Abstract
Purpose:
The purpose of the current study was to evaluate associations between geographic rurality and tobacco use patterns among adolescents.
Methods:
High school students (N = 566) from north-central Appalachia reported on their lifetime and/or current use of cigarettes, electronic cigarettes (ECIGs), cigars, and smokeless tobacco. Geographic rurality was measured via the Isolation scale, whereby residential ZIP Codes determined the degree to which respondents have access to health-related resources. Latent class analysis (LCA) was used to identify discrete classes of adolescent tobacco users based on their use of tobacco products. Then, associations between participants’ geographic rurality and class membership were evaluated using a series of multinomial logistic regressions.
Findings:
LCA classified participants as Nonusers, Current ECIG Users, Cigarette/ECIG Experimenters, and Polytobacco Users. Individuals with higher Isolation scores were more likely to be Polytobacco Users and Cigarette/ECIG Experimenters than Nonusers, and were more likely to be Polytobacco Users than Current ECIG Users.
Conclusions:
The continuous Isolation scale used in the present study predicted polytobacco use patterns among adolescents in a manner that is consistent with, while simultaneously expanding upon, prior work. Tobacco control practices and policies should be viewed through a lens that considers the unique needs of geographically isolated areas.
Keywords: health disparities, polytobacco, rural, tobacco, youth
Not all populations in the United States have experienced the steady decline in tobacco use observed over the past decade.1 For instance, both adolescent and adult residents of more rural areas reveal significantly higher rates of cigarette and smokeless tobacco (SLT) use relative to their urban counterparts.1-3 These rates are markedly high in areas considered most geographically isolated, such as Central Appalachia and the Deep South.4,5 Nicotine addiction may also be more severe among those living in rural (vs nonrural) communities; rural adolescents begin smoking at younger ages6 and rural adults tend to be heavier smokers.7 Related to this inequality are multiple tobacco-related disadvantages experienced by rural populations, including weaker tobacco control policies, more positive cultural norms around tobacco use, targeted protobacco advertising, more barriers to health-promoting resources, and lower socioeconomic status (SES).3,6,8-13 Given that rural residents carry a heavier tobacco-related health burden than do those from more urban areas, the US Food & Drug Administration has designated them as “vulnerable.”14,15
Notably, these geographic patterns of cigarette and SLT use may not hold for other tobacco products. For instance, rates of water-pipe/hookah and cigarillo use are higher for adults in urban relative to rural areas,16 whereas rates for cigars/pipes do not differ by area for adolescents or adults.3,16,17 Findings regarding electronic cigarette (ECIG) use rates are mixed, with no differences between rural and urban adolescents or adults,2,17,18 higher rates for urban (vs rural) adolescents who also smoke cigarettes,2 higher rates for urban (vs rural) adult males but not females,16 and higher rates for urban (vs rural) adults only in the northern and western regions of the United States.19 Still, work that addresses geographic differences for these less traditional tobacco products is limited despite the staggering growth of their use in recent years.8,20-22 Such work also is limited for polytobacco use (ie, the concurrent use of multiple tobacco products), which is common among both adolescent and adult tobacco users.23-27 For adults, use of multiple traditional products (eg, cigarettes, SLT, and cigars/pipes) is associated with rural residence, whereas polytobacco use of alternative tobacco products (eg, ECIGs, cigarillos, and water-pipe/hookah) is associated with urban residence.16 When traditional and alternative product types are combined, however, adult polytobacco use patterns do not differ as a function of geography.16 For adolescents, polytobacco use may be more likely to occur for those residing in rural areas17; however, product type was not distinguished in this study (ie, any combination of traditional and/or alternative products was considered polytobacco use), making it difficult to elucidate specific patterns of polytobacco use. Clearly, more work is needed to address geographic disparities in these present day use patterns, particularly among vulnerable adolescent populations.
The purpose of the current study was to evaluate associations between geographic rurality and tobacco use patterns among adolescents. First, latent class analysis (LCA) was used to identify discrete classes of adolescent tobacco users based on their use of cigarettes, SLT, ECIGs, and cigars. Then, associations between participants’ geographic rurality and class membership were evaluated using a series of multinomial logistic regressions. Degree of geographic rurality was determined using the continuous Isolation scale,28 which is based on participants’ ZIP Codes and provides more variability than do other characterizations of rurality (eg, US Census, RUCA). Geographic isolation is a critical health-related characteristic of rural areas, which tend to be isolated from resources that support healthy living: basic infrastructure, employment, easy access to healthy food and health care, and reasonably good access to health-related information or products provided through internet services.28
METHOD
Participants
A convenience sample of adolescents (N = 566) was recruited from 4 high schools (n = 513) and one primary care adolescent medicine clinic (n = 53) located in north-central Appalachia (suburban Ohio, suburban West Virginia, rural West Virginia, and rural Pennsylvania) between fall 2015 and spring 2017. An attempt was made to recruit schools located in both rural and nonrural regions, while the medicine clinic allowed for continued recruitment into the summer months. This clinic services students primarily from 2 of the schools who participated in the study. Participants were 14-18 years of age (Mage = 15.95 years, SD = 1.16), currently enrolled in high school, and English speakers. The final sample consisted of primarily females (59.4% female) and White students (83.0% White vs 3.6% African American/Black, 4.1% Asian, 1.8% Hispanic/Latinx, and 5.5% Mixed race). Adolescents who exhibited significant cognitive impairment, as identified by teachers or clinic staff, were excluded from participating in the survey.
