Abstract
Background
Infrapatellar branch of the saphenous nerve lies subcutaneously and supplies the anterolateral aspect of knee below the patella. It is extremely susceptible to iatrogenic injuries during the surgeries around the knee, mainly total knee replacements (TKRs). Post operatively the patients present with localised area of numbness and in some instances a traumatic eczematous reaction termed autonomous denervation dermatitis (ADD) is witnessed, leading to skin manifestations that range from a simple rash to extensive lesions.
Methodology
A review of literature was conducted with search of relevant articles from Medline (PubMed), Embase, and Scopus which discussed eczematous skin lesions secondary to total knee replacements. Additionally, we noted studies which described these lesions in other surgeries around the knee like arthroscopies and fracture fixations.
Results
Eight studies including atleast one case after TKR were reviewed. There was only one cohort study while the remaining included case reports and small case series. There were 69 cases of ADD appearing after TKR. The appearance of the skin lesions was lateral to the incision in 30/34 operated knees and on both sides of the incision in four knees after TKRs. Bilateral lesions were seen in only six patients of TKRs. There was no functional limitation caused by these lesions and they resolved either spontaneously or after using topical steroids.
Conclusion
ADD is a relatively uncommonly reported complication of TKRs, which can reduce patient satisfaction and increase surgeon apprehension. Although all cases of nerve damage do not manifest as cutaneous lesions, steps to minimise the damage to the nerve intra operatively should be taken. The diagnosis requires a high index of suspicion, and should not be dispelled as a simple allergic reaction without adequate investigations. Patients should be counselled to alleviate unnecessary fear and apprehensions.
Keywords: Autosomal denervation dermatitis, ADD, SKINTED, Total knee replacements, Infra patellar branch, Saphenous nerve
Introduction
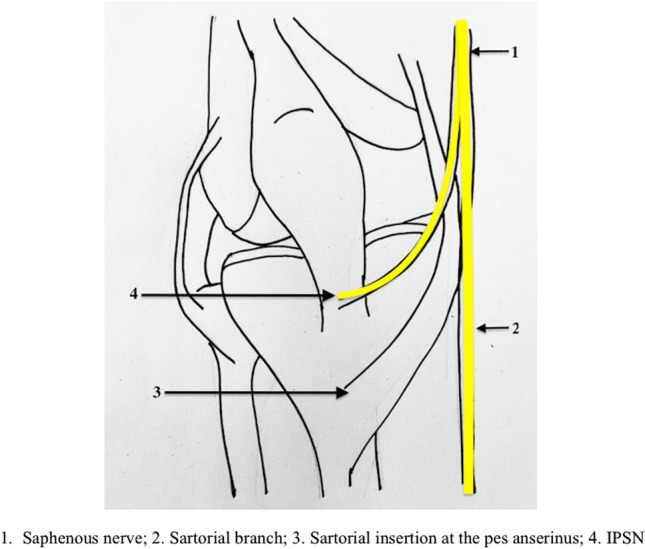
Knee surgeries, including total knee replacements (TKRs), are among the most common orthopaedic surgeries performed worldwide; TKRs, are mostly performed via a midline incision with medial parapatellar arthrotomy. The saphenous nerve after it branches off the femoral nerve extends distally, descending medial to the patellar tendon and gives off an infrapatellar branch through the adductor hiatus (IPSN), which becomes subcutaneous and goes from the medial to lateral side below the patella [1] (Fig. 1). Besides being subcutaneous, multiple anatomical variations in its course have also been documented, making the IPSN highly susceptible to iatrogenic insult; it is reportedly injured in up to 70% of cases with the use of midline incision for these surgeries [1–3]. The IPSN supplies sensations to the front of the knee, and the innervation may extend to the lateral aspect; its injury presents as localised numbness over the area supplied [1]. In addition to damage by midline incisions, there are occasional reports of IPSN injury even with knee arthroscopies, mainly when bone-patellar tendon bone (BPTB) grafts are used for cruciate reconstructions; rarely antero-medial portal placement or hamstring harvests have resulted in its injury [3].
