Abstract
Objective:
to examine the geographic distribution of gynecologic oncologists (GO) and assess if the GO workforce is meeting the demand for oncology services for patients with gynecologic cancers.
Methods:
We identified GO by National Provider Identifiers (NPI) and calculated county-level density of GO. County-level gynecologic cancer rates were derived from the U.S. Cancer Statistics to represent demand for GO services. A spatial data plot compared GO workforce to gynecologic cancer service demand. U.S. census county-level demographic information was collected and compared.
Results:
In 2019, 1,527 GO had a registered NPI. Of 3,142 counties in the US, 2,864 (91.2%) counties had no GO in their local county and 1,943 (61.8%) counties had no GO in local or adjacent (neighboring) counties. As the gynecologic cancer rate increases (described in quintiles) in counties, there are fewer counties without a GO or adjacent GO. However, county-level GO density (number of GO per 100,000 women) did not significantly increase as the county-level incidence of gynecologic cancer increased (r=−0.12, p=0.06)... Women living in counties with the highest gynecologic cancer rates and without access to a GO were more likely to reside in a rural area where residents had a lower median income and were predominately of White race..
Conclusion:
There are a significant number of counties in the U.S. without a GO. As county-level gynecologic cancer incidence increased, the proportion of counties without a GO decreased; GO density did not increase with increasing cancer rates. Rural counties with high gynecologic incidence rates are underserved by GO. This information can inform initiatives to improve outreach and collaboration to better meet the needs of patients in different geographic areas.
Introduction
In 2006 the American Society for Clinical Oncology (ASCO) reported that there would be a significant shortage of oncologists to serve the growing United States cancer population (1). While the supply of oncology services was expected to grow by 40% by 2025, the supply of oncologists was expected to grow by only 25%, resulting in a shortage of over 2,200 oncologists (2). In a study examining the current oncology workforce, Shih et al. reported that 16% of counties in the US did not have access to an oncologist in their local or adjacent counties, with even less oncology workforce noted in some counties burdened by the highest cancer incidences (3). While this study looked at the entire oncology population and included gynecologic oncologists in the oncology workforce, its conclusions apply to the general oncology population.
Access to high quality, high-volume specialty providers is important in the care of women with gynecologic cancer and has been shown to result in improved treatment and survival outcomes (4, 5). Over 116,000 women are expected to be diagnosed with gynecologic cancer in 2021 and will require treatment and follow-up care with a gynecologic oncologist (6, 7). This population represents 12.6% of all women’s cancers and 6.2% of all US cancers, yet among the oncology workforce, gynecologic oncologists represent roughly 5% of all oncologists (3, 6, 8).
There is only limited information on the adequacy and geographic distribution of the gynecologic oncologist workforce in the U.S. For example, in a previous population-based study, Shalowitz et al. reported that around 10% of the US female population did not have access to a gynecologic oncologist less than 50 miles from their home county (9). Multiple studies in gynecologic cancer have documented the association between geographic barriers to access and worse treatment outcomes (including survival) in patients with cervical, endometrial, and ovarian cancer (10–12). However, no previous study has examined the geographic density of the gynecologic oncologist (GO) workforce and the relationship of GO density to the distribution of gynecologic cancer incidence. The primary objective of this study was to assess the geographic distribution and density of gynecologic oncologist overall and compared to gynecologic cancer incidence rates. We sought to assess whether the distribution of the GO workforce matches the geographic demand for cancer care for patients with gynecologic cancers. This analysis will help identify geographic areas that may benefit from future efforts to increase supply and access. Our secondary objective was to characterize census-reported socioeconomic factors in counties that do not have a gynecologic oncologist.
1. Methods
1.1. Provider Data
Individual physician information was obtained from the Full Replacement Monthly National Provider Identifier (NPI) data downloaded from the Centers for Medicare and Medicaid Services (CMS) National Plan and Provider Enumeration System (NPPES) downloadable file (13). This data set is publicly available and contains information on specialty and practice characteristics (including geographic location) for any physician enrolled in billable claims to public and private insurance. Participating providers are required by law (NPI Final Rule 45 CFR 162.410) to update practice location data within 30 days of practice changes (including address, specialty). The data for each NPI number included enumeration date (first date registered with CMS), last updated date, healthcare provider taxonomy code (207VX0201X for gynecologic oncology), sex of provider, solo proprietor status, and geographic information of practice location including zip code, address, state, and country. All NPIs with a gynecologic oncology taxonomy code in the 50 United States and DC were included. The study sample was extracted from the NPPES website on October 1, 2019 and details regarding the data file are outlined in methods described in Shih et al (3). A previous study examining the reliability of the NPPES file found that NPI information reported in the NPPES was a good representation of the physician workforce. This study randomly sampled 1,200 NPIs in NPPES and found that 72–94% of NPI information found in the dataset was accurate (14).
For each NPI, provider practice addresses were geo-coded for county information using OpenCage Geocoder (2013–2021 OpenCage GmbH) (15). To quantify the density of GO workforce at the county level, the total number of gynecologic oncologists in each county were summated and converted to gynecologic oncologists per 100,000 women by linking county codes to 2019 county-level US Census bureau data (16). We used the 2010 census county adjacent file to determine the presence of gynecologic oncologists in adjacent counties, which is defined as any county neighboring to or with a physical border with the local county (15).
1.2. Cancer Incidence Data
County-level gynecologic cancer incidence was determined to interpret the oncology workforce data with respect to oncology service demands. Data for cancer incidence was identified in the United States Cancer Statistics (USCS) registry, which includes data from the two federally funded population-based sources of cancer cases in the United States, the Centers for Disease Control and Prevention’s (CDC’s) National Program of Cancer Registries (NPCR) and the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program. Data on county-level crude (i.e., not age-adjusted) cancer incidence are available for the all the states except Minnesota and Kansas. For Kansas, county-level cancer crude numbers were extracted from the Kansas Cancer Registry website and cancer crude rates per 100,000 women were calculated (17). Gynecologic cancer data were not available for Minnesota as the state only publicly reports data on the top 20 most common cancers in Minnesota, which do not include the three gynecologic cancers. Therefore, Minnesota was not included in reporting of gynecologic cancer rates. County-level cancer rates per 100,000 women for gynecologic cancer groups (Cervix, Ovary, and Uterine) were derived and compiled from the 2020 report of 2013– 2017 cancer incidence from the United States (18). Rates were suppressed for counties with less than 16 cases and therefore counties meeting this criterion were grouped into the lowest incidence category.