Procedure
All study procedures were approved by the university’s Institutional Review Board, as well as the collaborating schools and medicine clinic prior to data collection. The initial visit to schools consisted of an introduction to the study (participation requirements, potential risks and benefits) by a member of the research team, followed by distribution of the invitation letters and assent/consent forms for students to take home to their parents/legal guardians. The second visit to schools occurred ~2-7 days after the first visit and involved collection of the signed consent forms. Those who consented to participate were asked to complete a variety of measures (eg, tobacco product use, risk behaviors, smoking expectancies, and self-efficacy). Participants completed all questionnaires via paper-and-pencil during regular class time; research staff were available to answer questions. At the medicine clinic, physicians screened for youth who appeared to meet inclusion criteria. For those who expressed interest in the study, research staff explained participation requirements and then obtained assent/consent from youth as well as consent from parents. Clinic youth completed the same packet of paper-and-pencil questionnaires as school-based participants, and in locations separated from their parents. Both students and clinic patients who completed all questionnaires were entered into a lottery drawing for the chance to win one of 40 gift cards at a value of $20 each. To reduce potential data entry errors, questionnaire data were transferred from paper into 2 separate SPSS (IBM Corp., Armonk, NY) data files by independent researchers. Comparisons between the 2 data files were made and discrepancies were resolved prior to data analysis.
Predictors/measures
Student information form
This form contained questions regarding demographic characteristics, including age, sex (male or female), and mother/father education (used as a proxy for SES). For the latter characteristic, participants were categorized as having none (32.3%), 1 (23.9%), or 2 parents (42.4%) with a college education or higher. If participants reported on the education of only 1 parent, the education level of that single parent was used.
Tobacco product use
Measures of tobacco product use were derived from the Youth Risk Behavior Survey (YRBS). Lifetime use of cigarettes (“Have you ever tried cigarette smoking, even one or two puffs?”) and ECIGs (“Have you ever used an electronic vapor product?”; examples, such as “Blu,” “NJOY,” “vaping pens,” and “e-cigarette” were provided) was measured using a dichotomous scale. Adolescents provided an answer of “no” (classified as “nonuser”) or “yes” (classified as “lifetime user”). Lifetime users were then asked whether they currently used a particular product: cigarettes (“During the past 30 days, on how many days did you smoke cigarettes?”) or ECIGs (“During the past 30 days, on how many days did you use an electronic vapor product?”). Their answers to these latter questions were provided on a 7-point Likert scale that ranged from 0 (0 days) to 6 (all 30 days). Those who reported use of that product on at least 1 day of the past 30 days were considered “current users.” Note that the YRBS does not assess lifetime use of other tobacco products.
Adolescents were also asked about their current use of SLT (“During the past 30 days, on how many days did you use chewing tobacco, snuff, or dip, such as Redman, Levi Garrett, Beechnut, Skoal, Skoal Bandits, or Copenhagen?”) and cigar products (“During the past 30 days, on how many days did you smoke cigars, cigarillos, or little cigars?”). Answers were provided on the same 7-point Likert scale as that for cigarettes and ECIGs; youth were categorized as “current users” if they reported product use on at least 1 day of the past 30 days.
Isolation scale
All measures of rurality in common use in the United States capture the construct of geographic isolation, and do so with varying levels of precision (categorization) and at various levels of geography.29 The Isolation scale28 is a continuous measure of rurality based on the distance to populated areas and calibrated on the geographic distributions of health-related resources. It is calculated at the level of the US Census tract or ZIP Code. The continuous nature of the measure is valuable for this research because of the small area studied in which most measures of rurality do not provide sufficient variability. A detailed description of the calculation and validation of the Isolation scale is found in the work of Doogan and colleagues.28 These researchers found that the Isolation scale was well correlated with other measures of rurality and it was a better predictor of all 3 health outcomes that were evaluated—infant mortality rates, national smoking-related mortality rates, and smoking quit ratios—than any of the most commonly used measures of rurality in the United States.
Analytic plan
All analyses were conducted using Mplus 8.4.30 Full-information maximum likelihood (FIML) was used to estimate missing data in all analyses. First, an LCA was conducted to determine classes of tobacco use among adolescents using the lifetime and current use categorizations described above. LCA is a person-centered approach that classifies individuals into groups based on their pattern of scores from a set of dichotomous variables.31 The number of classes was empirically determined based on fit indexes, such as the Akaike Information Criterion (AIC)32 and the Bayesian Information Criterion (BIC),33 for which lower values represent more parsimonious models. Additionally, the Vuong Lo-Mendal Rubin LRT test was used to assess model fit. This fit index evaluates whether a model with k classes provides a significant improvement in fit over a model with k-1 classes. Finally, entropy values were considered in evaluating model fit. Entropy values range from 0 to 1, with values closer to 1 representing better classification quality. Starting with a 1-class solution, models were estimated with increasingly more classes until there was no further model improvement (ie, fit indexes show no substantive change or additional classes are small, conceptually unclear, or there are slight variations on already identified classes).31
Once latent classes were identified, univariate comparisons were made for Isolation scores, age, sex, and parental education across classes using chi-square tests for categorical variables and one-way ANOVAs for continuous variables. Tukey’s Honestly Significant Difference post-hoc tests were used to follow-up on ANOVA findings that were significant. Then, multinomial logistic regressions were used to determine whether Isolation predicted class membership after accounting for demographic covariates (ie, age, sex, and parent education) and nonindependence introduced by nesting.
Due to lack of variability, race/ethnicity was not included as a covariate. To account for nonindependence introduced by nesting, a cluster variable was created that represented individuals who were recruited from each site and thus, were nested within a school or the clinic. Effects were allowed to vary by cluster. Due to the analysis of clustered data, analyses employed maximum likelihood estimation with robust standard erorors (ie, MLR). All statistical tests were considered significant when P < .05.
