, but not nearly as high as the RR = 3.0 to 8.0 estimates obtained in the noncomparable trend studies that have been the major focus of media attention.
Changes in mental health disparities since before the pandemic
Another important question concerns disparities in the effects of the pandemic on population mental health. We know from previous research that the component stressors caused by the pandemic, including job loss,95 death of a loved one,96 social isolation,97 and a combination of multiple such stressors,98 have negative effects on mental health. Given that exposure to these experiences during the pandemic has been significantly higher in some already disadvantaged segments of the population99 , 100 and that the psychological impact of pandemic-related stressors might have been greater among already disadvantaged segments of the population,101 we might expect that prepandemic health disparities would be magnified by the pandemic.
Research on this possibility can be carried out most directly by making comparisons within cohorts. The one true cohort study we described above, the RAND ALP, did this and found that individual-level increases in psychological distress during compared with before the pandemic were significantly more common among women than men (odds ratio [OR] = 1.9), respondents younger than 60 compared with those 60+ years old (OR = 2.4–1.7), and Hispanic compared with non-Hispanic white individuals (OR = 1.9).51
Trend data can also be used to make such comparisons, but less powerfully so than in cohort studies because trend studies require evidence of variation in the associations of social disadvantage with mental disorder over time (ie, statistical interactions). However, as only one of the large government benchmark trend surveys with relevant information has been reported for 2020 (the BRFSS reported these data in August 2021, after this article was completed), data from noncomparable trend surveys are the only ones available to provide preliminary information, albeit with the recognition that the differences in sample frames, field procedures, and response rates could introduce bias into these comparisons.
The noncomparable trend survey reports all presented data on the sociodemographic correlates of anxiety-depression during the pandemic, but in most cases did not comment on the possibility that these associations predated the pandemic. The few studies that made such comparisons found consistently that anxiety-depression increased most dramatically among young adults and least among black individuals,23 , 36 but these were weak comparisons because the surveys carried out during the pandemic were relatively small.
We carried out a more thorough analysis of such differences by comparing associations of core sociodemographic variables (age, sex, race-ethnicity, education) with anxiety-depression in the publicly available 2018 to 2019 BRFSS (n = 839,366) and 2020 to 2021 CDC HPS (n = 2,373,044) data sets. The outcome was a dichotomous measure representing a clinically significant score for anxiety-depression on the PHQ-4 screening scale (6+ on the 0–12 response scale).34 Some preprocessing was needed before the comparisons could be made, though, as the PHQ-4 was administered only to a subsample of BRFSS respondents. We consequently imputed predicted probabilities of clinically significant PHQ-4 scores to the remainder of the BRFSS sample based on a logistic regression model estimated in the subsample where the PHQ-4 was administered. Predictors in the model included all the sociodemographic variables in the substantive analysis reported below plus scores on the screening scales of mental disorder included in all BRFSS interviews (questions about number of days in poor mental health and number of days of role impairment owing to poor mental or physical health). The model had strong cross-validated accuracy in a holdout test sample (area under the receiver operating characteristic curve [AUC = 0.90]). The associations of the sociodemographic variables with predicted scores were also comparable in cross-validation to those with the observed scores (Appendix Table 3). To make associations comparable in the 2 surveys, we coarsened the observed PHQ-4 score in the HPS to generate a predicted score similar to the predicted score in the BRFSS. That predicted score had a comparable association with the observed dichotomy for PHQ-4 = 6+ as in the BRFSS (AUC = .88, Appendix Fig. 1).
As expected, comparisons across the 2 surveys found that estimated prevalence of PHQ-4 = 6+ scores was substantially higher in the HPS (26.4%) than the BRFSS (10.9%; Table 1 ). However, the RR among women compared with men was the same in the 2 surveys (RR = 1.2), resulting in the HPS:BRFSS interaction with sex being RRH:B = 1.0. This suggests that prevalence increased by similar proportions among women and men. On the other hand, the prevalence of PHQ-4 = 6+ increased substantially more for respondents younger than 60 than those 60+ years of age. in the HPS (29.9%–41.8%) compared with before the pandemic (ie, 2018–2019 BRFSS, resulting in RRH:B = 1.6–1.7 for 18–59 compared with 60+). Unlike some previous reports suggesting that prevalence increased less among blacks than other individuals, we found that proportional prevalence was slightly higher among non-Hispanic black individuals than non-Hispanic white individuals in HPS than BRFSS (RRH:B = 1.2) and much higher among Hispanic individuals (RRH:B = 1.8) and other races (RRH:B = 1.8) than non-Hispanic white individuals. Finally, we found that individuals with lower education levels had higher PHQ-4 scores both before and during the pandemic, but that these differences became more pronounced during the pandemic, resulting in RRH:B being relatively comparable across the 3 lower levels of education relative to the highest level (1.5–1.7).
Table 1.
Change in the univariate and multivariate associations of sociodemographic variables with clinically significant anxiety-depression (PHQ-4 = 6+) between the 2018-2019 CDC Behavioral Risk Factors Surveillance Survey (n = 839,366) and April 2020 to July 2021 CDC Household Pulse Survey (n = 2,373,044)a
| Behavioral Risk Factors Surveillance Survey (BRFSS) |
Household Pulse Survey (HPS) |
HPS: BRFSS |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence |
Univariate |
Multivariate |
Prevalence |
Univariate |
Multivariate |
Univariate |
Multivariate |
|||||||||
| % | (SE) | RR | (95% CI) | RR | (95% CI) | % | (SE) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | RR | (95% CI) | |
| Sex | ||||||||||||||||