1.3. County-level census data
Using the 2019 U.S. Census bureau data, publicly-available county-level data on female race, Hispanic ethnicity, median income and classification of a county belonging to either a metro or non-metro area (based on the 2013 Metropolitan Area delineation set by the census bureau) was extracted (19, 20).
1.4. Analysis
Density of Gynecologic Oncologists
Descriptive statistics were performed on the characteristics of physicians with NPIs registered as gynecologic oncologists. We then identified counties without an active GO NPI and documented counties without an active GO NPI in the local or adjacent counties.
Incidence of Gynecologic Cancers
County-level gynecologic cancer (combined cervix, ovary, and uterine) incidence rates (per 100,000 women) were categorized into four categories by rates: those with < 16 cases representing the 1st and 2nd quintile (combined 38.2% of data) with the remaining three quintiles representing the remaining county gynecologic cancer rates (ranges 3rd: 16 to 42.0 cases/100,000, 4th: 42.1 to 54.7 cases/100,000, and 5th: 54.8 to 111.5 cases/100,000). County-level uterine cancer incidence rates were also categorized into four categories. In the cervical and ovarian cancer subsets, over 50% of counties were noted to have suppressed values for incidence rates; therefore, these two cancers were each divided into three groups. The largest group represents counties with < 16 cases per 100,000 women, and the remaining counties were divided into two groups by crude rates to represent the middle and high cancer rate groups. These categories were color-coded for each county and the density of oncologists per county was represented as a dot map overlaid on the crude gynecologic cancer rate map. Data for cancer rates for the 87 counties in Minnesota were treated as missing data. Given the disparity-driven rate of cervical and uterine cancer, three cancer-specific maps were created to observe differences between the cancer types. Individual maps for cervix, ovary, and uterine cancers were created using the same format as the previous map except that cancer rates were cancer-specific crude rates, respectively. Lastly, a map was created using overall gynecologic cancer crude rates as previously described and overlaying dots to mark counties with no access to a GO in a local county and the adjacent counties. In the graphical presentation of GO density at county level, larger dots represented a higher density of oncologists.
Comparison of Gynecologic Oncologist Density and Gynecologic Cancer Incidence
GO density, gynecologic cancer incidence rates, and census-reported demographics for the overall group and between-group quintiles were compared using ANOVA. Pearson correlation coefficient was used to assess a relationship between GO density and gynecologic cancer incidence rates. A subset analysis of the census-reported socio-demographics of counties in the quintile with the highest cancer rate were compared between counties who did and did not have a GO in a local or adjacent county using t-test, and chi-squared for nominal data.
Descriptive statistics and visual representation of spatial data was conducted using spmap command in STATA 15.1 (StataCorp LLC, College Station, TX)
Results
In 2019, the NPPES included 1,527 national provider identifiers (NPIs) with a healthcare provider taxonomy classified as “gynecologic oncology”. Table 1 displays characteristics of the gynecologic oncologist workforce. A larger proportion of the group were male (57.6%), were not solo proprietors (86.4%), and have been in practice since before 2011 (89.6%). All states included an NPI registered to a county within the state’s borders except for North Dakota. Analyses by 9 census divisions indicated that 64.9% of GOs were concentrated in four census divisions in the United States: South Atlantic (19.5%), Middle Atlantic (18.1%), Pacific (13.8%), and East North Central (13.5%). The crude number of GO per county increased as the population of women increased per county (r= 0.72, p<0.01). Figure 1 demonstrates the proportion of the counties in each census division with no GOs in the local and adjacent counties by census division. 2,864 (91.2%) counties in the U.S. were found to have no oncologist in their local county. Expanding analyses to include adjacent counties, there were 1,943 (61.8%) counties with no gynecologic oncologist in local or adjacent counties. The census divisions with the highest proportion of no GO available in local and adjacent counties included the West North Central and East South Central and the division with the highest proximity to a GO was “New England”.
Table 1:
Characteristics of Providers with National Provider Identification characterized as Gynecologic Oncology.
| Characteristic | Frequency (%)/Mean (SE) |
|---|---|
|
| |
| Total NPI with taxonomy of Gynecologic Oncology | 1,527 (100) |