RESULTS
Latent class descriptions
An LCA utilizing 6 dichotomous tobacco use indicators (ie, lifetime cigarette, lifetime ECIG, current cigarette, current ECIG, current SLT, and current cigar) indicated that a 4-class solution fit the data well (Table 1). The 4-class solution provided the lowest AIC value, a significant Vuong Lo-Mendal Rubin LRT test, entropy greater than 0.80, and conceptual clarity with sufficient sample sizes.
TABLE 1.
Fit indices for latent class analyses
| Number of classes | AIC | BIC | LRT test P value | Entropy | Smallest class (% of sample) |
|---|---|---|---|---|---|
| 2 | 2187.242 | 2243.961 | <0.001 | 0.894 | 28.97% |
| 3 | 2118.225 | 2205.486 | <0.001 | 0.871 | 12.07% |
| 4 | 2105.284 | 2223.086 | 0.032 | 0.945 | 8.10% |
| 5 | 2113.617 | 2261.960 | 0.270 | 0.960 | 0.86% |
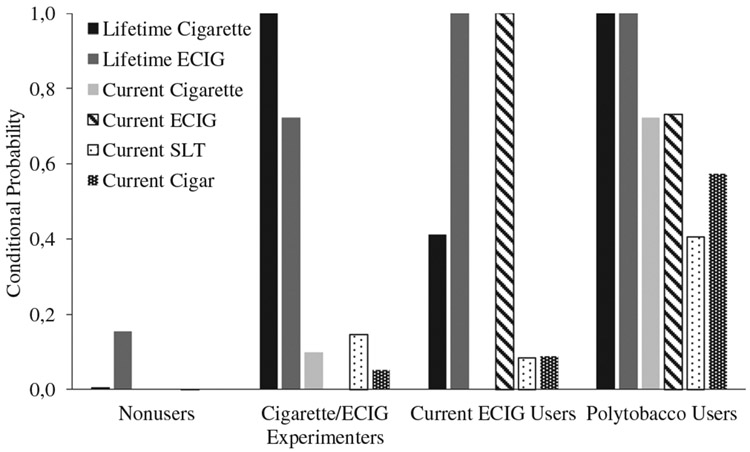
Figure 1 displays probabilities of endorsing each tobacco use item for each of the 4 latent classes, and Table 2 shows how many participants in each latent class endorsed lifetime and current use of tobacco products. Most participants were classified as Nonusers (67.8% of participants). None of the individuals in this class reported lifetime use of cigarettes or current use of any product; however, 15.5% of these individuals reported lifetime ECIG use. The second largest class was defined as Cigarette/ECIG Experimenters (12.5% of participants). Most youth in this class engaged in lifetime use of both cigarettes and ECIGS, but few reported current use of any product. Current ECIG Users (11.5% of participants) represented the third largest class; all participants in this class reported lifetime and current ECIG use, almost half reported lifetime cigarette use, and few reported use of other products. For the final class, Polytobacco Users (8.1% of participants), all participants reported lifetime use of cigarettes and ECIGs as well as current use of all products. Also among Polytobacco Users, nearly half (n = 21; 46.7%) indicated that they currently use 2 products: cigarettes concurrently with ECIGs (n = 11; 50.0%), cigars (n = 3; 13.6%) or SLT (n = 1; 4.6%); or cigars concurrently with ECIGs (n = 4; 18.2%) or SLT (n = 3; 13.6%). One-third (n = 15) of Polytobacco Users reported current use of 3 products: cigarettes and ECIGs concurrently with cigars (n = 8; 53.3%) or SLT (n = 2; 13.3%); or SLT and cigars concurrently with ECIGs (n = 4; 26.7%) or cigarettes (n = 1; 6.7%). The remaining Polytobacco Users (n = 8; 17.8%) reported current use of all 4 tobacco products.
FIGURE 1.
Conditional probabilities of endorsing each tobacco use item for the 4 latent classes
TABLE 2.
Tobacco use patterns as a function of latent class membership
| n (%) | |||||
|---|---|---|---|---|---|
| Full sample (N = 566) |
Nonusers (n = 386) |
Cigarette/ECIG experimenters (n = 70) |
Current ECIG users (n = 65) |
Polytobacco users (n = 45) |
|
| Lifetime cigarette | 144 (25.5) | 0 (0.0) | 70 (100.0) | 29 (44.6) | 45 (100.0) |
| Lifetime ECIG | 220 (38.9) | 60 (15.5) | 50 (71.4) | 65 (100.0) | 45 (100.0) |
| Current cigarette | 43 (7.6) | 0 (0.0) | 7 (10.0) | 0 (0.0) | 36 (80.0) |
| Current ECIG | 100 (17.8) | 0 (0.0) | 0 (0.0) | 65 (100.0) | 35 (77.8) |
| Current SLT | 36 (6.4) | 1 (0.3) | 9 (12.9) | 7 (10.8) | 19 (42.2) |
| Current cigar | 38 (6.7) | 0 (0.0) | 3 (4.3) | 4 (6.2) | 31 (68.9) |
Associations with latent classes
Table 3 presents descriptive statistics and univariate comparisons for participant characteristics as a function of latent class. Isolation scores, sex, and age differed significantly across classes (P’s < .05). Post-hoc tests revealed that, for Isolation, scores were significantly higher (ie, corresponding with a greater degree of rurality) for Cigarette/ECIG Experimenters and Polytobacco Users than for Nonusers. Cigarette/ECIG Experimenters also had significantly higher Isolation scores than did Current ECIG Users. For sex, the Polytobacco Users class included significantly more male participants than were in the Nonusers class. For age, Current ECIG Users were significantly younger than were Cigarette/ECIG Experimenters and Polytobacco Users. Nonusers were also significantly younger than were Cigarette/ECIG Experimenters and Polytobacco Users.
