Abstract
Dual-mobility (DM) articulations are increasingly utilized to prevent or manage hip instability after total hip arthroplasty (THA). DM cups offer enhanced stability due to the dual articulation resulting in larger jump distance and greater range of motion before impingement. Improvement in design features and biomaterials has contributed to increased interest in dual-mobility articulations due to lower risk of complications compared to their historic rates. The incidence of implant-specific complications like intra-prosthetic dislocation (IPD) and wear has reduced with newer-generation implants. DM THAs are used in primary THA in patients with high risk for dislocation, e.g. neuromuscular disorder, femoral neck fracture, spinopelvic deformity, etc. They offer an attractive alternative option to constrained liner for treatment of hip instability in revision THA. The medium- to short-term results with DM THA have been encouraging in primary and revision THA. However, there are concerns of fretting, corrosion and long-term survivorship with DM THA. Hence, longer-term studies and surveillance are required for the safe use of DM THA in clinical practice.
Keywords: Dual-mobility, Total hip arthroplasty, Instability, Complications
Introduction
Total hip arthroplasty is one of the most successful and cost-effective procedures in orthopedics [1, 2]. Despite advances in techniques and biomaterials, instability remains one of the major and common postoperative complications necessitating revision procedure. The incidence of dislocation after primary total hip arthroplasty can vary from 1 to 6% depending upon indication, risk factors and approach [3]. Instability can be multifactorial, and several strategies have been recommended to mitigate its incidence. Besides recommendations in surgical approaches and technique (e.g. capsular closure), certain prosthetic options like large femoral heads and constrained liners have been traditionally utilized to prevent or treat hip instability after total hip arthroplasty.
Recently, there has been increased interest in dual-mobility articulations for total hip arthroplasty (THA) to address the issue of hip instability. Dual-mobility (DM) cups offer increased stability by virtue of their dual articulation resulting in larger jump distance and greater range of motion before impingement. It has gained widespread acceptance and appears to be one of the major current strategies for prevention and treatment of hip instability [4, 5]. The number of DM THAs performed in the United States and Europe have increased incrementally over the last decade [6]. Dual-mobility cups have been utilized in primary THA in patients for high risk of dislocation, e.g. neuromuscular disorder, femoral neck fracture, spinopelvic deformity, etc. It is performed in revision scenarios to treat or prevent instability in anticipated high-risk patient population.
In view of growing interest on this topic, we elected to review its history, biomechanics, indications and outcomes in primary and revision THA, complications and concerns associated with DM articulations.
Historical Background
Bosquet pioneered the development of DM designs in 1970s in an effort to reduce the risk of instability following total hip arthroplasty. His initial designs incorporated low friction arthroplasty principle of John Charnley and the concept of inherent stability of larger heads proposed by Mckee [7, 8]. The first-generation DM cups composed of cementless metallic acetabular shell and a mobile polyethylene liner that captured prosthetic femoral head. Press fit fixation of those acetabular cups was achieved by pegs driven into pubis and ischium with alumina surface coating and a dome screw [9]. However, the first-generation designs were associated with risk of delamination and loosening. Additionally, there were several reports of intra-prosthetic dislocation (IPD) with older implant designs [10, 11]. This complication is unique to dual-mobility constructs secondary to failure of retentive mechanism between the mobile polyethylene liner and head leading to direct articulation of the head and shell. It was attributed to polyethylene wear as well as some design features of the construct. The combination of design and biomaterial improvements has contributed to reduction of implant-related failures with current generation of DM constructs [12, 13].