|
| |
| Gender – Female | 663 (43.4) |
|
| |
| Solo Proprietor | 207 (13.6) |
|
| |
| Census Division | |
| New England | 97 (6.4) |
| Middle Atlantic | 276 (18.1) |
| East North Central | 206 (13.5) |
| West North Central | 98 (6.4) |
| South Atlantic | 298 (19.5) |
| East South Central | 97 (6.4) |
| West South Central | 153 (10.0) |
| Mountain | 91 (6.0) |
| Pacific | 211 (13.8) |
|
| |
| Enumeration Year | |
| 2005–2010 | 1,369 (89.6) |
| 2011–2014 | 120 (7.9) |
| 2015–2019 | 38 (2.5) |
|
| |
| Last Update Year | |
| 2007–2010 | 325 (21.3) |
| 2011–2014 | 395 (25.9) |
| 2015–2019 | 807 (52.8) |
|
| |
| Mean number of gynecologic oncologists (per 100,000 women)± | |
| In all counties | 0.11 ± 0.01 |
| In counties with at least one GO | 1.24 ± 0.09 |
Figure 1:
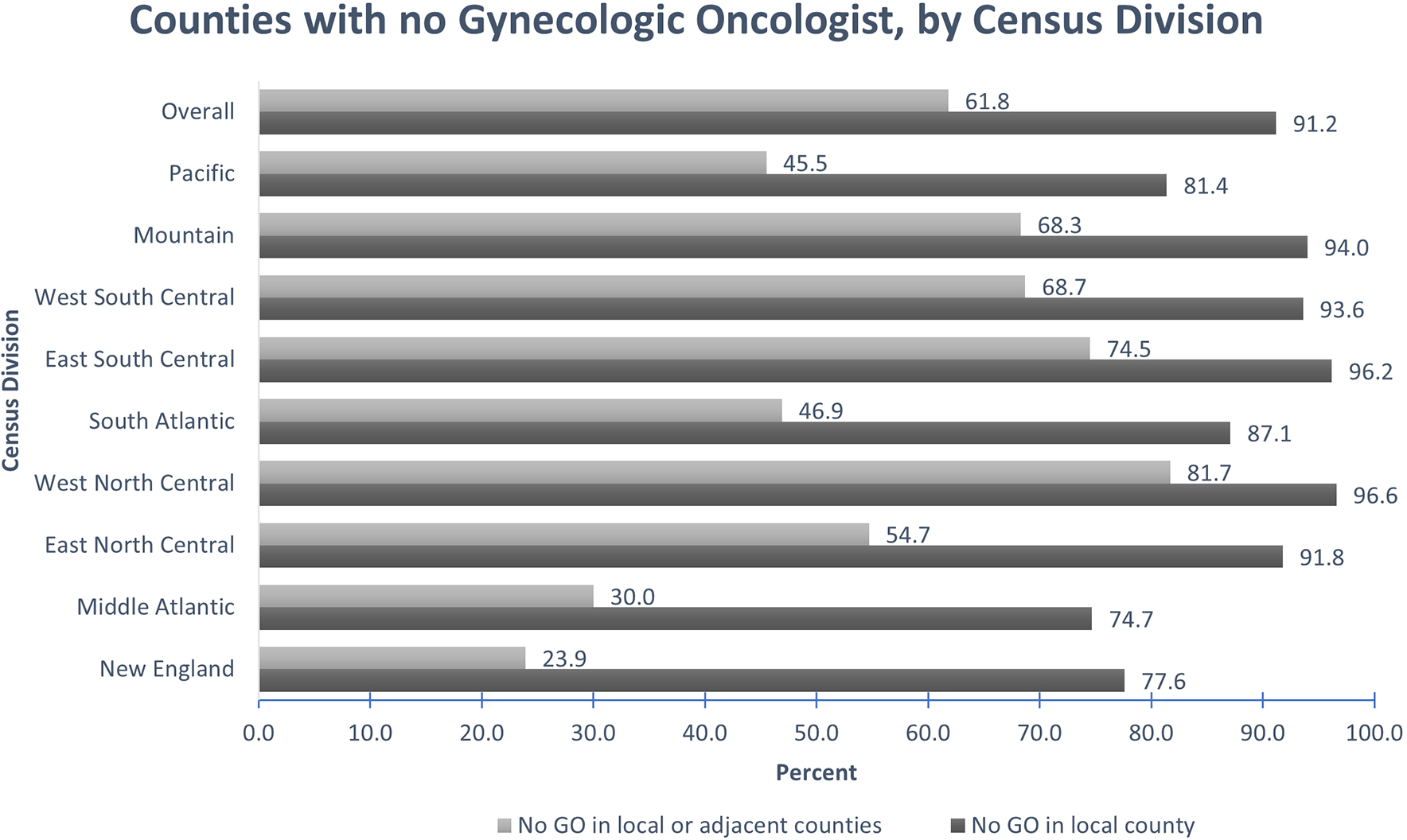
Counties with no gynecologic oncologist, by census division
Footnote: All 3,142 counties (including Minnesota) were included in data collection for Gynecologic Oncologist county location by NPI number.
GO distribution was compared to gynecologic cancer incidence rates to examine whether supply of GOs was more abundant in areas with higher demand for care. Of the 3,142 counties in the U.S., data on gynecologic cancer incidence rates, including cervix, ovary, and uterine cancers was available for 3,055 counties. Thirty-eight percent (38.2%) of counties had suppressed data reported (less than 16 cases). County quintiles were separated into the following groups by gynecologic cancer incidence rates: <16 cases/county representing 38.2% of the counties in the lowest two quintiles, with the remaining 61.8% of counties separated into the three remaining quintiles. The overall mean crude rate of gynecologic cancer incidence in the United States is 49.0 per 100,000 women. Gynecologic cancer rates per group and demographic comparisons between groups are displayed in Table 2. Compared with the lowest quintile counties, the counties in the top quintile of gynecologic cancer rate had a higher proportion of counties classified as metro (56.9% vs. 14.1%, p<0.01), higher median income ($59,856 vs. $50,981, p<0.01), lower proportion of Hispanic population (7.4% vs. 9.9%, p<0.01), and higher proportion of White population (86.7% vs. 85.2%, p<0.01).
Table 2:
Characteristics of counties by quintiles of Gynecologic cancer rate
| Overall | 1st and 2nd quintile (<16 cases/county) | 3rd quintile | 4th quintile | 5th quintile (highest cancer rate) | p-value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Number of counties | 3,055 | 1,168 | 631 | 627 | 629 | |
|
| ||||||
| Number of counties with no GO: | ||||||
| In local county | 2,782 (91.1) | 1,166 (99.8) | 600 (95.1) | 507 (80.9) | 509 (80.9) | <0.01 |
| In local or adjacent county | 1,876 (61.4) | 1,001 (85.7) | 378 (59.9) | 263 (41.9) | 234 (37.2) | <0.01 |
|
| ||||||
| Metro (n, %)± | 1,165 (37.1) | 165 (14.1) | 261 (41.4) | 354 (56.5) | 358 (56.9) | <0.01 |
|
| ||||||
| Median Household Income ($) (SE of median)± | 55,468 ± 262 | 50,981 ± 345 | 55,502 ± 613 | 59,381 ± 625 | 59,856 ± 574 | <0.01 |
|
| ||||||
| Race (Mean %/SE)± | ||||||
| White | 84.78 ± 0.30 | 85.19 ± 0.56 | 82.58 ± 0.67 | 83.21 ± 0.64 | 86.74 ± 0.49 | <0.01 |
| Black | 8.86 ± 0.26 | 7.86 ± 0.47 | 11.65 ± 0.65 | 10.33 ± 0.59 | 7.48 ± 0.41 | <0.01 |
| Asian American | 1.64 ± 0.05 | 0.89 ± 0.06 | 1.51 ± 0.08 | 2.49 ± 0.17 | 2.27 ± 0.15 | <0.01 |
| Indian American | 2.42 ± 0.14 | 3.83 ± 0.34 | 2.02 ± 0.22 | 1.58 ± 0.20 | 1.03 ± 0.09 | <0.01 |
| Native Hawaiian | 0.14 ± 0.02 | 0.14 ± 0.05 | 0.13 ± 0.01 | 0.15 ± 0.01 | 0.16 ± 0.03 | 0.95 |
| Two or more races | 2.17 ± 0.03 | 2.08 ± 0.05 | 2.11 ± 0.05 | 2.24 ± 0.05 | 2.32 ± 0.09 | <0.05 |
|
| ||||||
| Hispanic ethnicity± | 9.36 ± 0.25 | 9.87 ± 0.46 | 10.33 ± 0.61 | 10.03 ± 0.54 | 7.42 ± 0.35 | <0.01 |
|
| ||||||
| Mean crude Gynecologic cancer rate (per 100,000 women)* | 48.96 ± 0.32 | NR | 33.90 ± 0.25 | 48.32 ± 0.14 | 64.71 ± 0.33 | <0.01 |
|
| ||||||
| Mean number of gynecologic oncologists in counties with a GO (per 100,000 women) ± | 1.22 ± 0.09 | NR | 1.62 ± 0.38 | 1.09 ± 0.11 | 1.15 ± 0.11 | 0.14 |
The mean density of GO across all U.S. counties was 0.12 ± 0.57 per 100,000 women but in counties with at least one GO, this rate was 1.24 ± 1.53 GO per 100,000 women. The mean density of GO by cancer rate quintiles is displayed in Table 2. Overall, the density of GO did not increase significantly with increasing gynecologic cancer incidence across quintiles (p=0.14). There was no statistically significant correlation between gynecologic cancer rate and GO density (r=−0.12, p=0.06). Figure 2 displays the proportion of counties with no GO in a local county or a local and adjacent county, stratified by gynecologic cancer rate quintiles. The proportion of counties without a GO decreased with increasing gynecologic cancer incidence quintiles (p<0.01).