TABLE 3.
Isolation scores and sociodemograhics as a function of latent class membership
| n (%) or M (SD) | P value | |||||
|---|---|---|---|---|---|---|
| Full sample (N = 566) |
Nonusers (n = 386) |
Cigarette/ECIG experimenters (n = 70) |
Current ECIG users (n = 65) |
Polytobacco users (n = 45) |
||
| Isolation score | 6.1 (1.1) | 5.7 (0.9) | 6.4 (1.2) | 5.9 (1.1) | 6.4 (1.4) | <.001 |
| % Female sex | 343 (60.6) | 246 (63.6) | 43 (61.1) | 34 (52.3) | 20 (43.5) | .035 |
| Age | 16.2 (1.2) | 15.7 (1.2) | 16.5 (1.2) | 16.0 (1.2) | 16.6 (1.2) | <.001 |
| % Parents with ≥ | .118 | |||||
| college degree | ||||||
| 0 | 165 (29.2) | 88 (22.7) | 39 (54.2) | 25 (38.5) | 15 (32.6) | |
| 1 | 127 (22.4) | 77 (20.0) | 20 (27.8) | 17 (26.2) | 13 (28.3) | |
| 2 | 241 (42.6) | 201 (52.0) | 10 (13.9) | 18 (27.7) | 12 (26.1) | |
Note. M, mean; SD, standard deviation; P values are from one-way ANOVA (df = 563) for continuous variables and chi-square tests (df = 2) for categorical variables.
Table 4 illustrates the statistical outcomes for multinomial logistic regressions associating participant characteristics with latent class membership. After controlling for participant sex, age, and parental education, individuals with higher geographic Isolation scores (corresponding with a higher degree of rurality) were more likely to be Polytobacco Users than to be Current ECIG Users (OR = 1.61, CI = 1.10, 2.37) and Nonusers (OR = 1.51, CI = 1.06, 2.17). Those with higher Isolation scores were also more likely to be Cigarette/ECIG Experimenters than Nonusers (OR = 1.30, CI = 1.09, 1.54).
TABLE 4.
Multivariate associations between Isolation scores, sociodemographic covariates, and latent class membership
| Isolation score | Sex | Age | Parental education | ||
|---|---|---|---|---|---|
| ECIG (vs non) | B (SE), P value | −0.06 (0.08), .445 | −0.47 (0.29), .042 | 0.21 (0.10), .036 | −0.65 (0.08), <.001 |
| OR (CI) | 0.94 (0.82, 1.08) | 0.63 (0.39, 1.00) | 1.24 (1.05, 1.47) | 0.52 (0.46, 0.59) | |
| Exp (vs non) | B (SE), P value | 0.26 (0.11), .013 | −0.17 (0.46), .714 | 0.44 (0.13), .001 | −0.96 (0.20), <.001 |
| OR (CI) | 1.30 (1.09, 1.54) | 0.84 (0.39, 1.81) | 1.55 (1.26, 1.90) | 0.39 (0.28, 0.54) | |
| Poly (vs non) | B (SE), P value | 0.42 (0.22), .039 | −0.90 (0.35), .009 | 0.52 (0.19), .007 | −0.43 (0.35), .043 |
| OR (CI) | 1.51 (1.06, 2.17) | 0.41 (0.23, 0.72) | 1.67 (1.22, 2.30) | 0.65 (0.37, 1.16) | |
| Exp (vs ECIG) | B (SE), P value | 0.32 (0.16), .057 | 0.30 (0.45), .512 | 0.22 (0.16), .163 | −0.31 (0.20), .123 |
| OR (CI) | 1.38 (1.07, 1.78) | 1.34 (0.64, 2.82) | 1.25 (0.96, 1.62) | 0.74 (0.53, 1.02) | |
| Poly (vs ECIG) | B (SE), P value | 0.48 (0.23), .041 | −0.44 (0.46), .342 | 0.30 (0.22), .163 | 0.22 (0.32), .485 |
| OR (CI) | 1.61 (1.10, 2.37) | 0.65 (0.31, 1.38) | 1.35 (0.95, 1.93) | 1.25 (0.74, 2.10) | |
| Poly (vs Exp) | B (SE), P value | 0.16 (0.26), .548 | −0.73 (0.39), .046 | 0.08 (0.20), .699 | 0.53 (0.36), .039 |
| OR (CI) | 1.17 (0.76, 1.17) | 0.48 (0.25, 0.91) | 1.08 (0.77, 1.51) | 1.69 (0.94, 3.04) |
Abbreviations: CI, 95% confidence interval; ECIG, current ECIG users; Exp, cigarette/ECIG experimenters; Non, nonusers; OR, odds ratio; Poly, polytobacco users.
Note. Parental education was entered into models as a continuous variable.
For sociodemographic covariates, females were less likely to be Current ECIG Users (OR = 0.63, CI = 0.39, 1.00) and Polytobacco Users (OR = 0.41, CI = 0.23, 0.72) than to be Nonusers. Females were also more likely to be Cigarette/ECIG Experiementers than Polytobacco Users (OR = 2.08, CI = 1.10, 3.93). Older adolescents were more likely to be Cigarette/ECIG Experimenters (OR = 1.55, CI = 1.26, 1.90) and Polytobacco Users (OR = 1.67, CI = 1.22, 2.30) than to be Nonusers. Finally, higher parental education (ie, more parents with a college degree or higher) was associated with reduced odds of being Current ECIG Users (OR = 0.52, CI = 0.46, 0.59), Cigarette/ECIG Experimenters (OR = 0.39, CI = 0.28, 0.54), and Polytobacco Users (OR=0.65, CI=0.37, 1.16) as compared to being Nonusers; lower parental education was also associated with increased odds of being Polytobacco Users than Cigarette/ECIG Experimenters (OR = 1.69, CI = 0.94, 3.04).