Dual-mobility implants have been available in US following food and drug administration (FDA) approval of its first design in 2009. Variations of this concept have been used clinically in Europe for last 35 years. The improvement in surface coating (e.g. Hydroxyapatite, titanium plasma spray) of the acetabular cups lends themselves to better osteointegration, thus reducing the risk of loosening. Newer designs have been modified to include provision for screw fixation which can aid to improve initial mechanical fixation of the acetabular cup. Furthermore, modifications of the femoral neck in the form of thin and polished neck have helped with reduction of impingement around the edges of the mobile polyethylene insert. The use of skirted femoral heads is discouraged to prevent impingement and hence IPD. Finally, the introduction of highly crosslinked polyethylene in early 2000s has been associated with very low wear rates in long-term clinical studies for standard bearings in total hip arthroplasty [14]. Laboratory studies of highly crosslinked polyethylene in DM constructs have shown encouraging results with low wear rates even in adverse conditions [15, 16]. This can reduce the incidence of late IPD attributed to polyethylene liner wear in the previous generation of the implants.
The newer designs utilize cobalt alloy bearing as opposed to stainless steel which was widely used historically in Europe. The stainless-steel bearings (Polar cup) offer advantage of cemented fixation for complex acetabular reconstruction in revision scenarios. Additionally, there are some subtle variations in implant design and biomaterials between different manufacturers, e.g. anatomic (right and left implants) components with cutout to prevent psoas impingement (Restoration) (Fig. 1), Vit E-infused polyethylene which has shown to reduce wear in stimulated studies (Fig. 2).
Fig. 1.

Stryker dual mobility implant A MDM and B anatomic (ADM)
Fig. 2.

Zimmer Biomet dual-mobility system (cup, metal liner, Vit E mobile poly and head)
Biomechanics of Dual Mobility
Dual-mobility cup designs comprise two main articulations: primary between the prosthetic femoral head and mobile polyethylene and secondary articulation between outer surface of mobile bearing and the metallic acetabular cup. Additional less conspicuous articulation has been described between the rim of the mobile liner and the neck. The primary articulation is engaged during majority of activities of daily livings, whereas the secondary articulation is engaged with activities that exceed normal range of motion (Fig. 3). The dual articulations permit greater range of motion, superior head-to-neck ratio and large jump distance (the magnitude of lateral femoral translation required to dislocate the prosthetic hip joint) reducing the risk of dislocation [17]. Design improvements including chamfered polyethylene and low-profile polished neck can theoretically reduce impingement concerns with DM cups. Terrier et al conducted a comparative biomechanical study between standard, constrained and DM acetabular constructs using finite element analysis [18]. They noted highest range of motion to impingement with DM construct compared to conventional and constrained designs. Furthermore, DM constructs demonstrated lower resistive torque during subluxation events and lower stress on the polyethylene and at the implant–bone interface.
Fig. 3.
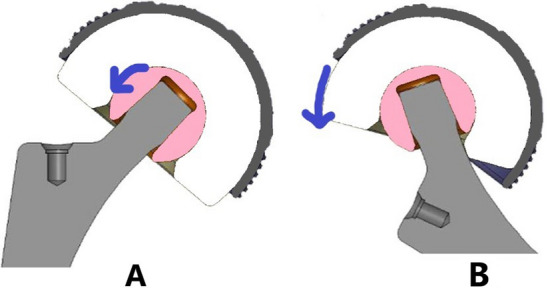
Biomechanics: A primary between the prosthetic femoral head and mobile polyethylene and B secondary articulation between outer surface of mobile bearing and the metallic acetabular cup
Primary Total Hip Arthroplasty
DM hip arthroplasty appears to have gained popularity in patients with high risk for hip instability following total hip arthroplasty. Patients at increased risk for instability include those undergoing THA with spinopelvic deformity, neuromuscular disorder, femoral neck fractures and tumor resection. The results of contemporary DM articulations have been encouraging in high-risk patients [13].
(1) DM in femoral neck fractures: hip fractures are one of the most common injuries treated by orthopedic surgeons worldwide. Historically, displaced femoral neck fractures in elderly have been treated with hemiarthroplasty (HA) versus total hip arthroplasty. There have been concerns of hip instability with THA in this patient population and inferior functional outcomes with HA [19]. DM total hip arthroplasty is an attractive option for surgeons wanting to maximize functional outcome while reducing dislocation rates. Several large-scale studies and registry data have demonstrated good clinical outcome with low dislocation rates in patients undergoing DM THA for femoral neck fractures [13, 19]. Furthermore, DMTHA is a good option as a salvage procedure for failed fixation of hip fractures [20]. Long-term studies are required to validate its widespread use in this patient population.
