Abstract
Aim and objective
To evaluate the success rate of stainless-steel crowns (SSCs) placed on permanent molars among adolescents in King Abdulaziz University Dental Hospital (KAUDH).
Materials and methods
Electronic records of KAUDH patients aged 10 to 15 years who had an SSC placed on a permanent molar from 2013 to 2018 were reviewed. The patients were contacted by telephone and were invited to participate in the study. The patients were examined clinically and radiographically.
Results
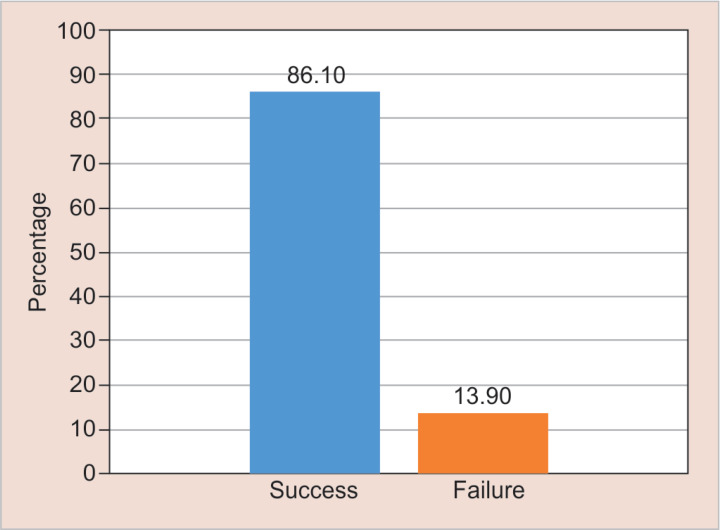
The response rate was 42.6%. The total number of SSCs included in the study was 36 crowns. The mean age was 11.75 ± 1.95. Males represented 75.76% of the subjects. The success rate of SSCs placed on permanent molars was 86.10%.
Conclusion
Placement of SSCs on permanent molars is a highly successful long-term temporary restoration that preserves badly destructed molars in adolescents until definitive prosthetic treatment can be done.
Clinical significance
To provide updated knowledge to healthcare providers and researchers about the success rate of SSCs when placed on permanent molars.
How to cite this article
Felemban O, Alagl H, Aloufi W, et al. Success Rate of Stainless-steel Crowns Placed on Permanent Molars among Adolescents. Int J Clin Pediatr Dent 2021;14(4):488–491.
Keywords: Adolescents, Permanent molars, Stainless-steel crowns
Introduction
Preformed metal crowns, also known as stainless-steel crowns “SSCs”, are usually used to restore primary molars and badly broken-down permanent molars. Primary SSCs are indicated in teeth with developmental defects, large carious lesions involving multiple surfaces, and after pulpotomy/pulpectomy procedures.1,2
Stainless-steel crowns that are performed on permanent teeth are used as an interim restoration to restore badly broken-down molars until the final restoration is to be placed.3 The SSCs placed on the first permanent molars have similarities compared with the SSCs on primary molars such as adapting these crowns, cementation, and acting as an interim restoration.3 However, they differ in the anatomical variation, the extent of preparation, degree of eruption, time of the procedure, and the longevity of the restoration.3 There are some situations where placing SSCs on permanent first molars is indicated such as restoring a badly broken-down endodontically treated tooth, extensive multisurface caries, financial consideration until permanent restorations are affordable, and in disorders in the tooth development such as molar-incisor hypomineralization (MIH), amelogenesis imperfecta, and dentinogenesis imperfecta.3
Stainless-steel crowns used to treat permanent first molars are inexpensive compared with other types of restorations, highly durable, provide the tooth with the benefits of the full coverage restorations and the minimal technique sensitivity during crown placement. On the other hand, there is one main disadvantage for these SSCs is the esthetics and the appearance during smiling, especially if the patients were highly concerned about their appearance.4
Only a few studies assessed the success rate of SSCs covering permanent teeth in adolescents. Therefore, the present study aimed to evaluate the success rate of SSCs placed on permanent molars among adolescents in King Abdulaziz University Dental Hospital (KAUDH).
Materials and Methods
Study Design
This study was designed as a cross-sectional study.
Ethical Approval
Ethical approval was acquired from the Research Ethics Committee, Faculty of Dentistry, King Abdulaziz University “KAU”, Jeddah, Saudi Arabia.