DISCUSSION
The purpose of this study was to classify patterns of adolescent tobacco use and determine whether such classes are associated with geographic rurality as measured by the Isolation scale. Tobacco use patterns were determined by LCA, and the classes observed herein mirror those in previous work with adolescents: the largest class was characterized by limited to no tobacco use, the smallest class was characterized by current use of multiple products, and one class appeared to be dominated by ECIG use.23,34-36 National-level survey data support these patterns, with ~60% of adolescents reporting no current or lifetime use of tobacco products, nearly 30% reporting lifetime polytobacco use, and over 10% reporting current polytobacco use.37 These same data show that lifetime and current rates of ECIG use have surpassed those even for cigarette smoking37 and that nearly 64% of current ECIG users report exclusive use of ECIGs.38 In the current sample, rates of lifetime and current ECIG use (39.0% and 17.7%, respectively) were higher than those for cigarette smoking (25.6% and 7.6%, respectively), and 55% of the Current ECIG Users reported no current cigarette smoking. The observed polytobacco use patterns also included primarily use of ECIGs (82.2% of participants) or cigarettes (75.6% of participants), followed by cigars (68.9% of participants) and SLT (42.2% of participants). Most dual product users reported the use of ECIGs and cigarettes (50.0%), and most users of 3 products reported the use of ECIGs, cigarettes, and cigars (53.3%).
Study findings of classes of polytobacco use differed as a function of geographic rurality, with the patterns supporting and extending previous work.2,16,17 Youth with higher Isolation scores were more likely to be Polytobacco Users and Cigarette/ECIG Experimenters than Nonusers, as well as more likely to be Polytobacco Users than Current ECIG Users. Polytobacco use among adults has been shown to be associated with both rural and urban residence, depending on the types of products used; concurrent use of only traditional products (eg, cigarettes, SLT, and cigars) is more likely among rural residents, whereas the opposite is observed for use of only alternative products (eg, ECIGs and hookah).16 When these product types are combined, however, differences by geographic area are not observed.16 Polytobacco use among youth has also been shown to be associated with rural residence.17 Unfortuantely, the specific types of products used concurrently in this youth sample were not reported; however, rates for current use of cigarettes or cigars (~5%-7%) were higher than for ECIGs or SLT (~3% each).17
Critically, individuals in classes who are more isolated may be less likely to seek out and utilize health-related resources because the costs to access them are too high. Of course, individuals who access such resources may not be the youth themselves, but rather their parents. Still, the potential negative consequences are likely the same. Youth and adults living in rural communities face not only inadequate health care systems and tobacco control programs, but also lower income levels and fewer transportation options.6 These tobacco prevention and cessation barriers are exacerbated by the fact that rural areas have long been the target of marketing campaigns and promotions by the tobacco industry.10,39,40 Indeed, rural residents report less exposure to antitobacco messages41 and more exposure to tobacco product advertisements42 than do their urban counterparts. Therefore, it is not surprising that classes with relatively high levels of lifetime and current use of various tobacco products (ie, Polytobacco Users and Cigarette/ECIG Experimenters) would be considered more isolated than classes with little history of use (ie, Nonusers).
Polytobacco Users also had higher Isolation scores than did Current ECIG Users. This former class was defined not only by lower levels of current ECIG use, but also higher overall levels of tobacco use, relative to the latter class. These Isolation score differences may be due to a myriad of factors. For instance, vape shops may be more heavily concentrated in urban, versus rural, areas,43,44 and ECIG availability may be more likely in high-, versus low-, income neighborhoods.45,46 Another possibility is that ECIG use is more common in urban areas where use of other tobacco products is made difficult by stricter clean indoor air policies.47,48 Future work should consider these factors as potential mediators of the relationship between tobacco use patterns and geographic isolation.
In addition to geographic isolation, classes differed as a function of demographic characteristics in the expected directions. Parental education, which served as a proxy for SES, was higher for Nonusers as compared to each of the 3 tobacco use classes. Lower educational attainment (both individual and parental) and/or SES has been associated reliably with higher rates of single49,50 or polytobacco use36,51,52 in adolescent and young adult samples. For cigar and ECIG use, results are mixed,53-55 and perhaps based on whether those sampled also use other tobacco products. Most cigar and ECIG users smoke cigarettes concurrently,56,57 including in adolescent populations.55,58 Results for sex differences support findings from the previous literature for use of all tobacco products. Females were at increased odds of being Nonusers as compared to Polytobacco Users and Current ECIG Users. Compared to their female counterparts, males are more likely to engage in single use of all products12,59-61 and to engage in polytobacco use.36,62 Also, younger participants were more likely to be Nonusers than Cigarette/ECIG Experimenters, consistent with work showing that older adolescents report more experimentation and continued use of tobacco products than younger adolescents.63
Limitations
Results must be considered in light of study limitations. First, the Isolation scale28 was validated using national-level data and includes scores that range from 0.0 to 12.1, representing a range of the greatest access to virtually no access to health-related resources. In the current study with a regional sample, scores were restricted within the range of 4.5-9.5. Although there was sufficient variability to predict class membership successfully among our sample of adolescents, results should be replicated using nationally representative data with greater variability in scores and a larger sample size. Another limitation involves the YRBS items used to measure certain tobacco products. For instance, items that assess the use of SLT (eg, snuff, chew, and snus) and cigar (eg, large, small, and cigarillo) products are aggregate in nature, preventing the differentiation between more and less traditional product types. These same survey items assessed current, but not lifetime, use of SLT and cigar products. Moreover, the items that assess ECIG use referred to such devices as “electronic vape products.” While a list of other terms/brands (eg, e-cigarette, vaping pens, Blu, NJOY, and Starbuzz) was provided to help guide respondents, more relevant examples may have been excluded (eg, personal vaporizer and pods)64 and led to an underestimation of ECIG use.65 The current study also relied solely on parental education as a proxy for SES. Although we did not assess other SES attributes (eg, parental occupation or income), previous studies show that adolescents’ report of parental education is (1) consistent with parents’ own report of education, (2) significantly associated with parental occupation and income, and (3) a stronger predictor of later developmental outcomes among youth compared to other SES-related attributes.66,67 Still, future research should consider the role of multiple proxies of SES on adolescents’ tobacco-related outcomes, specifically. Finally, the temporal relation between rurality and tobacco use cannot be established given the cross-sectional nature of this study.