(2) DM in fixed spinopelvic alignment: there is increasing evidence of higher rates of dislocations in patients with fixed spinopelvic alignment undergoing THA [21, 22].The alterations in spinopelvic mechanics and ante inclination with loss of compensatory mechanisms in these patients put them at higher risk for dislocation with change of posture. Recommendations to tackle this issue include patient-specific functional zone placement of acetabular component and consideration of DM implants. Nessler et al. reported encouraging results in a multicenter study on 93 patients who underwent DMTHA with prior history of instrumented spine fusion. There were no cases of instability at a mean follow-up of 2.7 years [23].
(3) DM in patients with neuromuscular disorders: patients with cerebral palsy and acquired neuromuscular disorder, e.g. parkinsonism, traumatic brain injury are at increased risk of dislocation following THA with standard bearings [24, 25]. Anterior surgical approaches and use of constrained implants are some of measures recommended to mitigate the risk of instability in these patients [26]. DM THA is also an effective option in patients with neuromuscular disorders. Harwin et al. reported results on group of patients with neuromuscular disorders at a mean follow-up of 3.3 years [27]. There were no dislocations in this patient cohort. Few other studies have demonstrated promising results in these patients with unique challenges [28, 29]. There is limited evidence on the use of DM articulations in patients with neuromuscular disorders and further long-term studies are necessary to substantiate its benefit in these patients.
Revision Hip Arthroplasty