Figure 2:
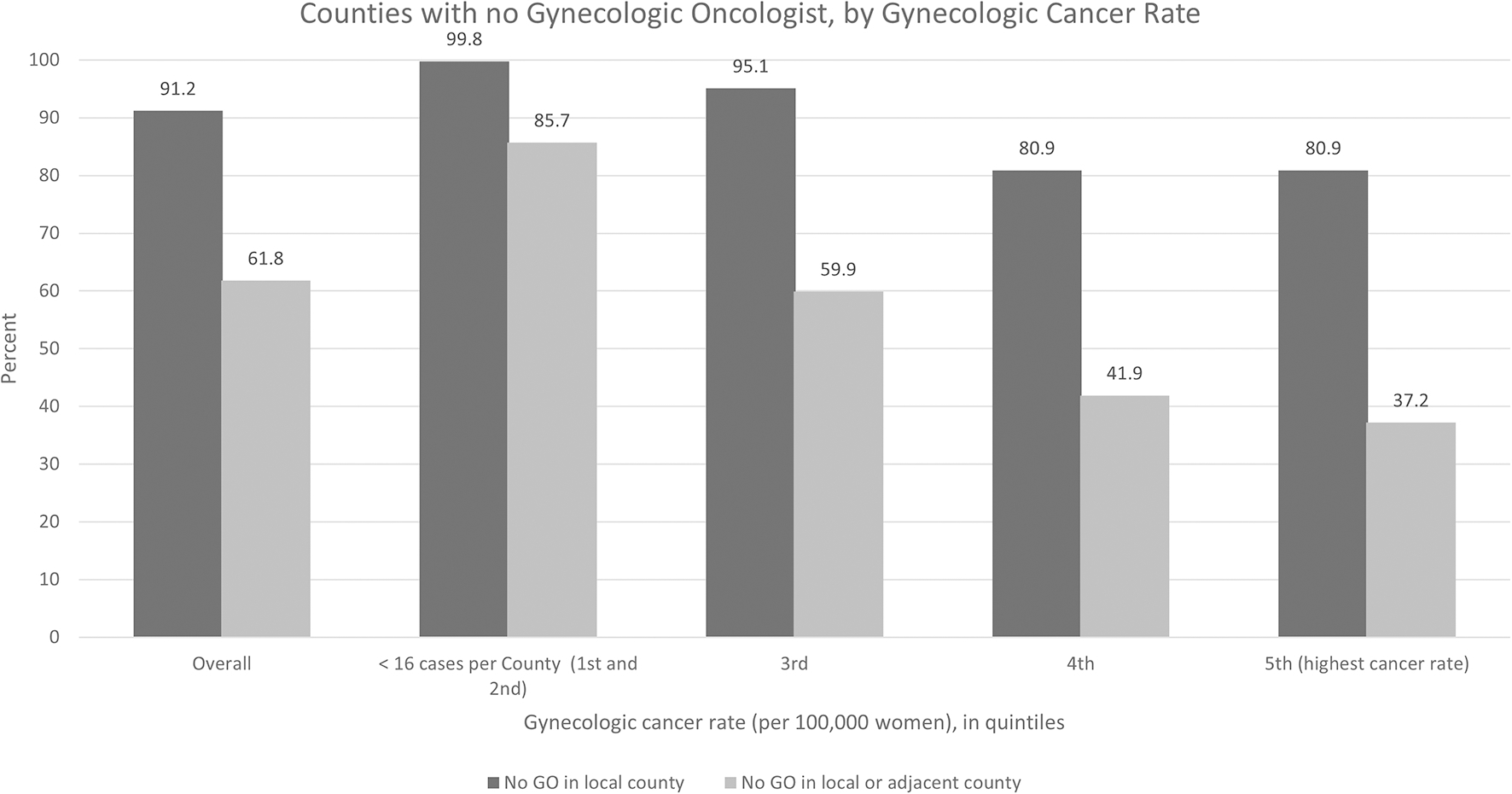
Counties with no Gynecologic Oncologist, by Cancer Rate and Mean population-adjusted density of Gynecologic Oncologist per 100,000 women.
Figure 3a presents a map of gynecologic cancer (Cervix, Ovary, and Uterine combined) rate per 100,000 women for each county with density of gynecologic oncologists illustrated by dots with larger dots representing a higher density. The map demonstrates a wide geographic variation, with many counties without a GO available but no correlation between gynecologic cancer incidence and GO density per county was appreciated. County-level density of GO with relationship to Cervix, Uterine, and Ovary cancer independently is displayed in Supplementary Figure 1. Figure 4 represents the distribution of areas where no GO is present in the local and adjacent counties. States in the census division of West North Central and East South Central had the highest proportion of no access to a GO within a local county and adjacent counties. The East North Central and South Atlantic regions contained the most counties in the highest quartile of gynecologic cancer rates but no GO, with 65 and 44 counties with no GO in local or adjacent counties, respectively.