Fig. 1.
Flow diagram for selection of studies including total knee replacements
Skin lesions after surgery have been reported around the TKR incisions; these can be a result of allergy from adhesive tapes, use of iodine solution for dressing and rarely due to metal hypersensitivity [4]. In recent times an entity in the form of “traumatic eczematous dermatitis” has also been reported, and has been called autonomic denervation dermatitis (ADD) or SKINTED (surgery of the knee, injury to infra patellar branch of the saphenous nerve, traumatic eczematous dermatitis), which occurs due to iatrogenic injury to the IPSN following midline incisions. Manifesting as cutaneous lesions, ADD can range from a simple rash to extensive eruptions, or even an excoriated zone of papules or macules [5] (Fig. 2). The lesions could be highly pruritic, and has been postulated to be a form of “traumatic eczema” which is often self-limiting, but causes significant dermal lesions; lack of awareness in both the patient and surgeon may be frightening to both the doctor and the patient. The probable mechanism behind this entity is disruption of the autonomic constituents of the skin, causing alternation in the microcirculation, which could aberrantly differentiate and proliferate keratinocytes causing these lesions [6]. Neuropeptides like neurotensin and substance P are released from the nerve ends, which are involved in hypersensitivity reactions and skin inflammatory cascade; this can be another potential mechanism [7].
Fig. 2.
Clinical pictures depicting skin lesions of autonomous denervation dermatitis after TKRs
The problem is that these lesions are often not recognized as what they are, and since these dermal lesions generally occur more than 2 weeks after the surgery, confusions in diagnosis manifest themselves; if undiagnosed, they may get secondarily infected, making early recognition and differentiation from other dermal complications necessary. Due to limited available literature, and often lack of awareness in the average surgeon, we conceptualized this systematic review to identify the reported cases of ADD in literature in relation with knee replacements, and discuss its incidence, management, and prevention.
Methodology
Search Strategy
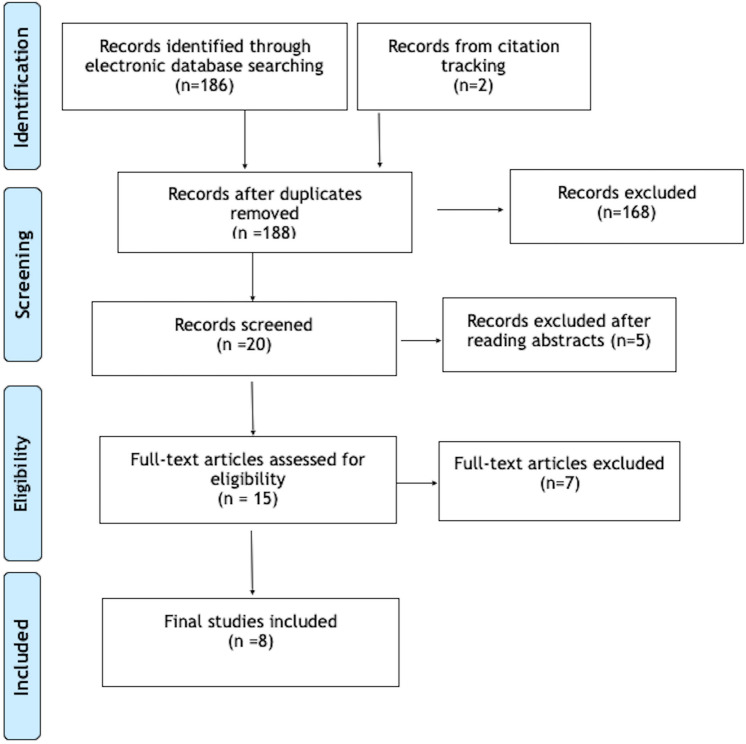
An electronic database search of Medline (PubMed), Embase, and Scopus was conducted from inception to 27th May 2021 with combinations of specific keywords (Table 1). This yielded a total of 186 hits. Seven articles were included from these hits. A secondary search from the bibliography of these included articles was done, which yielded one additional article (Fig. 3).