Historically, the risk of recurrent dislocation has been greater after revision THA than primary surgery. The reported incidence of instability following revision THA varies from 2 to 11% [30]. In the past, constrained liners were frequently used implants for treatment of hip instability. However, they were associated with high failure rates [31]. DM constructs appear to be a viable option for revision procedures for the management of hip instability following primary THA with lower failure rates compared to constrained liners. Contemporary modular dual-mobility implants provide option of adjunct multiple screw fixation in compromised bone stock in complex revision cases. Furthermore, certain dual-mobility metal liners (e.g. polar cup) can be cemented into revision acetabular constructs, thus reducing the risk of potential instability in some of those challenging revision procedures (Fig. 4).
Fig. 4.
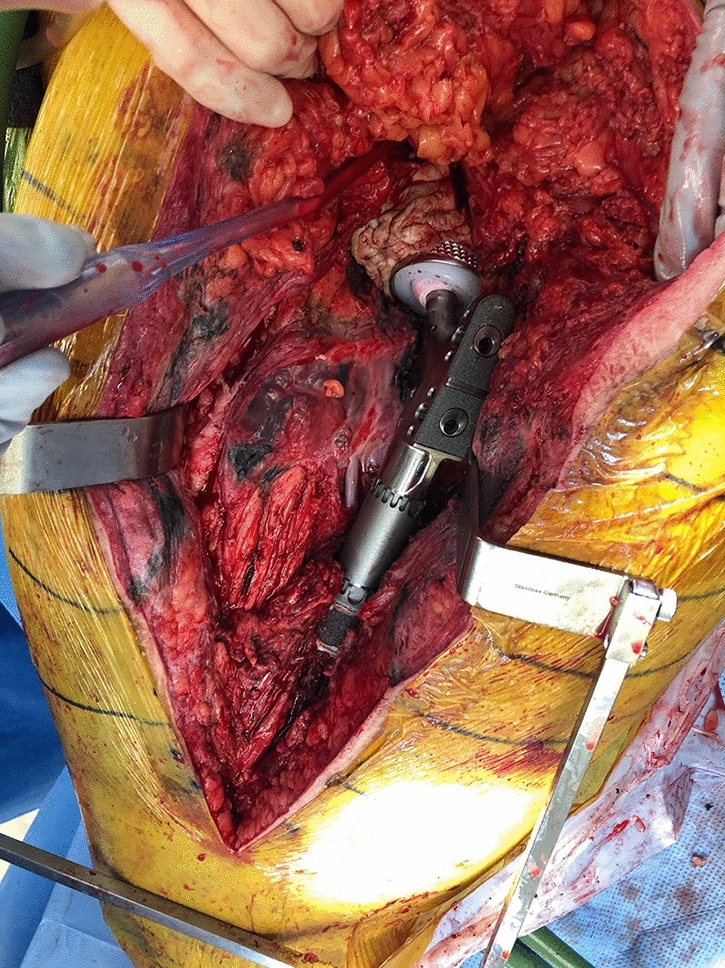
Intraoperative photograph of cemented dual-mobility liner in revision THA
Several of these factors make dual-mobility constructs an attractive option in revision scenarios. Multiple studies have demonstrated excellent outcomes with regard to low rates of aseptic loosening and dislocation in revision THA [32–35]. Chalmers et al compared the rates of dislocation and survival of large heads (36 mm and greater) with dual-mobility constructs in the conversion of THA after hip hemiarthroplasty. They reported lower dislocation rates for the dual-mobility construct group at 2-year follow-up [34]. Similarly, Wegrzyn et al. reported a dislocation rate of 1.5% at 7.3 years in a large study on 994 revision dual-mobility constructs [35]. Finally, it has proved to be highly effective strategy for treatment of recurrent hip instability [5].
Complications and Concerns
IPD and dislocation of the DMTHA are some of the common complications seen with this implant (Figs. 5, 6). Additionally, there have been recent concerns of metal liner interface corrosion and stem notching leading to raised metal ion levels.
Fig. 5.
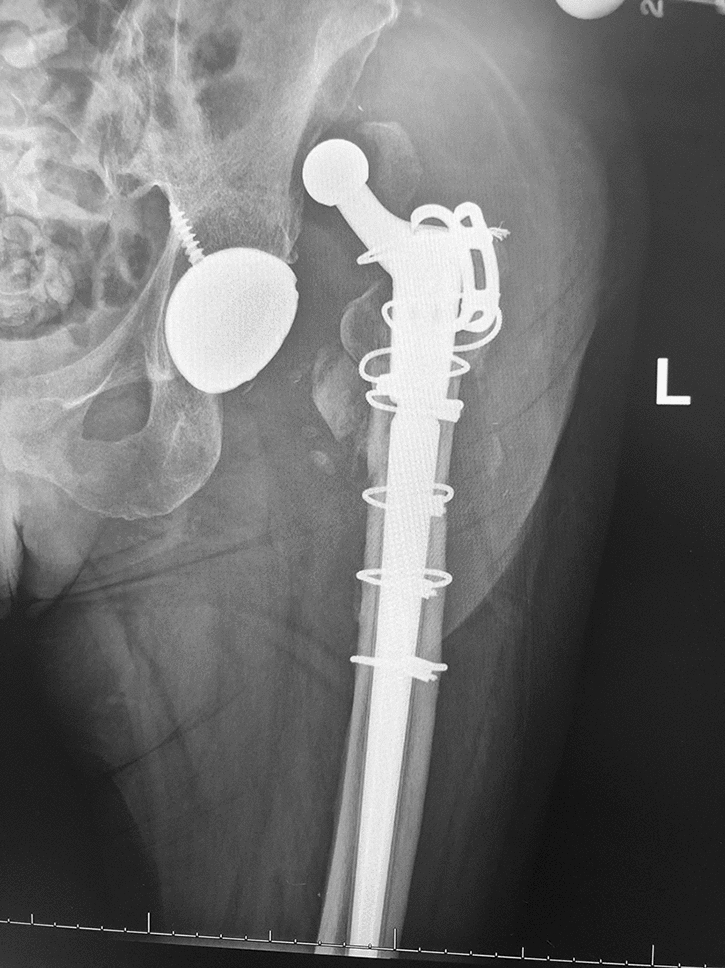
Radiograph of dislocated DM THA
Fig. 6.