Figure 3a:
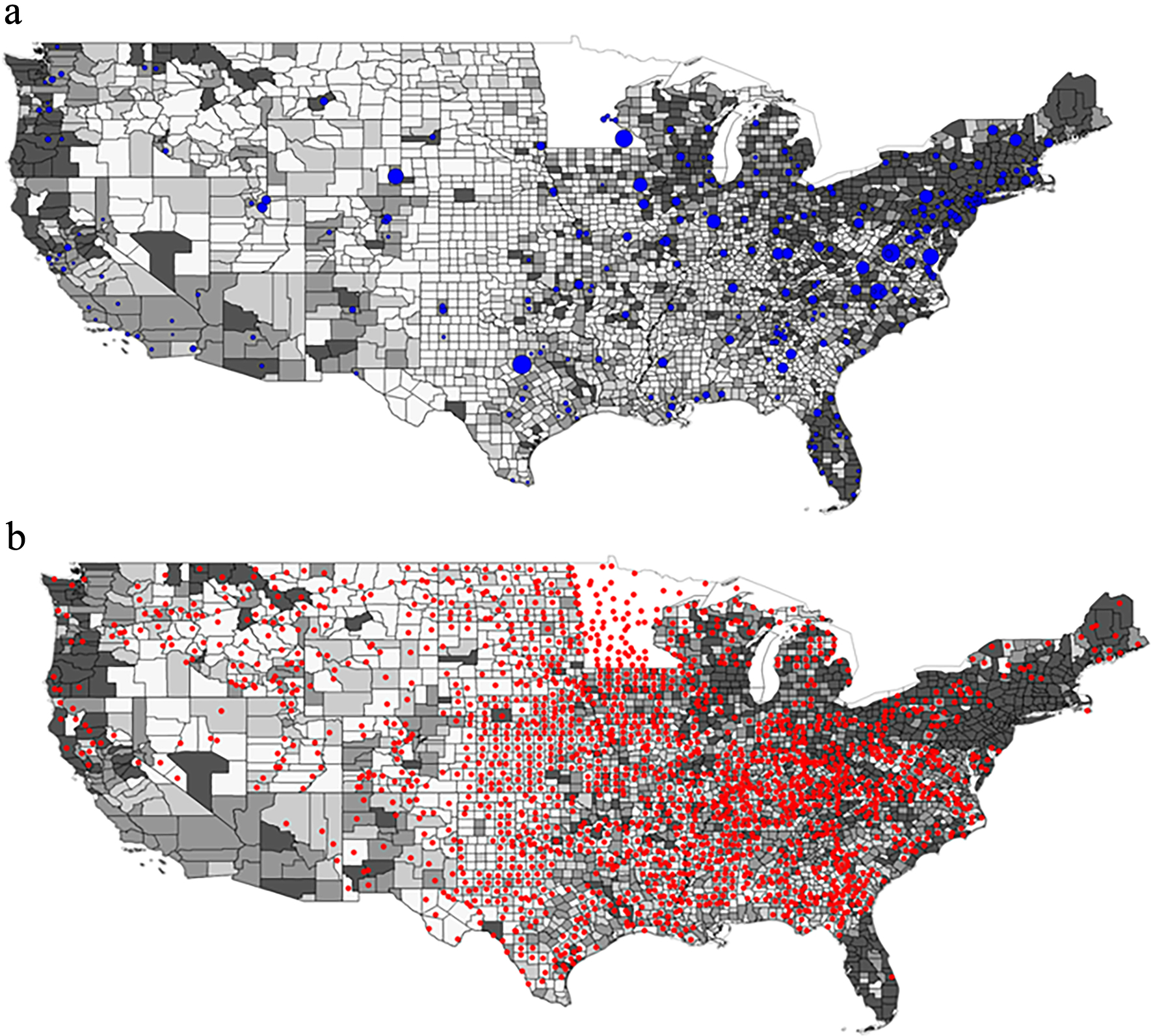
Gynecologic oncologist density and Gynecologic Cancer (Cervix, Ovary, and Uterine) rates (in quantiles) by U.S. counties. 3b: U.S. Counties without Gynecologic oncologists in the Home and Adjacent Counties and Gynecologic Cancer Rates (in Quantiles)
Footnote: Rates represent annual incidence of gynecologic cancer per 100,000 women. ‘Less than 16’ category represents two lowest quintiles. Source: 2013–2017 U.S. Cancer Statistics (17).