CONCLUSION
The tobacco use landscape in the United States has been in flux over the past few decades, particularly among youth. Their steady decline in cigarette smoking has been overshadowed by their remarkable rates of use of alterative products like hookah and ECIGs, as well as their concurrent use of multiple tobacco products.68 Moreover, factors that reliably explain the use of cigarettes or other traditional products (eg, SLT) may not hold for use of these latter products. One such factor is geographic rurality, which has historically been associated with high rates of cigarette smoking and SLT use.1-5 In contrast, the literature is mixed regarding the association between rurality and use of alternative products, whether examined alone or in combination with more traditional ones.2,17,18 Therefore, the purpose of this study was to examine patterns of traditional and alternative tobacco use as a function of geographic rurality among youth. The continuous Isolation scale used in the present study28 predicted polytobacco use patterns among adolescents in a manner that is consistent with, while simultaneously expanding upon, prior work. Specifically, polyuse of traditional and alternative tobacco products was associated with higher levels of isolation, relative not only to nontobacco users but also those whose use was defined primarily by ECIGs. Given that all classes revealed relatively high rates of ECIG use, more work is needed to elucidate the characteristics that distinguish between ECIG users who do and do not use other tobacco products.
Findings support a recommendation that tobacco intervention efforts should be tailored to different classes of users and that users’ geographic isolation be considered in those efforts.69,70 In a similar fashion, policy makers could give attention to culturally competent approaches to addressing isolation-related disparities in youth tobacco use. The Centers for Disease Control and Prevention (2014)71 has stressed the importance of such approaches given the unique needs of rural communities, and recommends working directly with community members to identify the most optimal messages, media campaigns, and policies. More contextually relevant practice and policy efforts will reduce the unfortunate tobacco use disparities in rural youth, thereby enhancing health equity for this most vulnerable population.
Acknowledgments
FUNDING
This work was supported by the WV Prevention Research Center under Cooperative Agreement Numbers U48 DP005004 (2014-2019) and U48DP006391 (2019-2024) from the Centers for Disease Control and Prevention (CDC), and by the National Institute on Drug Abuse from the National Institutes of Health (NIH) and the Center for Tobacco Products of the US Food & Drug Administration (FDA) under R21DA051628. The content is solely the responsibility of the authors and does not necessarily represent the views of the CDC, NIH, or FDA.
REFERENCES
- 1.American Lung Association. Top 10 Populations Disproportionately Affected by Cigarette Smoking and Tobacco use. 2020. [Google Scholar]
- 2.Noland M, Rayens MK, Wiggins AT, et al. Current use of e-cigarettes and conventional cigarettes among US high school students in urban and rural locations: 2014 National Youth Tobacco Survey. Am J Health Promot. 2018;32(5):1239–1247. [DOI] [PubMed] [Google Scholar]
- 3.Roberts ME, Doogan NJ, Kurti AN, et al. Rural tobacco use across the United States: how rural and urban areas differ, broken down by census regions and divisions. Health Place. 2016;39:153–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hart JL, Walker KL, Sears CG, et al. The ‘state’ of tobacco: perceptions of tobacco among Appalachian youth in Kentucky. Tob Prev Cessat. 2018;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu SS, Homa DM, Wang T, et al. State-specific patterns of cigarette smoking, smokeless tobacco use, and e-cigarette use among adults — United States. Prev Chron Dis. 2016;16(17): 180362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Lung Association. Cutting Tobacco’s Rural Roots: Tobacco Use in Rural Communities. 2015. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance Survey. Analysis by the American Lung Association Epidemiology and Statistics Unit Using SPSS Software. 2018. [Google Scholar]
- 8.Harrell PT, Naqvi SMH, Plunk AD, Ji M, Martins SS. Patterns of youth tobacco and polytobacco usage: the shift to alternative tobacco products. Am J Drug Alcohol Abuse. 2017;43(6):694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henriksen L, Schleicher NC, Johnson TO, Roeseler A, Zhu SH. Retail tobacco marketing in rural versus nonrural counties: product availability, discounts, and prices. Health Promot Pract. 2020;21:36S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JGL, Henriksen L, Rose SW, Moreland-Russell S, Ribisl KM. A systematic review of neighborhood disparities in point-of-sale tobacco marketing. Am J Public Health. 2015;105(9):e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roberts ME, Berman ML, Slater MD, Hinton A, Ferketich AK. Point-of-sale tobacco marketing in rural and urban Ohio: could the new landscape of tobacco products widen inequalities? Prev Med. 2015;81:232–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sutter ME, Everhart RS, Miadich S, Rudy AK, Nasim A, CO Cobb. Patterns and profiles of adolescent tobacco users: results from the Virginia Youth Survey. Nicotine Tob Res. 2018;20:S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Agriculture. USDA ERS Geography of Poverty. 2017. [Google Scholar]
- 14.Food US and Administration Drug. Research Priorities. Washington, DC: USDA; 2019. [Google Scholar]
- 15.Higgins ST, Kurti AN, Palmer M, et al. A review of tobacco regulatory science research on vulnerable populations. Prev Med. 2019;128:105709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts ME, Doogan NJ, Stanton CA, et al. Rural versus urban use of traditional and emerging tobacco products in the United States. Am J Public Health. 2017;107(10):1554–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pesko MF, Robarts AMT. Adolescent tobacco use in urban versus rural areas of the United States: the influence of tobacco control policy environments. J Adolesc Health. 2017;61:70–76. [DOI] [PubMed] [Google Scholar]
- 18.Lewis-Thames MW, Langston ME, Fuzzell L, Khan S, Moore JX, Han Y. Rural-urban differences e-cigarette ever use, the perception of harm, and e-cigarette information seeking behaviors among U.S. adults in a nationally representative study. Prev Med. 2020;130:105898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mumford EA,Stillman FA,Tanenbaum E,et al. Regional rural-urban differences in e-cigarette use and reasons for use in the United States. J Rural Health. 2019;35:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Academy of Family Physicians. CDC: Adolescents Curious, Susceptible to Hookah Smoking. 2019.