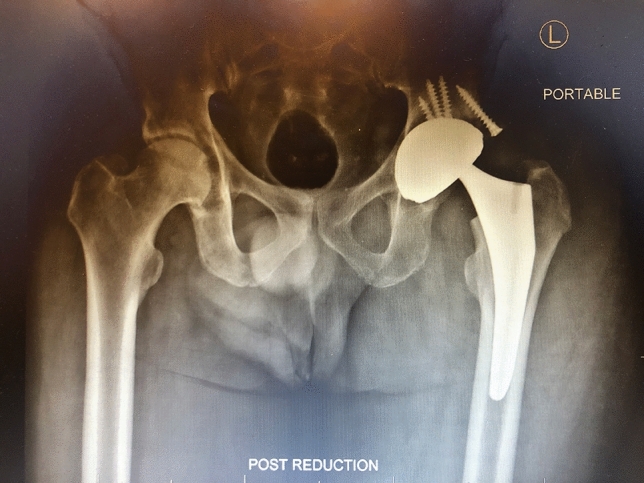
Radiograph of intra-prosthetic dislocation following closed reduction of DM THA. Note the eccentric position of the head in the cup
(A) Intra-prosthetic dislocation: intra-prosthetic dislocation is a unique and disconcerting complication associated with dual-mobility articulation THA [11]. It is characterized by disengagement of the mobile polyethylene liner from the head resulting in direct articulation of prosthetic head with the acetabular cup. It may be insidious or of sudden onset associated with hip pain and shortening in the lower extremity. Radiographic findings are subtle with eccentric positioning of the head (Fig. 6) and radiolucent bubble sign in the vicinity of the greater trochanter and acetabulum. High index of suspicion should be maintained for diagnosis of this entity.
The incidence of IPD is much lower with newer-generation of DM constructs [36]. However, there have been recent reports of IPD after closed reduction of dislocated DM THA. Addona et al reported a case series of IPDs following closed reduction of DM THA. [37] It may have been related to loss of retentive mechanism during forceful manipulation during closed reduction. They recommended closed reduction in operating room under regional or general anesthesia and the use of fluoroscopy to potentially avoid this complication. Typically, acute IPD can be managed with bearing exchange whereas chronic cases with metallosis may require component revision.
(B) Raised metal ion levels: there have been concerns of raised metal ion levels with modular DM implants. Gkiatis et al analyzed 248 DM THA performed using cobalt chromium liners [38]. They noted elevated serum cobalt ions in 5.2% of patients at a mean follow-up of 27.4 months. There was a trend towards reduction in metal ion levels between 1 and 2 years and no patients were revised for metal ion-related complications. The use of ceramic head for metal head may help to mitigate metal ion release [38, 39]. Besides malseating of the metal liner should be avoided by meticulous technique to avoid corrosion at modular metal interface [40].
There are recent case reports of femoral stem notching with DM THA [41]. It was noted to occur with titanium stems and attributed to impingement which could be multifactorial in nature. This can lead to high metal ion levels and or catastrophic stem fracture. Hence, close surveillance of DM THA implants over long term is critical with its widespread use.