Study Subjects
Electronic records of KAUDH patients aged 10 to 15 years who had an SSC “3M ESPE, St. Paul, Minn” placed on a permanent molar during the time period from 2013 to 2018 were reviewed. The patients were contacted by telephone and were invited to participate in the study. The patients were examined clinically and radiographically.
Selection criteria for inclusion in the study were: “1. Healthy patients, 2. The patients were between 10 and 15 years of age when the SSCs ‘3M ESPE, St. Paul, Minn’ were placed, 3. Each patient had at least one permanent first molar restored with an SSC”.
Written informed consent was obtained from the patients/parents before the clinical examination.
Dental Record Review
Demographic data, information of each patient's medical history, date of the dental rehabilitation, and the type of dental procedure performed were recorded from the patient dental record. Out of the reviewed dental records, 23 records satisfied the inclusion criteria.
Clinical and Radiographic Examination
The crowned permanent molars were examined both clinically (visually and with a mirror and explorer) and radiographically (periapical radiographs “Kodak, Carestream Health, USA”).5 The following clinical parameters were recorded: “1. Crown marginal adaptation was measured at buccal and lingual walls and was either good with sealed margins or poor when the explorer detected an open margin, 2. The proximal contact area was recorded as intact or open by passing a dental floss. When the neighboring tooth was not present this criterion was ignored. 3. Presence of swelling or mobility. Mobility is graded clinically by holding the tooth firmly between the handles of two metallic instruments, and an effort is made to move it in all directions. Abnormal mobility often occurs buccolingually and is graded according to the ease and extent of tooth movement”.6 The following radiographic criteria were viewed: “1. Extension and adaptation of crown margins. Crowns were considered inadequate when crown margins appeared too short or extend below the cementoenamel junction (CEJ) or away from the tooth surface by a distance of >1 mm or when any critical defects in the crown were detected,7 2. Pathological external or internal root resorption. Radiolucency is observed in the external root surface of the dentin and adjacent bone, or in the internal root canal dentinal walls,8 3. Periapical or furcation radiolucency”.
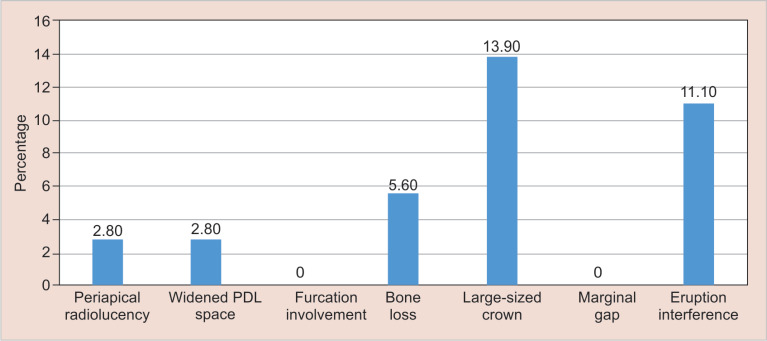
Stainless-steel crown clinical failure was defined as the presence of gingival inflammation, pain on percussion, mobility grade II, gingival abscess, fistula, deep pockets, or extraction. Radiographic failure was defined as the presence of a periapical lesion, bone loss, furcation radiolucency, widening of the periodontal ligament “PDL” space, large-sized crown, marginal gap, eruption interference.
Statistical Analysis
Data analysis was conducted utilizing the “Statistical Package for Social Sciences (SPSS) version 20.0” “SPSS Inc., Chicago, IL”. Data were tabulated and summarized as frequencies and percentages.
Results
Twenty-three out of 54 patients agreed to participate. The response rate was 42.6%. The total number of SSCs included in the study was 36 crowns. The mean age was 11.75 ± 1.95. Males represented 75.76% of the subjects. The success rate of SSCs placed on permanent molars was 86.10% (Tables 1 and 2).
Table 1.
Data distribution among the sample
| Demographics | Category | Frequency (%) |
|---|---|---|
| Gender | Male | 28 (77.8) |
| Female | 8 (22.2) | |
| Tooth # | 16 | 7 (19.4) |
| 26 | 5 (13.9) | |
| 36 | 10 (27.8) | |
| 46 | 14 (38.9) | |
| The students who placed the crown | Undergraduate students | 8 (22.2) |
| Postgraduate students | 28 (77.8) | |
| Year of crown placement | 2015 | 4 (11.1) |
| 2016 | 4 (11.1) | |
| 2017 | 7 (19.4) | |
| 2018 | 21 (58.3) | |
| Was the tooth endodontically treated before placing the crown? | Yes | 15 (41.7) |
Table 2.