- 21.Corey CG, King BA, Coleman BN, et al. Little filtered cigar, cigarillo, and premium cigar smoking among adults — United States, 2012–2013. Morb Mortal Wkly Rep. 2014;63(30):650–654. [PMC free article] [PubMed] [Google Scholar]
- 22.Cullen KA, Ambrose BK, Gentzke AS, Apelberg BJ, Jamal A, King BA. Notes from the field: use of electronic cigarettes and any tobacco product among middle and high school students — United States, 2011–2018. Morb Mortal Wkly Rep. 2018;67(45):1276–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cole AG, Chaurasia A, Kennedy RD, Leatherdale ST. Identifying behavioural characteristics of tobacco product and e-cigarette use clusters: a repeat cross-sectional analysis. Addict Behav. 2018;90:77–84. [DOI] [PubMed] [Google Scholar]
- 24.Kasza KA, Ambrose BK, Conway KP, et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N Engl J Med. 2017;376(4):342–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Osman A, Kowitt SD, Ranney LM, Heck C, Goldstein AO. Trends and racial disparities in mono, dual, and poly use of tobacco products among youth. Nicotine Tob Res. 2018;20:S22–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sung HY, Wang Y, Yao T, Lightwood J, Max W. Polytobacco use of cigarettes, cigars, chewing tobacco, and snuff among US adults. Nicotine Tob Res. 2016;18(5):817–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang TW, Asman K, Gentzke AS, et al. Tobacco product use among adults — United States, 2017. Morb Mortal Wkly Rep. 2018;67(44):1225–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doogan NJ, Roberts ME, Wewers ME, Tanenbaum ER, Mumford EA, Stillman FA. Validation of a new continuous geographic isolation scale: a tool for rural health disparities research. Soc Sci Med. 2018;215:123–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Academies of Sciences, Engineering, and Medicine. Rationalizing Rural Area Classifications for the Economic Research Service: A Workshop Summary. Washington, DC: National Academies Press; 2016. [Google Scholar]
- 30.Muthen LK, Muthen BO. Mplus User’s Guide. 7th ed. Los Angeles, CA:1998–2012. Muthen & Muthen. https://www.statmodel.com/download/usersguide/MplusUserGuideVer_7.pdf. [Google Scholar]
- 31.Nylund KL. Latent Transition Analysis: Modeling Extensions and An Application to Peer Victimization. Los Angeles, CA: 2007. [Google Scholar]
- 32.Akaike H A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19:716–723. [Google Scholar]
- 33.Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14:535–569. [Google Scholar]
- 34.Gilreath TD, Leventhal A, Barrington-Trimis JL, et al. Patterns of alternative tobacco product use: emergence of hookah and e-cigarettes as preferred products amongst youth. J Adolesc Health. 2016;58(2):181–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huh J, Leventhal AM. Progression of poly-tobacco product use patterns in adolescents. Am J Prev Med. 2016;51(4):513–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simon P, Camenga DR, Kong G, et al. Youth e-cigarette, blunt, and other tobacco use profiles: does SES matter? Tob Regul Sci. 2017;3(1):115–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and associated factors among middle and high school students — United States, 2019. MMWR Surveill Summ. 2019;68(12):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cullen KA, Gentzke AS, Sawdey MD, et al. E-cigarette use among youth in the United States. J Am Med Assoc. 2019;322(21):2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hendlin YH, Veffer JR, Lewis MJ, Ling PM. Beyond the brotherhood: Skoal Bandits’ role in the evolution of marketing moist smokeless tobacco pouches. Tob Induc Dis. 2017;15:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ling PM, Haber LA, Wedl S. Branding the rodeo: a case study of tobacco sports sponsorship. Am J Public Health. 2010;100:32–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zollinger TW, Saywell RM, Overgaard AD, Przbylski MJ, Dutta-Bergman M. Antitobacco media awareness of rural youth compared to suburban and urban youth in Indiana. Tobacco. 2006:22(2), 119–123. [DOI] [PubMed] [Google Scholar]
- 42.Burgoon ML, Albani T, Keller-Hamilton B, et al. Exposures to the tobacco retail environment among adolescent boys in urban and rural environments. Am J Drug Alcohol Abuse. 2019;45(2):217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dai H, Hao J. Geographic density and proximity of vape shops to colleges in the USA. Tob Control. 2017;26:379–385. [DOI] [PubMed] [Google Scholar]
- 44.Dai H, Hao J, Catley D. Vape shop density and socio-demographic disparities: a US census tract analysis. Nicotine Tob Res. 2017;19(11):1338–1344. [DOI] [PubMed] [Google Scholar]
- 45.Giovenco DP, Spillance TE, Merizier JM. Neighborhood differences in alternative tobacco product availability and advertising in New York City: implications for health disparities. Nicotine Tob Res. 2019;21(7):896–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rose SW, Barker DC, D’Angelo H, et al. The availability of electronic cigarettes in US retail outlets, 2012: results of two national studies. Tob Control. 2014;23:iii10–iii16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hafez AY, Gonzalez M, Kulik MC, Vijayaraghavan M, Glantz SA. Uneven access to smoke-free laws and policies and its effect on health equity in the United States: 2000–2019. Am J Public Health. 2019;109(11):1568–1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Centers for Disease Control and Prevention. Tobacco Use by Geographic Region. Atlanta, GA; 2019. [Google Scholar]