Figure 4:
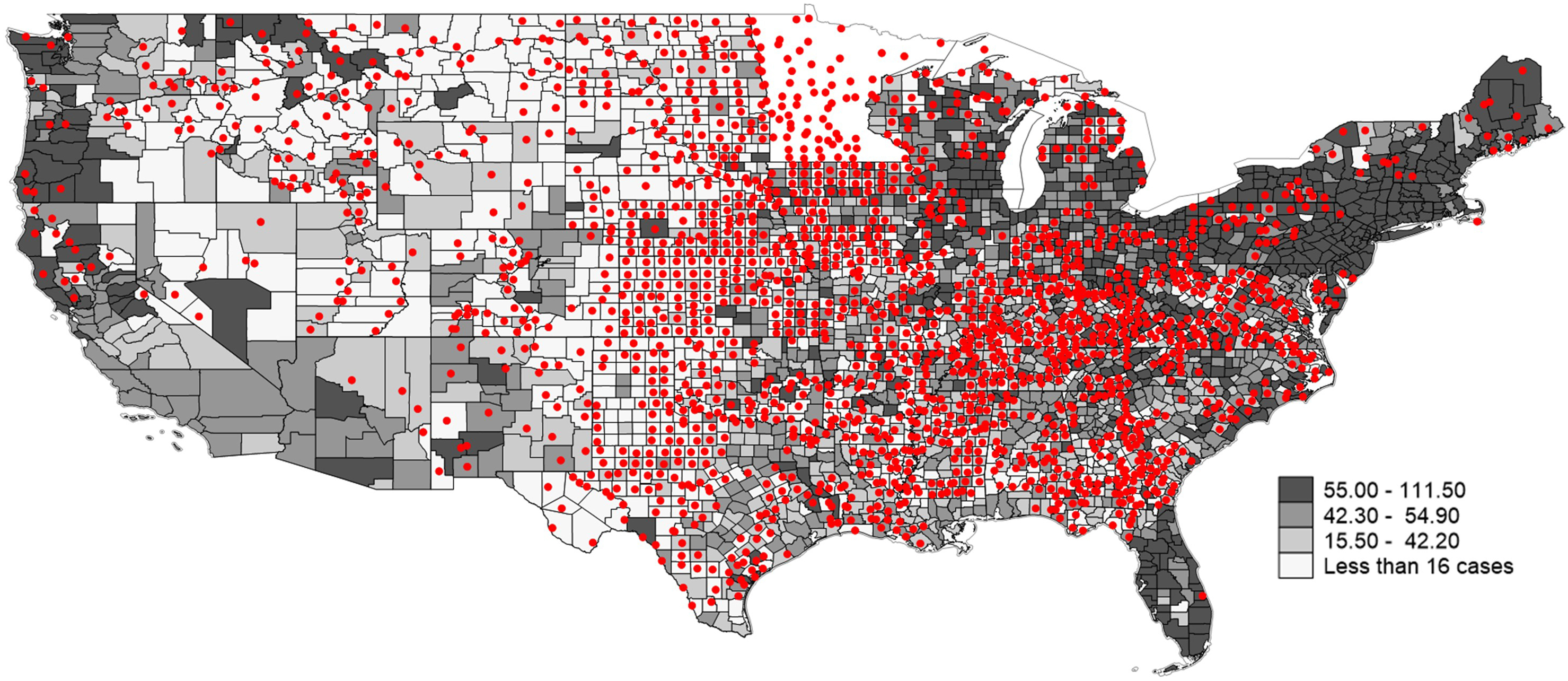
U.S. Counties without Gynecologic oncologists in the Home and Adjacent Counties and Gynecologic Cancer Rates (in Quantiles) Footnote: Rates represent annual incidence of gynecologic cancer per 100,000 women. ‘Less than 16’ category represents two lowest quintiles. Source: 2013–2017 U.S. Cancer Statistics (17).
A sub-group analysis of the counties in the highest quintile of gynecologic cancer rates was performed to investigate differences in census-demographics in counties with and without access to a GO. Results are displayed in table 3. Compared to counties without a GO, counties with a GO were noted to have a higher median income ($64,176 vs. $52,565), a lower proportion of White females (85.31% vs. 89.15%), higher proportion of Black females (8.66% vs. 5.49%) as well as Hispanic population (8.28% vs. 5.99%) (all p<0.01). Furthermore, counties with a GO were more likely to be classified as a metro area with 72.9% of counties classified as “metro” compared to 29.9% of counties in the counties without a GO in a local or adjacent county (p<0.01).
Table 3:
Characteristics of counties with the highest quintile of Gynecologic cancer rates
| No GO Available in local/adjacent county N= 234 | GO in local/adjacent county N= 395 | p-value | |
|---|---|---|---|
|
| |||
| Race (mean percent, SE) ± | |||
| White | 89.15 (0.79) | 85.31 (0.62) | <0.01 |
| Black/African-American | 5.49 (0.63) | 8.66 (0.53) | <0.01 |
| Asian American | 1.50 (0.22) | 2.72 (0.19) | <0.01 |
| Indian or Alaskan American | 1.26 (0.18) | 0.90 (0.10) | 0.05 |
| Hawaiian | 0.23 (0.08) | 0.12 (0.02) | 0.10 |
| Two or more races | 2.37 (0.20) | 2.29 (0.07) | 0.65 |
|
| |||
| Hispanic Ethnicity± | 5.99 (0.62) | 8.28 (0.41) | <0.01 |
|
| |||
| Metro (n, %)± | 70 (29.9) | 288 (72.9) | <0.01 |
|
| |||
| Median Household Income ($) (SE of median)± | 52,565 ± 836 | 64,176 ± 931 | <0.01 |
|
| |||
Discussion
In 2007, ASCO commissioned a workforce strategic plan to meet the growing demand of oncology services in the U.S (1, 21).Shih et al. examined the workforce distribution for overall oncology and oncology pharmacy providers and reported up to 16% of counties in the US without access to an oncologist in their local or adjacent counties (3). Our analysis in the gynecologic oncologist workforce demonstrates an even greater lack of county-level distribution, with only 8.8% of US counties having a GO in a local county and 38.2% of U.S. counties with a GO in a local or adjacent county.
Gynecologic cancer treatment with a gynecologic oncology specialist versus non-GOs has been linked with improved delivery of guideline-based treatments and improved survival outcomes (4, 5). Our analysis demonstrates that there are several census divisions that do not have access to a specialist, including areas that have higher incidence rates of gynecologic cancers. The proportion of counties with a GO (locally or in adjacent counties) increased with increasing gynecologic cancer incidence quintiles; however, even at the highest gynecologic cancer incidence quintile, 37.2% of counties did not have a local or adjacent county GO. As gynecologic cancer incidence increased, the distribution of GO per 100,000 women did not increase and remained similar across quintiles, suggesting a smaller pool of GOs to care for areas with a higher burden of cancer cases.
Receiving care from a specialty gynecologic oncologist is linked with improved outcomes (5). We found that counties with the highest gynecologic cancer rates and without access to a GO tended to be in rural areas and the women living in these counties had a lower median household income, and were predominately White. This suggests that rural White women may be underserved by gynecologic oncologists. Previous research has demonstrated that women with gynecologic cancers from rural areas are less likely to receive early, high-quality and comprehensive care, resulting in worse treatment and survival outcomes (7, 12, 22). Based on these findings, outreach efforts to provide specialty care should target rural populations. This information is important to improve screening, access, and outreach strategies targeting areas with high gynecologic cancer rates and inadequate supplies of GO.