Criteria of radiographic examination
| Periapical radiolucency | 1 (2.8%) |
| Widened PDL space | 1 (2.8%) |
| Furcation involvement | 0 (0.0%) |
| Vertical or horizontal bone loss | 2 (5.6%) |
| Large-sized crown | 5 (13.9%) |
| Marginal gap | 0 (0.0%) |
| Interference with the eruption of an adjacent tooth | 4 (11.1%) |
Reasons for failure included deep pockets, bone loss, and widening of the PDL space. None of the permanent SSCs showed any sign of failure of the following clinical features: gingival inflammation around the margins of the crown, gingival abscess, fistula or sinus tract, pain on percussion, increased mobility, crown perforation, traumatic occlusion, and extraction (Figs 1 to 3).
Fig. 1.
Overall success of permanent stainless-steel crowns
Fig. 3.
Criteria of radiographic examination
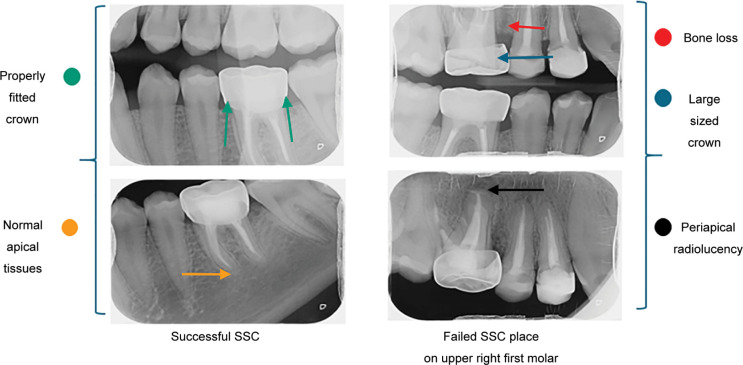
Radiographs showing a successful and a failed SSC on a permanent first molar are presented in Figure 4.
Fig. 4.
Radiographs show a successful and a failed stainless-steel crown on a permanent first molar
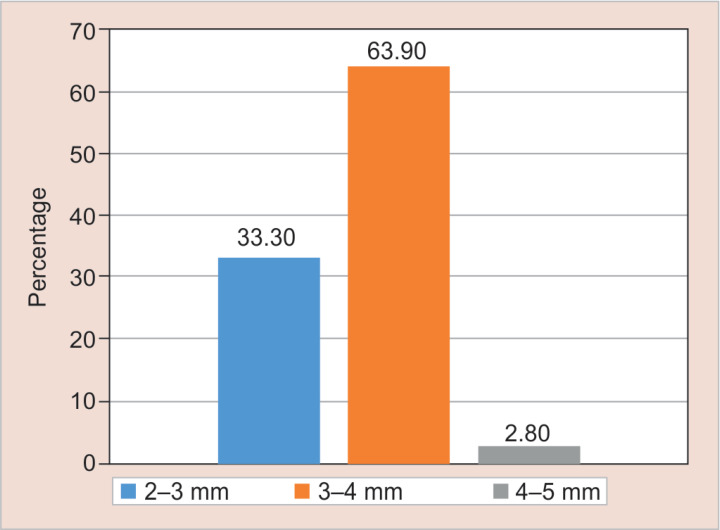
Fig. 2.
Average pocket depth
Discussion
Stainless-steel crowns have many features that make them preferable to use compared with other filling materials such as durability, full coverage, and low cost.2 On the other hand, several studies reported problems with using SSCs in primary teeth owing to plaque accumulation and marginal poor adaptation leading to periodontal diseases such as gingivitis. Therefore, it is important to adjust the crown carefully before cementation. Another disadvantage is the esthetics concerns. Many parents/children do not like to restore the teeth with SSCs especially the anterior teeth because of the metal color of the crown.1
Many studies evaluated the longevity and durability of primary SSC. The first study was published by Dawson et al. in 1981,9 who compared class I and class II amalgam restorations with SSCs in primary molar teeth. He concluded that the majority of amalgam restorations ended up by replacing a new one, unlike SSCs which have a high survival rate. Einwag and Dünninger10 also reached the same result as Dawson et al., by evaluating SSCs and 2-surface amalgam restorations in 66 patients over 8 years. The survival rate of SSCs was about 92, 90, and 83% in 3, 4.5, and 8 years, respectively. However, the survival rate of amalgam restorations was 66 and 36% at 3 and 4.5 years, respectively. Additionally, Gruythuysen and Weerheijm11 assessed the success rate of 106 pulpotomized primary molars restored with SSCs or amalgam in 57 pediatric patients. They concluded that the success rate for pulpotomies was significantly higher in teeth restored by SSCs (85%) than with an amalgam (68%) over 2 years.