| Female | 12.0 | (0.1) | 1.2b | (1.2–1.3) | 1.3b | (1.3–1.3) | 28.8 | (0.0) | 1.2b | (1.2–1.2) | 1.3b | (1.3–1.3) | 1.0b | (0.9–1.0) | 1.0 | (1.0–1.0) |
| Male | 9.8 | (0.1) | 1.0 | 1.0 | 24.2 | (0.0) | 1.0 | 1.0 | 1.0 | 1.0 | ||||||
| χ21 | 229.7b | 387.2b | 310.3b | 748.2b | 3.9b | 0.5 | ||||||||||
| Age | ||||||||||||||||
| 18–29 | 14.4 | (0.1) | 1.8b | (1.8–1.9) | 2.0b | (1.9–2.0) | 41.8 | (0.1) | 3.1b | (3.0–3.2) | 2.9b | (2.8–3.0) | 1.7b | (1.6–1.8) | 1.5b | (1.4–1.6) |
| 30–44 | 11.2 | (0.1) | 1.4b | (1.4–1.5) | 1.7b | (1.6–1.7) | 29.9 | (0.1) | 2.2b | (2.1–2.3) | 2.3b | (2.2–2.4) | 1.6b | (1.5–1.6) | 1.4b | (1.3–1.5) |
| 45–59 | 11.5 | (0.1) | 1.5b | (1.4–1.5) | 1.6b | (1.5–1.6) | 31.4 | (0.1) | 2.3b | (2.3–2.4) | 2.3b | (2.2–2.4) | 1.6b | (1.5–1.7) | 1.5b | (1.4–1.5) |
| 60+ | 7.9 | (0.0) | 1.0 | 1.0 | 13.5 | (0.0) | 1.0 | 1.0 | 1.0 | |||||||
| χ23 | 1029.0b | 1345.9b | 4231.6b | 4135.6b | 507.3b | 311.0b | ||||||||||
| Education | ||||||||||||||||
| Less than high school | 19.5 | (0.2) | 4.2b | (4.0–4.3) | 5.0b | (4.8–5.2) | 59.5 | (0.2) | 6.8b | (6.6–7.0) | 6.5b | (6.3–6.7) | 1.6b | (1.5–1.7) | 1.3b | (1.2–1.4) |
| High school graduate | 13.4 | (0.1) | 2.9b | (2.8–3.0) | 2.9b | (2.8–3.0) | 37.3 | (0.1) | 4.3b | (4.2–4.4) | 4.4b | (4.3–4.5) | 1.5b | (1.4–1.6) | 1.5b | (1.5–1.6) |
| Some college | 10.7 | (0.1) | 2.3b | (2.2–2.4) | 2.3b | (2.2–2.3) | 34.2 | (0.1) | 3.9b | (3.8–4.0) | 3.8b | (3.8–3.9) | 1.7b | (1.6–1.8) | 1.7b | (1.6–1.8) |
| College graduate/more | 4.7 | (0.0) | 1.0 | 1.0 | 8.8 | (0.0) | 1.0 | 1.0 | 1.0 | |||||||
| χ23 | 4706.8b | 5395.0b | 22,755.0b | 21,496.2b | 625.1b | 623.3b | ||||||||||
| Race | ||||||||||||||||
| Non-Hispanic black | 15.8 | (0.1) | 1.5b | (1.4–1.5) | 1.2b | (1.2–1.3) | 39.9 | (0.1) | 1.8b | (1.8–1.9) | 1.3b | (1.3–1.3) | 1.2b | (1.2–1.3) | 1.1b | (1.0–1.1) |
| Hispanic | 9.5 | (0.1) | 0.9b | (0.8–0.9) | 0.6b | (0.5–0.6) | 34.1 | (0.1) | 1.6b | (1.5–1.6) | 1.0 | (1.0–1.0) | 1.8b | (1.7–1.9) | 1.7b | (1.6–1.8) |
| Other race | 8.9 | (0.1) | 0.8b | (0.8–0.9) | 0.8b | (0.7–0.8) | 32.5 | (0.1) | 1.5b | (1.4–1.6) | 1.3b | (1.2–1.3) | 1.8b | (1.7–1.9) | 1.6b | (1.5–1.7) |
| Non-Hispanic white | 10.7 | (0.0) | 1.0 | 1.0 | 21.7 | (0.0) | 1.0 | 1.0 | 1.0 | |||||||
| χ23 | 578.7b | 744.0b | 2838.6b | 533.1b | 722.6b | 517.1b | ||||||||||
| Total | 10.9 | (0.0) | 26.4 | (0.0) | ||||||||||||
Estimated using robust Poisson regression models.102 The dependent variable was a random 0/1 draw from a Bernoulli distribution with a fixed random seed from a separate predicted probability assigned to each respondent from an imputed predicted probability generated by a separate internally cross-validated logistic regression in each sample. These models are described in Appendix Tables 3 (BRFSS) and 4 (HPS). The imputation was necessary in BRFSS because the PHQ-4 was administered only in 3 stated in 2018, although, as detailed in Appendix Table 3, other measures assessed in the entre sample were strongly associated with PHQ 4 = 6+ (AUC = .90). The imputation was not necessary in HPS because the PHQ-4 was administered in the entire sample. However, for purposes of making a fair comparison of predictors with the outcome across the 2 surveys, we coarsened the PHQ score (Appendix Table 4) to make the association between true scores and predicted probabilities comparable across surveys. In addition, a propensity score 1/p weight was imposed on the HPS data to adjust for the fact that the 12% of respondents missing the PHQ-4 questions were not random with respect to sociodemographic characteristics, geography, or time. Logistic regression with the same predictors as in the substantive model as well as dummy variables for state and survey wave was used to estimate predicted probability of answering the PHQ-4 questions for purposes of generating the 1/p weight.
Significant at the 0.05 level.
Changes in mental disorder prevalence over the course of the pandemic
Although the HPS is by far the largest trend survey carried out during the pandemic, several nongovernment multiwave trend surveys were initiated shortly after the onset of the pandemic to track the prevalence and correlates of diverse policy-related issues (eg, Refs.103, 104, 105, 106). The 2 largest and with the most waves among these are as follows: (i) The COVID States Project (CSP), a series of Internet trend surveys carried out roughly monthly in samples mostly of n = 20,000 to 25,000 respondents from nonprobability consumer panels107; and (ii) The University of Southern California Understanding America Study (UAS) Panel, a panel of approximately n = 9500 people assembled by the USC Center for Economic and Social Research beginning in 2014 to carry out diverse surveys on a wide range of topics,108 but carrying out an ongoing tracking survey on COVID-related topics beginning at the very onset of the pandemic. Each UAS panel member was invited to respond on one assigned day every 2 weeks beginning in early March 2020, with the rotation changing to 1 day every month since mid-March 2021.109 This design allows for aggregation of trend data over weekly, biweekly, or other designated time intervals and allows analysis of cohort (ie, within-person) changes.
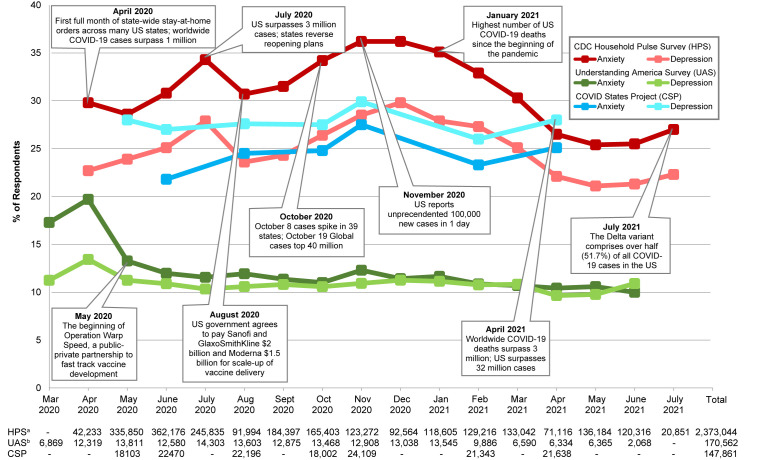
The HPS, CSP, and UAS all use either the PHQ-4, which includes separate 2-item subscales of anxiety (Generalized Anxiety Disorder (GAD)-2) and depression (PHQ-2), or, in the case of the CSP, the full PHQ-9 depression scale in addition to the GAD-2, to track anxiety-depression during the pandemic. We aggregated prevalence estimates by month within surveys using standard thresholds of clinically significant anxiety (GAD-2 = 3+) and depression (PHQ-2 = 3+ or PHQ-9 = 10+) and plotted trends (Fig. 1 ). These trends are quite different across surveys, with Pearson correlations of month-by-month variation in the range r = 0.39 (UAS anxiety and CSP depression) to r = −0.13 (UAS depression and CPS anxiety; Table 2 ). Overall, correlations (mean [range]) are highest between HPS and CSP (r = 0.26 [0.15–0.38]) and lower between these surveys and UAS (r = 0.08 [−0.13–0.39]). It is noteworthy in this regard that HPS and CSP are both trend surveys in which only a subset of respondents participate in more than one wave, whereas the UAS is a rolling panel trend survey in which the n = 9500 UAS panel members were surveyed many times both before and since the onset of the pandemic. This repeated surveying might have led to panel fatigue, which could account for why prevalence estimates are substantially lower in UAS than the other 2 surveys even though all 3 surveys were weighted to be nationally representative on the cross-classification of demographic-geographic variables.110
Fig. 1.