There are several ways that the gynecologic oncology community has worked to help address the increasing needs of patients and overcome geographic-related barriers. . One strategy to provide GO care over a larger geographic area is to expand practice locations. A recent study by Hicks-Courant et al. found that from 2015 to 2019 although there was not a significant change in the number of gynecologic oncologists, individual practices and health care networks had an increase in clinical site locations, thereby increasing the geographic coverage by this specialty (23). This was found similarly in the medical oncology population and resulted in decreased travel time for patients (24). Expanded telemedicine capabilities have allowed many health systems to accommodate patients at a distance. Telehealth in general oncology in rural Utah was found to decrease patient travel time by over 4 hours and over 300 miles per encounter (25) and gynecologic oncology patients in Wisconsin reported telehealth prevented them from driving on average 40 miles to an appointment (26) Multiple studies show patients are satisfied with telehealth (26, 27). With patient and provider acceptance, integrating telemedicine into areas with geographic barriers can help to mitigate access issues.
The supply of gynecologic oncologist has also grown. According to data from the National Residency Matching Program, from 2011 until 2020, the number of new fellowship positions increased by 43% with 51 positioned offered in 2011 to 73 in 2020 (28, 29). This likely reflects the opening of new programs as well as programs increasing fellowship-training capacity. However, it is unknown whether this influx in graduates or existing providers are moving to practice in underserved areas. We saw that the number of GO increased with increasing populations of women, regardless of cancer incidence. Further exploration of GO motivation to work in different areas may be helpful to address workforce shortages.
Lastly, the use of diversified care is also an option to increase access. Medical oncologists, primary gynecologists, and other medical care professionals have provided care for gynecologic cancer patients without ready access to GO. Collaborating with other providers in remote areas and educating them on gynecologic-cancer specific care may improve patient access. Advanced practice providers such as nurse practitioners and physician assistants can help to increase the supply of care for gynecologic cancer patients. The most recent Society of Gynecologic Oncology State of the Society report included 132 registered nurse practitioner and physician assistance members (30). An ASCO report noted there were an estimated 5,300–7,000 APP who work in an oncology practice and help to provide patient-centered care for individuals with cancer (31). In this study, patients reported equivalent satisfaction in their care when seen by a non-physician as part of their oncologic care. Further growth in collaborative efforts between oncologists and APPs may help extend the gynecologic oncology reach to areas of lower access.
Our study includes several limitations. First, gynecologic cancer incidence is not fully captured through our methods given the rarity of gynecologic cancer on the cancer spectrum. Several counties were unable to provide detailed information on rates for specific types of gynecologic cancers due to patient anonymity concerns and lack of consistent numbers over time resulting in inaccurate incidence data. Second, our representation of the GO workforce is a cross-section of when our NPEES report was retrieved (September 2019) and therefore only represents a snapshot of the workforce at that time. Our study utilized NPI locations for the primary site only but did not include additional outreach satellite locations where an NPI may be registered secondarily; this may leave out counties with satellite access. Additionally, GO were identified by taxonomy code, which was self-selected by physicians, and we acknowledge that patients with gynecologic cancers may receive care from medical oncologists or general gynecologists who do not register under this taxonomy code. The purpose of our study, however, was to highlight the distribution of specialty care provided by GO, which has been linked to better patient outcomes. While we would have liked to look at the effect on patient mortality, a majority of mortality data (85%) at the county level was suppressed due to low case counts, therefore meaningful analysis were unable to be performed. Census and sociodemographic data used for this study represent characteristics of the female population in US counties; however, this is cross-sectional data and may not fully represent patients affected by gynecologic cancer in each county. It is important to note that although having a GO in a county may be helpful; this does not address access issues for uninsured patients, under-insured patients and patients with network-preference insurance plans. Furthermore, with our data we are unable to define the physical distance and time required for patients to travel between counties. This information would be helpful to understand the burden of travel required.
We assessed the distribution of gynecologic oncologists in the United States and compared this with incidence rates of gynecologic cancer. In conclusion, our analysis found that a significant portion of counties in the United States did not have access to a gynecologic oncology specialist in their home county or nearby counties. Even in counties where the gynecologic cancer rate was highest, over one-third of these counties had no access to a gynecologic oncologist. These counties represent geographically underserved areas and included a larger proportion of White race, lower income, rural counties. In gynecologic oncology, both the supply and type of providers available to patients has increased but there are still substantial geographic gaps in care. New mechanisms to extend patient care through office locations and telemedicine can help increase access (23, 26). There is still considerable work to be done to further develop this framework in areas of the country with geographically limited access.
Supplementary Material
Supplementary Figure 1a-c: Maps representing density of Gynecologic oncologists and Gynecologic Cancer (Cervix, Ovary, and Uterine) rates by US Counties
Footnote: Rates represent annual incidence of gynecologic cancer per 100,000 women. SOURCE: 2013–2017 Source: U.S. Cancer Statistics (17).
Highlights.
In 2019, there were 1,527 gynecologic oncologists (GO) registered with a NPI in the United States.
61.8% of US counties did not have a gynecologic oncologist in their local or adjacent county.
37.2% of counties with the highest gynecologic cancer rates did not have a gynecologic oncologist locally.
Women in counties with the highest gynecologic cancer rate and no GO were lower income, majority white and in non-metro areas.
Funding:
SAA is funded by the Bears Care, the philanthropic organization for the Chicago Bears. Shih acknowledges funding from the National Cancer Institute (R01CA207216, R01CA225647).
Footnotes
Conflict of Interest Statement:
Authors SAA and NKL report no conflict of interest. Shih received consulting fees, travel, and accommodations for serving on a grants review panel for Pfizer Inc and an advisory board for AstraZeneca in 2019.