Table 1.
Search Strategy followed in the MEDLINE (PubMed), Embase and Scopus Databases
| Data bases | Key words used for search from inception to 27th May 2021 | Results |
|---|---|---|
| MEDLINE (PubMed) | (((((((((Total knee arthroplasty) OR (Total knee replacement)) OR (TKA)) OR (TKR)) AND (SKINTED)) OR (((((Total knee arthroplasty) OR (Total knee replacement)) OR (TKA)) OR (TKR)) AND (traumatic eczematous dermatitis))) OR ((Total knee arthroplasty) AND (Neuropathy dermatitis))) OR (((((Total knee arthroplasty) OR (Total knee replacement)) OR (TKA)) OR (TKR)) AND (autonomic denervation dermatitis))) OR (((((Total knee arthroplasty) OR (Total knee replacement)) OR (TKA)) OR (TKR)) AND (Dermatitis))) OR (((((knee arthroscopy) AND (dermatitis)) OR (("knee"[MeSH Terms] OR "knee"[All Fields] OR "knee joint"[MeSH Terms] OR ("knee"[All Fields] AND "joint"[All Fields]) OR "knee joint"[All Fields]) AND ("arthroscopy"[MeSH Terms] OR "arthroscopy"[All Fields] OR "arthroscopies"[All Fields]) AND "SKINTED"[All Fields])) OR ("knee"[All Fields] AND "arthroscopy"[All Fields] AND ("Neuropathy"[All Fields] AND "dermatitis"[All Fields]))) OR ("knee"[All Fields] AND "arthroscopy"[All Fields] AND ("Autonomic"[All Fields] AND "denervation"[All Fields] AND "dermatitis"[All Fields]))) | 64 |
| Embase | (total AND knee AND arthroplasty OR (total AND knee AND replacement)) AND skinted OR ((total AND knee AND arthroplasty OR (total AND knee AND replacement)) AND traumatic AND eczematous AND dermatitis) OR ((total AND knee AND arthroplasty OR (total AND knee AND replacement)) AND neuropathy AND dermatitis) OR ((total AND knee AND arthroplasty OR (total AND knee AND replacement)) AND autonomic AND denervation AND dermatitis) OR ((total AND knee AND arthroplasty OR (total AND knee AND replacement)) AND dermatitis) OR (knee AND arthroscopy AND dermatitis) | 84 |
| Scopus | (ALL (total AND knee AND arthroplasty) OR TITLE-ABS- KEY (total AND knee AND replacement) AND ALL (skinned)) OR (ALL (total AND knee AND arthroplasty) OR TITLE-ABS-KEY (total AND knee AND replacement) AND ALL (traumatic AND eczematous AND dermatitis)) OR (ALL (total AND knee AND arthroplasty) OR TITLE-ABS-KEY (total AND knee AND replacement) AND ALL ((autonomic AND denervation AND dermatitis))) | 38 |
| Total | 186 |
Fig. 3.
Diagrammatic representation of the course of infra patellar branch of the saphenous nerve
Inclusion and Exclusion Criteria
Studies of any design in the English language discussing eczematous skin lesion (including terms autonomic denervation dermatitis or SKINTED) secondary to total knee replacements were included. Additionally, we noted studies which described these lesions in other surgeries around the knee like arthroscopies and fracture fixations. Animal studies, conference abstracts, e-posters, and studies describing skin lesions not related to arthroplasties around the knee were excluded.
Data Collection and Extraction
All the hits were screened for inclusion by two authors independently based on titles and abstracts.
After reading full texts, studies with sufficient relevance to the topic were only included. Discussions among the authors resolved discrepancies.