Comparing trends in anxiety and depression during the pandemic across studies: HPS, CSP, UAS. aThere were 2,745,185 observations in the HPS from April 2020 to July 2021. In this figure, the authors excluded any observations that were missing values for questions on anxiety or depression from the PHQ-4 for a total sample size of 2,373,044 observations. In instances when multiple waves of the survey were carried out in a single month, equal weight was given to the surveys as a function of number of days in the month covered rather than comparative sample size. In instances when a single wave was carried out across 2 months, the overall prevalence in that wave to both months was attributed based on number of days covered. For example, if a single wave was carried out in the last 5 days of 1 month and the first 2 days of the next month, the prevalence in the survey was counted as applying to 5 days in the first month and 2 days in the second month. If one additional wave was carried out over in the first month for a total of 14 days, for example, the prevalence in the overlapping wave would contribute 5/19 to the estimated prevalence in the month (and the first wave would contribute 14/19 to the estimated prevalence). bThere were 173,823 observations in the UAS. In this figure, the authors excluded 3261 observations that were missing values for questions on anxiety or depression from the PHQ-4 or who had an incomplete survey date for a total sample size of 170,562 observations. It is noteworthy in this regard that HPS and CSP are both trend surveys in which only a tiny proportion of respondents participate in more than one wave, whereas the UAS is a rolling panel trend survey in which the n = 9500 UAS panel members are surveyed repeatedly over time. This might have led to panel fatigue, which could account for why prevalence estimates are substantially lower in UAS than the other 2 surveys even though all 3 surveys were weighted to be nationally representative on the cross-classification of demographic-geographic characteristics.
Table 2.
Pearson correlations between monthly trends in clinically significant anxiety-depression prevalence across major within-pandemic tracking surveys between March 2020 and July 2021
| HPS |
UAS |
CSP |
||||
|---|---|---|---|---|---|---|
| Anx | Dep | Anx | Dep | Anx | Dep | |
| Household Pulse Survey (HPS) | ||||||
| Anxiety (Anx) | 1.0 | |||||
| Anxiety (Anx) and Depression (Dep) should be slightly indented under Household Pulse Survey (HPS) | ||||||
| Depression (Dep) | 1.0a | 1.0 | ||||
| Understanding America Survey (UAS) | ||||||
| Anxiety (Anx) | 0.0 | −0.1 | 1.0 | |||
| Anxiety (Anx) and Depression (Dep) should be slightly indented under Understanding America Survey (UAS) | ||||||
| Depression (Dep) | 0.2 | 0.1 | 0.8a | 1.0 | ||
| COVID States Project (CSP) | ||||||
| Anxiety (Anx) | 0.4 | 0.3 | 0.2 | −0.1 | 1.0 | |
| Anxiety (Anx) and Depression (Dep) should be slightly indented under COVID States Project (CSP) | ||||||
| Depression (Dep) | 0.2 | 0.2 | 0.4 | 0.0 | 0.9a | 1.0 |
Significant at the 0.05 level, 2-sided test based on a sample of between 6 and 16 mo. See Fig. 1 for the number of common monthly data points for each pair of surveys.
Several other patterns in the trend figure are noteworthy. First, the UAS panel was already active before the pandemic, allowing the first COVID-19 survey to be fielded more quickly, 1 month after the United States declared COVID-19 a public health emergency111 than the HPS and CSP surveys. This allowed UAS to pick up an acute upswing in both anxiety-depression associated with the statewide stay-at-home orders that began in late March (eg, California, 19 March 2020; New York and Illinois, 20 March 2020; New Jersey, 21 March 2020; Ohio, 22 March 2020; and many other states. 23 March 2020). However, UAS prevalence estimates dropped precipitously after the April spike and showed only attenuated evidence of subsequent spikes that were picked up in the other surveys.
HPS, in comparison, picked up a 1-month spike in prevalence in July 2020, the month the United States surpassed 3 million COVID-19 cases. CSP did not field a wave that month. An increase in prevalence between August 2020 and November 2020 (the first time 100,000 COVID-19 cases were reported in a single day112) was then detected by all 3 surveys, with the increase continuing in December for depression in HPS (CSP did not have a December 2020 wave), although this trend was weak and only for anxiety in UAS. The time between August and November coincided with the most dramatic increase to date in COVID-19 deaths, with a peak at the end of December (4169 COVID-19 deaths, January 13, 2021).113 Anxiety-depression prevalence declined after that time period in conjunction with a precipitous decline in COVID-19 cases through mid-June (8463 cases, June 14, 2021 compared with a high of 292,713 cases, January 6, 2021) and COVID-19 deaths through early July (140 deaths, July 11, 2021). A slight upswing in HPS anxiety-depression and UAS depression occurred near the end of the time series, which coincided with the emergence of the Delta variant114 and subsequent increases in cases and deaths. The last CSP wave was in April but showed an upswing in anxiety-depression prevalence before the other surveys.
Changes in mental health disparities over the course of the pandemic
The bulk of research on mental health disparities during the pandemic has focused on comparative cross-sectional analyses. These show clearly that socially disadvantaged segments of the population are at increased risk of exposure to pandemic-related stressors, including personal infection, death of a loved one, and financial loss.99 , 100 , 115 , 116 These analyses also document significant over-time associations between aggregate changes in pandemic-related stressors and changes in anxiety-depression.117, 118, 119, 120, 121, 122 We are not aware of studies investigating the possibility that the associations of individual-level exposure to pandemic-related stressors with subsequent onset-worsening of anxiety-depression are different among disadvantaged than other segments of the population. The latter studies would require the use of cohort data, as it would be necessary to control for baseline anxiety-depression owing to the existence of reciprocal relationships between prior mental disorders and some types of stressor exposure.123 , 124 Nonetheless, the existing evidence on stressor exposure is sufficient to think that mental health disparities might have increased over the course of the pandemic.
We are not aware of any attempt to determine whether systematic changes have occurred in these disparities over the course of the pandemic. We expanded our earlier analysis of sociodemographic correlates in the HPS to do this. We began by disaggregating the HPS data over 6 time periods within the pandemic, indicating corresponding to changes in anxiety-depression prevalence. We then estimated the same model as in Table 1 separately within each of these time periods and compared results. To facilitate these comparisons, the RR estimates were centered within each of the 6 time periods so that they multiplied to 1.0 across categories of each predictor.
Women had an elevated risk of clinically significant PHQ-4 scores compared with men over the full HPS series (29.6% vs 23.5%, χ2 1 = 650.8, P<.001) with an unadjusted RR of 1.3 that varied only modestly) across the time periods defined here and were not changed meaningfully by multivariate controls for other sociodemographics (Table 3 ). A similar consistency over time can be seen in the association between age and PHQ-4 scores. The univariate association is significant in the total sample (χ2 3 = 3582.5, P<.001) based on a monotonically decreasing prevalence with age from a high of 38.7% among respondents ages 18 to 29 to a low of 17.6% among those 60+ years and intermediate prevalence among those ages 30 to 44 years (30.8%) and 45 to 59 years (27.0%). Centered RR among the youngest respondents varies monotonically but modestly with time in the range RR = 1.3 to 1.6. Similarly small but nonmonotonic changes in centered RR can be seen in the other age groups.
Table 3.