Conclusion
There has been renewed interest in DM THA primarily due to its potential benefit in prevention and management of instability in high-risk patient population. The indications for DM THA have expanded to different clinical scenarios, e.g. spinopelvic deformity and femoral neck fractures in addition to management of hip instability. DM THA has demonstrated significant reduction in dislocation rates compared to conventional bearings in both primary and revision THA. There may be added theoretical advantages of reduction in wear rates and implant loosening with DM THA. It is critical to have thorough knowledge of the nuances of different implant designs available in the market so that it can be used in appropriate clinical setting. Several studies have shown lower incidence of IPD with the new-generation implants. However, there are concerns of fretting, corrosion and survivorship in younger patients undergoing DM THA. Hence, further long-term studies and surveillance are required for the safe use of DM THA in clinical practice.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Austin MS, Higuera CA, Rothman RH. Total hip arthroplasty at the Rothman institute. HSS Journal. 2012;8(2):146–150. doi: 10.1007/s11420-012-9268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gilson M, Gossec L, Mariette X, Gheriss D, Guyot MH, Berthelot JM. NIH consensus conference: total hip replacement. NIH consensus development panel on total hip replacement. The Journal of the American Medical Association. 1995;273(24):1950–1956. doi: 10.1001/jama.1995.03520480070043. [DOI] [PubMed] [Google Scholar]
- 3.Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. The Journal of Bone and Joint Surgery-American Volume. 2009;91(1):128–133. doi: 10.2106/JBJS.H.00155. [DOI] [PubMed] [Google Scholar]
- 4.Giacomo P, Giulia B, ValerioVincenzoPierluigi PSA. Dual mobility for total hip arthroplasty revision surgery: A systematic review and metanalysis. SICOT J. 2021;7:18. doi: 10.1051/sicotj/2021015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Romagnoli M, Grassi A, Costa GG, Lazaro LE, Presti ML, Zaffagnini S. The efficacy of dual-mobility cup in preventing dislocation after total hip arthroplasty: A systematic review and meta-analysis of comparative studies. International Orthopaedics. 2019;43(5):1071–1082. doi: 10.1007/s00264-018-4062-0. [DOI] [PubMed] [Google Scholar]
- 6.The American Joint Replacement Registry. (2020). https://www.aaos.org/registries/publications/ajrr-annual-report/2020
- 7.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. Journal of Bone and Joint Surgery. British Volume. 1972;54:61–76. doi: 10.1302/0301-620X.54B1.61. [DOI] [PubMed] [Google Scholar]
- 8.McKee GK, Watson-Farrar J. Replacement of arthritic hips by the McKee–Farrar prosthesis. Journal of Bone and Joint Surgery. British Volume. 1966;48:245–259. doi: 10.1302/0301-620X.48B2.245. [DOI] [PubMed] [Google Scholar]
- 9.Bousquet G, Argenson C, Godeneche JL, Cisterne JP, Gazielly DF, Girardin P, Debiesse JL. Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet’s cementless prosthesis: apropos of 136 cases. Revue de chirurgie orthopedique et reparatrice de l'appareil moteur. 1986;72:70–74. [PubMed] [Google Scholar]
- 10.Neri T, Boyer B, Geringer J, Di Iorio A, Caton JH, Philippot R, Farizon F. Intraprosthetic dislocation of dual mobility total hip arthroplasty: Still occurring? International Orthopaedics. 2018;42:2733. doi: 10.1007/s00264-018-4107-4. [DOI] [PubMed] [Google Scholar]
- 11.Philippot R, Boyer B, Farizon F. Intraprosthetic dislocation: A specific complication of the dual-mobility system. Clinical Orthopaedics and Related Research. 2013;471:965–970. doi: 10.1007/s11999-012-2639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aslanian T. All dual mobility cups are not the same. International Orthopaedics. 2017;41:573–581. doi: 10.1007/s00264-016-3380-3. [DOI] [PubMed] [Google Scholar]