The data extraction was performed from each included article and entered in a pre-specified data collection excel sheets, mentioning the name of the authors, year of publication, study design, number of patients/cases included, surgeries done in the past, location of skin lesions concerning incision, duration between surgery and the appearance of skin lesions, average time for complete healing, treatment given and the diagnostic tests done (Table 2). The risk of bias was assessed using the Methodological index for non-randomised studies (MINORS) [8].
Table 2.
Studies showcasing ADD in TKR patients
| Sl no. | Author/year | Study design | Number of cases of ADD in TKR | Age/sex | Site of skin lesion in relation to incision | Time since surgery to appearance of skin lesion | Mean time taken for complete healing lesion | Diagnostic tests done | Treatment | Knee function |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Satku et al. [9] | Case series | 4 (1 bilateral) | 71.33 ± 3.5 years; 2M/1F | Lateral to the incision-TKA | 5.5 ± 2.38 (4–9 months) | 8–12 months | Skin scraping for gram staining and culture; sweat test | Betamethasone ointment | NR |
| 2 | Verma et al. [14] | Case series | 55 (only 16 were available for regular follow-up) | NR; 11M/5F | Lateral in 12 and in 4 patients on both sides of incision | 3 weeks–4 months | NR | Skin scraping for gram staining and culture; patch test | Topical emollients and topical steroids | NR |
| 3 | Sharquie et al. [7] | Case series (6 patients of saphenous vein grafting) | 1 | 60 year F | Lateral to incision | 3 months | NR | NR | NR | NR |
| 4 | Madke et al. [6] | Case series (4 patients of saphenous vein grafting and 1 OR for fracture femur) | 5 |
60.8 ± 2.48 years; 3M/2F |
NR | 10 months–2 years | NR | Sweat test (starch–iodine test); patch test; biopsy | Topical moisturizers and topical steroids | NR |
| 5 | Barbera et al. [10] | Case report | 2 (1 bilateral) | 65 year M | Lateral to incision | 3 months | 6 months | Biopsy | Topical steroids | NR |
| 6 | Pathania et al. [13] | Case report | 2 (1 bilateral) | 60 year F | Lateral to incision | 3 months | 2 weeks for improvement | Skin scraping for gram staining and culture | NR | NR |
| 7 | Mathur et al. [11] | Case report | 4 (2 bilateral) | 54.5 ± 7.7 years; 1M/1F | NR |
Case 1–16 months Case 2–11 months |
NR | Biopsy | NR | NR |
| 8 | Nazeer et al. [12] | Prospective cohort study | 9 TKA out of 203 knees (1 bilateral) | 64.5 ± 7.03 years; 1M/7F | Lateral to incision | Mean 4 (3–6) months | 6.33 (4–10) weeks | Skin scraping for gram staining and culture; Biopsy | Topical steroids | Stable, mean KSS-90 (84–94)- in all |
TKR total knee replacement, KSS Knee Society Score, OR open reduction, NR not reported, ADD autonomic denervation dermatitis
Results
Eight studies were included in this review which described ADD in Orthopaedic knee surgeries, which included at least 1 case after TKRs [6, 7, 9–14]. 1 study reported a case after knee arthroscopy [15]. Three of these studies [7, 10, 13] reported single cases, while the other five studies reported on 2–55 cases [6, 9, 11, 12, 14] making a total of 82 overall cases available for review from the literature. Verma et al. [14] noted ADD in 55 of their patients, however only 16 of these patients were followed up. 69 cases (84.1%) were documented in TKRs, with the problem also documented in one arthroscopic meniscectomy, one patellar chondroplasty, 10 saphenous vein grafts and 1 case of distal femur fracture fixation.
The appearance of the skin lesion after TKRs was lateral to the incision in 30/34 operated knees and on both sides of the incision in 4 knees. Bilateral lesions were seen in only 6 patients of TKR. The mean time of appearance of the lesions from surgery was 6.56 ± 5.68 months (range 3 weeks–2 years). The time to complete healing of lesion was documented in only 17 cases from 4 studies, with mean of 4.15 ± 6.05 months (range 2 weeks–1 year). 5 studies reported the use of local steroid cream for the treatment of the lesions. None of the cases had any history of any topical agent/allergen contact in pre-operative or post-operative period or any metal allergy.