Variation in the multivariate associations of sociodemographic variables with clinically significant anxiety-depression (PHQ-4 = 6+) across weeks of the CDC Household Pulse Survey, April 2020 to July 2021 (n = 2,373,044)b,c
| April–June 2020 (n = 650,000) |
Late June–July 2020 (n = 336,084) |
August–October 2020 (n = 426,584) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence |
Prevalence |
Prevalence |
||||||||||
| % | (SE) | RR | (95% CI) | % | (SE) | RR | (95% CI) | % | (SE) | RR | (95% CI) | |
| Sex | ||||||||||||
| Female | 28.7 | (0.1) | 1.1a | (1.1–1.2) | 31.8 | (0.1) | 1.1a | (1.1–1.1) | 29.3 | (0.1) | 1.1a | (1.1–1.2) |
| Male | 22.3 | (0.1) | 0.9a | (0.9–0.9) | 26.5 | (0.1) | 0.9a | (0.9–0.9) | 22.6 | (0.1) | 0.9a | (0.9–0.9) |
| χ21 | 244.5a | 101.9a | 441.6a | |||||||||
| Age | ||||||||||||
| 18–29 | 36.5 | (0.2) | 1.4a | (1.3–1.4) | 40.5 | (0.3) | 1.3a | (1.3–1.4) | 37.8 | (0.3) | 1.4a | (1.3–1.4) |
| 30–44 | 28.7 | (0.1) | 1.1a | (1.1–1.2) | 34.5 | (0.1) | 1.2a | (1.1–1.2) | 31.4 | (0.1) | 1.2a | (1.1–1.2) |
| 45–59 | 26.2 | (0.1) | 1.0 | (1.0–1.0) | 30.0 | (0.1) | 1.0 | (1.0–1.0) | 26.2 | (0.1) | 1.0a | (0.9–1.0) |
| 60+ | 16.3 | (0.1) | 0.6a | (0.6–0.7) | 19.3 | (0.1) | 0.6a | (0.6–0.7) | 18.3 | (0.1) | 0.7a | (0.6–0.7) |
| χ23 | 806.4a | 633.7a | 1276.5a | |||||||||
| Education | ||||||||||||
| Less than high school | 31.9 | (0.4) | 1.2a | (1.1–1.2) | 37.7 | (0.6) | 1.2a | (1.1–1.3) | 32.6 | (0.5) | 1.2a | (1.1–1.3) |
| High school graduate | 27.8 | (0.2) | 1.1a | (1.0–1.1) | 30.3 | (0.2) | 1.0 | (1.0–1.1) | 26.3 | (0.2) | 1.0 | (0.9–1.0) |
| Some college | 27.9 | (0.1) | 1.0 | (1.0–1.1) | 32.6 | (0.2) | 1.0a | (1.0–1.1) | 29.7 | (0.1) | 1.0a | (1.0–1.1) |
| College graduate/more | 20.9 | (0.1) | 0.8a | (0.8–0.8) | 24.6 | (0.1) | 0.8a | (0.8–0.8) | 23.0 | (0.1) | 0.8a | (0.8–0.8) |
| χ23 | 457.8a | 328.5a | 627.2a | |||||||||
| Race | ||||||||||||
| Non-Hispanic black | 29.2 | (0.2) | 1.0 | (1.0–1.1) | 30.3 | (0.3) | 0.9 | (0.9–1.0) | 27.0 | (0.3) | 1.0 | (0.9–1.0) |
| Hispanic | 29.0 | (0.2) | 1.0 | (1.0–1.0) | 32.3 | (0.3) | 0.9a | (0.9–1.0) | 30.3 | (0.2) | 1.0 | (1.0–1.1) |
| Other race | 26.9 | (0.2) | 1.0 | (1.0–1.1) | 34.5 | (0.3) | 1.1a | (1.1–1.2) | 27.0 | (0.2) | 1.0 | (0.9–1.0) |
| Non-Hispanic white | 23.6 | (0.1) | 1.0a | (0.9–1.0) | 27.2 | (0.1) | 1.0 | (1.0–1.0) | 24.9 | (0.1) | 1.0 | (1.0–1.0) |
| χ23 | 5.7 | 17.5a | 3.2 | |||||||||
| Total | 25.4 | (0.0) | 29.0 | (0.1) | 26.0 | (0.1) | ||||||
| November–February 2021 (n = 354,843) |
February–March 2021 (n = 257,066) |
April–July 2021 (n = 348,467) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence |
Prevalence |
Prevalence |
||||||||||
| % | (SE) | RR | (95% CI) | % | (SE) | RR | (95% CI) | % | (SE) | RR | (95% CI) | |
| Sex | ||||||||||||
| Female | 33.9 | (0.1) | 1.1a | (1.1–1.2) | 30.0 | (0.1) | 1.1a | (1.1–1.1) | 23.9 | (0.1) | 1.1a | (1.1–1.2) |
| Male | 26.5 | (0.1) | 0.9a | (0.9–0.9) | 24.2 | (0.1) | 0.9a | (0.9–0.9) | 18.9 | (0.1) | 0.9a | (0.9–0.9) |
| χ21 | 328.8a | 202.5a | 230.7a | |||||||||
| Age | ||||||||||||
| 18–29 | 44.7 | (0.3) | 1.4a | (1.3–1.4) | 41.4 | (0.4) | 1.4a | (1.4–1.5) | 36.2 | (0.3) | 1.6a | (1.5–1.6) |
| 30–44 | 35.7 | (0.1) | 1.1a | (1.1–1.2) | 31.8 | (0.2) | 1.1a | (1.1–1.2) | 26.2 | (0.1) | 1.2a | (1.1–1.2) |
| 45–59 | 30.6 | (0.1) | 1.0a | (0.9–1.0) | 26.3 | (0.2) | 0.9a | (0.9–1.0) | 21.3 | (0.1) | 0.9a | (0.9–1.0) |
| 60+ | 21.4 | (0.1) | 0.7a | (0.6–0.7) | 18.4 | (0.1) | 0.6a | (0.6–0.7) | 13.0 | (0.1) | 0.6a | (0.5–0.6) |
| χ23 | 993.5a | 1010.5a | 1377.0a | |||||||||
| Education | ||||||||||||
| Less than high school | 40.1 | (0.6) | 1.2a | (1.1–1.3) | 35.3 | (0.7) | 1.2a | (1.1–1.3) | 29.9 | (0.6) | 1.3a | (1.2–1.3) |
| High school graduate | 32.0 | (0.2) | 1.0 | (1.0–1.0) | 28.5 | (0.3) | 1.0 | (1.0–1.0) | 23.5 | (0.2) | 1.0a | (1.0–1.1) |
| Some college | 33.9 | (0.2) | 1.0a | (1.0–1.0) | 31.4 | (0.2) | 1.0a | (1.0–1.1) | 25.3 | (0.2) | 1.1a | (1.0–1.1) |
| College graduate/more | 26.0 | (0.1) | 0.8a | (0.8–0.8) | 22.9 | (0.1) | 0.8a | (0.8–0.8) | 16.9 | (0.1) | 0.7a | (0.7–0.7) |
| χ23 | 765.5a | 586.2a | 1055.2a | |||||||||
| Race | ||||||||||||
| Non-Hispanic black | 34.4 | (0.3) | 1.1 | (1.0–1.1) | 30.3 | (0.3) | 1.0 | (1.0–1.1) | 24.0 | (0.3) | 1.0 | (0.9–1.1) |
| Hispanic | 34.6 | (0.3) | 1.0 | (0.9–1.0) | 30.6 | (0.3) | 1.0 | (0.9–1.0) | 26.5 | (0.2) | 1.0 | (1.0–1.1) |
| Other race | 31.3 | (0.3) | 1.0 | (0.9–1.0) | 29.2 | (0.3) | 1.0 | (1.0–1.1) | 23.7 | (0.2) | 1.0 | (1.0–1.1) |
| Non-Hispanic white | 28.7 | (0.1) | 1.0 | (0.9–1.0) | 25.7 | (0.1) | 1.0 | (1.0–1.0) | 19.7 | (0.1) | 0.9a | (0.9–1.0) |
| χ23 | 4.5 | 4.8 | 11.7a | |||||||||
| Total | 30.3 | (0.1) | 27.1 | (0.1) | 21.4 | (0.1) | ||||||
Significant at the 0.05 level.
Estimated in multivariate robust Poisson regression models102 with dummy variable controls for the separate waves within the time intervals. The time intervals were as follows: (1) 8 waves between April 23 and June 23, 2020; (2) 4 waves between June 25 and July 21; (3) 5 waves between August 19 and October 26; (4) 5 waves between October 28 and February 1,2021; (5) 4 waves between February 3 and March 29; (6) 6 waves between April 14 and July 5,2021. Time intervals were selected by inspection of consistency and changes in prevalence across waves.
Controlled by weeks 1.0 within variables within time period.