- 13.Darrith B, Courtney PM, Della Valle CJ. Outcomes of dual mobility components in total hip arthroplasty: A systematic review of the literature. The Bone & Joint Journal. 2018;100-B:11–19. doi: 10.1302/0301-620X.100B1.BJJ-2017-0462.R1. [DOI] [PubMed] [Google Scholar]
- 14.Prock-Gibbs H, Pumilia CA, Meckmongkol T, Lovejoy J, Mumith A, Coathup M. Incidence of osteolysis and aseptic loosening following metal-on-highly cross-linked polyethylene hip arthroplasty: A systematic review of studies with up to 15-year follow-up. Journal of Bone and Joint Surgery. 2021;103(8):728–740. doi: 10.2106/JBJS.20.01086. [DOI] [PubMed] [Google Scholar]
- 15.Loving L, Lee RK, Herrera L, Essner AP, Nevelos JE. Wear performance evaluation of a contemporary dual mobility hip bearing using multiple hip simulator testing conditions. Journal of Arthroplasty. 2013;28:1041–1046. doi: 10.1016/j.arth.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Netter JD, Hermida JC, Chen PC, Nevelos JE, D’Lima DD. Effect of microseparation and third-body particles on dual-mobility crosslinked hip liner wear. Journal of Arthroplasty. 2014;29:1849–1853. doi: 10.1016/j.arth.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Ghaffari M, Nickmanesh R, Tamannaee N, Farahmand F. The impingement-dislocation risk of total hip replacement: Effects of cup orientation and patient maneuvers. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. 2012;2012:6801–6804. doi: 10.1109/EMBC.2012.6347556. [DOI] [PubMed] [Google Scholar]
- 18.Terrier A, Latypova A, Guillemin M, Parvex V, Guyen O. Dual mobility cups provide biomechanical advantages in situations at risk for dislocation: A finite element analysis. International Orthopaedics. 2017;41(3):551–556. doi: 10.1007/s00264-016-3368-z. [DOI] [PubMed] [Google Scholar]
- 19.Jobory A, KärrholmOvergaard JS. Reduced revision risk for dual-mobility cup in total hip replacement due to hip fracture: A matched-pair analysis of 9040 cases from the nordic arthroplasty register association (NARA) Journal of Bone and Joint Surgery. American Volume. 2019;101(14):1278–2128. doi: 10.2106/JBJS.18.00614. [DOI] [PubMed] [Google Scholar]
- 20.Archibeck MJ, Carothers JT, Tripuraneni KR, White RE., Jr Total hip arthroplasty after failed internal fixation of proximal femoral fractures. Journal of Arthroplasty. 2013;28:168–171. doi: 10.1016/j.arth.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 21.Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. Journal of Arthroplasty. 2018;33:1449–1454. doi: 10.1016/j.arth.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD. Spinopelvic mobility and acetabular component position for total hip arthroplasty. The Bone & Joint Journal. 2017;99-B:37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. [DOI] [PubMed] [Google Scholar]
- 23.Nessler JM, Malkani AL, Sachdeva S, Nessler JP, Westrich G, Harwin SF, Mayman D, Jerabek S. Use of dual mobility cups in patients undergoing primary total hip arthroplasty with prior lumbar spine fusion. International Orthopaedics. 2020;44(5):857–862. doi: 10.1007/s00264-020-04507-y. [DOI] [PubMed] [Google Scholar]
- 24.Alosh H, Kamath AF, Baldwin KD, Keenan M, Lee GC. Outcomes of total hip arthroplasty in spastic patients. Journal of Arthroplasty. 2014;29(8):1566–1570. doi: 10.1016/j.arth.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Hernigou P, Filippini P, Flouzat-Lachaniette CH, Batista SU, Poignard A. Constrained liner in neurologic or cognitively impaired patients undergoing primary THA A. Clinical Orthopaedics and Related Research. 2010;468(12):3255–3262. doi: 10.1007/s11999-010-1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fontalis A, Kenanidis E, Bennett-Brown K, Tsiridis E. Clinical outcomes in elective total hip arthroplasty in Parkinson's disease: A systematic review of the literature. EFORT Open Reviews. 2020;5(12):856–865. doi: 10.1302/2058-5241.5.200034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harwin SF, Mistry JB, Chughtai M, Khlopas A, Gwam C, Newman JM, Higuera CA, Bonutti PM, Malkani AL, Kolisek FR, Delanois RE, Mont MA. Dual mobility acetabular cups in primary total hip arthroplasty in patients at high risk for dislocation. Surgical Technology International. 2017;25(30):251–258. [PubMed] [Google Scholar]