ADD was a diagnosis of exclusion, however the previous authors had used various techniques to identify the cause of these dermal lesions. These included gram staining from skin scrapings (4 studies), patch test for contact allergy (2 studies), starch–iodine test for lack of sweating (2 studies) and biopsies which showed dense lymphocytic infiltrates with no acute inflammatory cells (4 studies).
Risk of Bias
The overall risk of bias was high in the included studies (Table 3). This could be due to the low awareness of this entity with low quality of studies with limited evidence.
Table 3.
MINORS tool for risk of bias
| Study | Clearly stated aim | Inclusion of consecutive patients | Prospective data collection | Endpoints appropriate to study aim | Unbiased assessment of study endpoint | Follow-up period appropriate to study aim | < 5% lost to follow-up | Prospective calculation of study size | Total |
|---|---|---|---|---|---|---|---|---|---|
| Satku et al. [9] | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 0 | 10/16 |
| Verma and Mody [14] | 1 | 0 | 1 | 2 | 1 | 2 | 1 | 0 | 8/16 |
| Sharquie et al. [7] | 2 | 1 | 2 | 2 | 1 | 1 | 2 | 0 | 11/16 |
| Madke et al. [6] | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0 | 11/16 |
| Barbera et al. [10] | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 0 | 10/16 |
| Pathania and Singh [13] | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 0 | 10/16 |
| Mathur and Sharda [11] | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 11/16 |
| Nazeer et al. [12] | 2 | 1 | 2 | 2 | 1 | 2 | 2 | 0 | 12/16 |
Discussion
The IPSN is reported as very often compromised during knee surgeries due to its subcutaneous course, with the reported incidence of iatrogenic injuries ranging from 22 to 70% [1, 12]. The published literature on this cutaneous entity, labelled ADD however is limited, as we found only 82 documented cases, mostly as case reports or small case series. It was noted that the overall documentation of ADD after ISPN injuries is low, and one possible reason for this could be under reporting due to lack of awareness of the condition among the Orthopaedic surgeons. In terms of incidence in association with TKRs, there is lack of data in the literature; only one study by Nazeer et al. has been a prospective cohort study and has reported an incidence of 4.4%. Other publications have only reported case reports of patients with these findings of ADD; other reasons of low reporting of ADD as an entity could be the tendency to confuse it with other commoner skin changes related to allergies or dryness after TKRs [10]. However, the conditions can be easily differentiated, with ADD being more location-specific; most ADD cases are localized at the inferolateral aspect of the knee along with numbness in ISPN distribution; this numbness usually resolves with re-innervation of the area by the surrounding neural structures.
A point of note is that although the IPSN injury is relatively common, only a small subset report skin lesions, as seen in the present review. There is no suitable explanation for this as to why some develop ADD and many do not, as the available literature and the authors’ personal experience are limited. The probable theory behind this phenomenon may be the extent of nerve damage, wherein a larger incision of a TKR with some crushing component due to retraction, may lead to more chances of developing ADD, compared to a relatively straightforward smaller incision in BPTB or hamstring grafting. However, this purely is conjecture with limited evidence in literature and there is need to assess probable factors that may make one particular case more prone to develop these skin lesions than another. Similar traumatic eczematous skin lesions have also been occasionally documented in areas of numbness or scar tissue in amputation stumps, carpal tunnel syndrome and trigeminal neuralgia due to self-manipulation, but again not all cases develop these and associated factors need to be ascertained [16, 17].