An even stronger consistency over time can be seen in the association between education and PHQ-4 scores. The total sample association is significant (χ2 3 = 1900.8, P<.001) based on a monotonically decreasing prevalence from 34.2% at the lowest level (less than high school) to a low of 22.2% at the highest level (college graduate) and intermediate prevalence of 28.3% to 29.7% in the 2 middle categories (high school graduate, some college). In the adjusted model, centered RR was 1.2 to 1.3 among those with lowest education, RR = 0.7 to 0.8 among those with highest education, and RR = 1.0 to 1.1 among those with intermediate education. A significant association of race ethnicity with PHQ-4 scores, finally, was found in the total sample (χ2 3 = 331.3, P<.001), with highest prevalence among Hispanic individuals (30.3%), lowest among non-Hispanic white individuals (24.8%), and intermediate among non-Hispanic black individuals (29.3%) and other races (28.8%). However, this association decreased dramatically in magnitude in the multivariate model that adjusted for age, sex, and education model (χ2 3 = 11.6, P = .009) resulting in the centered RR becoming nonsignificantly different from the total sample average in only 1 of the 6 intervals each among Hispanic individuals (RR = 0.95) and other races (RR = 1.1), none of the 6 among non-Hispanic black individuals, and 2 of the 6 among non-Hispanic white individuals (RR = 0.95–0.97).
Taken as a whole, these results suggest that mental health disparities based on sex, age, education, and race ethnicity have not changed substantially as of this stage in the pandemic despite the clear evidence that disadvantaged segments of society have been more highly exposed than others to pandemic-related stressors. Whether this is due to a greater resilience among disadvantaged segments of the population is unclear from the simple analyses reported here. More nuanced analysis would be needed to investigate this issue directly by estimating interactions between individual-level exposure to pandemic-related stressors and disadvantaged social status to predict subsequent onset of worsening of anxiety-depression. This kind of analysis is beyond the scope of the current review but could be carried out in the UAS cohort, although the much lower estimated prevalence of anxiety-depression in the UAS than the other 2 major tracking surveys might undercut the persuasiveness of the results.
Another possibility is that the associations of disadvantaged social status with anxiety-depression are more complex than in the simple additive model considered here. For example, there might be important interactions among the indicators of disadvantage, or there might be important geographic variation in these associations. Consistent with the latter, a study carried out in the early months of the pandemic with HPS data showed that the associations of COVID-19-related financial stressors with anxiety-depression were dampened in states with supportive policies for dealing with reduced income (Medicaid, unemployment insurance, restrictions on landlord and utility company responses to nonpayment).125 Based on this result, it is plausible to think that more disaggregated analyses might show evidence of significant time-space variation in health disparities throughout the pandemic.
Finally, it is important to recognize that we examined RR rather than absolute-risk difference. This means that prevalence of clinically significant anxiety-depression across the segments of the population considered here has not changed proportionally over the pandemic, but absolute differences would increase as overall prevalence increased if overall prevalence increased during the pandemic. The same observation was made by Swaziek and Wozniak122 in an analysis comparing early waves of the HPS data with the BRFSS data.
Predicting future changes in mental disorder prevalence and disparities
If anything about the data reviewed here is clear, it is that the impact of COVID-19 on mental disorders is challenging to document. This is even truer for forecasting future effects of the pandemic on population mental health. There are some promising signs in the expansion of tele-mental health care to reach hard-to-reach people in need of care and the increased use of scalable interventions to address the rising demand for treatment of emotional problems during the pandemic. However, there are also enormous uncertainties. We noted in the previous section that the effects of some pandemic-related stressors have so far been buffered by government policies, but uncertainties exist about the long-term sustainability of these policies.126 Indeed, the Supreme Court recently ended the Biden administration’s eviction moratorium in the same week that the government announced the US inflation rate hit a 30-year high.127
In addition, uncertainties exist about the duration of the pandemic, with its ever-increasing number of variants, the long-term prognosis of the 10% to 30% of COVID-19 survivors128 who experience the post-COVID-19 syndrome now referred to as PASC (postacute sequelae of COVID),129 and the extent to which COVID-19 infection will have long-term neuropsychiatric effects.130 We know from research on prior infectious disease outbreaks and other natural disasters that prolongation of the physical threat phase,131 as is occurring in the evolving COVID-19 pandemic, along with the proliferation of secondary financial stressors we are experiencing can create what has been referred to as a “second disaster” with more severe negative effects on mental health than the original disaster.132 That these events are occurring in the fractious political environment in which we are now living only compounds the problem. The implications of this confluence of factors for population mental health are likely to be substantial, at least in the short term, and especially so for the more economically disadvantaged segment of society.
Acknowledgments
The authors appreciate the helpful comments of Alan Kazdin, Roy Perlis, Michael Schoenbaum, and Jose Zubizarreta on an earlier version of the paper. We appreciate being given access to data from surveys administered by the Understanding America Study, which is maintained by the Center for Economic and Social Research (CESR) at the University of Southern California and is supported in part by the Bill & Melinda Gates Foundation and by grant U01AG054580 from the National Institute on Aging. The authors also appreciate access to public use microdata files from the CDC Household Pulse Survey and CDC Behavioral Risk Factor Surveillance Survey. We thank Roy Perlis for providing us with summary data from the COVID States Project for use in Fig. 1. The COVID States Project is a joint project of Northeastern University, Harvard University, Rutgers University, and Northwestern University and is supported by the National Science Foundation under grants SES-2029292 and SES-2029792 and is also supported by a grant from the Knight Foundation, the Russell Sage Foundation, and the Peter G. Peterson Foundation. Their data collection was also supported in part by Amazon. Any opinions, findings, and conclusions or recommendations expressed herein are those of the authors and do not necessarily reflect the views of the principals or funders of these surveys.
Disclosure
In the past 3 years, Dr R.C. Kessler was a consultant for Datastat, Inc, Holmusk, RallyPoint Networks, Inc, and Sage Therapeutics. He has stock options in Mirah, PYM, and Roga Sciences. The other authors report no conflicts.
Supplementary data
▪.
References
- 1.Center for Disease Control and Prevention COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home Available at: Accessed August 6, 2021.
- 2.David K.B., Aborode A.T., Olaoye D.Q., et al. Increased risk of death triggered by domestic violence, hunger, suicide, exhausted health system during COVID-19 pandemic: why, how and solutions. Front Sociol. 2021;6:648395. doi: 10.3389/fsoc.2021.648395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falk G., Romero P.D., Carter J.A., et al. Unemployment rates during the COVID-19 pandemic. https://fas.org/sgp/crs/misc/R46554.pdf Available at: Accessed August 7, 2021.
- 4.Amadeo K. What is long-term unemployment? https://www.thebalance.com/long-term-unemployment-what-it-is-causes-and-effects-3305518 Available at: Accessed August 11, 2021.
- 5.U.S. Bureau of Labor Statistics Unemployed 27 weeks or longer as a percent of total unemployed. https://www.bls.gov/charts/employment-situation/unemployed-27-weeks-or-longer-as-a-percent-of-total-unemployed.htm Available at: Accessed August 7, 2021.
- 6.Center on Budget and Policy Priorities. Tracking the COVID-19 economy’s effects on food, housing, and employment hardships. https://www.cbpp.org/sites/default/files/atoms/files/8-13-20pov.pdf Available at: Accessed August 5, 2021.
- 7.Dimock M., Gramlich J. How America changed during Donald Trump's presidency. https://www.pewresearch.org/2021/01/29/how-america-changed-during-donald-trumps-presidency/ Available at: Accessed August 5, 2021.
- 8.Iacoella F., Justino P., Martorano B. Do pandemics lead to rebellion? Policy responses to COVID-19, inequality, and protests in the USA. https://www.wider.unu.edu/sites/default/files/Publications/Working-paper/PDF/wp2021-57-pandemics-rebellion-policy-responses-COVID-19-inequality-protests-USA.pdf Available at: Accessed August 6, 2021.