Disclaimer: The views expressed here are those of the authors and do not represent any official position of the National Cancer Institute or the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Erikson C, Salsberg E, Forte G, Bruinooge S, Goldstein M. Future supply and demand for oncologists : challenges to assuring access to oncology services. J Oncol Pract. 2007;3(2):79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang W, Williams JH, Hogan PF, Bruinooge SS, Rodriguez GI, Kosty MP, et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. J Oncol Pract. 2014;10(1):39–45. [DOI] [PubMed] [Google Scholar]
- 3.Shih YT, Kim B, Halpern MT. State of Physician and Pharmacist Oncology Workforce in the United States in 2019. JCO Oncol Pract. 2021;17(1):e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. [DOI] [PubMed] [Google Scholar]
- 5.Vernooij F, Heintz P, Witteveen E, van der Graaf Y. The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecol Oncol. 2007;105(3):801–12. [DOI] [PubMed] [Google Scholar]
- 6.Howlader N, Noone A, Krapcho M, Miller D, Brest A, Yu M, et al. SEER Cancer Statistics Review, 1975–2017. Bethesda, MD; 2020. April 2020. [Google Scholar]
- 7.Mercado C, Zingmond D, Karlan BY, Sekaris E, Gross J, Maggard-Gibbons M, et al. Quality of care in advanced ovarian cancer: the importance of provider specialty. Gynecol Oncol. 2010;117(1):18–22. [DOI] [PubMed] [Google Scholar]
- 8.American Cancer Society. Cancer Facts & Figures 2021. Atlanta, GA: American Cancer society; 2021. [Google Scholar]
- 9.Shalowitz DI, Vinograd AM, Giuntoli RL 2nd. Geographic access to gynecologic cancer care in the United States. Gynecol Oncol. 2015;138(1):115–20. [DOI] [PubMed] [Google Scholar]
- 10.Temkin SM, Rimel BJ, Bruegl AS, Gunderson CC, Beavis AL, Doll KM. A contemporary framework of health equity applied to gynecologic cancer care: A Society of Gynecologic Oncology evidenced-based review. Gynecol Oncol. 2018;149(1):70–7. [DOI] [PubMed] [Google Scholar]
- 11.Tan W, Stehman FB, Carter RL. Mortality rates due to gynecologic cancers in New York state by demographic factors and proximity to a Gynecologic Oncology Group member treatment center: 1979–2001. Gynecol Oncol. 2009;114(2):346–52. [DOI] [PubMed] [Google Scholar]
- 12.Bristow RE, Chang J, Ziogas A, Anton-Culver H, Vieira VM. Spatial analysis of adherence to treatment guidelines for advanced-stage ovarian cancer and the impact of race and socioeconomic status. Gynecol Oncol. 2014;134(1):60–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid. CMS: Data Dissemination: Announcing Changes to the National Plan and Provider Enumeration System (NPPES) Downloadable File. Baltimore, MD; 2019. 2019. [Google Scholar]
- 14.DesRoches CM, Barrett KA, Harvey BE, Kogan R, Reschovsky JD, Landon BE, et al. The Results Are Only as Good as the Sample: Assessing Three National Physician Sampling Frames. J Gen Intern Med. 2015;30 Suppl 3:S595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.United States Census Bureau. County Adjacent File. In: Commerce USDo, editor. 2010.
- 16.United States Census Bureau. County Population Totals: 2010–2019. In: Commerce USDo, editor. 2020.
- 17.Kansas Cancer Registry [Internet]. KU Medical Center. 2021. [cited 3/30/3021]. Available from: https://www.kumc.edu/kcr/zsearch.aspx. [Google Scholar]
- 18.U.S. Cancer Statistics Working Group. United States Cancer Statistics (USCS) Data Visualizations Tool, based on 2019 submission data (1999–2017). Atlanta, GA: U.S. Department of Health and Human Services, Control DoCPa; 2020. Accessed December 18, 2020. [Google Scholar]
- 19.United States Census Bureau. County Population Characteristics: 2010–2019. U.S. Census Bureau; 2019. [Google Scholar]
- 20.Service ER. Unemployment and median household income for the U.S., States and counties, 2000–19. In: Agriculture USDo, editor. 2021.
- 21.Erikson C, Schulman S, Kosty M, Hanley A. Oncology Workforce: Results of the ASCO 2007 Program Directors Survey. J Oncol Pract. 2009;5(2):62–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrington DA, Dilley SE, Landers EE, Thomas ED, Boone JD, Straughn JM Jr., et al. Distance from a Comprehensive Cancer Center: A proxy for poor cervical cancer outcomes? Gynecol Oncol. 2016;143(3):617–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hicks-Courant K, Kanter GP, Giuntoli RL 2nd, Schapira MM, Bekelman JE, Latif NA, et al. An increase in multi-site practices: The shifting paradigm for gynecologic cancer care delivery. Gynecol Oncol. 2021;160(1):3–9. [DOI] [PubMed] [Google Scholar]
- 24.Tracy R, Nam I, Gruca TS. The influence of visiting consultant clinics on measures of access to cancer care: evidence from the state of Iowa. Health Serv Res. 2013;48(5):1719–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thota R, Gill DM, Brant JL, Yeatman TJ, Haslem DS. Telehealth Is a Sustainable Population Health Strategy to Lower Costs and Increase Quality of Health Care in Rural Utah. JCO Oncol Pract. 2020;16(7):e557–e62. [DOI] [PubMed] [Google Scholar]
- 26.Mojdehbakhsh RP, Rose S, Peterson M, Rice L, Spencer R. A quality improvement pathway to rapidly increase telemedicine services in a gynecologic oncology clinic during the COVID-19 pandemic with patient satisfaction scores and environmental impact. Gynecol Oncol Rep. 2021;36:100708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmerman BS, Seidman D, Berger N, Cascetta KP, Nezolosky M, Trlica K, et al. Patient Perception of Telehealth Services for Breast and Gynecologic Oncology Care during the COVID-19 Pandemic: A Single Center Survey-based Study. J Breast Cancer. 2020;23(5):542–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Resident Matching Program. Results and Data: Specialties Matching Service 2020 Appointment Year. Washington, DC; 2020. [Google Scholar]
- 29.National Resident Matching Program. Results and Data: Specialties Matching Service 2011 Appointment Year. Washington, DC; 2011. [Google Scholar]
- 30.Oncology SoG. The Society of Gynecologic Oncology 2020 State of the Society Survey. Chicago, IL: Society for Gynecologic Oncology; 2020. [Google Scholar]
- 31.Bruinooge SS, Pickard TA, Vogel W, Hanley A, Schenkel C, Garrett-Mayer E, et al. Understanding the Role of Advanced Practice Providers in Oncology in the United States. J Oncol Pract. 2018;14(9):e518–e32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1a-c: Maps representing density of Gynecologic oncologists and Gynecologic Cancer (Cervix, Ovary, and Uterine) rates by US Counties
Footnote: Rates represent annual incidence of gynecologic cancer per 100,000 women. SOURCE: 2013–2017 Source: U.S. Cancer Statistics (17).