It is important to distinguish ADD from a hypersensitivity reaction to iodine or dressing patches; these tend to be localised to the application area only, could be anywhere around the knee and are not associated with sensation loss. Metal hypersensitivity reaction, which is more generalized, is present all around the knee and could be associated with swelling and fluid formation. Moreover, ADD tends to resolve spontaneously, while a metal hypersensitivity reaction would persist, and often may require implant removal. A careful history can elicit the susceptibility of these patients for these skin changes. Moreover, these hypersensitivity cases would tend to be bilateral if both knees are operated on. On the other hand, reports of bilateral ADD are rare, with only 6 bilateral knees noted in our review. This could be explained by anatomical variations in the course of the nerve between the two limbs, which maybe the cause of damage to the nerve in one knee being more than on the opposite side [14]. It is pertinent to comment that all of these ISPN injuries do not lead to ADD, and 1 or both the knees may be spared, for unknown reasons.
Up to 20% of patients of TKR have been reported to be dissatisfied with TKRs, mostly due to limitations in kneeling and function [19]. Although these skin lesions do not cause any significant effect on knee function per se, as they tend to either self-resolve over time or resolve with topical steroids after diagnosis [14], these could nevertheless cause dissatisfaction, undue stress and mental agony for the patients, which could be worse in cases who develop significant pruritus, or a secondary skin infection. This could even cause some deficiency in the rehabilitation of the knee that can hamper recovery [19]. This could be a cause of unnecessary worry and stress even in the surgeons who may be unaware of this rare complication. Therefore, it is hoped that this review, which is the first on this subject, would increase awareness and allow prompt diagnosis and effective treatment; adequate patient counselling is needed to allay patient apprehension.
All cases presenting with the classical lesions of well-defined plaques or scaly papules with or without itchiness and crusting should be viewed with high suspicion for ADD, especially with co-existent or previous numbness after knee surgery; however other allergies and infections should be looked at and ruled out. A biopsy from the lesion can help with the diagnosis, but the classical history and location with high suspicion are of more importance, and early collaboration with a dermatologist can dispel the patient's dissatisfaction and provide early resolution. Some studies [6, 10–12] have even done biopsy from the dermal lesions, and have found these lesions to be consistent with chronic spongiotic dermatitis showing dense lymphocytic infiltrate with no acute inflammatory cells.
In terms of preventing this condition, the aim should be at minimising the iatrogenic injury to the nerve, which begins this cascade leading to the skin lesions. In a cadaveric study by Tifford et al. [20], it has also been reported that the nerve moves distally with knee flexion. One option therefore is to make the anterior incision with the knees flexed initially, to avoid the IPSN damage. In TKR surgeries, alternatives to medial parapatellar approach like lateral arthrotomy may be looked at to avoid this injury [1]; anterolateral skin incisions have lesser chances of injuring the nerve than the midline and anteromedial incisions [21, 22]. Careful lookout and dissection for the nerve subcutaneously can be attempted to minimise the chances of injury, and undue pressure from the medial retractor should be avoided.
Steps to prevent damage to IPSN have been described for hamstring graft harvesting, which include the utilisation of an oblique incision (injury in 27.6%) instead of vertical (64.7%) or horizontal (50%) and harvesting of only semitendinous (injury in 36%) instead of bitendinous (semitendinous and gracilis) grafts (58%) in ligament reconstruction surgeries [23]. A modified oblique incision has also been described by Zhu et al. [23] to minimise the nerve damage and provide higher subjective satisfaction. The classical oblique incision is placed at three finger breadths distal to the joint line and 1–2 cm distal and medial to the tibial tuberosity. Zhu et al. [23] described the nerve's inner and inferior low-risk area as a triangle with its sides formed from a vertical line dropped from the inner edge of the proximal tibia and a sleeping line medially from the tibial tubercle. The zone lies distal to the midpoint of the vertical line and medial to 1/3rd point of the sleeping line. The modified oblique incision should start from the midpoint of the line connecting these two points, extending distally and anteriorly [18].