- 9.Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 10.Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N Engl J Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- 11.Cavicchioli M., Ferrucci R., Guidetti M., et al. What will be the impact of the Covid-19 quarantine on psychological distress? Considerations based on a systematic review of pandemic outbreaks. Healthcare (Basel). 2021;9(1) doi: 10.3390/healthcare9010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chu I.Y., Alam P., Larson H.J., et al. Social consequences of mass quarantine during epidemics: a systematic review with implications for the COVID-19 response. J Trav Med. 2020;27(7) doi: 10.1093/jtm/taaa192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah K., Kamrai D., Mekala H., et al. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12(3):e7405. doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldmann E., Galea S. Mental health consequences of disasters. Annu Rev Public Health. 2014;35(1):169–183. doi: 10.1146/annurev-publhealth-032013-182435. [DOI] [PubMed] [Google Scholar]
- 15.Paul K., Moser K. Unemployment impairs mental health: meta-analysis. J Vocat Behav. 2009;74:264–282. [Google Scholar]
- 16.Thimm J.C., Kristoffersen A.E., Ringberg U. The prevalence of severe grief reactions after bereavement and their associations with mental health, physical health, and health service utilization: a population-based study. Eur J Psychotraumatol. 2020;11(1):1844440. doi: 10.1080/20008198.2020.1844440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J., Lloyd-Evans B., Giacco D., et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2017;52(12):1451–1461. doi: 10.1007/s00127-017-1446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galea S., Brewin C.R., Gruber M., et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Majid U., Hussain S.A.S., Wasim A., et al. A systematic map of non-clinical evidence syntheses published globally on COVID-19. Disaster Med Public Health Prep. 2021:1–19. doi: 10.1017/dmp.2021.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen P.J., Pusica Y., Sohaei D., et al. An overview of mental health during the COVID-19 pandemic. Diagnosis (Berl) 2021;8(4):403–412. doi: 10.1515/dx-2021-0046. [DOI] [PubMed] [Google Scholar]
- 21.Phiri P., Ramakrishnan R., Rathod S., et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. doi: 10.1016/j.eclinm.2021.100806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodríguez-Fernández P., González-Santos J., Santamaría-Peláez M., et al. Psychological effects of home confinement and social distancing derived from COVID-19 in the general population–a systematic review. Int J Environ Res Public Health. 2021;18(12) doi: 10.3390/ijerph18126528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Twenge J.M., Joiner T.E. Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol. 2020;76(12):2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lucid Holdings L.L.C. Academic research with Lucid. https://luc.id/academic-solutions/ Available at: Accessed August 6, 2021.
- 25.Kessler R.C., Barker P.R., Colpe L.J., et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 26.National Center for Health Statistics National health interview survey. https://www.cdc.gov/nchs/nhis/index.htm Available at: Accessed August 6, 2021.
- 27.American Association for Public Opinion Research AAPOR report on online panels. https://www.aapor.org/Education-Resources/Reports/Report-on-Online-Panels Available at: Accessed August 8, 2021.
- 28.Czeisler M., Lane R.I., Petrosky E., et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daly M., Sutin A.R., Robinson E. Depression reported by US adults in 2017-2018 and March and April 2020. J Affect Disord. 2021;278:131–135. doi: 10.1016/j.jad.2020.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ettman C.K., Abdalla S.M., Cohen G.H., et al. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGinty E.E., Presskreischer R., Han H., et al. Psychological distress and loneliness reported by US adults in 2018 and april 2020. JAMA. 2020;324(1):93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang S., Kim J.K., Song R. Doubly robust inference when combining probability and non-probability samples with high dimensional data. J R Stat Soc Ser B Stat Methodol. 2020;82(2):445–465. doi: 10.1111/rssb.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.United States Census Bureau Measuring household experiences during the Coronavirus pandemic. https://www.census.gov/data/experimental-data-products/household-pulse-survey.html Available at: Accessed August 8, 2021.
- 34.Kroenke K., Spitzer R.L., Williams J.B., et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 35.National Center for Chronic Disease Prevention and Health Promotion DoPH Behavioral risk factor surveillance system. https://www.cdc.gov/brfss/index.html Available at: Accessed August 8, 2021.
- 36.Twenge J.M., McAllister C., Joiner T.E. Anxiety and depressive symptoms in U.S. Census Bureau assessments of adults: trends from 2019 to fall 2020 across demographic groups. J Anxiety Disord. 2021;83:102455. doi: 10.1016/j.janxdis.2021.102455. [DOI] [PubMed] [Google Scholar]
- 37.United States Census Bureau Experimental data products. https://www.census.gov/data/experimental-data-products.html Available at: Accessed August 7, 2021.
- 38.United States Census Bureau Household pulse survey technical documentation. https://www.census.gov/programs-surveys/household-pulse-survey/technical-documentation.html Available at: Accessed August 8, 2021.
- 39.Peterson S., Toribio N., Farber J., et al. Nonresponse bias report for the 2020 Household Pulse Survey. https://www2.census.gov/programs-surveys/demo/technical-documentation/hhp/2020_HPS_NR_Bias_Report-final.pdf Available at: Accessed August 8, 2021.
- 40.He C. The Depressd project: changes in mental health symptoms. https://www.depressd.ca/research-question-1-symptom-changes Available at: Accessed August 8, 2021.
- 41.Sun Y., Wu Y., Bonardi O., et al. Comparison of mental health symptoms prior to and during COVID-19: evidence from a living systematic review and meta-analysis. medRxiv. 2021:21256920. doi: 10.1101/2021.05.10.21256920. [DOI] [Google Scholar]
- 42.Institute for Social and Economic Research (ISER) Understanding society: the UK household longitudinal study. https://www.understandingsociety.ac.uk/ Available at: Accessed August 7, 2021.
- 43.Pevalin D.J. Multiple applications of the GHQ-12 in a general population sample: an investigation of long-term retest effects. Soc Psychiatry Psychiatr Epidemiol. 2000;35(11):508–512. doi: 10.1007/s001270050272. [DOI] [PubMed] [Google Scholar]
- 44.Pierce M., Hope H., Ford T., et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/s2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Daly M., Robinson E. Longitudinal changes in psychological distress in the UK from 2019 to September 2020 during the COVID-19 pandemic: evidence from a large nationally representative study. Psychiatry Res. 2021;300:113920. doi: 10.1016/j.psychres.2021.113920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kessler R.C., Ustün T.B. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) composite international diagnostic interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Knudsen A.K.S., Stene-Larsen K., Gustavson K., et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg Health - Europe. 2021;4:100071. doi: 10.1016/j.lanepe.2021.100071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murad M.H., Wang Z., Chu H., et al. When continuous outcomes are measured using different scales: guide for meta-analysis and interpretation. BMJ. 2019;364:k4817. doi: 10.1136/bmj.k4817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.RAND Corporation. RAND American Life Panel (ALP) https://www.rand.org/research/data/alp.html Available at: Accessed August 8, 2021.
- 50.Kessler R.C., Green J.G., Gruber M.J., et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(Suppl 1):4–22. doi: 10.1002/mpr.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Breslau J., Finucane M.L., Locker A.R., et al. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med. 2021;143:106362. doi: 10.1016/j.ypmed.2020.106362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gutsche T.L., Kapteyn A., Meijer E., et al. The RAND continuous 2012 presidential election poll. Public Opin Q. 2014;78:233–254. [Google Scholar]
- 53.National Center for Health Statistics National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm Available at: Accessed August 8, 2021.
- 54.Gallup News Service Gallup Poll social series: health and healthcare. https://news.gallup.com/poll/327311/americans-mental-health-ratings-sink-new-low.aspx Available at: Accessed August 10, 2021.
- 55.Brenan M. Americans' mental health ratings sink to new low. https://news.gallup.com/poll/327311/americans-mental-health-ratings-sink-new-low.aspx Available at: Accessed August 8, 2021.