Several studies were conducted to evaluate the success rate of SSCs placed on permanent molars. Discepolo and Sultan4 evaluated permanent tooth SSC longevity as an interim restoration for teeth requiring full coverage restoration in pediatric patients. They assessed 155 SSCs as temporary restorations on permanent molars in pediatric patients. Of 155 SSCs, 137 were considered successfully functioning. Total failures were 18. The overall combined success rate for the study group was observed to be 88% with an average service period of 45.18 months. Significant success was noted in patients <9 years of age, and significant failure was observed in patients 12 years and older.
Another study evaluated the long-term success rates based on clinical and radiographic findings of the SSC as a posterior restoration placed on permanent tooth compared with other restorations. This study included a total of 271 patients (2,621 posterior restorations were reported). Among these, 766 SSCs were assessed and documented with a 10-year survival rate (79.2%) in comparison with other different restorative modalities.12
Conclusion
Placement of SSCs on permanent molars is a highly successful long-term temporary restoration that preserves badly destructed molars in adolescents until definitive prosthetic treatment can be done.
Clinical Significance
To provide updated knowledge to healthcare providers and researchers about the success rate of SSCs when placed on permanent molars.
Authors Contributions
Osama Felemban: Contributed to the research idea, data analysis, results in interpretation, and in writing the manuscript. Haifa Alagl, Waad Aloufi: Participated in study design, clinical work, and in writing the manuscript. Omar El Meligy: Contributed to critically reviewing and revising the manuscript. All authors have read and approved the final manuscript.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Randall RC, Vrijhoef MMA, Wilson NHF. Efficacy of preformed metal crowns vs amalgam restorations in primary molar teeth: a systematic review. JADA. 2000;131(3):337–343. doi: 10.14219/jada.archive.2000.0177. [DOI] [PubMed] [Google Scholar]
- 2.Seale S. The use of stainless-steel crowns. Pediatric Dent. 2002;24(5):501–505. [PubMed] [Google Scholar]
- 3.Croll TP, Castaldi CR. The preformed stainless-steel crown for restoration of permanent posterior teeth in special cases. J Am Dent Assoc. 1978;97(4):644–649. doi: 10.14219/jada.archive.1978.0368. [DOI] [PubMed] [Google Scholar]
- 4.Discepolo K, Sultan M. Investigation of adult stainless-steel crown longevity as an interim restoration in pediatric patients. Int J Paediatr Dent. 2017;27(4):247–254. doi: 10.1111/ipd.12255. [DOI] [PubMed] [Google Scholar]
- 5.Sharaf AA, Farsi NM. A clinical and radiographic evaluation of stainless-steel crowns for primary molars. J Dent. 2004;32(1):27–33. doi: 10.1016/s0300-5712(03)00136-2. [DOI] [PubMed] [Google Scholar]
- 6.George AK. Tooth mobility. Review. SRM Univers J Dent Sci. 2011;2(4):324–327. [Google Scholar]
- 7.Salama FS, Alowyyed IS. Quality assessment of primary molar stainless–steel crowns. Dent News (Lond) 2001;8:17–20. [Google Scholar]
- 8.Fuss Z, Tsesis I, Lin S. Root resorption–diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19(4):175–182. doi: 10.1034/j.1600-9657.2003.00192.x. [DOI] [PubMed] [Google Scholar]
- 9.Dawson LR, Simon JF, Taylor PP. Use of amalgam and stainless–steel restorations for primary molars. ASDC J Dent Child. 1981;48(6):420–422. [PubMed] [Google Scholar]
- 10.Einwag J, Dünninger P. Stainless–steel crown vs multisurface amalgam restorations: an 8–year longitudinal study. Quintessence Int. 1996;27(5):321–323. [PubMed] [Google Scholar]
- 11.Gruythuysen RJ, Weerheijm KL. Calcium hydroxide pulpotomy with a light–cured cavity–sealing material after two years. ASDC J Dent Child. 1997;64(4):251–253. [PubMed] [Google Scholar]
- 12.Sigal AV, Sigal MJ, Titley KC, et al. Stainless steel crowns as a restoration for permanent posterior teeth in people with special needs: a retrospective study. J Am Dent Assoc. 2020;151(2):136–144. doi: 10.1016/j.adaj.2019.10.002. [DOI] [PubMed] [Google Scholar]