Overall our evaluation of the limited data in literature could not give the actual incidence of traumatic eczematous dermatitis after TKRs; the associated causative factors have been identified to some extent, but adequate awareness is limited. It is hoped that this review will make surgeons aware of this ‘ADD’itional complication after TKR, which although is self-limiting but can be a cause undue stress and dissatisfaction for the patient as well as the treating surgeon.
Conclusion
ADD is a rarely reported entity that can influence the post-operative course after TKR in the form of reduced patient satisfaction and surgeon apprehension; it however does not compromise knee function. Steps to minimise the damage to the nerve should be taken during these surgeries. The diagnosis requires a high index of suspicion, and should not be dispelled as a simple allergic reaction without adequate investigations. Proper preoperative counselling with adequate postoperative monitoring can help to achieve an overall satisfactory outcome.
Author Contributions
MSD: Conception of idea and editing. KJ: Data Analysis and Preparation of manuscript. VDS: Final review and editing of manuscript. PK: Preparation of manuscript. RKR: Review of literature.
Funding
Nil.
Availability of Data and Material
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Code Availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
Our study is a review article and does not include any human or animal participation. So we did not require ethical approval.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mandeep Singh Dhillon, Email: drdhillon@gmail.com.
Karan Jindal, Email: karan.121@hotmail.com.
Vijay D. Shetty, Email: vijaydshetty@gmail.com
Prasoon Kumar, Email: drprasoonksingh@gmail.com.
Rajesh Kumar Rajnish, Email: duktiraj@gmail.com.
References
- 1.Thomas Ackmann M, Monika Von Düring M, Wolfram Teske M, Ole Ackermann M, Peter Müller M, Von Schulze C, Pellengahr M. Anatomy of the infrapatellar branch in relation to skin incisions and as the basis to treat neuropathic pain by percutaneous cryodenervation. Pain Physician. 2014;17:E339–E348. doi: 10.36076/ppj.2014/17/E339. [DOI] [PubMed] [Google Scholar]
- 2.Kalthur SG, Sumalatha S, Nair N, Pandey A, Sequeria S, Shobha L. Anatomic study of infrapatellar branch of saphenous nerve in male cadavers. Irish Journal of Medical Science (1971-) 2015;184(1):201–206. doi: 10.1007/s11845-014-1087-2. [DOI] [PubMed] [Google Scholar]
- 3.Kerver A, Leliveld M, den Hartog D, Verhofstad M, Kleinrensink GJ. The surgical anatomy of the infrapatellar branch of the saphenous nerve in relation to incisions for anteromedial knee surgery. JBJS. 2013;95(23):2119–2125. doi: 10.2106/JBJS.L.01297. [DOI] [PubMed] [Google Scholar]
- 4.Chalmers BP, Melugin HP, Sculco PK, Schoch JJ, Sierra RJ, Pagnano MW, Stuart MJ, Taunton MJ. Characterizing the diagnosis and treatment of allergic contact dermatitis to 2-octyl cyanoacrylate used for skin closure in elective orthopedic surgery. Journal of Arthroplasty. 2017;32(12):3742–3747. doi: 10.1016/j.arth.2017.07.012. [DOI] [PubMed] [Google Scholar]
- 5.Mistry D, O'Meeghan C. Fate of the infrapatellar branch of the saphenous nerve post total knee arthroplasty. ANZ Journal of Surgery. 2005;75(9):822–824. doi: 10.1111/j.1445-2197.2005.03532.x. [DOI] [PubMed] [Google Scholar]
- 6.Madke B, Mhatre M, Kumar P, Singh AL, Patki A. Autonomic denervation dermatitis: A new type of eczematous dermatitis. Clinical Dermatology Review. 2017;1(2):61. doi: 10.4103/CDR.CDR_8_17. [DOI] [Google Scholar]
- 7.Sharquie KE, Noaimi AA, Alaboudi AS. Neuropathy dermatitis following surgical nerve injury. Case Reports in Dermatological Medicine. 2011;2011:1–3. doi: 10.1155/2011/234185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ Journal of Surgery. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 9.Satku K, Fong P, Kumar V, Lee Y. Dermatitis complicating operatively induced anesthetic regions around the knee. A report of four cases. JBJS. 1993;75(1):116–118. doi: 10.2106/00004623-199301000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Barbera J, van der Ven A, Amjad I. Bilateral neuropathy dermatitis following simultaneous bilateral total knee arthroplasty: A case report. JBJS Case Connector. 2018;8(2):e23. doi: 10.2106/JBJS.CC.17.00174. [DOI] [PubMed] [Google Scholar]
- 11.Mathur D, Sharda S (2019) Autonomic denervation dermatitis in two patients. Indian Journal of Clinical Dermatology, 2(03),96-7.