- 56.Hartnett K.P., Kite-Powell A., DeVies J., et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Adjemian J., Hartnett K.P., Kite-Powell A., et al. Update: COVID-19 pandemic-associated changes in emergency department visits - United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70(15):552–556. doi: 10.15585/mmwr.mm7015a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bhambhvani H.P., Rodrigues A.J., Yu J.S., et al. Hospital volumes of 5 medical emergencies in the COVID-19 pandemic in 2 US medical centers. JAMA Intern Med. 2021;181(2):272–274. doi: 10.1001/jamainternmed.2020.3982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lange S.J., Ritchey M.D., Goodman A.B., et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(25):795–800. doi: 10.15585/mmwr.mm6925e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Holland K.M., Jones C., Vivolo-Kantor A.M., et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(4):372–379. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pathak E.B., Garcia R.B., Menard J.M., et al. Out-of-hospital COVID-19 deaths: consequences for quality of medical care and accuracy of cause of death coding. Am J Public Health. 2021;111(S2):S101–S106. doi: 10.2105/AJPH.2021.306428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schoenbaum M., Colpe L. Challenges to behavioral health and injury surveillance during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(8):924–925. doi: 10.1001/jamapsychiatry.2021.1201. [DOI] [PubMed] [Google Scholar]
- 63.Orthopoulos G., Santone E., Izzo F., et al. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg. 2021;221(5):1056–1060. doi: 10.1016/j.amjsurg.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yard E., Radhakrishnan L., Ballesteros M.F., et al. Emergency department visits for suspected suicide attempts among persons aged 12-25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021;70(24):888–894. doi: 10.15585/mmwr.mm7024e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Friedman J., Mann N.C., Hansen H., et al. Racial/ethnic, social, and geographic trends in overdose-associated cardiac arrests observed by US Emergency Medical Services during the COVID-19 pandemic. JAMA Psychiatry. 2021;78(8):886–895. doi: 10.1001/jamapsychiatry.2021.0967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ahmad F.B., Cisewski J.A., Miniño A., et al. Provisional mortality data - United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(14):519–522. doi: 10.15585/mmwr.mm7014e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.National Center for Health Statistics Instructions for classification of underlying and multiple causes of death. https://www.cdc.gov/nchs/nvss/manuals/2a-2021.htm Available at: Accessed August 19, 2021.
- 68.Ahmad F.B., Anderson R.N. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gupta S., Hayek S.S., Wang W., et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020;180(11):1436–1447. doi: 10.1001/jamainternmed.2020.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pirkis J., John A., Shin S., et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8(7):579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Leaune E., Samuel M., Oh H., et al. Suicidal behaviors and ideation during emerging viral disease outbreaks before the COVID-19 pandemic: a systematic rapid review. Prev Med. 2020;141:106264. doi: 10.1016/j.ypmed.2020.106264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021;5(2):229–238. doi: 10.1038/s41562-020-01042-z. [DOI] [PubMed] [Google Scholar]
- 73.Faust J.S., Du C., Mayes K.D., et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, march-august 2020. JAMA. 2021;326(1):84–86. doi: 10.1001/jama.2021.8012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ahmad FB, Cisewski JA. Quarterly provisional estimates for selected indicators of mortality, 2019-Quarter 1, 2021. Available at: Available at: https://www.cdc.gov/nchs/nvss/vsrr/mortality-dashboard.htm. Accessed August 10, 2021.
- 75.Statista. Percentage of homicides by firearm in the United States from 2006 to 2019. https://www.statista.com/statistics/249783/percentage-of-homicides-by-firearm-in-the-united-states/ Available at: Accessed August 8, 2021.
- 76.Levine P., McKnight R. Three million more guns: the Spring 2020 spike in firearm sales. https://www.brookings.edu/blog/up-front/2020/07/13/three-million-more-guns-the-spring-2020-spike-in-firearm-sales/ Available at: Accessed August 20, 2021.
- 77.Schleimer J.P., McCort C.D., Shev A.B., et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a cross-sectional study. Inj Epidemiol. 2021;8(1):43. doi: 10.1186/s40621-021-00339-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahmad F.B., Rossen L., Sutton P. National Center for Health Statistics; 2021. Provisional drug overdose death counts. [Google Scholar]
- 79.Wilson N., Kariisa M., Seth P., et al. Drug and opioid-involved overdose deaths — United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69:290–297. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.CDC Health Alert Network Emergency preparedness and response. https://emergency.cdc.gov/han/2020/han00438.asp Available at: Accessed August 19, 2021.
- 81.Levine P.B., McKnight R. Firearms and accidental deaths: evidence from the aftermath of the Sandy Hook school shooting. Science. 2017;358(6368):1324–1328. doi: 10.1126/science.aan8179. [DOI] [PubMed] [Google Scholar]
- 82.Cohen J.S., Donnelly K., Patel S.J., et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148(1) doi: 10.1542/peds.2020-042697. e2020042697. [DOI] [PubMed] [Google Scholar]
- 83.National Safety Council Motor vehicle deaths in 2020 estimated to be highest in 13 years, despite dramatic drops in miles driven. https://www.nsc.org/newsroom/motor-vehicle-deaths-2020-estimated-to-be-highest Available at: Accessed October 2, 2021.
- 84.National Highway Traffic Safety Administration’s National Center for Statistics and Analysis Early estimate of motor vehicle traffic fatalities in 2020. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/813115 Available at: Accessed October 2, 2021.
- 85.Hirt S. As calls to crisis hotlines spike amid the coronavirus, those who respond feel the strain. https://www.usatoday.com/story/news/2020/06/15/crisis-hotline-call-volume-spikes-straining-social-workers/5266072002/ Available at: Accessed August 20, 2021.
- 86.Cooke K., Pell M., Lesser B. As school activity shut down amid COVID, 911 drug calls for youth skyrocketed. https://www.reuters.com/investigates/special-report/health-coronavirus-trauma/ Available at: Accessed August 19, 2020.
- 87.The National Suicide Prevention Lifeline. About the Lifeline. https://suicidepreventionlifeline.org/about/ Available at: Accessed August 20, 2021.
- 88.Tjeltveit A. COVID-19 and the National Suicide Prevention Lifeline. https://storymaps.arcgis.com/stories/063fbdbfb7c743b78e56abf79fc284b9 Available at:
- 89.Lersch K.M. COVID-19 and mental health: an examination of 911 calls for service. Policing: A J Policy Pract. 2020 doi: 10.1093/police/paaa049. paaa049. [DOI] [Google Scholar]
- 90.National Association of Emergency Medical Technicians How COVID-19 has impacted our nation's EMS agencies. https://www.naemt.org/docs/default-source/covid-19/covid-impact-survey-06-03-2021.pdf?sfvrsn=c62fea93_4 Available at: Accessed August 20, 2021.
- 91.Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38(12):2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.McCrary J., Sanga S. The impact of the coronavirus lockdown on domestic violence. Am L Econ Rev. 2021;23(1):137–163. [Google Scholar]
- 93.National Domestic Violence Hotline A snapshot of domestic violence during COVID-19. https://www.thehotline.org/resources/a-snapshot-of-domestic-violence-during-covid-19/ Available at: Accessed August 20, 2021.
- 94.Ta M., Collins H., Neal S., et al. Domestic violence patterns in King County, WA: March – August 2020. https://kingcounty.gov/depts/health/covid-19/∼/media/depts/health/communicable-diseases/documents/C19/domestic-violence-patterns-in-king-county.ashx Available at: Accessed August 19, 2020.