- 28.Sanders RJ, Swierstra BA, Goosen JH. The use of a dual-mobility concept in total hip arthroplasty patients with spastic disorders: No dislocations in a series of ten cases at midterm follow-up. Archives of Orthopaedic and Trauma Surgery. 2013;133(7):1011–1016. doi: 10.1007/s00402-013-1759-9. [DOI] [PubMed] [Google Scholar]
- 29.Lazennec JY, Kim Y, Pour AE. Total hip arthroplasty in patients with Parkinson disease: Improved outcomes with dual mobility implants and cementless fixation. Journal of Arthroplasty. 2018;33(5):1455–1461. doi: 10.1016/j.arth.2017.11.062. [DOI] [PubMed] [Google Scholar]
- 30.Abdel MP, Padgett DE. Constrained liners in revision total hip replacement. The Bone & Joint Journal. 2013;95-B:1–4. doi: 10.1302/0301-620X.95B5.30964. [DOI] [Google Scholar]
- 31.Fricka KB, Marshall A, Paprosky WG. Constrained liners in revision total hip arthroplasty: An overuse syndrome: In the affirmative. Journal of Arthroplasty. 2006;21(4 Suppl 1):121–125. doi: 10.1016/j.arth.2006.02.100. [DOI] [PubMed] [Google Scholar]
- 32.Jauregui JJ, Pierce TP, Elmallah RK, Cherian JJ, Delanois RE, Mont MA. Dual mobility cups: An effective prosthesis in revision total hip arthroplasties for preventing dislocations. Hip International. 2016;26:57–61. doi: 10.5301/hipint.5000295. [DOI] [PubMed] [Google Scholar]
- 33.Gonzalez AI, Bartolone P, Lubbeke A, Dupuis Lozeron E, Peter R, HoffmeyerChristofilopoulos PP. Comparison of dual-mobility cup and unipolar cup for prevention of dislocation after revision total hip arthroplasty. Acta Orthopaedica. 2017;88:18–23. doi: 10.1080/17453674.2016.1255482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chalmers BP, Perry KI, Hanssen AD, Pagnano MW, Abdel MP. Conversion of hip hemiarthroplasty to total hip arthroplasty utilizing a dual-mobility construct compared with large femoral heads. Journal of Arthroplasty. 2017;32:3071–3075. doi: 10.1016/j.arth.2017.04.061. [DOI] [PubMed] [Google Scholar]
- 35.Wegrzyn J, Tebaa E, Jacquel A, Carret JP, Bejui-Hugues J, Pibarot V. Can dual mobility cups prevent dislocation in all situations after revision total hip arthroplasty? Journal of Arthroplasty. 2015;30:631–640. doi: 10.1016/j.arth.2014.10.034. [DOI] [PubMed] [Google Scholar]
- 36.Batailler C, Fary C, Verdier R, Aslanian T, Caton J, Lustig S. The evolution of outcomes and indications for the dual-mobility cup: A systematic review. International Orthopaedics. 2017;41(3):645–659. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 37.Addona JL, Gu A, De Martino I, MalahiasSculcoSculco MATPPK. High rate of early intraprosthetic dislocations of dual mobility implants: A single surgeon series of primary and revision total hip replacements. Journal of Arthroplasty. 2019;34(11):2793–2798. doi: 10.1016/j.arth.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 38.Gkiatas I, Sharma AK, Greenberg A, Duncan ST, Chalmers BP, Sculco PK. Serum metal ion levels in modular dual mobility acetabular components: A systematic review. Journal of Orthopaedics. 2020;25(21):432–443. doi: 10.1016/j.jor.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kamath AF, Courtney PM, Lee GC. Metal ion levels with use of modular dual mobility constructs: Can the evidence guide us on clinical use? Journal of Orthopaedics. 2021;20(24):91–95. doi: 10.1016/j.jor.2021.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romero J, Wach A, Silberberg S, Chiu YF, Westrich G, Wright TM, Padgett DE. 2020 Otto Aufranc Award: Malseating of modular dual mobility liners. The Bone & Joint Journal. 2020;102-B(7_Supple_B):20–26. doi: 10.1302/0301-620X.102B7.BJJ-2019-1633.R1. [DOI] [PubMed] [Google Scholar]
- 41.Lygrisse KA, Matzko C, Shah RP, Macaulay W, Cooper JH, Schwarzkopf R, Hepinstall MS. Femoral neck notching in dual mobility implants: Is this a reason for concern? The Journal of Arthroplasty. 2021 doi: 10.1016/j.arth.2021.03.043. [DOI] [PubMed] [Google Scholar]