- 49.Atkins LA, Oman RF, Vesely SK, Aspy CB, McLeroy K. Adolescent tobacco use: the protective effects of developmental assets. Am J Health Promot. 2002;16(4):198–205. [DOI] [PubMed] [Google Scholar]
- 50.Bauman KE, Koch GG, Lentz GM. Parent characteristics, perceived health risk, and smokeless tobacco use among white adolescent males. NCI Monogr. 1989;8:43–48. [PubMed] [Google Scholar]
- 51.Bombard JM, Pederson LL, Nelson DE, Malarcher AM. Are smokers only using cigarettes? Exploring current polytobacco use among an adult population. Addict Behav. 2007;32(10):2411–2419. [DOI] [PubMed] [Google Scholar]
- 52.Butler KM, Ickes MJ, Rayens MK, Wiggins AT, Hahn EJ. Polytobacco use among college students. Nicotine Tob Res. 2016;18(2):163–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Assari S, Mistry R, Bazargan M. Race, educational attainment, and e-cigarette use. J Med Res Innov. 2019;4(1):e000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Friedman AS, Horn SJL. Socioeconomic disparities in electronic cigarette use and transitions from smoking. Nicotine Tob Res. 2019;21(10):1363–1370. [DOI] [PubMed] [Google Scholar]
- 55.Jaber RM, Mirbolouk M, DeFilippis AP, et al. Electronic cigarette use prevalence, associated factors, and pattern by cigarette smoking status in the United States from NHANES (National Health and Nutrition Examination Survey) 2013–2014. J Am Heart Assoc. 2018;7(14):e008178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chang CM, Rostron BL, Chang JT, et al. Biomarkers of exposure among U.S. adult cigar smokers: Population Assessment of Tobacco and Health (PATH) study wave 1 (2013–2014). Cancer Epidemiology. Biomark Prev. 2019;28:943–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coleman BN, Rostron B, Johnson SE, et al. Electronic cigarette use among US adults in the Population Assessment of Tobacco and Health (PATH) study. Tobacco Control. 2017;26(e2):e117–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Brooks A, Gaier Larkin EM, Kishore S, Frank S. Cigars, cigarettes, and adolescents. Am J Health Behav. 2008;32(6):640–649. [DOI] [PubMed] [Google Scholar]
- 59.Cheng YC, Rostron BL, Day HR, et al. Patterns of use of smokeless tobacco in US adults, 2013–2014. Am J Public Health. 2017;107:1508–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kong G, Kuguru KE, Krishnan-Sarin S. Gender differences in U.S. adolescent e-cigarette use. Curr Addict Rep. 2017;4:422–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Odani S, Armour BS, Agaku IT. Racial/ethnic disparities in tobacco product use among middle and high school students — United States, 2014–2017. Morb Mortal Wkly Rep. 2018;67:952–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leventhal AM, Urman R, Barrington-Trimis JL, et al. Perceived stress and poly-tobacco product use across adolescence: patterns of association and gender differences. J Psychiatric Res. 2017;94:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Silveira ML, Green VR, Iannaccone R, Kimmel HL, Conway KP. Patterns and correlates of polysubstance use among US youth aged 15–17 years: wave 1 of the Population Assessment of Tobacco and Health (PATH) study. Addiction. 2019;114(5):907–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weaver SR, Kim H, Glasser AM, et al. Establishing concensus on survey measures for electronic nicotine and non-nicotine delivery system use: current challenges and considerations for researchers. Addict Behav. 2017;79:203–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hrywna M, Bover Manderski MT, Delnevo CD. Prevalence of electronic cigarette use among adolescents in New Jersey and association with social factors. J Am Med Assoc. 2020;3(2):e1920961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Erola J, Jalonen S, Lehti H. Parental education, class and income over early life course and children’s achievement. Res Soc Strat Mobil. 2016;44:33–43. [Google Scholar]
- 67.Lien N, Friestad C, Klepp KI. Adolescents’ proxy reports of parents’ socioeconomic status: how valid are they? J Epidemiol Commun Health. 2001;55:731–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gentzk AS, Creamer M, Cullen KA, et al. Vital signs: tobacco product use among middle and high school students — United States. Morb Mortal Wkly Rep. 2019;68:157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Butler KM, Hedgecock S, Record RA, et al. An evidence-based cessation strategy using rural smokers’ experiences with tobacco. Nurs Clin North Am. 2012;47(1):31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Northridge ME, Vallone D, Xiao H, et al. The importance of location for tobacco cessation: rural-urban disparities in quit success in underserved West Virginia counties. J Rural Health. 2008;24:106–115. [DOI] [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—2014. Atlanta, GA: National Center for Chronic Disease Prevention and Health Promotion; 2014. [Google Scholar]