- 12.Nazeer M, Ravindran R, Katragadda BC, Muhammed EN, Rema DT, Muhammed MN. SKINTED: A rare complication after total knee arthroplasty. Arthroplasty Today. 2020;6(4):1028–1032. doi: 10.1016/j.artd.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pathania YS, Singh S. SKINTED: An autonomic denervation dermatitis. International Journal of Dermatology. 2020;59(5):613–614. doi: 10.1111/ijd.14572. [DOI] [PubMed] [Google Scholar]
- 14.Verma S, Mody B. Explaining a hitherto nameless condition: ‘SKINTED’. Clinical and Experimental Dermatology: Viewpoints in Dermatology. 2009;34(7):e465–e466. doi: 10.1111/j.1365-2230.2009.03522.x. [DOI] [PubMed] [Google Scholar]
- 15.Logue EJ, III, Drez D., Jr Dermatitis complicating saphenous nerve injury after arthroscopic debridement of a medial meniscal cyst. Arthroscopy: The Journal of Arthroscopic and Related Surgery. 1996;12(2):228–231. doi: 10.1016/S0749-8063(96)90017-1. [DOI] [PubMed] [Google Scholar]
- 16.Bove D, Lupoli A, Caccavale S, Piccolo V, Ruocco E. Dermatological and immunological conditions due to nerve lesions. Functional Neurology. 2013;28(2):83. doi: 10.11138/FNeur/2013.28.2.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cassler NM, Burris AM, Nguyen JC. Asteatotic eczema in hypoesthetic skin: A case series. JAMA Dermatology. 2014;150(10):1088–1090. doi: 10.1001/jamadermatol.2014.394. [DOI] [PubMed] [Google Scholar]
- 18.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clinical Orthopaedics and Related Research. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Padua VBCd, Nascimento PED, Silva SC, Canuto SMdG, Zuppi GN, Carvalho SMRd. Saphenous nerve injury during harvesting of one or two hamstring tendons for anterior cruciate ligament reconstruction. Revista brasileira de ortopedia. 2015;50:546–549. doi: 10.1016/j.rbo.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tifford CD, Spero L, Luke T, Plancher KD. The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for anterior cruciate ligament surgery: An anatomic study. The American Journal of Sports Medicine. 2000;28(4):562–567. doi: 10.1177/03635465000280042001. [DOI] [PubMed] [Google Scholar]
- 21.Maniar RN, Singhi T, Nanivadekar A, Maniar PR, Singh J. A prospective randomized study in 20 patients undergoing bilateral TKA comparing midline incision to anterolateral incision. Journal of Orthopaedics and Traumatology. 2017;18(4):325–333. doi: 10.1007/s10195-017-0444-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsukada S, Kurosaka K, Nishino M, Hirasawa N. Cutaneous hypesthesia and kneeling ability after total knee arthroplasty: A randomized controlled trial comparing anterolateral and anteromedial skin incision. The Journal of Arthroplasty. 2018;33(10):3174–3180. doi: 10.1016/j.arth.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 23.Zhu B, Li X, Lou T. A modified oblique incision in hamstring tendon graft harvesting during ACL reconstruction. Journal of Orthopaedic Surgery and Research. 2021;16(1):1–8. doi: 10.1186/s13018-020-02056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Not applicable.