- 95.Krueger A.B., Mueller A.I. The lot of the unemployed: a time use perspective. J Eur Econ Assoc. 2012;10(4):765–794. [Google Scholar]
- 96.Fernández-Alcántara M., Kokou-Kpolou C.K., Cruz-Quintana F., et al. Editorial: New perspectives in bereavement and loss: complicated and disenfranchised grief along the life cycle. Front Psychol. 2021;12:691464. doi: 10.3389/fpsyg.2021.691464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Erzen E., Ö Çikrikci. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry. 2018;64(5):427–435. doi: 10.1177/0020764018776349. [DOI] [PubMed] [Google Scholar]
- 98.Mortazavi S.S., Assari S., Alimohamadi A., et al. Fear, loss, social isolation, and incomplete grief due to COVID-19: a recipe for a psychiatric pandemic. Basic Clin Neurosci. 2020;11(2):225–232. doi: 10.32598/bcn.11.covid19.2549.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Center on Budget and Policy Priorities. Tracking the COVID-19 recession’s effects on food, housing, and employment hardships. https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and Available at: Accessed August 20, 2021.
- 100.Gould E., Kassa M. Young workers hit hard by the COVID-19 economy: workers ages 16–24 face high unemployment and an uncertain future. https://files.epi.org/pdf/203139.pdf Available at: Accessed August 19, 2020.
- 101.Saban M., Myers V., Luxenburg O., et al. Tipping the scales: a theoretical model to describe the differential effects of the COVID-19 pandemic on mortality. Int J Equity Health. 2021;20(1):140. doi: 10.1186/s12939-021-01470-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chen W., Qian L., Shi J., et al. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18(1):63. doi: 10.1186/s12874-018-0519-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Han H., Anderson K., Barry C.L., et al. The Johns Hopkins COVID-19 Civic Life and Public Health Survey. https://snfagora.jhu.edu/project/the-johns-hopkins-covid-19-civic-life-and-public-health-survey/ Available at: Accessed August 19, 2021.
- 104.The Data Foundation Improving government and society by using data to inform public policymaking. https://www.datafoundation.org/ Available at: Accessed August 19, 2021.
- 105.Pew Research Center About Pew Research center. https://www.pewresearch.org/about/ Available at: Accessed August 22, 2021.
- 106.Czeisler M.É., Howard M.E., Czeisler C.A., et al. The COPE Initiative: findings. https://www.thecopeinitiative.org/findings Available at: Accessed August 20, 2021.
- 107.Lazer D., Baum M.A., Ognyanova K., et al. The state of the nation: a 50-state COVID-19 survey. https://covidstates.org/ Available at: Accessed August 20, 2021.
- 108.The University of Southern California Welcome to the Understanding America Study. https://uasdata.usc.edu/index.php Available at: Accessed August 19, 2020.
- 109.The University of Southern California Understanding Coronavirus in America. https://covid19pulse.usc.edu/ Available at: Accessed August 19, 2020.
- 110.Czeisler M.É., Wiley J.F., Czeisler C.A., et al. Tempering optimism from repeated longitudinal mental health surveys. Lancet Psychiatry. 2021;8(4):274–275. doi: 10.1016/S2215-0366(21)00045-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Staff A.J.M.C. What we're reading: U.S. declares coronavirus a public health emergency; FDA approves peanut allergy drug; California healthcare tax rejected. https://www.ajmc.com/view/what-were-reading-us-declares-coronavirus-a-public-health-emergency-fda-approves-peanut-allergy-drug-california-healthcare-tax-rejected Available at: Accessed August 22, 2021.
- 112.Staff A.J.M.C. What we’re reading: U.S. records 100,000 COVID-19 cases; FDA staff support Alzheimer drug; CDC director urges asymptomatic testing. https://www.ajmc.com/view/what-we-re-reading-us-records-100-000-covid-19-cases-fda-staff-support-alzheimer-drug-cdc-director-urges-asymptomatic-testing Available at: Accessed August 22, 2021.
- 113.Center for Disease Control and Prevention Trends in number of COVID-19 cases and deaths in the U.S. reported to CDC, by state/territory. https://covid.cdc.gov/covid-data-tracker/#trends_dailycases Available at: Accessed August 22, 2021.
- 114.Center for Disease Control and Prevention Variant proportions. https://covid.cdc.gov/covid-data-tracker/#monitoring-varaint-heading Available at: Accessed August 21, 2021.
- 115.Chakrabarti S., Hamlet L.C., Kaminsky J., et al. Association of human mobility restrictions and race/ethnicity-based, sex-based, and income-based factors with inequities in well-being during the COVID-19 pandemic in the United States. JAMA Netw Open. 2021;4(4):e217373. doi: 10.1001/jamanetworkopen.2021.7373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Thomas K., Darling J., Cassil A. U.S. pandemic Misery Index tracks COVID-19 hardships no. 3, May 2021. https://uasdata.usc.edu/index.php Available at: Accessed August 20, 2021.
- 117.Daly M., Robinson E. Acute and longer-term psychological distress associated with testing positive for COVID-19: longitudinal evidence from a population-based study of US adults. Psychol Med. 2021:1–8. doi: 10.1017/S003329172100324X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Holman E.A., Thompson R.R., Garfin D.R., et al. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the United States. Sci Adv. 2020;6(42) doi: 10.1126/sciadv.abd5390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pai N., Vella S.L. COVID-19 and loneliness: a rapid systematic review. Aust N Z J Psychiatry. 2021 doi: 10.1177/00048674211031489. 48674211031489. [DOI] [PubMed] [Google Scholar]
- 120.Perlis R.H., Ognyanova K., Santillana M., et al. Association of acute symptoms of COVID-19 and symptoms of depression in adults. JAMA Netw Open. 2021;4(3):e213223. doi: 10.1001/jamanetworkopen.2021.3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Robinson E., Daly M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: longitudinal evidence from the Understanding America Study. Br J Health Psychol. 2021;26(2):570–587. doi: 10.1111/bjhp.12493. [DOI] [PubMed] [Google Scholar]
- 122.Swaziek Z., Wozniak A. Disparities old and new in US mental health during the COVID-19 pandemic. Fisc Stud. 2020;41(3):709–732. doi: 10.1111/1475-5890.12244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kessler R.C., Heeringa S., Lakoma M.D., et al. Individual and societal effects of mental disorders on earnings in the United States: results from the national comorbidity survey replication. Am J Psychiatry. 2008;165(6):703–711. doi: 10.1176/appi.ajp.2008.08010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Taquet M., Luciano S., Geddes J.R., et al. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Donnelly R., Farina M.P. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Soc Sci Med. 2021;269:113557. doi: 10.1016/j.socscimed.2020.113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rigby E. The COVID-19 economy, unemployment insurance, and population health. JAMA Netw Open. 2021;4(1):e2035955. doi: 10.1001/jamanetworkopen.2020.35955. [DOI] [PubMed] [Google Scholar]
- 127.Bartash J. Inflation rate hits 30-year high, PCE shows, as U.S. confronts major shortages. https://www.marketwatch.com/story/inflation-rate-hits-30-year-high-pce-shows-as-u-s-confronts-major-shortages-11630068319 Available at: Accessed August 22, 2021.
- 128.Moghimi N., Di Napoli M., Biller J., et al. The neurological manifestations of post-acute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021;21(9):44. doi: 10.1007/s11910-021-01130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lerner A.M., Robinson D.A., Yang L., et al. Toward understanding COVID-19 recovery: National Institutes of Health workshop on postacute COVID-19. Ann Intern Med. 2021;174(7):999–1003. doi: 10.7326/M21-1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kumar S., Veldhuis A., Malhotra T. Neuropsychiatric and cognitive sequelae of COVID-19. Front Psychol. 2021;12(553) doi: 10.3389/fpsyg.2021.577529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Raphael B. Basic Books; New York: 1986. When disaster strikes: how individuals and communities cope with catastrophe. [Google Scholar]
- 132.Gersons B.P.R., Smid G.E., Smit A.S., et al. Can a 'second disaster' during and after the COVID-19 pandemic be mitigated? Eur J Psychotraumatol. 2020;11(1):1815283. doi: 10.1080/20008198.2020.1815283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
▪.